Abstract
Our previous experimental animal data suggest a beneficial effect of leptin on LV structure and function. We hypothesized that leptin levels are associated with lower LV mass and myocardial stiffness which are important risk factors for the development of heart failure with preserved ejection fraction (HFpEF). We evaluated 1172 blacks, in which the prevalence of HFpEF is quite high, with preserved LV ejection fraction (EF>50%) from the Genetic Epidemiology Network of Arteriopathy Study (mean age 62.9 years, 72% women), a community-based study to identify genes influencing blood pressure and target organ damage due to hypertension. Associations between leptin levels and indices of LV structure and function were evaluated using generalized estimating equations accounting for clustering in siblings. LV myocardial stiffness was evaluated using diastolic wall strain (DWS) measured by echocardiography. Analyses were stratified by sex because leptin levels were three times higher in women than men (p <0.001). After adjustment for confounders, higher leptin levels were associated with lower LV mass (coefficient for 1 s.d. increase of leptin level: −5.825 g, 95% CI: −9.755 to −1.895 g, P = 0.004) and higher DWS (lower LV stiffness) (coefficient for 1 s.d. increase of leptin level: 0.009, 95% CI: 0.002–0.015, P = 0.007) in women. There were no statistically significant associations in men. In women, there were interactions between leptin levels and body mass index quartiles on LV mass and stiffness (p < 0.05 for both). Higher leptin levels were associated with lower LV mass and stiffness in obese but not lean black women.
Introduction
Leptin, a hormone produced by adipocytes [1], increases in accordance with body mass index (BMI) [2]. Leptin acts through the brain to decrease appetite, increase energy expenditure, and it may also increase blood pressure through activation of the sympathetic nervous system [3, 4]. Because of its function to activate the sympathetic nervous system, it has been hypothesized that leptin may contribute to cardiac hypertrophy and heart failure [5–7]. Several recent reports have shown a relationship between leptin and cardiovascular diseases. For example, plasma leptin levels were increased in patients with hypertension [8], coronary artery disease [9], and heart failure [5]. Studies have also demonstrated a positive correlation between plasma leptin levels and left ventricular (LV) mass or LV wall thickness in obese patients [6, 7]. On the other hand, other studies have found a negative correlation between plasma leptin levels and LV mass or LV wall thickness after adjustment for several confounding factors [10, 11].
At the cellular level, leptin administration increased the growth of cultured cardiomyocytes, supporting its pro-hypertrophic effect [12, 13]. However, we have shown that overexpression of cardiac leptin receptors in obese mice (db/db) with whole body leptin receptor mutation and high circulating leptin levels improved LV diastolic function and did not cause LV hypertrophy [14]. Previous studies have shown causal relationships of obesity with LV hypertrophy and heart failure, and a recent study demonstrated that substantial weight reduction reduces the risk of incident heart failure [15]. Leptin has some possible beneficial cardiac effects such as weight loss, improved myocardial metabolism, and possibly direct beneficial myocardial effects that may protect against heart failure; however, other effects such as activation of the sympathetic nervous system and elevated blood pressure may be detrimental. It appears that resistance to some of the beneficial effects of leptin (i.e., appetite suppression) occurs in obesity. It remains unclear if similar resistance to cardioprotective effects of leptin occurs in obesity individuals.
LV hypertrophy and myocardial stiffening play important roles in the development of heart failure with preserved ejection fraction (HFpEF) for which good therapeutic strategies have not been established yet. It has been reported that the prevalence of HFpEF among blacks is quite high [16] and it may be attributed to its higher prevalence of obesity and hypertension [17–19]. Thus, we were motivated to investigate the beneficial effect of leptin on LV hypertrophy and stiffening among African Americans. We hypothesized that high leptin levels are significantly associated with reduced LV mass and LV myocardial stiffness among obese blacks. The objective of this study was to investigate the relationships between plasma leptin levels and cardiac structure and function among blacks in a large cohort study, Genetic Epidemiology Network of Arteriopathy (GENOA).
Materials and methods
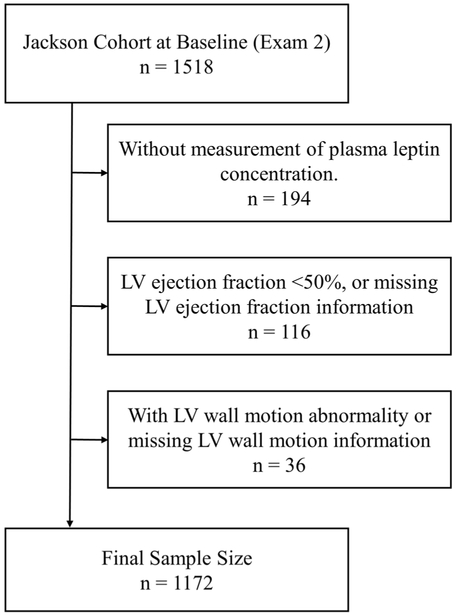
The study population for this investigation consisted of participants from the Jackson, Mississippi cohort of the GENOA study. This study was approved by the Institutional Review Board of the University of Mississippi Medical Center, Jackson, Mississippi, and participants provided written informed consent. The design and procedures for the GENOA study have been reported in detail previously [20]. Briefly, two GENOA cohorts were originally ascertained (1995–2000) through sibships in which at least two siblings had essential hypertension diagnosed prior to age 60 years. All siblings in the sibship were invited to participate, both normotensive and hypertensive including blacks from Jackson, Mississippi (N = 1854 at the first exam) and whites from Rochester, Minnesota (N = 1583 at the first exam). We used the black cohort for this study (“Jackson cohort”) due to the availability of echo-cardiographic data (no echocardiograms were performed in the white cohort). Figure 1 shows the exclusion process. Of the Jackson Cohort who returned the second exam (n = 1518), we excluded the following participants from this study: 194 participants who had no measurement of leptin concentration, 78 participants with a LV EF <50%, 38 participants whose LV EF had not been measured, 34 participants who had a LV wall motion abnormality, and 2 participants whose wall motion abnormality had not been evaluated. The remaining 1172 participants were included in our study.
