We review recent studies of the effects of dietary nitrate on human muscle contractile function and discuss possible underlying mechanisms.
Key Words: dietary nitrate, nitric oxide, muscle contractile function, free intracellular calcium, calcium sensitivity, ryanodine receptor, cyclic guanosine monophosphate
Abstract
Dietary nitrate, a source of nitric oxide (NO), improves the contractile properties of human muscle. We present the hypothesis that this is due to nitrosylation of the ryanodine receptor and increased NO signaling via the soluble guanyl cyclase-cyclic guanosine monophosphate-protein kinase G pathway, which together increase the free intracellular Ca2+ concentration along with the Ca2+ sensitivity of the myofilaments themselves.
Key Points
Ingestion of nitrate (NO3−), found in green leafy vegetables and especially beets, increases the production of nitric oxide (NO).
Acute or chronic (NO3−) intake also improves muscle contractile function in a variety of subject populations, including healthy young and middle-aged individuals, athletes, patients with heart failure, and the elderly.
Precisely how dietary (NO3−) intake enhances the contractile properties of human muscle is still unclear.
We hypothesize that such improvements are the result of increased NO bioavailability and hence changes in Ca2+ signaling in muscle.
INTRODUCTION
In recent years, a burgeoning number of studies have examined the effects of dietary nitrate (NO3−) on various physiological responses. This is because it is now recognized that inorganic NO3− can be a significant source of nitric oxide (NO) in the body ((1); see as follows). Because NO is a potent vasodilator, work in this area originally focused on changes in blood pressure (e.g., (2)). In 2007, however, Larsen et al. (3) reported that ingestion of NO3− at a dose of 100 μmol·kg−1 per day for 3 d lowered the steady-state rate of O2 uptake (V˙O2) during submaximal exercise. This O2-sparing effect of NO3− supplementation (often in the form of beetroot juice (BRJ)) has since been replicated in many, albeit not all (4), subsequent investigations, and seems to be especially evident in untrained subjects and during higher intensity exercise (cf. (5) for review). Dietary NO3− also has been shown to enhance muscle blood flow during exercise in both rats (6) and humans (7). At least in rats, the relative increase in flow is greatest in primarily fast-twitch muscles with lower baseline blood flows, but is also present, albeit to a lesser extent, in primarily slow-twitch muscles (6). Presumably as a consequence of these changes in O2 demand and supply, and hence in muscle energetics, dietary NO3− improves endurance performance, as measured by average power, or, conversely, time-to-completion, during high-intensity, time trial–type exercise tests by ~2% (8,9). Because of the shallow slope of the exercise intensity-duration relationship beyond the first few minutes, time-to-fatigue during constant-intensity exercise may be enhanced by up to 16% (5,6). For additional discussion of the effects of dietary NO3− on the responses to endurance exercise, readers are referred to these recent reviews (5,8,9).
More recently, dietary NO3− (or nitrite (NO2−)) also has been shown to enhance the inherent contractile properties of human muscle (10–20). Positive effects have been found in a wide range of subjects, that is, younger untrained individuals (10–12,14), trained athletes (13,15–17), patients with heart failure (HF) (18), and the elderly (19,20), and can occur in the absence of changes in submaximal V˙O2 in the same population and even in some of the same individuals (i.e., (4) vs (18)). Furthermore, NO3−-induced improvements in muscle contractility have been observed even when resistance to fatigue during high-intensity exercise is unaltered (11,13–15). These results suggest that the effects of dietary NO3− on muscle contractile properties and on V˙O2/blood flow/energetics may be due to different physiological/biochemical mechanisms, reflecting the widely varying actions of NO in various tissues, including muscle.
The purpose of the present article is to review the previously mentioned studies of the influence of dietary NO3− on the contractile properties of human muscle and to discuss possible mechanisms accounting for such effects. Although animal data are considered, especially in formulating our mechanistic hypotheses, we focus primarily upon humans because 1) most studies of the effects of NO3− intake on muscle function have been performed in people and 2) there are significant differences between rodents and humans in dietary NO3− metabolism (21), NO3−-induced changes in muscle protein expression (12,22), fiber type-specific regulation of muscle contraction (23), and NO production (24), etc., that could influence the results of such research. As will be discussed, it is our hypothesis that dietary NO3− acutely enhances human muscle function by simultaneously increasing both the free intracellular Ca2+ concentration ([Ca2+]i) during contractions and the Ca2+ sensitivity of the myofilaments themselves (Figure). These twin effects are hypothesized to result from nitrosylation of the ryanodine receptor (RyR) along with increased NO signaling via the canonical soluble guanyl cyclase (sGC)–cyclic guanosine monophosphate (cGMP)–protein kinase G (PKG) pathway. Together, these two mechanisms could explain the dietary NO3−-induced changes in human muscle contractile properties that have been reported.
Figure.

