Abstract
Background
Sapovirus (SV) infection is a public health concern which plays an important role in the burden of diarrhoeal diseases, causing acute gastroenteritis in people of all ages in both outbreaks and sporadic cases worldwide.
Objective/Study Design
The purpose of this report is to summarise the available data on the detection of human SV in low and middle income countries. A systematic search on PubMed and ScienceDirect database for SV studies published between 2004 and 2017 in low and middle income countries was done. Studies of SV in stool and water samples were part of the inclusion criteria.
Results
From 19 low and middle income countries, 45 published studies were identified. The prevalence rate for SV was 6.5%. A significant difference (P=0) in SV prevalent rate was observed between low income and middle income countries. Thirty-three (78.6%) of the studies reported on children and 8 (19%) studies reported on all age groups with diarrhoea. The majority (66.7%) of studies reported on hospitalised patients with acute gastroenteritis. Sapovirus GI was shown as the dominant genogroup, followed by SV-GII.
Conclusion
The detection of human SV in low and middle income countries is evident; however the reports on its prevalence are limited. There is therefore a need for systematic surveillance of the circulation of SV, and their role in diarrhoeal disease and outbreaks, especially in low and middle income countries.
1. Introduction
An estimated number of 6.3 million deaths of children under the age of 5 years suffering from diarrhoea have been reported worldwide [1, 2]. In Africa, death due to diarrhoeal disease remains a major health concern, though it has decreased from 2.6 million to 1.3 million between 1990 and 2013 [3]. Diarrhoeal disease is the important cause of morbidity and mortality in low and middle income countries, also the third most frequent cause of death and greatest contributor to the burden of disease in children younger than 5 years of age [4]. The infection of human intestinal tract occurs through transmission at the household level due to different pathways such as ingestion of contaminated food and water, poor waste disposal, and person-to-person interactions in the households and community [4, 5]. Low and middle income countries still face challenges like inadequate human waste disposal, poor water quality, poor health status, and disease transmission through faecal-oral route [6].
Amongst diarrhoeal causing agents, Sapovirus (SV) is one of the enteric viruses that cause acute gastroenteritis in humans and animals. Sapoviruses were previously called “typical human Caliciviruses” or “Sapporo-like viruses” in the family Caliciviridae [7]. They are identified as nonenveloped, positive-sense, single-stranded ribonucleic acid (RNA) genome of approximately 7.1 to 7.7 kb in size with a poly(A) tail at the 3'-end [8–10]. Amongst the five designated genogroups (GI to GV), GIII infects porcine species [11–14], while GI, GII, GIV, and GV infect humans [15]. Currently, human SV genogroups are classified into 16 genotypes (comprising seven genotypes for GI and GII, respectively, and one genotype each for GIV and GV) through phylogenetic analysis of the complete capsid gene [15, 16]. Coinfections of SVs with other enteric viruses (such as noroviruses [NoVs], rotaviruses [RVs], astroviruses [AstVs], adenoviruses [AdVs], enteroviruses [EVs], and kobuviruses [KbVs]) have been noted in acute gastroenteritis outbreaks in humans [17–19].
This review summarises reports on SV detection and typing in low and middle income countries. In addition, it highlights the need to establish the relatedness of circulating SV strains in environmental (water) samples and clinical samples from communities in low and middle income countries (particularly rural settings). The time-frame chosen was 2004 to 2017 because of the availability of published data on human SV within the low and middle income countries.
2. Methodology
Two literature searches were carried out. The first literature search was performed using the terms: calicivirus, sapovirus, and developing countries, as listed by National Institutes of Health PUBMED library and ScienceDirect. A second literature search was independently done for each of the 139 “developing” countries accessed from the list published by the Society for the Study of Reproduction (http://www.ssr.org). Furthermore, the identified countries were then assessed according to the 2018 World Bank analytical classification report (http://datahelpdesk.worldbank.org/knowledgebase/articles/906519). For a successful search, each of the countries' names was combined with the following keywords: calicivirus, sapovirus, enteric viruses, and gastroenteritis. Studies identified by the search terms were selected for inclusion in the review based on the following inclusion criteria:
Studies limited to human SV detected in clinical specimen and environmental water samples, reported in the 21st century.
SV studies using laboratory molecular techniques including nested-PCR (nPCR), real time-PCR (RT-PCR), and RT-multiplex PCR.
Studies were excluded from the review if SV was detected in other mammalian species or animals or if the study was conducted in high income countries. In case of duplication of studies by authors, only one article was included.
Data was extracted from each selected study when provided: country name and its economic status (i.e., low income, lower, and upper middle income) as per the analytical classification report by World Bank, study setting (hospitalised, outpatient, and environment), study population (age group), population size, duration of the study, diagnostic method used, number of samples tested for SV (including their genogroups and genotypes), first author, and year of publication (Tables 1, 2 and 3).
Table 1.
Summary of human SV detection from 33 studies (stool samples) conducted in 14 non-African low and middle income countries.
