Abstract
The updated 2015 Dietary Guidelines for Americans, published in January 2016, have stirred much controversy since the advisory report first appeared. Several important changes have been made, with some recommendations having greater scientific evidence for their support than others. The focus of this review is to discuss specific recommendations from the 2015 Dietary Guidelines for Americans that lack sound scientific evidence; these include:
Allowing approximately half of all grains to be refined;
The continued recommendations for fat-free or low-fat dairy and limitation of saturated fat intake to <10% of calories;
Sodium intake < 2,300 mg/day; and
Consumption of up to 27 grams/day of “oils” (high in polyunsaturated fat or monounsaturated fat).
Based on our review, the aforementioned recommendations found in the updated 2015 Dietary Guidelines for Americans may increase the incidence of cardiometabolic disease, diabetes, obesity, dyslipidemia, cardiovascular disease, and possibly cancer.
Introduction
The Dietary Guidelines for Americans (DGA) is an extremely important nutritional document that influences the dietary habits of most Americans and can directly impact the health of the nation.1 While lack of randomized controlled trials does not necessarily prohibit the prescribing of certain dietary recommendations, the overall evidence—from populations, observational studies, and clinical trials—must be taken into account to ascertain if each recommendation is scientifically sound. Thus, we reviewed the recommendations in the 2015 DGA and have noted several that not only lack sound scientific evidence but may have unintended consequences, such as promoting the very diseases they are trying to prevent.
Specific recommendations in the 2015 DGA that may increase the incidence of cardiometabolic disease, cardiovascular (CV) disease, and possibly cancer.
“Grains, at Least Half of Which are Whole Grains”
The DGA report defines whole-grains as: whole-wheat bread; oatmeal; whole-grain cereals; popcorn; brown rice and whole-grain pasta. Refined grains are listed as: white bakery goods; bagels; pizza; grain-based desserts; refined cereals (corn flakes, rice cereals); tortillas; white rice and white pasta.2 The 2010 DGA acknowledged that usual whole-grain consumption in the United States (US) met only 15% of the target, while refined grain consumption was nearly twice the goal level.3
Grains are a relatively recent addition to the human diet, added approximately 10,000 years ago with the invention of agriculture. Their integration into the diet allowed human beings to move away from their traditional hunter-gatherer-type eating pattern. Cereal grains as consumed today, whether defined as whole or refined, would not be found in nature and thus humans did not evolve eating such substances. Common sense would advise caution being applied to recommendations to consume more of relatively recent adaptations to the food chain.
As the DGA documented consumption confirms, most grain intake is refined and most grain intake is part of a more broadly processed product, for example pizza, desserts, cookies, and muffins. Refined and whole-grain products tend to be high in added sugar and ingredients generally added during manufacture. Grain-based desserts are the single highest source of calories in American citizens aged two years and older.3 In addition to the harm of added sugar, grains are nutritionally poor when compared with the essential fats, complete protein and micronutrients provided by meat, fish, eggs, vegetables, fruits, nuts and seeds—the diet for which humans are evolutionarily adapted.4
The recommendation to consume grains is ultimately a recommendation to increase the consumption of carbohydrate. Allowing almost half of all grains to be of the more refined type may particularly increase the incidence of cardiometabolic disease, diabetes, and obesity. Indeed, replacing fat with carbohydrate (in most instances refined grains) has been found to increase small-dense low density lipoprotein (LDL).5–7 This results from an increase in triglyceride in very low LDL (VLDL), leading to triglyceride-rich LDL and the formation of small-dense LDL.8 Small-dense LDL does not bind to the liver’s LDL-receptors as well as native LDL and thus remains present in the blood longer, making these LDL particles more susceptible to oxidation. Moreover, small-dense LDL particles are inherently more susceptible to oxidation and penetrate into the sub-endothelium more readily than large buoyant LDL because they are smaller and denser.9 Hence, small-dense LDL are undoubtedly more atherogenic than large buoyant LDL.10 Thus, the consumption of grains, and in particular refined grains in the place of dietary fat may increase the amounts of small-dense LDL shifting the LDL pattern from the less atherogenic type (Pattern A) to one that is more atherogenic (Pattern B). Moreover, if grain replaces dietary fat, this may also lead to an increase in weight gain, fat mass, insulin resistance, a reduction in HDL, and an increase in triglycerides.11–13 Thus, the recommendation to consume grains (whole as well as the more refined type) may increase the incidence of cardiometabolic disease and hence, CV disease.