Fig. 1.
Exclusion process of the study participants
Blood was collected by venipuncture after an overnight fast and processed using standardized protocols at second exam. Blood was centrifuged for 10 min at 4 °C, aliquoted in 0.5–1 ml volumes of plasma and serum, and stored at −80 °C within 2 h. of venipuncture. Plasma leptin con-centration levels were measured as previously described [21]. Briefly, aliquots of samples frozen to − 80 °C were shipped to Rochester, MN overnight on dry ice. Samples were visually inspected for evidence of thawing and then stored at − 80 °C. For protein measurements, samples were thawed on ice and aliquoted into bar-coded Eppendorf tubes. Leptin levels were measured in duplicate by radio-immunoassay (Linco Research, Inc., St. Louis, MO). Intra-assay coefficients of variation were 6.1% at 3.8ng/ml and 7.7% at 39.7 ng/ml, and inter-assay coefficients of variation were 11% at 3.0 ng/ml and 13% at 20.4 ng/ml [21]. Serum creatinine concentrations were measured by standard enzymatic methods, and estimated glomerular filtration rate (eGFR) was calculated from the serum creatinine con-centration [22, 23].
Essential hypertension, diagnosed prior to age 60 years of age, was defined as: (1) average of the last two out of three systolic BP readings ≥140mmHg, or (2) an average of the last two out of three diastolic BP readings ≥90 mmHg, or (3) a previous diagnosis of hypertension and antihypertensive medication prescribed by a physician to be taken daily during the last month. Diabetes was defined as present if a participant was receiving treatment with insulin, oral antidiabetic agents, or had fasting serum glucose levels ≥126 mg/dL. Dyslipidemia was defined as present if a participant was receiving treatment with lipid lowering agents, had fasting serum low-density lipoprotein concentration ≥160 mg/dL, fasting serum high-density lipoprotein concentration <40, or fasting serum triglycerides ≥160 mg/dL. Coronary artery disease was defined as present if a participant had undergone coronary arteriography before and had a narrowing of artery or obstruction, or had a past history of myocardial infarction.
In the GENOA study, standardized echocardiography methods, along with training and certification, were used by field-center technicians to achieve high-quality recordings. Readings were performed at the New York Presbyterian Hospital-Weill Cornell Medical Center and a single highly experienced investigator verified them. Measurements were made using a computerized review station equipped with digitizing tablet and monitor screen overlay for calibration and performance of each measurement. LV internal dimension and interventricular septal and posterior wall thicknesses were measured at end-diastole and end-systole on two-dimensional (2D) image in three cardiac cycles according to the recommendations of the American Society of Echocardiography [24]. Calculations of LV mass were made using the following equation as recommended by American Society of Echocardiography [24] LV mass index (g/m2.7) = (0.8*{1.04*[(LVDd + IVSd + PWd)3 – (LVDd)3]} + 0.6)/Height2.7. Where LVDd is left ventricular diastolic dimension, IVSd is interventricular septum thickness at end-diastole, and PWd is posterior wall thick-ness at end-diastole. Relative wall thickness (RWT) was calculated as 2*(PWd)/LVDd. LVEF was calculated from LV diastolic and systolic diameter using the Teichholz method. LV fractional shortening (FS) was calculated as the percent change in the LV internal diameter between diastole and systole. LV mid-wall fractional shortening (MFS) is a measure of LV systolic function which is more reliable in case of LV concentric hypertrophy geometry [25]. LV MFS was calculated as previously described in the guidelines of the American Society of Echocardiography [24]. Peak early mitral E wave velocity, late mitral A wave velocity, the ratio of E wave velocity over A wave velocity (E/A), and deceleration time of E wave velocity were measured from the trans-mitral pulsed Doppler wave profile. We also used E wave velocity/deceleration time of E wave (EDT) as a diastolic function indicator [26]. Diastolic wall strain (DWS) is a recently developed indicator which can evaluate LV myocardial stiffness, and was calculated as (PWs – PWd) / PWs [27, 28]. Where PWs is posterior wall thick-ness at end-systole and PWd is posterior wall thickness at end-diastole. Left atrial dimension was measured on 2D image. We used echocardiography to evaluate LV mass. Cardiac MRI provides more accurate measurements of LV mass than echocardiography, however, cardiac MRI was not performed as part of this study. However, LV mass measurements by echocardiography by the formula we used is closely related to actual LV weight at necropsy (r = 0.90, p < 0.001) in 52 adults and showed excellent reproducibility in a series of 183 hypertensive patients [29, 30]. To our knowledge, there are not any other non-invasive methods to evaluate LV myocardial stiffness rather than DWS. Thus, we chose echocardiography to evaluate LV mass and myocardial stiffness in this study. Furthermore, echo-cardiography is readily available at most institutions and may increase the generalizability of results to a broader population.
Data are presented as mean with standard deviations for normally distributed continuous variables, median with interquartile ranges for non-normally distributed continuous variables and frequencies and proportions for categorical variables. Student’s t-test, Mann-Whitney U test, and Chi-squared testing were used for comparison of variables between two groups if applicable. Because of the well-known differences in leptin levels of men and women, all the following analyses were stratified by sex [11, 31]. We additionally examined the interaction of sex on the relationship between leptin levels and LV mass or myocardial stiffness without stratification by sex. Generalized estimating equations (GEEs) with identity link were used to estimate the association of leptin and cardiac structure and function while accounting for potential correlation among siblings in the study participants. Two models were included in the analyses: Model 1, adjusted for age and BMI; Model 2, adjusted for age, BMI as a continuous variable, systolic blood pressure, anti-hypertensive medication use, past history of diabetes, coronary artery disease, eGFR, and current smoking status. Additionally, the marginal effects of leptin on LV mass and DWS were plotted as previously described [32]. In this analysis, model 2 GEE was performed with adjustment of the sex-specific BMI quartiles instead of BMI, to visualize the relationship between log leptin concentration and LV mass or DWS in each BMI quartiles, and also to examine the interactions between log leptin concentration and the BMI quartiles. P <0.05 was considered statistically significant, and in the analyses stratified by sexes, P < 0.025 was considered significant using Bonferroni correction. All statistical analyses were performed with STATA version 14 (STATA Corp, College Station, TX).
