Abstract
Background
The incidence of tuberculosis (TB) is changing in India. The commonest extra pulmonary manifestation of TB is tuberculous lymphadenitis.
Aims and objectives
To detect changes in occurrence of TB lymphadenitis by comparing current data with that from 10 years back.
Methods
Fine Needle Aspiration Cytology (FNAC) findings of patients presenting with lymphadenopathy between January 2014 and December 2015 were included in the study as current data. Cases of TB lymphadenitis were analysed for cyto-morphological patterns and frequency of acid fast bacilli (AFB) positivity. Cytological data of patients with lymphadenopathy between January 2002 and December 2003, were collected from records. Subsequently, comparison was done between previous data and current observation.
Results
Total 302 cases of lymphadenopathy were included in 2014 and 2015. Tuberculous lymphadenitis accounted for 96 (31.7%) cases, among which AFB was present in 47 (49%) cases. Data collected from registers of the years 2002 and 2003 included 318 cases where tuberculous lymphadenitis accounted for 161 (50.6%) cases and AFB was detected in 101 (63%) patients. Maximum AFB positivity was found in smears with caseous necrosis only.
Conclusion
Presently occurrence of TB lymphadenopathy has reduced compared to the period of 2002–2003. Despite this declining trend, the disease continues to be one of the leading causes of lymphadenopathy in both periods.
Keywords: Lymphadenopathy, Tuberculous lymphadenopathy, Trend, Fine needle aspiration cytology (FNAC)
At a glance commentary
Scientific background on the subject
Fine needle aspiration cytology (FNAC) minimizes the requirement of an invasive excisional biopsy. In India as the burden of TB is high and limited resources restrict use of expensive diagnostic techniques, FNAC is being used as a diagnostic tool. Prevalence of all forms of TB as well as mortality rate is on the decline in the country.
What this study adds to the field
Among cases of lymphadenopathy, occurrence of TB lymphadenopathy has decreased in the study period of 2014–2015 in comparison to the period of 2002–2003. However the disease continues to be one of the leading causes of lymphadenopathy in this geographic region. Appropriate interpretation of different morphological patterns of TB lymhadenitis is essential for the cytological diagnosis in the absence of AFB positivity.
In developing countries like India, the incidence of tuberculosis (TB) is high and tuberculous lymphadenitis is the commonest extra pulmonary manifestation of the disease [1]. Extra pulmonary TB accounts for approximately 15–20% of all cases of TB and tuberculous lymphadenitis is encountered in nearly 35% of these cases [2].
Fine needle aspiration cytology (FNAC) is one of the most important diagnostic investigations in the evaluation of tuberculous lymphadenitis. It is a safe, easy and cost effective procedure which minimizes the requirement of an invasive excisional biopsy in majority of cases [3]. Since the burden of TB is high in India and limited resources restrict use of expensive diagnostic techniques in most cases, presence of epithelioid cell granulomas is considered as evidence of tuberculous lymphadenitis, even if AFB are absent in ZN stained smears [4].
Although it is a well-known fact that India bears the largest burden of TB in the world, according to the WHO (World Health Organization) global report 2013, prevalence of all forms of TB is on the decline in the country. The relevant numbers are rather significant with the prevalence of TB in India, in the year 1990, being 465 per lakh, compared to that being 230 per lakh population in 2012. The mortality rate from TB has also significantly decreased [5].
The present study is a novel attempt to find out if the same trend was true for TB lymphadenitis. It was noted by the authors that data regarding occurrence of TB lymphadenitis from the eastern part of the country is rather scarce. No previous study could be found which dealt with the changing trend of TB lymphadenitis, if any, over the years, in this region.
The aim of the present study was to detect changes in the occurrence of TB lymphadenitis among all cases of lymphadenopathy by comparing current data with that available from 10 years back. Emphasis was also imparted to changes in morphological patterns of cytologic smears of TB lymphadenitis and percentage of AFB positivity over the same time span.
