Abstract
Improvements in early hip arthroplasties focused on surgical techniques with subsequent studies emphasizing restoration of the hip center of rotation for longevity of the implant. Current literature suggests femoral stem anteversion of 10–20°, cup anteversion of 20–25° and a combined anteversion of 25–40° in males, 30–45° in females. Inclination goal appears to be 45° precisely to balance between impingement & dislocation versus edge loading & accelerated wear. Restoration of the acetabular center of rotation will improve joint reactive forces and reduce wear. Here we describe techniques to achieve a well balanced total hip with restoration of the center of rotation.
1. History
The initial results of the cemented Charnley low-friction arthroplasty was met with significant enthusiasm. Charnley's original design included maintenance of femoral head diameter not larger than the radius of the acetabular socket to ensure low torque generation and avoid early radiolucent lines, a surrogate for high joint reactive forces, early loosening and failure.8 Combined with greater trochanter advancement for appropriate abductor tension, hip balance combined with hip center medialization, Charnley successfully pioneered total hip arthroplasty (THA) as the operation of the century.9,10
Improvements in the early THAs focused on surgical techniques to avoid the high non-union rate of the greater trochanter and subsequent abductor limp. Johnston et al.11 calculated a mathematical model for lowering hip joint reactive forces based upon geometric factors of the hip. A medialized, inferior and anterior center demonstrated lower joint forces, while small femoral shaft-neck angles and their junction between 130 and 140° also lowered joint loads. A shorter femoral neck of 35 mm had less moment force compared with a 45 mm length neck. This suggested an additional element of surgical technique to lower joint forces, a surrogate of early loosening and wear. It also may allude to the complexity of the hip biomechanics and joint reactive forces.
Subsequent reports emphasized identification and meticulous restoration of the hip center of rotation (COR) for longevity of the implant. Ranawat et al.12 identified 35 THAs with 4.3 years followup performed in the setting of rheumatoid protrusio acetabuli. They reported 94% acetabular radiolucency (a surrogate for loosening) with hip centers migrated more than 1 cm medially or superiorly compared to zero radiolucency when the hip center was within 5 mm of the anatomical position. Karachialos et al.13 reported on 12–18 year followup on 95 Charnley cemented total hip arthroplasties. They noted changes in hip COR as small as 2 mm were related to unfavorable radiographic signs such as cup migration, wear, stem and acetabular demarcation, and calcar resorption. They suggested avoiding superior & medial hip COR while emphasizing the importance of anatomic cup placement. While these cemented acetabular cups seem to have a small tolerance for anatomic placement, newer literature appears to have larger tolerances for achieving acceptable uncemented cup COR.
2. Wear and impingement
THA component position can affect tribologic mechanisms in the hip as well. Femoral offset, defined as distance between the center of the femoral head and a line bisecting the long axis of the femur, affects the abductor lever arm mechanism and thus affects hip joint reactive forces14,15 Lecerf et al.15 correlated the importance between femoral offset, abductor lever arm and hip abductor strength. As femoral offset increases, so does the mechanical advantage of the hip abductors and thus decrease related joint reactive forces. Of note, they found hip resurfacing implants tended to lower hip offset while total hip arthroplasty tended to increase overall offset. Lastly, they noted a lower survival rate with high offset cement stems in the Swedish registry, a possible cause of increased stress at the implant interface in the setting of cement. On the contrary, Salkalkale et al.16 compared polyethylene wear in seventeen bilateral THAs with one standard and one high offset on either side. At 5 years, they reported a linear wear rate of 0.21 mm/yr for standard and 0.01 mm/yr for high offset femoral components. In their study, uncemented stems were utilized, a potential benefit of ingrowth fixation.