Results
Baseline characteristics of men and women included in our study are shown in Table 1. The participants were predominantly female (72%) and characterized by a high prevalence of hypertension (79%). Women had higher BMI, systolic blood pressure, heart rate, prevalence of hypertension, and LV EF (all p value <0.05). Men had higher diastolic blood pressure, eGFR, rates of smoking, prevalence of dyslipidemia, prevalence of coronary artery disease, LV mass index, and left atrial size (all p value <0.05). LV structure and systolic functional measures were within normal range for both women and men. However, LV relaxation evaluated by E/A ratio was slightly impaired in both. Plasma leptin levels were almost three times higher in women than men (30.9 (21.7 – 42.6) vs 8.8 (5.2 – 13) ng/ml, p <0.001).
Table 1.
Baseline characteristics
| Variables | Men (n = 324) |
Women (n = 848) |
p Value |
|---|---|---|---|
| Age, years | 63.4 ±8.9 | 62.8 ±9.4 | 0.341 |
| BMI, kg/m2 | 29.1 ± 4.8 | 32.4 ± 6.8 | <0.001 |
| Systolic BP, mmHg | 136 ± 20 | 140 ± 21 | 0.007 |
| Diastolic BP, mmHg | 81 ± 10 | 78 ± 11 | <0.001 |
| Heart rate, bpm | 64 ± 12 | 66 ± 11 | 0.002 |
| Hypertension, % | 74.1% | 80.5% | 0.015 |
| Diabetes, % | 26.9% | 28.3% | 0.621 |
| Dyslipidemia, % | 57.1% | 46.6% | 0.001 |
| Coronary artery disease, % | 7.4% | 3.9% | 0.012 |
| Current smoker, % | 20.4% | 11.0% | <0.001 |
| Estimated GFR, mL/min | 94 ± 14 | 84 ± 19 | 0.014 |
| Leptin, ng/ml | 8.8 (5.2–13) | 30.9 (21.7–42.6) | <0.001 |
| Log-Leptin, ng/ml | 2.14 ± 0.78 | 3.37 ± 0.58 | <0.001 |
| LVDd, mm | 53.4 ± 4.5 | 50.2 ± 3.9 | <0.001 |
| LVPWd, mm | 8.5 ± 1.2 | 8.0 ± 1.2 | <0.001 |
| RWT | 0.32 ± 0.05 | 0.32 ± 0.05 | 0.603 |
| LV mass, g | 176 ± 43 | 148 ± 37 | <0.001 |
| LV mass index, g/m2.7 | 37.4 ± 9.3 | 39.0 ± 10.1 | 0.012 |
| LVEF, % | 60.7 ± 5.0 | 62.8 ± 5.0 | <0.001 |
| LVFS, % | 32.8 ± 3.6 | 34.2 ± 3.6 | <0.001 |
| LVMFS, % | 12.8 ± 2.6 | 12.4 ± 2.5 | 0.022 |
| E wave velocity, cm/s | 46.9 ± 13.7 | 47.5 ± 14.1 | 0.493 |
| A wave velocity, cm/s | 59.0 ± 13.0 | 61.1 ± 13.7 | 0.019 |
| E/A | 0.81 ± 0.24 | 0.80 ± 0.26 | 0.578 |
| DT, ms | 175 ± 41 | 174 ± 43 | 0.601 |
| IVRT, ms | 96 ± 18 | 94± 16 | 0.038 |
| DWS | 0.35 ± 0.05 | 0.36 ± 0.05 | 0.004 |
| LAD, mm | 36.4± 5.0 | 35.2± 5.0 | <0.001 |
BP blood pressure, DT deceleration time, DWS diastolic wall strain, IVRT isovolumic relaxation time, LA left atrium, LAD left atrium dimension, LVDd LV dimension at end-diastole, LVEF LV ejection fraction, LVFS LV fractional shortening, LVMFS LV midwall fractional shortening, LVPWd LV posterior wall thickness at end-diastole, RWT relative wall thickness
The associations between leptin levels and LV structure and function are shown in Table 2. Leptin levels were inversely associated with LVPWd (coefficient [95% CI]: −0.252, [−0.376 to −0.129], p <0.001), RWT (−0.009, [−0.015 to −0.004], p = 0.001), LV mass (−5.825, [−9.755 to −1.895], p = 0.004), Left atrial dimension (−0.664, [−1.223 to −0.106], p = 0.020) and positively associated with DWS (0.009, [0.002 – 0.015], p = 0.007) (#all coefficients represents 1 s.d. increase in Log leptin and the unit change in the corresponding outcome) in women after adjustment for confounders (Model 2). Thus, in women, higher leptin levels were associated with less LV concentric hypertrophy and stiffening. In men, leptin levels tended to be negatively associated with LV mass and positively associated with DWS. However, these associations were not statistically significant after adjustment for confounders. There was a significant interaction of sex on the relationship between leptin levels and LV mass (p = 0.029), but not on the relationship between leptin levels and myocardial stiffness (p = 0.974). Leptin levels tended to be negatively associated with LVEF and LVFS, though they were not associated with LVMFS in women. Leptin levels were not associated with any LV systolic function indicators in men. Leptin levels were not associated with LV relaxation abnormalities evaluated by E/A ratio after adjustment for confounding factors in women and men.
Table 2.