Summary
The recommendation to consume grains (particularly of the refined type) will likely lead to a decrease in HDL and an increase in triglycerides, small-dense LDL, insulin resistance, obesity, and hence increase the risk of the metabolic syndrome, diabetes, dyslipidemia, obesity, atherosclerosis, and CV disease.
An Alternative Recommendation
Avoid grains and consume instead more natural, nutrient dense foods, such as meat, fish, eggs, vegetables, fruits, nuts, and seeds.
“Choose Fat-free or Low-fat Dairy” and “Consume < 10% of Calories from Saturated Fat”
Numerous clinical trials in humans have either recommended consuming less animal/saturated fat (and hence an increased consumption of fat-free/low-fat dairy) or replacing animal/saturated fat (full-fat dairy for example) with polyunsaturated fat (mainly vegetable oils), which has not led to a reduction in CV disease.13 More importantly, there is no evidence that consuming fat-free or low-fat dairy or reducing the intake of saturated fat in general from clinical trials in humans improves health outcomes.14–16 Moreover, low-fat dairy formulations are generally higher in added sugars and thus this recommendation may lead to an increase in the consumption of added sugars and hence increase CV risk.17
Dietary fat not only provides satiety but also enhances absorption of fat-soluble vitamins.14 The recommendation to consume fat-free or low-fat dairy may increase the risk of deficiencies of fat-soluble vitamins (A, D, E, and K). The low-fat advice beginning in the 1980s was associated with a steep increase in rates of diabetes and obesity in the U.S.13 Hence, the continued advice to consume low-fat dairy and restrict saturated fat intake to < 10% of calories is repeating history but expecting a different outcome. The unintended consequences of eating low-fat dairy or restricting saturated fat intake includes an increase in the intake of refined carbohydrates and sugar (despite a recommendation to restrict the latter to < 10% of total calories). It is illogical to presume that low-fat versions of natural foods (which have had their inherent fat artificially removed) are healthier than their full-fat versions (as they are found in nature). Some populations with exceptional longevity, such as the Sardinians of Italy, do not consume fat-free or low-fat diary but full-fat dairy. The French, have the highest intake of saturated fat in Europe and the lowest rate of CV disease.18 Massai and Samburu warriors, who consume ample amounts of full-fat milk, have much lower rates of hypertension and CV disease compared to the Western world.19,20 The Kitavans, who consume 17% of total energy as saturated fat (from coconuts) appear to have a virtual absence of ischemic heart disease and stroke.21 The body needs to obtain dietary fat from somewhere, and if dairy fat (or saturated fat) is replaced with fat from vegetable oils, this may lead to an increased risk of CV events, CV death, premature mortality, and cancer.13,22 Moreover, low-fat versions of natural foods such as dairy are less satiating and will likely result in an increased total caloric intake throughout the day, increasing the risk of obesity.14
Summary
Reducing the intake of full-fat dairy and saturated fat in general may lead to an increased intake of refined carbohydrate and sugar, and hence may increase the risk of diabetes, obesity, and CV disease. Moreover, reducing the intake of these natural animal fats may increase the risk for fat-soluble vitamin deficiency.
An Alternative Recommendation
Eat natural foods, meat, fish, eggs, dairy products, avocados, nuts and seeds, and the natural fats contained therein.
