Abstract
Type 1 and type 2 diabetes are growing public health problems. Despite having different pathophysiologies, both diseases are associated with defects in immune regulation. Invariant natural killer T (iNKT) cells are innate-like T cells that recognize glycolipids presented by CD1d. These cells not only play a key role in the defense against pathogens, but also exert potent immunoregulatory functions. The regulatory role of iNKT cells in the prevention of type 1 diabetes has been demonstrated in murine models and analyzed in diabetic patients. The decreased frequency of iNKT cells in non-obese diabetic mice initially suggested the regulatory role of this cell subset. Increasing the frequency or the activation of iNKT cells with agonists protects non-obese diabetic mice from the development of diabetes. Several mechanisms mediate iNKT regulatory functions. They can rapidly produce immunoregulatory cytokines, interleukin (IL)-4 and IL-10. They induce tolerogenic dendritic cells, thereby inducing the anergy of autoreactive anti-islet T cells and increasing the frequency of T regulatory cells (Treg cells). Synthetic agonists are able to activate iNKT cells and represent potential therapeutic treatment in order to prevent type 1 diabetes. Growing evidence points to a role of immune system in glucose intolerance and type 2 diabetes. iNKT cells are resident cells of adipose tissue and their local and systemic frequencies are reduced in obese patients, suggesting their involvement in local and systemic inflammation during obesity. With the discovery of potential continuity between type 1 and type 2 diabetes in some patients, the role of iNKT cells in these diseases deserves further investigation.
Keywords: Autoimmunity, Diabetes, Immune regulation, Metabolism, NKT

Type 1 diabetes (T1D) is an autoimmune disease characterized by the selective destruction of pancreatic islet β-cells, in the context of an underlying multigenetic inheritance [1]. When 80% of the β-cells are destroyed, the consecutive lack of insulin results in hyperglycemia and requires a life-long insulin replacement therapy. The physiopathology of T1D is complex and still not entirely understood. It involves both innate and adaptive immune systems; both are inappropriately activated by a triggering event, initiating an immune cascade that results in loss of self-tolerance and islet destruction [2], [3]. T1D is a typical Th1 cell-mediated autoimmune disease characterized by the presence of autoreactive anti-islet T cells, which play a prominent role in the development of the disease [4]. Autoreactive B cells produce autoantibodies targeting β-cell antigens, and could act as antigen-presenting cells (APCs), but have a limited role in the pathophysiology. The emergence of diabetogenic T cells appears to be associated with defective immunoregulation [5]. Numerical and functional deficiencies of CD4+ FoxP3+ T regulatory (Treg) cells have been demonstrated in T1D [6], [7]. However, Treg cells do not account for the entire regulatory functions; another regulatory T cell subset, invariant natural killer T (iNKT) cells, has also been demonstrated to be involved in the pathophysiology of the disease.
Type 2 diabetes (T2D) accounts for over 90% of the diagnosed cases of diabetes. It is a heterogeneous disorder characterized by peripheral insulin resistance, impaired regulation of hepatic glucose production, and β-cell dysfunction. T2D is frequently associated with obesity or overweight, and insulin resistance could be mostly secondary to the coexistence of this increased adiposity [8], [9]. If insulin resistance is present, the β-cells increase insulin output in order to maintain glucose homeostasis. When the β-cells cannot release sufficient insulin, blood glucose concentration rises, leading to glucose intolerance and T2D. As in T1D, genetic factors and environment interact in the development of the disease. In contrast to T1D, genome-wide association studies found that most of the genes implicated in T2D are linked to β-cell function, whereas genes associated with an increased risk of T1D mostly involve the immune system. A link between obesity, systemic inflammation, and metabolic complications has been proposed for decades [9]. Recent studies demonstrated that metabolism and the immune system are strongly associated in the development of obesity-dependent insulin resistance, where both innate and adaptive immune systems play a role.
In this review, we will discuss the role of NKT cells in the pathophysiology of T1D and T2D: protective, pathologic, and still partially mysterious.
iNKT cells
NKT cells are a non-conventional subtype of αβ T lymphocytes. Contrary to conventional αβ T cells that recognize peptides presented by major histocompatibility complex (MHC) molecules, NKT cells recognize lipids presented by CD1d molecules. CD1d is a non-polymorphic MHC class I-like molecule that is mainly expressed by dendritic cells (DCs) and other APCs. The name NKT reflects one of their phenotypical characteristics, as they express cell surface markers associated with the natural killer (NK) cell lineage, and particularly CD161 in humans or NK1.1 in mice [10]. NKT cells are remarkably conserved among mammals, suggesting a crucial role in immunity [11]. Classically, NKT lymphocytes are divided into three groups: iNKT, type II NKT, and NKT-like lymphocytes, according to their antigenic specificity and the expression of their T cell receptor (TCR) [12].
iNKT cells represent the majority of NKT cells. They express a semi-invariant TCR α-chain, Vα24Jα18 in humans and Vα14Jα18 in mice, associated to a restricted set of β-chains, usually Vβ11 in humans and Vβ8, Vβ7, or Vβ2 in mice. They recognize glycosphingolipids that are presented by CD1d, such as glycosylceramides. A glycolipid isolated from a marine sponge, α-galactosylceramide (α-GalCer), has been shown to be a potent activator of iNKT lymphocytes in both mice and humans. iNKT cells are either CD4+ or CD4−CD8− double-negative (DN). iNKT lymphocytes are considered as innate-like T lymphocytes as they harbor an activated/memory phenotype (CD69+, CD44hi, CD62L−), and are rapidly able to produce large amounts of cytokines after the stimulation of their TCR [13]. They can rapidly produce interleukin (IL)-4 and interferon (IFN)-γ, but also have cytotoxic effects. After activation, they interact with both innate and adaptive immune systems, such as NK cells, DCs, T and B cells, through the rapid production of Th1 and Th2 cytokines and the expression of cell surface markers.
Type II NKT lymphocytes display both variable TCR-α and -β chains. These cells do not recognize α-GalCer, but recognize other antigens such as sulfatides and lysophosphatidylcholine and are also restricted by CD1d [14], [15]. NKT-like lymphocytes represent a more heterogeneous population, with variant and invariant TCRs that express NK markers. Among NKT-like is the recently described mucosal associated invariant T (MAIT) cell, which TCR has the invariant Vα7.2-Jα33 chain in humans and Vα19-Jα33 in mice. The ligands of MAIT cells are metabolites from riboflavin synthesis by bacteria, modified by small molecules such as methylglyoxal [16].
iNKT cells are a relatively rare lymphocyte population in humans, as they represent less than 0.1% of peripheral white blood cells. However, the development of Vα14-Jα18 transgenic mice and the improvement of the specific detection of iNKT cells with CD1d–α-GalCer tetramers and 6B11 antibodies have permitted a thorough study of these cells. iNKT cells exert various functions in immunity. They play a key role in the defense against pathogens such as bacteria, viruses, and parasites [11], [17], [18], [19]. They are also involved in defense against tumors and metastases. Although iNKT cells have cytotoxic properties, they are also major players in immune regulation.
Among other immune alterations, a defect of iNKT cells has been observed and correlated with susceptibility to various autoimmune diseases in mice and humans. In lpr C57BL/6 mice, an animal model of systemic lupus erythematosus, the development of autoimmunity is correlated with a decrease of iNKT cell frequency [20], [21]. A defect of frequency and function of iNKT cells was observed in non-obese diabetic (NOD) mice, as discussed below [22], [23]. Similar iNKT cell abnormalities were also described in patients with autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis, and T1D [24], [25], [26], [27], [28].
iNKT cells in T1D
The role of iNKT cells in the physiopathology of T1D has been evidenced in animal models and suggested in humans [12].
iNKT cells in mouse models of T1D
NOD mice, created in Japan in the early 1980s, are one of the most studied animal models of T1D as they spontaneously develop an autoimmune diabetes, very similar to human T1D [3], [6]. Like in human T1D, class II MHC plays a major role with other genetic risk factors as well as with the environment. Infiltration of pancreatic islets by hematopoietic cells, called insulitis, begins at 3–5 weeks of age, causing β-cell destruction, which leads to diabetes at 4–6 months of age, mostly among females [29]. This time delay suggests an immune regulation that is temporarily able to protect β-cells. Characterization of iNKT cells in NOD mice showed reduced frequency and absolute number of iNKT lymphocytes in the thymus and spleen compared to control mice (BALB/c, C57BL/6), as early as 3 weeks of age [22], [30]. These data, demonstrating a very early defect in iNKT cells, first suggested that this population could be involved in the genesis of the pathophysiology of the disease.