| Country | World Bank Classification as of year 2018 | Study setup | Prevalence (seasons or defined period of incidence) | Method used | Rate of Detected Genotypes | Reference | |||
|---|---|---|---|---|---|---|---|---|---|
| Study population | Population size | Study setting | Duration of study | ||||||
| Bangladesh | Lower middle income | Infants/ Children | 917 | HP with AGE | From 2004 to 2005 | Oct 2004 – Jan 2005, Sept 2005 |
RT-PCR | 2.7 % SV (All in <3 yrs of age) SV-GI.1, GI.2 |
Dey et al [20] |
|
| |||||||||
| Brazil | Upper middle income | Children | 305 | HP severe GE | From March to September 2003 | March, May - September | RT-PCR | 15/305 (4.9%), mixed infection of SV and Astv in 1 sample SV-GII.1, SV-GI.1, SV-GI.2 |
Aragao et al [21] |
| Children (0 – 10 yrs | 159 | OP (81 = diar; 78 = non-diar) | From April 2008 to July 2010 | February, April | RT-PCR | 2 of 81: 2.5% SV (GI.1, GII.2) | Aragao et al [22] | ||
| Children (6-55 mn old) | 539 | Day Care (Healthy) | From October 2009 to October 2011 | Not defined | RT- multiplex PCR | 25/539 (4.6%) SV, SV-GI.1, GI.3 |
de Oliveira et al [23] |
||
| Children, outpatients | 212 129 |
HP OP With AGE |
From 2012 to 2014 | Not defined | Quantitative real-time PCR (qPCR) | 12/341 (3.5%) [9/12 – HP, 3/12 – OP]. SV-GI.1 dominant, GI.2, GI.6, GII.1, GV.1 |
Fioretti et al [24] | ||
| Children < 10yrs |
426 (156 of <3yrs tested) |
HP with AGE | From January 2010 to October 2011 | Aug & Sept | RT-PCR | 6/156 (3.8%), SV-GI.1, GI.2, GII.2, GII.4 |
Reymao et al [25] | ||
| Children | 172 | Community | From 1990 t0 1992 | Not defined | Nested PCR | 9/172 (5.2%) SV-GI.1, GI.7, GII.1, GV.2 |
Costa et al [26] | ||
|
| |||||||||
| China | Upper Middle income | Children <5yrs old |
500 | OP with acute (477)/ persistent (23) diar | From August to November 2010 | Aug – Nov 2010 | RT-PCR | 9/477: 1.89% SV (<24 month children), mixed infection of SV & AdV in 1 sample, SV-GI dominant, SV-GII & SV-GIV |
Ren et al [27] |
| Patients (1mn – 78yrs) | 412 | HP & OP with AGE | From August 2014 to September 2015 | Not defined | RT-PCR | [9/412] 2.2% SV single infection, Co-infection: 2/412 ETEC with SV, 1/412 Salmonella sp with SV, 1/412 Salmonella sp with SV & AdV Genogroups not defined |
Shen et al [28] | ||
|
| |||||||||
| India (New Delhi) | Lower middle income | Children <10yrs | 226 | HP with AGE | From August 2000 to December 2001 | Not defined | Multiplex two-step RT-PCR | 23/226 (39%), mixed infection in 5 samples {NV-GII and SV-GI} SV-GI [22], GII [1] |
Rachakonda et al [29] |
|
| |||||||||
| Iran | Upper middle income | Children | 200 | HP with AGE | From 2008 to 2009 | Winter and in fall | RT-PCR | 6/200 (3%), SV-GII |
Parsa-Nahad et al [30] |
| Patients (3 mn - 69yrs; mean 15.3yrs |
42 | HP with AGE | From May to July 2009 | May – July 2009 | RT-PCR | 11.9% SV (patients with <5yrs of age) SV-GI.2 |
Romani et al [31] | ||
|
| |||||||||
| Mongolia | Lower middle income | Infants | 36 | households | From July to August 2003 | Jul – Aug 2003 | RT-PCR | 1/36 (2.8%) pos for SV SV-GI |
Hansman et al [11, 12] |
|
| |||||||||
| Nicaragua | Lower middle income | Children <5yrs | 330 | (175 HP; 155 OP), with AGE /diar | From September 2009 to October 2010 | Nov 2009- Feb/Mar 2010, May-Aug/Sept 2010 | Real-time PCR | 57/330 (17%): HP = 15% [27/175], OP = 19% [30/155]. SV-GI, GII, GIV {HP: GI.1, GI.2; OP: GII.2, GII.3 |
Bucardo et al [32] |
|
| |||||||||
| Pakistan | Lower middle income | Infants <6 to >35 mn |
122 Pos: Enteric Viruses | HP with AGE | From 1990 to 1994 | Mar, Aug - Oct | RT-PCR | 13.9% SV detection (12.3% SV mono-infections, 1.6 mixed infection – AstV & SV), SV-GI | Phan et al [33] |
| Infants & children <1 mn – 5yrs |
517 | HP with AGE | From 1990 to 1994 | 1990: Aug, Sept, Oct 1991: Jan, May, Jul, Oct 1992: Mar, Aug, Sep 1993: Sep 1994: Apr, July |
RT-PCR |
3.2 % SV SV-GI dominated, followed by GII, and GIV |
Phan et al [34] | ||
|
| |||||||||
| Papua New Guinea (Goroka) | Lower middle income | Children <5yrs | 199 | HP with AGE | From August 2009 to November 2010 | Not defined | RT-PCR | 4/199 (2%) SV, Genogroups not defined |
Soli et al [35] |
|
| |||||||||
| Peru | Upper middle income | Children <2yrs | 599 | 300 non-diar, 299 diar | From 2007 to 2010 | Four seasons | Quantitative reverse transcription-real-time PCR (qPCR) | 9.0% overall: ∗ 12.4% [37/299] diarrhoeal – SV-GI/1/2/6/7, GII.1/2/4/5, GIV, GV/1; ∗ 5.7% [17/300] non-diarrhoeal – SV-GII.5, GIV |
Liu et al [36] |
|
| |||||||||
| Philippines | Lower middle income | Children <5yrs | 417 | HP with AGE | From June 2012 to August 2013 | Not defined | Real-time PCR | 29/417 (7%) detection, (co-infection in 10/29: 6/10 with RV, 2/10 with NV, 2/10 with AstV). SV-GI.1, GI.2, GII.1, GII.4 & GV |
Liu et al [1, 2] |
|
| |||||||||
| Thailand | Upper middle income | Infants | 80 randomly selected | HP with AGE | From November 2002 to April 2003 | Nov 2002 – April 2003 | RT-PCR | 15%: 11% single infection, 4% mixed infection – NoV & SV), SV-GI |
Guntapong et al [37] |
| Children <5yrs | 248 | HP with AGE | From 2002 to 2004 | Not defined | RT-PCR | 3/248 (1.2%) SV- single infections SV-GI [GI.1 &GI.2], GIV |
Khamrin et al [38] | ||
| Children | 296 | HP with AGE | From May 2000 to March 2002 | Jun-Jul, Jan-Mar, May-Jul, Mar. | RT-PCR | 25%, mixed infection I 1 sample (NV-GI and SV) SV-GI.1, GI.4, GI.5, GII.1, GII.2 |
Malasao et al [39] | ||
