Abstract
Background
The current housing crisis in the U.S. requires the consideration and promotion of policies that improve the circumstances of severe housing cost burdens. Building public awareness of the health impacts associated with housing affordability may be a key prerequisite for policy change.
Methods
Quantitative and qualitative data from a national survey were used to investigate public understandings about housing affordability as a key driver of health. Quantitative and qualitative findings were integrated to test whether any relationships existed between respondents’ considerations and concerns about housing affordability and their perceptions about housing affordability as a social determinant of health.
Findings
These data support four key findings. First, understandings of the relationship between affordable housing and health are partisan and income-based driven, with Republicans and high-income respondents less likely to acknowledge the effects of housing affordability on health. Second, varied frames of communication about the relationship between housing affordability and health may produce significantly different reactions among political and income subgroups.
Third, while there is considerable agreement that housing affordability promotes health when using forced-choice measures, connections between affordable housing and health are not readily volunteered. Finally, the themes of personal responsibility and stability and security significantly resonate with Republicans and high-income earners.
Conclusions
Contextualizing the issue of housing affordability within various domains in ways that effectively resonate with the American public and policymakers and across political and income spectra, is highly imperative.
Keywords: Mixed methods, Affordable housing, Health, Public opinion, Values, Policy
Highlights
-
•
When using forced-choice measures, the public agrees that affordable housing promotes health.
-
•
However, the housing/health connection doesn’t necessarily “stick” or exist in respondents’ minds.
-
•
Agreement about affordable housing/health connection is divided along political and income lines.
-
•
Values are intertwined in public discourse about the affordable housing/health connection.
-
•
Discussing affordable housing with health and other themes may resonate across political and income spectra.
1. Introduction
Housing is a critical social determinant of health (Kavanagh et al., 2016; Braubach, 2011; Gibson et al., 2011; Shaw, 2004). There are four major connections between housing and poor health outcomes. The first is substandard housing quality, which increases risk of experiencing adverse physical and mental health conditions, such as lead poisoning, asthma, injury and stress (Fukuzawa & Karnas, 2015; Lubell et al., 2013). The second includes characteristics of unhealthy neighborhoods, such as the lack of recreational areas, low walkability, and decreased access to full service grocery stores (Fukuzawa & Karnas, 2015; Lubell et al., 2013). The third consists of poor social and community attributes, including low levels of neighborhood security and social cohesion, residential segregation, and concentrated poverty (Fukuzawa & Karnas, 2015; Lubell et al., 2013).The fourth connection between housing and poor health is affordability – the cost of housing relative to household income (Maqbool, Viveiros, & Ault, 2015).
1.1. Unaffordable housing and health
Housing affordability is linked to numerous physical and psychological health consequences (Krieger and Higgins, 2002, Lubell et al., 2007, Pollack et al., 2010, Mason et al., 2013) and high health care spending (Sandel, Cook, et al. 2016). Behavioral health issues, such as alcoholism (Bentley, Baker, Mason, Subramanian, & Kavanagh, 2011), are associated with living in homes at-risk of foreclosure, or in neighborhoods experiencing high rates of foreclosure (Downing, 2016). Lack of stable housing due to cost creates barriers to accessing health care, which is particularly detrimental to vulnerable populations and individuals living with chronic conditions (Kushel et al., 2006, Aidala et al., 2016).
Macro-level policy decisions around planning and zoning prevent low- and moderate-income households, and racial/ethnic minorities, from obtaining and maintaining affordable housing (U.S. Department of Housing and Urban Development, 2005, Wiley and Powell, 2006, Reeves and Halikias, 2016). These structural constraints include restrictive zoning laws that limit construction of residential housing, producing housing shortages and dramatic spikes in prices of existing homes (Brown Calder, 2017, Nino, 2017). Rent control laws have contributed to a shortage of affordable housing, and incited discriminatory renting practices as well (Chiland, 2018). For example, California’s rent control act, Costa-Hawkins, has had a disproportionate negative effect on low-income and minority residents (Kamel, 2012) and serves as a legal obstacle to rental inclusionary housing programs (Wiener & Barton, 2014). The shortage of available housing generated by these and other policies has been further compounded by stagnant wage growth among Americans. Since 1960, rents in the U.S. have risen 64% while incomes have only increased 18% (Woo, 2016).
The confluence of these phenomena has resulted in housing cost burden and severe cost burden (mortgage/rent greater than 30% of income, or, 50% of income, respectively), which present formidable challenges to low- and moderate-income families in both urban and rural communities (Murray and Schuetz, 2018, National Rural Housing Coalition, 2018). An estimated 12 million renter and homeowner households in the U.S. pay more than 50% of their annual incomes on housing (Steffen et al., 2015). Housing cost burden is not only a risk factor for poor health and the postponement of health care services but is also at least as important as other housing risk factors, including measures of physical quality (Coley et al., 2013, Meltzer and Schwartz, 2016).
Housing burden, as well as property owners disproportionately targeting vulnerable groups for eviction (Desmond, An, Winkler, & Ferriss, 2013), has led to approximately 500,000 homeless individuals on any given night in the U.S. (National Alliance to End Homelessness, 2018), and nearly one million evictions in 2016 (Brancaccio & Long, 2018). Indeed, among tenants facing or experiencing eviction due to housing arrears, the psychological and physical health effects are striking. Children and caregivers in low-income households struggling to pay rent have increased risk of poor health, including increased child hospitalizations and maternal depressive symptoms (Sandel et al., 2018). Similarly, mothers experiencing eviction have significantly more material hardship and depression, and are more likely to report worse health for their children and greater parenting stress (Desmond & Kimbro, 2015). Eviction has also been associated with both psychological trauma (Fullilove & Shock, 2004) and as a risk factor for suicide (Serby, Brody, Amin, & Yanowitch, 2006).
Housing burden also causes individuals and families to live in housing with an insufficient number of rooms relative to the number of people living in the dwelling (Leventhal and Newman, 2010, Solari and Mare, 2012). In addition to poor physical and behavioral health outcomes, crowding has been linked to lower math and reading scores among school-age children, which may impede their ability to succeed later in life (Leventhal and Newman, 2010, Solari and Mare, 2012). Notably, crowding not only affects low-income populations, but impacts middle-class dwellers as well (Thornberg, 2016)
1.2. Public views on housing affordability as a social & economic determinant of health
Research suggests that the public has little understanding of how social and economic forces align to produce poor health (Robert et al., 2008, RWJF et al., 2010). For the most part, Americans attribute health to individual-based behaviors and access to medical care as opposed to broad-based social and economic factors, such as housing, income, and employment (i.e. social determinants of health) (Robert et al., 2008, Gollust et al., 2009). The Robert Wood Johnson Foundation’s (RWJF) 2010 study, “A New Way to Talk About The Social Determinants of Health”, ascertained public beliefs regarding variations in health and why these variations exist among population sub-groups. Although the phrase ‘social determinants of health’ elicited negative public reactions, its underlying construct was nonetheless well received (RWJF et al., 2010).
