Abstract
With further advances in medical genetics, genetic tests to determine predisposition to disease are becoming viable for a growing number of diseases. Accordingly, it has also become important to identify various viewpoints on genetic testing. The aims of this study were to examine awareness of and attitudes toward genetic testing among the general public (public), cancer patients (patients), and health-care professionals (clinicians and researchers) in Korea. The present survey was conducted from November 2016 to February 2017. The public and patients were surveyed via face-to-face interviews conducted by trained interviewers. Health-care professionals were surveyed via self-administered questionnaires. In total, 1500 individuals from the general public, 1500 cancer patients, 113 clinicians, and 413 researchers were surveyed. Most respondents from the public and patients had previously heard about genetic testing (public, 89.4%; patients, 92.7%, p < 0.01). Differences in attitudes toward genetic testing among the public, patients, and professionals were noted, although most respondents in the present study were aware of genetic testing. Most of the cancer patients tended to overestimate the potential benefit of genetic testing, whereas clinicians expressed concerns for genetic testing. Providing correct information to people who are scheduled to undergo or order genetic testing could help in making an informed decision thereon.
Introduction
Improved understanding of medical genetics has allowed clinicians to employ the use of genetic testing for personalized approaches to disease prevention and treatment [1]: for example, genetic testing for BRCA mutation has been widely used to identify cancer predisposition [2]. With further advances in medical genetics, genetic tests to determine predisposition to disease are becoming viable for a growing number of diseases, including cancer, dementia, and diabetes [3, 4].
Consequently, identifying differences in viewpoints on genetic testing has grown in importance, and studies have begun to assess awareness and attitudes toward genetic testing among people throughout the world [1, 3–11]. Overall, most of these studies have focused on particular demographic groups or specific medical conditions, and while recent literature reviews suggest that public attitudes toward genetic testing are positive, they have been found to vary according to sex, age, education level, health status, etc [4]. Few studies have examined patient attitudes toward genetic testing in cancer care [9, 12, 13], and only a limited number of studies have reported on knowledge of genetic testing among health-care professionals [6]. In addition, most prior studies have been carried out in the US or Europe countries. Although some of those studies assessed the awareness of and attitude toward genetic testing by stratifying race/ethnicity, the authors concluded that their results should not be generalized for countries other than the ones that were studied [10]. As medical practices vary widely among different regions around the world due to differences in sociopolitical, economical, and cultural environments, people from different regions may have drastically different attitudes toward genetic testing [14].
To our knowledge, research has yet to exhaustively explore public awareness of and attitudes toward genetic testing in Asia, such as India, Japan, Taiwan, China, and South Korea, and the few that have attempted to do so suggest a need to increase awareness [15–18]. Accordingly, through the present study, we sought (1) to examine awareness of genetic testing in Korea; (2) to assess difference in attitudes toward genetic testing among the general public, cancer patients, and health-care professionals; and (3) to suggest ways in which to improve and utilize knowledge of genetic testing for better patient care.
Materials and methods
Study participants
We surveyed the general public (n = 1500), cancer patients (n = 1500), and health-care professionals (n = 542) in Korea. Three different sampling methods were employed for each study group, and data collection was carried out during the period from November 2016 to February 2017. People who were not able to communicate were excluded from this survey. We collected data from the general public using a purposive sampling method. We approached participants asking their age (20–64 years), gender, and location of residency in order to make the distributions thereof in our sample population analogous to those for the general Korean population. We recruited cancer patients using a quota sampling method. As there are five major cancers in Korea (gastric, colon, lung, breast, and gynecological cancer), we assigned a sample size of 300 observations to each of those five major cancer subgroups and recruited cancer patients who had visited the National Cancer Center or Samsung Medical Center in Seoul. We collected data from health-care professionals, including clinicians, nurses, professors, and researchers, using a convenience sampling method, at the 21st Annual Fall Symposium of the Korean Cancer Association, one of the largest oncologic symposiums, held on November 18, 2016.
Conduction of survey
We requested a professional research company to review our survey instruments and carry out the survey. In addition, we obtained verbal agreement from all participants prior to proceeding with the survey. The public and patients were surveyed via face-to-face interviews conducted by trained interviewers in order to prevent them from misunderstanding the concepts or terminology regarding genetic testing. Health-care professionals were surveyed via self-administered questionnaires. The institutional review boards of the National Cancer Center and Samsung Medical Center Seoul approved the study protocol (IRB #NCC 2016-0256 and #SMC 2016-12-040-001).
Survey design
To design the survey, we conducted a thorough review of the literature [19–22] and received consultation with health-care experts in the field. The survey contained 69 items divided into four sections: sociodemographic (14 items), big data (18 items), precision medicine (12 items), and genetic testing (25 items). The genetic testing section assessed awareness of and attitudes toward general genetic testing and testing for BRCA 1/2 mutation.