A protective role in NOD mice
The protective role of iNKT cells against autoimmune diabetes was demonstrated in different experiments using the NOD mouse model. CD1d-deficient NOD mice, lacking iNKT cells, have a higher risk of developing diabetes and an earlier onset [31]. On the contrary, Vα14-Jα18 transgenic NOD mice, possessing increased number of iNKT cells, present a reduced incidence of diabetes [32]. They present a higher frequency of functional iNKT cells in the spleen, as early as 3 weeks of age, before islet infiltration begins. The level of protection of the different lines of transgenic mice was correlated with the increase in iNKT cell numbers. Islet infiltration at 12 weeks of age was present in transgenic mice and their negative littermates, but was less invasive in transgenic mice, evoking a better immunoregulation. These concordant results suggest that iNKT cells can suppress anti-islet autoreactive T cells.
Transfer experiences demonstrated the regulatory role of iNKT cells. Whereas a co-transfer of Treg cells and BDC2.5 T cells failed to protect NOD Severe Combined Immunodeficiency (SCID) mice from diabetes, the co-transfer of iNKT cells and BDC2.5 T cells or diabetogenic splenocytes from a non-transgenic diabetic NOD mice into NOD SCID recipients induced a strong protection from the disease [32], [33]. Transfer of splenocytes from BDC2.5 Cα−/− mice into Cα−/− NOD mice induced diabetes in 80–100% of recipients, compared to less than 10% when the recipient is a Vα14 Cα−/− NOD mice [34]. The protection afforded by iNKT cells was associated with the inhibition of differentiation of BDC2.5 T cells into effector T cells, and their decreased homing and local accumulation in the pancreas. The immunoregulation of BDC2.5 T cells occurred in pancreatic draining lymph nodes [34] as well as in pancreas [3], [33].
A similar protection was observed after specific stimulation of iNKT cells with their specific ligands, principally α-GalCer. Several groups have demonstrated that repeated injections of the specific iNKT cell ligand α-GalCer decrease insulitis, and protect NOD mice from the development of diabetes, in a CD1d-dependent manner [31], [35]. The treatment is more effective when started early, around the time when insulitis begins [35].
These studies and others have demonstrated the protective role of iNKT cells in T1D mouse models, which involves various regulatory mechanisms.
Regulatory role through immune deviation and cytokines
The presence of anti-islet autoreactive effector Th1 T cells is associated with the development of autoimmune diabetes, whereas a Th2 profile is frequently associated with its protection [3]. In NOD mice, it was evidenced that IL-4 exerts a major negative effect on the progression to diabetes, as systemic administration of IL-4 prevents diabetes onset [36]. If iNKT cells are able to produce various amounts of cytokines, including IFN-γ and Granzyme B, they can also rapidly produce large amounts of IL-4. IL-4 produced by iNKT cells could then play a major role in inhibiting Th1 autoimmune responses and inducing Th2 cell responses to islet antigens in order to protect from diabetes onset, and their defect in T1D could contribute to the pathogenesis of the disease.
Interestingly, iNKT lymphocytes in NOD mice present functional deficiencies, as they produce lower levels of IL-4 after TCR stimulation, as early as 3 weeks of age, compared to control mice (BALB/c, C57BL/6) [22], [30]. The correction of this functional defect by the administration of exogenous IL-4 or by the expression of IL-4 under the control of promoter insulin prevented diabetes in NOD mice. Therefore, the defect in IL-4 production in NOD mice could be responsible, in part, for the emergence of autoreactive anti-islet Th1 cells, leading to the onset of insulitis and diabetes. Indeed, the protection against diabetes in Vα14-Jα18 transgenic NOD mice is not only associated with an increased production of IL-4 in splenocytes, but also in pancreatic islets, and a locally reduced production of IFN-γ within pancreas [32], [37]. This protection is abolished after the administration of antibodies neutralizing IL-4 and IL-10 [37], [38]. Similarly, after in vivo stimulation with α-GalCer, iNKT cells from pancreatic lymph nodes (PLNs) of NOD mice preferentially produce IL-4 [39]. This increase in IL-4 production could be associated with the fact that α-GalCer treatment preferentially expands CD4+ iNKT cells, which produce IL-4 rather than IFN-γ [40].
In parallel, the up-regulation of CD1d expression in pancreatic beta cells as a transgene protected NOD mice from autoimmune diabetes [41]. iNKT cells were not increased in the lymphocyte infiltrates within pancreatic islets, but were slightly increased in the PLNs. Moreover, protection from diabetes was associated with an increase of IL-4 production in the PLNs in these transgenic mice [41].
Other cytokines might be implicated in this immunoregulation process, and surprisingly, some studies showed that IFN-γ is necessary for the protective action of iNKT cells. The regulation of BDC2.5 T cells by NKT cells was lost in a co-transfer experiment in an NOD SCID mice, if the NKT cells were obtained from a NOD Ifng−/− mouse, and also if NKT cells were transferred in an IFN-γ receptor deficient host [33]. These experiments demonstrated that the production of IFN-γ by iNKT cells was necessary to induce regulation by the host, and not on autoreactive T cells. Similarly, upon infection with Coxsackie virus B4, IFN-γ production by iNKT cell induced the expression of indoleamine dioxygenase by macrophages that became suppressive and inhibited pathogenic T cell responses [42]. Thus, iNKT cells modulate APCs and macrophages in an IFN-γ–dependent way, inducing immune regulation.
Several studies highlighted that iNKT cells can also exert an immunoregulatory role through mechanisms independent of cytokine production.
iNKT cells can inhibit the differentiation of autoreactive T cells into effector T cells
There are many evidences that autoreactive T cells are essential for the development and progression of T1D. Several studies tended to demonstrate that T1D could result from defects in negative selection and peripheral tolerance induction [43]. β-cell antigens can be captured by pancreatic APCs that secondarily migrate in PLNs and can activate autoreactive T cells. After activation, autoreactive anti-islet T cells can migrate into the islets [44]. There, they can participate in the destruction of β-cells through different mechanisms: through direct MHC class I-mediated cytotoxicity; through the production of pro-inflammatory cytokines, such as IFN-γ, which induce chemokine production, and by the expression of the death receptor FAS by β-cells. IFN-γ can also activate macrophages, increasing the inflammation in the islets and producing cytokines including IL-1β which can directly induce the apoptosis of β-cells [3].
Our group demonstrated that iNKT lymphocytes could induce anergy of pathogenic T cells. First, we evidenced that iNKT cells prevented diabetes development by inhibiting pancreatic islet inflammation by autoreactive T cells, as Vα14 Cα−/− recipients of BDC2.5 naive T cells presented some levels of peri-insulitis, but less inflammation and β-cell destruction compared to Cα−/− recipients [34]. iNKT cells did not affect the activation and early proliferation of BDC2.5 T cells, but inhibited their differentiation into IFN-γ producing cells and altered their capacity to sustain IL-2 production. At later stages, it appeared that BDC2.5 T cells stimulated in the presence of iNKT cells become anergic. Thus, iNKT cells can protect from diabetes not only through Th2 bias induction but also through the induction of anergy of autoreactive T cells. Lack of IFN-γ production by autoreactive T cells is the key for the protection against diabetes.
Moreover, it was demonstrated that iNKT cells induce the expansion of Treg cells. After transfer of BDC2.5 T cells, Treg cells were found to be more frequent in the PLNs and pancreatic islets of Vα14 Cα−/− recipients compared to Cα−/− recipients [40]. This effect of iNKT cells on the expansion of Treg cells was explored in proinsulin2−/− NOD mice, an animal model developing accelerated diabetes. α-GalCer treatment was demonstrated to induce strong Treg cell expansion both in transferred BDC2.5 T cells and endogenous T cells, in PLNs, and in pancreatic islets [40]. Moreover, these Treg cells were more potent in suppressing naive T cell proliferation. This expansion was not secondary to the proliferation of the initial Treg cell population, but rather to the conversion of naive diabetogenic T cells into Treg cells. The induction of anergy and the conversion of naive T cells into Treg cells are associated with the induction of tolerogenic DCs by iNKT cells.
The dual role of iNKT cells in T1D
Pathogens, particularly viruses, can accelerate the development of T1D, through a pancreatic tropism and the successive inflammatory responses [45]. On the contrary, many studies also described that infections, including viral infections, could induce a protection against T1D [42], [46]. iNKT cells exhibit dual functions, as they are not only able to exert a tolerogenic response in T1D, but also participate in responses against some pathogens. During viral infections, iNKT cells are rapidly activated and promptly produce Th1 cytokines. The question is then: Could iNKT cells exert at the same time an anti-infectious role and a tolerogenic one?
