Abstract
Background
Rapid placement of a reliable airway is the most important task in anesthesia practice. Airway management is a critical skill to provide safe anesthesia since morbidity. In addition, mortality due to anesthesia could be linked to difficulty or failure in airway management. In this study, intubation success was compared between two methods, AirQ-ILA and LMAfastrach, among candidates for elective surgery under general anesthesia.
Methods
In this clinical trial, patients, who were candidates for elective surgery under general anesthesia at Firoozgar and Rasoul Akram Hospitals, were randomly divided into LMAfastrach and AirQ-ILA groups. Heart rate before and after induction and intubation, diastolic blood pressure, systolic blood pressure, duration of device insertion, intubation time, number of attempts until successful device insertion and trachea intubation, and success or failure in the insertion of the device and the tube were recorded; as for statistical analysis, SPSS version 21 was considered.
Results
In comparison with the LMAfastrach group, the device insertion time and intubation time were significantly longer in the AirQ-ILA group (P < 0.05). However, the groups showed no significant difference regarding the number of device and tube insertion attempts (P > 0.05). Moreover, no significant difference was observed in the success of device insertion and intubation in either LMAfastrach or AirQ-ILA group (P > 0.05).
Conclusions
The LMAfastrach and AirQ-ILA methods were not significantly different regarding the success of airway instrument application and intubation, while the device insertion time and intubation time were significantly longer in the AirQ-ILA group in comparison with the LMAfastrach group.
Keywords: LMAfastrach, AirQ-ILA, Endotracheal Tube
1. Background
General anesthesia has several effects on the respiratory system, the most important of which is the reduction of airway reflex mechanism, laxity of muscle pharynx and larynx, hypoventilation, and apnea (1). Airway management in patients undergoing general anesthesia is a set of actions that result in the creation of a safe and secure airway for ventilation (2). Failure in the airway management and hypoxia can lead to irreversible brain damage within only a few minutes. Therefore, establishing a fast and secure airway is one of the most important tasks of an anesthesiologist.
Morbidity and mortality due to anesthesia might be attributed to difficulty or failure in airway management (3). The safest and most effective method to establish the airway is the use of direct laryngoscopy and tracheal tube placement (4). Since 1880, when the use of airway intubation was firstly simulated, several methods and devices have been introduced. As a matter of fact, direct laryngoscopy and tracheal intubation remain the gold standard (5). Depending on the circumstances, intubation with direct laryngoscopy may sometimes fail and it also may be dangerous for anesthesiologists; therefore, the use of new alternative tools is always considered.
The main reason for failure in laryngoscopy is the anatomical condition of the patient and the physician’s experience in performing a laryngoscopy (6). The availability of alternative equipment and methods may increase the success rate for anesthesiologists. Some alternative facilities are used to ease airway management with less manipulation. All of these devices are placed at the top of the glottis. In fact, they are fixed in the pharynx, which is another auxiliary airway management method not requiring a laryngoscope (7). However, devices such as the LMA (laryngeal mask airway), Igel (8) and combitube could be very helpful for patient ventilation. However, endotracheal intubation is a better way to prevent aspiration of the gastric contents, and in some cases, it has restrictions with positive pressure ventilation (9). The replacement devices of laryngoscopy for the tracheal tube include lighted stylet and c-trach (10). Additionally, some other devices are used, and their usefulness has been confirmed in ventilation of patients. The benefits of this tool include the following: ease of placement, no special skills needed, and general intubation of the trachea (11).
The intubating LMA or LMA Fastrach was designed specifically to facilitate tracheal intubation during maintaining ventilation (12). The ILMA overcomes the diameter-length limitations for the tracheal tube imposed by classic LMA and facilitates guidance of the tracheal tube towards the glottis (2). Nonetheless, the ILMA method comes with some limitations, it requires the use of expensive (high pressure cuffed, reinforced) silicone and it may not be used for the pediatric population under 30 kilogram (13).
A newer device similar to Fastrach was recently designed with the name of Air-Q. It is also named as Intubating Laryngeal Airway. Some facilities have been considered in the design of this device, such as the epiglottis elevator, to ease intubation with an endotracheal tube, breathing tube is shorter and wider than ILMA, and use of inexpensive tracheal tube PVC (Polyvinyl chloride) (14, 15).
The efficacy and success of the new tool have been studied and compared with other devices of the airway management. Due to its ease of use, speed of implantation, and success rate, the aim is to compare AirQ-ILA (AirQ- intubating laryngeal mask) (Cookgas LLC., St. Louis, MO) and LMAfastrach (Laryngeal Mask Company, Jersey, UK) methods in patients undergoing elective surgery during general anesthesia to evaluate whether it is an acceptable alternative for airway management.