Awareness of genetic testing
This study assumed that health-care professionals had much greater awareness of genetic testing than the public and patients. Therefore, we assessed awareness of genetic testing among the public and patients with the following research questions: (1) “What comes to mind when you hear the word ‘genetic testing’?” (Short-answer response), (2) “Have you ever heard of genetic testing?” (3) “From what sources have you read or heard of genetic testing?” and (4) “What kinds of genetic tests would you be willing to undergo?”
Attitudes toward genetic testing
Eight questions were used to evaluate attitudes toward genetic testing among the public, patients, and health-care professionals. Responses to these questions were reported on a four-point Likert scale, with possible responses ranging from “strongly agree” (1) to “strongly disagree” (4).
Statistical analysis
Descriptive statistics were analyzed to summarize the respondents’ general characteristics, awareness of genetic testing, and attitudes toward genetic testing. Chi-square tests and one-way analysis of variance test with Scheffe post-hoc test were used to compare differences among the study groups. Multivariate logistic regression models were used to evaluate associations between demographic characteristics and awareness of genetic testing. This analysis was also conducted to identify differences in levels of awareness of genetic testing among cancer patients. All analyses were conducted using STATA, version 12.1 (StataCorp LP., College Station, TX). Statistical significance for all analyses was set at P-value <0.05.
Results
General characteristics
In total, 3542 participants were surveyed. The public sample group comprised 1500 participants. Of the 1500 surveyed participants in the patients sample group, 300 had gastric cancer, 300 had colon cancer, 300 had lung cancer, 300 had breast cancer, and 300 had gynecological cancer. Health-care professionals comprised 542 participants. From the public sample group, four respondents who had cancer were excluded. Also, 16 respondents among the health-care professionals were excluded owing to incomplete questionnaires. Finally, 3522 respondents were analyzed in this study. For more accurate analysis, health-care professionals were categorized as clinicians and researchers due to differences in their characteristics.
Characteristics of the respondents
The characteristics of the respondents are summarized in Table 1. The average ages of the respondents among the public, patients, clinicians, and researchers were 43.0 (range, 20–64 years), 56.0 (range, 20–85 years), 40.9 (range, 26–67 years), and 33.7 years (range, 21–60 years), respectively. The proportions of females among the sample groups were 48.3%, 60.1%, 47.8%, and 69.0%, respectively. Among respondents in the public and patients sample groups, 46.7% and 38.4% reported a college-level education or higher, whereas all respondents among the clinicians and researchers reported a college-level education or higher.
Table 1.
Comparison of sociodemographic characteristics among the general public, cancer patients, clinicians, and researchers
| Variables | General public (n = 1496) |
Cancer patients (n = 1500) |
Clinicians (n = 113) |
Researchers (n = 413) |
P-valueb |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Sex | <0.01 | ||||
| Male | 773 (51.7)1 | 599 (39.9)2 | 59 (52.2)1,2,3 | 128 (31.0)3 | |
| Female | 723 (48.3) | 901 (60.1) | 54 (47.8) | 285 (69.0) | |
| Age, years | <0.01 | ||||
| Mean (SD) | 43.0 (12.0)1 | 56.0 (11.1) | 40.9 (8.5)1 | 33.7 (8.0) | |
| 20–39 | 615 (41.1) | 109 (7.3) | 53 (46.9) | 320 (77.5) | |
| 40–49 | 381 (25.5) | 313 (20.9) | 40 (35.4) | 71 (17.2) | |
| ≥50 | 500 (33.4) | 1078 (71.9) | 20 (17.7) | 22 (5.3) | |
| Education level | <0.01 | ||||
| ≤High school graduate | 797 (53.3)1 | 924 (61.6)1 | — | — | |