Proposed mechanisms by which dietary NO3− influences muscle contractile function in humans. After ingestion, NO3− is converted to NO2− by bacterial nitroreductases in the oral cavity and endogenous nitroreductases (e.g., xanthine oxidoreductase) in muscle itself. This increase in NO2− in turn leads to enhanced production of the free radical NO. Elevated NO bioavailability then results in multiple effects, as shown in the figure. These include nitrosylation of the sarcroendoplasmic reticululm RyR, which increases Ca2+ release by “locking” this channel in the open configuration. The subsequent increase in free intracellular [Ca2+]i contributes to the improvements in twitch force (Ftw), rate of force development (dF/dt), estimated maximal shortening velocity (Vmax), and maximal power (Pmax) of muscle that have been observed after dietary NO3− intake. Simultaneously, however, the increase in [Ca2+]i also results in activation of skeletal muscle myosin light chain kinase (skMLCK) via the Ca2+-CaM pathway and hence an increase in myosin regulatory light chain phosphorylation (pRLC). This results in greater Ca2+ sensitivity of the contractile apparatus, thereby also contributing to the increases in Ftw, dF/dt, Vmax, and Pmax. Paralleling these events, the increase in NO also results in activation of sGC and hence an increase in cGMP production. This increase in cGMP stimulates PKG activity, which in turn enhances regulatory light chain phosphorylation and hence Ca2+ sensitivity, thus improving muscle contractile function. Finally, also shown are the effects of increased NO on TropI, on the myosin heavy chain, and on the SERCA. An increase in NO can enhance nitrosylation of TropI in fast-twitch (but not slow-twitch) fibers, but this inhibits (lines) Ca2+ sensitivity, which is the opposite of what has been observed after dietary NO3− supplementation. Similarly, elevation in NO could increase nitrosylation of myosin, but this would diminish, not enhance, muscle contractile function. Elevated NO also can inhibit SERCA directly, but this would also tend to diminish muscle function, by slowing the rate of relaxation and resulting in eventual depletion of sarcoplasmic reticulum Ca2+ stores. Thus, these other potential effects of NO cannot explain the dietary NO3−-induced improvements in contractility that have been found repeatedly. cGMP, cyclic guanosine monophosphate; NO, nitric oxide; NO2−, nitrite; NO3−, nitrate; PKG, protein kinase G; RyR, ryanodine receptor; SERCA, sarcoendoplasmic reticulum Ca2+ ATPase; sGC, soluble guanyl cyclase.
NO Production in Muscle
Most NO in the body is produced by conversion of L-arginine to citrulline, a reaction catalyzed by NO synthase (NOS) and requiring O2 as well as other substrates and cofactors. NOS exists in three isoforms, that is, neuronal (nNOS, or NOS-1), inducible (iNOS, or NOS-2), and endothelial (eNOS, or NOS-3) (24). Although all three types are present in muscle, NOS-1 is considered to be the primary source of NO in this tissue, and in rodents, is almost exclusively expressed in fast-twitch muscle fibers (24). In humans, however, NOS-1 expression is similar, or even greater, in slow-twitch versus fast-twitch fibers (24). NOS activity increases several-fold during muscle contractions, apparently as a result of Ca2+-dependent activation of NOS-1, and at least in mice is accompanied by a quantitatively-similar increase in cGMP levels in fast-twitch but not slow-twitch muscle (24). This contraction-induced increase in NO production potentially influences numerous aspects of muscle physiology, for example, blood flow, glucose uptake, mitochondrial respiration, etc., via both cGMP-dependent and cGMP-independent pathways (24). These effects are beyond the scope of this review and hence will not be considered further here. Conversely, the effects of NO muscle contractile properties are directly relevant and in fact have been studied for many years, primarily in isolated animal muscle using pharmacological inhibitors or activators of NOS. In general, these studies have emphasized the possible suppressive effects of NO on muscle function, especially maximal isometric force (cf. (25) for review). As discussed by Maréchal and Gailly (25), however, this direct “braking” effect seems to be countered a cGMP-mediated enhancement of maximal shortening velocity, which improves contractile function during twitch or isotonic contractions. The specific pathways by which NO modulates skeletal muscle contraction are considered in greater detail under the Mechanisms section.
Dietary NO3− as a Source of NO in Muscle
In addition to the NOS pathway, NO also can be produced via a NOS-independent, “backup” pathway, that is, via reduction of NO3− to NO2− by oral bacteria (1) or endogenous nitroreductases (e.g., xanthine oxidase) (26), followed by further reduction of NO2− to NO within various tissues. As emphasized by Piknova et al. (26), the latter process would be favored by the low pH and O2 tension found in resting and especially contracting muscle. Conversely, NO2− and hence NO3− can be generated via oxidation of L-arginine-derived NO, or, alternatively, obtained from dietary sources. Indeed, numerous studies have demonstrated that acute ingestion of NO3− increases plasma NO3− and NO2− concentrations (e.g., (2,3,10,12–14,16–20)), as well as the levels of NO in expired breath (frequently used as a biomarker of whole-body NO production) (11,14,18,19). Until very recently, though, no study had demonstrated directly that dietary NO3− supplementation increases muscle NO3− or NO2− levels in either animals or humans. Working in Schechter’s laboratory, however, Gilliard et al. (27) recently reported that feeding rats a high NO3− diet for 7 d increased (P < 0.05) muscle NO3− and NO2− content by ~33% and >100%, respectively. Acute ingestion of 150 μmol·kg−1 (~12.3 mmol) of NO3− has also recently been shown to more than triple (P < 0.001) the NO3− content of muscle biopsy samples from older men with diabetes (28), although the small size of such samples apparently precluded measurement of NO2− content using the standard chemiluminescent approach. Schechter’s group has reported also that strenuous endurance exercise results in a dramatic reduction in muscle NO3− and NO2− levels in rats, which in the absence of NO3− intake remain suppressed for at least 12 h (26). Taken together, these data indicate that muscle NO3− and NO2− are both highly responsive to, and highly dependent upon, dietary intake. The effects of dietary NO3− on muscle contractile function as discussed as follows are presumably the result of increased NO production via this NOS-independent pathway. However, the precise mechanism by which dietary NO3− might alter human muscle contractile properties is still unknown, and direct effects of NO2− and other reactive nitrogen species (e.g., peroxynitrite) cannot be ruled out completely.