Materials and methods
The present study was done in the Department of Pathology of a tertiary care hospital of Kolkata. Patients from different districts of West Bengal as well as from different states of Eastern region of India are being referred in this institution. Cytological findings of patients presenting with lymphadenopathy in the FNAC clinic between January 2014 and December 2015 were included in the study as current data. Before the FNA procedure each patient was evaluated clinically. Cases in which aspirations were done for follow up of the treatment in previously diagnosed patients of TB lymphadenitis or other conditions were excluded. Similarly, cases with inconclusive cytologic diagnosis were not included in the study.
The aspirates were performed using 21- or 22-gauge needle with 10-ml disposable plastic syringe, smears were prepared in standard microscopic slide, stained by Leishman–Giemsa (LG), Hematoxylin & Eosin (H&E) and ZN stains for AFB. Patients diagnosed as tuberculous lymphadenitis were included in the study group. Cases of tuberculous lymphadenitis were specifically analysed for morphological patterns of cytologic smears together with frequency of AFB positivity.
The cytologic smears were morphologically categorized in the same manner as found in a study conducted by Chand P et al. [6] The following categories were delineated -
-
(i)
Caseous necrosis only
-
(ii)
Caseous necrosis with degenerated inflammatory cells
-
(iii)
Caseous necrosis with epithelioid cell granulomas
-
(iv)
Epithelioid cell granulomas without any necrosis
A correlation was performed between the nature of cytologic smear with the percentage of AFB positivity.
Data regarding patients who presented with lymphadenopathy and were subjected to FNA between January 2002 and December 2003, were collected from the record. A comparative analysis in respect to various causes of lymphadenopathy was performed. Subsequently a comparison was done between the previous data and the current observation.
Results
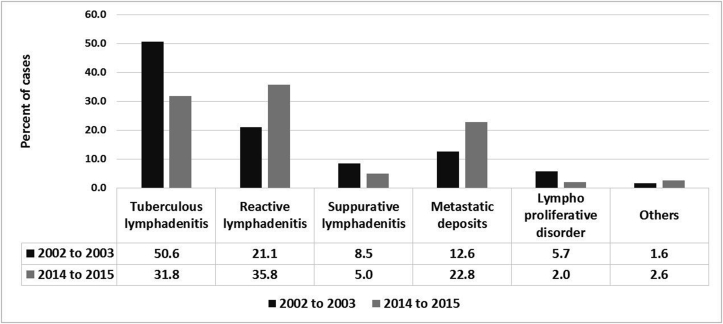
A total of 302 cases of lymphadenopathy were included in 2014 and 2015 in the study group. Tuberculous lymphadenitis accounted for 96 (31.7%) cases. Data collected from registers of the years 2002 and 2003 included 318 cases where tuberculous lymphadenitis accounted for 161 (50.6%). Significant causes of lymphadenopathies, other than tuberculous lymphadenitis, among the study population of 2014–2015 included reactive lymphadenitis in 108 (35.8%) cases and metastatic lymph node in 69 (23%) patients. Data from the previous period of 2002–2003 revealed 67 (21%) cases of reactive lymphadenitis, 40 (12.6%) patients with metastatic deposits in lymph node and 27 (8.5%) cases of suppurative lymphadenitis (Table 1). The category designated as “Others” encompasses some uncommon causes of lymphadenopathies identified in study groups. These included Rosai Dorfman syndrome, Castleman disease, Toxoplasma sp. infestation, Tinea sp. infection, lymphoepithelial lesion and foreign body reactions. Comparison of occurrence of various causes of lymphadenopathies found in the two time period has been shown in Fig. 1, Fig. 2, Fig. 3.
Table 1.
Causes of lymphadenopathies in periods of 2002–2003 and 2014–2015.
| Causes | 2002–2003 |
2014–2015 |
||
|---|---|---|---|---|
| Number of cases | Percent | Number of cases | Percent | |
| Tuberculous lymphadenitis | 161 | 50.6 | 96 | 31.8 |
| Reactive lymphadenitis | 67 | 21.1 | 108 | 35.8 |
| Suppurative lymphadenitis | 27 | 8.5 | 15 | 5.0 |
| Metastatic deposits | 40 | 12.6 | 69 | 22.8 |
| Lympho proliferative disorder | 18 | 5.7 | 6 | 2.0 |
| Others | 5 | 1.6 | 8 | 2.6 |
| Total | 318 | 100.0 | 302 | 100 |
Fig. 1.