2. Methods
This single-blinded clinical trial was approved by the Ethical Committee of Iran University of Medical Sciences (IR.IUMS.REC1394.9211174014) and registered in Iranian Clinical Trial site (IRCT20151107024909N7). This study was conducted in Firoozgar and Rasoul Akram Hospitals affiliated to the Iran University of Medical Sciences. After complete explanation to the patients and obtaining written consent, patients candidate to surgeries under general anesthesia were classified randomly into 2 groups using even and odd numbers (AirQ-ILA and LMAfastrach, respectively).
The inclusion criteria were as follows: fasting for at least 8 hours, age range of 18 - 60 years, ASA I and II, elective surgeries within a predicted duration of less than three hours, and airway profile (thyromental distance (TMD) of more than 6 cm, mouth opening of more than two finger widths, and Modified Mallampati classification (15) of I, II, and III).
The exclusion criteria were as follows: body mass index (BMI) above 30 kg/m2, diagnosis of gastroesophageal reflux disease (GERD), and a modified Mallampati classification of ІV. Peripheral oxygen saturation (SpO2), electrocardiography (ECG), heart rate (HR), mean arterial pressure (MAP), diastolic blood pressure (DBP), systolic blood pressure (SBP), and end-tidal CO2 were also monitored. HR and BP were recorded. Afterwards, anesthesia was induced according to the following method. Acccording to Jagannathan et al. (15) study and power = 90% and confident interval = 0.05; sample size was calculated and equal to 63 in each group.
Upon arrival at the operating room, patients’ airway class were assessed according to modified Mallampati classification (16) and recorded. All the patients received 5 mg/kg of crystalloid solution and were preoxygenated with 100% oxygen for 3 minutes. Then, they were premedicated with 0.02 mg/kg of midadzolam and 2 µg/kg of fentanyl. Thiopental and atracurium (0.5 mg/kg of each) were used to induce general anesthesia. After the ‘patients were ventilated for 3 minutes, the patients’ head were placed in neutral position and the devices (Air Q-ILA or LMAfastrach) were applied. For insertion of ILMA, the device was inserted by one-handed rotational movement in the sagittal plane. The deflated cuff was lubricated with 2% lidocaine jelly applied to the posterior surface of the mask bowl and was flattened against the palate with its rim facing posterioirly. ILMA was inserted in a circular movement by holding the handle, while maintaining contact against the curve of the palate and posterior pharynx. Then, the handle was released and the cuff was inflated. To obtain the optimal position for tracheal intubation, the handle was moved side to side, in and out, or even lifted anteriorly to reach optimised ventilation.
For patients assigned to the Air-Q group, the posterior surface of the device was lubricated with 2% lidocaine jelly. The tongue was pushed downwards using a tongue depressor. With the right hand of the operator, the device was inserted touching the palate and was gently pushed forward, until it was stopped with a resistance, then, the cuff was inflated with the volume recommended by the manufacturer. An assistant lifted the patient’s mandibule during passage of the device to the phrynx. If the air-Q device got stuck during insertion, the left index finger of the operator was placed behind the mask to push it forward along the curve of palate and posterior pharyngeal wall.
The cuff inflated with air as per manufacture’s recommendation.
After confirming proper device insertion through observing end-tidal CO2 increase and bilateral chest rise on capnography, the trachea was intubated (disposable reinforced PVC in Air-Q group and reinforced silicon tube in ILMA group). The tracheal tube size was selected according to the device’s size (Tables 1 and 2).
Table 1. LMAfastrach Size Relative to Body Weight and Endotracheal Tube Size According to the LMAfastrach Size.
| LMAfastrach Size | Patient’s Weight, kg | Endotracheal Tube Size, ID |
|---|---|---|
| 3 | 30 - 50 | 7 |
| 4 | 50 - 70 | 7.5 |
| 5 | 70 - 100 | > 7.5 |
Abbreviation: ID, internal diameter (millimeter).