| All age groups | 273 | HP with AGE/diar | From January 2006 to February 2007 | Early summer: March & April | RT-PCR | 0.8% SV SV-GII/3 |
Kittigul et al [40] | ||
| Children (Neonate to 5yrs old) | 147 | HP with AGE/watery | January to December 2005 | Not defined | RT-PCR | 5/147 (3.4%) SV SV-GI [GI.2, GI.1, GI.5] dominating, SV-GII.3 |
Khamrin et al [41] | ||
| Pediatric patients | 160 | HP with AGE | January to December 2007 | Throughout the year | RT-multiplex PCR | 5/160 (3.1%) SV Genogroup not defined |
Chaimongkol et al [42] | ||
| Children <5yrs | 567 | HP with AGE | In 2007, and from 2010 to 2011 | 2007: Feb, Sept, Oct. & 2010: Dec | Semi-nested RT-PCR | 7/567 (1.2%), SV-GI.1 |
Chaimongkol et al [43] | ||
| Adult (15yrs – 90yrs) | 332 | HP with diar | Year 2008 | Not defined | RT- multiplex PCR | No SV detected | Saikruang et al [44] | ||
| Patients | 1141 | HP with AGE | From 2006 to 2008 | May - July | RT-PCR | 1.1% SV, mixed infection of NoV-GII & SV in 2 samples Genogroup not defined |
Pongsuwanna et al [45] | ||
|
| |||||||||
| Vietnam | Lower middle income | Children | 448 | HP with acute sporadic gastroenteritis | From December 1999 to November 2000 | Not defined | RT-PCR | 1/448 (0.2%) SV SV-GI |
Hansman et al [46] |
| Paediatric patients | 1010 | HP with viral AGE | From October 2002 to September 2003 | Oct 2002 – Sep 2003, Rainy season (July) |
RT-PCR | 0.8% SV (0.4% monoinfection, 0.4% coinfection), Genogroup not defined |
Nguyen et al [47] | ||
| Pediatric | 502 | HP with AGE | From December 2005 to November 2006 | Dry season | RT-PCR | 1.2% SV | Nguyen et al [48] | ||
| Children <5yrs | 501 | HP with AGE | From November 2007 to October 2008 | Cooler months (Oct – Feb) | Real-time RT-PCR | 1.4% SV SV-GI and SV-GII Co-infection of (NoV & SV) in 1 sample, of (NoV, SV, and RV) in 1 sample |
Trang et al [49] | ||
|
| |||||||||
| Independent States of the former Soviet Union | See information below describing the States | Children | 495 | HP with AGE | From January to December 2009 | Jan - Mar, May – Aug | Real-time PCR | 16/495 (3.2%) SV-GI.1 dominating |
Chhabra et al [50] |
HP = hospitalised patient; OP = outpatient; AGE = acute gastroenteritis; mn= month; yr(s) = year(s); diar = diarrhoea; SV = Sapovirus; G (I-IV) = genogroup (I-IV)
∗ Independent States of the former Soviet Union refers to Armenia, Azerbaijan & Belarus ( upper middle income status ), and Georgia, Republic of Moldova & Ukraine ( lower middle income status ).
Table 2.
Summary of human SV detection from 9 studies (stool samples) conducted in 5 African countries.
| Country | World Bank Classification as of year 2018 | Study setup | Prevalence (seasons or defined period of incidence) | Method used | Rate of Detected Genotypes | Reference | |||
|---|---|---|---|---|---|---|---|---|---|
| Study population | Population size | Study setting | Duration of study | ||||||
| Burkina Faso | Low income | Children | 263 diarrhoeal, 50 non-diarrhoeal | Urban area (HP & OP) | From November 2011 to September 2012 | Not defined | Real-time RT-PCR | 9%: 27/263 (10.3%) {5/27 = hospitalised, 22/27 = non-hospitalised} & 3/50 (6%) SV-GII [GII.2, GII.1, GII.3], SV-GI.2 |
Ouedraogo et al [51] |
| Children <5yrs | 309 diarrhoeal | Not defined | From May 2009 to March 2010 | Not defined | Real-time PCR | 56/309 (18%) [mixed infection: with RV 25/56, with NV 5/56; single infection 20/56] Genogrouping {34/56}: SV-GI [GI.1, GI.4], GII [GII.1, GII.4, GII.6], GIV.1 & GV.1 |
Matussek et al [16] | ||
|
| |||||||||
| Ethiopia | Low income | All age groups | 213 diarrheic samples | Government Health Care Centre | From June to September 2013 | June-sept 2013 | RT-PCR | 9/213 (4.2%) One sequenced (SV-GII.1) |
Sisay et al [52] |
|
| |||||||||
| Kenya | Lower middle income | All age groups | 334-Lwak & 524-Kibera. | Clinics with diar | From June 2007 to October 2008 | Not defined | RT-PCR | 5%: 13/334 (4%) and 31/524 (6%) SV Genogroups not defined |
Shioda et al [3] |
|
| |||||||||
| South Africa | Upper middle income | Paediatric <13yrs | 245 | HP gastroenteritis | Year 2008 | Not defined |
Real-time RT-PCR | 10/245 (4.1%) incl. one Mixed infection with NV Genogroups not defined |
Mans et al [53] |
| Patients 1mn to 87yrs mean 14yrs | 190 94 diar 93 non-diar 3 unknown |
Bio-wipes from rural households | From July 2007 to December 2008 | Not defined | Real-time RT-PCR | 16/190 (8.4%): (1 - 62yrs: mean 24yrs) Genogroups not defined |
Mans et al [54] | ||
| Children | Selected) 296 of 477 SV-Pos (for characterisation) |
HP with gastroenteritis | From April 2009 to December 2013 | Not defined | Nested PCR | 221 were characterised (genotyped) SV-GI [GI.1 – GI.3, GI.5, GI.6, GI.7], SV-GII [GII.1 – GII.7], SV-GIV |
Murray et al [55] | ||
| Children <5yrs | 3103 | HP diar | From 2009 to 2013 | Higher in Summer & Autumn (Nov to Apr) | Real-time PCR | 238/3103 (7.7%) SV Genogroups not defined |
Page et al [56] | ||
|
| |||||||||
| Tunisia | Lower middle income | Children | 788 [408 HP, 380 OP] |
Consulting for AGE | From January 2003 to April 2007 | Not defined | RT-PCR Primer Noel, 1997 |
6/788 (0.8%) [Mixed infection: with RV 2/6; single infection 4/6]. Positive from OP samples SV-GI.1 |
Sdiri-Loulizi et al [57] |
HP = hospitalised patient; OP = outpatient; AGE = acute gastroenteritis; mn= month; yr(s) = year(s); diar = diarrhoea; SV = Sapovirus; G (I-IV) = genogroup (I-IV).
Table 3.