This was studied in the model of diabetes induced by the lymphocyte choriomeningitis virus (LCMV). In this context, iNKT cells not only play an active role in the antiviral response, but also play a major role in the protection against diabetes [46]. All NOD CD1d−/− mice infected with LCMV develop diabetes, whereas only 50% of NOD-infected mice become diabetic and only 10% become diabetic if they are treated with α-GalCer at the time of infection. Thus, the LCMV infection can protect from diabetes in an iNKT-dependent way. After infection, splenic iNKT cells activate conventional DCs (cDCs), which produce IL-12 inducing a strong anti-LCMV CD8+ response, which is necessary for the elimination of the virus. In the pancreas, activated iNKT cells do not interact with cDCs, but rather with plasmacytoid DCs (pDCs). The interaction between iNKT cells and pDCs induces different actions. They promote the recruitment of pDCs in the pancreatic islets and the local production of IFN-α by pDCs, an antiviral cytokine, reducing the viral-induced destruction of β-cells by anti-LCMV CD8 T cells. The activated pDCs then migrate to the PLNs, where they produce transforming growth factor-beta (TGF-β), which induces the conversion of naive T lymphocytes into Foxp3+ Treg cells. Thus, the interactions between iNKT lymphocytes and pDCs both control the viral infection and improve self-tolerance to β-cells, preventing the development of diabetes. The induction of tolerogenic pDCs required the production of IL-10 by iNKT cells and a cell–cell contact through the programmed cell death protein-1 (PD-1), expressed by iNKT cells, and the programmed death-ligand 1 (PD-L1), expressed by pDCs [46].
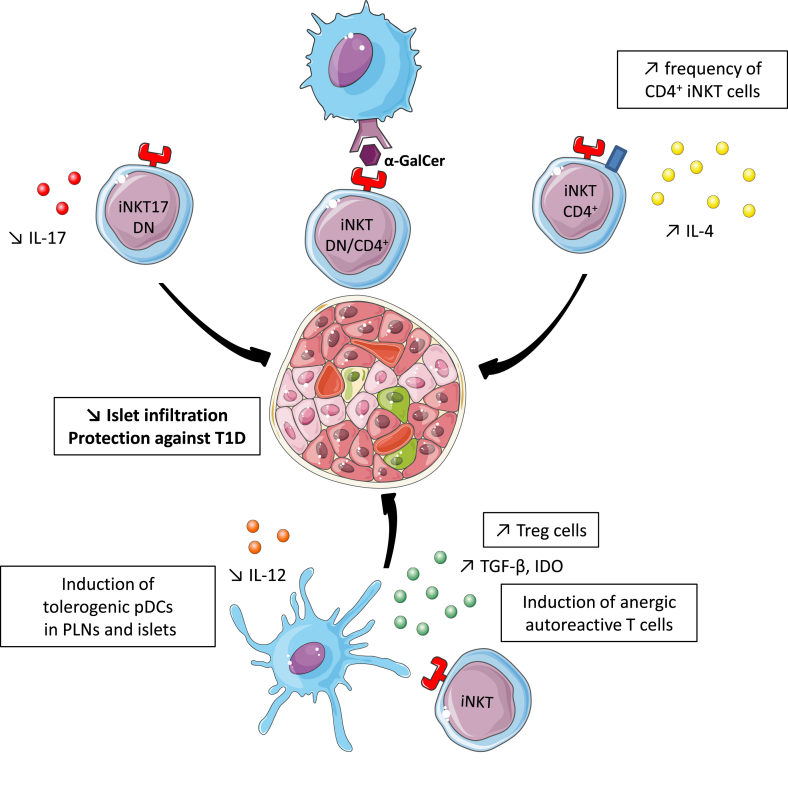
Similarly, α-GalCer treatment induces tolerogenic DCs and pDCs in the PLNs [40], [47]. pDCs produce less IL-12, limiting the Th1 bias, and have a reduced expression of the co-stimulatory receptors CD80 and CD86. Thus, these pDCs can induce a tolerogenic response or anergy. Activated pDCs license Treg cells to migrate into pancreatic islets through the induction of CXCR3 expression. Like in the LCMV model, this conversion is dependent on TGF-β secretion [Fig. 1].
Fig. 1.
α-GalCer treatment protects from type 1 diabetes. After multi-dose α-GalCer injections, the infiltration of pancreatic islets is reduced and NOD mice are protected from diabetes through different mechanisms. α-GalCer preferentially increases CD4+ iNKT cell frequency, the subset producing IL-4. After α-GalCer treatment, iNKT17 cells produce less IL-17. Finally, this treatment induces tolerogenic pDCs in pancreatic islets that secondarily migrate in PLNs. These tolerogenic pDCs, which produce less IL-12 and more TGF-β, favor the anergy of autoreactive T cells and promote the conversion of naive autoreactive T cells into Treg cells.
A pathogenic role of iNKT cells in the development of T1D
IL-17 has recently been shown to be involved in the induction of autoinflammatory and autoimmune diseases [48]. The first identified source of IL-17 was CD4+ T cells that differentiated into Th17 cells. In addition to these CD4+ T cells, recent studies have demonstrated the production of IL-17 by other cell types such as CD8+ T cells and γδ T cells [49], [50]. iNKT cells are divided into subpopulations harboring different cell surface markers and having various functions. A new subset of iNKT cells has recently been described: iNKT17 cells [51], [52]. This population of CD4− NK1.1− iNKT cells produces high level of IL-17 and low levels of IL-4 and IFN-γ after stimulation with its specific ligand. They constitutively express IL-23R and retinoic acid receptor-related orphan receptor γt (RORγt), and IL-1β promotes IL-17 production [53]. Simoni et al. described that iNKT17 cells could play a pathogenic role in the pathophysiology of diabetes [54]. iNKT17 cells are four to six times more frequent in the thymus, spleen, and PLNs from NOD than from C57BL/6 control mice [55]. Moreover, they infiltrate pancreatic islets, and are locally activated as they express IL-17 predominantly in the pancreas in a CD1d-dependent manner [54], [56]. Transfer experiments of iNKT cell subsets revealed the pathogenic role of iNKT17 cells in T1D. Transfer of CD4− NK1.1− iNKT cells, containing iNKT17 cells, into NOD Cα−/− recipients co-transferred with anti-islet BDC2.5 T cells increased the incidence of diabetes. The frequency of BDC2.5 T cells infiltrating the pancreas was increased in mice reconstituted with CD4− iNKT cells. The deleterious effect was abolished after treatment with an anti-IL-17 antibody. In the pancreas, it was demonstrated that IL-17, in collaboration with other cytokines such as IFN-γ and IL-1β, induces inducible nitric oxide synthase (iNOS) expression and NO production. Then, IL-17 produced by iNKT17 cells could interact with IFN-γ produced by BDC2.5 T cells infiltrating the pancreas, inducing the deleterious production of NO in pancreatic β-cells, leading to their death. Thus, the iNKT17 cells exacerbate the incidence of diabetes in NOD mouse models in an IL-17–dependent manner. Interestingly, α-GalCer treatment suppresses the production of IL-17 by iNKT17 cells. Thus, it could be another mechanism by which α-GalCer protects NOD mice from diabetes.
The genetics of iNKT cells
The frequency of iNKT cells is already reduced in the thymus of NOD mice as compared to other strains of mice. The genetic control of iNKT cell numbers has been explored by comparing NOD and C57BL/6 mouse genome. Two loci were identified: Nkt1 and Nkt2. Nkt1 is localized in the same region as one of the NOD mouse lupus susceptibility loci. Nkt2 is located in the same region as Idd13, an NOD-derived diabetes susceptibility locus [57]. This second identified region also includes a peroxisome-associated protein. This finding suggests that peroxisome could play a role in modulating glycolipid availability for CD1d presentation, influencing iNKT cell activation and function [58]. Facciotti et al. demonstrated that mice deficient in peroxysomal enzymes essential for the synthesis of lipids had a significant alteration of iNKT cell frequency and maturation [59].
iNKT cells defects in T1D patients
A challenge in the study of iNKT cells in human blood is their very low frequency, as they often represent less than 0.1% of total peripheral blood lymphocytes. However, the development of CD1d–α-GalCer tetramers and anti-Vα24-Jα18 antibodies (6B11) allowed specific study of iNKT cells in humans [60], [61]. In humans, CD4+ and DN iNKT cells are functionally distinct subsets, with Th2 cytokines being exclusively produced by the CD4+ subset, and they also harbor different patterns of chemokine receptors and integrins, suggesting different migratory properties [60], [62]. Human iNKT cells were demonstrated to be able to induce peripheral tolerance through their interaction with monocytes, inducing their differentiation into myeloid DCs. These myeloid DCs have a tolerogenic phenotype, as they produce IL-10 and little or no IL-12, and do not efficiently activate T lymphocyte proliferation or IFN-γ production [63].
