Abstract
Autoimmune diseases often have overlapping symptoms and laboratory somewhat unfamiliar to the non-rheumatologist. Characteristic signs, symptoms, and autoantibodies define specific connective tissue diseases. Some patients have some characteristic symptoms, but cannot be definitively classified. Still other patients meet criteria for more than one specific connective tissue disease. These patients can be confusing with regard to diagnosis and prognosis. Clarification of each patient’s condition can lead to improved patient care.
Introduction
Autoimmune diseases are complex and in general, relatively rare. Characteristic signs, symptoms, and autoantibodies define specific connective tissue diseases. Some patients meet criteria for more than one defined connective tissue disease (CTD), while others have several symptoms characteristic of autoimmune diseases yet cannot be definitively classified. This variability can lead to confusion, especially to the non-rheumatologist. This article will help remove confusion regarding the diagnoses mixed connective tissue disease (MCTD), overlap syndromes, and undifferentiated connective tissue disease (UCTD), as well as in enhance understanding of these conditions.
Currently, there are criteria for classification for five defined autoimmune connective tissue diseases. These include: Systemic lupus erythematosus (SLE), scleroderma, myositis, rheumatoid arthritis (RA), and Sjogren’s syndrome. All five are variable in presentation, but generally over time, the diagnosis of a defined CTD is readily apparent. Some patients, however, may have features characteristic of autoimmune diseases such as Raynaud’s phenomenon (RP), arthralgias, myalgias, or a positive anti-nuclear antibody (ANA), but not meet criteria for a defined condition; in those cases, the diagnosis may not be obvious. Such patients are often diagnosed as “UCTD.” Other patients may meet criteria for two or more defined autoimmune conditions; these patients are often referred to as having an “overlap syndrome.” MCTD is one such overlap syndrome, and will be discussed further in this article.
Undifferentiated Connective Tissue Disease
Patients who have symptoms and laboratory findings consistent with a systemic CTD, but do not meet the criteria for classification of a particular disease are often considered to have UCTD. This concept was initially proposed by LeRoy and colleagues in 19801 to refer to the early phases of connective tissue diseases that were initially undefined; they questioned whether a portion of these patients might remain undifferentiated indefinitely or experience complete remission or whether they might all eventually develop a defined autoimmune disease. There are not defined criteria for such patients; however, these patients often have laboratory evidence of positive anti-nuclear antibodies without specific autoantibodies. RP as well as arthritis/arthralgias, nonspecific rash, or sicca symptoms are common features seen in these patients.
Studies have observed cohorts of patients diagnosed with UCTD for several years. Bodolay, et al reported on 665 Hungarian patients with UCTD followed for five years.2 In that cohort, 34% of the patients eventually developed a well-defined CTD: RA in 13.1%, Sjogren’s syndrome in 6.8%, SLE in 4.2%, scleroderma, in 2.8%, MCTD in 4.0%, systemic vasculitis in 3.3% and myositis in 0.5%. 12.3% of the patient’s achieved complete remission. They observed that the highest probability of evolution to a differentiated CTD is within the first two years after onset of symptoms.
In another study, a U.S. multi-institutional outpatient inception cohort of 213 UCTD patients was evaluated after ten years.3 The patients were divided into three categories: isolated RP (31 patients), unexplained polyarthritis (UPA) (67 patients), and UCTD (115 patients) defined as meeting at least three of 11 specific manifestations of connective tissue disease. In the 115 UCTD patients, 47 were lost to follow up. Twelve patients had died (one with RA and one with SLE). Twelve patients were in remission, six patients developed RA, eleven were diagnosed with SLE, three with systemic sclerosis, one with psoriatic arthritis, and one was diagnosed with myasthenia gravis. The remaining 26 continued to have unclassified disease.
Other groups have examined similar patients;4–7 an average of 30% of UCTD eventually developed a defined CTD, while the majority remained active but with undifferentiated disease. Fortunately, in patients who remained undifferentiated, there tended to be absence of major organ involvement.
Since evolution to a defined CTD can occur, it is important to monitor these patients regularly, especially during the first two years of manifestations, or during conditions which may interfere with the course of an autoimmune disease such as severe infection or pregnancy. Careful management of UCTD patients is reasonable, but at times difficult. Consideration of the severity of the symptoms, potential for organ damage, and potential responses or side effects to treatment must be weighed. Often the symptoms can be managed with non-steroidal anti-inflammatory drugs (NSAIDs) and hydroxychloroquine for musculoskeletal symptoms or serositis, and calcium channel blockers for Raynaud’s symptoms.