Comparison of various causes of lymphadenopathies in patients of the period 2014 to 2015 and 2002 to 2003.
Fig. 2.

Cervical lymphadenopathy in a 30 year old female patient.
Fig. 3.
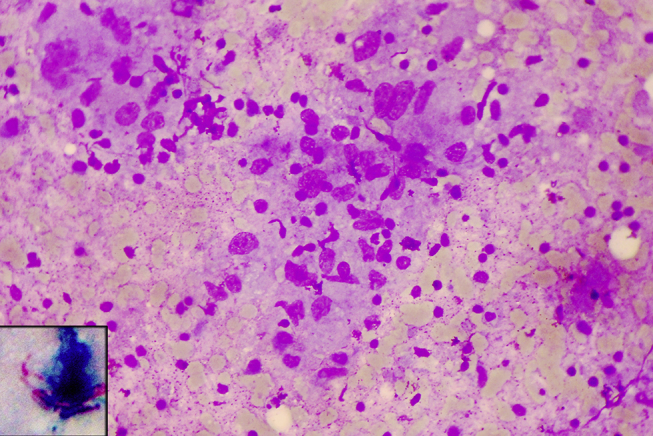
Cytologic smear showing clusters of epithelioid cells in a background of caseous necrosis (LG stain, ×400); Inset shows presence of acid fast bacilli (ZN stain, ×1000).
Data from the years 2002 and 2003 revealed that among 161 (50.6%) patients of tuberculous lymphadenitis, AFB was detected in 101 (63%) cases (Table 2). Age of patients with tuberculous lymphadenitis ranged between 1.5 and 66 years with a mean of 31 ± 1.5 years. The site was cervical region in all but 14 cases, 8 (5%) of which presented with axillary, 3 (1.9%) with inguinal and another 3 (1.9%) with supraclavicular lymphadenopathy.
Table 2.
Comparison of cases of tubercular lymphadenitis in the two time periods.
| Time period | 2002 and 2003 | 2014 and 2015 |
|---|---|---|
| Mean age of patients | 31 ± 1.5 years | 30 ± 2.2 years |
| Total number of lymphadenopathies | 318 | 302 |
| Number of cases of TB lymphadenitis | 161 (50.6%) | 96 (31.7%) |
| AFB positivity | 101 (63%) | 47 (49%) |
Current data of the period 2014 and 2015 revealed that 96 (31.7%) cases among 302 were of tuberculous lymphadenitis, among which 47 (49%) cases showed presence of AFB (Table 2). The age range of patients of tuberculous lymphadenitis was between 11 and 65 years with a mean of 30 ± 2.2 years. All cases were that of cervical lymphadenopathy except 7, 2 (2%) of which presented with axillary, another 2 (2%) with inguinal and 3 (3%) with supraclavicular lymphadenopathy.
Among total 257 cases of tuberculous lymphadenitis in the two time periods, the sex ratio of the patients was 1.6:1 in favour of the female gender. Of the total 620 cases of lymphadenopathies included in the two time periods, 160 (25.8%) cases were in the paediatric age group. Out of these 160 cases, 47 (29%) were those of tuberculous lymphadenitis. Adult patients constituted 460 (74%) cases, of which 210 (45.6%) patients were suffering from tuberculous lymphadenitis.
Out of the total of 257 cases of tuberculous lymphadenitis, 88 (34%) patients were smokers. 172 (66.9%) patients were from the urban areas. Among adult females, 68 (52%) were housewives, 23 (18%) were students and 39 (30%) were workers. Among the adult males, 64 (80%) were workers and 16 (20%) were students.
Frequency of occurrence of tubercular lymphadenitis in the two time periods has been shown in Table 3. This data was compared in Fisher Exact Test, which revealed the two-tailed p value less than 0.0001. Thus the change of occurrence of TB lymphadenitis may be considered as extremely statistically significant (significant at p < 0.01).