Summary of human SV detection from 4 studies (water samples) conducted in low and middle income countries.
| Country | World Bank Classification as of year 2018 | Samples | Prevalence (season) | Method used | Rate of detection | Reference | ||
|---|---|---|---|---|---|---|---|---|
| Type | Size | Duration | ||||||
| Brazil | Upper middle income | Wastewater | 156 | From 2012 to 2014 | Summer and Autumn | Quantitative real-time PCR (qPCR) | 51/156 (33%) | Fioretti et al [24] |
|
| ||||||||
| South Africa | Upper middle income | River water | 99 | From 2009 to 2010 | May, Aug, Nov (2009); Jan, April (2010) | RT-PCR | 48/99 (48.5%) | Murray et al [58] |
| Wastewater | 51 | From August 2010 to December 2011 | August (2010), June, July (2011) | Real-Time qPCR | 37/51 (72.5%) | Murray et al [59] | ||
| Water (various source) | 10 | January and March 2012 | January and March 2012 | Real-Time PCR | 8/10 (80%) | Murray and Taylor [60] | ||
The difference of SV data in middle and low income countries was analysed for statistical significance by Student's t-test using the simple interactive statistical analysis (SISA) at http:home.clara.net/sisa. Result with P < 0.05 was considered significant.
3. Results
A total of 138 articles published from 2004 to 2017 were identified from 19 low and middle income countries. After selection based on the selection criteria (Figure 1), a total of 45 studies met the inclusion criteria. From 45 publications, 41 reported on clinical (stool) samples, 3 on environmental (water) samples, and 1 on both. Of the 42 studies conducted on clinical specimens, 66.7% (n=28) were done in hospitalised patients, 23.8% (n=10) in outpatients, and 9.5% (n=4) in both hospitalised and outpatient settings.
Figure 1.
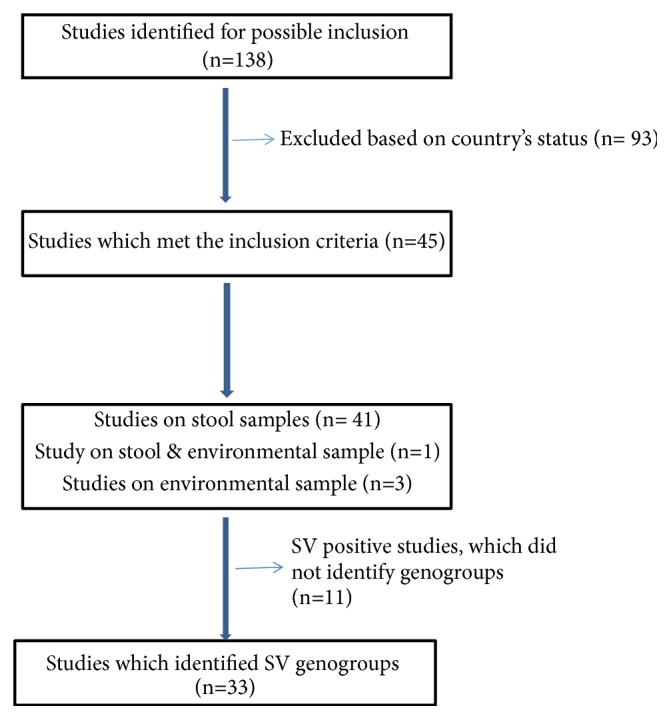
Schematic diagram showing search process for selection of studies reported.
3.1. SV Age Distribution in Human Populations
The majority of studies (78.6%; 33/42) investigated SV in children less than 5 years of age and a further 19% (8/42) included all ages. However, only a single study investigated SV in adults with diarrhoea or acute gastroenteritis.
3.2. Seasonality
The detection of SV from clinical samples based on seasonality was reported in only 14.3% (6/42) of the studies. The majority (42.9%, 18/42) of the studies did not report on the time-frame of detection, 38% (16/42) of the studies showed inconsistent time-frame of detection, and 4.8% (2/42) of the studies showed detection throughout the year. Studies investigating SV in water sources in South Africa (SA) did not detect any seasonal peaks.
Five studies reported on samples collected within a period of 2 to 4 months, and these cases were not defined as outbreaks, while the duration period of sample collection for other 40 studies ranged over periods from 1 year to 5 years.
3.3. Sapovirus Detection and Genotyping
From the 42 included studies, 41 of these reported SV positive cases while only one study on adults reported negative results (Tables 1 and 2). Mixed infection of SV with bacteria and/or other enteric viruses was identified in 19.5% (8/41) of the studies, a SV single strain was identified in 36.6% (15/41) of the studies, and mixed strains of SV were identified in 43.9% (18/41) of the studies. From the 41 studies, only 31 studies reported SV detection with identification of the genogroups/genotypes. Overall detection of SV strains showed SV-GI.1 and GI.2 as the most dominant [90% (28/31)] strain from different settings of studies, followed by SV-GII.1, GII.2, GII.3, and GII.4 with the least detection of SV-GIV strain and –GV (GV.2) strain. No study showed the occurrence of SV-GIV as a single detection but only in mixed infection cases.
The prevalence rate of SV from the 41 documented studies in low and middle countries was 6.19% with a range from 0.2% to 39%. Further breakdown showed significant difference (P =0) in SV prevalence rate between low income (10.40%) and middle income (5.86%) countries. Although data on the prevalence of SV in African countries is limited, thus far, eight studies have been conducted in urban settings. Detection of SV from children in Africa is recorded with different incidence rates: in Tunisia [0.8%] [57], Burkina Faso [18%, 10.3%, respectively] [16, 51], and South Africa [4.1%, 7.7%, respectively] [53, 56]. The prevalence of SV in all ages was reported from South Africa [8.4%] [54], Ethiopia [4.2%] [52], and Kenya [4%] [3]. A predominance of SV-GIV (53/221, 24%) was noted in the South African study done on stool samples from hospitalised children with gastroenteritis [55].
Only 8.9% of studies reported SV in the environmental and waste water samples from low and middle income countries. The detection of SV-GI, SV-GII, and SV-GIV has been reported from polluted water sources by wastewaters and also on samples collected from treatment plants within selected areas of SA [58–60]. Sapovirus genogroups I and II were identified from river water samples, with detection rate of 48.5% (48/99) [58], while, in Brazil, SV-GI (genotypes 1 and 2) were detected (33%, 51/156) from the wastewaters [22], Table 3.