“Consume Less than 2,300 mg of Sodium per Day”
The Institute of Medicine (IOM) recently reviewed the literature regarding sodium intake relating to CV risk. They concluded that there was no evidence for reducing the intake of sodium to < 2300 mg/day.23 Furthermore, the IOM noted that this recommendation may increase the risk of CV disease/premature mortality. Additionally, there is no evidence from clinical trials that reducing the intake of sodium per se reduces the risk of CV disease. A meta-analysis of prospective cohort studies and randomized clinical trials indicates that restricting sodium intake to less than 2.65 grams per day will likely increase the risk of CV events and all-cause mortality.24 While reducing the intake of sodium may lower blood pressure, the increase in heart rate and adverse changes in counter-regulatory hormone levels more than offsets its supposed benefit.25 When the increases in noradrenaline, adrenaline, renin, angiotensin-II, aldosterone, triglycerides, and cholesterol are taken into account, sodium restriction seems to cause an overall increased CV risk.26 Numerous studies indicate that sodium restriction increases the risk of CV events and total mortality.24,27,28 Sodium intake in animals, just like humans, is determined by need.29 It is illogical to think that conscious sodium restriction is possible, or that it will lead to improved health outcomes. The sodium issue may have arisen from a lack of distinction being made between sodium and the sources of sodium in modern diets. The DGA documents sources of sodium in the American diet in great detail, from soups and condiments to burritos and ready meals.3 Virtually no natural food is reported as a source of sodium. Processed food per se is generally unhealthy; sodium per se is not.
Summary
Reducing the intake of sodium leads to the activation of the renin angiotensin aldosterone system as well as the sympathetic nervous system. These effects seem to outweigh any small reduction in blood pressure.
An Alternative Recommendation
Eat natural foods, meat, fish, eggs, dairy products, nuts and seeds and the natural sodium contained therein.
“Oils High in Polyunsaturated (Omega-6) Fat”
The DGA state, “The recommendation for oils in the Healthy US-Style Eating Pattern at the 2,000-calorie level is 27 g (about 5 teaspoons) per day.”1 “Commonly consumed oils extracted from plants include canola, corn, olive, peanut, safflower, soybean, and sunflower oils.” “The fat in some tropical plants, such as coconut oil, palm kernel oil, and palm oil, are not included in the oils category because they do not resemble other oils in their composition.”
The strongest evidence from meta-analyses of randomized controlled trials suggests that the recommendation to replace saturated fat with omega-6 fat high in linoleic acid (mainly from industrial seed/vegetable oils) will increase the risk of cardiovascular events, cardiovascular death, all-cause mortality.13,22,30 Additionally, the recommendation to consume up to 27 grams per day as vegetable oils may increase the risk of insulin resistance, diabetes, obesity, and cancer.13,31 An increase in vegetable oils (and hence linoleic acid) will likely increase the susceptibility of LDL to oxidation and hence increase atherosclerotic plaque formation and cardiovascular events.32
Vegetable oils were never a part of the diet of early humans. Only in the past century have human beings consumed vegetable oils in any substantial quantity. The increase in the intake of vegetable oils has paralleled the rise in chronic disease in the U.S.33,34 Moreover, we are unaware of any population that is relatively free of heart disease that consumes such high amounts of industrial seed/vegetable oils as recommended by the Dietary Guidelines.
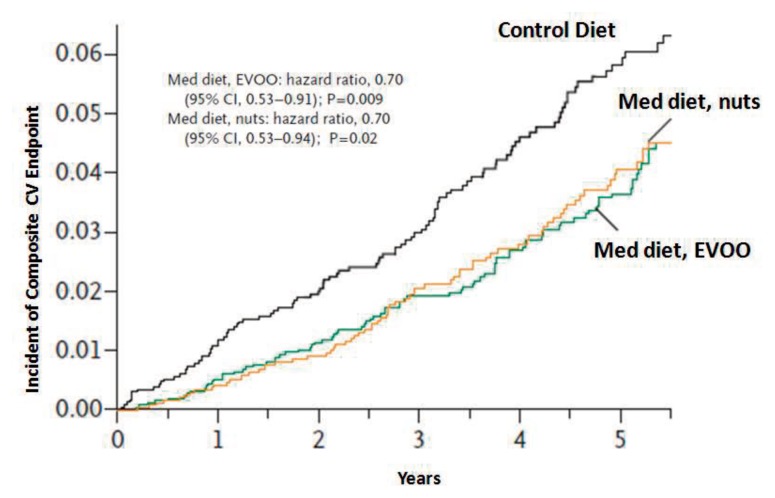
Among the strongest randomized controlled trial evidence available comes from the PREDIMED Study,35 which tested Mediterranean diets (MeDiets) supplemented with either olive oil or nuts, versus a control group assigned to a low-fat American Heart Association (AHA) Diet. The two MeDiets were quite high in total fat (about 40% of total calories) and in the 7,447-patients significantly lowered the primary endpoint (myocardial infarction, stroke, or death from CV causes) by 30% and 28% in the olive oil and nuts arms, respectively compared to the AHA Diet. (See Figure 1) These high-fat MeDiets also reduced the occurrence of new diabetes, atrial fibrillation, breast cancer, cognitive decline, blood pressure, and also slowed progression or induced regression of carotid artery intimal-medial thickness and carotid plaque.36–41 Another MeDiet in a secondary prevention trial led to an approximate 70% reduction in cardiovascular events and all-cause mortality in the secondary prevention Lyon Diet Heart Study.42 MeDiets do not encourage intake of industrial seed oils, which may be related their health benefits.. Table 1 summarizes our recommendations.