Dietary NO3− and Muscle Contractile Function
In 2012, Hernández et al. (22) demonstrated that, in mice, 7 d of (NO3−) supplementation markedly increased the force generated by fast-twitch, but not slow-twitch, muscle during lower frequency electrical stimulation. There were, though, no changes at higher frequencies of stimulation, that is, in tetanic force, or in the rate of force development. The results of this study will be considered in greater detail later. The first human study to touch upon the question at hand, however, was that of Fulford et al. (29), who in 2013 determined the effects of ingesting 10.2 mmol of NO3− either acutely or daily for 5–15 d, including on the day of testing, during isometric knee extensor exercise in healthy, untrained young men (Table). This reduced the energetic cost of exercise, as determined using 31P magnetic resonance spectroscopy, but maximal voluntary force production was unchanged. No other measurements of muscle function were obtained, however, nor was there any evidence of any chronic effects of NO3− supplementation on muscle energetics (i.e., similar results were obtained during all three trials). The latter finding is consistent with the apparent absence of any chronic effects of dietary NO3− supplementation on human muscle contractile properties, as will be discussed.
TABLE.
Studies of the effects of dietary NO3− on human muscle contractile properties
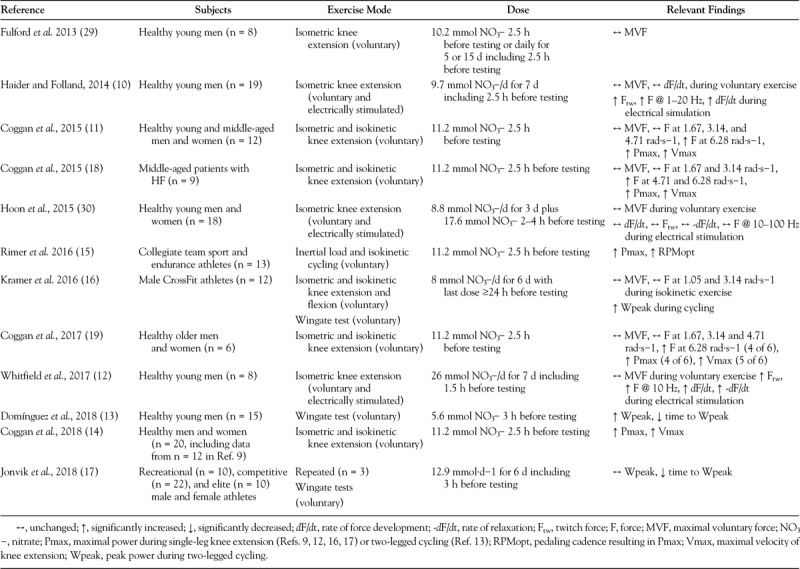
Haider and Folland (10) in 2014 were the first to extensively assess the impact of dietary NO3− on human muscle contractility, by determining the effects of ingesting 9.7 mmol of NO3−/d for 7 d, including on the day of testing, on voluntary and electrically stimulated isometric knee extension exercise in healthy, untrained young men. Although no differences were observed during voluntary exercise, small (i.e., 3%–15%), but statistically significant (i.e., P < 0.01–0.05), improvements in twitch force, force at 10 Hz, and force during the first 50 ms of contraction were found during transcutaneous electrical stimulation. Similar, but slightly larger, improvements (P < 0.01–0.05) have since been reported by Whitfield et al. (12) in healthy, untrained young men ingesting 26 mmol of NO3−/d for 7 d (including on the day of testing).
The data of Haider and Folland (10) and later Whitfield et al. (12) clearly demonstrate that ingestion of NO3− can alter human muscle contractile function, at least during electrically stimulated isometric exercise. In contrast, using very similar methods, Hoon et al. (30) found no changes in maximal voluntary force or in twitch force, the rate of force development, the rate of relaxation, or in force at 10–100 Hz of electrical stimulation after 3 d of NO3− supplementation at (ostensibly) 8.8 mmol·d−1 plus 17.6 mmol on the day of testing. (NO3− supplementation did attenuate the rate of fatigue development during repetitive stimulation for ≥80 s, but only when blood flow was restricted.) Although it might be tempting to speculate that these largely negative results are due to the shorter supplementation period, this seems unlikely given that improvements in muscle function have been observed even after an acute dose of NO3− (see as follows). The reasons why Hoon et al. (30) did not find any changes in unfatigued muscle are unclear, although it is worth noting that these investigators used a BRJ product of unverified NO3− content and did not measure any markers of NO bioavailability (e.g., plasma NO2−, breath NO).