Table 2. AirQ-ILA Size According to the Patient’s Weight and Endotracheal Tube Size According to AirQ-ILA.
| AirQ-ILA Size | Patient’s Weight, kg | Endotracheal Tube Size, ID |
|---|---|---|
| 3.5 | 50 - 70 | 7 - 7.5 |
| 4.5 | 70 - 100 | 8 - 8.5 |
The tracheal tube was cuffed after intubation. The correct position of the endotracheal tube was ensured using capnography and auscultation of breath sounds. If failure occurred at the first attempt of device insertion, the device was removed and inserted again. If tracheal intubation was not successful, the tracheal tube was removed by keeping the device in place, and tracheal intubation was then attempted again. After removing the device, intubation was carried out via direct laryngoscopy if either device insertion or tracheal intubation was unsuccessful despite three attempts. The number of patients with a successful device insertion attempt was recorded and used for subsequent analysis. The interval between the time the device passed through the mouth opening and ventilation without air leakage (airway pressure, 20 cm H2O) was interpreted as the device insertion time, while the interval between intubation with the endotracheal tube through the device and confirmation of successful intubation was interpreted as intubation time; both intervals were recorded. Moreover, the number of tracheal intubation attempts was recorded.
Neostigmine and atropine (0.04 and 0.02 mg/kg, respectively) were used to reverse the neuromuscular blockade; after extubation, the patient’s throat was checked for bleeding. The patient was kept for at least half an hour in the recovery room. After complete consciousness was achieved, the patient was asked about complications, including sore throat and hoarseness, and the answer was recorded. All of the above mentioned procedures were accomplished by one person (named the executive of the project). Before starting the project, the executive of the project practiced with the device as well as the tube placement at least 30 times to gain the needed skills.
The gathered data were analyzed by SPSS version 22. First, the normality of the quantitative variables was assessed based on a Kolmogorov-Smirnov test and was not confirmed. Therefore, to compare quantitative variables, Mann-Whitney U test or Independent t-test was applied, while to compare qualitative variables, Chi square or Fisher’s exact test was used. The significance level was set at 0.05.
For sample size calculation, a pilot study comparing the difference in time duration of device insertion with 10 patients in each group was performed. Based on the results of the pilot study, the time difference in the duration of device insertion between the two groups was three minutes (17 ± 5 minutes in LMAfastrach group versus 20 ± 6 minutes in AirQ-ILA group. With the consideration of 95% confidence interval and 80% power, the number of patients in each group was calculated by 53. Due to the probability of attrition and non-response, 63 patients were assigned to (in) each group.
3. Results
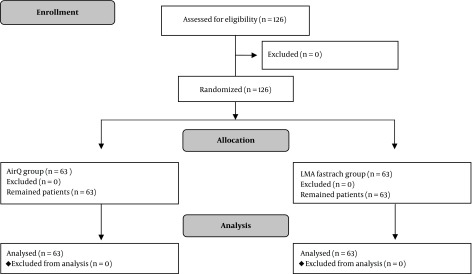
In this study, 126 eligible patients undergoing elective surgery were enrolled (Figure 1), and 63 (50%) patients were assigned to each group (LMAfastrach and AirQ-ILA groups). Table 3 presents the demographic information. No significant differences were found regarding gender, weight, or age between the LMAfastrach and AirQ-ILA groups (P > 0.05) (Table 3).
Figure 1. Consort flow chart of the study.
Table 3. Demographic Data in the LMAfastrach and AirQ-ILA Groupsa.
| Variable | Group | Total | P Value | |
|---|---|---|---|---|
| AirQ-ILA | LMAfastrach | |||
| Age, y | 36 ± 13.88 | 39.73 ± 15.28 | 37.86 ± 14.66 | 0.146 |
| Sex, male | 37 (58.7) | 34 (54) | 71 (56.3) | 0.72 |
| Weight, kg | 73.95 ± 12.54 | 75.28 ± 15.1 | 74.61 ± 13.84 | 0.924 |
aValues are expressed as mean ± SD or frequency (%).
The LMAfastrach and AirQ-ILA groups were not significantly different in terms of DBP, SBP, MAP, or HR after induction (P > 0.05). In addition, the LMAfastrach and AirQ-ILA groups were not significantly different regarding SBP, DBP, MAP, and HR after intubation (P >0.05). However, a significant increase was reported in SBP, DBP, MAP, and HR after induction and intubation in both the LMAfastrach (P < 0.05) and AirQ-ILA (P < 0.05) groups (Table 4).