| College graduate | 687 (45.9) | 522 (34.8) | 15 (13.3) | 175 (42.4) | |
| Graduate degree | 12 (0.8) | 54 (3.6) | 98 (86.7) | 232 (56.2) | |
| Household monthly income | <0.01 | ||||
| <$3,000 | 261 (17.5) | 668 (44.5) | — | 70 (17.0) | |
| $3000–$4999 | 864 (57.8) | 592 (39.5) | 10 (8.9) | 93 (22.5) | |
| ≥$5,000 | 371 (24.8) | 240 (16.0) | 103 (91.2) | 219 (53.0) | |
| Living area | <0.01 | ||||
| Metroa | 1051 (70.3) | 944 (62.9) | 105 (92.9)1 | 377 (91.3)1 | |
| Non-metro | 445 (29.8) | 556 (37.1) | 8 (7.1) | 36 (8.7) | |
| Health status | <0.01 | ||||
| Excellent/good | 1024 (68.5)1 | 665 (44.3) | 76 (67.3)1,2 | 231 (55.9)2 | |
| Fair/poor | 472 (31.6) | 835 (55.7) | 37 (32.7) | 182 (44.1) | |
| Private health insurance | <0.01 | ||||
| Yes | 1280 (85.6) | 1116 (74.4)1 | 66 (58.4)2 | 286 (69.2)1,2 | |
| No | 216 (14.4) | 384 (25.6) | 47 (41.6) | 127 (30.8) | |
| Days of physical activity per week | <0.01 | ||||
| 0–2 days | 1110 (74.2)1,2 | 1188 (79.2)1,3 | 80 (70.8)2,3,4 | 274 (66.3)4 | |
| 3–7 days | 386 (25.8) | 312 (20.8) | 33 (29.2) | 139 (33.7) | |
| Ever heard of genetic testing? | <0.01 | ||||
| Yes | 1338 (89.4) | 1391 (92.7) | — | — | |
| No | 158 (10.6) | 107 (7.3) | — | — |
1–4Values with the same number are not significantly different
aMetro was defined as a city with a population of >500,000 individuals
bP-value was tested by ANOVA with Scheffe’s post-hoc test (p < 0.05)
Awareness of genetic testing
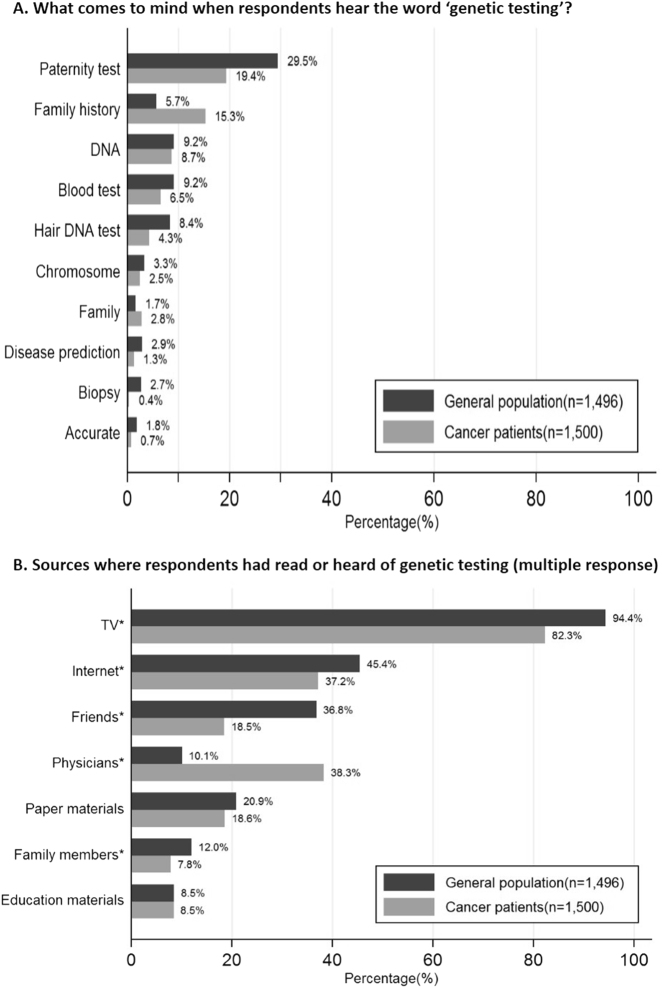
As shown in Table 1, 89.4% of the public and 92.7% of the patients had previously heard about genetic testing. Female respondents were more likely to be aware of genetic testing than male respondents (89.9% vs. 89.0% in the public; 94.0% vs. 90.8% in the patients; respectively). Awareness of genetic testing among the public and patients is presented in Fig. 1. In response to the question “What comes to mind when you hear the word ‘genetic testing’?”, 29.5% of the public and 19.4% of the patients answered “paternity test.” The majority of the public had read or heard of genetic testing from TV (94.4%), the Internet (45.4%), and friends (36.9%). Among the patients, the majority respondents had read or heard of genetic testing from TV (82.3%), clinicians (38.3%), and the Internet (37.2%).
Fig. 1.
a Responses to the question, “What comes to mind when you hear the word ‘genetic testing’?” b Sources from where respondents had read or heard about genetic testing (multiple response) Asterisk (*) indicates a P-value <0.05 for differences between the general public and cancer patients, χ2 test
The most common the type of genetic testing that respondents reported being willing to undergo was that for dementia (public, 17.1%; patients, 29.3%). Among the public sample group, genetic testing for obesity (14.5%) and gastric cancer (12.6%) were frequently reported. Among the patients, genetic testing for breast cancer or ovarian cancer (19.1%) and gastric cancer (19.0%) were reported. The most common reasons why respondents wanted to undergo genetic testing were to prevent diseases and to know their family history of disease.
In multivariate logistic regression analysis controlling for sex, age, education level, and monthly household income, patients showed a significant association with awareness of genetic testing (Table 2). Females were significantly more likely to be aware of genetic testing than males, and respondents with a monthly household income of $5,000 or more were significantly more likely to be aware of genetic testing than the other income groups. Also, respondents who lived in non-metro areas and who had a health status of fair or poor were inversely associated with awareness of genetic testing. Of the cancer patients, those with gynecological cancer were significantly more likely to be aware of genetic testing than those with other cancer types (adjusted odds ratio = 2.7, 95% confidence interval (CI) = 1.5–4.9).