Given the data previously discussed, it is natural to wonder whether dietary NO3− can influence human muscle function during voluntary, dynamic exercise. Indeed, contemporaneous with Haider and Folland’s (10) research, we used isokinetic dynamometry to address this question in healthy, young and middle-aged men and women (11). We found that a single dose of 11.2 mmol of NO3− 2–3 h before testing did not increase maximal isometric force or the force (torque) generated at slower velocities of knee extension. Acute NO3− ingestion did, however, enhance force at higher velocities, resulting in 11% and 6% increases (both P < 0.05) in calculated maximal speed (Vmax) and power (Pmax), respectively. Subsequently, we found even greater improvements in Vmax and Pmax (i.e., of 12% and 13%, respectively; both P < 0.05) in response to the same dose of NO3− in middle-aged patients with HF (18), presumably because such patients are NO deficient (31,32). Because NO bioavailability also decreases with age (33), we have since examined the effects of acute NO3− ingestion on the Vmax and Pmax of the knee extensors of healthy, elderly subjects (19). Although preliminary in nature, the data from this study indicate that older subjects also demonstrate improvements in Vmax and Pmax, at least provided that the dose of NO3− ingested is >125 μmol·kg−1. The conclusion that NO3− ingestion can improve contractile function even in aged muscle is supported by the findings of Justice et al. (20), who found that daily supplementation with NO2− for 10 wk increased (P < 0.01) the rate of force development during voluntary knee extension and flexion in healthy, middle-aged and older men and women. Finally, we have expanded recently upon our original study (11) to investigate determinants of interindividual differences in the effects of dietary NO2− on muscle function in a larger cohort (14). As before, we observed significant increases in Vmax and Pmax (both P < 0.05) in response to NO3− intake, with the size of these improvements being positively associated with the magnitude of the increase in plasma NO2− concentration (P < 0.01) and possibly female sex (P < 0.08), but not with other parameters, including baseline Vmax or decline in force during a 50 contraction fatigue test (in vivo indicators of muscle fiber type distribution).
All of the data described previously were obtained during isolated contractions performed by a single muscle/muscle group acting across a single joint. To determine whether dietary NO3− also improves contractile performance during repeated multi-muscle, multi-joint movements, we collaborated with Dr. Jim Martin and Ernie Rimer at the University of Utah to determine the effects of acute supplementation with 11.2 mmol of NO3− on performance during inertial load sprint cycling (15). Similar to our isokinetic dynamometry results, we found that NO3−intake increased (P < 0.05) both cycling Pmax and the associated pedaling rate by 6% in a heterogeneous group of endurance and collegiate team sport athletes. These results have since essentially been confirmed by Domínguez et al. (13), who found that ingestion of 5.6 mmol of NO3− 3 h before a Wingate cycling test increased (P < 0.05) peak power by 6%. Time-to-peak power also tended to be reduced (P = 0.06). Jonvik et al. (17) also recently reported that ingestion of 12.9 mmol of NO3−/d for 6 (including 3 h before testing) significantly (i.e., P < 0.01) reduced time-to-peak power (by 3%) during Wingate testing of speed skaters, although peak power itself was unchanged.
Along the same lines, Kramer et al. (16) recently found that ingesting 8 mmol of NO3−/d for 6 d improved the peak power of male CrossFit athletes during a Wingate test by 7% (P < 0.01), even though it did not alter force during isometric or isokinetic knee extension or flexion at slow velocities. Unlike in other studies, however, subjects were tested ≥24 h after the last dose of NO3−, after which plasma NO3− and NO2− levels would be expected to have returned to near normal. Nonetheless, it seems unlikely that the results of Kramer et al. (16) represent any sort of long-term structural adaptation, because similar improvements have been observed after just a single dose of NO3− (13,15). Furthermore, recent data from Whitfield et al. (12) demonstrate that, unlike in mice (22), NO3− supplementation of humans does not alter the expression of key Ca2+ handling proteins in muscle (see Mechanisms). Thus, the results of Kramer et al. (16) are presumably simply the result of a “loading” effect of previous NO3− intake on intramuscular NO3− and NO2− stores, versus any more permanent adaptations in muscle.
Finally, several recent studies of male team sport athletes by Jones et al. (34–36) also provide indirect evidence that dietary NO3− can enhance the contractile properties of human muscle. In the first (34), ingestion of 12.8 mmol of NO3−/d for 7 d (including 2.5 h before testing) was shown to improve (i.e., P < 0.05) performance during the early phases of an intermittent sprint cycling protocol designed to mimic the demands of, for example, international field hockey. Similar results were obtained by Wylie et al. (35) in subjects ingesting 8.2 mmol of NO3−/d for 5 d (including 2.5 h before testing) and performing repeated 6 s (but not 30 or 60 s) all-out efforts. Finally, in another study (35), supplementation with 6.4 mmol of NO3−/d for 5 d (including 2.5 before testing) was found to improve significantly (i.e., P < 0.05) 0–5 and 5–10, but not 10–20, m split times during an intermittent sprint running test. Although somewhat indirect, the results of these studies are consistent with the dietary NO3−-induced increases in muscle contractility found both by ourselves (11,14,15,18,19) and others (10,12,13,16,17,20).
In summary, numerous recent studies have demonstrated that ingestion of NO3− significantly enhances muscle contractile function in humans. This effect seems to be the result of an increase in the number of active actomyosin cross-bridges and in the rate of cross-bridge cycling under load, and not an increase in the force generated per active cross-bridge. This interpretation is based upon the improvements observed in isometric twitch force (10,12), rate of isometric force development (10,12,20), isometric force during low-frequency electrical stimulation (10,12), isokinetic/dynamic force and power during high-velocity muscle shortening (11,13–17), and increased estimated maximal speed of shortening (11,15,19), all in the absence of any significant improvement in the force-generating capacity of muscle during maximal voluntary contractions (10–12,14,16,19,20,30) or at higher frequencies of electrical stimulation (10,12). The specific biochemical mechanisms by which dietary NO3− might alter the contractile characteristics of human muscle are considered in greater detail as follows.