Table 4. Comparison of DBP, SBP, MAP, and HR Among Candidates for Elective Surgery in the LMAfastrach and AirQ-ILA Groupsa.
| Variable | Group | P1 Value | |
|---|---|---|---|
| AirQ-ILA | LMAfastrach | ||
| SBP, mmHg | |||
| Before induction | 115.04 ± 21 | 117.92 ± 15.43 | 0.171 |
| After intubation | 122.2 ± 21.84 | 122.25 ± 14.1 | 0.828 |
| P2 value | < 0.001 | 0.009 | |
| DBP, mmHg | |||
| Before induction | 74.25 ± 12.61 | 76.57 ± 10.61 | 0.171 |
| After intubation | 81.93 ± 11.65 | 79.3 ± 9.8 | 0.828 |
| P2 value | < 0.001 | 0.035 | |
| MAP | |||
| Before induction | 101.44 ± 17.67 | 104.13 ± 12.89 | 0.093 |
| After intubation | 108.78 ± 17.74 | 107.93 ± 12.2 | 0.756 |
| P2 value | < 0.001 | 0.007 | |
| HR | |||
| Before induction | 77.01 ± 13.87 | 78.3 ± 14.77 | 0.397 |
| After intubation | 84.03 ± 10.99 | 84.55 ± 10.54 | 0.785 |
| P2 value | < 0.001 | < 0.001 | |
aValues are expressed as mean ± SD.
In the AirQ-ILA group, the intubation time and device insertion time were significantly longer than the LMAfastrach group (P < 0.05). However, the groups were not significantly different considering the number of device and tube insertion attempts (P > 0.05). Moreover, the groups were not significantly different regarding success in device and tube insertion (P > 0.05) (Table 5).
Table 5. Comparison of Device and Tube Insertion in Patients Undergoing Elective Surgery in the LMAfastrach and AirQ-ILA Groupsa.
| Variable | Group | P Value | |
|---|---|---|---|
| AirQ-ILA | LMAfastrach | ||
| Time insertion of device, s | 21.92 ± 5.4 | 17.92 ± 5.94 | < 0.001 |
| Time insertion of tube, s | 23.92 ± 7.08 | 17.93 ± 4.4 | < 0.001 |
| Number of insertion attempts to device | 0.201 | ||
| One | 56 (88.9) | 61 (96.8) | |
| Two | 6 (9.5) | 2 (3.2) | |
| Three | 1 (1.6) | 0 (0) | |
| Number of insertion attempts to tube | 0.708 | ||
| One | 51 (92.7) | 57 (95) | |
| Two | 7 (7.3) | 3 (5) | |
| Insertion of device | 1 | ||
| Success | 63 (100) | 63 (100) | |
| Failure | 0 (0) | 0 (0) | |
| Insertion of tube | 0.205 | ||
| Success | 60 (95.2) | 55 (87.3) | |
| Failure | 3 (4.8) | 8 (12.7) | |
aValues are expressed as mean ± SD or No. (%).
There was no significant difference regarding complications, including sore throat, hoarseness, and bleeding between the LMAfastrach and AirQ-ILA groups (P > 0.05) (Table 6).
Table 6. Comparison of Complications in the LMAfastrach and AirQ-ILA Groupsa.
| Complication | Group | P Value | |
|---|---|---|---|
| AirQ-ILA | LMAfastrach | ||
| Sore throat | 21 (33.3) | 14 (22.2) | 0.232 |
| Hoarseness | 2 (3.2) | 1 (1.6) | 1 |
| Bleeding | 21 (33.3) | 15 (23.8) | 0.324 |
aValues are expressed as frequency (%).
No significant relationship was observed between the success of device insertion and Mallampati score of patients in the LMAfastrach and AirQ-ILA groups (P > 0.05) (Table 7).
Table 7. Relationship Between the Success of Device Insertion and Mallampati in the LMAfastrach and AirQ-ILA Groupsa.
| Group | Mallampati | Insertion of Device | P Value | |
|---|---|---|---|---|
| Success | Failure | |||
| AirQ-ILA | 1 | |||
| 1 | 16 (100) | 0 (0) | ||
| 2 | 33 (100) | 0 (0) | ||
| 3 | 14 (100) | 0 (0) | ||
| LMAfastrach | 1 | |||
| 1 | 16 (100) | 0 (0) | ||
| 2 | 35 (100) | 0 (0) | ||
| 3 | 12 (100) | 0 (0) | ||
aValues are expressed as frequency (%).
Successful intubation through the device and Mallampati were not significantly associated in the LMAfastrach and AirQ-ILA groups (P > 0.05) (Table 8).