Public agreement about the impact of social and economic determinants may be steadily growing. For example, a recent study found growing numbers of Americans now acknowledge social and economic factors as having “a strong influence on individual health” (Bye, Ghirardelli, & Fontes, 2016). In regard to housing, such views correspond with earlier findings regarding public opinion about housing quality and its effects on health and educational opportunities (Belden, Shashaty, & Zipperer, 2004). Though these studies suggest heightened public awareness of the influence of the social and economic determinants of health, less is known about the extent of public understanding about whether or how housing affordability impacts health (Manuel & Kendall-Taylor, 2016) or the current state of public support for policies targeting housing affordability to improve health.
1.3. Building public awareness of the link between housing affordability and health
In light of the critical connection between housing affordability and health, the U.S. housing crisis calls for the consideration and promotion of policies that improve the circumstances of housing cost burdens (Freeman, 2002, National Law Center on Homelessness & Poverty, 2016). Generally, affordable housing policies can be classified into three major categories: rental assistance, homeownership assistance, and land use and regulatory incentives (Kalugina, 2016). Specifically, these policies include Low Income Housing Tax Credit (LIHTC) and housing vouchers, subsidization of for-sale housing, government construction of shelter housing, inclusionary zoning, and policies to reduce the regulatory burden on new home construction (Kalugina, 2016, Taylor, 2016). Other proposed policies have geared towards decreasing housing cost burdens to prevent adverse health outcomes, such as providing monetary assistance to families heavily strained by rent or mortgage to improve self-perceived health status (Novoa, Amat, et al., 2017).
Building public awareness of the health impacts associated with housing affordability may be a key prerequisite for policy change (Fukuzawa & Karnas, 2015). The dearth of understanding about public views regarding the relationship between housing affordability and health may attenuate U.S. policymakers’ proclivity to champion robust housing policies (Robert et al., 2008, Robert and Booske, 2011). Gauging public understandings of housing affordability through a social determinants of health lens (Raphael, Curry-Stevens, & Bryant, 2008) may also be integral to promoting and advancing an effective housing policy agenda (Shiue, 2014). Whereas some studies have examined public opinion regarding the importance of housing quality on health (Robert et al., 2008, Robert and Booske, 2011), to our knowledge, no prior studies have explicitly tested whether people believe that housing affordability is a key driver of health. An initial task, therefore, is to examine whether and in what specific ways Americans regard housing affordability as a fundamental driver of overall health and well-being.
We test whether five characteristics are associated with public belief about the relationship between housing affordability and health. The first characteristic is political affiliation. Previous research suggests that public opinion on disease causality and receptivity to policies to address health and social concerns is correlated with political orientation (Gollust, Barry, & Niederdeppe, 2014). The second characteristic, annual household income, is based on evidence suggesting the role of income polarization within local efforts to block the construction of affordable housing units in wealthier neighborhoods (Nguyen et al., 2013, Davison et al., 2016). The third characteristic is geographic political context. Research shows that the public, in general, are not routinely attentive to public policy matters (Bennett, 1995) and that neighborhood political context significantly conditions attitudes and behaviors (DeSante & Perry, 2016). Therefore, it may be that the geographic political context in which one lives shapes public perception about the relationship between affordable housing and health. Finally, because the salience of housing affordability as a social concern for respondents may depend on the state of local housing market conditions, the final two characteristics we examine are severe housing burden (rent or mortgage).
2. Research methodology
2.1. Design
We apply a convergent parallel mixed-methods research design (Creswell & Plano Clark, 2011) to gain an understanding of current beliefs regarding the relationship between housing affordability and health. This design analyzes different, but complementary, strands of quantitative and qualitative data (Creswell, 2014). The quantitative and qualitative data strands were collected in the same phase. After separate analysis, results from the qualitative data strand were transformed and merged with the quantitative data strand into one dataset. As a result, the design allows us to examine variations about perceptions regarding the link between housing affordability and health across different sub-groups or levels of agreement.
2.2. Data source
Data come from a proprietary, online cross-sectional national survey (FWI Housing Affordability Survey) administered by the FrameWorks Institute between November 2015 and January 2016.
2.3. Study population
The study sample includes 400 adults, age 18 and older who are members of the Survey Sampling International (SSI) online research panel. SSI recruits panelists from over 11.5 million people who complete SSI surveys each month. Using a quota sampling design, SSI surveys are self-administered and accessible throughout a 24-hour period. For every completed survey, SSI panelists earn points that are redeemed for Amazon.com Gift Cards* or cash via PayPal. Overall, the research panel is reflective of the U.S. population in terms of gender, age, race/ethnicity, marital status, income, and educational level. Ethics approval for this study was obtained from the Institutional Review Board of The Pennsylvania State University.
2.4. Survey instrument
Close-ended survey questions were drawn from previous studies, including the National Health Interview Survey, the California Health Interview Survey, and the American National Election Studies (California Department of Public Health, 2013, American National Election Studies, 2014, Parsons et al., 2014). A series of questions pertaining to general social and demographic characteristics and political affiliation was posed to all respondents. Respondents were subsequently asked about their level of agreement with a randomized series of statements pertaining to housing affordability, including statements focusing on renters, homeowners, development, wages, low-income communities, and health. Using an iterative review process to ensure the topic under investigation was effectively captured (content validity), all quantitative statements were developed and validated by cognitive linguists and health policy scholars at the FrameWorks Institute and housing experts at Enterprise Community Partners (ECP), a non-profit organization that creates opportunity for low- and moderate-income people through affordable housing (Enterprise Community Partners, 2017). These statements were followed by an open-ended survey question asking why housing affordability mattered. Questions regarding marital status and current homeownership status were asked at the conclusion of the survey.
Response randomization for the order of all responses was used to alleviate order and survey-fatigue bias. The survey was pilot tested to evaluate the clarity of survey directions, item format, response options and length.
2.5. Measures
2.5.1. Quantitative outcomes
Our quantitative dependent outcomes are two randomly-ordered, conceptually similar statements that measure respondents’ level of agreement about the relationship between housing affordability and health on a five-point ordinal scale (ranging from “strongly disagree” to “strongly agree”): (1) The cost of housing matters for people’s health and (2) The affordability of people’s homes affects their health, not just their pocketbook.
2.5.2. Explanatory variables
The first explanatory variable is political affiliation and is measured by a set of three dummy variables (Republican, Independent, and Democrat). The second explanatory variable, annual household income, is measured by a set of five categorical variables (< $24,999; $25,000-$49,999; $50,000-$99,999; $100,000-$149,999; and > $150,000). The third explanatory variable, geographic political context, is a binary variable (0 = no; 1 = yes) measuring whether the U.S. congressional representative in a respondent’s zip code (or ‘representatives’ in those zip codes with more than one U.S. congressional representative) is a Democrat (or primarily Democrat) compared to a Republican (or primarily Republican). The last set of explanatory variables estimates severe housing burden, which measure whether a respondent resides within the top 25 percent of zip codes as measured by the percentage of households spending more than half of their income on rent (0 = no; 1 = yes) or mortgage (0 = no; 1 = yes).