4. Discussion
This review provides a summary of studies conducted in developing countries on the detection of human SV. Only 45 (41 stool samples, 3 water samples, and 1 both stool and water sample) studies satisfied the inclusion criteria of this review highlighting the importance for systematic surveillance monitoring human SV circulating in developing countries (rural and urban communities). Very little is known about the contribution of human SV to diarrhoeal disease in developing countries; this is reflected in the fact that reported studies were only from 19 identified countries which include 5 African countries, namely, Burkina Faso, Ethiopia, Kenya, South Africa, and Tunisia (Table 2). A total of 78.6% (33/42) studies reported on children ≤5 years of age from the collected data, highlighting the role of SV in diarrhoeal disease amongst children in the developing countries. Hence, SV and other emerging enteric viruses, being underappreciated, can be an important cause of Norovirus negative outbreaks as reported by Lee and colleagues [61]. In addition, since it is difficult to culture human SV on cell lines [13], specialised molecular laboratories are needed for the investigation of such virus in the developing countries. Because of lack of funding and skills, the prevalence of enteric viruses is underreported in Africa and other developing countries [62]
Most of the studies (66.7%; 28/42) were done in hospitalised patients, and this might be due to the fact that SV infection sometimes leads to hospitalisation as illustrated from other studies [49, 63]. GEMS study reported SV amongst other enteric pathogens to have been associated with moderate to severe diarrhoea in developing countries [64]. The Millennium Development Goals (MDG) 2015 report shows disadvantaged settings being vulnerable as compared with the advantaged or developed settings, highlighting the effectiveness and affordability of treatments, and improved service delivery and political commitment playing a role in such settings. The statistical analysis of this review similarly showed a significant difference in the prevalence of SV in low income than in middle income countries (P=0).
The circulation of SV genogroups shows variability, with SV-GI and SV-GII detected frequently, while SV-GIV and SV-GV are rarely detected comparing to other genogroups [16]. An African study (Burkina Faso) reported SV-GII as the predominated strain, mostly in outpatients with diarrhoea (81.5%: 22/27), suggesting that this genogroup may be less virulent and require fewer hospital admissions. However, additional studies on outpatients will have to be conducted to confirm this observation. Although the detection of SV-GII is seen in diarrhoeal samples, it might be less virulent to cause severe symptoms leading to hospitalisation of patients, unlike SV-GI which is commonly known to be associated with severe symptoms and frequently detected in patients presenting with gastroenteritis [16, 32]. The detection of SV (GI, GII, GIV, and GV) in gastroenteritis outbreak cases has been reported in high income countries, however with less detection rate of SV-GII in both cases [14, 17, 61, 65].
Human SV infections cases relating to acute gastroenteritis in people of all ages have been identified worldwide [14]. Notwithstanding the potential selection biases present based on the studies available for inclusion, this review shows that the prevalence in children may be higher than in adults in low and middle income countries. In addition, the GEMS study in low and middle income countries highlights diarrheal disease in children as a leading cause of illness and death and also increasing the risk of delayed physical and intellectual development [66]. It has been reported that sporadic and outbreak cases caused by enteric viruses spread mainly by person-to-person contact, contaminated surfaces or objects, and contaminated water or food [67]. Therefore children are more vulnerable than adults within such exposed environment, probably because of immune system development. However, previous studies noted that gastroenteritis symptoms are usually self-limiting, and patients usually recover within a couple of days depending on the individual immune's response [49, 63]. Adults are likely to consider self-treatment by oral rehydration solution (ORS) which is the safe, effective, and low cost therapeutic option preventing dehydration [68], hence not consulting in healthcare facilities or likely due to self-respect.
Sapoviruses, like other enteric viruses, play an important role in the burden of disease worldwide. The GEMS conducted a three-year study in selected low and middle income countries, amongst children aged 0 to 59 months, and reported the detection of SV (3.5%) associated with diarrhoea [64]. However, there is no surveillance system on SV infection and prevalence in low and middle income countries, which means underreporting of sporadic cases of human SV and its epidemic are underestimated. Nevertheless, detection and comparison of the SV strains circulating in low and middle income countries (especially Africa) are currently underreported and this could be due to various techniques used for sampling and detection, including study site conditions.
Information on seasonality, patient history, area settings, and predicated pattern of transmission of viruses within the community provides knowledge needed to implement public health intervention strategies. Furthermore, detection of enteric viruses (such as SV) in environmental samples gives awareness of the circulation of infectious viral particles within the population and health-hazards which might be associated with the environment. The predictable effects of human waste disposal, water quality, and high rate of immunocompromised society have been a big concern in low and middle income countries, but there are still few documented reports on the detection of SV from environmental samples. This is highlighted by the finding of this study with high prevalence of SV in low income countries. The survival and development of children depend on good hygiene practices and use of clean drinking and domestic water on daily basis [4]. Monitoring of genetic diversity of the current circulating or emerging SV genogroups, possible water-borne transmission, and possible zoonotic infections amongst the communities is critical, and studies which can show the transmission of SV between the environment(s) (especially river water), domestic animals, and human should be considered, and the role that SV plays in diarrhoeal diseases [69].