Auto-Antibodies
Characteristics of autoimmune connective tissue diseases generally include the presence of autoantibodies combined with particular clinical characteristics. There is increasing evidence that the development of autoantibodies precedes the clinical manifestations of the disease in question; these autoantibodies are often involved in the disease pathogenesis.8, 9 Researchers have reported numerous clinical correlations or particular patterns of clinical features associated with specific autoantibodies. The presence of a particular autoantibody may not only be frequently associated with a particular disease, but a particular manifestation of that disease. Presence of specific auto antibodies should often raise suspicion and vigilance for particular diseases or patterns of clinical involvement. A complete review of autoantibodies can be found in the article by Moore in this issue of Missouri Medicine on page 140.
Overlap Syndromes
Overlap syndromes are generally defined as meeting criteria for more than one classic autoimmune CTD. Patients may present with evidence of more than one disease simultaneously or they may develop different diseases sequentially. Some patients may exhibit two or more diseases with characteristic serologic markers for those conditions. At times it can be useful to categorize patients based on patterns of clinical features. Over time researchers have studied groups of patients with similar overlap clinical features and identified specific autoantibodies, which have helped further define some overlap syndromes and facilitate disease management.10 Examples of these overlap syndromes and autoantibody associations can be seen in Table 1. A full discussion of these overlap syndromes is beyond the scope of this article; however, one particular overlap, MCTD, will be discussed further.
Table 1.
Specific overlap syndromes and associated auto-antibodies.
| Auto-antibodies | Clinical Features |
|---|---|
| Anti U1-snRNP Ab (MCTD) | SLE+ myositis+ scleroderma+ RA |
| Anti PM-Scl Ab | Myositis + Raynaud’s |
| Anti synthetase Ab (Jo-1 etc) | Myositis + arthritis + interstitial lung disease |
| Anti SSA/B + RF+ anti CCP Ab | RA + Sjogren’s |
Mixed Connective Tissue Disease
MCTD was initially described by Gordon C. Sharp, MD and William S. Irvin, MD during their training at Stanford University.11 Subsequently, both practiced rheumatology in Columbia, Missouri. Dr. Sharp was Chairman of the Division of Immunology and Rheumatology at the University of Missouri for many years. Many of the early long term investigations and follow-up of the patients with MCTD were done at the University of Missouri under his leadership. (See Sidebar on page 66.)
MCTD was originally described as a connective tissue disorder characterized by the presence of high titers of a distinct autoantibody to ribonucleoprotein and clinical features of SLE, systemic sclerosis, and polymyositis. RA was later added to the mix. The autoantibody was later found to be anti-U1 RNP antibody. MCTD was the first overlap syndrome that was defined in terms of association with a specific autoantibody. Whether MCTD should be thought of as a distinct entity or merely a subcategory of a defined connective tissue disease has been a matter of debate; however over time the unique characteristics of these patients have been well delineated and have helped us to better understand a number of overlap syndromes.
Clinical Features
Serologically, the first clue to a diagnosis of MCTD is a very high titer ANA and anti U1-RNP antibodies. Absence of other specific autoantibodies is also important. Antibodies to double-stranded DNA (dsDNA), Sm, and SSA/SSB are occasionally seen as transient phenomenon, but when they are found as the predominant antibody, the clinical course is typically more consistent with SLE.
Although MCTD is an overlap of SLE, scleroderma, myositis, and RA, the overlap of these conditions typically occurs sequentially over time rather than simultaneously. Early in the course of disease, patients may have somewhat nonspecific symptoms such as fatigue, myalgias, arthralgias, and Raynaud’s phenomenon. Often, initially a diagnosis of UCTD is most appropriate given the full clinical picture. The most common clinical associations include hand edema, arthritis, RP, inflammatory muscle disease, and sclerodactyly. A high titer ANA and anti-U1 RNP should alert the clinician to follow the patient closely over time for the development of MCTD.12
Although there are no American College of Rheumatology criteria for the classification of MCTD, several criteria for classification have been published.13 Many clinicians favor the criteria proposed by Alarcon-Segovia and Villarreal 14 based largely on simplicity and general applicability.15 They are shown in Table 2. These criteria incorporate some of the early features seen in MCTD.
Table 2.