Leptin concentration levels were inversely associated with LVM and positively associated with DWS in women
| Variables | Men |
Women |
||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 |
Model 2 |
Model 1 |
Model 2 |
|||||
| Coefficienta (95% CI) | p | Coefficienta (95% CI) | p | Coefficienta (95% CI) | p | Coefficienta (95% CI) | p | |
| LVDd, mm | −0.519 (−1.183, 0.145) | 0.126 | −0.628 (−1.306, 0.051) | 0.070 | −0.078 (−0.496, 0.340) | 0.716 | −0.086 (−0.512, 0.340) | 0.692 |
| LVPWd, mm | −0.021 (−0.182, 0.139) | 0.795 | −0.057 (−0.215, 0.101) | 0.480 | −0.250 (−0.373, −0.127) | <0.001 | −0.252 (−0.376, −0.129) | <0.001 |
| RWT | 0.002 (−0.005, 0.010) | 0.539 | 0.002 (−0.005, 0.009) | 0.550 | −0.009 (−0.015, −0.004) | <0.001 | −0.009 (−0.015, −0.004) | 0.001 |
| LV mass, g | −3.487 (−9.514, 2.540) | 0.257 | −5.011 (−11.026, 1.004) | 0.102 | −5.385 (−9.344, −1.427) | 0.008 | −5.825 (−9.755, −1.895) | 0.004 |
| LVEF, % | −0.036 (−0.740, 0.666) | 0.918 | 0.115 (−0.570, 0.800) | 0.742 | −0.700 (−1.344, −0.056) | 0.033 | −0.686 (−1.340, −0.032) | 0.040 |
| LVFS, % | −0.038 (−0.534, 0.457) | 0.879 | 0.063 (−0.420, 0.546) | 0.798 | −0.532 (−1.002, −0.062) | 0.027 | −0.519 (−0.998, −0.041) | 0.033 |
| LVMFS, % | −0.107 (0.343, 0.129) | 0.372 | −0.066 (−0.296, 0.163) | 0.572 | 0.002 (−0.214, 0.217) | 0.988 | 0.004 (−0.207, 0.215) | 0.971 |
| E/A | −0.035 (−0.104, 0.033) | 0.306 | −0.031 (−0.106, 0.044) | 0.418 | −0.010 (−0.049, 0.029) | 0.617 | −0.013 (−0.053, 0.027) | 0.533 |
| DT, ms | −2.384 (−9.572, 4.805) | 0.516 | −1.651 (−8.634, 5.333) | 0.643 | −1.189 (−6.528, 4.148) | 0.662 | −3.321 (−8.902, 2.261) | 0.244 |
| IVRT, ms | −0.089 (−2.658, 2.478) | 0.945 | −0.375 (−3.119, 2.368) | 0.789 | 0.988 (−0.619, 2.595) | 0.228 | 0.627 (−1.064, 2.317) | 0.468 |
| DWS | 0.006 (−0.001, 0.013) | 0.106 | 0.007 (−0.000, 0.014) | 0.067 | 0.009 (0.003, 0.015) | 0.004 | 0.009 (0.002, 0.015) | 0.007 |
| E/DT | −0.009 (−0.031, 0.013) | 0.415 | −0.111 (−0.036, 0.014) | 0.383 | −0.007 (−0.032, 0.017) | 0.563 | −0.003 (−0.026, 0.019) | 0.766 |
| LAD, mm | 0.049 (−0.679, 0.778) | 0.895 | −0.052 (−0.776, 0.671) | 0.887 | −0.692 (−1.232, −0.151) | 0.012 | −0.664 (−1.223, −0.106) | 0.020 |
DT deceleration time, IVRT isovolumic relaxation time, LVDd left ventricular diastolic dimension at end-diastole, LVEF left ventricular ejection fraction, LVFS left ventricular fractional shortening, LVPWd left ventricular posterior thickness at end-diastole, RWT relative wall thickness
Represents 1 s.d. increase in Log leptin and the unit change in the corresponding outcome. All models account for correlation among family members; Model 1: adjusted for age and BMI. Model 2: adjusted for age, BMI, past history of diabetes, coronary heart disease, systolic blood pressure, blood pressure lowering medication, estimated glomerular filtration rate, and current smoking status
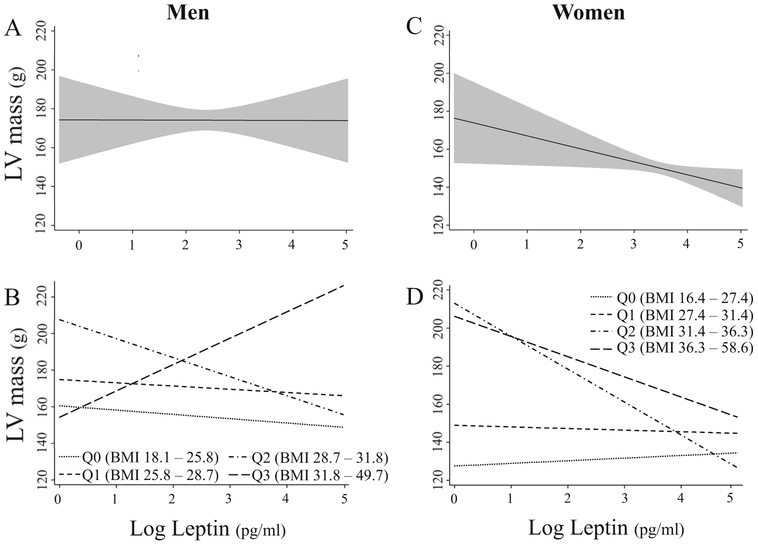
Figure 2 shows the relationships between leptin levels and LV mass (log leptin alone: A [Men], C [Women]; log leptin by sex-specific BMI quartiles: B [Men], D [Women]). The ranges of sex-specific BMI quartiles are 18.1–25.8 k/m2, 25.8–28.7 k/m2, 28.7–31.8 k/m2, 31.8–49.7 k/m2 in men and 16.4–27.4 k/m2, 27.4–31.4 k/m2, 31.4–36.3 k/m2, 36.3–58.6 k/m2 in women. Panels b and d show the effects of BMI (quartiles) on the relationship between leptin levels and LV mass. For obese participants, the coefficients for interactions between leptin levels and the 3rd and 4th BMI quartiles in women are −18.6 (95% CI: −35.8 to −1.5, p = 0.033), and −12.0 (95% CI: −25.8 to 1.9, p = 0.090), respectively. Thus, in women, leptin levels were negatively associated with LV mass only in obese participants. In men, there were no significant interactions between leptin levels and sex-specific BMI quartiles on LV mass.