Figure 1.
Kaplan-Meier Estimates of the Incidence of Outcome Events in the Total Study Population
The incidence of the primary end-point (a composite of acute myocardial infarction, stroke, and death from CV causes). Hazard radios were stratified according to center (Cox model with robust variance estimators). CI denotes confidence interval, EVOO extra-virgin olive oil, and Med Mediterranean.
Table 1.
Summary of recommendations in the 2015 DGA that may increase the incidence of cardiometabolic disease, diabetes, obesity, dyslipidemia, CV disease and cancer.
| RECOMMENDATION | REPLACE WITH | REASONING |
|---|---|---|
| “Grains, at least half of which are whole grains” | Avoid grains and consume instead more natural, nutrient dense foods, such as meat, fish, eggs, vegetables, nuts and seeds. | The recommendation to consume refined grains will likely lead to an increase in triglycerides, small-dense LDL, insulin resistance, fat mass and reduce HDL, hence increase the risk of the metabolic syndrome, diabetes, dyslipidemia, obesity, atherosclerosis, and CV events. |
| “Consume fat-free or low-fat dairy” and “< 10% of calories from saturated fat” | Eat natural foods, meat, fish, eggs, dairy products, nuts and seeds and the natural fats contained therein. | Reducing the intake of full-fat dairy and saturated fat may increase the intake of refined carbohydrates and sugar, hence may increase the risk of CV disease. Moreover, reducing the intake of these natural animal fats may increase the risk for fat-soluble vitamin deficiency and obesity. |
| “Consume less than 2,300 mg of sodium per day” | Eat natural foods, meat, fish, eggs, dairy products, nuts and seeds and the natural sodium contained therein | Restricting the intake of sodium to < 2,300 mg/day will likely increase the risk of CV events and all-cause mortality. |
| Oils high in polyunsaturated (omega-6) fat | Eat natural foods, meat, fish, eggs, dairy products, and seeds and the natural saturated and unsaturated fats contained therein. | The recommendation to replace saturated fat with industrial seeds oils will likely increase the risk of CV events, CV death, mortality, and cancer. |
Summary
The recommendation to consume up to 27 grams per day of industrial seed/vegetable oils should instead be specifically recommending increased intake of olive oil and nuts, particularly in the context of a traditional MeDiet that is high in vegetables and fish, and low in processed foods, refined carbohydrates, and added sugars.
An Alternative Recommendation
Eat natural foods, meat, fish, eggs, dairy products, and seeds and the natural saturated and unsaturated fats contained therein.
Conclusion
Several recommendations in the 2015 DGA lack sound scientific evidence. The recommendations discussed in this review, such as the consumption of grains, low-fat dairy, saturated fat intake < 10% total calories, sodium < 2,300 mg/day, and industrial seed/vegetable oils up to 27 grams per day, may lead to unintended consequences such as an increased incidence of cardiometabolic disease, diabetes, obesity, dyslipidemia, CV disease, and cancer. The DGA have, once more, missed the opportunity to deliver a simple, memorable, effective dietary message to Americans: eat natural food and avoid processed food.