Table 8. Relationship Between the Successful Intubation Through the Device and Mallampati in Patients Undergoing Elective Surgery in the LMAfastrach and AirQ-ILA Groupsa.
| Group | Mallampati | Intubation Through the Device | P Value | |
|---|---|---|---|---|
| Success | Failure | |||
| AirQ-ILA | 0.578 | |||
| 1 | 16 (100) | 0 (0) | ||
| 2 | 31 (88.5) | 2 (11.5) | ||
| 3 | 13 (92.8) | 1 (7.2) | ||
| LMAfastrach | 0.132 | |||
| 1 | 16 (100) | 0 (0) | ||
| 2 | 30 (85.7) | 5 (14.3) | ||
| 3 | 9 (75) | 3 (25) | ||
aValues are expressed as frequency (%).
No significant difference was detected in successful tube insertion through the device (intubation) in patients with a Mallampati of 3 in the LMAfastrach and AirQ-ILA groups (P > 0.05) (Table 9).
Table 9. Comparison of Successful tube Insertion in Patients Undergoing Elective Surgery with Mallampati Score of 3 in the LMAfastrach and AirQ-ILA Groupsa.
| Insertion of Tube | Group | P Value | |
|---|---|---|---|
| AirQ-ILA | LMAfastrach | ||
| Success | 9 (75) | 13 (92.8) | 0.306 |
| Failure | 3 (25) | 1 (7.22) | |
aValues are expressed as No. (%).
4. Discussion
Based on the present findings, the LMAfastrach and AirQ-ILA groups were not significantly different regarding the duration of attempts to place the airway device and tracheal tube properly. Additionally, no significant difference was found in the success of device insertion and intubation with the device between patients undergoing elective surgery in the groups. However, the duration of the time to insert the instrument and tube in AirQ-ILA group was longer than that of the LMAfastrach group.
In the study of Malhotra et al. which showed similar results to our study, the authors concluded that the success rate for insertion of the tube in patients undergoing elective surgery after three attempts for the AirQ-ILA and LMAfastrach methods was 96% and 91%, respectively, with no meaningful difference. Additionally, the LMAfastrach and AirQ-ILA groups were not significantly different regarding the number of attempts to place the device and tracheal tube properly. However, unlike the present study, the time to successfully insert the device and intubate the trachea through the device was shorter in the AirQ-ILA group in comparison with the LMAfastrach group (17). In a similar study, Shamaa et al. reported that the success rates of inserting the tube in patients under elective surgery after two attempts in the AirQ-ILA and LMA fastrach methods were 83% and 89%, respectively, with no meaningful difference. The difference between the attempts to properly place the airway instrument and intubation was not significant for the LMAfastrach and AirQ-ILA groups. Additionally, the duration of the time to correctly place the instrument and tracheal tube was longer in the AirQ-ILA method than in the ILMA fastrach method (18). In consistence with our study, Garzon Sanchez et al. (19) showed that both LMAfastrach and AirQ-ILA methods have similar success rates for applying the tracheal tube.
Badawi et al. showed results consistent with our study and noticed that the success rates for intubation in patients under elective surgery after two attempts in the AirQ-ILA and LMAfastrach methods were 94% and 96%, respectively, and had no meaningful difference. Additionally, the application times of the instrument in the AirQ-ILA group was greater than that of the LMA fastrach group. However, the time to successfully intubate the patients was shorter in the AirQ-ILA group, compared to the LMA fastrach group (20). In a study by Abdel-Halim et al. which showed consistent results with our study, no significant difference was observed in the time of applying the airway instrument in the LMA fastrach and AirQ-ILA groups. Additionally, the success rate for applying the tube equals 100% after two attempts in both groups. However, unlike in our study, the application time of the instrument and tube in the AirQ-ILA group was less than that of the LMAfastrach group (21). In the study of Neoh and Choy in which the results were consistent with our study, they concluded that there was no difference between the success rate for applying the airway instrument in patients under elective surgery for the LMAfastrach and AirQILA groups. However, unlike in our study, the rate of success for applying the tracheal tube in patients undergoing elective surgery in the LMAfastrach method was higher than that of the AirQ-ILA method (22).
In the study of Erlacher et al. the success rates for applying the tracheal tube by CobraPLUS, AirQ, and LMA fastrach were 47%, 57%, and 95%, respectively, and as in our study, they observed that after three attempts, the success rate for applying the tracheal tube in every three instruments was 100% (23). According to a study by Karim and Swanson which was consistent with our study, the duration of intubation in patients undergoing elective surgery in the AirQ-ILA method was longer than that of the LMAfastrach method. The success rates for applying the tube after three attempts in the AirQ-ILA and LMAfastrach methods were 100% and 95%, respectively. Hence, in the results that were inconsistent with our study, they concluded that the duration of applying the instrument for patients undergoing elective surgery in the method of AirQ-ILA was shorter than that of the LMAfastrach method (13).