Charles et al.14 performed a nice review of the current knowledge on hip offset and balance. The overall average femoral offset is 44 mm, with a range 27–57 mm. Inability to restore these parameters may lead to gait imbalance, weakness, affected range of motion (ROM), impingement and dislocation. Preoperative planning is helpful for femoral offset restoration to ensure accuracy and avoidance of complications. Femoral offset can be affected by 5 factors: neck length, a varus femoral component, medialization of the femoral component, cup offset (and this may be most important because femoral offset by itself is only a factor if cup COR is restored – otherwise hip offset is the relevant measurement) and a combination of factors such as a varus component with increased neck length. Paying attention to a patient's anatomy such as a varus neck can notify the surgeon to have a high offset femoral component or a specialized varus neck-shaft angle component available.
Maintaining the center of rotation of the hip can help improve wear characteristics.17,18 As the COR migrates superolaterally in certain arthritic patterns, increased abductor tension is required to maintain balance, resulting in elevated joint reactive forces. Charnley would recommend medialization of the hip center to improve forces, a surrogate for early failure. Asayama et al.19 evaluated 30 patients with unilateral THA with regards to femoral offset, hip COR, cup height, abductor strength in comparison to their non-arthritic contralateral side. They found that hip abductor strength was significantly higher (p = 0.020) with slightly increased femoral offset and normal or slight inferomedial hip COR. Their results are similar to others as well.11,15,20
The concept of hip offset was popularized by Dastane et al.7 A combination of femoral offset and hip center of rotation, they reported upon their results of 82 THAs with respect to hip COR, femoral offset, and leg length. Their offset was within 6 mm in 78 of 82 hips. They observed that as hip COR displaced superiorly from 3 mm to 6 mm, femoral offset had to be substantially increased to match hip offset. A COR within 3 mm predicted reproducible offset within 5 mm. Since stems have a fixed amount of offset, if hip COR is not within these parameters, stem offset is compromised by cup position. The authors concluded that precise hip COR is critical to restore total hip offset.
Optimal acetabular anteversion and inclination can vary per individual patient, and can affect impingement and subsequent dislocation.7,20, 21, 22, 23 Brown concluded that impingement is the major precursor for dislocation.21 Malik et al.22 emphasized the importance of avoiding impingement structures, such as acetabular bone or osteophytes with femoral trochanter, femoral neck with acetabular liner or shell, or a combination of both. They recommended an acetabular anteversion of 10–20 and femoral anteversion of 10–15 with a combined anteversion of 25–40° in male and 30–45° in female. Inclination of <45° may have some advantages in wear mechanics.17,24 Little et al.24 reported on 43 uncemented THAs with minimum follow-up of 49 months regarding conventional polyethylene wear with respect to femoral offset and acetabular inclination. They found lower wear rates with inclination angles of under 45 deg and femoral offset restoration within 5 mm (0.12 mm/year vs 0.18 mm/year and 0.12 mm/year vs 0.16 mm/year, respectively). On the contrary, recent evidence may suggest that too little inclination may have deleterious effects as well. Lum et al.23 suggested that too low of an inclination may result in impingement and dislocation from abnormal pelvic tilt due to spinopelvic imbalance. The studies appear to suggest a precise inclination of 40–45° may lower overall complication rates and wear.