Mechanisms
As mentioned previously, using mice, Hernández et al. (22) were the first to determine the effects of dietary NO3− on muscle contractility. Along with the fast twitch fiber-specific changes in function described previously, these authors found that NO3− supplementation increased [Ca2+]i in muscle, both at rest and during tetanic contractions, and also shifted the force-Ca2+ relation, resulting in increased force at moderately high, but sub-saturating, Ca2+ levels. These effects were ascribed to increased expression of the Ca2+-handling proteins calsequestrin (CSQ) and the dihydropyridine (DHPR) receptor. More recently, however, Whitfield et al. (12) found that NO3− supplementation did not alter the expression of CSQ, DHPR, or other Ca2+-handling proteins, that is, RyR or the sarcoendoplasmic reticulum Ca2+ ATPase (SERCA), in human muscle. Furthermore, changes in protein expression cannot explain the improvements in muscle contractile function that we (11,14,15,18,19) and others (13) have observed repeatedly after acute NO3− ingestion, nor could the changes in CSQ and DHPR reported by Hernández et al. (22) seemingly explain the altered Ca2+ sensitivity that these authors also found.
In the absence of changes in protein expression, Whitfield et al. (12) speculated that NO3−-induced improvements in muscle function may be due to enhanced production of reactive O2 species. This hypothesis was based on the observations of Andrade et al. (37), who reported that H2O2 reduces Ca2+ release but increases maximal tetanic force in isolated mouse muscle fibers. However, Whitfield et al. (12) found no changes in the levels of protein carbonylation or lipid peroxidation or in the ratio of reduced to oxidized glutathione, which would argue against significant changes in cellular redox status. More importantly, dietary NO3− actually increases Ca2+ release in mice (22) and has failed routinely to increase either maximal voluntary or maximal electrically stimulated force in numerous human studies ((10–12,16,18,19,30); Table), effects that are precisely the opposite of those due to H2O2 (37). Increased production of reactive O2 species also cannot account for the improvements in muscle contractility that result from NO3− intake.
Given that neither changes in protein expression nor in redox state can seemingly explain dietary NO3−-induced improvements in human muscle contractile function, what mechanism(s) is (are) responsible? Historically, NO was considered to act exclusively via the sGC-cGMP-PKG pathway (38). In the last few decades, however, it has become increasingly recognized that NO also can influence cellular events more directly, either by itself or after nitrosylation or transnitrosylation of thiols, especially cysteine residues of proteins (39). In skeletal muscle, however, most non–cGMP-mediated effects of NO are actually inhibitory, that is, they tend to diminish, not enhance, muscle contractile function. For example, it has been shown that NO directly inhibits the activity of SERCA in rabbit fast twitch muscle (40). This would be expected to slow the rate of relaxation and limit the amount of Ca2+ released (and hence force generated) during subsequent contractions, due to depletion of Ca2+ from the sarcoplasmic reticulum. Somewhat along the same lines, high-intensity exercise has been found to stimulate transnitrosylation of myosin in rat fast twitch muscle (41), but this inhibited the Mg2+ ATPase activity of the protein. All else being equal, this would reduce maximal shortening velocity. Increased NO availability may lead also to reversible transnitrosylation of troponin I (TropI) (42), but the consequence of this is a reduction in Ca2+ sensitivity of rat and human fast-twitch and no change in slow-twitch fibers. All of these effects (i.e., decline in Ca2+ release, decrease in speed of shortening, reduction or no change in Ca2+ sensitivity) are the opposite of those that have been observed after dietary NO3− supplementation.
In contrast to the inhibitory effects described previously, transnitrosylation of RyR may be one mechanism by which NO could enhance muscle contractile function. This posttranslational modification of the protein enhances Ca2+ release (43), by increasing the probability of the channel being in the open state (44). In particular, at low O2 tensions typical of skeletal muscle in vivo even submicromolar concentrations of NO will activate type 1 RyRs (45), as a result of transnitrosylation of a single cysteine residue (46). This blocks the inhibitory effects of calmodulin (CaM) on RyR1, thereby enhancing Ca2+ release and force production. Thus, although excessive nitrosylation of RyRs and hence sustained elevations in [Ca2+]i in muscle are thought to play a key role in exertional heatstroke and malignant hyperthermia (47), physiological (rather than pathophysiological) increases in NO and hence in RyR nitrosylation and Ca2+ release as a result of dietary NO3− intake could be responsible for the accompanying improvements in muscle contractile function. Specifically, under sub-saturating conditions dietary NO3−-induced increases in [Ca2+]i (22) would enhance twitch force, rate of force development, shortening velocity, and power, whereas no changes would be expected to occur under saturating conditions, for example, during a sustained maximal isometric contraction. These functional changes are, of course, precisely those that have been observed in response to acute and chronic NO3− supplementation. An increase in [Ca2+]i during contractions due to RyR nitrosylation could explain also the increase in Ca2+ sensitivity observed by Hernández et al. (22), by enhancing myosin regulatory light chain phosphorylation (pRLC) via the Ca2+-CaM-skeletal muscle myosin light chain kinase (skMLCK) pathway (23). Indeed, the effects of dietary NO3− on muscle contractile properties are essentially identical to those resulting from increased pRLC (23). Together, these two effects (i.e., an increase in [Ca2+]i and in Ca2+ sensitivity, both as a result of RyR nitrosylation) could account for all of the changes in muscle contractile properties that have been observed in response to dietary NO3− intake.