A defect in iNKT cells was observed in diverse autoimmune diseases in humans [24], [25]. However, human studies of iNKT lymphocytes in T1D have yielded contradictory results, with the frequencies of iNKT cells reported as increased, normal, or decreased compared to healthy subjects, and also in terms of functional defects [64]. A defect in iNKT cells in T1D patients was first described in 1998: Wilson et al. reported that among siblings discordant for diabetes, the diabetic siblings had lower frequencies of DN Vα24JαQ+ T cells [65]. Moreover, these Vα24JαQ+ T cells had a Th1 bias, as they lost the ability to secrete IL-4, and mainly produced IFN-γ after anti-CD3 stimulation [65]. Similarly, Kukreja et al. described a reduced frequency of iNKT cells not only among newly diagnosed and long-diagnosed T1D patients, but also in some autoantibody-positive non-diabetic patients, compared to healthy controls, and iNKT cells of diabetic patients produced less IL-4 and also less IFN-γ [26]. This did not seem to be associated with a genetic abnormality of the CD1d gene. Conversely, Lee et al. found no difference in terms of frequency and function of iNKT cells between diabetic patients, whether newly or long diagnosed, and healthy controls [66]. More recently, Roman-Gonzalez et al. found no differences between T1D patients and healthy controls in terms of frequency of iNKT cells, iNKT cell subsets, and production of Th1 or Th2 cytokines [64]. Finally, Li et al. found no differences in the frequency of iNKT cells identified with tetramers between T1D patients and controls, and did not detect iNKT17 cells in the peripheral blood of both groups [56]. However, after expansion with IL-1β, the expanded iNKT cells from T1D patients comprised a higher frequency of iNKT17 cells compared to healthy donors.
The differences found between the studies could be due to the following: the large heterogeneity of iNKT cell frequencies in humans; the low number of patients included; the various methods of detection of iNKT cells, which are not very specific in the early studies; and the different genetic backgrounds, as the studies were conducted in different countries. “Different” T1D could also explain these contradictory results: it progressively appears that there is no one T1D, but probably different types, with different etiologies and different mechanisms leading to anti-islet auto-immunity, which could have various consequences on the homeostasis of iNKT cells. Thus, the role of iNKT cells in the development of human T1D is not yet elucidated.
It would still be interesting to study these cells in the blood of a larger cohort of patients with T1D and to compare the characteristics of these cells at different stages of the disease: before the onset, at recent onset, at early and late follow-up of T1D. Moreover, characterization of the precise autoimmune events happening within pancreatic islets and PLN is difficult in humans. However, the network for pancreatic organ donors with diabetes (nPOD network) allows the study of pancreas, PLNs, and mesenteric lymph nodes from cadaveric organ donors with T1D as well as from those who are islet autoantibody positive, and then could permit the study of iNKT cells in those tissues. In 2005, Kent et al. found that in PLNs, iNKT cells from T1D secrete IFN-γ and little IL-4, whereas iNKT cells from healthy controls produce IL-4 and IFN-γ after TCR activation [67]. This could be further studied, in order to establish if iNKT cell subsets are different in the PLNs of diabetic patients, and could explain the production of different cytokines.
iNKT cells in the prevention of T1D
As Treg cell restoration is a therapeutic approach in T1D, iNKT cells could represent an interesting therapeutic target in order to prevent or cure T1D. As previously described, α-GalCer(C26:0) multi-dose treatment was associated with a protection against diabetes in NOD mice. In humans, α-GalCer loaded on mature DCs has shown some beneficial effects in the protection from cancer [68]. Even though α-GalCer is used in a soluble form to induce tolerogenic effect, other iNKT cell agonists might be more appropriate for therapeutic use in T1D patients. α-GalCer is associated with some side effects in mice: hepatitis and hepatocyte damage, enhanced allergic responses, and exacerbation of atherosclerosis. In addition, a prolonged treatment seemed to be associated with a reduction of iNKT cell frequency in the PLNs and could be associated with a diminished efficacy. Thus, this ligand might not be the most accurate and new iNKT cell agonists are being studied in animal models.
α-GalCer analogs
Structural modifications of α-GalCer influence the type of cytokines produced by iNKT cells. An α-GalCer analog, C16:0, only induces a low production of cytokines, including IL-4, by iNKT cells, but is efficient to protect NOD mice from diabetes [69]. This analog can activate tolerogenic DCs in PLNs and does not transactivate NK cells. Moreover, C16:0 had a rapid kinetic of induction and recovery of iNKT cell anergy. Thus, a thorough study of the action of C16:0 on the development of T1D or of other similar analogs could lead to the discovery of the adequate iNKT cell ligand, which could prevent diabetes.
Increasing the number of iNKT cells
In mice, increased numbers of iNKT cells, through α-GalCer treatment, transgenic models, or through transfer experiments, are associated with protection against diabetes. Therefore, increasing the number of iNKT cells could be a promising strategy in humans.
Some laboratories have developed in vitro methods in order to increase the number of iNKT cells from peripheral blood. A Phase 1 clinical trial showed that the injection of iNKT cells expanded in vitro was well tolerated and without side effects [70]. With this strategy, specific iNKT cell subsets, such as CD4+ iNKT cells, which are protective in NOD mice could be preferentially expanded and other pathogenic subsets, such as iNKT17 cells, could be excluded.
iNKT cells, environment, microbiota, and metabolism
T1D is a multi-hit induced disease, in which genetics and environment interact. The role of environment in the physiopathology of the disease was first suggested by the incomplete concordance in identical twins. As environment plays a key role, the role of the intestinal microbiota in autoimmunity has recently acquired a growing interest, with evidence suggesting its role in various autoimmune diseases, particularly in the development of T1D. The intestinal microbiome represents a complex, symbiotic community that influences human health and immune development. Patients with T1D have an altered microbiota – those who eventually develop T1D have higher levels of Bacteroidetes relative to Firmicutes approximately 6 months after birth, the preceding clinical signs of the disease, suggesting that this ratio of Bacteroidetes to Firmicutes increases in autoimmune cases but declines in those who do not develop the disease [71], [72]. Several human studies revealed mucosal alterations and increased intestinal permeability in diabetic patients, beginning in the preclinical phase of the disease [73]. These alterations could be due to modification of the microbiota composition: bacterial genes associated with the production of short-chain fatty acids and gut integrity are less abundant in autoantibodies-positive cases, with an increased risk for T1D, than in healthy controls [72].
Therefore, we could propose that this modification of the gut microbiota, associated with increased gut permeability could allow the penetration of different glycolipids, which could be ligands of iNKT cells and modulate their activation. This differential activation in patients compared to healthy subjects could modulate iNKT cell proliferation and functions toward exhaustion, and could explain their reduced number and loss of function. Conversely, a recent study performed in mice revealed that sphingolipids produced by a symbiotic microbe, Bacteroides fragilis, inhibit the proliferation of iNKT cells in the gut of newborns and limit their local accumulation [72]. Interestingly, these sphingolipids are more abundant in T1D patients [74]. In humans, during the second trimester of pregnancy, iNKT cells are present and mature in the small intestine, underlining the potential link between gut microbiota and iNKT cell function in humans [75], [76].
On the other hand, recent studies pointed out that microbiota could influence the host metabolism. A recent study by Markle et al. evaluated the impact of gut microbiota in NOD mice on the incidence of diabetes and the host metabolism [77]. Whereas NOD mice display a strong female-to-male bias, germ-free NOD mice have a similar T1D incidence, with males losing their relative protection. The relative protection of NOD males appears to be dependent on the presence of some commensal organisms that increase testosterone levels. Indeed, male and female NOD mice harbor different gut microbiota after puberty. The investigators evaluated the impact of the gut microbiota on serum metabolites. Male and female NOD mice present a distinct cluster of glycerophospholipid and sphingolipid metabolites. A transfer of male microbiota to female recipients increased their testosterone levels, modified the concentration of some glycerophospholipids and sphingolipids, and protected them from diabetes. Moreover, T cells from male microbiota manipulated females had an impaired ability to transfer diabetes.
Thus, we can propose that the altered microbiota among diabetic patients and at-risk patients could influence the host metabolites and modify the proportion of some endogenous glycerophospholipids, some of them being iNKT cell ligands. Thus, alteration of these ligands could reduce iNKT stimulation and proliferation, but could also induce a bias toward IL-17 iNKT, with an ability to promote diabetes.
Type II NKT cells in T1D
The immunoregulatory role of type II NKT cells in various diseases is emerging. Type II NKT cells are CD1d-restricted, but contain a diverse TCR repertoire, and do not recognize α-GalCer but recognize sulfatides. Type II NKT cells appear to be less frequent than iNKT cells in mice, but are more frequent in humans. Their understanding in humans remains limited, but animal models revealed that type II NKT cells are important in antitumor immunity and in the protection against experimental autoimmune encephalomyelitis [14], [78].