3. What does current literature say about cup and stem position?
Femoral and acetabular component positioning must be tailored to the individual patient. Restoration of hip offset may be achieved with normal to slight medialization of the hip COR and increased femoral offset to improve abductor lever mechanism and resting tension, resulting in lower joint reaction forces and improved wear mechanics in cementless designs. Inclination angles at 45° may have lower wear rates while avoiding impingement/dislocation.24 Current literature suggests femoral stem anteversion of approximate 10–20° if proximal femoral anatomy allows, cup anteversion of 20–25° in order to reach a combined anteversion of 25–40 in males, 30–45 in females.5,6
4. Radiographic methods for locating center of rotation (COR)
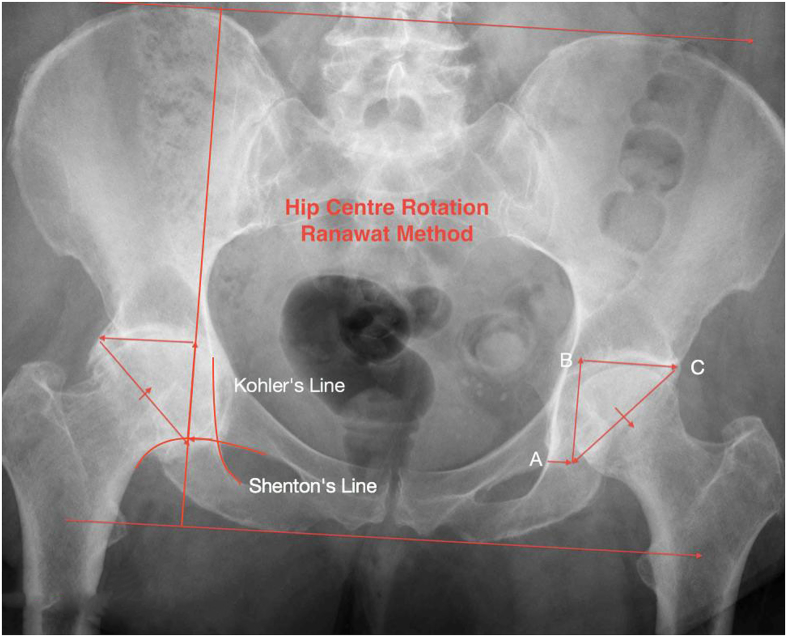
The classic Ranawat triangle described to locate the anatomic position of the acetabulum was first described in rheumatoid arthritics with protrusion.12 On the AP pelvis radiograph, horizontal lines drawn at the level of the iliac crests and ischial tuberosities are connected by a vertical perpendicular line passing through point A. Point A is defined by the point 5 mm lateral to the intersection of Kohler's line and Shenton's line (Fig. 1). Point B is found along the vertical line at the horizontal level of the subchondral acetabular roof in normal hips. In abnormal hips, line AB is 20% of the entire vertical distance of the pelvis. Point C is found along the horizontal line BC, at the level of the subchondral acetabular roof, and is equidistant to line AB. Line AC is the hypotenuse of this isosceles triangle, and represents the opening cup of the acetabulum.
Fig. 1.
Ranawat Triangle for locating the center of rotation of the acetabulum.
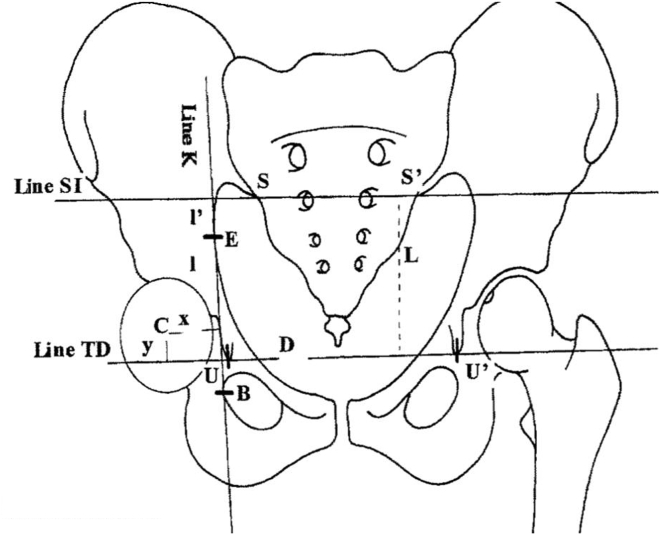
Another method described by the French, modified by Fessy et al.25,26 locates the respective hip center by reconstructing the hip joint in several stages (Fig. 2). The first stage consisted of defining the following points: The center C of the hip by the method of concentric circles imposed on the femoral head, point U, the most distal point of the radiological U ("tear-drop"), point S, the most distal point of the sacroiliac joint, point B, the most lateral point of the obturator foramen, point E, the most lateral point of the arcuate line. The same points were located on the opposite side and identified respectively by the letters U′, S′, B′ and E'. The second stage consisted in tracing the following lines: the line K of Kohler which passed through points E and B, line TD passing through points U and U′, and line SI passing through points S and S'. The third stage consisted of determining the coordinates X and Y of the center of rotation of the hip with X in relation to Kohler's line K, and Y in relation to line TD. In a fourth stage, we defined the horizontal indices and the vertical indices. The horizontal indices were: D = distance UU′, d = distance SS′, m = distance BB'. The vertical indices were: L = distance SI-TD, I = distance E-TD on Kohler's line, I' = distance E− SI on K6hler's line, H = total height of the pelvis.