Alternatively and in addition, enhanced NO signaling via the original sGC-cGMP-PKG pathway is another possible mechanism by which NO3− supplementation improves muscle contractile function in humans. In this scenario, which is based on that originally hypothesized by Maréchal and Beckers-Bleukx (48), an increase in NO bioavailability resulting from dietary NO3− intake results in activation of sGC, and hence an increase in cGMP production. Increased cGMP levels in turn result in activation of PKG and hence in skMLCK activity, leading to an increase in pRLC. This would enhance Ca2+ sensitivity of the contractile apparatus, thereby accounting for all of the functional changes mentioned previously. (An increase in skMLCK activity would not explain the increase in Ca2+ release reported by Hernández et al. (22), as the SR is not a target of this enzyme.) In support of this hypothesis, Maréchal and Beckers-Bleukx (48) demonstrated that sGC inhibitors or activators respectively diminished or augmented the maximal shortening velocity of mouse muscle without altering maximal isometric force, effects that resemble those of dietary NO3−. Maréchal and Beckers-Bleukx (48) also found that inhibition of NOS reduced basal cGMP levels by 12%–27%, whereas others have reported (in abstract) that NOS inhibition reduces pRLC by a similar amount in C2C12 myotubes (49). Thus, although it remains to be demonstrated that an increase in NO bioavailability as a result of dietary NO3− intake results in an increase in either cGMP or in pRLC in either animal or human muscle, this alternative or parallel mechanism may also be operative.
Effects of Muscle Fiber Type
As indicated previously, studies of rodents have demonstrated that the effects of dietary NO3− on contractile properties are specific to fast-twitch muscle (22). In rats, however, muscle contraction results in an increase in pRLC only in fast-twitch fibers, whereas in humans this occurs in both fast-twitch and slow-twitch fibers (23). Furthermore, human (and rat) fast- and slow-twitch muscle fibers primarily or even exclusively express the same isoform of RyR, that is, RyR1 (50). Thus, based on the mechanisms described previously, there would be no reason to hypothesize a fiber type-specific effect of dietary NO3− on the contractile properties of human muscle, even though one exists in rats. In fact, as previously mentioned, we were recently unable to detect any relation between in vivo indicators in muscle fiber type distribution and the magnitude of the dietary NO3−-inducted increase in Pmax (14). Muscle fiber type distribution was not determined directly in this study, however, so at least at present a fiber type-specific benefit of dietary NO3− supplementation on human muscle function cannot be ruled out completely.
Significance
Additional research is required to test the previous hypotheses and may prove to be particularly challenging given the previously mentioned differences between humans and rodents, including in the acute responses (21) and chronic adaptations (i.e., (12) vs (22)) to dietary NO3− supplementation. The “crosstalk” between the proposed RyR and sGC-cGMP-PKG pathways (at the level of pRLC) may also make it difficult to determine the relative importance of nitrosylation versus canonical NO signaling, as is true in other situations. Regardless of the precise mechanism(s) involved, however, the improvements in human muscle contractile function resulting from NO3− ingestion are potentially significant. This is true in the contexts of both sports and general health and well-being. For example, as previously discussed (11), even a 1% improvement in performance would double the probability of an elite athlete winning a particular competition. Comparatively speaking, the 4%–13% increase in maximal neuromuscular power resulting from dietary NO3− intake (11,13–16,18,30) is enormous. More importantly, muscle power plays a key role in activities of daily living yet is compromised markedly in, for example, patients with HF due to systolic dysfunction (31). Indeed, reduced muscle contractile function strongly contributes to the whole-body exercise intolerance that is characteristic of the latter “cardiomuscular” disease, and in fact is a powerful predictor of survival in those with HF (31). In this context, as previously discussed (31), the magnitude of the dietary NO3−-induced increase in maximal neuromuscular power we have found in HF patients (18) is sufficient to have acutely erased approximately one third of their expected deficit in this parameter. It is also similar to that resulting from 2 to 3 months of resistance exercise training in such individuals, which has been shown to result in improvement in Minnesota Living with Heart Failure Questionnaire Scores (18). Thus, significant improvements in skeletal muscle contractility due to NO3− ingestion could have a positive impact on quality of life and possibly even lifespan in patients with HF, as well as other subject groups.
Summary
Numerous recent studies, both by ourselves (11,14,15,18,19) and by others (10,12,13,16,17,20), have demonstrated that acute or chronic NO3− (or NO2−(20)) ingestion significantly enhances the contractile properties of human skeletal muscle, especially speed and hence power. Such improvements have been observed in a wide range of subjects, including younger, untrained individuals (10–12,14), trained athletes (13,15–17), patients with HF (18), and the elderly (19,20). The precise mechanisms responsible for this NO3−-induced increase in human muscle contractility are still unknown, but changes in Ca2+ signaling due to increased NO bioavailability are likely to play a role. Additional research will be needed to test this hypothesis and to determine the practical and clinical benefits of using NO3− supplementation to augment muscle function in healthy and diseased populations.
Acknowledgments
This study was supported by award no. R34HL138253 from the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI or NIH.
Footnotes
Editor: Stephen E. Alway, Ph.D., FACSM.
