Abstract
OBJECTIVE.
Long indwelling times for inferior vena cava (IVC) filters that are used to prevent venous thromboembolism can result in complications. To improve care for patients receiving retrievable IVC filters, we developed and evaluated an informatics-based initiative to facilitate patient tracking, clinical decision-making, and care coordination.
MATERIALS AND METHODS.
A semiautomated filter-tracking application was custom-built to query our radiology information system to extract and transfer key data elements related to IVC filter insertion procedures into a database. A web-based interface displayed key information and facilitated communication between the interventional radiology clinical team and referring physicians. A set of filter management options was provided depending on each patient’s clinical condition. The system was launched in April 2016. Using retrospective observational cohort methods, we compared filter retrieval rates during a test period from July through December 2016 with a control period of the same 6 months in 2015.
RESULTS.
System development required approximately 100 hours of development time. Two hundred ninety-three IVC filter placements and 83 filter retrievals were tracked during the study periods. The overall filter retrieval rate was 23% in the control period and 34% in the test period. Mean times from filter placement to retrieval in the control and test periods were not significantly different (88.9 and 102.7 days, respectively; p = 0.32).
CONCLUSION.
A semiautomated approach to tracking patients with IVC filters can facilitate care coordination and clinical decision-making for a device with known potential complications. Similar applications designed to improve provider communication and documentation of filter management plans, including appropriateness for retrieval, can be replicated.
Keywords: filter clinic, inferior vena cava (IVC) filter, retrievable filter, safety, U.S. Food and Drug Administration (FDA)
Inferior vena cava (IVC) filters are devices designed to prevent the potentially life-threatening migration of blood clots from the lower extremities into the pulmonary circulation. Although studies have shown that they are effective for the prevention of pulmonary embolism compared with anticoagulation therapy alone [1, 2], these devices are associated with a variety of complications including device migration, breakage, embolization, vascular injury, and venous thrombosis.
Although most modern IVC filters are retrievable, these devices are infrequently removed when the risk of pulmonary embolism subsides [3]. Long indwelling times in turn can increase the risk of complications or can limit the ability to remove filters. To address these concerns, the U. S. Food and Drug Administration (FDA) issued communications regarding the clinical care for patients receiving IVC filters and device safety. The safety communication released on May 6, 2014, stated the following:
The FDA recommends that implanting physicians and clinicians responsible for the ongoing care of patients with retrievable IVC filters consider removing the filter as soon as protection from pulmonary embolism is no longer needed.
To follow and manage patients with IVC filters, some groups have created dedicated IVC filter clinics [4]. After a review of our clinic need and workflow, we determined that a dedicated IVC filter clinic for scheduling all patients with filters for subsequent management discussions would in many cases use resources but leave clinical management unchanged. We therefore proposed an alternative initiative that uses informatics-based methods to track patients receiving IVC filters, with the goal of optimizing the value of physician-patient discussions in clinic. By designing a platform to facilitate physician communication before scheduling clinic visits, we intended to identify which patients could benefit from face-to-face discussion regarding a filter retrieval procedure or an ongoing need for filtration. Patients with changes in clinical status warranting permanent venous filtration or patients whose risks of filter retrieval outweighed the risk of attempting removal were not required to schedule a clinic visit with interventional radiology (IR) unless requested.
In this article, we describe a system and workflow devised to enhance communication between physicians, track and manage timetables for IVC filter clinical reassessment, and improve documentation and data collection for filter-related events. We also describe the impact of the IVC filter–tracking system on filter retrieval rate and timing with respect to a control period before implementation of the system.
Materials and Methods
The retrospective data review and analysis for this study were approved with a waiver of informed consent by our institutional review board.
Clinical Needs and Workflow Assessment
Before the development of a filter-tracking system, representatives from the IR clinical service, radiology nursing, and informatics teams at our institution examined clinical needs and existing workflows. Based on this needs assessment, a new workflow (Fig. 1) was proposed with the following tenets: First, the system should be able to automatically record the date of every IVC filter placement and retrieval within the institution. Second, the system should track expected reassessment dates after IVC filter placement. Third, the system should facilitate communication between IR providers and the patient’s referring or current care provider for reassessment. Fourth, the system should support decision-making with sufficient flexibility to account for clinical uncertainty. The options to remove the filter, maintain the filter permanently, or reassess after a specified time interval should be provided.