5. Conclusion
This review found substantial evidence of SV proportion associated with diarrhoeal disease in low and middle income countries. However there is limited data reporting the detection of circulating SV strains. Therefore systematic surveillance of SV circulation within the communities in low and middle income countries is needed to assess sufficiently its role in diarrhoea disease.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Liu L., Oza S., Hogan D., et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet. 2015;385(9966):430–440. doi: 10.1016/s0140-6736(14)61695-0. [DOI] [PubMed] [Google Scholar]
- 2.Liu X., Yamamoto D., Saito M., et al. Molecular detection and characterization of sapovirus in hospitalized children with acute gastroenteritis in the Philippines. Journal of Clinical Virology. 2015;68:83–88. doi: 10.1016/j.jcv.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Shioda K., Cosmas L., Audi A., et al. Population-based incidence rates of diarrheal disease associated with norovirus, sapovirus, and astrovirus in Kenya. PLoS ONE. 2016;11(4) doi: 10.1371/journal.pone.0145943.e0145943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Govender T., Barnes J. M., Pieper C. H. Contribution of water pollution from inadequate sanitation and housing quality to diarrheal disease in low-cost housing settlements of Cape Town, South Africa. American Journal of Public Health. 2011;101(7):p. -e9. doi: 10.2105/AJPH.2010.300107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisenberg J. N. S., Scott J. C., Porco T. Integrating disease control strategies: Balancing water sanitation and hygiene interventions to reduce diarrheal disease burden. American Journal of Public Health. 2007;97(5):846–852. doi: 10.2105/AJPH.2006.086207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infectious Diseases. 2015;17:909–948. doi: 10.1016/S1473-3099(17)30276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayo M. A. A summary of taxonomic changes recently approved by ICTV. Archives of Virology. 2002;147(8):1655–1656. doi: 10.1007/s007050200039. [DOI] [PubMed] [Google Scholar]
- 8.Oka T., Lu Z., Phan T., Delwart E. L., Saif L. J., Wang Q. Genetic characterization and classification of human and animal sapoviruses. PLoS ONE. 2016;11(5) doi: 10.1371/journal.pone.0156373.e0156373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green KY. Caliciviridae: the noroviruses: specific virus families. In: Howley P. M., Griffin D. E., Lamb R. A., Martin M. A., Roizman B., Straus S. E., editors. Fields virology. 5th. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2007. pp. 949–979. [Google Scholar]
- 10.Chang K.-O., Sosnovtsev S. S., Belliot G., Wang Q., Saif L. J., Green K. Y. Reverse genetics system for porcine enteric calicivirus, a prototype sapovirus in the Caliciviridae. Journal of Virology. 2005;79(3):1409–1416. doi: 10.1128/JVI.79.3.1409-1416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansman G. S., Natori K., Oka T., et al. Cross-reactivity among sapovirus recombinant capsid proteins. Archives of Virology. 2005;150(1):21–36. doi: 10.1007/s00705-004-0406-8. [DOI] [PubMed] [Google Scholar]
- 12.Hansman G. S., Kuramitsu M., Yoshida H., et al. Viral gastroenteritis in Mongolian infants [10] Emerging Infectious Diseases. 2005;11(1):180–182. doi: 10.3201/eid1101.040337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hansman G. S., Saito H., Shibata C., et al. Outbreak of gastroenteritis due to sapovirus. Journal of Clinical Microbiology. 2007;45(4):1347–1349. doi: 10.1128/JCM.01854-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oka T., Wang Q., Katayama K., Saif L. J. Comprehensive review of human sapoviruses. Clinical Microbiology Reviews. 2015;28(1):32–53. doi: 10.1128/cmr.00011-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oka T., Mori K., Iritani N., et al. Human sapovirus classification based on complete capsid nucleotide sequences. Archives of Virology. 2012;157(2):349–352. doi: 10.1007/s00705-011-1161-2. [DOI] [PubMed] [Google Scholar]
- 16.Matussek A., Dienus O., Djeneba O., Simpore J., Nitiema L., Nordgren J. Molecular characterization and genetic susceptibility of sapovirus in children with diarrhea in Burkina Faso. Infection, Genetics and Evolution. 2015;32:396–400. doi: 10.1016/j.meegid.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 17.Iritani N., Kaida A., Abe N., et al. Detection and genetic characterization of human enteric viruses in oyster-associated gastroenteritis outbreaks between 2001 and 2012 in Osaka City, Japan. Journal of Medical Virology. 2014;86(12):2019–2025. doi: 10.1002/jmv.23883. [DOI] [PubMed] [Google Scholar]
- 18.Iizuka S., Oka T., Tabara K., et al. Detection of sapoviruses and noroviruses in an outbreak of gastroenteritis linked genetically to shellfish. Journal of Medical Virology. 2010;82(7):1247–1254. doi: 10.1002/jmv.21791. [DOI] [PubMed] [Google Scholar]
- 19.Räsänen S., Lappalainen S., Kaikkonen S., Hämäläinen M., Salminen M., Vesikari T. Mixed viral infections causing acute gastroenteritis in children in a waterborne outbreak. Epidemiology and Infection. 2010;138(9):1227–1234. doi: 10.1017/S0950268809991671. [DOI] [PubMed] [Google Scholar]
- 20.Dey S. K., Phan T. G., Nguyen T. A., et al. Prevalence of sapovirus infection among infants and children with acute gastroenteritis in Dhaka City, Bangladesh during 2004-2005. Journal of Medical Virology. 2007;79(5):633–638. doi: 10.1002/jmv.20859. [DOI] [PubMed] [Google Scholar]
- 21.Aragão G. C., Oliveira D. d., Santos M. C., et al. Molecular characterization of norovirus, sapovirus and astrovirus in children with acute gastroenteritis from Belém, Pará, Brazil. Revista Pan-Amazônica de Saúde. 2010;1(1) doi: 10.5123/S2176-62232010000100021. [DOI] [Google Scholar]
- 22.Aragão G. C., Mascarenhas J. D., Kaiano J. H., et al. Norovirus Diversity in Diarrheic Children from an African-Descendant Settlement in Belém, Northern Brazil. PLoS ONE. 2013;8(2):p. e56608. doi: 10.1371/journal.pone.0056608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marques Mendanha de Oliveira D., Souza M., Souza Fiaccadori F., César Pereira Santos H., das Dôres de Paula Cardoso D. Monitoring of calicivirus among day-care children: Evidence of asymptomatic viral excretion and first report of GI.7 norovirus and GI.3 sapovirus in Brazil. Journal of Medical Virology. 2014;86(9):1569–1575. doi: 10.1002/jmv.23791. [DOI] [PubMed] [Google Scholar]