Fig. 2.
Marginal effect of log leptin concentration on LV mass with a pointwise 95% confidence interval from a linear regression model in men (a), and women (c), and at each BMI quartiles in males (b), and females (d). The model used for a and c included: log leptin concentration, age, sex-specific BMI quartiles, systolic blood pressure, anti-hypertensive medication, past history of diabetes, coronary artery disease, estimated glomerular filtration ratio, and current smoking status. The model used for b and d additionally included interaction term between log leptin concentration and sex-specific BMI quartiles
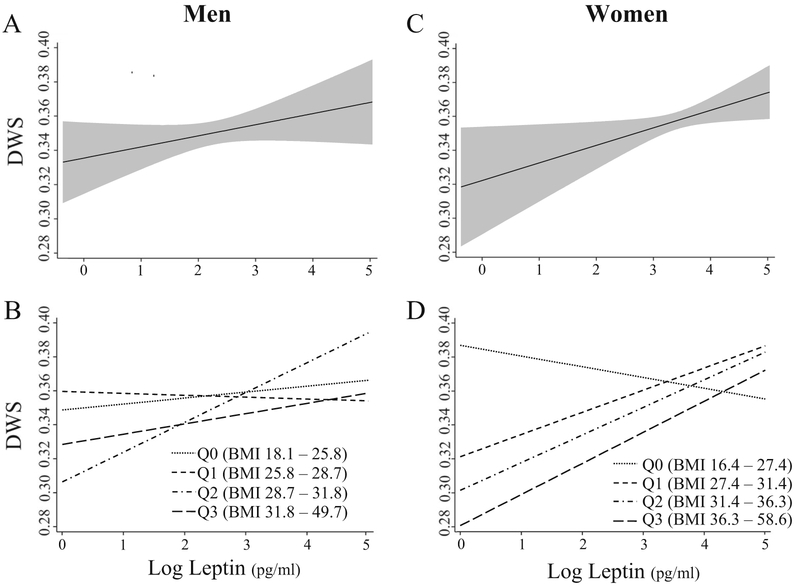
Figure 3 shows the relationships between leptin levels and DWS (log leptin alone: A [Men], C [Women]); log leptin by sex-specific BMI quartile: B [Men], D [Women]). Panels b and d show the effects of the BMI (quartiles) on the relationship between leptin levels and DWS. For those obese participants, the coefficients for the interactions between leptin levels and the 3rd and 4th BMI quartiles in women are 0.023 (95% CI: −0.001 to 0.047, p = 0.065) and 0.025 (95% CI: 0.002–0.047, p = 0.033). Thus, in women, leptin levels were positively associated with DWS only in obese participants. In men, there were no significant interactions between leptin levels and sex-specific BMI quartiles on DWS.
Fig. 3.
Marginal effect of log Leptin concentration on DWS with a pointwise 95% confidence interval from a linear regression model in men (a), and women (c), and at each BMI quartiles in males (b), and females (d). The model used for a and c included: log Leptin concentration, age, sex-specific BMI quartiles, systolic blood pressure, anti-hypertensive medication, past history of diabetes, coronary artery disease, estimated glomerular filtration ratio, and current smoking status. The model used for b and d additionally included interaction term between log leptin concentration and sex-specific BMI quartiles
Discussion
The main findings of this study were that higher plasma leptin levels were associated with lower LV mass and less LV myocardial stiffness after adjustment for confounding factors in obese black women. In men, higher leptin levels also tended to be associated with lower LV mass and less LV myocardial stiffness, but these relationships were not statistically significant. Leptin was associated with reduced LV hypertrophy and stiffening in obese women suggesting a potential protective role against precursors to heart failure.
Several epidemiologic studies have reported positive associations between leptin levels and LV mass [6, 7]. However, in these studies, leptin levels and BMI were also highly correlated. Obesity is closely associated with cardiac hypertrophy and is possibly mediated by increased blood pressure, activation of the renin–angiotensin–aldosterone or sympathetic nervous systems, insulin resistance and hyperglycemia, increased blood volume or arterioscrelosis [33–35]. Thus, the results from the previous studies may be confounded by several factors associated with obesity. After we adjusted for BMI in addition to several possible confounding factors, plasma leptin levels were inversely associated with LV mass in women. Furthermore, the association of leptin with LV mass and LV myocardial stiffness was significant only in higher BMI (obese) participants but not in lower BMI (non-obese) participants. Thus, the results of our study suggest that leptin is negatively associated with LV hypertrophy and myocardial stiffening in obese women.
In ob/ob mice, which develop LV hypertrophy and lack leptin, leptin infusion completely reversed the increases in LV wall thickness compared to calorie-restricted mice had no reduction in wall thickness [36]. In another study, db/db mice lacking functional leptin receptors, cardiac-specific rescue of the leptin receptor led to lower LV wall thicknesses [14]. This is in comparison with db/db mice without functional leptin signaling even though both groups were equally obese, hyperglycemic, and had high plasma trigly-cerides [14]. This experiment directly demonstrates that leptin is not pro-hypertrophic. Our current study further supports the results from studies in experimental animals and suggests a protective effect of leptin against cardiac hypertrophy.