Table 2.
Predictors of awarenessa of genetic testing among respondents from the general public and cancer patients
| Variables | Total (n = 2996) |
Cancer type | ||||
|---|---|---|---|---|---|---|
| Gastric (n = 300) |
Lung (n = 300) |
Colon (n = 300) |
Breast (n = 300) |
Gynecological (n = 300) |
||
|
n (%)/ AORb (95% CI) |
n (%)/ AOR (95% CI) |
n (%)/ AOR (95% CI) |
n (%)/ AOR (95% CI) |
n (%)/ AOR (95% CI) |
n (%)/ AOR (95% CI) |
|
| Awareness of genetic testing | 2729 (91.1) | 275 (91.7) | 270 (90.0) | 277 (92.3) | 283 (94.3) | 286 (95.3) |
| Type | ||||||
| General | Reference | Reference | Reference | Reference | Reference | Reference |
| Cancer | 2.1 (1.5–2.9) | 1.8 (1.1–3.0) | 1.7 (1.0–2.7) | 1.9 (1.1–3.2) | 2.0 (1.2–3.6) | 2.7 (1.5–4.9) |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 0.8 (0.6–0.97) | 0.5 (0.2–1.4) | 1.4 (0.6–3.5) | 0.9 (0.4–2.3) | — | — |
| Age, yearsc | ||||||
| <56 | Reference | Reference | Reference | Reference | Reference | Reference |
| ≥56 | 0.8 (0.6–1.1) | 0.5 (0.2–1.7) | 0.1 (0.01–0.9) | 1.0 (0.4–2.8) | 1.0 (0.3–3.4) | 0.3 (0.1–1.0) |
| Education level | ||||||
| ≤High school graduate | Reference | Reference | Reference | Reference | Reference | Reference |
| College graduate | 1.3 (1.0–1.7) | 1.4 (0.5–4.4) | 1.8 (0.5–6.6) | 3.8 (0.8–17.4) | 1.3 (0.4–4.2) | 0.7 (0.2–2.8) |
| Graduate degree | 1.4 (0.5–4.0) | — | — | 0.7 (0.1–7.4) | 1.1 (0.1–10.9) | 0.5 (0.1–4.9) |
| Household monthly income | ||||||
| <$3000 | Reference | Reference | Reference | Reference | Reference | Reference |
| $3000–$4999 | 1.1 (0.8–1.5) | 1.6 (0.5–4.5) | 1.6 (0.5–4.7) | 0.7 (0.3–2.0) | 1.9 (0.6–5.9) | 1.0 (0.3–3.7) |
| ≥$5000 | 1.6 (1.0–2.4) | 3.5 (0.4–29.3) | 0.4 (0.1–1.4) | 1.5 (0.3–7.7) | 1.1 (0.1–10.9) | 1.4 (0.2–8.4) |
| Living area | ||||||
| Metro | Reference | Reference | Reference | Reference | Reference | Reference |
| Non-metro | 0.7 (0.5–0.9) | 0.5 (0.2–1.2) | 0.7 (0.3–1.6) | 1.6 (0.6–4.2) | 1.3 (0.4–3.7) | 1.2 (0.3–3.9) |
| Private health insurance | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.3 (1.0–1.8) | 1.4 (0.5–3.7) | 2.0 (0.8–4.8) | 1.4 (0.5–3.7) | 1.3 (0.3–5.0) | 1.7 (0.5–5.9) |
| Health status | ||||||
| Excellent/good | Reference | Reference | Reference | Reference | Reference | Reference |
| Fair/poor | 0.7 (0.5–0.9) | 0.9 (0.4–2.0) | 1.1 (0.5–2.6) | 0.9 (0.4–2.0) | 0.3 (0.1–1.1) | 0.8 (0.2–3.0) |
| Days of physical activity per week | ||||||
| 0–2 days | Reference | Reference | Reference | Reference | Reference | Reference |
| 3–7 days | 1.2 (0.9–1.6) | 0.4 (0.2–1.1) | 1.5 (0.4–5.5) | 0.4 (0.2–1.1) | 0.4 (0.1–1.1) | 1.2 (0.2–5.9) |
Note: Boldface indicates statistical significant (p < 0.05)
aAwareness was recorded in instances where respondents had ever heard of “genetic testing”
bAOR, adjusted odds ratio; adjusted for sex, age, household income, and education level
cThe mean ages (years) of respondents by cancer type: gastric (60.0), lung (61.7), colon (58.4), breast (50.2), and gynecological (50.2)
Attitudes toward genetic testing
The respondents’ attitudes toward genetic testing are presented in Table 3. In all, 73.2% of the public and 67.7% of the patients agreed that genetic testing should be included in the national health screening program, whereas only 30.1% of clinicians agreed. The majority of respondents from all groups agreed that “If genetic testing was free, I would take the test,” (public, 89.3%; patients, 94.3%; clinicians, 88.5%; and researchers, 93.7%) and that people have the right to know about their genes in order to be able to protect their own health and lives (public, 85.4%; patients, 87.5%; clinicians, 70.8%; and researchers, 84.2%). Most respondents expressed that the results of genetic tests would help them and their doctor with planning (public, 85.9%; patients, 96.4%; clinicians, 91.1%; and researchers, 95.2%). More than two thirds of respondents in the public (67.4%) and patient (78.7%) sample groups agreed that “I would provide the results of genetic tests to the government,” whereas 54.0% of clinicians agreed. When asked whether knowledge of test results may lead to discrimination, most respondents (public, 70.7%; patients, 68.8%; clinicians, 87.6%; and researchers, 81.4%) expressed concerns. More than two thirds of the respondents in the public (76.3%) and patient (67.5%) sample groups agreed with the statement “I would not like to marry someone who had a positive genetic test result,” whereas 59.8% and 52.2% of clinicians and researchers agreed with the statement.