Fig. 2.
The French method by Fessy et al.26 locating the center of rotation of the hip.
These techniques to find the hip center are helpful as patient's anatomy can be variable and does change in the setting of osteoarthritis.27 Intraoperatively, to avoid impingement, nesting the acetabular component within the acetabular bone stock and taking the hip through an impingement-free range of motion is important, as impingement cannot be diagnosed by imaging techniques.28
5. Authors technique to restoration of center of hip rotation
The fundamental principle of total hip replacement (THR) is to reconstruct the destroyed articulation of the hip joint. Osteoarthritis of the hip usually occurs in a joint that incorrectly developed. In most patients the hip does not just “wear out”. There are non-osteoarthritic causes such as rheumatoid arthritis, avascular necrosis, and post-traumatic arthritis, but the majority of operations are performed in hips which have osteoarthritis due to secondary geometric deformity of the hip. Many men under the age of 65 have cam impingement as the underlying etiology and women under 65 years tend to have dysplasia or pincer impingement. The occurrence of geometric deformities in the hip as the cause of arthritis has been well described by Stulberg and Harris and by Ganz.1,2 These geometric deformities tend to have a genetic component. Primary osteoarthritis tends to be a disease of European ancestry while Asians usually have dysplasia and osteonecrosis as their cause of arthritis.3
In an arthritic joint the cartilage no longer is functional, and is typically absent in the weight bearing anterior superior surface. With the cartilage worn away, the femoral head slides in the joint and migrates: lateral and superior in 60% of hips and medially in 25%. Other deformities are coxa profunda with protrusio of the head, and osteophyte formation of the acetabulum which grips the femoral head superiorly and inferiorly. As the femoral head migrates in the acetabulum, the body's reaction is to constrain the migration by forming osteophytes and to fill the void behind. Thus, an arthritic hip with superior-lateral migration of the head will have an acetabular floor osteophyte which will cover the cotyloid notch and the transverse acetabular ligament (TAL). An anterior wall osteophyte is usually seen with pincer impingement or medial migration.
THR is a mechanical operation in a biological environment. Biology will support the durability, longevity and resulting success only if the mechanics are correct. The stem and cup implants themselves are important for fixation but are simply biomechanical bearings for the recreated hip joint. The mechanical and biomechanical aspects of the operation really determine its fate. Additionally, it is not the position of the incision that determines the outcome of THR based upon the scientific data; it is not important whether the incision is anterior or posterior. The incision is not one of the principles of THR. It is simply a method to get inside the hip to perform the true operation, and the surgeon should use that incision which is most comfortable for him/her and provides for him/her the desired results.
The mechanics are first with the recreation of the center of rotation (COR) of the joint. It is this reconstruction that determines the joint reaction force, the resting tension of the muscles, and facilitates the range of motion. The second mechanical construction is the cup position, both inclination angle and anteversion with cup anteversion mated to the femoral anteversion.
The biomechanical reconstruction is second, with regards to balancing the correct hip offset and hip length. This balance is an integral part of the resting muscle length-tension, and is necessary for clearance between implants and bone during function of the hip by avoiding of impingement.