In the present study, higher leptin levels were associated with higher DWS reflecting lower LV diastolic myocardial stiffness. There are very few noninvasive indices of myocardial stiffness; however, we and others have utilized DWS in both animal and human studies. Higher leptin levels were also associated with smaller left atrial dimension and this finding may support the association between higher leptin levels and lower LV diastolic myocardial stiffness. More diastolic LV stiffness would lead to impaired LV filling, increased left atrial pressure and subsequent left atrial dilation. A previous report indicates that cardiac-specific rescue of the leptin receptor in db/db mice improved LV diastolic function, and prevented cardiac triglyceride accumulation [14]. Myocardial steatosis has been associated with LV diastolic dysfunction in humans in several previous studies [37, 38]. In these studies, there were no direct measurements of LV myocardial stiffness, but some showed a higher E/e’ which reflects LV filling pressure in patients with myocardial steatosis compared with the control group. Furthermore, LV dimensions and systolic function were comparable between groups suggesting that patients with myocardial steatosis have increased LV chamber stiffness [38]. Thus, although speculative, it is possible that the inverse relationship between leptin levels and LV myocardial stiffening observed in our study might be due to leptin’s effect to reduce myocardial steatosis in obesity.
In this study, leptin levels tended to be inversely associated with LV EF and FS in women, however, not with LV MFS. In patients with concentric LV hypertrophy, LV systolic function tends to be overestimated by LVEF or LVFS [25, 39]. Thus, conditions which attenuate LV hypertrophy may contribute to reductions in LV EF or LV FS. In this study, leptin levels were not associated with LV MFS, suggesting that leptin is not associated with decreases in LV systolic function.
Our study showed an inverse relationship between leptin levels and LV mass index and myocardial stiffness among black women. It has been reported that leptin levels were inversely associated with LV mass index in the Framingham Heart Study population whose participants are white [11]. Thus, the relationship between leptin levels and LV mass index may not be limited to blacks. Further investigation is warranted to clarify whether the relationship between leptin and LV mass and myocardial stiffness is generalizable to other ethnicities. We did not find a significant association between leptin and LV mass index or LV myocardial stiffness in men. Other studies have shown that leptin levels differ in men and women [11, 31]. It is not clear whether there is a sex difference on the influence of leptin on LV structure and function. However, leptin may have less of an impact on LV structure and function in men compared to women. Previous reports suggest that women exhibit increased cardiac work and lower myocardial efficiency compared to men [40]. Fat storage patterns are different between women and men, and fatty acid utilization is higher in women than men in conditions such as LV hypertrophy [40, 41]. Thus, women may be more susceptible to lipid accumulation and toxicity in the heart. The sex differences found in our results may be related to these previous findings. Of note, the number of male participants in this study was about one third of the female participants. Therefore, the study may be underpowered to detect a significant difference in men, albeit we included 324 men in our analysis.
This study has several strengths. First, to our knowledge, this is the first study to investigate the relationship between leptin levels and LV myocardial stiffness in humans. Second, this study is using a large, diverse, middle-aged and older population, standardized measures of echocardiography, and adequate clinical data for proper assessment. Third, this study investigated LV myocardial stiffness in blacks. There are very little published data on myocardial stiffness in blacks who are disproportionately affected by HFpEF [16, 42]. Finally, we used a direct indicator of LV myocardial stiffness rather than traditional echocardio-graphic measures of diastolic filling which have several limitations including dependency on volume status [43]. However, these findings should be viewed in the context of the following limitations. First, this is a cross-sectional study and therefore, causality cannot be determined. While the population was diverse, it consisted of only blacks. In the GENOA study, only the black cohort (Jackson, MS) had echocardiography performed. Therefore, other large multiethnic studies are warranted to determine the generalizability of our findings to other racial/ethnic groups. Our cohort consisted of individuals belonging to hypertensive families, and may limit applicability to the general population. Although uniform measurement techniques and multiple measures of leptin levels were assessed to minimize the variability (and we adjusted for several possible confounding factors in regression analyses), there is potential for biological variability between the individual participants and it could affect the study results. While the GENOA study has a wide range of covariates for which we adjusted for that may affect cardiac structure and function, there is the possibility that unmeasured confounding may influence the results. Other potential limitations including lack of information related to medications which may have positive myocardial effects (ie diabetes medications including metformin) or lack of coronary angiography or myocardial perfusion scans to rule out significant coronary artery disease are inherent limitations in many epidemiologic studies including ours. Unfortunately, tissue Doppler imaging which provides valuable information related to LV diastolic function was not performed in the GENOA study. We recognize that E/A changes, while important and commonly performed in clinical practice, do not fully evaluate LV diastolic function alone. However, we also evaluated an indicator of myocardial stiffness (DWS) rather than indirect measures of diastolic filling which have limitations, including dependency on volume status. Future large-scale studies with comprehensive analysis of LV diastolic function including tissue Doppler are warranted.
Our results suggest that leptin is associated with lower LV mass and LV myocardial stiffening in obese black women. Left ventricular hypertrophy is a well-known risk factor for heart failure, and LV hypertrophy and LV myocardial stiffness play an important role in the development of HFpEF for which a therapeutic strategy has not been well established [44–46]. Thus, our findings motivate further investigation of the potential cardioprotective role of leptin in preventing or treating heart failure.
In a community-based cohort of blacks, higher plasma leptin levels were independently associated with lower LV mass and decreased LV myocardial stiffness in obese women. This suggests that leptin may play a cardioprotective role against precursors of heart failure in subgroup. Further investigation is warranted to examine whether the findings of this study is generalizable to other ethnic populations.
Acknowledgements
We would like to thank the families that participated in the GENOA study.
Funding This work was supported in part by grants U01-HL054463 (THM) from the National Institutes of Health and M01-RR000585 (IJK) from the Mayo Clinic’s Center for Translational Science Activities, and the Mayo Clinic. MEH is supported by 1K08DK099415 from the National Institutes of Health.