Table 3.
Attitudes toward genetic testing among the general public, cancer patients, clinicians, and researchers
| Question | General public (n = 1496) |
Cancer patients (n = 1500) |
Clinicians (n = 113) |
Researchers (n = 413) |
P-valuea |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Genetic testing should be included to national health screening program | 1095 (73.2)1 | 1016 (67.7)1 | 34 (30.1) | 207 (50.1) | <0.01 |
| People have the right to know about their genes to be able to protect their own health and lives | 1277 (85.4)1,2 | 1312 (87.5)1,3 | 80 (70.8) | 347 (84.2)2,3 | <0.01 |
| If genetic testing was free, I would take the test | 1336 (89.3)1,2 | 1419 (94.3)3,4 | 100 (88.5)1,3,5 | 387 (93.7)2,4,5 | <0.01 |
| The results of genetic testing would help me and my doctor plan | 1285 (85.9)1 | 1446 (96.4)2,3 | 102 (91.1)1,2,4 | 393 (95.2)3,4 | <0.01 |
| I would provide the results of genetic tests to the government | 1008 (67.4)1,2 | 1181 (78.7) | 61 (54.0)1,3 | 258 (63.1)2,3 | <0.01 |
| Knowledge of test results may lead to discrimination (e.g., in employment) | 1058 (70.7)1 | 1032 (68.8)1 | 99 (87.6)2 | 336 (81.4)2 | <0.01 |
| People who have a positive genetic test result should inform their spouse | 1163 (77.7)1,2 | 1242 (82.8) | 74 (65.5)1,3 | 298 (72.5)2,3 | <0.01 |
| I would not like to marry someone who had a positive genetic test result | 1141 (76.3) | 1012 (67.5)1 | 67 (59.8)1,2 | 215 (52.2)2 | <0.01 |
Note: Numbers and percentages (%) represent respondents who answered “strongly agree” or “agree”
1–5Values with the same superscript numbers are not significantly different
aP-value was tested by ANOVA with Scheffe’s post-hoc test (p < 0.05).
Discussion
In the present study, we identified differences in attitudes toward genetic testing among the general public, cancer patients, and health-care professionals in Korea. In total, 3522 Korean adults were recruited and surveyed in this study. Most respondents had heard about genetic testing before. Interestingly, in contrast to clinicians, the majority of respondents among the cancer patents reported less concerns for privacy-related issues.
In the present study, the proportion of respondents who had prior knowledge of genetic testing was much higher than that reported in prior studies conducted in other countries [3, 7, 8, 23]. Phuong et al. indicated that 47% (95% CI 46.1–48.0%) of the U.S. population was aware of genetic testing. Similar to another study [24], female respondents in the present study were significantly more likely to be aware of genetic testing than their male counterparts. These findings may suggest that genetic testing is an important issue in the minds of Korean people.
The awareness of paternity tests among Korean people may have contributed to the high proportion of individuals aware of genetic testing. When asked, “What comes to mind when you hear the word ‘genetic testing’?” a greater number of respondents answered “paternity test” than those who responded “family history” or “disease prevention.” This tendency may be influenced by mass media, such as TV. In other countries, genetic testing is recognized as an effective method of preventing disease, whereas genetic testing is often portrayed as being used for paternity tests in popular Korean TV dramas. In addition, these respondents may have also been influenced by a headline event regarding a paternity test that happened prior to our survey being initiated. Indeed, in the present study, we found that TV was the primary source from where respondents had read or heard of genetic testing. Similarly, Kolor et al. [24]. also reported that mass media, including TV and radio, was the most likely source of genetic testing information.