Consistent with our study, Sastre et al. (24) showed no significant difference in intubation success between the LMAfastrach and AirQ-ILA methods in candidates for elective surgery. Similarly, in a study by Kim et al. the success of applying the tracheal tube in mannequin simulation in the AirQ-ILA method was lower than the LMAfastrach method. However, unlike in our study, the duration for applying the tracheal tube under mannequin simulation in the AirQ-ILA group was less than that of the LMAfastrach group (25).
In the study of Attarde et al. they noticed that the success rates for applying tubes with the size of 3.5 and 4.5 in the AirQ-ILA group were 80% and 67%, respectively. They recommended that the size of the AirQ be selected based on weight and the amount of opening the mouth of patients. In addition, it should be confirmed based on the physiological and anatomical specifications of the patient (14). In two studies by Yamada et al. no significant differences were found between the AirQILA and LMAfastrach groups in the success of tubing after three attempts in two different positions of the patient’s head. Hence, after two attempts in an unnatural head position, the success of tubing in the AirQ-ILA group was less than the LMAfastrach group (26, 27). The lack of consistency between some of our results and other studies may be due to differences in physiological and anatomical specifications of patients, position of the patient during application of the airway instrument and tracheal tube, size of the airway instrument and tracheal tube, different factory products of the airway instrument and tracheal tube, or different methods of general anesthesia.
In this study, no significant difference was found in hemodynamic changes (i.e., SBP, DBP, MAP, and HR) between the LMAfastrach and AirQ-ILA groups after induction and intubation. In a study by Malhotra et al. (17) which found similar results to this one, hemodynamic changes were not significantly different between the LMAfastrach and AirQ-ILA groups. Furthermore, in a study by Shamaa et al. which found similar results to this study, no difference was found in HR after induction and intubation between the LMA fastrach and AirQ-ILA groups. Additionally, no significant difference was found in terms of MAP after induction and intubation between the groups, although the increase in MAP after intubation was higher in the AirQ-ILA group (18). Consistent with the study here, Abdel-Halim et al. showed no significant differences in MAP and HR one minute after device placement and intubation in the LMAfastrach and AirQ-ILA groups. However, unlike this study, after applying the tracheal tube, there was a difference between the HR of the two groups (21). Badawi et al. (20) in a study consistent with this one, noticed that before and after applying instrument there was a difference between the hemodynamic changes (e.g., HR and blood pressure) in patients undergoing elective surgery between the LMAfastrach and AirQ-IL groups.
Based on the present results, there was no meaningful difference between the indicating effects, including sore throat, harshness of voice, and bleeding of patients under elective surgery between the LMAfastrach and AirQ-IL groups. The study of Malhotra et al. (17) which showed similar results to this one, reached the same conclusion as did this study. In the other study done by Shamaa et al. (18) no difference was observed in complications, including sore throat, voice disorder, and bleeding, between the LMAfastrach and AirQ-IL groups. In the study of Garzon Sanchez et al. (19) which showed results consistent with our study, they stated that both the LMAfastrach and AirQ-IL methods have the same rate of side effects, including sore throat and harshness of voice. The study of Abdel-Halim et al. (21) which showed results consistent with our study, concluded that there was no difference between indicating effects, including a sore throat, in patients under surgery between the LMAfastrach and AirQIL groups. Badawi et al. (20) who showed consistent results with this study, indicated no difference in sore throat, harshness of voice, and bleeding between the LMAfastrach and AirQ-IL groups. In the study of Neoh and Choy (22) which showed results consistent with those of this study, they noticed that there was no significant difference between the indicating effects, including sore throat, harshness of voice, and bleeding in patients under elective surgery between the LMAfastrach and AirQ-IL groups. Karim and Swanson (13) which showed results similar to those of the study here, understood that there was no difference between the indicating effects, including sore throat, harshness of voice, and bleeding of patients undergoing elective surgery in the LMAfastrach and AirQ-IL groups. Similarly, in the study by Sastre et al. (24) the side effects (sore throat and harshness of voice) were similar in the LMAfastrach and AirQ-IL groups.
As it is shown in Table 9, we also compared the success rate of tube insertion through the device in patients with high Mallampati class in the study groups, which was not performed in previous available studies. Although the number of patients on whom tube insertion through the device was larger in LMAfastrch group than those in AirQ-Ila group, the difference was not statistically significant. To reach a valuable conclusion in this matter, larger number of patients might be needed.