6. Mechanics of THR
6.1. COR of the hip
In simplistic terms, the goal of THR is to recreate the COR of the hip by returning the center of the migrated femoral head to the reconstructed COR of the acetabulum. This is the function of templating for implant size and position during preoperative planning: placing the cup in its correct position in the bony acetabulum to restore its COR. The femur template then must then determine where the stem selected for use needs to be implanted to most closely restore the femur COR. This femur templating determines the level of the bony neck cut, and the head length to achieve the COR.
Achieving perfection in every operation is difficult because it is not so easy to precisely restore the hip COR. Migration of the femoral head within the acetabulum results in geometric changes of the acetabular bony structure. The restoration of the femur COR is limited by a metal stem and fixed neck shaft angle which may not match the anatomy of the femur. It is the mental planning and necessary adjustments for these limitations that separates the good hip surgeon.
While planning the operation, the surgeon must decide if the COR of the acetabulum can be restored, and if so the technical performance of this must be accomplished. Success of the femoral side biomechanical reconstruction depends on the cup COR. Restoration of the COR of the hip facilitates the other mechanics of the operation such as the mating of the femoral head into the cup. This mating must maintain the head central in the cup throughout the function of the hip. Edge loading, or eccentric loading, of the head in the cup is a major factor for wear.
Reconstruction of the COR is dependant on precise reaming by the surgeon. Most often the surgeon is aggressive resulting in average COR 6.4 mm off from the center.4 When the error is more superior than medial it causes more difficulty in balancing the hip length and offset. The error in reaming most often results from the necessity to have coverage of a non-cemented cup. If the preoperative templating causes selection of a cup that is one size too large for the acetabulum, then reaming more medial and more superior by the surgeon is their solution to make this cup fit with more coverage. Charnley was always able to cover a cemented cup because the cup was smaller than the reamed bone. With an uncemented cup, the precision of cup placement/coverage is complex since the metal shell must be press-fit into the acetabular rim. The complexity is getting the correct inclination and combined anteversion as well as restoring the COR.
Initial reaming should be transversely to remove the lunate bone (acetabular ridge). It must not violate the cotyloid notch's cortical bone to allow recreation of the acetabular COR. This transverse reamer should simple brush the anterior and posterior walls of the acetabulum – remember the cup size is best determined by the anterior-posterior diameter of the acetabulum, not the superior-inferior diameter. The second reamer forms the bony hemisphere for the hemispheric cup. It should be the final size reamer which can be anywhere from 2 mm smaller than the cup to line-to-line, depending on the requirements of the cup used. The final reamer is directed superior and anterior, but is not “buried” deep beneath bone. It is easier to ream more than replace lost bone. The trial cup should be impacted into place and fit evaluated as follows:
-
1.
The medial edge of the metal shell (inferior medial if operating with the patient in the lateral position) should be over the transverse acetabular ligament (TAL).
-
2.
The anterior inferior edge should be below the pubis by no more than 2–3 mm, and the posterior inferior edge below the ischium by the same 2–3 mm.
-
3.
The posterior edge of the cup must be covered to avoid impingement with the metal neck during hip extension of walking.
-
4.
The anterior edge is covered by bone to avoid iliopsoas tendinitis.
-
5.
Posterior-superiorly the metal can be uncovered for 2–3 mm to permit 40° inclination (the average bony acetabulum has 55° inclination so in some hips the metal edge must be uncovered to avoid inclination more than 45°).
-
6.
The anterior superior metal edge must be covered to avoid impingement of the metal neck with flexion (and especially flexion-adduction-internal rotation).