- 24.Fioretti J. M., Rocha M. S., Fumian T. M., et al. Occurrence of human sapoviruses in wastewater and stool samples in Rio De Janeiro, Brazil. Journal of Applied Microbiology. 2016;121(3):855–862. doi: 10.1111/jam.13205. [DOI] [PubMed] [Google Scholar]
- 25.Reymão T. K. A., Hernandez J. D. M., Costa S. T. P. D., et al. Sapoviruses in children with acute gastroenteritis from manaus , Amazon region, Brazil, 2010-2011. Revista do Instituto de Medicina Tropical de São Paulo. 2016;58:p. 81. doi: 10.1590/S1678-9946201658081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Costa L. C. P. D. N., Siqueira J. A. M., Portal T. M., et al. Detection and genotyping of human adenovirus and sapovirus in children with acute gastroenteritis in Belém, Pará, between 1990 and 1992: First detection of GI.7 and GV.2 sapoviruses in Brazil. Journal of the Brazilian Society of Tropical Medicine. 2017;50(5):621–628. doi: 10.1590/0037-8682-0198-2017. [DOI] [PubMed] [Google Scholar]
- 27.Ren Z., Kong Y., Wang J., Wang Q., Huang A., Xu H. Etiological study of enteric viruses and the genetic diversity of norovirus, sapovirus, adenovirus, and astrovirus in children with diarrhea in Chongqing, China. BMC Infectious Diseases. 2013;13(1, article 412) doi: 10.1186/1471-2334-13-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shen H., Zhang J., Li Y., et al. The 12 gastrointestinal pathogens spectrum of acute infectious diarrhea in a sentinel hospital, Shenzhen, China. Frontiers in Microbiology. 2016;7 doi: 10.3389/fmicb.2016.01926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rachakonda G., Choudekar A., Parveen S., Bhatnagar S., Patwari A., Broor S. Genetic diversity of noroviruses and sapoviruses in children with acute sporadic gastroenteritis in New Delhi, India. Journal of Clinical Virology. 2008;43(1):42–48. doi: 10.1016/j.jcv.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Parsa-Nahad M., Samarbaf-Zadeh A. R., Makvandi M., et al. Relative frequency of sapovirus among children under 5 years of age with acute gastroenteritis at the Aboozar Hospital, Ahvaz, Iran. Jundishapur Journal of Microbiology. 2012;5(1):359–361. [Google Scholar]
- 31.Romani S., Azimzadeh P., Mohebbi S. R., Bozorgi S. M., Zali N., Jadali F. Prevalence of sapovirus infection among infant and adult patients with acute gastroenteritis in Tehran, Iran. Gastroenterology and Hepatology from Bed to Bench. 2012;5(1):43–48. [PMC free article] [PubMed] [Google Scholar]
- 32.Bucardo F., Reyes Y., Svensson L., Nordgren J. Predominance of norovirus and sapovirus in nicaragua after implementation of universal rotavirus vaccination. PLoS ONE. 2014;9(5) doi: 10.1371/journal.pone.0098201.e98201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phan T. G., Okame M., Nguyen T. A., et al. Human Astrovirus, Norovirus (GI, GII), and Sapovirus Infections in Pakistani Children with Diarrhea. Journal of Medical Virology. 2004;73(2):256–261. doi: 10.1002/jmv.20084. [DOI] [PubMed] [Google Scholar]
- 34.Phan T. G., Okame M., Nguyen T. A., Nishio O., Okitsu S., Ushijima H. Genetic diversity of sapovirus in fecal specimens from infants and children with acute gastroenteritis in Pakistan. Archives of Virology. 2005;150(2):371–377. doi: 10.1007/s00705-004-0401-0. [DOI] [PubMed] [Google Scholar]
- 35.Soli K. W., Maure T., Kas M. P., et al. Detection of enteric viral and bacterial pathogens associated with paediatric diarrhoea in Goroka, Papua New Guinea. International Journal of Infectious Diseases. 2014;27:54–58. doi: 10.1016/j.ijid.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 36.Liu X., Jahuira H., Gilman R. H., et al. Etiological role and repeated infections of sapovirus among children aged less than 2 years in a cohort study in a peri-urban community of Peru. Journal of Clinical Microbiology. 2016;54(6):1598–1604. doi: 10.1128/JCM.03133-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guntapong R., Hansman G. S., Oka T., et al. Norovirus and sapovirus infections in Thailand. Japanese Journal of Infectious Diseases. 2004;57(6):276–278. [PubMed] [Google Scholar]
- 38.Khamrin P., Maneekarn N., Peerakome S., et al. Genetic diversity of noroviruses and sapoviruses in children hospitalized with acute gastroenteritis in Chiang Mai, Thailand. Journal of Medical Virology. 2007;79(12):1921–1926. doi: 10.1002/jmv.21004. [DOI] [PubMed] [Google Scholar]
- 39.Malasao R., Maneekarn N., Khamrin P., et al. Genetic diversity of norovirus, sapovirus, and astrovirus isolated from children hospitalized with acute gastroenteritis in Chiang Mai, Thailand. Journal of Medical Virology. 2008;80(10):1749–1755. doi: 10.1002/jmv.21244. [DOI] [PubMed] [Google Scholar]
- 40.Kittigul L., Pombubpa K., Taweekate Y., Yeephoo T., Khamrin P., Ushijima H. Molecular characterization of rotaviruses, noroviruses, sapovirus, and adenoviruses in patients with acute gastroenteritis in Thailand. Journal of Medical Virology. 2009;81(2):345–353. doi: 10.1002/jmv.21380. [DOI] [PubMed] [Google Scholar]
- 41.Khamrin P., Maneekarn N., Thongprachum A., Chaimongkol N., Okitsu S., Ushijima H. Emergence of new norovirus variants and genetic heterogeneity of noroviruses and sapoviruses in children admitted to hospital with diarrhea in Thailand. Journal of Medical Virology. 2010;82(2):289–296. doi: 10.1002/jmv.21640. [DOI] [PubMed] [Google Scholar]
- 42.Chaimongkol N., Khamrin P., Suantai B., et al. A wide variety of diarrhea viruses circulating in pediatric patients in Thailand. Clinical Laboratory. 2012;58(1-2):117–123. [PubMed] [Google Scholar]
- 43.Chaimongkol N., Khamrin P., Malasao R., et al. Molecular characterization of norovirus variants and genetic diversity of noroviruses and sapoviruses in Thailand. Journal of Medical Virology. 2014;86(7):1210–1218. doi: 10.1002/jmv.23781. [DOI] [PubMed] [Google Scholar]
- 44.Saikruang W., Khamrin P., Suantai B., et al. Detection of diarrheal viruses circulating in adult patients in Thailand. Archives of Virology. 2014;159(12):3371–3375. doi: 10.1007/s00705-014-2191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pongsuwanna Y., Tacharoenmuang R., Prapanpoj M., et al. Monthly distribution of norovirus and sapovirus causing viral gastroenteritis in Thailand. Japanese Journal of Infectious Diseases. 2017;70(1):84–86. doi: 10.7883/yoken.JJID.2015.440. [DOI] [PubMed] [Google Scholar]
- 46.Hansman G. S., Doan L. T. P., Kguyen T. A., et al. Detection of norovirus and sapovirus infection among children with gastroenteritis in Ho Chi Minh City, Vietnam. Archives of Virology. 2004;149(9):1673–1688. doi: 10.1007/s00705-004-0345-4. [DOI] [PubMed] [Google Scholar]