2.5.3. Other variables of interest
All models adjust for sociodemographic characteristics that may confound the relationship between the explanatory variables and outcomes of interest, including gender; age; race/ethnicity; educational attainment; homeownership status; marital status; and rural residence.
2.5.4. Qualitative outcome
Our qualitative measure includes responses to an open-ended survey item: “How and why does affordable housing matter?” Survey respondents typed replies within a text window, providing information regarding beliefs on how and why housing affordability is important, in general and within the context of health and well-being.
2.6. Statistical analysis
2.6.1. Quantitative analysis
Ordinal logistic regression within fully adjusted models was used to test the association between the explanatory variables and the two outcomes of interest. The validity of the proportional odds assumption in the ordinal logistic regression models was met by testing the similarity of odds ratios (ORs) for contrasts between each level of the dependent variable (results available upon request). Parameter estimates from these models indicate the odds of having a higher level of agreement that housing affordability is linked to health above any threshold compared with those below that threshold.
Population weights were applied to adjust for race/ethnicity and educational attainment differences between the study sample and the national population. We used an alpha level of p< 0.05 for all statistical two-tailed tests. All analyses were conducted using Stata version 14.2 (Stata Corp, College Station, TX).
2.6.2. Qualitative data analysis
To analyze the qualitative data, text responses for the open-ended item were imported verbatim from Excel into NVivo 11 Pro (QSR International, Burlington, MA). Using a grounded theory approach (Bernard, 2011), two independent coders first conducted a general review of a randomly drawn sample of responses (n=80) followed by open coding to identify major themes and sub-themes, respectively, until saturation was reached. Next, thematic coding was iteratively conducted using a series of random samples. Disagreements between coders were resolved by a third coder. Intercoder agreement measured by Cohen’s κ, provided reliability to the analysis and ranged between 0.70 and 1.00 (substantial to perfect agreement) for all identified themes (McHugh, 2012). Coders did not access the survey data throughout the coding process.
2.6.3. Mixed-methods data analysis
Both the quantitative and qualitative data were merged in the final analysis and interpretation phases of the study. In a convergent parallel design, this is accomplished by transforming one type of data into the other type of data. For our purposes, the qualitative data were quantified into counts to examine the relationships between respondents’ level of agreement regarding housing affordability as a social determinant of health (as measured by the two outcome variables) and their extemporaneous views about the ways in which affordable housing mattered. Themes that were raised by at least 20% of the sample (i.e. > 50 respondents) were transformed into quantitative data categories and used throughout subsequent statistical analyses. Each category was coded “1” if it emerged at least once in a respondent’s comments and coded “0” otherwise.
3. Results
3.1. Quantitative results
Table 1 presents descriptive statistics of the study population. Overall, the weighted study sample was reflective of the U.S. population, though it included fewer, younger adults between the ages of 18 to 29 as well as a greater number of individuals who politically identified as Independents. Table 2 presents weighted frequencies regarding the strength of agreement with each of the two outcome variables of interest by political affiliation and annual household income. Overall, most respondents agreed with each of the two outcome statements (69% and 73%, respectively). Differences in level of agreement existed among the three political groups for the first outcome (p< 0.001). Approximately, 83% of Democrats strongly agreed or agreed with the first and second statement, compared to 65% of Independents and 61% of Republicans. Differences in level of agreement for the first statement were also found among income-level groups (p< 0.001), with respondents in the highest income level having lower percentages of agreement (43%) compared to those in lower income levels (70%).
Table 1.
Demographics of study sample and U.S. population.
| Variables (%) |
(N= 400) |
U.S. Populationb, c, d |
|---|---|---|
| Weighted Meana | ||
| Gender | ||
| Female | 52.7 | 50.8 |
| Male | 47.3 | 49.2 |
| Age | ||
| 18 to 29 years | 13.3 | 21.7 |
| 30 to 44 years | 27.3 | 25.1 |
| 45 to 60 years | 28.8 | 27.9 |
| >61 years | 30.6 | 25.3 |
| Race/Ethnicity | ||
| Asian/Pacific Islander | 5.9 | 5.1 |
| Black/African American | 12.1 | 12.3 |
| Hispanic | 14.8 | 17.1 |
| Non-Hispanic White | 67.2 | 62.3 |
| Other | 0.0 | 3.2 |
| Marital Status | ||
| Never Married | 30.9 | 33.5 |
| Married | 48.1 | 47.5 |
| Separated or Divorced | 14.7 | 13.1 |
| Widowed | 6.2 | 5.8 |
| Annual Household Income | ||
| 0 to 24,999 K | 27.5 | 23.1 |
| 25Kto 49,999 K | 27.8 | 23.5 |
| 50 K to 99,999 K | 26.1 | 29.9 |
| 100 K to 149,999 K | 12.7 | 13.1 |
| > 150 K | 5.9 | 10.4 |
| Educational Attainment | ||
| High School Degree or less | 41.1 | 41.2 |
| Some College | 26.3 | 26.3 |
| Bachelor’s Degree | 20.5 | 20.5 |
| Graduate Degree | 12.0 | 12.0 |
| Homeownership Status | ||
| Own | 63.6 | 65.1 |
| Rent | 36.4 | 34.6 |
| Political Affiliation | ||
| Democrat | 41.1 | 46.7 |
| Independent | 33.8 | 24.8 |
| Republican | 27.5 | 32.8 |
Note. Columns sum to 100% down rows in variable blocks. Percentages may not sum to 100 because of rounding error.
Population weights were applied to adjust for race/ethnicity and educational attainment differences.
U.S. population gender, race/ethnicity, marital status, income, educational attainment, and homeownership status data come from the 2011–2015 American Community Survey (ACS) 5-year estimates.
U.S. population age data come from the 2015 ACS Population single-year of age estimates.
U.S. population political affiliation data come from the American National Election Studies 2012.
Table 2.