Additionally, it is important for the surgeon to remember the operation is on a joint, so the femoral side counts! Unfortunately, too often the only emphasis is placed on the acetabular reconstruction. The natural hip joint was created with combined anteversion as described by McKibben in infant cadaver pelvises. (4) The average femoral anteversion was 15° and the combined anteversion was 30°-40°. Combined anteversion below 25° resulted in impingement, and below 20° resulted in frank retroversion, howevere in arthritic hips the femoral anteversion (or certainly the cementless stem) is not always 15° anteverted, and the combined anteversion is not 30°-40°. For THR stability, the combined anteversion must be reconstructed within the safe zone of 25°-45°.5 There is less flexibility in implanting cementless hip components so that combined anteversion in the safe zone is not always easy to reconstruct. This is especially true regarding hips that are retroverted, a common finding with cam impingement and pincer impingement. Thus, attention must be paid to the femoral side, and its anteversion factored into the implanted acetabular anteversion.
7. Biomechanical reconstruction
Balancing the mechanical reconstruction appropriately so that the biology of the joint can function normally is a critical task of the surgeon. The biology of the hip joint is to propel the leg forward and provide flexibility for positional changes of the body. To do this comfortably and efficiently (efficiency of normal oxygen consumption) requires the joint be stable, and the muscles across it function correctly. This reconstruction requires the surgeon balance the hip length and offset. The conundrum is created by the COR of the hip being in an abnormal position. With a distorted hip COR, the femur and stem cannot be restored to its correct position and the ball-in-socket motion of the hip joint is off center. With this distortion, forces on the joint change, and instability and accelerated wear can occur.
If the hip COR (acetabular COR) cannot be restored to within 3 mm of its normal position, at least the surgeon must restore hip length (and therefore leg length in most patients) and offset. With THR the hip offset is more important than just femoral offset. For instance, if the cup COR is moved 5 mm or more superior or medial, an offset stem is often required to obtain balance of length and offset. Manual reaming of the acetabulum often creates an off center COR, because surgeons commonly overream by a mean 6.4 mm (3) On the other hand, use of the offset stem for every hip creates its own problem because increasing offset by more than 5 mm will increase wear. These are examples of the intraoperative decisions a surgeon must make – and issues to be adjusted intraoperatively, that are addressed by the techniques in this chapter.
It is naturally intuitive that the mechanics and the biomechanical reconstruction of the hip are linked. The hip length (and the leg length) and offset can be balanced easily if the COR of the hip has been restored within 3 mm superior and 5 mm medial.7 The decisions by the surgeon become more difficult when the COR is not restored. Device modifications may help the surgeon. A lateralized COR polyethylene liner can compensate for overreaming, or a geometrically deformed acetabulum on the pelvic side of the joint. An offset femoral stem can do the same on the femur side.
The restoration of the COR is important for biomechanical reconstruction because it allows the preoperative planning of the neck cut of the femur to be validated. If the COR is displaced by reaming cephalad by 5 mm or more, or greater than 5 mm medially, use of device modifications will be necessary in most patients. If there is anticipation of the distortion of the hip COR, then modification of the femoral neck cut can often overcome this COR change. Likewise, a correct femoral neck cut can compensate for an anatomic valgus or varus hip structure. With a neck shaft angle of 120° or less, an offset stem is usually needed even with a correct neck cut.
Correct hip length and offset is important because it allows near normal muscle function; it minimizes hip impingement; and it increases comfort for the patient by preventing impingement pain and preventing fatigue to muscles due to decreased tension. Length and offset must be manually evaluated after the reconstruction. This is a sound reason for using trials, certainly for the femoral stem.
The hip can be manually evaluated as follows:
-
1)
Palpate the lesser trochanter relationship to the tip of the ischium. The x-ray of the contralateral normal hip on the preoperative AP pelvic film will provide the information needed as to this relationship. If the contralateral hip is not normal, the relationship must be reconstructed so there is no impingement and the lesser trochanter is not below the tip of the ischium. This is an accurate measure of hip length once the surgeon has experience with this technical maneuver.
-
2)
Fully abduct and externally rotate the hip. The femoral neck should clear the posterior cup and acetabular bone and the greater trochanter should clear the ilium by one fingerbreadth.