Criteria for Classification for Mixed Connective Tissue Disease Alarcon-Segovia and Villarreal
Serologic
|
Clinical Criteria
|
Over time many organ systems may be involved in MCTD.16 Greater than 90% of patients experience arthralgias and 50–60% have arthritis. Rheumatoid factor and anti-CCP antibodies may be positive. As mentioned, myalgias are common and myositis may be seen in up to 70% of patients. There are typically mild muscle enzyme abnormalities. The myopathy typically responds well to corticosteroids and does not remain a prominent feature over time. Histologically the inflammatory myopathy is similar to idiopathic inflammatory myopathies with features of dermatomyositis and polymyositis.
Hematologic abnormalities are often seen in patients. They may have anemia, as well as leukopenia, lymphopenia, and thrombocytopenia. Dryness of the eyes and mouth is also seen. Esophageal dysmotility is common with occasional dysphasia. Pericarditis is the most common type of cardiac involvement. Profound central nervous system involvement is rare, but patients may experience headaches or trigeminal neuralgia. Peripheral nervous system involvement may be seen with polyneuropathy. Renal involvement is also relatively rare. Glomerulonephritis is typically membranous rather than proliferative. Scleroderma-like renal crisis has also been reported.
Dermatologic features may be varied. RP is an early feature in more than 90% of patients. Digital infarcts may be seen as well, in some patients. Sclerodactyly and nail fold vascular changes are also common. Truncal scleroderma is rare. Skin rashes may resemble lupus or dermatomyositis.
Pulmonary symptoms occur in up to 75% of patients. Patients may complain of cough, dyspnea on exertion, or pleuritic chest pain. Physical exam may be unremarkable or may demonstrate basilar rales. Interstitial lung disease may be seen in up to 50% of patients. Pulmonary hypertension is prognostically the most severe form of pulmonary involvement and is the most common disease related cause of death. Pulmonary arterial hypertension in MCTD is usually caused by bland intimal proliferation and medial hypertrophy of pulmonary arterioles, which is the characteristic vascular lesion in this disease. At times the presence of antiphospholipid antibodies in patients also correlates with the development of pulmonary hypertension. Decreased diffusing capacity of the lung for carbon monoxide (DLCO) is a sensitive measure for detecting pulmonary involvement. At times pulmonary involvement may help to distinguish patients with MCTD from those with lupus where pulmonary hypertension is less common.
Management of MCTD
Management of MCTD is compounded by the absence of controlled trials. Recommendations are based on conventional treatments for the specific autoimmune diseases of SLE, myositis, RA and scleroderma. Therapy for specific manifestations is reasonable such as NSAIDs or antimalarial medications for arthralgia, or calcium channel blockers for RP. Recent advances in the treatment of pulmonary hypertension have led to reduced morbidity and mortality. Consideration of the effects of medication on all aspects of a patient’s disease process is prudent in patients with MCTD or any overlap. For example, one should use caution with the use of methotrexate because of the concern for pulmonary toxicity or with the use of TNF inhibitors because of the concern for exacerbation of the SLE activity in a patient. Some symptoms may be responsive to short courses of corticosteroids; however, the long-term use of corticosteroids in these patients is not always appropriate and may lead to premature atherosclerosis or osteoporosis.
Monitoring for development of pulmonary disease is important with regular chest radiographs, annual pulmonary function studies including DLCO, and annual 2-D echocardiogram with Doppler for estimation of systolic pulmonary artery pressure to evaluate for pulmonary hypertension.
Outcome/Prognosis
The initial description of MCTD indicated that the patients had a relatively favorable prognosis with no renal involvement identified. Over time, renal disease has been recognized in some patients, but severe renal disease is uncommon. The prognosis is not generally as favorable as initially perceived however, with pulmonary disease, particularly pulmonary hypertension, contributing to the worst prognosis.
A report of long-term outcome of patients followed at University of Missouri for up to 29 years observed a favorable outcome in 62% of the patients.17 However, 38% had continued active disease or had died. 11 patients had died although two patients had been in a prolonged remission prior to their deaths. Most of the patients who died had pulmonary hypertension. In that study, the most frequent histopathological finding at autopsy was intimal proliferation and medial hypertrophy of arteries. In the lungs, the proliferative vascular lesions occurred with little or no interstitial fibrosis.
In another study from Hungary, 280 patients with MCTD were followed prospectively for up to 15 years.18 Five, Ten, and 15 year survival rates after diagnosis were 98, 96%, and 88% percent respectively. A total of 22 patients’ died. The cause of death was pulmonary arterial hypertension in nine, TTP in three, infection in three, and cardiovascular events in seven.
