Abstract
Gastro-esophageal varices (GEV) and variceal hemorrhage (VH) are clinical milestones in the natural history of cirrhosis, as they are closely related to the severity of portal hypertension and define specific stages in disease progression. Variceal hemorrhage is a life-threatening complication of cirrhosis and is one of the clinical complications that defines cirrhosis decompensation. The goal of screening and surveillance of varices is to identify patients with GEV at a high risk of bleeding, so that prevention strategies can be implemented. There have been significant updates in the management of GEV over the last years, particularly in the use of non-invasive methods to assess the degree of portal hypertension and the likelihood of having GEV. This paper is focused on esophageal varices with or without extension along the lesser curvature (type 1 or GOV1), as special considerations are required for the management of cardiofundal varices (GOV2 - esophageal varices extending into the fundus, or IGV1 - isolated gastric varices in the fundus) or isolated gastric varices type 2 (IGV2 – gastric varices elsewhere in the stomach, not in the fundus).
The clinical problem: who and how to evaluate for gastroesophageal varices
For the practicing clinician, the management of GEV starts with making the diagnosis of cirrhosis and determining its clinical stage (1,2). Cirrhosis should be suspected in any patient with chronic abnormalities in liver enzymes and/or known risk factors. The diagnosis should be based on clinical, laboratory, imaging and elastographic findings, and may require performance of a liver biopsy. Cirrhosis has two main stages: compensated and decompensated, with distinct presentation and prognosis (3). The compensated stage is asymptomatic, with a median survival of more than 12 years and it is at this stage where the diagnosis is difficult and requires a high index of suspicion (2,3). The decompensated stage includes patients who have obvious clinical complications of cirrhosis such as variceal hemorrhage (VH), ascites and/or hepatic encephalopathy, with a median survival of less than 2 years (2,3). If using Child-Turcotte-Pugh (CTP) classification, patients in CTP-A class are compensated, and those in CTP-B/C class are mostly decompensated.
Screening endoscopy is recommended in patients with cirrhosis to determine if they have varices at high risk of bleeding which will require treatment with either non-selective betablockers (NSBB) or endoscopic variceal ligation (EVL) in order to prevent VH, in accordance with the most recent American Association for the Study of Liver Diseases guidance (2). The risk of first VH is 5–15% per year, highest in patients with large varices, severe liver disease (Child class B/C), or with varices having endoscopic red wale marks (areas of thinning of the variceal wall). Variceal bleeding is associated with high mortality, especially if other decompensating events are present: 80% 5-year mortality versus 20% 5-year mortality if VH is the only complication of cirrhosis (3).
Screening and surveillance of varices in compensated cirrhosis
Non-invasive methods are increasingly used in clinical practice instead of liver biopsy to diagnose cirrhosis. As GEV can occur in patients with severe fibrosis and not only in patients with established cirrhosis, Baveno VI Consensus proposed the term of compensated advanced chronic liver disease (cACLD) to include patients with either severe fibrosis or compensated cirrhosis, at risk to develop GEV. Two separate measurements of liver stiffness (LS) by transient elastography (TE) of 15 kPa or more are highly suggestive of cACLD (1). The terms cACLD and compensated cirrhosis can be used interchangeably.
In compensated cirrhosis, the prevalence of any GEV is 30%– 40%, and only a minority (10%–20%) have high-risk varices (HRV) requiring treatment (4). These are medium or large varices or small varices with red wale marks, associated with an approximately 15% risk of bleeding per year. Patients with compensated cirrhosis and without clinically significant portal hypertension (CSPH) are at a very low risk of having or developing varices in the next 5 years. GEV usually occur once patients develop (CSPH), and patients with CSPH not only have a higher risk of developing varices but also have a higher risk of decompensation (5). The presence or absence of CSPH is determined by measuring the hepatic venous pressure gradient (HVPG) through transjugular hepatic vein catheterization, and is very useful in research but is impractical in routine clinical care. Non-invasive tests such as imaging showing porto-systemic collaterals or recanalized umbilical vein or reversal of portal flow, liver stiffness measurement, platelet count and spleen diameter can help identify patients with high risk of CSPH. More importantly, patients with very low risk of having HRV can also be identified non-invasively (6), although most data comes from patients with cirrhosis secondary to chronic hepatitis C. LS by TE of less than 20 kPa and platelet count higher than 150,000/mL (Baveno VI criteria) is associated with <5% chance of finding HRV, and endoscopy can be avoided in 30% of cACLD patients (1). Other cutoffs have been proposed, including a score that includes platelet count and MELD (without need for TE), but they require further validation (7).