4.1. Conclusion
The present study showed no significant difference between the LMA fastrach and AirQ-ILA groups in terms of success in airway instrument application and tracheal intubation, number of attempts to successfully place the airway instrument and intubate the trachea, hemodynamic changes, and side effects. However, the time needed to properly place the airway device and intubate the trachea was longer in the AirQ-ILA method than LMAfastrach method.
4.2. Further Suggestions
Since small sizes of the AirQ devices are available, performing future studies to evaluate the efficiency of this instrument in the intubation of children is needed. Furthermore, as one of the indications of application of these supraglotic airways is difficult airway management; further studies on patients with high Mallampati class and in larger number of patients are suggested.
Contributor Information
Seydalireza Seyed Siamdoust, Email: siamdoust.a@iums.ac.ir.
Faranak Rokhtabnak, Email: rkhtbnk@yahoo.com.
Soudabeh Djalali Motlagh, Email: djalalimotlagh@icloud.com.
Poupak Rahimzadeh, Email: poupak_rah@hotmail.com.
Valiollah Hassani, Email: valiollah_hassani@yahoo.com.
Mahdi Farnaghizad, Email: farnaghi@yahoo.com.
References
- 1.Benumof JL. Handbook of Difficult Airway Management. Philadelphia, Pa: Churchill Livingstone; 2000. The ASA difficult airway algorithm: new thoughts and considerations. pp. 31–4. [Google Scholar]
- 2.Brain AI, Verghese C, Addy EV, Kapila A, Brimacombe J. The intubating laryngeal mask. II: A preliminary clinical report of a new means of intubating the trachea. Br J Anaesth. 1997;79(6):704–9. doi: 10.1093/bja/79.6.704. [DOI] [PubMed] [Google Scholar]
- 3.Timmermann A, Russo SG. Which airway should I use? Curr Opin Anaesthesiol. 2007;20(6):595–9. doi: 10.1097/ACO.0b013e3282f13a77. [DOI] [PubMed] [Google Scholar]
- 4.Pandit JJ, MacLachlan K, Dravid RM, Popat MT. Comparison of times to achieve tracheal intubation with three techniques using the laryngeal or intubating laryngeal mask airway. Anaesthesia. 2002;57(2):128–32. doi: 10.1046/j.0003-2409.2001.02401.x. [DOI] [PubMed] [Google Scholar]
- 5.Martin C, Nefzger T, Lotz G. [Atemwegsmanagement – alternatives atemwegsmanagement im rettungsdienst] AINS-Anästhesiologie Intensivmedizin Notfallmedizin Schmerztherapie. 2016;51(04):254–62. doi: 10.1055/s-0041-103153. German. [DOI] [PubMed] [Google Scholar]
- 6.Rajagopal MR, Paul J. Applied anatomy and physiology of the airway and breathing. India J Anaesth. 2005 ;49(4):251–6. [Google Scholar]
- 7.Brimacombe J. A proposed classification system for extraglottic airway devices. Anesthesiology. 2004;101(2):559. doi: 10.1097/00000542-200408000-00054. [DOI] [PubMed] [Google Scholar]
- 8.Pournajafian A, Alimian M, Rokhtabnak F, Ghodraty M, Mojri M. Success rate of airway devices insertion: laryngeal mask airway versus supraglottic gel device. Anesth Pain Med. 2015;5(2):e22068. doi: 10.5812/aapm.22068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caponas G. Intubating laryngeal mask airway. Anaesth Intensive Care. 2002;30(5):551–69. doi: 10.1177/0310057X0203000503. [DOI] [PubMed] [Google Scholar]
- 10.Hagberg CA. Special devices and techniques. Anesthesiol Clin North America. 2002;20(4):907–32. doi: 10.1016/s0889-8537(02)00023-8. [DOI] [PubMed] [Google Scholar]
- 11.Cook TM, Lee G, Nolan JP. The ProSeal laryngeal mask airway: a review of the literature. Can J Anaesth. 2005;52(7):739–60. doi: 10.1007/BF03016565. [DOI] [PubMed] [Google Scholar]
- 12.Henderson JJ, Popat MT, Latto IP, Pearce AC Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59(7):675–94. doi: 10.1111/j.1365-2044.2004.03831.x. [DOI] [PubMed] [Google Scholar]
- 13.Karim YM, Swanson DE. Comparison of blind tracheal intubation through the intubating laryngeal mask airway (LMA Fastrach) and the Air-Q. Anaesthesia. 2011;66(3):185–90. doi: 10.1111/j.1365-2044.2011.06625.x. [DOI] [PubMed] [Google Scholar]