Strength of Agreement that Housing Affordability is linked to Health by Political Affiliation and Annual Household Income.a, b, c
| Outcome 1: The cost of housing matters for people’s health | Outcome 2: The affordability of people’s homes affects their health, not just their pocketbook | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables (%) | Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | p | Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | p |
| Overall Sample (N=400) | 2.0 | 9.9 | 19.6 | 40.6 | 27.9 | ### | 2.6 | 11.6 | 13.4 | 39.4 | 33.1 | ### |
| Political Affiliationd | *** | † | ||||||||||
| Democrat | < 0.01 | 6.5 | 10.5 | 42.7 | 40.3 | < 0.01 | 7.4 | 10.7 | 39.8 | 42.1 | ||
| Independent | 2.5 | 9.3 | 26.8 | 34.6 | 26.8 | 3.5 | 14.2 | 13.8 | 36.3 | 32.2 | ||
| Republican | 4.1 | 15.6 | 23.6 | 44.8 | 11.9 | 5.0 | 14.2 | 16.6 | 42.5 | 21.7 | ||
| Annual Household Incomee | *** | * | ||||||||||
| 0 to 24,999 K | < 0.01 | 8.4 | 22.3 | 37.1 | 32.2 | < 0.01 | 15.1 | 15.9 | 27.0 | 41.3 | ||
| 25Kto 49,999 K | 1.8 | 6.9 | 13.7 | 39.2 | 38.0 | 2.0 | 7.9 | 5.3 | 43.0 | 41.9 | ||
| 50 K to 99,999 K | 4.4 | 12.6 | 18.2 | 44.6 | 20.2 | 4.5 | 14.4 | 13.3 | 40.5 | 27.4 | ||
| 100 K to 149,999 K | < 0.01 | 10.2 | 24.0 | 43.9 | 22.0 | 2.4 | 10.9 | 23.6 | 44.2 | 19.0 | ||
| >150 K | 5.4 | 19.5 | 31.7 | 38.1 | 5.4 | 5.4 | 1.9 | 18.5 | 64.4 | 9.8 | ||
***p< 0.001, **p< 0.01, *p< 0.05, †p< 0.10 between all all levels
Rows sum to 100% down columns in variable blocks. Percentages may not sum to 100 because of rounding error.
Estimates are weighted using population weights.
Democrats (n = 167); Independents (n = 129); Republicans (n = 104)
0–24 K (n = 92); 25–49 K (n = 95); 50–99 K (n = 120); 100–149 K (n = 61); > 150 K (n = 32)
Kruskal-Wallis nonparametric tests with Dunn’s pairwise comparisons indicate that across all levels of agreement, political affiliation categories significantly differ from each other for Outcome 1 (p< 0.001).
Kruskal-Wallis nonparametric tests with Dunn’s pairwise comparisons indicate that significant differences exist across all levels of agreement between income category > 150 K and all other categories for Outcome 1 (p< 0.001). Significant differences also exist across most levels of agreement between income category > 150 K and income categories 0–24 K, 25–49 K, and 50–99 K for Outcome 2 (p< 0.05).
Table 3 presents adjusted odds ratios and their 95% confidence intervals of the associations between each of the explanatory variables and the two dependent outcomes. Three explanatory variables were significantly associated with the first outcome of interest (i.e. level of agreement regarding, “The cost of housing matters for people’s health”), adjusting for all other factors. First, Democrats had significantly greater odds of having higher levels of agreement compared to Independents (aOR = 2.09; 95% CI = 1.18, 3.70) and Republicans (not shown) (aOR = 2.95; 95% CI = 1.59, 5.49). Second, the odds of having higher levels of agreement were significantly lower among those with an annual household income of $150,000 or above compared to those making less than $25,000 (aOR = 0.22; 95% CI = 0.07, 0.711). Third, living within a zip code that was congressionally represented by all or mostly Democrats, compared to those represented by Independents or Republicans, was also associated with greater odds of having higher levels of agreement (aOR = 1.72; 95% CI = 1.03, 2.89). No other statistically significant associations existed between the outcomes of interest and the fourth explanatory variable (severe housing burden). Regarding the second outcome of interest (i.e. level of agreement with the statement, “The affordability of people’s homes affects their health, not just their pocketbook”), no statistically significant associations were found at the p< 0.05 level.
Table 3.
Ordinal logistic regression estimates for level of agreement that health is linked to housing affordability (N = 400).a,b
| The cost of housing matters for people’s health | The affordability of people’s homes affects their health, not just their pocketbook | |||
|---|---|---|---|---|
| Independent Variable | Unadjusted OR [95% CI] | aOR [95% CI]c | Unadjusted OR [95% CI] | aOR [95% CI]d |
| Political Affiliation | ||||
| Independent (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Democrat | 2.06 [1.15, 3.71] | 2.09 [1.18, 3.70] | 1.59 [0.92, 2.77] | 1.52 [0.87, 2.66] |
| Republican | 0.67 [0.35, 1.27] | 0.71 [0.37, 1.35] | 0.75 [0.40, 1.42] | 0.72 [0.38, 1.36] |
| Annual Household Income | ||||
| 0 to 24,999 K (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 25Kto 49 K | 1.44 [0.72, 2.90] | 1.38 [0.67, 2.85] | 1.51 [0.73, 3.12] | 1.42 [0.67, 3.00] |
| 50 K to 99 K | 0.66 [0.33, 1.30] | 0.50 [0.22, 1.16] | 0.60 [0.35, 1.48] | 0.68 [0.30, 1.53] |
| 100 K to 149 K | 0.77 [0.39, 1.53] | 0.64 [0.28, 1.48] | 0.60 [0.29, 1.24] | 0.61 [0.25, 1.47] |
| > 150 K | 0.29 [0.11, 0.70] | 0.22 [0.07, 0.71] | 0.62 [0.28, 1.37] | 0.53 [0.20, 1.42] |
| Geopolitical Context | ||||
| Congressional Rep - Republican (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Congressional Rep - Democrat | 1.85 [1.15, 2.99] | 1.72 [1.03, 2.89] | 1.38 [0.87, 2.18] | 1.45 [0.87, 2.42] |
| Severe Housing Burden | ||||
| Bottom 75th Percentile - Rent (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Top 25th Percentile - Rent | 0.89 [0.52, 1.55] | 0.82 [0.46, 1.46] | 1.07 [0.59, 1.93] | 1.03 [0.57, 1.86] |
| Bottom 75th Percentile - Mortgage (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Top 25th Percentile - Mortgage | 0.86 [0.52, 1.43] | 0.84 [0.50, 1.40] | 0.76 [0.45, 1.30] | 0.71 [0.43, 1.19] |
aOR indicates adjusted odds ratio; CI, confidence interval
Estimates reflect how strongly respondents agreed or disagreed with the following statements:“The cost of housing matters for people's health” and “If we want to improve people's health, we need to make affordable housing a priority”
Estimates are weighted using population weights.