Therefore, while screening endoscopy for varices is recommended in all patients with compensated cirrhosis, the use of non-invasive tools such as transient elastography has significantly changed clinical practice allowing an individualized approach: it expands the population at risk to include patients without established cirrhosis but with cACLD (LS>15 kPa), and identifies the highest risk patients – those with CSPH (imaging findings of portal hypertension and/or LS > 20–25 kPa) who absolutely need screening endoscopy, and the lowest risk patients – those with <5% of having HRV and who can avoid screening endoscopy (6).
The interval of surveillance endoscopy in compensated cirrhosis depends on specific factors associated with a higher risk of progression of portal hypertension: ongoing liver injury (untreated viral hepatitis, presence of other cofactors for liver injury i.e. obesity, alcohol), if small varices were found on endoscopy, or if clinical progression to decompensated cirrhosis.
Surveillance endoscopy to detect HRV in patients with compensated cirrhosis is recommended every 1–3 years, or when decompensation occurs. For compensated patients with ongoing liver injury, surveillance endoscopy should be repeated in 2 years if there were no varices at screening endoscopy, or in 1 year if small varices were found at screening endoscopy. In patients with inactive liver disease such as post hepatitis C eradication or if alcohol abstinence, endoscopy should be repeated in 3 years if there were no varices at screening endoscopy, or in 2 years if small varices were found at screening endoscopy. Importantly, once HRV are found and variceal bleeding prevention strategies are in place, there is no need for further surveillance endoscopy.
Screening and surveillance of varices in decompensated cirrhosis
As all patients with decompensated cirrhosis have CSPH, screening endoscopy is recommended at the time of diagnosis in all of them. GEV are present in the vast majority of patients (85%), and their management and prognosis depend on the presence/severity of other decompensating events (2,4). For decompensated patients, surveillance endoscopy is recommended every year. HRV requiring treatment to prevent VH include medium/large varices or small varices with red wale marks or small varices in CPT-C class patients (2). NSBB regimens used to prevent VH in decompensated patients with HRV will need adjustment if there is ascites. EVL is performed in patients with large varices who cannot tolerate NSBB (2).
Surveillance endoscopy post variceal hemorrhage
In patients who have bled from varices, the 1-year risk of recurrent VH can be as high as 60% in the absence of secondary prophylaxis. The recommended treatment to prevent recurrent hemorrhage consists of the combination of NSBB (used indefinitely) plus EVL every 2–6 weeks until varices are eradicated, followed by surveillance endoscopy at 3–6 months post variceal eradication, and every 6–12 months indefinitely (2). The key element of combination therapy is the NSBB particularly in decompensated patients (8). Patients who had a transjugular intrahepatic portosystemic shunt placed during the episode of acute VH should not receive NSBB or EVL as the shunt resolves portal hypertension and varices.
Special considerations regarding gastric varices
For patients in whom gastric varices are an extension of esophageal varices below the cardia into the lesser curvature (type 1 or GOV1), the management is as described above. Special considerations are required for other types of gastric varices, namely cardiofundal varices (which are gastric varices in the fundus, either as an extension of esophageal varices - GOV2, or isolated gastric varices type 1 - IGV1) or isolated gastric varices type 2 (varices in the stomach, but not in the fundus). Given lack of strong evidence to support a specific therapy for primary or secondary prophylaxis of VH in these patients, there are no firm recommendations (2). For primary prophylaxis of VH from GOV2 or IGV1, NSBB can be used, with the caveat that current data in the literature is limited (2). For secondary prophylaxis of VH from GOV2 or IGV1, TIPS or BRTO (Balloon Occluded Retrograde Transvenous Obliteration) or cyanoacrylate glue injection can be considered, depending on patient’s anatomy and local expertise, with insufficient data to choose one strategy versus others (2).