Type II NKT cells can prevent the development of T1D. Duarte et al. evidenced that overexpression of CD1d-restricted TCR Vα3.2 and Vβ9, as transgenes in NOD mice, induced a high frequency of type II NKT cells producing high levels of IFN-γ and low levels of IL-4, and led to protection against T1D [79]. It has been proposed that stimulation of type II NKT cells with C24:0 or C24:1 sulfatides multi-dose treatment protected NOD mice from diabetes in a CD1d-dependent manner [80]. The activation of type II NKT cells could inhibit autoreactive diabetogenic T cell proliferation and cytokine production in the PLNs. Type II NKT cells are enriched in PLNs, but no correlation was found between NKT cell numbers and the severity of diabetes [80]. Recently, Kadri et al. identified the mechanism by which type II NKT cells could prevent the development of T1D. In transfer experiments, CD4+ type II NKT cells down-regulated the proliferation and differentiation of diabetogenic BDC2.5 T cells, thereby blocking diabetes development [81]. The PD-1/PD-L1 pathway was essential for the immunoregulatory capacity of type II NKT cells. These results suggest that type II NKT cells represent potential therapeutic targets to prevent T1D in humans.
iNKT cells in T2D
Converging studies unraveled the interactions between immune system and metabolic abnormalities in T2D. In lean state, macrophages are present within the adipose tissue, presenting an anti-inflammatory phenotype that is referred to as M2. Their differentiation and survival depends on IL-4 and IL-13 [82]. During the development of obesity, they expand and also switch toward an M1 pro-inflammatory phenotype. M2 macrophages promote local and systemic insulin sensitivity, while M1 macrophages contribute to insulin resistance through different pathways, for example, tumor necrosis factor-alpha (TNF-α) produced by M1 macrophages inhibits insulin-receptor signaling and impairs adipokine secretion [83].
Recently, there has been a growing interest in the other players of both innate and adaptive immune systems in obesity and metabolic diseases. As iNKT cells have been shown to be resident cells of adipose tissue and to recognize glycolipids, they have been proposed to play a role in obesity-induced inflammation and insulin resistance [84]. The ability of iNKT cells to produce IL-4 could contribute to the activation of M2 macrophages. In obese patients, omental and circulating iNKT cell frequencies were lower than in healthy controls [84]. Thus, the lack of iNKT cells could favor the switch of macrophages toward M1 phenotype. Experiments in animal models have led to contradictory results. Lynch et al. reported that iNKT cell number is restored in the adipose tissue after weight loss in humans and mice [85]. Mice lacking iNKT cells show improved weight gain and insulin resistance on a high-fat diet, whereas adoptive transfer of iNKT cells into obese mice or in vivo specific stimulation of iNKT cells with α-GalCer decreases body fat and restores insulin sensitivity [85]. Moreover, Lynch et al. recently showed that iNKT cells in adipose tissue produce IL-2, which increases Treg cell frequency. These Treg cells produce IL-10 promoting the differentiation of M2 macrophages [86]. Interestingly, Schipper et al. described the beneficial role of iNKT cells against insulin resistance in low-fat diet [87]. In contrast, Ohmura et al. found opposite results: β2-microglobulin knock-out mice lacking NKT cells presented reduced macrophage infiltration in the adipose tissue and a better glucose tolerance, compared to control mice, whereas α-GalCer injections exacerbated glucose intolerance and macrophage infiltration. According to Mantell et al., NKT cell depletion in CD1d−/− mice on a high-fat diet was not associated with an improved outcome in terms of body weight and glucose tolerance, compared to wild-type littermate controls [88], [89]. These different experiments use different protocols and different knock-out animal models.
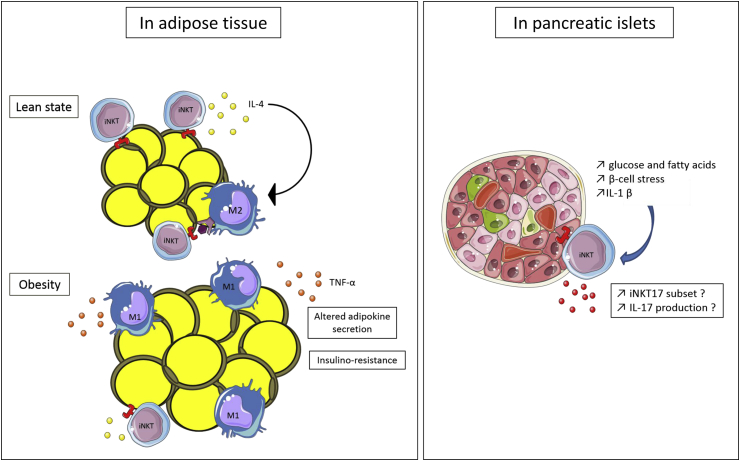
Glucose and fatty acids increase the production of IL-1β in pancreatic islets. The stress of β-cells following the need for an increased insulin output could favor β-cell death and a certain process of autoimmunity. iNKT cells could then have a role as immunoregulators within the islets. Interestingly, in the study of Simoni et al. about iNKT17 cells, where the production of IL-17 by this subset seemed CD1d dependent, a residual expression of IL-17 persisted in the absence of peripheral CD1d expression [54]. This suggested that local factors, such as IL-1β, could participate in the activation of iNKT17 cells. Moreover, Li et al. demonstrated that IL-1β was able to expand iNKT cells from the blood of T1D and T2D patients and healthy donors, and preferentially expanded iNKT17 cells from T1D patients [56]. Therefore, the presence of IL-1β within the inflamed islets during obesity and T2D could favor the expansion and activation of iNKT17 cells and promote the recruitment of auto-reactive T cells within the islets [Fig. 2].
Fig. 2.
The possible role of iNKT cells in the pathophysiology of type 2 diabetes. iNKT cells are present in lean adipose tissue and produce IL-4. This could favor the M2 anti-inflammatory phenotype of resident macrophages. During obesity, macrophages accumulate in the adipose tissue and iNKT cell frequency is reduced. The lack of IL-4, among other mechanisms, could participate in the switch of macrophages toward M1 pro-inflammatory phenotype that induces insulin resistance. In pancreatic islets, the increased concentration of glucose and fatty acids induces local inflammation and the production of IL-1β. This cytokine could activate iNKT cells, preferentially the iNKT17 cell subset, which then contribute to β-cell destruction.
Conclusion
This review highlights the regulatory role of iNKT cells and the emerging role of type II NKT cells in diabetes. Investigations in NOD mice have demonstrated the central role of iNKT cells in the pathogenesis of T1D. Furthermore, new insights into the role of microbiota and the interactions between metabolism and the immune system suggest possible interactions with NKT cells. The different results obtained in the human studies underline the requirement for further studies, using specific recognition of iNKT cells, in peripheral blood and tissues. New advances in the study of these cells and the selection of new agonists should permit the development of new therapeutic strategies in order to prevent the development of T1D and T2D, diseases with a growing incidence.
Source of support
The laboratory is supported by funds from INSERM, CNRS, ANR-2014 OBEMAIT, Fondation pour la Recherche Medicale no. DEQ20140329520, ANR-11-IDEX-0005-02 Laboratoire d’Excellence INFLAMEX, Universite Paris Descartes. Celine Tard was supported by a fellowship from Fondation pour la Recherche Medicale. Ophelie Rouxel is supported by doctoral fellowship from the Ministere de l’Education Nationale.
Conflict of interest
None declared.