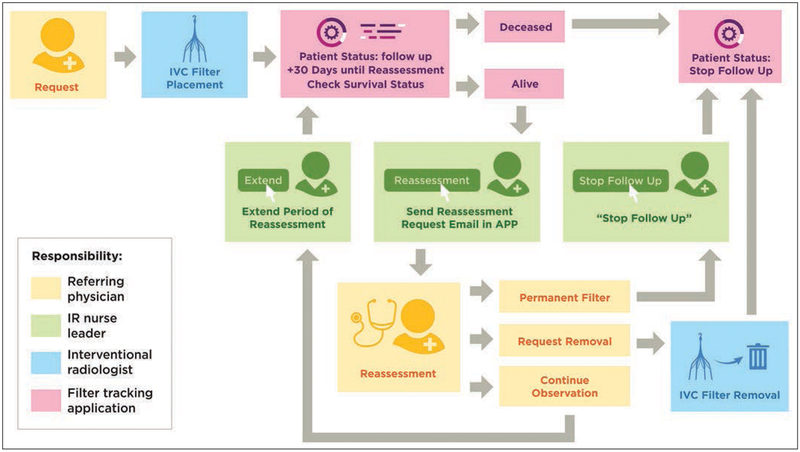
Fig. 1—
Overall workflow for inferior vena cava (IVC) filter tracking. After IVC filter placement, tracking application (APP) obtains key data elements from radiology information system. Application helps interventional radiology (IR) nurse leader to manage reassessment times and communicate with referring physicians until decision has been made to keep filter in place permanently or to retrieve filter. (Used with permission: © 2018, Memorial Sloan Kettering Cancer Center)
Inferior Vena Cava Filter–Tracking Initiative
An outpatient IR clinic nurse was selected to coordinate the IVC filter–tracking system oversight, education, and communication. Working with the IR physicians who performed filter insertion procedures, this nurse leader directed the day-to-day operations of the tracking system, including routing of communications, monitoring of filter reassessment dates, and updating the electronic medical record (EMR) documentation accordingly.
Filter-Tracking System Architecture
We created an IVC filter–tracking system with the following components: an application that queries the radiology information system (RIS), a database, and a web-based user interface. All components of the system reside inside a firewall within the hospital network. These components are described in the following sections.
Application That Queries the Radiology Information System
The back-end of the application was developed using C# (version 5.0, Microsoft) with ASP.NET model-view-controller framework (version 4.5.1, Microsoft) for web applications. The front-end was developed using HTML5 (World Wide Web Consortium), CSS3 (World Wide Web Consortium), and JavaScript (Netscape Communications [jQuery, jQuery Team]). This combination of tools is easy to implement at low cost for a project of this relatively small size. The application was installed on a server running Windows Server 2012 R2 (Microsoft) with a Xeon processor (CPU E5-2680 v2 at 2.80GHz, Intel) and 8 GB of random access memory.
Referring physicians request radiology procedures through electronic order entry applications within the institution’s EMR. All radiology procedures, whether diagnostic or interventional, are subsequently managed within the department’s RIS (Imagecast, version 10.8, GE Healthcare), which draws information from the institution’s EMR. Our application performs direct queries of the RIS database every hour to extract eight key information elements (Table 1) including patient identifiers, referring physician name, procedure name, accession number, and procedure date. IVC filter placements and retrievals are identified using two unique RIS procedure names: “IR IVC filter” and “IR IVC filter removal.” After an IR physician has performed either a filter placement or retrieval procedure and generates a procedure report, the RIS automatically records the completion date and name of the IR physician. A final data element queried by our application is the patient’s survival status (i.e., alive or deceased).