Meanwhile, respondents also indicated greater awareness of information on genetic testing due to medical reasons. In the present study, the two major reasons for wanting to undergo genetic testing among respondents were to prevent diseases and to know their family history. McGuire et al. [25] also found that social networking users (n = 1087) wanted to undergo genetic testing out of general curiosity for their genetic make-up (81%) and to determine whether a specific disease runs in their family or is present in their DNA (74%). Regarding tests for specific diseases, respondents to the present survey were most interested in genetic tests for dementia. Another study of the general public in the Netherlands also found that genetic testing for dementia was favored over other tests for cardiovascular disease and cancer [4].
Overall, the results of the present survey revealed much more positive attitudes toward genetic testing than previous studies. Herein, respondents from the general public most strongly expressed the belief that genetic testing should be included in Korea’s national health screening program (73%) than respondents from the other groups: via National Health Insurance Law, the national health screening program in Korea is to provide health-screening services at little expense, including (1) a medical examination by interview; (2) physical examinations for nutrition status, blood pressure, eyesight, and hearing; (3) chest X-ray, urine test, and blood test; (4) dental checkup; (5) health risk assessment, (6) cognitive dysfunction neuropsychological test; and (7) health counselling based on screening test results for individuals who satisfy eligible criteria [26]. In contrast to our results, Vermeulen et al. found that 24% of respondents from the general public in the Netherlands agreed that people should be preventively tested for all kinds of disease [4]. In addition, our results indicated that the majority of respondents (92%) would undergo genetic testing if it was offered at no cost, which is a much higher proportion than results from studies in the UK and Canada [22, 27]. Also, >85% of respondents reported a strong belief that the results of genetic testing would help improve their health care. Meanwhile, Blanchette et al. reported that 64% of patients thought genetic testing would significantly improve their cancer care [9].
Interestingly, a relatively large proportion of the general public (67.4%) answered that they would be willing to provide the results of genetic tests to the government, despite being concerned about social discrimination due to test results (70.7%). Along with the results above, we suspect that the general public of Korea may overestimate the benefits of genetic testing, outweighing concerns for potential discrimination. Potentially related thereto, the primary sources for learning about genetic testing among the public were TV and Internet, rather than medical experts, suggesting that those people may have insufficient or misleading information about genetic testing. In addition, Korean people generally have positive attitudes toward the health-care system. According to a report from the 2011 national survey for evaluating public health policy in Korea, 63.9% of all participants indicated that they were satisfied with current health policies [28]. To sum up, our results indicate that the general public of Korea may willingly seek to undergo genetic testing should it become offered as part of the national screening program at little-to-no cost, owing to high satisfaction with the health-care system rather than a clear understanding of the benefits and limitations of genetic testing.
Herein, clinicians reported being less likely to provide their results with the government than the other sample groups. In another study, >75% of participants (internists) in the U.S. expressed concerns for genetic privacy [6]. Clinicians who participated in the present study also voiced a stronger belief that knowledge of test results may lead to discrimination, compared to the other sample groups. Mirroring these concerns, a smaller study by Teng et al. [29] previously reported that “Patients with a positive test result may face discrimination at work or when seeking insurance,” was an important reason why clinicians did not refer patients for genetic testing. This concern has been raised in many countries, for example, the U.S. has passed legislation preventing employment and health insurance discrimination based on genetic testing [9].
To improve the utilization of genetic information, public awareness of genetic testing should be increased. Despite noting high public awareness of genetic testing in this study, we are not certain as to whether people correctly understood genetic testing. In the US, Mai et al. reported that public awareness of genetic testing was <50%, experiencing a slight increase from 2000 to 2010, although public exposure to genetic testing has been increasing [8]. They demonstrated that the estimated awareness in 2000 may have been inflated because respondents might have confused genetic tests with cancer screening or other tests, resulting in a slight increase in estimated public awareness [8]. Accordingly, future studies in Korea should seek to assess the correctness of public awareness of genetic testing.
In light of our results, we stress that providing people with information about the pros and cons of genetic testing is important and that measures to prevent discrimination and to protect information should be provided in order to advance genetic testing. The public should be made aware of laws protecting individuals from discrimination due to the results of genetic testing. Indeed, the Korean government strictly prohibits discrimination due to genetic information and penalizes violations under the Bioethics Law [30]. However, its principles are too broad to solve specific problems related to the use of genetic information, such as insurance and employment [30, 31]. Thus politicians should recognize those potential issues related to bioethics and propose legislation that strengthens protections against any discrimination due to the results of genetic testing [30, 31]. In addition, as stated by others, thorough assessment of interest in and the acceptability of genetic tests among potential users should be conducted prior to extending the applications of genetic testing [1, 32, 33].