Acknowledgments
The authors wish to thank Servier Medical Art for providing some of the illustrations used in this paper.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Atkinson M.A., Eisenbarth G.S., Michels A.W. Type 1 diabetes. Lancet. 2014;383:69–82. doi: 10.1016/S0140-6736(13)60591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diana J., Simoni Y., Furio L., Beaudoin L., Agerberth B., Barrat F. Crosstalk between neutrophils, B-1a cells and plasmacytoid dendritic cells initiates autoimmune diabetes. Nat Med. 2013;19:65–73. doi: 10.1038/nm.3042. [DOI] [PubMed] [Google Scholar]
- 3.Lehuen A., Diana J., Zaccone P., Cooke A. Immune cell crosstalk in type 1 diabetes. Nat Rev Immunol. 2010;10:501–513. doi: 10.1038/nri2787. [DOI] [PubMed] [Google Scholar]
- 4.Willcox A., Richardson S.J., Bone A.J., Foulis A.K., Morgan N.G. Analysis of islet inflammation in human type 1 diabetes. Clin Exp Immunol. 2009;155:173–181. doi: 10.1111/j.1365-2249.2008.03860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delovitch T.L., Singh B. The nonobese diabetic mouse as a model of autoimmune diabetes: immune dysregulation gets the NOD. Immunity. 1997;7:727–738. doi: 10.1016/s1074-7613(00)80392-1. [DOI] [PubMed] [Google Scholar]
- 6.Anderson M.S., Bluestone J.A. The NOD mouse: a model of immune dysregulation. Annu Rev Immunol. 2005;23:447–485. doi: 10.1146/annurev.immunol.23.021704.115643. [DOI] [PubMed] [Google Scholar]
- 7.Zhen Y., Sun L., Liu H., Duan K., Zeng C., Zhang L. Alterations of peripheral CD4+CD25+Foxp3+ T regulatory cells in mice with STZ-induced diabetes. Cell Mol Immunol. 2012;9:75–85. doi: 10.1038/cmi.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahler R.J., Adler M.L. Clinical review 102: type 2 diabetes mellitus: update on diagnosis, pathophysiology, and treatment. J Clin Endocrinol Metab. 1999;84:1165–1171. doi: 10.1210/jcem.84.4.5612. [DOI] [PubMed] [Google Scholar]
- 9.Kahn S.E., Cooper M.E., Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014;383:1068–1083. doi: 10.1016/S0140-6736(13)62154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bendelac A., Rivera M.N., Park S.H., Roark J.H. Mouse CD1-specific NK1 T cells: development, specificity, and function. Annu Rev Immunol. 1997;15:535–562. doi: 10.1146/annurev.immunol.15.1.535. [DOI] [PubMed] [Google Scholar]
- 11.Bendelac A., Savage P.B., Teyton L. The biology of NKT cells. Annu Rev Immunol. 2007;25:297–336. doi: 10.1146/annurev.immunol.25.022106.141711. [DOI] [PubMed] [Google Scholar]
- 12.Simoni Y., Diana J., Ghazarian L., Beaudoin L., Lehuen A. Therapeutic manipulation of natural killer (NK) T cells in autoimmunity: are we close to reality? Clin Exp Immunol. 2013;171:8–19. doi: 10.1111/j.1365-2249.2012.04625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kronenberg M., Gapin L. The unconventional lifestyle of NKT cells. Nat Rev Immunol. 2002;2:557–568. doi: 10.1038/nri854. [DOI] [PubMed] [Google Scholar]
- 14.Jahng A., Maricic I., Aguilera C., Cardell S., Halder R.C., Kumar V. Prevention of autoimmunity by targeting a distinct, noninvariant CD1d-reactive T cell population reactive to sulfatide. J Exp Med. 2004;199:947–957. doi: 10.1084/jem.20031389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arrenberg P., Halder R., Dai Y., Maricic I., Kumar V. Oligoclonality and innate-like features in the TCR repertoire of type II NKT cells reactive to a beta-linked self-glycolipid. Proc Natl Acad Sci U S A. 2010;107:10984–10989. doi: 10.1073/pnas.1000576107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Treiner E., Duban L., Bahram S., Radosavljevic M., Wanner V., Tilloy F. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422:164–169. doi: 10.1038/nature01433. [DOI] [PubMed] [Google Scholar]
- 17.Diana J., Lehuen A. NKT cells: friend or foe during viral infections? Eur J Immunol. 2009;39:3283–3291. doi: 10.1002/eji.200939800. [DOI] [PubMed] [Google Scholar]
- 18.Tupin E., Kinjo Y., Kronenberg M. The unique role of natural killer T cells in the response to microorganisms. Nat Rev Microbiol. 2007;5:405–417. doi: 10.1038/nrmicro1657. [DOI] [PubMed] [Google Scholar]
- 19.Cohen N.R., Garg S., Brenner M.B. Antigen presentation by CD1 lipids, T cells, and NKT cells in microbial immunity. Adv Immunol. 2009;102:1–94. doi: 10.1016/S0065-2776(09)01201-2. [DOI] [PubMed] [Google Scholar]
- 20.Mieza M.A., Itoh T., Cui J.Q., Makino Y., Kawano T., Tsuchida K. Selective reduction of V alpha 14+ NK T cells associated with disease development in autoimmune-prone mice. J Immunol. 1996;156:4035–4040. [PubMed] [Google Scholar]
- 21.Takeda K., Dennert G. The development of autoimmunity in C57BL/6 lpr mice correlates with the disappearance of natural killer type 1-positive cells: evidence for their suppressive action on bone marrow stem cell proliferation, B cell immunoglobulin secretion, and autoimmune symptoms. J Exp Med. 1993;177:155–164. doi: 10.1084/jem.177.1.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gombert J.M., Herbelin A., Tancrède-Bohin E., Dy M., Carnaud C., Bach J.F. Early quantitative and functional deficiency of NK1+-like thymocytes in the NOD mouse. Eur J Immunol. 1996;26:2989–2998. doi: 10.1002/eji.1830261226. [DOI] [PubMed] [Google Scholar]
- 23.Hammond K.J., Pellicci D.G., Poulton L.D., Naidenko O.V., Scalzo A.A., Baxter A.G. CD1d-restricted NKT cells: an interstrain comparison. J Immunol. 2001;167:1164–1173. doi: 10.4049/jimmunol.167.3.1164. [DOI] [PubMed] [Google Scholar]
- 24.Kojo S., Adachi Y., Keino H., Taniguchi M., Sumida T. Dysfunction of T cell receptor AV24AJ18+, BV11+ double-negative regulatory natural killer T cells in autoimmune diseases. Arthritis Rheum. 2001;44:1127–1138. doi: 10.1002/1529-0131(200105)44:5<1127::AID-ANR194>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 25.Illés Z., Kondo T., Newcombe J., Oka N., Tabira T., Yamamura T. Differential expression of NK T cell V alpha 24J alpha Q invariant TCR chain in the lesions of multiple sclerosis and chronic inflammatory demyelinating polyneuropathy. J Immunol. 2000;164:4375–4381. doi: 10.4049/jimmunol.164.8.4375. [DOI] [PubMed] [Google Scholar]
- 26.Kukreja A., Cost G., Marker J., Zhang C., Sun Z., Lin-Su K. Multiple immuno-regulatory defects in type-1 diabetes. J Clin Invest. 2002;109:131–140. doi: 10.1172/JCI13605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sumida T., Sakamoto A., Murata H., Makino Y., Takahashi H., Yoshida S. Selective reduction of T cells bearing invariant V alpha 24J alpha Q antigen receptor in patients with systemic sclerosis. J Exp Med. 1995;182:1163–1168. doi: 10.1084/jem.182.4.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van der Vliet H.J., von Blomberg B.M., Nishi N., Reijm M., Voskuyl A.E., van Bodegraven A.A. Circulating V(alpha24+) Vbeta11+ NKT cell numbers are decreased in a wide variety of diseases that are characterized by autoreactive tissue damage. Clin Immunol. 2001;100:144–148. doi: 10.1006/clim.2001.5060. [DOI] [PubMed] [Google Scholar]
- 29.Kikutani H., Makino S. The murine autoimmune diabetes model: NOD and related strains. Adv Immunol. 1992;51:285–322. doi: 10.1016/s0065-2776(08)60490-3. [DOI] [PubMed] [Google Scholar]
- 30.Godfrey D.I., Kinder S.J., Silvera P., Baxter A.G. Flow cytometric study of T cell development in NOD mice reveals a deficiency in alphabetaTCR+CDR-CD8- thymocytes. J Autoimmun. 1997;10:279–285. doi: 10.1006/jaut.1997.0129. [DOI] [PubMed] [Google Scholar]
- 31.Wang B., Geng Y.B., Wang C.R. CD1-restricted NK T cells protect nonobese diabetic mice from developing diabetes. J Exp Med. 2001;194:313–320. doi: 10.1084/jem.194.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lehuen A., Lantz O., Beaudoin L., Laloux V., Carnaud C., Bendelac A. Overexpression of natural killer T cells protects Valpha14- Jalpha281 transgenic nonobese diabetic mice against diabetes. J Exp Med. 1998;188:1831–1839. doi: 10.1084/jem.188.10.1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cain J.A., Smith J.A., Ondr J.K., Wang B., Katz J.D. NKT cells and IFN-gamma establish the regulatory environment for the control of diabetogenic T cells in the nonobese diabetic mouse. J Immunol. 2006;176:1645–1654. doi: 10.4049/jimmunol.176.3.1645. [DOI] [PubMed] [Google Scholar]