Table 3.
Frequency of occurrence of tubercular lymphadenitis in the two time periods.
| Period | TB (Percent) | Non TB (Percent) | Total |
|---|---|---|---|
| 2002 and 2003 | 161 (50.6) | 157 (49.4) | 318 |
| 2014 and 2015 | 96 (31.8) | 206 (68.2) | 302 |
| Total cases | 257 (41.5) | 363 (58.5) | 620 |
Study of the morphologic categories of smears of tuberculous lymphadenitis revealed that maximum AFB positivity was found in smears with caseous necrosis only. The least positivity was found in smears with epithelioid cell granulomas without any necrosis. This pattern was found to be similar in both sets of data (Table 4, Table 5). Chi square test was performed to assess the significance between AFB positivity and morphological categories among all tubercular lymphadenitis cases in the two time periods (Table 6). High possibility of AFB positivity was noted in cases with only caseous necrosis in smears (significant at p < 0.01). In contrast if there if only Epithelioid cell granulomas without any necrosis there is high probability of AFB negativity (significant at p < 0.01).
Table 4.
Correlation between morphologic appearance of cytological smears and AFB positivity among cases of the period 2014 and 2015.
| Nature of smears | Number of cases (percent) |
||
|---|---|---|---|
| AFB positive | AFB negative | Total | |
| Caseous necrosis only | 15 (88%) | 2 (12%) | 17 (18%) |
| Caseous necrosis with degenerated inflammatory cells | 17 (61%) | 11 (39%) | 28 (29%) |
| Caseous necrosis with epithelioid cell granulomas | 13 (59%) | 9 (41%) | 22 (23%) |
| Epithelioid cell granulomas without any necrosis | 2 (7%) | 27 (93%) | 29 (30%) |
| Total | 47 (49%) | 49 (51%) | 96 (100%) |
Table 5.
Correlation between morphologic appearance of cytological smear and AFB positivity among cases of the period 2002 and 2003.
| Nature of smears | Number of cases (percent) |
||
|---|---|---|---|
| AFB positive | AFB negative | Total | |
| Caseous necrosis only | 28 (93%) | 2 (7%) | 30 (19%) |
| Caseous necrosis with degenerated inflammatory cells | 39 (71%) | 16 (29%) | 55 (34%) |
| Caseous necrosis with epithelioid cell granulomas | 31 (74%) | 11 (26%) | 42 (26%) |
| Epithelioid cell granulomas without any necrosis | 3 (9%) | 31 (91%) | 34 (21%) |
| Total | 101 (63%) | 60 (37%) | 161 (100%) |
Table 6.
Chi square test for significance of AFB positivity in different morphological categories of smears.
| Nature of smears | Number of cases (percent) |
p value | ||
|---|---|---|---|---|
| AFB positive | AFB negative | Total | ||
| Caseous necrosis only | 43 (91.5) | 4 (8.5) | 47 | <0.00001. (significant at p < 0.01) |
| Caseous necrosis with degenerated inflammatory cells | 56 (67.5) | 27 (32.5) | 83 | 0.02683. (significant at p < 0.05) |
| Caseous necrosis with epithelioid cell granulomas | 44 (68.7) | 20 (31.3) | 64 | 0.03706. (significant at p < 0.05) |
| Epithelioid cell granulomas without any necrosis | 5 (7.9) | 58 (92.1) | 63 | <0.00001 (significant at p < 0.01) |
| Total | 148 (57.6) | 109 (42.4) | 257 | |
Discussion
One of the commonest causes of lymphadenopathy in developing countries is TB lymphadenitis. FNAC is a first line investigation for evaluation of any lymphadenopathy. In case of suspected TB lymphadenitis, the aspirated material is stained with ZN stain to confirm the presence of the causative organism [2]. Nidhi P et al. stated that FNAC is both safe and sensitive for the diagnosis of TB lymphadenitis [7].