Our study has some several limitations. First, our study includes the potential disadvantages of non-randomized sampling, and thus the results may or may not be biased. However, application of the selected sampling method allowed us to collect data from a large number of subjects and diverse groups during the short time period, as well as helped save on cost. As a second limitation, patients were recruited from only two major hospitals in Korea. However, those two are considered as two of the largest five cancer hospitals in Korea. Moreover, we found that the recruited patients were residents of various regions in Korea, and the distribution of our participants by region was analogous to that for the national population. Third, whether cancer patients were mutation carriers was not examined in our study, as we only sought to outline the cancer patients’ general views about genetic testing. Despite these limitations, however, the present study is, to our knowledge, the first to assess differences in awareness of and attitudes toward genetic testing among the people of Korea.
In conclusion, the majority of Korean respondents who participated in the present study were aware of genetic testing. Differences in attitudes toward genetic testing, however, among the general public, cancer patients, and health-care professionals were identified. Overall, the public and patients had more positive attitudes toward genetic testing than clinicians, and clinicians were generally more concerned about discrimination upon sharing genetic test results than other respondents. Further research should be conducted to determine how clinicians can ascertain concerns among the general public and patients and barriers to undergoing genetic testing. Above all, we emphasize that providing correct information to people who are scheduled to undergo or order genetic testing is of great importance to helping them make informed decisions.
Acknowledgements
This research was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (no. 1520240).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Sun-Young Kong, Phone: +82 31 920 1735, Email: ksy@ncc.re.kr.
Yoon Jung Chang, Phone: +82 31 920 2190, Email: eunicemd@ncc.re.kr.
References
- 1.Chokoshvili D, Belmans C, Poncelet R, et al. Public views on genetics and genetic testing: a survey of the general public in Belgium. Genet Test Mol Biomark. 2017;21:195–201. doi: 10.1089/gtmb.2016.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon KA, Park B, Lee BI, Yang MJ, Kong SY, Lee ES. Clinically significant unclassified variants in BRCA1 and BRCA2 genes among Korean breast cancer patients. Cancer Res Treat. 2017;49:627. doi: 10.4143/crt.2016.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henneman L, Vermeulen E, Van El CG, Claassen L, Timmermans DR, Cornel MC. Public attitudes towards genetic testing revisited: comparing opinions between 2002 and 2010. Eur J Hum Genet. 2013;21:793–9. doi: 10.1038/ejhg.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vermeulen E, Henneman L, van El CG, Cornel MC. Public attitudes towards preventive genomics and personal interest in genetic testing to prevent disease: a survey study. Eur J Public Health. 2014;24:768–75. doi: 10.1093/eurpub/ckt143. [DOI] [PubMed] [Google Scholar]
- 5.Houfek JF, Soltis-Vaughan BS, Atwood JR, Reiser GM, Schaefer GB. Adults’ perceptions of genetic counseling and genetic testing. Appl Nurs Res. 2015;28:25–30. doi: 10.1016/j.apnr.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Klitzman R, Chung W, Marder K, et al. Attitudes and practices among internists concerning genetic testing. J Genet Couns. 2013;22:90–100. doi: 10.1007/s10897-012-9504-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahram M, Soubani M, Abu Salem L, Saker H, Ahmad M. Knowledge, attitudes, and practice regarding genetic testing and genetic counselors in jordan: a population-based survey. J Genet Couns. 2015;24:1001–10. doi: 10.1007/s10897-015-9839-3. [DOI] [PubMed] [Google Scholar]
- 8.Mai PL, Vadaparampil ST, Breen N, McNeel TS, Wideroff L, Graubard BI. Awareness of cancer susceptibility genetic testing: the 2000, 2005, and 2010 National Health Interview Surveys. Am J Prev Med. 2014;46:440–8. doi: 10.1016/j.amepre.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blanchette PS, Spreafico A, Miller FA, et al. Genomic testing in cancer: patient knowledge, attitudes, and expectations. Cancer. 2014;120:3066–73. doi: 10.1002/cncr.28807. [DOI] [PubMed] [Google Scholar]