TABLE 1:
Data Elements Available in the Radiology Information System Used for Inferior Vena Cava Filter–Tracking Project
| Data Element No. | Definition |
|---|---|
| 1 | Patient identifiers (name, MRN) |
| 2 | Name of referring physician |
| 3 | Procedure name (filter placement or filter removal) |
| 4 | Procedure accession number |
| 5 | Procedure schedule date |
| 6 | Procedure completion date |
| 7 | Name of interventional radiologist |
| 8 | Patient survival status (alive or deceased) |
Note—MRN = medical record number.
The application records every IVC filter placement and retrieval procedure, which fulfills clinical needs assessment item 1. In addition, the application adds 30 calendar days to the date of the procedure, recording this date into another database field titled “Reassessment Date,” which fulfills clinical needs assessment item 2. A final field in the database, Follow-Up Status, is automatically set to “Follow-up” after IVC filter placement. If a patient’s vital status changes to deceased or if the application detects a completed IVC filter retrieval procedure, the application changes the value of the Follow-Up Status field to “Stop follow-up.” Vital status within the RIS is determined by several connected systems, including the institution’s patient registration system and the Social Security Death Index. Additionally, at the time of the 30-day follow-up, a referring physician can notify the IR clinic nurse if a patient has died.
Database
We used an SQL Server (version 2008 R2, Microsoft) database as part of our filter-tracking system because it was readily available through an institutional site license. Free open-source alternatives that would be equally effective for this kind of application include PostgreSQL (PostgreSQL Global Development Group) and MySQL Community Edition (Oracle).
Web-Based Patient Management Interface and Communication Tools
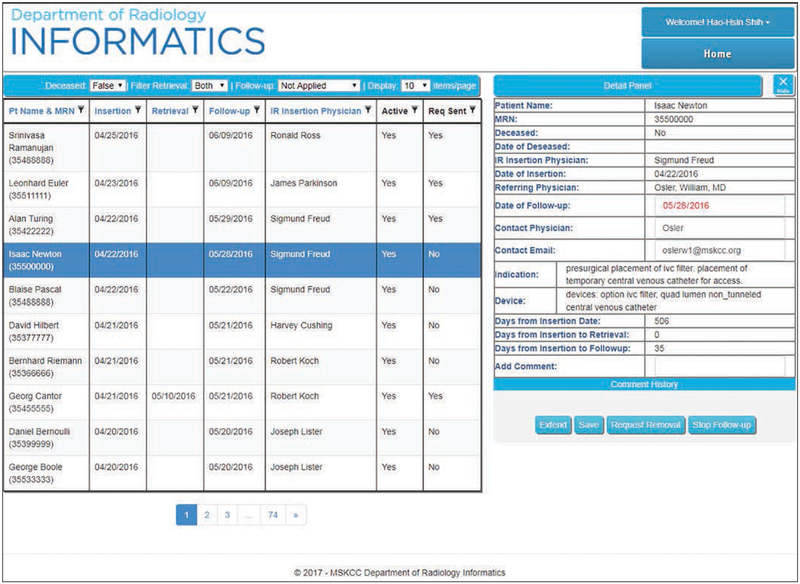
A web-based user interface allows project team members to access project information from the database, after authentication, from any web-browser within the hospital network. The eight key elements described as well as the reassessment date, survival status, and follow-up status are available for review and sorting. After sorting by reassessment date, users can readily determine the next patient due for review. A screen shot of the user interface is shown in Figure 2.