Models adjust for gender, age, race, marital status, educational attainment, homeownership status, and rural residence
Models adjust for gender, age, race, marital status, educational attainment, homeownership status, and rural residence
3.2. Qualitative results
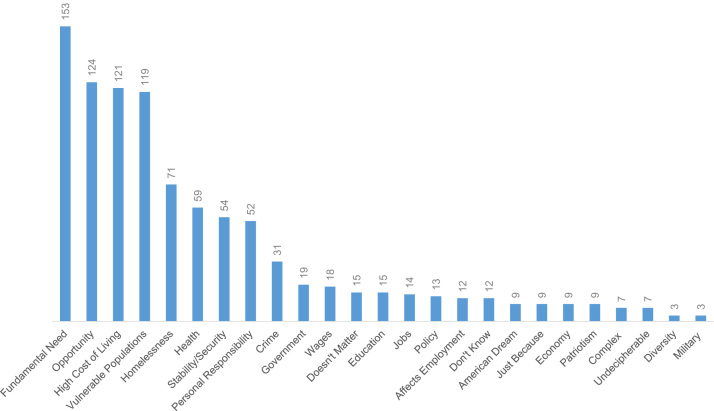
Responses to the open-ended question, “How and why does affordable housing matter?” were qualitatively analyzed to investigate respondents’ opinions about housing affordability. Comments were received from most of the respondents (n = 398). In total, 26 themes were identified (Fig. 1), with 8 themes (fundamental need, opportunity, high cost of living, vulnerable populations, homelessness, health, stability/security, and personal responsibility) emerging as the most referenced (n≥ 50 respondents).
Fig. 1.
Number of references made per qualitative theme.
3.2.1. Fundamental need, high cost of living, & stability/security
Over one-third of respondents (n = 153) depicted the issue of affordable housing as a fundamental need, comparable to food and clothing. These views were usually oriented within a rights-based framework. Many respondents also commented on how the lack of affordable housing contributed to a high cost of living (n = 121), which overwhelmed other, vital aspects of daily routines that compromised overall life satisfaction. For example:
Cost of housing affects familial relationships, causing undue stress on financial, educational, emotional elements. Travel to & from job(s) from out-of-the-way neighborhoods simply to make ends meet is poor time management, & takes away any quality of life.
Others stressed that affordable housing mattered for a more secure and stable lifestyle. Thus, at least for these respondents, affording your home enhanced financial, physical, and emotional stability and security (n = 54), which contributed to quality of life.
3.2.2. Vulnerable populations & homelessness
Some respondents identified the economically-disadvantaged as well as families and children as being most vulnerable to the adverse effects of housing insecurity (n = 119). Here, affordable housing was considered a necessary condition for fostering positive community engagement and for generating life-enhancing experiences, particularly for children. However, some asserted that government efforts to assist the poor were often unfair to the middle class.
The threat of becoming or remaining homeless was also cited (n = 71) to explain why affordable housing matters. Some respondents viewed homelessness as a cause of societal distress, burden, and national shame.
3.2.3. Values
Throughout respondents’ comments about why affordable housing mattered, two distinct values were invoked: opportunity (n = 124) and personal responsibility (n = 52). Often, the value of opportunity was employed to specify ways housing affordability enriched lives:
Affordable housing improves not only the lives of the people who are being housed but the communities within which those people live. In addition to the basic human decency and duty to care for our fellow persons, we must acknowledge that it is in our own best interest to care for the less advantaged.
The value of personal responsibility, was often raised by those who identified affordable housing as important for individual’s self-confidence and building a strong work ethic:
It [affordable housing] builds confidence in the worker to be able to buy a piece of America. If home prices are so high that only the rich are able to buy, then this discourages everyone. Once the dream is out of reach, the citizen wonders why they should continue to work hard if they can’t expect to achieve this goal.
A very small number of respondents simultaneously raised the values of opportunity and personal responsibility (n = 10), particularly within the context of government aid. For example, even after recognizing the lack of opportunities to purchase or rent affordable homes, these respondents still considered receiving government support as something to be avoided. In their view, government assistance jeopardized self-reliance and deterred individuals from securing stable housing on their own.
Finally, pejorative language (e.g. “stupid” or “lazy”) was used among some respondents to assign blame to individuals for failing to secure or maintain affordable housing while exempting government from assuming responsibility.
3.2.4. Health
Health was the sixth highest emerging theme among respondents (n = 59) and was discussed in terms of psychological health, general health, and medical care and health insurance. Comments on psychological health centered on housing affordability mattering for happiness; the alleviation of emotional and/or physical stress related to financial strain; and the improvement of self-confidence and independence. Comments on general health primarily credited affordable housing as paramount to universal health and overall well-being. Finally, comments on medical care and health insurance focused on the relationship between affordable housing and the ability to purchase health coverage, access timely care, and live in neighborhoods with higher quality physicians. Others noted the indirect, negative impact of unaffordable housing on the health care system, such as the need for more extreme, expensive medical care due to lack of primary care access:
3.3. Mixed-methods results
Our quantitative analysis revealed the level to which respondents agreed that affordable housing and health were connected. Our qualitative analysis identified emerging themes throughout respondents’ comments about how affordable housing mattered. The mixed methods analysis, by integrating these separate strands of data, allowed us to examine the frequencies of those themes by respondents’ political affiliation, annual household income, and geographic political context. The analyses (available upon request) suggest that the theme of personal responsibility was more frequently raised among Republicans than either Democrats (p< 0.001) or Independents (p< 0.05); as well as among respondents residing in zip codes not congressionally represented by a Democrat (p< 0.001). The analyses also showed that the theme of stability/security was raised more often among respondents with the highest level of income (≥ $150 K) compared to those with lower income (p< 0.001).
Frequency of themes raised per respondents’ level of agreement that housing affordability is linked to health were also examined. Analyses revealed that different levels of agreement (disagree, neutral, agree) for each of the two outcome statements were also significantly associated with particular themes over others. For example, the themes of homelessness and stability/security were more frequently raised among those who agreed with the first statement compared to those who disagreed (p< 0.05) while the theme of health was more frequently raised among those who agreed with the second statement compared to those who disagreed (p< 0.01). The data also suggest that the theme of personal responsibility significantly emerged more often among respondents who disagreed with either the first (p< 0.01) or the second statement (p< 0.01) compared to those who neither agreed nor disagreed or agreed, respectively.
4. Discussion
Our study employs a research design that integrates quantitative findings with supplemental qualitative data to gain a more comprehensive and nuanced understanding of public views regarding the importance of housing affordability on health – views that could ultimately encourage or inhibit the passage of policies that minimize housing cost burden and its health repercussions.
These data support four key findings. First, understandings of the relationship between housing affordability and health is both partisan and income-level driven. Beliefs regarding disease causation, as well as historical and contemporary politicization of efforts to address housing affordability, may work concordantly to shape disparate views on the relationship between affordable housing and health. Contrasting perspectives about the causes of poor health prevail, with the public far more likely to place greater emphasis on the relationship between personal health behaviors and health outcomes, as opposed to the effects of social and economic factors (Robert & Booske, 2011). Research has shown that attributing disease causation to individuals is directly related to political orientation (Lundell, Niederdeppe, & Clarke, 2013) as Democrats tend to attribute poor health to complex social, economic, cultural and biological conditions compared to Republicans, who view it as the result of individuals’ poor lifestyle choices (RWJF et al., 2010). Research also suggests that income levels may account for differences in perceptions of housing affordability as an important issue. For instance, concerns about the lack of affordable housing are as big as concerns about the lack of affordable health care among working-class families compared to those with higher income (Belden, Shashaty, et al., 2004).