Biography
James J. DiNicolantonio, PharmD, (left), and James H. O’Keefe, MD, (right), MSMA member since 2003, are at Saint Luke’s Mid America Heart Institute, Kansas City, Missouri. Zoë Harcombe, PhD, is at the Institute of Clinical Exercise and Health Science, University of the West of Scotland.
Contact: jjdinicol@gmail.com
Footnotes
Disclosure
ZH receives income from writing about diet and nutrition.
References
- 1.Government U; Agriculture UDoHaHSaUDo, editor. 2015–2020 Dietary Guidelines for Americans. US Department of Health and Human Service and US Department of Agriculture; 2015. http://health.gov/dietaryguidelines/2015/guidelines/ [Google Scholar]
- 2.Government U; Services UDoHaH, editor. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. US Department of Health and Human Services; 2015. http://health.gov/dietaryguidelines/2015-scientific-report/ [Google Scholar]
- 3.Government U; Services DoHaH, editor. Dietary Guidelines for Americans. Department of Health and Human Services; 2010. 2010. http://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf. [Google Scholar]
- 4.Harcombe Z, Baker JS, Davies B. Food for Thought: Have We Been Giving the Wrong Dietary Advice? Food and Nutrition Sciences. 2013;4:240–244. [Google Scholar]
- 5.Volek JS, Fernandez ML, Feinman RD, Phinney SD. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog Lipid Res. 2008;47:307–318. doi: 10.1016/j.plipres.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM, Kraemer WJ, Feinman RD, Volek JS. Comparison of low fat and low carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids. 2008;43:65–77. doi: 10.1007/s11745-007-3132-7. [DOI] [PubMed] [Google Scholar]
- 7.Krauss RM, Dreon DM. Low-density-lipoprotein subclasses and response to a low-fat diet in healthy men. Am J Clin Nutr. 1995;62:478S–487S. doi: 10.1093/ajcn/62.2.478S. [DOI] [PubMed] [Google Scholar]
- 8.Mittendorfer B, Sidossis LS. Mechanism for the increase in plasma triacylglycerol concentrations after consumption of short-term, high-carbohydrate diets. Am J Clin Nutr. 2001;73:892–899. doi: 10.1093/ajcn/73.5.892. [DOI] [PubMed] [Google Scholar]
- 9.Chait A, Brazg RL, Tribble DL, Krauss RM. Susceptibility of small, dense, low-density lipoproteins to oxidative modification in subjects with the atherogenic lipoprotein phenotype, pattern B. Am J Med. 1993;94:350–356. doi: 10.1016/0002-9343(93)90144-e. [DOI] [PubMed] [Google Scholar]
- 10.Superko HR, Gadesam RR. Is it LDL particle size or number that correlates with risk for cardiovascular disease? Curr Atheroscler Rep. 2008;10:377–385. doi: 10.1007/s11883-008-0059-2. [DOI] [PubMed] [Google Scholar]
- 11.Bazzano LA, Hu T, Reynolds K, Yao L, Bunol C, Liu Y, Chen CS, Klag MJ, Whelton PK, He J. Effects of low-carbohydrate and low-fat diets: a randomized trial. Ann Intern Med. 2014;161:309–318. doi: 10.7326/M14-0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu T, Mills KT, Yao L, Demanelis K, Eloustaz M, Yancy WS, Jr, Kelly TN, He J, Bazzano LA. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am J Epidemiol. 2012;176:S44–54. doi: 10.1093/aje/kws264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiNicolantonio JJ. The cardiometabolic consequences of replacing saturated fats with carbohydrates or Omega-6 polyunsaturated fats: Do the dietary guidelines have it wrong? Open Heart. 2014;1:e000032. doi: 10.1136/openhrt-2013-000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lucan SC, DiNicolantonio JJ. How calorie-focused thinking about obesity and related diseases may mislead and harm public health. An alternative. Public Health Nutr. 2014;18:571–581. doi: 10.1017/S1368980014002559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiNicolantonio JJ, Lucan SC, O’Keefe JH. The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease. Prog Cardiovasc Dis. 2015 doi: 10.1016/j.pcad.