Fig. 2—
Screen shot of inferior vena cava (IVC) filter–tracking application user interface (anonymized). Table on left shows patient identifiers and dates of filter insertion. Also shown are dates of filter retrieval if available (either scheduled or completed), dates of follow-up, filter activity (“Yes” if filter is being actively followed), and request sent (“Yes” if e-mail was sent to referring physician for reassessment). Right panel provides additional details and communications. Screen shot was obtained on approximately May 9, 2016. Patient Isaac Newton had filter placed on April 22, 2016, and is scheduled for reassessment on May 28, 2016. No request for reassessment on Isaac Newton’s filter has been sent. Patient Georg Cantor had filter placed on April 21, 2016, and is scheduled for reassessment on May 21, 2016. However, filter retrieval is scheduled for May 10, 2016. Because filter retrieval is scheduled but not yet completed, tracking status remains “Active: Yes.” When retrieval is completed, application will automatically change tracking status to “Active: No.” Pt = patient, MRN = medical record number, IR = interventional radiology, Reg = request. (Used with permission: © 2017, Department of Radiology Informatics, Memorial Sloan Kettering Cancer Center [MSKCC])
To facilitate communication among health care providers and fulfill clinical needs assessment items 3 and 4, integrated in our filter-tracking application is a tool that generates an e-mail to the referring physician, prepopulated with the individual patient’s information and a request to reassess the ongoing need for the IVC filter. The referring physician is asked to reply to the e-mail by selecting one of three options: “IR referral for IVC filter removal to be placed”; “filter to remain in place permanently”; or “removal indication not clear at this time; reconsider in 1 month.” The IR nurse documents all responses from referring physicians within the filter-tracking web-based user interface as well as in an “electronic communication” document type in the EMR. Further actions are determined by the nature of the physician’s response.
When filter removal is desired and scheduled, the system monitors the RIS for an electronic order for “IR IVC filter removal.” An IR clinic visit is scheduled to discuss the procedure and clinical rationale with the patient. If IVF filter removal is scheduled, the removal procedure date and time are stored in the system database and displayed in the web-based interface, including updates for rescheduled or cancelled procedures. For patients requiring permanent IVC filtration, a “Stop follow-up” interface button can be selected and the patient is removed from the active follow-up list.
When the referring physician replies by selecting the option to reconsider the patient’s clinical status in 1 month, an application button titled “Extend follow-up” automatically adds an additional 30 days to the “Reassessment Date” field in the database. In most “Stop follow-up”or “Extend follow-up” cases, an IR clinic visit is not scheduled, but an exchange of information between the referring clinician and ongoing care provider regarding IVC filter management is encouraged. However, if there is a communication that indicates that a discussion of the potential risks and benefits of IVC filter removal with an IR physician is either requested by the patient or considered by the referring clinician to provide value to the patient, a face-to-face visit with an IR physician in clinic is also scheduled.
For patients designated for extended followup, when the next reassessment date is reached, an e-mail communication is again automatically initiated. The process repeats until the filter is removed, the patient is determined to have an indication for a permanent filter, or the patient dies. The time frame between communications, when the clinical prognosis is unknown, can be modified using the web-based interface based on feedback from the referring provider.
Deployment and Statistical Analysis
The filter-tracking application was launched in April 2016 for testing. At that time, we began collecting retrospective data for all IVC filters placed from July 2015 and later. Active intervention through the application—namely, identification of patients who were due for reassessment and e-mails to referring physicians through the application—was initiated for filters placed after April 2016.
The impact of our filter-tracking system on filter retrieval rates was evaluated relative to a control period of 6 months from July 1, 2015, to December 31, 2015. During that time, the filter-tracking application captured data from IVC filter placement and retrieval procedures, but there was no active intervention using integrated tracking or communication tools. During a 6-month test period from July 1, 2016, to December 31, 2016, the application was used to track filter placements and retrievals and to contact referring physicians for clinical reassessment at 30-day intervals.
For the analysis in this study data were downloaded from the application on July 30, 2017. Therefore, an IVC filter placed on December 31, 2016, the last day of the test period, had a maximum opportunity for reassessment of 210 days. Filters placed before December 31, 2016, however, would have had a longer opportunity for reassessment. To enable an unbiased comparison of filter retrieval rates and address potential lead time bias, all filters were stratified into two groups: filter retrieved less than 210 days from insertion and filter not retrieved or retrieved 210 days or more from insertion. Summary statistics were calculated (Excel 2007, Microsoft), and mean filter retrieval times were compared between the control and test periods using an unpaired t test (GraphPad, GraphPad software). Statistical significance was defined as p < 0.05.
Results
System development required approximately 100 hours of developer time. The application successfully tracked 100% of IVC filter placements and retrievals during the test and control periods. Two hundred ninety-three IVC filter placements were captured; 142 were placed in the control period, and 151 were placed in the test period. Eighty-three IVC filter retrievals were captured: 32 retrieved in the control period and 51 retrieved in the test period. The overall filter retrieval rate was 23% (32/142) in the control period and 34% (51/151) in the test period. Summary statistics are shown in Tables 2 and 3.