- 47.Nguyen T. A., Yagyu F., Okame M., et al. Diversity of viruses associated with acute gastroenteritis in children hospitalized with diarrhea in Ho Chi Minh City, Vietnam. Journal of Medical Virology. 2007;79(5):582–590. doi: 10.1002/jmv.20857. [DOI] [PubMed] [Google Scholar]
- 48.Nguyen T. A., Hoang L., Pham L. D., et al. Norovirus and sapovirus infections among children with acute gastroenteritis in Ho Chi Minh City during 2005-2006. Journal of Tropical Pediatrics. 2008;54(2):102–113. doi: 10.1093/tropej/fmm096. [DOI] [PubMed] [Google Scholar]
- 49.Trang N. V., Luan L. T., Kim-Anh L. T., et al. Detection and molecular characterization of noroviruses and sapoviruses in children admitted to hospital with acute gastroenteritis in Vietnam. Journal of Medical Virology. 2012;84(2):290–297. doi: 10.1002/jmv.23185. [DOI] [PubMed] [Google Scholar]
- 50.Chhabra P., Samoilovich E., Yermalovich M., et al. Viral gastroenteritis in rotavirus negative hospitalized children <5 years of age from the independent states of the former Soviet Union. Infection, Genetics and Evolution. 2014;28:283–288. doi: 10.1016/j.meegid.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 51.Ouédraogo N., Kaplon J., Bonkoungou I. J. O., et al. Prevalence and genetic diversity of enteric viruses in children with diarrhea in Ouagadougou, Burkina Faso. PLoS ONE. 2016;11(4) doi: 10.1371/journal.pone.0153652.e0153652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sisay Z., Djikeng A., Berhe N., et al. Prevalence and molecular characterization of human noroviruses and sapoviruses in Ethiopia. Archives of Virology. 2016;161(8):2169–2182. doi: 10.1007/s00705-016-2887-7. [DOI] [PubMed] [Google Scholar]
- 53.Mans J., de Villiers J. C., Du Plessis N. M., Avenant T., Taylor M. B. Emerging norovirus GII.4 2008 variant detected in hospitalised paediatric patients in South Africa. Journal of Clinical Virology. 2008;49(4):258–264. doi: 10.1016/j.jcv.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 54.Mans J., van Zyl W. B., Taylor M. B., et al. Applicability of Bio-wipes for the collection of human faecal specimens for detection and characterisation of enteric viruses. Tropical Medicine & International Health. 2014;19(3):293–300. doi: 10.1111/tmi.12251. [DOI] [PubMed] [Google Scholar]
- 55.Murray T. Y., Nadan S., Page N. A., Taylor M. B. Diverse sapovirus genotypes identified in children hospitalised with gastroenteritis in selected regions of South Africa. Journal of Clinical Virology. 2016;76:24–29. doi: 10.1016/j.jcv.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 56.Page N., Groome M. J., Murray T., et al. Sapovirus prevalence in children less than five years of age hospitalised for diarrhoeal disease in South Africa, 2009–2013. Journal of Clinical Virology. 2016;78:82–88. doi: 10.1016/j.jcv.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 57.Sdiri-Loulizi K., Hassine M., Gharbi-Khelifi H., et al. Molecular detection of genogroup I sapovirus in Tunisian children suffering from acute gastroenteritis. Virus Genes. 2011;43(1):6–12. doi: 10.1007/s11262-011-0600-1. [DOI] [PubMed] [Google Scholar]
- 58.Murray T. Y., Mans J., Taylor M. B. Human calicivirus diversity in wastewater in south africa. Journal of Applied Microbiology. 2013;114(6):1843–1853. doi: 10.1111/jam.12167. [DOI] [PubMed] [Google Scholar]
- 59.Murray T. Y., Mans J., van Zyl W. B., Taylor M. B. Application of a Competitive Internal Amplification Control for the Detection of Sapoviruses in Wastewater. Food and Environmental Virology. 2013;5(1):61–68. doi: 10.1007/s12560-012-9101-1. [DOI] [PubMed] [Google Scholar]
- 60.Murray T. Y., Taylor M. B. Quantification and molecular characterisation of human sapoviruses in water sources impacted by highly polluted discharged wastewater in South Africa. Journal of Water and Health. 2015;13(4):1055–1059. doi: 10.2166/wh.2015.255. [DOI] [PubMed] [Google Scholar]
- 61.Lee L. E., Cebelinski E. A., Fuller C., et al. Sapovirus outbreaks in long-term care facilities, Oregon and Minnesota, USA, 2002-2009. Emerging Infectious Diseases. 2012;18(5):873–876. doi: 10.3201/eid1805.111843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kabue J. P., Meader E., Hunter P. R., Potgieter N. Human Norovirus prevalence in Africa: A review of studies from 1990 to 2013. Tropical Medicine & International Health. 2016;21(1):2–17. doi: 10.1111/tmi.12617. [DOI] [PubMed] [Google Scholar]
- 63.Lorrot M., Bon F., El Hajje M. J., et al. Epidemiology and clinical features of gastroenteritis in hospitalised children: Prospective survey during a 2-year period in a Parisian hospital, France. European Journal of Clinical Microbiology & Infectious Diseases. 2011;30(3):361–368. doi: 10.1007/s10096-010-1094-9. [DOI] [PubMed] [Google Scholar]
- 64.Kotloff K. L., Nataro J. P., Blackwelder W. C., et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. The Lancet. 2013;382(9888):209–222. doi: 10.1016/s0140-6736(13)60844-2. [DOI] [PubMed] [Google Scholar]
- 65.Pang X. L., Lee B. E., Tyrrell G. J., Preiksaitis J. K. Epidemiology and genotype analysis of sapovirus associated with gastroenteritis outbreaks in Alberta, Canada: 2004-2007. The Journal of Infectious Diseases. 2009;199(4):547–551. doi: 10.1086/596210. [DOI] [PubMed] [Google Scholar]
- 66.Kotloff K. L., Blackwelder W. C., Nasrin D., et al. The Global Enteric Multicenter Study (GEMS) of diarrheal disease in infants and young children in developing countries: epidemiologic and clinical methods of the case/control study. Clinical Infectious Diseases. 2012;55(supplement 4):S232–S245. doi: 10.1093/cid/cis753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lopman B., Gastañaduy P., Park G. W., Hall A. J., Parashar U. D., Vinjé J. Environmental transmission of norovirus gastroenteritis. Current Opinion in Virology. 2012;2(1):96–102. doi: 10.1016/j.coviro.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 68.Binder H. J., Brown I., Ramakrishna B. S., Young G. P. Oral rehydration therapy in the second decade of the twenty-first century. Current Fungal Infection Reports. 2014;16(3) doi: 10.1007/s11894-014-0376-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kumthip K., Khamrin P., Maneekarn N. Molecular epidemiology and genotype distributions of noroviruses and sapoviruses in Thailand 2000-2016: A review. Journal of Medical Virology. 2018;90(4):617–624. doi: 10.1002/jmv.25019. [DOI] [PubMed] [Google Scholar]