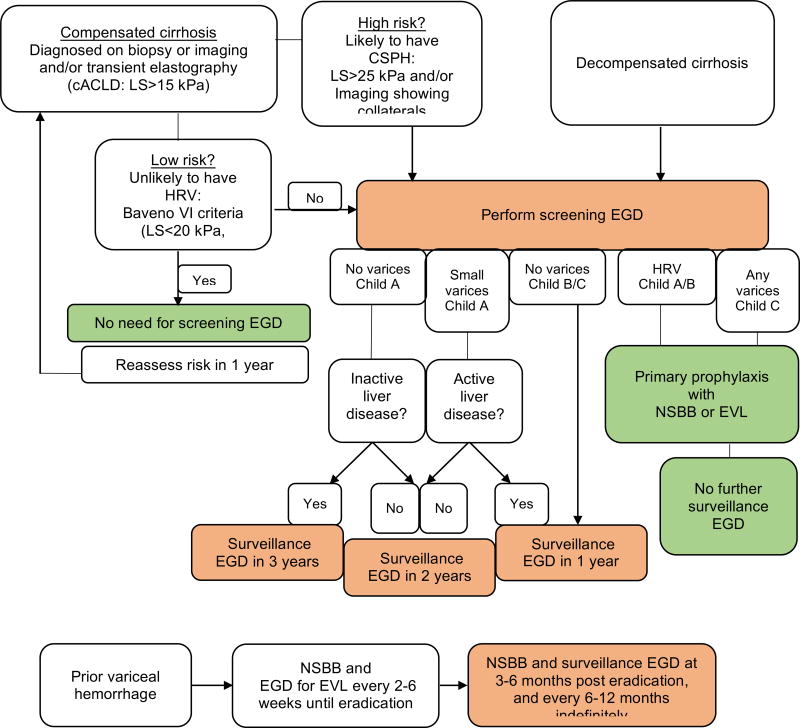
Figure 1.
Screening and surveillance of varices in patients with cirrhosis. cACLD, compensated advanced chronic liver disease; LS, liver stiffness; plts, platelet count (103/mL); CSPH, clinically significant portal hypertension; EGD, esophagogastroduodenoscopy; HRV, high-risk varices; NSBB, non-selective beta-blockers; EVL, endoscopic variceal ligation.
Take-home messages (Figure 1).
Screening endoscopy for gastroesophageal varices is indicated in select patients with cirrhosis to identify varices at a high-risk of variceal hemorrhage (HRV).
Patients with very low probability of having HRV can be identified non-invasively and endoscopy can be avoided in 20–30%.
Once HRV are identified by endoscopy, appropriate treatment to prevent VH (NSBB or EVL) should be initiated, and repeat endoscopic surveillance will no longer be necessary.
Intervals for endoscopic surveillance depend on stage (compensated vs decompensated), ongoing liver injury, and if small varices were found on prior endoscopy. In general, endoscopy should be repeated every 1–3 years in compensated patients, every year in decompensated patients.
Endoscopic surveillance in addition to NSBB is indicated for all patients who had variceal bleeding, with the exception of patients with functional TIPS.
Acknowledgments
Funding support: Yale Liver Center (NIH P30 DK34989)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No relevant conflicts of interest
References
- 1.Franchis R Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743–752. doi: 10.1016/j.jhep.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017 Jan;65(1):310–335. doi: 10.1002/hep.28906. [DOI] [PubMed] [Google Scholar]
- 3.D’Amico G, Pasta L, Morabito A, et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther. 2014;39:1180–1193. doi: 10.1111/apt.12721. [DOI] [PubMed] [Google Scholar]
- 4.Kovalak M, Lake J, Mattek N, et al. Endoscopic screening for varices in cirrhotic patients: data from a national endoscopic database. Gastrointest Endosc. 2007;65:82–88. doi: 10.1016/j.gie.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Tsao G, Groszmann RJ, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005 Nov 24;353(21):2254–61. doi: 10.1056/NEJMoa044456. [DOI] [PubMed] [Google Scholar]
- 6.Abraldes JG, Bureau C, Stefanescu H, et al. Noninvasive Tools and Risk of Clinically Significant Portal Hypertension and Varices in Compensated Cirrhosis: The “Anticipate” Study. Hepatology. 2016;64:2173–2184. doi: 10.1002/hep.28824. [DOI] [PubMed] [Google Scholar]
- 7.Jangouk P, Turco L, De Oliveira A, et al. Validating, deconstructing and refining Baveno criteria for ruling out high-risk varices in patients with compensated cirrhosis. Liver Int. 2017 Aug;37(8):1177–1183. doi: 10.1111/liv.13379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albillos A, Zamora J, Martínez J, et al. Stratifying risk in the prevention of recurrent variceal hemorrhage: Results of an individual patient meta-analysis. Hepatology. 2017 Oct;66(4):1219–1231. doi: 10.1002/hep.29267. [DOI] [PMC free article] [PubMed] [Google Scholar]