-
3)
Fully flex the knee at neutral rotation towards the chest. The femoral head cannot drop out of the cup. If it does, the combined anteversion is incorrect, or the leg length and offset is not balanced. The hip may need mechanical support to protect against lax biological support. Larger femoral head sizes reduce dislocation risks because they give protection against dropout. If a 28 mm or 32 mm femoral head is used, a polyethylene with a hood can simulate the protection of a large head by placing the apex of the hood at 4 o'clock (right hip) or 8 o'clock (left hip).
-
4)
Adduct and internally rotate the hip until resistance stops the internal rotation. The hip must be stable, and the femoral head should not be uncovered by more than 50% posteriorly or anteriorly. This test is best done by laying the leg across the table (if the patient is in the lateral position) and internally rotating it. This simulates the maximum postural position if someone is in bed and drops one leg over the other.
Leg length can be anatomically confirmed by relationship of the lesser trochanter to the ischium. It can be functionally confirmed by overlaying the legs and the level of the patellae and heels of the operated leg to the contralateral leg. Lastly, we finally confirm the leg length by measuring this after we have completed the operation and turned the patient to their side (just prior to transferring to a bed). If the surgeon is operating the patient in the supine position, this same leg length measure can be made prior to closing the hip wound. If the medial malleoli are not within 1 mm for a short person, and 3 mm for a tall person we correct the leg length immediately be repositioning the patient and reoperating upon the hip. Either the head length is changed or the cup and stem adjusted as needed. We do not allow patients to leave the operating room without equal leg lengths (unless anatomically impossible).
8. Summary
-
●
Total hip replacement is a mechanical operation. As surgeons, we must optimize the mechanics to provide our patients the best biologically functioning hip. Foremost, this means restore the center of rotation within 3 mm superior and 5 mm medial.
-
●
In hips which this is unachievable, device modification for the implants used give us the ability to compensate for reaming error or abnormal hip anatomic geometry.
-
●
Sound practical clinical decisions mean the surgeon does not leave the operating room without a hip length and offset that avoids manual impingement and equal leg lengths when possible.
-
●
The principles described herein have changed little since Charnley, with the exception of trochanteric transfer, as it is not used to achieve optimization of the joint reaction forces and avoidance of bone-on-bone impingement.
-
●
The principles to maintain the center of rotation, restoration of hip length and offset, and the attention to component placement are the most critical technical accomplishments for the surgeon. It is the surgeon's responsibility to create a mechanical reconstruction in a biological environment that will be comfortable for the patient and be durable for many years.
Disclosures
None.
Each author certifies that his institution approved or waived approval for the use of human subjects for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2018.08.040.
Contributor Information
Zachary C. Lum, Email: zclum@ucdavis.edu.
Lawrence D. Dorr, Email: patriciajpaul@yahoo.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Stulberg SDH W.H. Acetabular dysplasia, development of osteoarthritis of the hip. In: Harris W., editor. The Hip Proceedings of the Second Open Scientific Meeting of the Hip Society. C.V. Mosby Co.; MO): 1974. pp. 82–93. [Google Scholar]
- 2.Ganz R., Leunig M., Leunig-Ganz K., Harris W.H. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008 Feb;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorr L.D., Yohei Y. Chapter 3: principles of total hip replacement. Successful techniques for total hip replacement. In: Dorr L.D., editor. Future Medicine. August 2014. pp. 18–33. [Google Scholar]
- 4.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970 Feb;52(1):148–159. [PubMed] [Google Scholar]
- 5.Ranawat C.S., Maynard M.J. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;(6):17–25. [Google Scholar]