- 14.Attarde VB, Kotekar N, Shetty SM. Air-Q intubating laryngeal airway: A study of the second generation supraglottic airway device. Indian J Anaesth. 2016;60(5):343–8. doi: 10.4103/0019-5049.181596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air-Q intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: a case series. Paediatr Anaesth. 2009;19(6):618–22. doi: 10.1111/j.1460-9592.2009.02990.x. [DOI] [PubMed] [Google Scholar]
- 16.Ambesh SP, Singh N, Rao PB, Gupta D, Singh PK, Singh U. A combination of the modified Mallampati score, thyromental distance, anatomical abnormality, and cervical mobility (M-TAC) predicts difficult laryngoscopy better than Mallampati classification. Acta Anaesthesiol Taiwan. 2013;51(2):58–62. doi: 10.1016/j.aat.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Malhotra SK, Bharath KV, Saini V. Comparison of success rate of intubation through Air-Q with ILMA using two different endotracheal tubes. Indian J Anaesth. 2016;60(4):242–7. doi: 10.4103/0019-5049.179448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shamaa MA, Alia DA, El-Sayed M. Intubating laryngeal mask airway and air-Q for blind tracheal intubation. Res Opin Anesth Intensive Care. 2015;2(4):101. doi: 10.4103/2356-9115.178901. [DOI] [Google Scholar]
- 19.Garzon Sanchez JC, Lopez Correa T, Sastre Rincon JA. [Blind tracheal intubation with the air-Q((R)) (ILA-Cookgas) mask. A comparison with the ILMA-Fastrach laryngeal intubation mask]. Rev Esp Anestesiol Reanim. 2014;61(4):190–5. doi: 10.1016/j.redar.2013.11.002. Spanish. [DOI] [PubMed] [Google Scholar]
- 20.Badawi R, Mohamed NN, Al-Haq MMA. Tips and tricks to increase the success rate of blind tracheal intubation through the Air-Q™ versus the intubating laryngeal mask airway Fastrach™. Egypt J Anaesth. 2014;30(1):59–65. doi: 10.1016/j.egja.2013.08.002. [DOI] [Google Scholar]
- 21.Abdel-Halim TM, Abo El Enin MA, Elgoushi MM, Afifi MG, Atwa HS. Comparative study between Air-Q and intubating laryngeal mask airway when used as conduit for fiber-optic. Egypt J Anaesth. 2014;30(2):107–13. doi: 10.1016/j.egja.2013.10.004. [DOI] [Google Scholar]
- 22.Neoh EU, Choy YC. Comparison of the air-Q ILA™ and the LMA-Fastrach™ in airway management during general anaesthesia. South Afr J Anaesth Analg. 2014;18(3):150–5. doi: 10.1080/22201173.2012.10872844. [DOI] [Google Scholar]
- 23.Erlacher W, Tiefenbrunner H, Kastenbauer T, Schwarz S, Fitzgerald RD. CobraPLUS and Cookgas air-Q versus Fastrach for blind endotracheal intubation: a randomised controlled trial. Eur J Anaesthesiol. 2011;28(3):181–6. doi: 10.1097/EJA.0b013e328340c352. [DOI] [PubMed] [Google Scholar]
- 24.Sastre JA, López T, Garzón JC. Blind tracheal intubation through air-Q® supralaryngeal device: comparison with intubating laryngeal mask airway. Department of Anesthesiology and Resuscitation, University Hospital of Salamanca Walk of San Vicente; 2009. 124 p [Google Scholar]
- 25.Kim YY, Kang GH, Kim WH, Choi HY, Jang YS, Lee YJ, et al. Comparison of blind intubation through supraglottic devices and direct laryngoscopy by novices: a simulation manikin study. Clin Exp Emerg Med. 2016;3(2):75–80. doi: 10.15441/ceem.15.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamada R, Maruyama K, Hirabayashi G, Koyama Y, Andoh T. Effect of head position on the success rate of blind intubation using intubating supraglottic airway devices. Am J Emerg Med. 2016;34(7):1193–7. doi: 10.1016/j.ajem.2016.02.076. [DOI] [PubMed] [Google Scholar]
- 27.Yamada R, Maruyama K, Akihisa Y, Koyama Y, Andoh T. Comparison of success rate of blind intubation through Air-Q and LMA FastrachTM in sniffing position and neutral position. Eur J Anaesthesiol. 2013;30:249. doi: 10.1097/00003643-201306001-00778. [DOI] [Google Scholar]