Abstract
Uterine fibroid embolization has been proven effective in treating symptomatic uterine fibroids for appropriately selected patients as an alternative option to surgical approaches. The most common adult uterine position is anteverted followed by a retroverted uterus which can be found in roughly 15%-20% of normal adult females. The positioning of the uterus can change from anteversion to retroversion due to the filling of bladder or during pregnancy; however, changing from retroverted to anteverted position without prior pregnancy or endometriosis is rather uncommon. Here, we describe a case of uterine orientation change from retroversion to anteversion presenting 6 months after uterine fibroid embolization.
Keywords: Anteverted uterus, Retroverted uterus, Anteversion, UFE, Flipped uterus, Tipped uterus
Introduction
Uterine fibroid embolization (UFE) has been proven effective in treating symptomatic uterine fibroids for appropriately selected patients as an alternative option to surgical approaches [1], [2], [3]. The most common adult uterine position is anteverted followed by a retroverted uterus which can be found in roughly 15%-20% of normal adult females [4]. The positioning of the uterus can change from anteversion to retroversion due to the filling of bladder or during pregnancy; however, changing from retroverted to anteverted position without prior pregnancy or endometriosis is rather uncommon. Here, we describe a case of incidental uterine anteversion presenting 6-months after UFE.
Case report
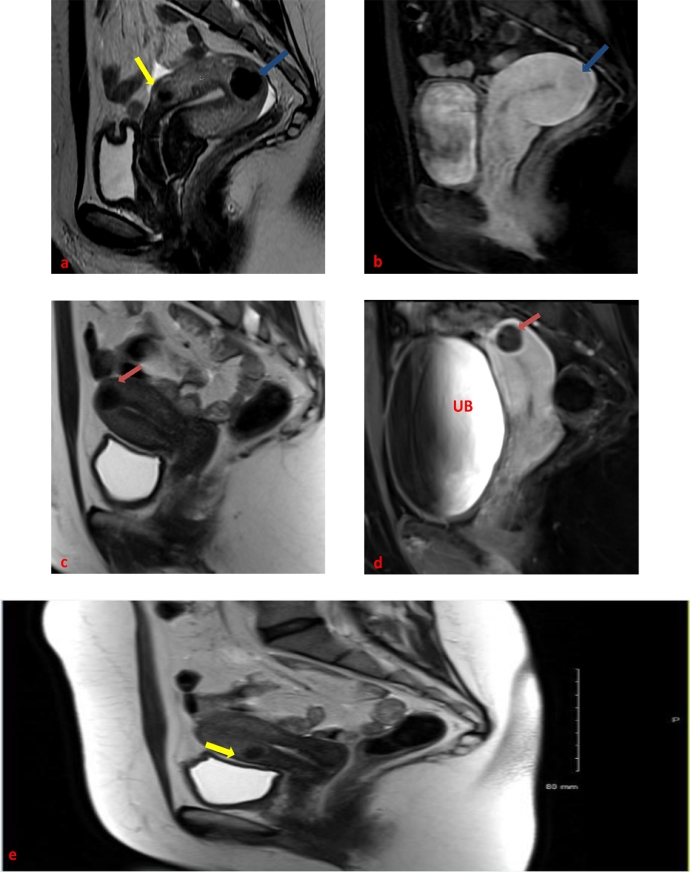
Forty-six-year old nulliparous female, status post prior myomectomy for dysfunctional uterine bleeding presented to our multidisciplinary uterine fibroid clinic with menometrorrhagia. Patient's preprocedural magnetic resonance imaging (MRI) revealed multiple intramural fibroids within an overall enlarged retroverted uterus measuring 9 cm × 6.3 cm × 5 cm. The largest fibroid which we termed the index fibroid was located within the uterine fundus and measured 2.3 cm × 2.1 cm × 2 cm. The second largest fibroid was located anteriorly and measured 1.8 cm × 1.7 cm × 1.5 cm. Both fibroids demonstrated post contrast isoenhancement compared to the background myometrium. Other much smaller intramural fibroids we also noted. (Fig. 1 a and b).
Fig. 1.
Forty-six-year-old female with multiple fibroids before and after embolization: pre-UFE T2-weighted (a) and postgadolinium T1-weighted (b) sagittal images showing an enhancing intramural fundal fibroid (blue arrows) within a retroverted uterus. An anteriorly located fibroid with similar imaging features can also be seen on pre-UFE imaging (yellow arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
All treatment options were reviewed with the patient, including myomectomy, hysterectomy, hormonal therapies, and uterine fibroid embolization. Patient decided to proceed with UFE. Pre procedural work-up included a pelvic MRI with and without contrast enhancement, a Pap smear and an endometrial biopsy. Tissue results were negative for atypia and/or malignancy. A routine UFE was carried out with selective left uterine artery embolization followed by right uterine artery embolization from right common femoral artery access, using multiple vials of 500-700 microns Embosphere (Embospheres, Biosphere Medical, Rockland, MA) particles followed by 700-900 microns Embosphere (Embospheres, Biosphere Medical, Rockland, MA) particles. Embolization proceeded to near stasis for both uterine arteries. (Fig. 2)
Fig. 2.