References
- 1.Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat. Rev. Drug Discov. 2008; 7:156–67. [DOI] [PubMed] [Google Scholar]
- 2.Larsen FJ, Ekblom B, Sahlin K, Lundberg JO, Weitzberg E. Effects of dietary nitrate on blood pressure in healthy volunteers. N. Engl. J. Med. 2006; 355:2792–3. [DOI] [PubMed] [Google Scholar]
- 3.Larsen FJ, Weitzberg E, Lundberg JO, Ekblom B. Effects of dietary nitrate on oxygen cost during exercise. Acta. Physiol. (Oxf.). 2007; 191:59–66. [DOI] [PubMed] [Google Scholar]
- 4.Coggan AR, Broadstreet SR, Mahmood K, et al. Dietary nitrate increases V˙O2peak and performance but does not alter ventilation or efficiency in patients with heart failure with reduced ejection fraction. J. Card. Fail. 2018; 24:65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pawlak-Chaouch M, Boissière J, Gamelin FX, Cuvelier G, Berthoin S, Aucouturier J. Effect of dietary nitrate supplementation on metabolic rate during rest and exercise in human: a systematic review and a meta-analysis. Nitric Oxide. 2016; 53:65–76. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson SK, Hirai DM, Copp SW, et al. Impact of dietary nitrate supplementation via beetroot juice on exercising muscle vascular control in rats. J. Physiol. 2013; 591:547–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casey DP, Treichler DP, Ganger CT, 4th, Schneider AC, Ueda K. Acute dietary nitrate supplementation enhances compensatory vasodilation during hypoxic exercise in older adults. J. Appl. Physiol. 2015; 118:178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones AM. Dietary nitrate supplementation and exercise performance. Sports Med. 2014; 44(1 Suppl):S35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones AM. Influence of dietary nitrate on the physiological determinants of exercise performance: a critical review. Appl. Physiol. Nutr. Metab. 2014; 39:1019–28. [DOI] [PubMed] [Google Scholar]
- 10.Haider G, Folland JP. Nitrate supplementation enhances the contractile properties of human skeletal muscle. Med. Sci. Sports Exerc. 2014; 46:2234–43. [DOI] [PubMed] [Google Scholar]
- 11.Coggan AR, Leibowitz JL, Kadkhodayan A, et al. Effect of acute dietary nitrate intake on maximal knee extensor speed and power in healthy men and women. Nitric Oxide. 2015; 48:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whitfield J, Gamu D, Heigenhauser GJF, et al. Beetroot juice increases human muscle force without changing Ca2+-handling proteins. Med. Sci. Sports Exerc. 2017; 49:2016–24. [DOI] [PubMed] [Google Scholar]
- 13.Domínguez R, Garnacho-Castaño MV, Cuenca E, et al. Effects of beetroot juice supplementation on a 30-s high-intensity inertial cycle ergometer test. Nutrients. 2017; 9:E1360 doi: 10.3390/nu9121360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coggan AR, Broadstreet SR, Mikhalkova D, et al. Dietary nitrate-induced increases in human muscle power: high versus low responders. Physiol. Rep. 2018; 6:e13575, https://doi.org/10.14814/phy2.13575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rimer EG, Peterson LR, Coggan AR, Martin JC. Increase in maximal cycling power with acute dietary nitrate supplementation. Int. J. Sports Physiol. Perform. 2016; 11:715–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kramer SJ, Baur DA, Spicer MT, Vukovich MD, Ormsbee MJ. The effect of six days of dietary nitrate supplementation on performance in trained CrossFit athletes. J. Int. Soc. Sports Nutr. 2016; 13:39 10.1186/s12970-016-0150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonvik KL, Nyakayiru J, van Dijk JW, et al. Repeated-sprint performance and plasma responses following beetroot juice supplementation do no differ between recreational, competitive, and elite sprint athletes. Eur. J. Sport Sci. 2018; 7:1–10. [DOI] [PubMed] [Google Scholar]
- 18.Coggan AR, Leibowitz JL, Spearie CA, et al. Acute dietary nitrate intake improves muscle contractile function in patients with heart failure: a double-blind, placebo-controlled, randomized trial. Circ. Heart Fail. 2015; 8:914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coggan AR, Broadstreet SR, Leibowitz JL, et al. Dietary nitrate and muscle power with aging. Med. Sci. Sports Exerc. 2017; 49:S816. [Google Scholar]
- 20.Justice JN, Johnson LC, DeVan AE, et al. Improved motor and cognitive performance with sodium nitrite supplementation is related to small metabolite signatures: a pilot trial in middle-aged and older adults. Aging (Albany NY). 2015; 7:1004–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montenegro MF, Sundqvist ML, Nihlén C, et al. Profound differences between humans and rodents in the ability to concentrate salivary nitrate: implications for translational research. Redox Biol. 2016; 10:206–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hernández A, Schiffer TA, Ivarsson N, et al. Dietary nitrate increases tetanic [Ca2+]i and contractile force in mouse fast-twitch muscle. J. Physiol. 2012; 590:3575–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vandeboom R. Modulation of skeletal muscle contraction by myosin phosphorylation. Compr. Physiol. 2017; 171–212. [DOI] [PubMed] [Google Scholar]
- 24.Stamler JS, Meissner G. Physiology of nitric oxide in skeletal muscle. Physiol. Rev. 2001; 81:209–37. [DOI] [PubMed] [Google Scholar]