It is clear that the course of MCTD is varied, and many patients do follow a benign course. However, some patients have increased morbidity and mortality, and the most serious complication is the development of pulmonary hypertension. Identification of patients with or at risk for MCTD is important in order to institute appropriate monitoring and therapy when indicated.
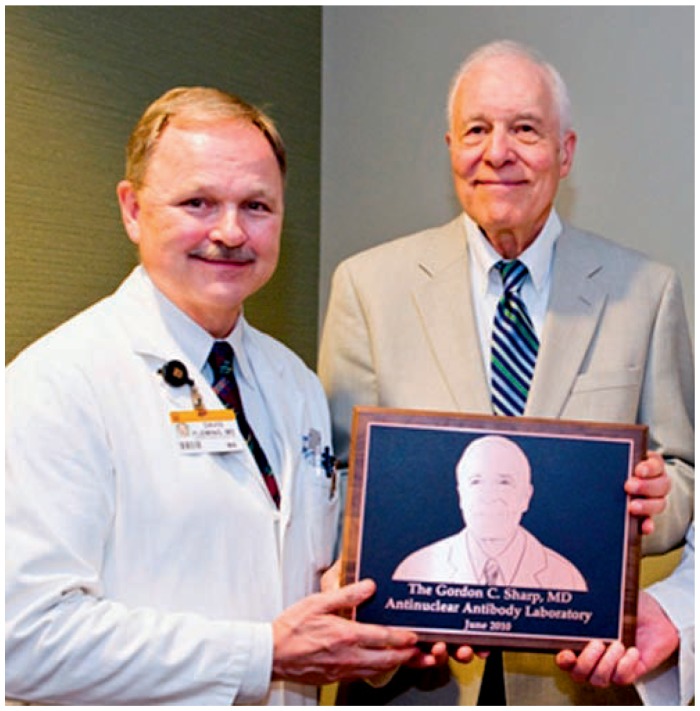
Gordon C. Sharp, MD, did much of the seminal work in MCTD.
The Antinuclear Antibody Laboratory at the University of Missouri School of Medicine was renamed the Gordon C. Sharp ANA Laboratory in a ceremony held on June 7, 2010. Dr. Sharp, Professor Emeritus of Immunology and Rheumatology, founded the ANA laboratory 32 years ago and has served as the laboratory director or co-director until September of 2009.
The ANA laboratory is recognized as one of the best in the nation, receives specimens from across the nation, and has become the repository for thousands of patient serum samples from around the country and beyond, providing a data base that offers research material for many of our faculty and fellows. The information reported by the ANA laboratory has enabled the early detection, definitive diagnosis, treatment, and exclusion of many potentially devastating autoimmune and rheumatic diseases. Dr. Sharp’s vision and leadership has brought this laboratory to a high level of international recognition and esteem among peer institutions. Dr. Sharp has also ensured the laboratory’s excellent reputation by continually updating its test panels as new scientific discoveries are made.
In the photo above, David A. Fleming, MD, Chair, MU Department of Medicine (left), Gordon C. Sharp, MD, MU Emeritus Professor of Immunology & Rheumatology.
Conclusion
The complexity and relative infrequency of autoimmune diseases can contribute to confusion and misunderstanding for non-rheumatology health care providers and patients. When patients exhibit symptoms of more than one condition, the problem may be compounded. Recognition of the existence of overlap syndromes such as MCTD and knowledge of autoantibodies identifying risks for certain clinical manifestations is one step toward a better understanding of these conditions. Additionally recognizing that many patients do not fulfill criteria for a particular autoimmune disease; yet require monitoring for development of a specific disease process or additional features of autoimmunity is important. Prudent therapy to improve outcomes and quality of life for these patients is critical.
Biography
Peri Hickman Pepmueller, MD, is Associate Professor of Internal Medicine and Pediatrics, Division of Rheumatology, Saint Louis University.
Contact: pepmueph@slu.edu

Footnotes
Disclosure
None reported.