Our results also demonstrate that beliefs about the relationship between housing affordability and health may be uniquely shaped by respondents’ local political environment, but not necessarily by whether respondents live in areas where the level of severe housing burden is high. Studies suggest that environmental context may matter because of the way information flow is structured (Cho, Gimpel, & Dyck, 2006), especially if it is structured to emphasize certain social issues over others. Knowledge levels among distinct groups have also been connected to whether a member of that group occupies a political seat (Bobo and Gilliam, 1990, Hutchings, 2001). Thus, respondents residing within a zip code with Democratic congressional representation may be more exposed or have more access to information about the adverse health effects of housing burden. Future investigations should examine whether and in what ways discourse among policymakers in areas impacted by severe housing burden highlights the relationship between housing affordability and health.
Second, these data suggest how related, though slightly varied statements on the same topic may produce significantly different results due to framing effects. In other words, even though the two outcome statements essentially measured the same concept, certain phrases included in the first statement (e.g. “the cost of housing”) may have triggered significantly different reactions and lower levels of support among political and income subgroups. Communication and framing research has found that certain words and phrases such as “housing” and “affordable housing” (Manuel & Kendall-Taylor, 2016), may serve to induce counterproductive ways of thinking about the relationship between housing affordability and health. Other research has found that the public responds poorly to messages that start with negative terms (RWJF et al., 2010). Explicitly testing the effects of various message framing on public perceptions about the links between housing affordability and health and support for housing affordability policies, particularly among certain populations, are highly recommended.
Third, the connection between affordable housing and health is not readily articulated nor expressed by the public as are other themes, such as the connection between affordable housing as a fundamental need or as an opportunity. This finding is consistent with previous findings that suggest Americans do not “naturally” contextualize health socially, particularly in relation to their environment (RWJF et al., 2010). While our analysis showed that most respondents (approximately 70%) agreed that housing affordability is linked to health, only a small percentage (< 15%) volunteered that it mattered in their open-ended responses, potentially suggesting that health is a less salient consideration when it comes to housing affordability. For instance, when encountered with explicit messaging about the role of affordable housing as a social determinant of health, respondents generally agree. However, the connection doesn’t necessarily “stick” or exist in respondents’ minds, even within the relatively narrow time frame it takes to participate in an online survey. Testing communication strategies that reify the interconnection between housing affordability and health, in ways that are simple, easily understood and remembered by the public (Heath & Heath, 2008), may bear critical fruit via increased support of housing affordability policies. Consensus mapping and developing deep metaphor frames (RWJF et al., 2010) may also be an effective way to ensure that these communication strategies are effective.
Analysis of the qualitative data also showed that governmental efforts to increase affordable housing opportunities were supported as a means for individuals to exercise personal responsibility. Similar understandings of the interplay between the values of personal responsibility, opportunity, and governmental intervention have been found in obesity research, with the availability of and access to healthy food considered a means by which to exercise personal responsibility in obesity prevention (Ortiz, Zimmerman, & Gilliam, 2015).
Finally, the mixed-methods analyses suggest that the themes of personal responsibility and stability and security significantly resonate with Republicans and high-income earners, respectively. This finding helps to understand how characteristics, such as political affiliation and income, represent particular meanings. As prior research has shown, Republicans generally believe that health is a direct product of personal decisions, however, they are also able to acknowledge that certain communities lack the means and ability to choose a path towards health (RWJF et al., 2010). Likewise, though high-income earners had significantly lower levels of agreement that housing affordability and health are related, they also recognize affordable housing as a matter of stability and security. To widen public support and to help assuage concerns of government overreach among conservatives and high-income earners, we recommend future studies that examine how communication emphasizing that the affordability of one’s home is essential to achieving and sustaining a secure and healthy lifestyle can be diffused throughout policy discourse.
Our findings could further help concretize the interconnection between housing affordability and health. There are strong indications that suggest understandings of the relationship between affordable housing and health have taken root. The 2017 launching of New York’s $20 billion strategy to address homelessness and increase access to affordable housing (The Governor’s Press Office, 2017) serves as a prime example. The plan includes $950 million for the building of a minimum of 6000 supportive housing units (The Governor’s Press Office, 2017). Supportive housing programs coordinate services from multiple agencies to address the health needs of residents, including primary health care, mental health care, and substance use disorder treatment (Henwood, Cabassa, Craig, & Padgett, 2013).
4.1. Limitations
This study has limitations. First, the study respondents are members of SSI’s online research panel, which is a non-probability sample. Therefore, the online panel may skew from the general U.S. population in a few ways, such as having higher income and education levels, or, excluding individuals who have no access to the Internet (such as the elderly), which raises external validity concerns. We recommend that future research be conducted with a nationally representative sample to strengthen the generalizability of these findings. Second, the sample size is small. However, sample size calculations indicated that the sample was large enough to produce quantitatively reliable results, at least for the overall sample population. Finally, the ordering of the survey questions (close-ended prior to open-ended) may have primed respondents to specifically consider the health implications of housing affordability, which may have resulted in positive bias and an overestimate of the number of respondents who mentioned health in their open-ended response. Due to the nature of the mixed-methods research design, some degree of priming was unavoidable and the order was deemed appropriate given our objective to elicit and collect respondents’ robust views on housing affordability and health.
5. Conclusion
Policy efforts that aim to mitigate the housing affordability crisis and are heavily reliant upon broad public support are underway. Contextualizing the issue of housing affordability within various themes, in ways that connect with and mobilize the American public, is both timely and highly imperative.
Acknowledgements
This research was supported by funding from the Wolf chair endowment at The Pennsylvania State University, a generous gift from Gregory H. Wolf. We would like to acknowledge The FrameWorks Institute and Enterprise Community Partners for their support in providing the data. Lastly, we thank Gary J. Adler, Jr. Frederick J. Zimmerman, and affiliates of the Population Research Institute at Penn State University for their extremely generous feedback throughout the development of this manuscript. We would also like to thank Bethany Shaw for her research assistance.
Ethics approval statement
The study received approval from the Pennsylvania State University Institutional Review Board in June 2016.
No identifying information was collected by the authors.
Appendix A. Conceptual framework
None.