TABLE 2:
Comparison of Inferior Vena Cava (IVC) Filters Placed and Retrieved During Control and Trial Periods
| IVC Filters | Control Period | Test Period | p |
|---|---|---|---|
| Retrieved < 210 d from insertion | |||
| No. of filters placed and retrieved | 24 | 43 | |
| Mean no. of days from insertion to retrieval | 88.9 | 102.7 | 0.32 |
| Maximum no. of days from insertion to retrieval | 203 | 204 | |
| Minimum no. of days from insertion to retrieval | 16 | 15 | |
| Retrieved ≥ 210 d from insertion | |||
| Filters placed and retrieved | 8 | 8 | |
| Mean no. of days from insertion to retrieval | 368.8 | 242.5 | 0.03 |
| Maximum no. of days from insertion to retrieval | 702 | 319 | |
| Minimum no. of days from insertion to retrieval | 218 | 213 | |
| Not retrieved | |||
| Deceased | 81 | 60 | |
| Reassessment: permanent filter (stop follow-up) | 26 | ||
| Reassessment: continue observation | 14 | ||
| Not followed | 29 | ||
| Total no. of filters placed | 142 | 151 | |
| Total no. of filters retrieved | 32 | 51 | |
| Mean no. of days from insertion to retrieval | 158.8 | 124.6 | 0.17 |
TABLE 3:
Patient Survival Status as of July 30, 2017
| Inferior Vena Cava Filter | Control Period | Test Period | ||||
|---|---|---|---|---|---|---|
| Alive | Deceased | Subtotal | Alive | Deceased | Subtotal | |
| Filters placed and retrieved | 28 | 4 | 32 | 49 | 2 | 51 |
| Filters placed and not retrieved | ||||||
| Follow-up | 14 | 14 | ||||
| Stop follow-up | 26 | 60 | 86 | |||
| Not followed | 29 | 81 | 110 | |||
| Total | 57 | 85 | 142 | 89 | 62 | 151 |
Note—Data are reported as numbers of patients.
When comparing retrieval rates stratified by duration of filter implantation, 24 filters inserted during the control period and 43 inserted during the test period were retrieved less than 210 days from the date of insertion. Within this population of filters retrieved less than 210 days from insertion, filter retrieval rates were 17% (24/142) and 28% (43/151) in the control and test periods, respectively. The mean times from filter placement to retrieval in the control and test periods were not significantly different (88.9 and 102.7 days, respectively; p = 0.32).
Of the 118 (i.e., 142 – 24) filters placed in the control period that were not retrieved within 210 days, eight (7%) filters were retrieved at a later time. Of the remaining 110 (i.e., 118 – 8) patients, the application found that 81 (74%) patients had died. The remaining 29 (i.e., 110 – 81) patients were not being systematically followed by definition of the control period.
Of the 108 (i.e., 151 – 43) filters placed in the test period that were not retrieved within 210 days from insertion, eight (7%) were retrieved at a later time. Of the remaining 100 (i.e., 108 – 8) patients, the application found that 60 (60%) patients had subsequently died and automatically changed the status to “Stop follow-up.” Of the remaining 40 (i.e., 100 – 60) patients, referring physicians provided notification to the IR clinic nurses that 26 filters should remain in place permanently. The remaining 14 (i.e., 40 – 26) filters placed in the test period continued to be followed in 30-day intervals.
Of the 16 filters retrieved 210 days or more from insertion in the control (n = 8 filters) and test (n = 8 filters) periods, the mean times from placement to retrieval were 368.8 and 242.5 days, respectively (p = 0.03). The expected statistically significant difference in these times is due to lead time bias, as discussed in the Materials and Methods section, and justifies the stratification of filter retrieval duration using a 210-day threshold.