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harcombe Z, Baker JS, Cooper SM, Davies B, Sculthorpe N, DiNicolantonio JJ, Grace F. Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart. 2015;2:e000196. doi: 10.1136/openhrt-2014-000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DiNicolantonio JJ, Lucan SC. The wrong white crystals: not salt but sugar as aetiological in hypertension and cardiometabolic disease. Open Heart. 2014;1:e000167. doi: 10.1136/openhrt-2014-000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allender S, Scarborough P, Peto V, Rayner M, Leal J, Luengo-Fernandez R, Gray A. Group BHFHDR, editor. European cardiovascular disease statistics. European Union Heart Network; 2008. p. 112. [Google Scholar]
- 19.Gleibermann L. Blood pressure and dietary salt in human populations. Ecol Food Nutr. 1973;2:143–156. [Google Scholar]
- 20.Mann GV, Shaffer RD, Anderson RS, Sandstead HH. Cardiovascular Disease in the Masai. J Atheroscler Res. 1964;4:289–312. doi: 10.1016/s0368-1319(64)80041-7. [DOI] [PubMed] [Google Scholar]
- 21.Lindeberg S, Nilsson-Ehle P, Vessby B. Lipoprotein composition and serum cholesterol ester fatty acids in nonwesternized Melanesians. Lipids. 1996;31:153–158. doi: 10.1007/BF02522614. [DOI] [PubMed] [Google Scholar]
- 22.Ramsden CE, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, Ringel A, Davis JM, Hibbeln JR. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346:e8707. doi: 10.1136/bmj.e8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strom B, Anderson CAM, Ard J, Cook N, Box MK, Graudal N, He J, Ix J, Kimmel S, Lichtenstein A, Weinberger M. Sodium Intake in Populations: Assessment of Evidence. Nat Acad Sci. 2013. May, pp. 1–4. http://iom.nationalacademies.org/~/media/Files/Report%20Files/2013/Sodium-Intake-Populations/SodiumIntakeinPopulations_RB.pdf.
- 24.Graudal N, Jurgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a metaanalysis. Am J Hypertens. 2014;27:1129–1137. doi: 10.1093/ajh/hpu028. [DOI] [PubMed] [Google Scholar]
- 25.Folkow B, Ely D. Importance of the blood pressure-heart rate relationship. Blood Press. 1998;7:133–138. doi: 10.1080/080370598437321. [DOI] [PubMed] [Google Scholar]
- 26.Graudal NA, Galloe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride: a meta-analysis. JAMA. 1998;279:1383–1391. doi: 10.1001/jama.279.17.1383. [DOI] [PubMed] [Google Scholar]
- 27.O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, Yan H, Lee SF, Mony P, Devanath A, Rosengren A, Lopez-Jaramillo P, Diaz R, Avezum A, Lanas F, Yusoff K, Iqbal R, Ilow R, Mohammadifard N, Gulec S, Yusufali AH, Kruger L, Yusuf R, Chifamba J, Kabali C, Dagenais G, Lear SA, Teo K, Yusuf S. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 28.DiNicolantonio JJ, Niazi AK, Sadaf R, JHOK, Lucan SC, Lavie CJ. Dietary sodium restriction: take it with a grain of salt. Am J Med. 2013;126:951–955. doi: 10.1016/j.amjmed.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 29.Ghooi RB, Valanju VV, Rajarshi MG. Salt restriction in hypertension. Med Hypotheses. 1993;41:137–140. doi: 10.1016/0306-9877(93)90060-4. [DOI] [PubMed] [Google Scholar]
- 30.Ramsden CE, Hibbeln JR, Majchrzak SF, Davis JM. n-6 fatty acid-specific and mixed polyunsaturate dietary interventions have different effects on CHD risk: a meta-analysis of randomised controlled trials. Br J Nutr. 2010;104:1586–1600. doi: 10.1017/S0007114510004010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DiNicolantonio JJ, Lucan SC. Could So-Called ‘Healthy’ Vegetable And Seed Oils Be Making Us Fat And Sick? 2015. http://www.forbes.com/sites/realspin/2015/09/29/could-so-called-healthy-vegetable-and-seed-oils-be-making-us-fat-and-sick/#5024d0596753Forbes.