References
- Aidala A.A., Wilson M.G., Shubert V., Goglishvili D., Globerman J., Rueda S., Bozack A.K., Caban M., Rourke S.B. Housing status, medical care, and health outcomes among people living with HIV/AIDS: A systematic review. American Journal of Public Health Research. 2016;106(1):e1–e23. doi: 10.2105/AJPH.2015.302905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American National Election Studies . The University of Michigan and Stanford University; Ann Arbor, MI and Palo Alto, CA: 2014. User’s guide and codebook for the ANES 2012 time series study. [Google Scholar]
- Belden N., Shashaty A., Zipperer J. Belden Russonello & Stewart; Washington, DC: 2004. What we know about public attitudes on affordable housign: A review of existing public opinion research; pp. 1–72. [Google Scholar]
- Bennett S.E. Comparing Americans’ political information in 1988 and 1992. The Journal of Politics. 1995;57(2):521–532. [Google Scholar]
- Bentley R., Baker E., Mason K., Subramanian S., Kavanagh A.M. Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia. American Journal of Epidemiology. 2011;174(7):753–760. doi: 10.1093/aje/kwr161. [DOI] [PubMed] [Google Scholar]
- Bernard H.R. AltaMira Press; California, United States: 2011. Research methods in anthropology: Qualitative and quantitative approaches. [Google Scholar]
- Bobo L., Gilliam F.D. Race, sociopolitical participation, and black empowerment. American Political Science Review. 1990;84(2):377–393. [Google Scholar]
- Brancaccio, D., Long, K., (2018, April 9, 2018). “Millions of Americans are evicted every year -- and not just in big cities.” Retrieved July 26, 2018, from 〈https://www.marketplace.org/2018/04/09/economy/eviction-desmond-princeton-housing-crisis-rent〉.
- Braubach, M., Organization, W.H., (2011). Environmental burden of disease associated with inadequate housing: a method guide to the quantification of health effects of selected housing risks in the WHO European Region.
- Brown Calder V. The Cato Institute; 2017. Zoning, land-use planning, and housing affordability; pp. 1–16. [Google Scholar]
- Bye L., Ghirardelli A., Fontes A. Promoting health equity and population health: how Americans’ views differ. Health Affairs. 2016;35(11):1982–1990. doi: 10.1377/hlthaff.2016.0730. [DOI] [PubMed] [Google Scholar]
- California Department of Public Health (2013). California Health Interview Survey (CHIS).
- Chiland, E. (2018, April 26, 2018). “Costa Hawkins, California’s rent control law, explained.” Retrieved July 26, 2018, from 〈https://la.curbed.com/2018/1/12/16883276/rent-control-california-costa-hawkins-explained〉.
- Cho W.K.T., Gimpel J.G., Dyck J.J. Residential concentration, political socialization, and voter turnout. The Journal of Politics. 2006;68(1):156–167. [Google Scholar]
- Coley R.L., Leventhal T., Lynch A.D., Kull M. Relations between housing characteristics and the well-being of low-income children and adolescents. Developmental Psychology. 2013;49(9):1775. doi: 10.1037/a0031033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J.W. SAGE Publications; Thousand Oaks, California: 2014. Research design: qualitative, quantitative, and mixed methods approaches. [Google Scholar]
- Creswell J.W., Plano Clark V.L. SAGE Publications; Los Angeles: 2011. Designing and conducting mixed methods research. [Google Scholar]
- Davison G., Legacy C., Liu E., Darcy M. The factors driving the escalation of community opposition to affordable housing development. Urban Policy and Research. 2016;34(4):386–400. [Google Scholar]
- DeSante C.D., Perry B.N. Bridging the gap: How geographic context affects political knowledge among citizen and non-citizen latinos. American Politics Research. 2016;44(3):548–577. [Google Scholar]
- Desmond M., An W., Winkler R., Ferriss T. Evicting children. Social Forces. 2013;92(1):303–327. [Google Scholar]
- Desmond M., Kimbro R.T. Eviction’s fallout: Housing, hardship, and health. Social Forces. 2015;94(1):295–324. [Google Scholar]
- Downing J. The health effects of the foreclosure crisis and unaffordable housing: A systematic review and explanation of evidence. Social Science & Medicine. 2016;162:88–96. doi: 10.1016/j.socscimed.2016.06.014. [DOI] [PubMed] [Google Scholar]
- Enterprise Community Partners, I. (2017). “Why are people across the U.S. struggling to afford a decent place to call home?”, from 〈http://www.housinginsecurity.org/〉.
- Freeman L. America’s affordable housing crisis: A contract unfulfilled. American Journal of Public Health. 2002;92(5):709–712. doi: 10.2105/ajph.92.5.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuzawa D.D., Karnas F. Reconnecting health and housing: Philanthropy’s new opportunity. Environmental Justice. 2015;8(3):86–94. [Google Scholar]
- Fullilove M.T., Shock M.R. One World, Ballantine Books; New York: 2004. How tearing up city neighborhoods hurts America, and what we can do about it. [Google Scholar]
- Gibson M., Petticrew M., Bambra C., Sowden A.J., Wright K.E., Whitehead M. Housing and health inequalities: a synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health & place. 2011;17(1):175–184. doi: 10.1016/j.healthplace.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollust S.E., Barry C.L., Niederdeppe J. Americans’ opinions about policies to reduce consumption of sugar-sweetened beverages. Preventive Medicine. 2014;63:52–57. doi: 10.1016/j.ypmed.2014.03.002. [DOI] [PubMed] [Google Scholar]
- Gollust S.E., Lantz P.M., Ubel P.A. The polarizing effect of news media messages about the social determinants of health. American Journal of Public Health. 2009;99(12):2160–2167. doi: 10.2105/AJPH.2009.161414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath C., Heath D. Random House; New York, NY: 2008. Made to stick: Why some ideas survive and others die. [Google Scholar]
- Henwood B.F., Cabassa L.J., Craig C.M., Padgett D.K. Permanent supportive housing: addressing homelessness and health disparities? American Journal of Public Health. 2013;103(S2):S188–S192. doi: 10.2105/AJPH.2013.301490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchings V.L. Political context, issue salience, and selective attentiveness: Constituent knowledge of the Clarence Thomas confirmation vote. Journal of Politics. 2001;63(3):846–868. [Google Scholar]
- Kalugina A. Affordable housing policies: An overview. Cornell Real Estate Review. 2016;14(1):76–83. [Google Scholar]
- Kamel N. The actualization of neoliberal space and the loss of housing affordability in Santa Monica, California. Geoforum. 2012;43(3):453–463. [Google Scholar]
- Kavanagh A.M., Aitken Z., Baker E., LaMontagne A.D., Milner A., Bentley R. Housing tenure and affordability and mental health following disability acquisition in adulthood. Social science & medicine. 2016;151:225–232. doi: 10.1016/j.socscimed.2016.01.010. [DOI] [PubMed] [Google Scholar]
- Krieger J., Higgins D.L. Housing and health: Time again for public health action. American Journal of Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel M.B., Gupta R., Gee L., Haas J.S. Housing instability and food insecurity as barriers to health care among low‐income Americans. Journal of General Internal Medicine. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal T., Newman S. Housing and child development. Children and Youth Services Review. 2010;32(9):1165–1174. [Google Scholar]
- Lubell J., Crain R., Cohen R. Framing the issues—the positive impacts of affordable housing on health. Center for Housing Policy. 2007;34 [Google Scholar]
- Lundell H., Niederdeppe J., Clarke C. Public views about health causation, attributions of responsibility, and inequality. Journal of health communication. 2013;18(9):1116–1130. doi: 10.1080/10810730.2013.768724. [DOI] [PubMed] [Google Scholar]
- Manuel T., Kendall-Taylor N. Enterprise Community Partners, Inc. and the FrameWorks Institute; Washington, DC: 2016. You don’t have to live here”: Why housing messages are backfiring and 10 things we can do about it. [Google Scholar]
- Maqbool, N., Viveiros, J., Ault, M. (2015). The impacts of affordable housing on health: A research summary. Insights from Housing Policy Research. Center for Housing Policy, National Housing Conference: 1-12.