Discussion
Longitudinal clinical care is an essential component of the modern practice of IR. To facilitate clinical decision-making and long-term follow-up for patients with retrievable IVC filters, we designed and deployed a system to track filter placement and retrieval procedures. Our main objectives were to automatically capture all relevant patients in the system, standardize postprocedural provider communication, and document filter-related care plans within the EMR. Before implementation of this system, patients who received retrievable IVC filters were not systematically followed, routine communication between referring providers and interventional radiologists related to filter management was uncommon, and complications related to long-term filter indwelling times were encountered. After FDA safety announcements highlighting the need for improved care coordination with respect to the ongoing mechanical venous filtration, we sought solutions that would address clinical needs and responsibilities without creating undue administrative burden.
An alternative to our informatics-based approach to patient tracking is a dedicated IVC filter clinic, as described by Minocha et al. [4]. In that study, a clinical nurse coordinator updated a prospective IVC filter spreadsheet after every IVC filter placement at their institution. An interventional radiologist contacted referring physicians approximately 2–3 weeks after filter placement to discuss clinical management. These communications were repeated in regular intervals until filter removal or until a decision to leave the filter permanently. In that study, only 15 of 100 patients attended a clinic appointment before retrieval because study investigators opted to address most clinical reassessments via telephone communication with other care providers. We share a similar opinion that many reassessments can be performed through direct communication with the referring physicians. Furthermore, we believe in the importance of face-to-face discussions between IR physicians and patients when appropriate to answer questions, explain clinical recommendations, and obtain procedural consent. Our tracking system was able to improve clinic visit scheduling workflows, achieving increased efficiency by avoiding unnecessary visits and enhancing the value of patient discussions by focusing on patients for whom changes in filter management plans were considered appropriate.
Other studies have taken similar approaches. In three studies, Klinken et al. [5], Inagaki et al. [6], and Lynch [7] describe prospectively tracking patients who received IVC filters in a database. In all of these studies, an IR team assumed responsibility for follow-up of patients, and Inagaki et al. described the creation of a multidisciplinary task force. Although each study reported improved retrieval rates in the patients who were tracked, the authors did not discuss limitations imposed by manual data entry or the efforts involved in collecting and curating these data. These approaches become less sustainable over the long term as the work of information gathering and record maintenance increases.
The application described in our study can both complement and enhance these previously described methods. The process of tracking filter placements and retrievals in this study was semiautomated. Filter tracking with all the necessary data elements began automatically the moment the placement was recorded in the RIS, limiting the potential for loss to follow-up due to human error. Our system requirements included tracking of reassessment dates, facilitating communication between health care teams, and providing a clear set of filter reassessment categories for documentation. Also key to the success of this initiative was an IR nurse leader who coordinated application use and served as an educator for outpatient nurses using the application to track filters and communicate with referring physicians.
Successful operation of the filter-tracking system depends on several factors. First, there must be an accurate, reliable source of information. We identified eight key data elements required to support the workflow. These queries were performed on a copy of the primary (production) RIS database that we maintain as a disaster-recovery platform. Our intent was to avoid overloading the production database with queries that could affect performance. This solution worked well in our environment; however, for other institutions that may not have query access to the RIS database, an equally viable alternative would be to use a Health Level 7 interface engine that records events sent out by the RIS. Free, open-source solutions exist, such as Mirth Connect (Mirth Corporation), that have been used in other large-scale health care data integration projects [8].
As in a prior study [9], we show how a relatively low-cost set of components can be used to create a clinically meaningful tool in a large, multifacility academic medical center. Developed by our radiology informatics team, this tool was composed of an application that queried our RIS, a database, and a web-based user interface. Total development time was approximately 100 hours. Assuming an industry rate of $100 per hour, the development cost can be estimated to be $10,000. Additional infrastructure costs are low. Because of low computational demands, the tool can be run on most modern, low-end computing platforms costing less than $2000. We know of no other similar, commercially available tools on the market.