- 10.Hann KE, Freeman M, Fraser L, et al. Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health. 2017;17:503. doi: 10.1186/s12889-017-4375-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dominguez-Carral J, Lopez-Pison J, Macaya A, Campaña MB, García-Pérez M, Natera-de Benito D. Genetic testing among Spanish pediatric neurologists: knowledge, attitudes and practices. Eur J Med Genet. 2017;60:124–9. doi: 10.1016/j.ejmg.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Gray SW, Hicks-Courant K, Lathan CS, Garraway L, Park ER, Weeks JC. Attitudes of patients with cancer about personalized medicine and somatic genetic testing. J Oncol Pract. 2012;8:329–35. doi: 10.1200/JOP.2012.000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romero-Hidalgo S, Urraca N, Parra D, Villa AR, Lisker R, Carnevale A. Attitudes and anticipated reactions to genetic testing for cancer among patients in Mexico City. Genet Test Mol Biomark. 2009;13:477–83. doi: 10.1089/gtmb.2009.0004. [DOI] [PubMed] [Google Scholar]
- 14.Shen J. Precision assessment of public attitudes toward genetic testing. Am J Med Genet A. 2016;170:3185–8. doi: 10.1002/ajmg.a.37936. [DOI] [PubMed] [Google Scholar]
- 15.Leader AE, Mohanty S, Selvan P, Lum R, Giri VN. Exploring Asian Indian and Pakistani views about cancer and participation in cancer genetics research: toward the development of a community genetics intervention. J Community Genet. 2018;9:27–35. doi: 10.1007/s12687-017-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pang J, Sullivan DR, Harada-Shiba M, et al. Significant gaps in awareness of familial hypercholesterolemia among physicians in selected Asia-Pacific countries: a pilot study. J Clin Lipidol. 2015;9:42–48. doi: 10.1016/j.jacl.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Zhao X, Wang P, Tao X, Zhong N. Genetic services and testing in China. J Community Genet. 2013;4:379–90. doi: 10.1007/s12687-013-0144-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li J, Xu T, Yashar BM. Genetics educational needs in China: physicians’ experience and knowledge of genetic testing. Genet Med. 2015;17:757–60. doi: 10.1038/gim.2014.182. [DOI] [PubMed] [Google Scholar]
- 19.Roberts JS. Anticipating response to predictive genetic testing for Alzheimer’s disease: a survey of first-degree relatives. Gerontologist. 2000;40:43–52. doi: 10.1093/geront/40.1.43. [DOI] [PubMed] [Google Scholar]
- 20.Petersen GM, Larkin E, Codori AM, et al. Attitudes toward colon cancer gene testing: survey of relatives of colon cancer patients. Cancer Epidemiol Biomark Prev. 1999;8(4 Pt 2):337–44. [PubMed] [Google Scholar]
- 21.Hietala M, Hakonen A, Aro AR, Niemelä P, Peltonen L, Aula P. Attitudes toward genetic testing among the general population and relatives of patients with a severe genetic disease: a survey from Finland. Am J Hum Genet. 1995;56:1493. [PMC free article] [PubMed] [Google Scholar]
- 22.Cherkas LF, Harris JM, Levinson E, Spector TD, Prainsack B. A survey of UK public interest in internet-based personal genome testing. PLoS ONE. 2010;5:e13473. doi: 10.1371/journal.pone.0013473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olwi D, Merdad L, Ramadan E. Knowledge of genetics and attitudes toward genetic testing among college students in Saudi Arabia. Public Health Genom. 2016;19:260–8. doi: 10.1159/000446511. [DOI] [PubMed] [Google Scholar]
- 24.Kolor K, Duquette D, Zlot A, et al. Public awareness and use of direct-to-consumer personal genomic tests from four state population-based surveys, and implications for clinical and public health practice. Genet Med. 2012;14:860–7. doi: 10.1038/gim.2012.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGuire AL, Diaz CM, Wang T, Hilsenbeck SG. Social networkers’ attitudes toward direct-to-consumer personal genome testing. Am J Bioeth. 2009;9:3–10. doi: 10.1080/15265160902928209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee WC, Lee Sy. National Health Screening Program of Korea. J Korean Med Assoc. 2010;53:8. [Google Scholar]
- 27.Ries NM, Hyde-Lay R, Caulfield T. Willingness to pay for genetic testing: a study of attitudes in a Canadian population. Public Health Genom. 2010;13:292–300. doi: 10.1159/000253120. [DOI] [PubMed] [Google Scholar]
- 28.Shin Y. National Survey for Evaluating current Public Health Policy. In: Korea Institute for Health and Affairs, ed. Ministry of Health and Welfare of the Republic of Korea; 2011:1-211.
- 29.Teng I, Spigelman A. Attitudes and knowledge of medical practitioners to hereditary cancer clinics and cancer genetic testing. Fam Cancer. 2014;13:311–24. doi: 10.1007/s10689-013-9695-y. [DOI] [PubMed] [Google Scholar]
- 30.Yang JH, Kim SY. Legal and Regulatory Issues in Genetic Information Discrimination - Focusing on Overseas Regulatory Trends and Domestic Implications. The Korea Society of Law and Medicine. 2017;18(1):237-264
- 31.Han CH. A study on genetic information and the insurance. Korean Insur J. 2009;82:33–60. [Google Scholar]
- 32.Fortuny D, Balmaña J, Graña B, et al. Opinion about reproductive decision making among individuals undergoing BRCA1/2 genetic testing in a multicentre Spanish cohort. Hum Reprod. 2008;24:1000–6. doi: 10.1093/humrep/den471. [DOI] [PubMed] [Google Scholar]
- 33.Thompson HS, Valdimarsdottir HB, Duteau-Buck C, et al. Psychosocial predictors of BRCA counseling and testing decisions among urban African-American women. Cancer Epidemiol Prev Biomark. 2002;11:1579–85. [PubMed] [Google Scholar]