References
- 1.LeRoy EC, Maricq HR, Kahaleh MB. Undifferentiated connective tissue syndromes. Arthritis and Rheumatism. 1980;23(3):341–343. doi: 10.1002/art.1780230312. [DOI] [PubMed] [Google Scholar]
- 2.Bodolay E, Csiki Z, Szekanecz Z, Ben T, Kiss E, Zeher M, Szucs G, Danko K, Szegedi G. Five-year follow-up of 665 Hungarian patients with undifferentiated connective tissue disease (UCTD) Clinical and Experimental Rheumatology. 2003;21:313–320. [PubMed] [Google Scholar]
- 3.Williams HJ, Alarcon GS, Joks R, et al. Early undifferentiated connective tissue disease (CTD). Vi. An inception cohort after 10 years: disease remissions and changes in diagnoses in well established and undifferentiated CTD. J Rheumatol. 1999;26:816–825. [PubMed] [Google Scholar]
- 4.Vaz CC, Couto M, Medeiros D, et al. Undifferentiated connective tissue disease: a seven-center cross-sectional study of 184 patients. Clin Rheumatol. 2009;28:915–921. doi: 10.1007/s10067-009-1175-2. [DOI] [PubMed] [Google Scholar]
- 5.Mosca M, Neri R, Bombardieri S. Undifferentiated connective tissue diseases (UCTD): A review of the literature and a proposal for preliminary classification criteria. Clin Exp Rheumatol. 1999;17:615–620. [PubMed] [Google Scholar]
- 6.Mosca M, Tani C, Neri C, Baldini C, Bombardieri S. Undifferentiated connective tissue diseases (UCTD) Autoimmunity Review. 2006;6:1–4. doi: 10.1016/j.autrev.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Conti V, Esposito A, Cagliuso, et al. Undifferentiated connective tissue disease-An unsolved problem: Revision of literature and case studies. International Journal of Immunopathology and Pharmacology. 2010;23(1):271–278. doi: 10.1177/039463201002300125. [DOI] [PubMed] [Google Scholar]
- 8.Arbuckle MR, McClain MT, Rubertone MV, et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med. 2003;349:1526–1533. doi: 10.1056/NEJMoa021933. [DOI] [PubMed] [Google Scholar]
- 9.Shmerling RH. Autoantibodies in systemic lupus erythematosus-there before you know it. N Engl J Med. 2003;349(16):1499–1500. doi: 10.1056/NEJMp038142. [DOI] [PubMed] [Google Scholar]
- 10.Jury EC, D’Cruz D, Morrow WJW. Autoantibodies and overlap syndromes in autoimmune rheumatic disease. J Clin Pathol. 2001;54:340–347. doi: 10.1136/jcp.54.5.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharp GC, Irvin WS, Tan EM, et al. Mixed connective tissue disease: an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA) Am J Med. 1972;52:148–159. doi: 10.1016/0002-9343(72)90064-2. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman RW. Mixed connective tissue disease and overlap syndromes. In: Wallace DJ, Hahn BH, editors. Dubois’ Lupus Erythematosus. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. pp. 975–990. [Google Scholar]
- 13.Amigues JM, Cantagrel A, Abbal M, Mazieres B. Comparative study of 4 diagnosis criteria sets for mixed connective tissue disease in patients with anti-RNP antibodies. J Rheumatol. 1996;23(12):2055–2062. [PubMed] [Google Scholar]
- 14.Alarcon-Segovia D, Villarreal M. Classification and diagnostic criteria for mixed connective tissue disease. In: Kasukawawa R, Sharp GC, editors. Mixed connective tissue disease and anti-nuclear antibodies. Amsterdam: Exerpta Medica; 1987. pp. 33–40. [Google Scholar]
- 15.Bennett R. Overlap syndromes. In: Firestein G, Budd RC, Gabriel SE, McInnes IB, O’Dell JR, editors. Kelley’s Textbook of Rheumatology. 9th ed. Philadelphia, PA: Elsevier Inc; 2013. pp. 1431–1451. [Google Scholar]
- 16.Hoffman RW, Maldonado ME. Immune pathogenesis of mixed connective tissue disease: A short analytical review. Clinical Immunology. 2008;128:8–17. doi: 10.1016/j.clim.2008.03.461. [DOI] [PubMed] [Google Scholar]
- 17.Burdt MA, Hoffman RW, Deutscher SL, Wang GS, Johnson JC, Sharp GC. Long-term outcome in mixed connective tissue disease. Arthritis & Rheumatism. 1999;42(5):899–909. doi: 10.1002/1529-0131(199905)42:5<899::AID-ANR8>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.Hajas A, Szodoray P, Nakken B, Gaal J, et al. Clinical Course, prognosis, and causes of death in mixed connective tissue disease. J Rheumatol. 2013;40(7):1134–1142. doi: 10.3899/jrheum.121272. [DOI] [PubMed] [Google Scholar]