There are some limitations to the tools and workflows established in this study. As in many institutions, our patients receive care from teams of physicians and other health care providers, and the physician who placed the referral for an IVC filter placement might not be the one to make the final decision regarding retrieval. The IR care teams found that they were directed in many instances after contacting the referring physician to another health care provider for the filter reassessment determination. For instance, the inpatient physician who requested an IVC filter placement during an acute phase of a patient’s illness would defer a filter reassessment to the judgment of the outpatient physician managing the patient’s long-term care. These redirects from one health care provider to another cause delays in appropriate care and waste the time of multiple providers. Challenges in communication within multidisciplinary health care teams have been described [10]. There is a need in the health care industry for solutions that comprehensively document various members of a patient’s health care team to help streamline communications between team members. At our institution, a new hospitalwide clinical guideline to reinforce the need to assume responsibility for IVC filter management was instituted on the basis of the findings from this tracking initiative.
A second limitation is that, at this time, the system is effective for only tracking filters placed within our institution, because it is the presence of a filter placement order within our RIS that initiates the tracking workflow. Patients referred to us after filter placement at an outside institution are not automatically tracked. There is a need in the health care industry for solutions that effectively document implantable devices within the health record. Methods for generating automated problem lists have been described, but specific strategies to document implantable devices are lacking [11]. If all implantable devices within a patient could be recorded in a machine-queryable format at the time of initial consultation, then this record could be used to initiate IVC filter tracking regardless of which institution or provider placed the filter. Additionally, informatics-based solutions such as this one could be extended to track other removable medical devices.
Conclusion
We describe a semiautomated approach to IVC filter tracking to improve clinical care for patients receiving retrievable IVC filters and to comply with FDA safety communications. During the test period, the application reliably and consistently tracked all IVC filter placements within our institution, facilitated communication between the IR service and referring physicians, and was associated with a trend toward increased filter retrieval rates over a short-term evaluation period.
Acknowledgments
We thank Joanne Chin for valuable assistance in the preparation and submission of this manuscript. We thank Wenjing Wu for creating the illustration in Figure 1.
Supported in part through an NIH/NCI Cancer Center support grant (P30 CA008748).
Footnotes
WEB
This is a web exclusive article, AJR 2018; 211:W178–W184, 0361–803X/18/2113–W178
References
- 1.Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med 1998; 338:409–415 [DOI] [PubMed] [Google Scholar]
- 2.PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 2005; 112:416–422 [DOI] [PubMed] [Google Scholar]
- 3.Duszak R, Parker L, Levin DC, Rao VM. Placement and removal of inferior vena cava filters: national trends in the medicare population. J Am Coll Radiol 2011; 8:483–489 [DOI] [PubMed] [Google Scholar]
- 4.Minocha J, Idakoji I, Riaz A, et al. Improving inferior vena cava filter retrieval rates: impact of a dedicated inferior vena cava filter clinic. J Vasc Interv Radiol 2010; 21:1847–1851 [DOI] [PubMed] [Google Scholar]
- 5.Klinken S, Humphries C, Ferguson J. Establishment of an inferior vena cava filter database and interventional radiology led follow-up: retrieval rates and patients lost to follow-up. J Med Imaging Radial Oncol 2017; 61:630–635 [DOI] [PubMed] [Google Scholar]
- 6.Inagaki E, Farber A, Eslami MH, et al. Improving the retrieval rate of inferior vena cava filters with a multidisciplinary team approach. J Vasc Surg Venous Lymphat Disord 2016; 4:276–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch FC. A method for following patients with retrievable inferior vena cava filters: results and lessons learned from the first 1,100 patients. J Vasc Interv Radiol 2011; 22:1507–1512 [DOI] [PubMed] [Google Scholar]
- 8.Rea S, Pathak J, Savova G, et al. Building a robust, scalable and standards-driven infrastructure for secondary use of EHR data: the SHARPn project. J Biomed Inform 2012; 45:763–771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong L, Elnajjar P, Nyman CG, Mair T, Juluru K. Implementation of a point-of-care radiologist-technologist communication tool in a quality assurance program. A JR 2017; 209: [web]W18–W25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr 2010; 2010:72–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bui AAT, Taira RK, El-Saden S, Dordoni A, Aberle DR. Automated medical problem list generation: towards a patient timeline. Stud Health Technol Inform 2004; 107:587–591 [PubMed] [Google Scholar]