- 34.Beaudoin L., Laloux V., Novak J., Lucas B., Lehuen A. NKT cells inhibit the onset of diabetes by impairing the development of pathogenic T cells specific for pancreatic beta cells. Immunity. 2002;17:725–736. doi: 10.1016/s1074-7613(02)00473-9. [DOI] [PubMed] [Google Scholar]
- 35.Sharif S., Arreaza G.A., Zucker P., Mi Q.S., Sondhi J., Naidenko O.V. Activation of natural killer T cells by alpha-galactosylceramide treatment prevents the onset and recurrence of autoimmune Type 1 diabetes. Nat Med. 2001;7:1057–1062. doi: 10.1038/nm0901-1057. [DOI] [PubMed] [Google Scholar]
- 36.Rapoport M.J., Jaramillo A., Zipris D., Lazarus A.H., Serreze D.V., Leiter E.H. Interleukin 4 reverses T cell proliferative unresponsiveness and prevents the onset of diabetes in nonobese diabetic mice. J Exp Med. 1993;178:87–99. doi: 10.1084/jem.178.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laloux V., Beaudoin L., Jeske D., Carnaud C., Lehuen A.N.K. T cell-induced protection against diabetes in V alpha 14-J alpha 281 transgenic nonobese diabetic mice is associated with a Th2 shift circumscribed regionally to the islets and functionally to islet autoantigen. J Immunol. 2001;166:3749–3756. doi: 10.4049/jimmunol.166.6.3749. [DOI] [PubMed] [Google Scholar]
- 38.Hammond K.J., Poulton L.D., Palmisano L.J., Silveira P.A., Godfrey D.I., Baxter A.G. alpha/beta-T cell receptor (TCR)+CD4-CD8- (NKT) thymocytes prevent insulin-dependent diabetes mellitus in nonobese diabetic (NOD)/Lt mice by the influence of interleukin (IL)-4 and/or IL-10. J Exp Med. 1998;187:1047–1056. doi: 10.1084/jem.187.7.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laloux V., Beaudoin L., Ronet C., Lehuen A. Phenotypic and functional differences between NKT cells colonizing splanchnic and peripheral lymph nodes. J Immunol Balt. 2002;168:3251–3258. doi: 10.4049/jimmunol.168.7.3251. [DOI] [PubMed] [Google Scholar]
- 40.Beaudoin L., Diana J., Ghazarian L., Simoni Y., Boitard C., Lehuen A. Plasmacytoid dendritic cells license regulatory T cells, upon iNKT-cell stimulation, to prevent autoimmune diabetes. Eur J Immunol. 2014;44:1454–1466. doi: 10.1002/eji.201343910. [DOI] [PubMed] [Google Scholar]
- 41.Falcone M., Facciotti F., Ghidoli N., Monti P., Olivieri S., Zaccagnino L. Up-regulation of CD1d expression restores the immunoregulatory function of NKT cells and prevents autoimmune diabetes in nonobese diabetic mice. J Immunol Balt. 2004;172:5908–5916. doi: 10.4049/jimmunol.172.10.5908. [DOI] [PubMed] [Google Scholar]
- 42.Ghazarian L., Diana J., Beaudoin L., Larsson P.G., Puri R.K., van Rooijen N. Protection against type 1 diabetes upon Coxsackievirus B4 infection and iNKT-cell stimulation: role of suppressive macrophages. Diabetes. 2013;62:3785–3796. doi: 10.2337/db12-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen G., Han G., Wang J., Wang R., Xu R., Shen B. Natural killer cells modulate overt autoimmunity to homeostasis in nonobese diabetic mice after anti-CD3 F(ab')2 antibody treatment through secreting transforming growth factor-β. Am J Pathol. 2009;175:1086–1094. doi: 10.2353/ajpath.2009.080488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Höglund P., Mintern J., Waltzinger C., Heath W., Benoist C., Mathis D. Initiation of autoimmune diabetes by developmentally regulated presentation of islet cell antigens in the pancreatic lymph nodes. J Exp Med. 1999;189:331–339. doi: 10.1084/jem.189.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ghazarian L., Diana J., Simoni Y., Beaudoin L., Lehuen A. Prevention or acceleration of type 1 diabetes by viruses. Cell Mol Life Sci. 2013;70:239–255. doi: 10.1007/s00018-012-1042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diana J., Brezar V., Beaudoin L., Dalod M., Mellor A., Tafuri A. Viral infection prevents diabetes by inducing regulatory T cells through NKT cell-plasmacytoid dendritic cell interplay. J Exp Med. 2011;208:729–745. doi: 10.1084/jem.20101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Y.G., Choisy-Rossi C.-M., Holl T.M., Chapman H.D., Besra G.S., Porcelli S.A. Activated NKT cells inhibit autoimmune diabetes through tolerogenic recruitment of dendritic cells to pancreatic lymph nodes. J Immunol. 2005;174:1196–1204. doi: 10.4049/jimmunol.174.3.1196. [DOI] [PubMed] [Google Scholar]
- 48.Spolski R., Leonard W.J. Cytokine mediators of Th17 function. Eur J Immunol. 2009;39:658–661. doi: 10.1002/eji.200839066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Happel K.I., Zheng M., Young E., Quinton L.J., Lockhart E., Ramsay A.J. Cutting edge: roles of Toll-like receptor 4 and IL-23 in IL-17 expression in response to Klebsiella pneumoniae infection. J Immunol Balt. 2003;170:4432–4436. doi: 10.4049/jimmunol.170.9.4432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shibata K., Yamada H., Hara H., Kishihara K., Yoshikai Y. Resident Vdelta1+ gammadelta T cells control early infiltration of neutrophils after Escherichia coli infection via IL-17 production. J Immunol. 2007;178:4466–4472. doi: 10.4049/jimmunol.178.7.4466. [DOI] [PubMed] [Google Scholar]
- 51.Doisne J.M., Becourt C., Amniai L., Duarte N., Le Luduec J.B., Eberl G. Skin and peripheral lymph node invariant NKT cells are mainly retinoic acid receptor-related orphan receptor (gamma)t+ and respond preferentially under inflammatory conditions. J Immunol Balt. 2009;183:2142–2149. doi: 10.4049/jimmunol.0901059. [DOI] [PubMed] [Google Scholar]
- 52.Michel M.L., Keller A.C., Paget C., Fujio M., Trottein F., Savage P.B. Identification of an IL-17-producing NK1.1(neg) iNKT cell population involved in airway neutrophilia. J Exp Med. 2007;204:995–1001. doi: 10.1084/jem.20061551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Doisne J.M., Soulard V., Bécourt C., Amniai L., Henrot P., Havenar-Daughton C. Cutting edge: crucial role of IL-1 and IL-23 in the innate IL-17 response of peripheral lymph node NK1.1- invariant NKT cells to bacteria. J Immunol Balt. 2011;186:662–666. doi: 10.4049/jimmunol.1002725. [DOI] [PubMed] [Google Scholar]
- 54.Simoni Y., Gautron A.S., Beaudoin L., Bui L.C., Michel M.L., Coumoul X. NOD mice contain an elevated frequency of iNKT17 cells that exacerbate diabetes. Eur J Immunol. 2011;41:3574–3585. doi: 10.1002/eji.201141751. [DOI] [PubMed] [Google Scholar]
- 55.Ghazarian L., Simoni Y., Magalhaes I., Lehuen A. Invariant NKT cell development: focus on NOD mice. Curr Opin Immunol. 2014;27:83–88. doi: 10.1016/j.coi.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 56.Li S., Joseph C., Becourt C., Klibi J., Luce S., Dubois-Laforgue D. Potential role of IL-17-producing iNKT cells in type 1 diabetes. PloS One. 2014;9:e96151. doi: 10.1371/journal.pone.0096151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Esteban L.M., Tsoutsman T., Jordan M.A., Roach D., Poulton L.D., Brooks A. Genetic control of NKT cell numbers maps to major diabetes and lupus loci. J Immunol Balt. 2003;171:2873–2878. doi: 10.4049/jimmunol.171.6.2873. [DOI] [PubMed] [Google Scholar]
- 58.Fletcher J.M., Jordan M.A., Snelgrove S.L., Slattery R.M., Dufour F.D., Kyparissoudis K. Congenic analysis of the NKT cell control gene Nkt2 implicates the peroxisomal protein Pxmp4. J Immunol Balt. 2008;181:3400–3412. doi: 10.4049/jimmunol.181.5.3400. [DOI] [PubMed] [Google Scholar]
- 59.Facciotti F., Ramanjaneyulu G.S., Lepore M., Sansano S., Cavallari M., Kistowska M. Peroxisome-derived lipids are self antigens that stimulate invariant natural killer T cells in the thymus. Nat Immunol. 2012;13:474–480. doi: 10.1038/ni.2245. [DOI] [PubMed] [Google Scholar]