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier JS. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995;1:1311–4. [DOI] [PubMed] [Google Scholar]
- 2.Couillard C, Lamarche B, Mauriege P, Cantin B, Dagenais GR, Moorjani S, Lupien PJ, Despres JP. Leptinemia is not a risk factor for ischemic heart disease in men. Prospective results from the Quebec Cardiovascular Study. Diabetes Care. 1998;21:782–6. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz MW, Seeley RJ, Campfield LA, Burn P, Baskin DG. Identification of targets of leptin action in rat hypothalamus. J Clin Invest. 1996;98:1101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shek EW, Brands MW, Hall JE. Chronic leptin infusion increases arterial pressure. Hypertension. 1998;31:409–14. [DOI] [PubMed] [Google Scholar]
- 5.Leyva F, Anker SD, Egerer K, Stevenson JC, Kox WJ, Coats AJ. Hyperleptinaemia in chronic heart failure. Relationship with insulin. Eur Heart J. 1998;19:1547–51. [DOI] [PubMed] [Google Scholar]
- 6.Paolisso G, Tagliamonte MR, Galderisi M, Zito GA, D’Errico A, Marfella R, Carella C, de Divitiis O, Varricchio M. Plasma leptin concentration, insulin sensitivity, and 24-hour ambulatory blood pressure and left ventricular geometry. Am J Hypertens. 2001;14:114–20. [DOI] [PubMed] [Google Scholar]
- 7.Perego L, Pizzocri P, Corradi D, Maisano F, Paganelli M, Fiorina P, Barbieri M, Morabito A, Paolisso G, Folli F, Pontiroli AE. Circulating leptin correlates with left ventricular mass in morbid (grade III) obesity before and after weight loss induced by bariatric surgery: a potential role for leptin in mediating human left ventricular hypertrophy. J Clin Endocrinol Metab. 2005;90:4087–93. [DOI] [PubMed] [Google Scholar]
- 8.Agata J, Masuda A, Takada M, Higashiura K, Murakami H, Miyazaki Y, Shimamoto K. High plasma immunoreactive leptin level in essential hypertension. Am J Hypertens. 1997;10:1171–4. [DOI] [PubMed] [Google Scholar]
- 9.Wolk R, Berger P, Lennon RJ, Brilakis ES, Johnson BD, Somers VK. Plasma leptin and prognosis in patients with established coronary atherosclerosis. J Am Coll Cardiol. 2004;44:1819–24. [DOI] [PubMed] [Google Scholar]
- 10.Pladevall M, Williams K, Guyer H, Sadurni J, Falces C, Ribes A, Pare C, Brotons C, Gabriel R, Serrano-Rios M, Haffner S. The association between leptin and left ventricular hypertrophy: a population-based cross-sectional study. J Hypertens. 2003;21:1467–73. [DOI] [PubMed] [Google Scholar]
- 11.Lieb W, Sullivan LM, Aragam J, Harris TB, Roubenoff R, Benjamin EJ, Vasan RS. Relation of serum leptin with cardiac mass and left atrial dimension in individuals >70 years of age. Am J Cardiol. 2009;104:602–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajapurohitam V, Gan XT, Kirshenbaum LA, Karmazyn M. The obesity-associated peptide leptin induces hypertrophy in neonatal rat ventricular myocytes. Circ Res. 2003;93:277–9. [DOI] [PubMed] [Google Scholar]
- 13.Madani S, De Girolamo S, Munoz DM, Li RK, Sweeney G. Direct effects of leptin on size and extracellular matrix components of human pediatric ventricular myocytes. Cardiovasc Res. 2006;69:716–25. [DOI] [PubMed] [Google Scholar]
- 14.Hall ME, Maready MW, Hall JE, Stec DE. Rescue of cardiac leptin receptors in db/db mice prevents myocardial triglyceride accumulation. Am J Physiol Endocrinol Metab. 2014;307: E316–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sundstrom J, Bruze G, Ottosson J, Marcus C, Naslund I, Neovius M. Weight loss and heart failure: a nationwide study of gastric bypass surgery versus intensive lifestyle treatment. Circulation. 2017;135:1577–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta DK, Shah AM, Castagno D, Takeuchi M, Loehr LR, Fox ER, Butler KR, Mosley TH, Kitzman DW, Solomon SD. Heart failure with preserved ejection fraction in African Americans: The ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail. 2013;1:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wali RK, Weir MR. Hypertensive cardiovascular disease in African Americans. Curr Hypertens Rep. 1999;1:521–8. [DOI] [PubMed] [Google Scholar]
- 18.Jones DW. What is the role of obesity in hypertension and target organ injury in African Americans? Am J Med Sci. 1999;317:147–51. [DOI] [PubMed] [Google Scholar]
- 19.Krzesinski P, Stanczyk A, Piotrowicz K, Gielerak G, Uzieblo-Zyczkowska B, Skrobowski A. Abdominal obesity and hypertension a double burden to the heart. Hypertens Res. 2016;39:349–55. [DOI] [PubMed] [Google Scholar]
- 20.O’Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–8. [DOI] [PubMed] [Google Scholar]
- 21.Kim CX, Bailey KR, Klee GG, Ellington AA, Liu G, Mosley TH Jr, Rehman H, Kullo IJ. Sex and ethnic differences in 47 candidate proteomic markers of cardiovascular disease: the Mayo Clinic proteomic markers of arteriosclerosis study. PLoS One. 2010;5: e9065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med. 2004;141:929–37. [DOI] [PubMed] [Google Scholar]
- 23.Rigalleau V, Lasseur C, Raffaitin C, Perlemoine C, Barthe N, Chauveau P, Combe C, Gin H. The Mayo Clinic quadratic equation improves the prediction of glomerular filtration rate in diabetic subjects. Nephrol Dial Transplant. 2007;22:813–8. [DOI] [PubMed] [Google Scholar]