- 25.Maréchal G, Gailly P. Effects of nitric oxide on the contraction of skeletal muscle. Cell. Mol. Life Sci. 1999; 55:1088–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piknova B, Park JW, Kwan Jeff Lam K, Schechter AN. Nitrate as a source of nitrite and nitric oxide during exercise hyperemia in rat skeletal muscle. Nitric Oxide. 2016; 55–56:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilliard CN, Lam JK, Cassel KS, Park JW, Schechter AN, Piknova B. Effect of dietary nitrate levels on nitrate fluxes in rat skeletal muscle and liver. Nitric Oxide. 2018; 75:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nyakayiru J, Kouw IWK, Cermak NM, Senden JM, van Loon LJC, Verdijk LB. Sodium nitrate ingestion increases skeletal muscle nitrate content in humans. J. Appl. Physiol. 2017; 123:637–44. [DOI] [PubMed] [Google Scholar]
- 29.Fulford J, Winyard PG, Vanhatalo A, Bailey SJ, Blackwell JR, Jones AM. Influence of dietary nitrate supplementation on skeletal muscle metabolism and force production during maximal voluntary contractions. Pflüger Arch. 2013; 465:517–28. [DOI] [PubMed] [Google Scholar]
- 30.Hoon MW, Fornusek C, Chapman PG, Johnson NA. The effect of nitrate supplementation on muscle contraction in healthy adults. Eur. J. Sport Sci. 2015; 8:712–9. [DOI] [PubMed] [Google Scholar]
- 31.Coggan AR, Peterson LR. Dietary nitrate and skeletal muscle contractile function in heart failure. Curr. Heart Fail. Rep. 2016; 13:158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang L, Wang H, Ziolo MT. Targeting NOS as a therapeutic approach for heart failure. Pharmacol. Ther. 2014; 142:306–15. [DOI] [PubMed] [Google Scholar]
- 33.Di Massimo C, Scarpelli P, Di Lorenzo N, Caimi G, di Orio F, Ciancarelli MG. Impaired plasma nitric oxide availability and extracellular superoxide dismutase activity in healthy humans with advancing age. Life Sci. 2006; 78:1163–7. [DOI] [PubMed] [Google Scholar]
- 34.Thompson C, Wylie LJ, Fulford J, et al. Dietary nitrate improves sprint performance and cognitive function during prolonged intermittent exercise. Eur. J. Appl. Physiol. 2015; 115:1825–34. [DOI] [PubMed] [Google Scholar]
- 35.Wylie LJ, Bailey SJ, Kelly J, Blackwell JR, Vanhtatalo A, Jones AM. Influence of beetroot juice supplementation on intermittent exercise performance. Eur. J. Appl. Physiol. 2016; 116:415–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thompson C, Vanhatalo A, Jell H, et al. Dietary nitrate supplementation improves sprint and high-intensity intermittent running performance. Nitric Oxide. 2016; 61:55–61. [DOI] [PubMed] [Google Scholar]
- 37.Andrade FH, Reid MB, Westerblad H. Contractile response of skeletal muscle to low peroxide concentrations: myofibrillar calcium sensitivity as a likely target for redox-modulation. FASEB J. 2001; 15:309–11. [DOI] [PubMed] [Google Scholar]
- 38.Murad F. The nitric oxide-cyclic GMP signal transduction system for intracellular and intercellular communication. Recent Prog. Horm. Res. 1994; 49:239–48. [DOI] [PubMed] [Google Scholar]
- 39.Gould N, Doulias PT, Tenopoulou M, Raju K, Ischiropoulos H. Regulation of protein function and signaling by reversible cysteine S-nitrosylation. J. Biol. Chem. 2013; 288:26473–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ishii T, Sunami O, Saitoh N, Nishio H, Takeuchi T, Hata F. Inhibition of skeletal muscle sarcoplasmic reticulum Ca2+-ATPase by nitric oxide. FEBS Lett. 1998; 440:218–22. [DOI] [PubMed] [Google Scholar]
- 41.Nogueira L, Figueiredo-Freitas C, Casimiro-Lopes G, Magdesian MH, Assreuy J, Sorenson MM. Myosin is reversibly inhibited by S-nitrosylation. Biochem. J. 2009; 424:221–31. [DOI] [PubMed] [Google Scholar]
- 42.Dutka TL, Mollica JP, Lamboley CR, et al. S-nitrosylation and S-glutathionylation of Cys134 on troponin I have opposing competitive actions on Ca2+ sensitivity in rat fast-twitch muscle fibers. Am. J. Physiol. Cell Physiol. 2017; 321:C316–27. [DOI] [PubMed] [Google Scholar]
- 43.Stoyanovsky D, Murphy T, Anno PR, Kim YM, Salama G. Nitric oxide activates skeletal and cardiac ryanodine receptors. Cell Calcium. 1997; 21:19–29. [DOI] [PubMed] [Google Scholar]
- 44.Pouvreau S, Allard B, Berthier C, Jacquemond V. Control of intracellular calcium in the presence of nitric oxide donors in isolated skeletal muscle fibres from mouse. J. Physiol. 2004; 560:779–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eu JP, Sun JH, Xu L, Stamler JS, Meissner G. The skeletal muscle calcium release channel: coupled O2 sensor and NO signaling functions. Cell. 2000; 102:499–509. [DOI] [PubMed] [Google Scholar]
- 46.Porter Moore C, Zhang JZ, Hamilton SL. A role for cysteine 3635 of RYR1 in redox modulation and calmodulin binding. J. Biol. Chem. 1999; 274:36831–4 doi:10.1074/jbc.274.52.36831. [DOI] [PubMed] [Google Scholar]
- 47.Durham WJ, Aracena-Parks P, Long C, et al. RyR1 S-nitrosylation underlies environmental heat stroke and sudden death in Y522S RyR1 knockin mice. Cell. 2008; 133:53–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maréchal G, Beckers-Bleukx G. Effect of nitric oxide on the maximal velocity of shortening of a mouse skeletal muscle. Pflugers Arch. 1998; 436:906–13. [DOI] [PubMed] [Google Scholar]
- 49.Lai S, Collins BC, Lowe DA. Regulation of skeletal muscle strength by estradiol: myosin regulatory light chain and neuronal nitric oxide synthase. FASEB J. 2013; 27:939.14. [Google Scholar]
- 50.Gehlert S, Bloch W, Suhr F. Ca2+ dependent regulations and signaling in skeletal muscle: from electro-mechanical coupling to adaptation. Int. J. Mol. Sci. 2015; 16:1066–95. [DOI] [PMC free article] [PubMed] [Google Scholar]