- 6.Dorr L.D., Malik A., Dastane M., Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009 Jan;467(1):119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dastane M., Dorr L.D., Tarwala R., Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res. 2011 Feb;469(2):429–436. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wroblewski B.M., Siney P.D., Fleming P.A. The principle of low frictional torque in the Charnley total hip replacement. J Bone Joint Surg Br. 2009 Jul;91(7):855–858. doi: 10.1302/0301-620X.91B7.22027. [DOI] [PubMed] [Google Scholar]
- 9.Charnley J., Ferreiraade S. Transplantation of the greater trochanter in arthroplasty of the hip. J Bone Joint Surg Br. 1964 May;46:191–197. [PubMed] [Google Scholar]
- 10.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 11.Johnston R.C., Brand R.A., Crowninshield R.D. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979 Jul;61(5):639–652. [PubMed] [Google Scholar]
- 12.Ranawat C.S., Dorr L.D., Inglis A.E. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980 Oct;62(7):1059–1065. [PubMed] [Google Scholar]
- 13.Karachalios T., Hartofilakidis G., Zacharakis N., Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res. 1993 Nov;(296):140–147. [PubMed] [Google Scholar]
- 14.Charles M.N., Bourne R.B., Davey J.R., Greenwald A.S., Morrey B.F., Rorabeck C.H. Soft-tissue balancing of the hip: the role of femoral offset restoration. J Bone Joint Surg Am. 2004 May;86(5):1078–1088. [PubMed] [Google Scholar]
- 15.Lecerf G., Fessy M.H., Philippot R. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009 May;95(3):210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 16.Sakalkale D.P., Sharkey P.F., Eng K., Hozack W.J., Rothman R.H. Effect of femoral component off- set on polyethylene wear in total hip arthroplasty. Clin Orthop. 2001;388:125–134. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Wan Z., Boutary M., Dorr L.D. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008 Jan;23(1):51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Kim D.H., Cho S.H., Jeong S.T., Park H.B., Hwang S.C., Park J.S. Restoration of the center of rotation in revision total hip arthroplasty. J Arthroplasty. 2010 Oct;25(7):1041–1046. doi: 10.1016/j.arth.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 19.Asayama I., Chamnongkich S., Simpson K.J., Kinsey T.L., Mahoney O.M. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005 Jun;20(4):414–420. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 20.Scheerlinck T. Cup positioning in total hip arthroplasty. Acta Orthop Belg. 2014 Sep;80(3):336–347. [PubMed] [Google Scholar]
- 21.Brown T.D., Callaghan J.J. Impingement in total hip replacement: mechanisms and consequences. Curr Orthop. 2008;22:376–391. doi: 10.1016/j.cuor.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malik A., Maheshwari A., Dorr L.D. Impingement with total hip replacement. J Bone Joint Surg Am. 2007 Aug;89(8):1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 23.Lum Z.C., Coury J.G., Cohen J.L., Dorr L.D. The current knowledge on spinopelvic Mobility. J Arthroplasty. 2018 Jan;33(1):291–296. doi: 10.1016/j.arth.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 24.Little N.J., Busch C.A., Gallagher J.A., Rorabeck C.H., Bourne R.B. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467(11):2895–2900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pierchon F., Migaud H., Fontaine C., Duquennoy A. Determination thorique du centre de l'art, coxo-ffmorale en cas de dysplasie ou de luxation bilatrale de hanche. Rev Chir Orthopédique. 1993;79:281–284. [PubMed] [Google Scholar]
- 26.Fessy M.H., N'Diaye A., Carret J.P., Fischer L.P. Locating the center of rotation of the hip. Surg Radiol Anat. 1999;21(4):247–250. doi: 10.1007/BF01631394. [DOI] [PubMed] [Google Scholar]
- 27.Dorr L.D., Bechtol C.O., Watkins R.G., Wan Z. Radiographic anatomic structure of the arthritic acetabulum and its influence on total hip arthroplasty. J Arthroplasty. 2000 Oct;15(7):890–900. doi: 10.1054/arth.2000.8323. [DOI] [PubMed] [Google Scholar]
- 28.Widmer K.H. Containment versus impingement: finding a compromise for cup placement in total hip arthroplasty. Int Orthop. 2007 Aug;31(Suppl 1):S29–S33. doi: 10.1007/s00264-007-0429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.