- 24.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing G, American Society of Echocardiography’s G, Standards C and European Association of Echocardiography Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. [DOI] [PubMed] [Google Scholar]
- 25.de Simone G, Devereux RB, Roman MJ, Ganau A, Saba PS, Alderman MH, Laragh JH. Assessment of left ventricular function by the midwall fractional shortening/end-systolic stress relation in human hypertension. J Am Coll Cardiol. 1994;23:1444–51. [DOI] [PubMed] [Google Scholar]
- 26.Feissel M, Maizel J, Robles G, Badie J, Faller JP, Slama M. Clinical relevance of echocardiography in acute severe dyspnea. J Am Soc Echocardiogr. 2009;22:1159–64. [DOI] [PubMed] [Google Scholar]
- 27.Ohtani T, Mohammed SF, Yamamoto K, Dunlay SM, Weston SA, Sakata Y, Rodeheffer RJ, Roger VL, Redfield MM. Diastolic stiffness as assessed by diastolic wall strain is associated with adverse remodelling and poor outcomes in heart failure with preserved ejection fraction. Eur Heart J. 2012;33:1742–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takeda Y, Sakata Y, Higashimori M, Mano T, Nishio M, Ohtani T, Hori M, Masuyama T, Kaneko M, Yamamoto K. Noninvasive assessment of wall distensibility with the evaluation of diastolic epicardial movement. J Card Fail. 2009;15:68–77. [DOI] [PubMed] [Google Scholar]
- 29. Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8. [DOI] [PubMed] [Google Scholar]
- 30.Palmieri V, Dahlof B, DeQuattro V, Sharpe N, Bella JN, de Simone G, Paranicas M, Fishman D, Devereux RB. Reliability of echocardiographic assessment of left ventricular structure and function: the PRESERVE study. Prospective randomized study evaluating regression of ventricular enlargement. J Am Coll Cardiol. 1999;34:1625–32. [DOI] [PubMed] [Google Scholar]
- 31.Hickey MS, Israel RG, Gardiner SN, Considine RV, McCammon MR, Tyndall GL, Houmard JA, Marks RH, Caro JF. Gender differences in serum leptin levels in humans. Biochem Mol Med. 1996;59:1–6. [DOI] [PubMed] [Google Scholar]
- 32.Royston P marginscontplot: Plotting the marginal effects of continuous predictors. Stata J. 2013;13:510–27. [Google Scholar]
- 33.Owan T, Litwin SE. Is there a cardiomyopathy of obesity? Curr Heart Fail Rep. 2007;4:221–8. [DOI] [PubMed] [Google Scholar]
- 34.Hosoo S, Koyama M, Watanabe A, Ishida R, Hirata T, Yama-guchi Y, Yamasaki H, Wada K, Higashi Y, Nakamura K. Preventive effect of Eucommia leaf extract on aortic media hypertrophy in Wistar-Kyoto rats fed a high-fat diet. Hypertens Res. 2017;40:546–51. [DOI] [PubMed] [Google Scholar]
- 35.Dimitriadis K, Tsioufis C, Mazaraki A, Liatakis I, Koutra E, Kordalis A, Kasiakogias A, Flessas D, Tentolouris N, Tousoulis D. Waist circumference compared with other obesity parameters as determinants of coronary artery disease in essential hypertension: a 6-year follow-up study. Hypertens Res. 2016;39:475–9. [DOI] [PubMed] [Google Scholar]
- 36.Barouch LA, Berkowitz DE, Harrison RW, O’Donnell CP, Hare JM. Disruption of leptin signaling contributes to cardiac hypertrophy independently of body weight in mice. Circulation. 2003;108:754–9. [DOI] [PubMed] [Google Scholar]
- 37.Rijzewijk LJ, van der Meer RW, Smit JW, Diamant M, Bax JJ, Hammer S, Romijn JA, de Roos A, Lamb HJ. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol. 2008;52:1793–9. [DOI] [PubMed] [Google Scholar]
- 38.Pacifico L, Di Martino M, De Merulis A, Bezzi M, Osborn JF, Catalano C, Chiesa C. Left ventricular dysfunction in obese children and adolescents with nonalcoholic fatty liver disease. Hepatology. 2014;59:461–70. [DOI] [PubMed] [Google Scholar]
- 39.Shimizu G, Hirota Y, Kita Y, Kawamura K, Saito T, Gaasch WH. Left ventricular midwall mechanics in systemic arterial hypertension. Myocardial function is depressed in pressure-overload hypertrophy. Circulation. 1991;83:1676–84. [DOI] [PubMed] [Google Scholar]
- 40.Peterson LR, Soto PF, Herrero P, Mohammed BS, Avidan MS, Schechtman KB, Dence C, Gropler RJ. Impact of gender on the myocardial metabolic response to obesity. JACC Cardiovasc Imaging. 2008;1:424–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall ME, Brinkley TE, Chughtai H, Morgan TM, Hamilton CA, Jordan JH, Stacey RB, Soots S, Hundley WG. Adiposity is associated with gender-specific reductions in left ventricular myocardial perfusion during dobutamine stress. PLoS ONE 2016;11:e0146519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.East MA, Peterson ED, Shaw LK, Gattis WA, O’Connor CM. Racial differences in the outcomes of patients with diastolic heart failure. Am Heart J. 2004;148:151–6. [DOI] [PubMed] [Google Scholar]
- 43.Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol. 2008;51:679–89. [DOI] [PubMed] [Google Scholar]
- 44.Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE and Investigators IP. Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation. 2011;124:2491–501. [DOI] [PubMed] [Google Scholar]
- 45.Zile MR, Baicu CF, Ikonomidis JS, Stroud RE, Nietert PJ, Bradshaw AD, Slater R, Palmer BM, Van Buren P, Meyer M, Redfield MM, Bull DA, Granzier HL, LeWinter MM. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation. 2015;131:1247–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cuspidi C, Sala C, Casati A, Bombelli M, Grassi G, Mancia G. Clinical and prognostic value of hypertensive cardiac damage in the PAMELA study. Hypertens Res. 2017;40:329–35. [DOI] [PubMed] [Google Scholar]