Jha BC et al. reported in their study, conducted in Chandigarh, a high incidence of TB lymphadenitis (63.8%) in the year 2001 [8]. On the other hand, a study conducted in the year 2013 by Roy A et al. in a tertiary care hospital of south India reported the incidence of TB lymphadenitis to be 18% [9]. A thorough search of available literature reveals very few studies of similar nature from West Bengal. One of them was conducted by Mitra S et al. who reported an incidence of TB lymphadenitis of 46.7% in the year 2013 [10]. This result does not conform to that found in the present study, which further highlights the fact that an enriched database is indeed required from this part of the country to arrive at definitive conclusions. The present study is one of the first attempts at highlighting any changing trends in the incidence of TB lymphadenitis over the years. Such epidemiological studies are of utmost importance in understanding the various facets of this infectious disease which still takes a heavy toll on the quality of lives of inhabitants of developing countries like India.
The two sets of data collected in the present study show a trend towards decline in the occurrence of TB lymphadenitis over the years, in accordance with WHO data regarding TB in India [5]. Data from the years 2002 and 2003 revealed an incidence of 50.7% whereas that collected in the years 2014 and 2015 showed that the incidence of TB lymphadenitis has reduced to 31.7%. This decline of incidence probably reflects an improvement environmental hygiene and also easy availability of treatment facilities which may contribute to the reduction of spread of the disease to the community with the passage of time.
Mohapatra PR et al. found maximum incidence of TB lymphadenitis in the second and third decades and they stated that the disease rarely affects patients in their extremes of age [4]. A female preponderance of TB lymphadenitis has been reported in most Indian studies [1], [4], [7].
The most common site affected by TB lymphadenitis is the cervical region. Various authors have reported that solitary lymphadenopathy is the commonest mode of presentation [1], [6]. However it must be recalled that the commonest cause of supraclavicular lymphadenopathy is metastatic deposits of malignant tumour. Mitra S et al. studied 215 patients of supraclavicular lymphadenopathy and reported only 28 (14.2%) cases of TB lymphadenitis among them [11].
AFB positivity in smears of patients of TB lymphadenitis was found to be 71% in a study conducted by Nidhi P et al. [7] In this study 63% cases in the years 2002 and 2003 showed presence of AFB. Chand P et al. however found a lower incidence of AFB positivity of 44.5% [6]. Authors of the present study noted AFB positivity to be 49% in the years 2014 and 2015. It was noted that AFB positivity ranges from 10% to 70% in various studies conducted over the years [12].
AFB positivity was most commonly found in those smears in which there was only caseous necrosis present. Nidhi P et al. found similar correlation between morphologic appearance of cytologic smear and AFB positivity in cases of TB lymphadenitis [7].
Other diagnostic methods of TB lymphadenitis include culture and polymerase chain reaction (PCR). However culture is time consuming and PCR is expensive. Demonstration of acid fast bacilli (AFB) by Ziehl Neelson (ZN) stain of cytologic smears is a simple yet reliable test for conclusively diagnosing tuberculous lymphadenitis. ZN stained smear, as a diagnostic modality, has positive predictive value of 100% and negative predictive value of 83.33% [13].
Mitra S et al. stated in their study that FNAC must be regarded as an accurate and reliable first line investigation for patients presenting with lymphadenopathy [10]. However interpretation of FNAC smears requires expertise and reporting should be done only after taking into account relevant history and reports of laboratory and radiological investigations [14]. This is mostly due to the fact that FNAC is a blind procedure and the needle may not always reach the representative area of the lesion. Whenever in doubt, a repeat aspiration is advised before rendering a diagnosis [6].
There were however few limitations of the present study. The incidence of pulmonary tuberculosis in the patients of tuberculous lymphadenitis was not studied. It was not recorded whether the patients were suffering from any systemic illness at the time. It was beyond the scope to undertake culture or PCR for detection of tuberculous infection. The study compared the incidence of TB lymphadenitis between two years (2002–2003 and 2014–2015) separately and not in consecutive years.