Pre-embolization digital subtracted angiogram (DSA) of the right (a) and left (c) uterine arteries showed filling of bilateral uterine arteries and distal branches (red circles); post-embolization DSA of the right (b) and left (d) uterine arteries demonstrated near stasis of the bilateral uterine artery branches (blue circles). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
At our institution, patients undergoing UFE are given epidural patient-controlled analgesia post procedurally and admitted for 23-hour observation. In our case, the patient's subsequent hospitalization course was uneventful with well-controlled post procedural pain. The patient came back to our multidisciplinary clinic for her 6-month post UFE follow-up. She reported complete resolution of her original presenting symptoms, including her menstrual pain and heavy bleeding. Her 6-months post UFE contrast enhanced MRI images showed complete devascularization and shrinkage of her fibroids with overall decrease of uterine volume from 9 cm × 6.3 cm × 5 cm down to 7.2 cm × 4.8 cm × 3.2 cm. The index fibroid located in the uterine fundus had an estimated volume decrease from 5575 mm3 down to 2144 mm3. Interestingly, the anteriorly located fibroid decreased even further from 2572 mm3 down to 696 mm3. Upon review of her post procedural MRI, we noted the interval change in uterine orientation from retroverted to anteverted compared with her pre procedural MRI images. (Figs. 1c, d and e).
Discussion
Anteverted uterus is the most commonly seen position of the adult uterus, while retroverted uterus is less common, representing about 15%-20% of normal adult females. It is well accepted that the positioning of the uterus can change from anteversion to retroversion due to the filling of bladder or during pregnancy; however, changing from retroverted to anteverted position without prior pregnancy or endometriosis is rather uncommon.
In our case, the treated uterus flipped from its original retroverted position to anteverted position after decrease in overall uterine volume and shrinkage of the fibroid bulk. Specifically, the significant decrease in size of the anterior uterine fibroid was theorized to be responsible for the change in uterine orientation given its positioning along the uterus’ longitudinal axis of rotation from retroversion to anteversion. However, our patient reported no significant complaints related to this finding. In our case, underlying fibroid disease could have been the potential cause for the patient's uterine retroversion as fibroids have been reported in the literature as a risk factor for retroversion [5].
A retroverted uterus may rarely be associated with unexplained pelvic pain, especially during coitus as its lower position within the pelvis increases the likelihood of dyspareunia. In intractable severe situations, laparoscopic uterine ventrosuspension may be performed for pain relief [6]. Also, C-section delivery associated scarring is reported to change the uterine orientation to retroversion [7]. However, while a native anteverted uterus has no known clinical consequence; anteversion of the uterus after UFE or surgical intervention has not been described and may simply represent a benign asymptomatic process. Awareness of this change in uterine orientation may alter approach in any future surgical intervention.
References
- 1.Spies JB, Scialli AR, Jha RC. Initial results from uterine fibroid embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 1999;10(9):1149–1157. doi: 10.1016/s1051-0443(99)70212-5. [DOI] [PubMed] [Google Scholar]
- 2.Goodwin SC, McLucas B, Lee M. Uterine artery embolization for the treatment of uterine leiomyomata midterm results. J Vasc Interv Radiol. 1999;10(9):1159–1165. doi: 10.1016/s1051-0443(99)70213-7. [DOI] [PubMed] [Google Scholar]
- 3.Edwards RD, Moss JG, Lumsden MA. Committee of the randomized trial of embolization versus surgical treatment for fibroids. Uterine-artery embolization versus surgery for symptomatic uterine fibroids . N Engl J Med. 2007;356(4):360–370. doi: 10.1056/NEJMoa062003. [DOI] [PubMed] [Google Scholar]
- 4.Haylen BT. The retroverted uterus: ignored to date but core to prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(6):555–558. doi: 10.1007/s00192-005-0051-0. Epub 2006 Jul 5. [DOI] [PubMed] [Google Scholar]
- 5.Wu CQ, Lefebvre G, Frecker H, Husslein H. Urinary retention and uterine leiomyomas: a case series and systematic review of the literature. Int Urogynecol J. 2015;26(9):1277–1284. doi: 10.1007/s00192-015-2665-1. Epub 2015 Mar 10. [DOI] [PubMed] [Google Scholar]
- 6.Perry CP, Presthus J, Nieves A. Laparoscopic uterine suspension for pain relief: a multicenter study. J Reprod Med. 2005;50(8):567–570. [PubMed] [Google Scholar]
- 7.Kaelin Agten Andrea, Honart Anne, Monteagudo Ana, Mcclelland Spencer, Basher Basmy, Timor-Tritsch IlanE. Cesarean delivery changes the natural position of the uterus on transvaginal ultrasonography. J Ultrasound Med. 2018;37:1179–1183. doi: 10.1002/jum.14461. [DOI] [PubMed] [Google Scholar]