- 32.Reaven P, Parthasarathy S, Grasse BJ, Miller E, Steinberg D, Witztum JL. Effects of oleate-rich and linoleate-rich diets on the susceptibility of low density lipoprotein to oxidative modification in mildly hypercholesterolemic subjects. J Clin Invest. 1993;91:668–676. doi: 10.1172/JCI116247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ravnskov U, DiNicolantonio JJ, Harcombe Z, Kummerow FA, Okuyama H, Worm N. The questionable benefits of exchanging saturated fat with polyunsaturated fat. Mayo Clin Proc. 2014;89:451–453. doi: 10.1016/j.mayocp.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 34.Blasbalg TL, Hibbeln JR, Ramsden CE, Majchrzak SF, Rawlings RR. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am J Clin Nutr. 2011;93:950–962. doi: 10.3945/ajcn.110.006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pinto X, Basora J, Munoz MA, Sorli JV, Martinez JA, Martinez-Gonzalez MA. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 36.Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, Corella D, Salas-Salvado J, Ruiz-Gutierrez V, Lamuela-Raventos RM, Toledo E, Estruch R, Coca A, Ros E. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64:69–76. doi: 10.1161/HYPERTENSIONAHA.113.03353. [DOI] [PubMed] [Google Scholar]
- 37.Martinez-Gonzalez MA, Toledo E, Aros F, Fiol M, Corella D, Salas-Salvado J, Ros E, Covas MI, Fernandez-Crehuet J, Lapetra J, Munoz MA, Fito M, Serra-Majem L, Pinto X, Lamuela-Raventos RM, Sorli JV, Babio N, Buil-Cosiales P, Ruiz-Gutierrez V, Estruch R, Alonso A. Extra virgin olive oil consumption reduces risk of atrial fibrillation: the PREDIMED (Prevencion con Dieta Mediterranea) trial. Circulation. 2014;130:18–26. doi: 10.1161/CIRCULATIONAHA.113.006921. [DOI] [PubMed] [Google Scholar]
- 38.Salas-Salvado J, Bullo M, Estruch R, Ros E, Covas MI, Ibarrola-Jurado N, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Romaguera D, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pinto X, Basora J, Munoz MA, Sorli JV, Martinez-Gonzalez MA. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med. 2014;160:1–10. doi: 10.7326/M13-1725. [DOI] [PubMed] [Google Scholar]
- 39.Sala-Vila A, Romero-Mamani ES, Gilabert R, Nunez I, de la Torre R, Corella D, Ruiz-Gutierrez V, Lopez-Sabater MC, Pinto X, Rekondo J, Martinez-Gonzalez MA, Estruch R, Ros E. Changes in ultrasound-assessed carotid intima-media thickness and plaque with a Mediterranean diet: a substudy of the PREDIMED trial. Arterioscler Thromb Vasc Biol. 2014;34:439–445. doi: 10.1161/ATVBAHA.113.302327. [DOI] [PubMed] [Google Scholar]
- 40.Toledo E, Salas-Salvado J, Donat-Vargas C, Buil-Cosiales P, Estruch R, Ros E, Corella D, Fito M, Hu FB, Aros F, Gomez-Gracia E, Romaguera D, Ortega-Calvo M, Serra-Majem L, Pinto X, Schroder H, Basora J, Sorli JV, Bullo M, Serra-Mir M, Martinez-Gonzalez MA. Mediterranean Diet and Invasive Breast Cancer Risk Among Women at High Cardiovascular Risk in the PREDIMED Trial: A Randomized Clinical Trial. JAMA Intern Med. 2015;175:1752–1760. doi: 10.1001/jamainternmed.2015.4838. [DOI] [PubMed] [Google Scholar]
- 41.Valls-Pedret C, Sala-Vila A, Serra-Mir M, Corella D, de la Torre R, Martinez-Gonzalez MA, Martinez-Lapiscina EH, Fito M, Perez-Heras A, Salas-Salvado J, Estruch R, Ros E. Mediterranean Diet and Age-Related Cognitive Decline: A Randomized Clinical Trial. JAMA Intern Med. 2015;175:1094–1103. doi: 10.1001/jamainternmed.2015.1668. [DOI] [PubMed] [Google Scholar]
- 42.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]