To conclude, the present study revealed that occurrence of TB lymphadenopathy has reduced in the study period of 2014–2015 when compared to the period of 2002–2003 among the cases of lymphadenopathy. The study also corroborated the fact that though TB lymphadenitis has declined over the last 10 years, in this geographic region, the disease continues to be one of the leading causes of lymphadenopathy in developing countries. As many cases of TB lymphadenitis did not reveal AFB positivity, a meticulous interpretation of different morphological patterns of TB lymhadenitis is essential for appropriate cytological diagnosis.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Khajuria R., Goswami K.C., Singh K., Dubey V.K. Pattern of lymphadenopathy on fine needle aspiration cytology in Jammu. JK Sci. 2006;8:158–160. [Google Scholar]
- 2.Hemalatha A., Shruti P., Kumar M.U., Bhaskaran A. Cytomorphological patterns of tubercular lymphadenitis revisited. Ann Med Health Sci Res. 2014;4:393–396. doi: 10.4103/2141-9248.133466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakhey M., Bhatta C.P., Mishra S. Diagnosis of tubercular lymphadenopathy by fine needle aspiration cytology, acid-fast staining and mantoux test. J Nepal Med Assoc. 2009;48:230–233. [PubMed] [Google Scholar]
- 4.Mohapatra P.R., Janmeja A.K. Tuberculous lymphadenitis. J Assoc Phys India. 2009;57:585–590. [PubMed] [Google Scholar]
- 5.Gupta R.S. Update on revised national tuberculosis programme. Indian J Tuberc. 2014;60:30–34. [PubMed] [Google Scholar]
- 6.Chand P., Dogra R., Chauhan N., Gupta R., Khare P. Cytopathological pattern of tubercular lymphadenopathy on FNAC: analysis of 550 consecutive cases. J Clin Diagn Res. 2014;8:FC16–FC19. doi: 10.7860/JCDR/2014/9956.4910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nidhi P., Sapna T., Shalini M., Kumud G. FNAC in tuberculous lymphadenitis: experience from a tertiary level referral centre. Indian J Tuberc. 2011;58:102–107. [PubMed] [Google Scholar]
- 8.Jha B.C., Dass A., Nagarkar N.M., Gupta R., Singhal S. Cervical tuberculous lymphadenopathy: changing clinical pattern and concepts in management. Postgrad Med J. 2001;77:185–187. doi: 10.1136/pmj.77.905.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roy A., Kar R., Basu D., Badhe B.A. Spectrum of histopathologic diagnosis of lymph node biopsies: a descriptive study from a tertiary care center in South India over 5½ years. Indian J Pathol Microbiol. 2013;56:103–108. doi: 10.4103/0377-4929.118692. [DOI] [PubMed] [Google Scholar]
- 10.Mitra S., Ray S., Mitra P.K. Analysis of FNAC of cervical lymph nodes: experience over a three-year period. J Indian Med Assoc. 2013;111:599–602. [PubMed] [Google Scholar]
- 11.Mitra S., Ray S., Mitra P.K. Fine needle aspiration cytology of supraclavicular lymph nodes: our experience over a three-year period. J Cytol. 2011;28:108–110. doi: 10.4103/0970-9371.83465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar H., Chandanwale S.S., Gore C.R., Buch A.C., Satav V.H., Pagaro P.M. Role of fine needle aspiration cytology in assessment of cervical lymphadenopathy. Med J DY Patil Univ. 2013;6:400–404. [Google Scholar]
- 13.Mudduwa L.K., Nagahawatte A.S. Diagnosis of tuberculous lymphadenitis: combining cytomorphology, microbiology and molecular techniques - a study from Sri Lanka. Indian J Pathol Microbiol. 2008;51:195–197. doi: 10.4103/0377-4929.41680. [DOI] [PubMed] [Google Scholar]
- 14.Hafez N.H., Tahoun N.S. Reliability of fine needle aspiration cytology (FNAC) as a tool in cases of cervical lymphadenopathy. J Egypt Natl Canc Inst. 2011;23:105–114. doi: 10.1016/j.jnci.2011.09.009. [DOI] [PubMed] [Google Scholar]