- Mason K.E., Baker E., Blakely T., Bentley R.J. Housing affordability and mental health: does the relationship differ for renters and home purchasers? Social Science & Medicine. 2013;94:91–97. doi: 10.1016/j.socscimed.2013.06.023. [DOI] [PubMed] [Google Scholar]
- McHugh M.L. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- Meltzer R., Schwartz A. Housing affordability and health: Evidence from New York City. Housing Policy Debate. 2016;26(1):80–104. [Google Scholar]
- Murray, C., Schuetz, J. (2018). Housing in the US is too expensive, too cheap, and just right. It depends on where you live., from 〈https://www.brookings.edu/research/housing-in-the-u-s-is-too-expensive-too-cheap-and-just-right-it-depends-on-where-you-live/〉.
- National Alliance to End Homelessness, (2018). The State of Homelessness in America. from 〈https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness-report/〉.
- National Law Center on Homelessness & Poverty . 2016. The 2016 human right to housing report card; pp. 1–40. [Google Scholar]
- National Rural Housing Coalition . National Rural Housing Coalition; 2018. Barriers to affordable rural housing.〈http://ruralhousingcoalition.org/overcoming-barriers-to-affordable-rural-housing/〉 [Google Scholar]
- Nguyen M.T., Basolo V., Tiwari A. Opposition to affordable housing in the USA: Debate framing and the responses of local actors. Housing, Theory and Society. 2013;30(2):107–130. [Google Scholar]
- Nino, J. (2017, November 7. 2017). “Zoning: The Nemesis of Housing Affordability.” Retrieved July 26, 2018, 2018, from 〈https://www.aier.org/article/zoning-nemesis-housing-affordability〉.
- Novoa A.M., Amat J., Malmusi D., Diaz F., Darnell M., Trilla C., Bosch J., Borrell C. Changes in health following housing improvement in a vulnerable population in Spain: A follow-up study. International Journal of Health Services. 2017;47(1):83–107. doi: 10.1177/0020731416676228. [DOI] [PubMed] [Google Scholar]
- Ortiz, S. E., Zimmerman, F. J., Gilliam, F. D. (2015). Weighing in: The taste-engineering frame in obesity expert discourse. American Journal of Public Health 105(3): 554-559. [DOI] [PMC free article] [PubMed]
- Parsons, V. L., Moriarity, C. L., Jonas, K., Moore, T. F., Davis, K. E., Tompkins, L. (2014). “Design and estimation for the national health interview survey, 2006-2015.” [PubMed]
- Pollack C.E., Griffin B.A., Lynch J. Housing affordability and health among homeowners and renters. American Journal of Preventive Medicine. 2010;39(6):515–521. doi: 10.1016/j.amepre.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Raphael D., Curry-Stevens A., Bryant T. Barriers to addressing the social determinants of health: Insights from the Canadian experience. Journal of Health Policy. 2008;88:222–235. doi: 10.1016/j.healthpol.2008.03.015. [DOI] [PubMed] [Google Scholar]
- Reeves R.V., Halikias D. Brookings; 2016. How land use regulations are zoning out low-income families.〈https://www.brookings.edu/blog/social-mobility-memos/2016/08/16/zoning-as-opportunity-hoarding/〉 [Google Scholar]
- Robert S.A., Booske B.C. US opinions on health determinants and social policy as health policy. American Journal of Public Health. 2011;101(9):1655–1663. doi: 10.2105/AJPH.2011.300217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert S.A., Booske B.C., Rigby E., Rohan A.M. Public views on determinants of health, interventions to improve health, and priorities for government. Wisconsin Medical Journal. 2008;107(3):124–130. [PubMed] [Google Scholar]
- RWJF, Carger E., Westen D. Robert Wood Johnson Foundation; Princeton, NJ: 2010. A new way to talk about the social determinants of health. [Google Scholar]
- Sandel, M., Cook, J., Poblacion, A., Sheward, R., Coleman, S. M., Vivieros, J., Sturtevant, L., (2016). Housing as a Health Care Investment: Affordable Housing Supports Children’s Health. Insights from Housing Policy Research, National Housing Conference and Children's HealthWatch.
- Sandel M., Sheward R., de Cuba S.E., Coleman S.M., Frank D.A., Chilton M., Black M., Heeren T., Pasquariello J., Casey P. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018:e20172199. doi: 10.1542/peds.2017-2199. [DOI] [PubMed] [Google Scholar]
- Serby M.J., Brody D., Amin S., Yanowitch P. Eviction as a risk factor for suicide. Psychiatric Services. 2006;57(2) doi: 10.1176/appi.ps.57.2.273-b. 273-b-274. [DOI] [PubMed] [Google Scholar]
- Shaw M. Housing and public health. Annual Review Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- Shiue I. Public perceptions of housing improvement and self-rated health: World values survey, 2005-2007. Housing, Care and Support. 2014;17(2):69–74. [Google Scholar]
- Solari C.D., Mare R.D. Housing crowding effects on children's wellbeing. Social Science Research. 2012;41(2):464–476. doi: 10.1016/j.ssresearch.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen, B. L., Carter, G. R. Martin, M., Pelletiere, D., Vandenbroucke, D. A., Yao, Y.-G. D., (2015). Worst Case Housing Needs: 2015 Report to Congress. O. o. P. D. a. R. U.S. Department of Housing and Urban Development. Washington, DC.
- Taylor, M., (2016). Perspectives on Helping Low-Income Californians Afford Housing. L. A. s. Office. Sacramento, CA.
- The Governor’s Press Office, (2017). Governor Cuomo Launches Landmark $20 Billion Plan to Combat Homelessness and Create Affordable Housing For All New Yorkers. New York, NY.
- Thornberg C. The San Deigo Union-Tribune; San Diego, California: 2016. Housing a middle-class crisis in California. [Google Scholar]
- U.S. Department of Housing and Urban Development . HUD USER; 2005. Why note in our community?”: Removing barriers to affordable housing. [Google Scholar]
- Wiener R.J., Barton S.E. The underpinnings of inclusionary housing in California: current practice and emerging market and legal challenges. Journal of Housing and the Built Environment. 2014;29(3):403–422. [Google Scholar]
- Wiley M., Powell J.A. Tearing Down Structural Racism and Rebuilding Communities. Clearinghouse. 2006;40(68) [Google Scholar]
- Woo A. How have rents changed since 1960? Apartment List Rentonomics. 2016 [Google Scholar]