- 60.Gumperz J.E., Miyake S., Yamamura T., Brenner M.B. Functionally distinct subsets of CD1d-restricted natural killer T cells revealed by CD1d tetramer staining. J Exp Med. 2002;195:625–636. doi: 10.1084/jem.20011786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Montoya C.J., Pollard D., Martinson J., Kumari K., Wasserfall C., Mulder C.B. Characterization of human invariant natural killer T subsets in health and disease using a novel invariant natural killer T cell-clonotypic monoclonal antibody, 6B11. Immunology. 2007;122:1–14. doi: 10.1111/j.1365-2567.2007.02647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee P.T., Benlagha K., Teyton L., Bendelac A. Distinct functional lineages of human V(alpha)24 natural killer T cells. J Exp Med. 2002;195:637–641. doi: 10.1084/jem.20011908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hegde S., Lockridge J.L., Becker Y.A., Ma S., Kenney S.C., Gumperz J.E. Human NKT cells direct the differentiation of myeloid APCs that regulate T cell responses via expression of programmed cell death ligands. J Autoimmun. 2011;37:28–38. doi: 10.1016/j.jaut.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roman-Gonzalez A., Moreno M.E., Alfaro J.M., Uribe F., Latorre-Sierra G., Rugeles M.T. Frequency and function of circulating invariant NKT cells in autoimmune diabetes mellitus and thyroid diseases in Colombian patients. Hum Immunol. 2009;70:262–268. doi: 10.1016/j.humimm.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 65.Wilson S.B., Kent S.C., Patton K.T., Orban T., Jackson R.A., Exley M. Extreme Th1 bias of invariant Valpha24JalphaQ T cells in type 1 diabetes. Nature. 1998;391:177–181. doi: 10.1038/34419. [DOI] [PubMed] [Google Scholar]
- 66.Lee P.T., Putnam A., Benlagha K., Teyton L., Gottlieb P.A., Bendelac A. Testing the NKT cell hypothesis of human IDDM pathogenesis. J Clin Invest. 2002;110:793–800. doi: 10.1172/JCI15832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kent S.C., Chen Y., Clemmings S.M., Viglietta V., Kenyon N.S., Ricordi C. Loss of IL-4 secretion from human type 1a diabetic pancreatic draining lymph node NKT cells. J Immunol Balt. 2005;175:4458–4464. doi: 10.4049/jimmunol.175.7.4458. [DOI] [PubMed] [Google Scholar]
- 68.Chang D.H., Osman K., Connolly J., Kukreja A., Krasovsky J., Pack M. Sustained expansion of NKT cells and antigen-specific T cells after injection of alpha-galactosyl-ceramide loaded mature dendritic cells in cancer patients. J Exp Med. 2005;201:1503–1517. doi: 10.1084/jem.20042592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blumenfeld H.J., Tohn R., Haeryfar S.M., Liu Y., Savage P.B., Delovitch T.L. Structure-guided design of an invariant natural killer T cell agonist for optimum protection from type 1 diabetes in non-obese diabetic mice. Clin Exp Immunol. 2011;166:121–133. doi: 10.1111/j.1365-2249.2011.04454.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Motohashi S., Ishikawa A., Ishikawa E., Otsuji M., Iizasa T., Hanaoka H. A phase I study of in vitro expanded natural killer T cells in patients with advanced and recurrent non-small cell lung cancer. Clin Cancer Res. 2006;12:6079–6086. doi: 10.1158/1078-0432.CCR-06-0114. [DOI] [PubMed] [Google Scholar]
- 71.Giongo A., Gano K.A., Crabb D.B., Mukherjee N., Novelo L.L., Casella G. Toward defining the autoimmune microbiome for type 1 diabetes. ISME J. 2011;5:82–91. doi: 10.1038/ismej.2010.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brown C.T., Davis-Richardson A.G., Giongo A., Gano K.A., Crabb D.B., Mukherjee N. Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PloS One. 2011;6:e25792. doi: 10.1371/journal.pone.0025792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sorini C., Falcone M. Shaping the (auto)immune response in the gut: the role of intestinal immune regulation in the prevention of type 1 diabetes. Am J Clin Exp Immunol. 2013;2:156–171. [PMC free article] [PubMed] [Google Scholar]
- 74.Kostic A.D., Gevers D., Siljander H., Vatanen T., Hyötyläinen T., Hämäläinen A.M. The dynamics of the human infant gut microbiome in development and in progression toward type 1 diabetes. Cell Host Microbe. 2015;17:260–273. doi: 10.1016/j.chom.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Loh L., Ivarsson M.A., Michaëlsson J., Sandberg J.K., Nixon D.F. Invariant natural killer T cells developing in the human fetus accumulate and mature in the small intestine. Mucosal Immunol. 2014;7:1233–1243. doi: 10.1038/mi.2014.13. [DOI] [PubMed] [Google Scholar]
- 76.Zeissig S., Blumberg R.S. Commensal microbiota and NKT cells in the control of inflammatory diseases at mucosal surfaces. Curr Opin Immunol. 2013;25:690–696. doi: 10.1016/j.coi.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Markle J.G., Frank D.N., Mortin-Toth S., Robertson C.E., Feazel L.M., Rolle-Kampczyk U. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013;339:1084–1088. doi: 10.1126/science.1233521. [DOI] [PubMed] [Google Scholar]
- 78.Terabe M., Swann J., Ambrosino E., Sinha P., Takaku S., Hayakawa Y. A nonclassical non-Valpha14Jalpha18 CD1d-restricted (type II) NKT cell is sufficient for down-regulation of tumor immunosurveillance. J Exp Med. 2005;202:1627–1633. doi: 10.1084/jem.20051381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Duarte N., Stenström M., Campino S., Bergman M.L., Lundholm M., Holmberg D. Prevention of diabetes in nonobese diabetic mice mediated by CD1d-restricted nonclassical NKT cells. J Immunol Balt. 2004;173:3112–3118. doi: 10.4049/jimmunol.173.5.3112. [DOI] [PubMed] [Google Scholar]
- 80.Subramanian L., Blumenfeld H., Tohn R., Ly D., Aguilera C., Maricic I. NKT cells stimulated by long fatty acyl chain sulfatides significantly reduce the incidence of type 1 diabetes in nonobese diabetic mice [corrected] PloS One. 2012;7:e37771. doi: 10.1371/journal.pone.0037771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kadri N., Korpos E., Gupta S., Briet C., Löfbom L., Yagita H. CD4(+) type II NKT cells mediate ICOS and programmed death-1-dependent regulation of type 1 diabetes. J Immunol Balt. 2012;188:3138–3149. doi: 10.4049/jimmunol.1101390. [DOI] [PubMed] [Google Scholar]
- 82.Mathis D. Immunological goings-on in visceral adipose tissue. Cell Metab. 2013;17:851–859. doi: 10.1016/j.cmet.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tateya S., Kim F., Tamori Y. Recent advances in obesity-induced inflammation and insulin resistance. Front Endocrinol (Lausanne) 2013;4:93. doi: 10.3389/fendo.2013.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lynch L., O'Shea D., Winter D.C., Geoghegan J., Doherty D.G., O'Farrelly C. Invariant NKT cells and CD1d(+) cells amass in human omentum and are depleted in patients with cancer and obesity. Eur J Immunol. 2009;39:1893–1901. doi: 10.1002/eji.200939349. [DOI] [PubMed] [Google Scholar]
- 85.Lynch L., Nowak M., Varghese B., Clark J., Hogan A.E., Toxavidis V. Adipose tissue invariant NKT cells protect against diet-induced obesity and metabolic disorder through regulatory cytokine production. Immunity. 2012;37:574–587. doi: 10.1016/j.immuni.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lynch L., Michelet X., Zhang S., Brennan P.J., Moseman A., Lester C. Regulatory iNKT cells lack expression of the transcription factor PLZF and control the homeostasis of T(reg) cells and macrophages in adipose tissue. Nat Immunol. 2015;16:85–95. doi: 10.1038/ni.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schipper H.S., Rakhshandehroo M., van de Graaf S.F.J., Venken K., Koppen A., Stienstra R. Natural killer T cells in adipose tissue prevent insulin resistance. J Clin Invest. 2012;122:3343–3354. doi: 10.1172/JCI62739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ohmura K., Ishimori N., Ohmura Y., Tokuhara S., Nozawa A., Horii S. Natural killer T cells are involved in adipose tissues inflammation and glucose intolerance in diet-induced obese mice. Arterioscler Thromb Vasc Biol. 2010;30:193–199. doi: 10.1161/ATVBAHA.109.198614. [DOI] [PubMed] [Google Scholar]
- 89.Mantell B.S., Stefanovic-Racic M., Yang X., Dedousis N., Sipula I.J., O'Doherty R.M. Mice lacking NKT cells but with a complete complement of CD8+ T-cells are not protected against the metabolic abnormalities of diet-induced obesity. PloS One. 2011;6:e19831. doi: 10.1371/journal.pone.0019831. [DOI] [PMC free article] [PubMed] [Google Scholar]