Abstract
Introduction:
Maternal health during pregnancy plays a part in child health, and several conditions have been associated with adverse child outcomes.
Objectives:
To determine the socioeconomic determinants and maternal health factors associated with dental caries in young children.
Methods:
This cross-sectional study is part of a register-based cohort study including all children who were born from 2000 to 2003 and were residing in Stockholm County, Sweden, at age 3 y (n = 73,658). The study followed the cohort until individuals were 7 y old. The final study cohort comprised all children examined at 3 and 7 y (n = 65,259). Data on socioeconomic conditions, maternal health, and maternal health behavior were extracted from Swedish national registries. The multivariate analyses used 2 outcomes: caries experience at age 3 and 7 y (deft > 0 [decayed, extracted, and filled teeth]).
Results:
The results of this study show that socioeconomic and maternal health behaviors during pregnancy are important determinants of oral health in their preschool offspring. When all significant risk factors were present, the cumulative probability of being diagnosed with dental caries at age 7 y was 75%.
Conclusion:
This study also showed that maternal obesity and smoking during pregnancy were predictors of dental caries in preschool children. Strategies must be developed for increasing maternal motivation and self-efficacy and providing mothers with knowledge and caries-preventive tools.
Knowledge Transfer Statement:
The results of this study inform clinicians about the importance of including a more detailed history regarding maternal health and maternal health behaviors during pregnancy to assess caries risk in preschool children. Education, income, and other socioeconomic factors are difficult to modify in the short term. Therefore, strategies must be developed to increase parental motivation and self-efficacy to give parents the determination, knowledge, and tools for prevention.
Keywords: dental health survey, lifestyle, pediatrics, health services research, risk factor, epidemiology
Introduction
Dental caries is still a significant public health problem and a major contributor to poor general health among children (Bagramian et al. 2009). The prevalence of dental caries in primary schoolchildren is 5 times higher than that of asthma, the next-most common chronic health condition of children (Dye et al. 2007). In many countries, multiple dental extractions are the most common reason for children receiving general anesthesia (Armfield et al. 2006).
Evidence shows that only a small proportion of children in a population bear the major burden of disease and that socioeconomic and lifestyle factors are important determinants of dental caries (Watanabe et al. 2014). This gradient in health outcomes endures from infancy to adulthood (Starfield et al. 2002). It is problematic that recent studies showed that caries prevention in high-risk groups is not effective (Anderson et al. 2016; Braun et al. 2016).
Maternal health during pregnancy is important for child health. Several maternal health conditions have been associated with a variety of adverse child outcomes. Maternal obesity was linked to autism spectrum disorders (Li et al. 2016) and cerebral palsy (Villamor et al. 2017). Maternal smoking during pregnancy was linked to adverse physical, behavioral, and cognitive child health outcomes (Zhou et al. 2014). In a register-based study, Julihn et al. (2009) reported that mothers being overweight (body mass index >25) and mothers smoking during pregnancy were significantly associated with a high proximal caries increment in their offspring during the teenage period (Julihn et al. 2009). Mothers who were overweight (Wigen and Wang 2011), who smoked during pregnancy, and who were exposed to postnatal household smoking were all linked to caries development in preschool children (Tanaka et al. 2015).
This register-based study comprised a cohort >65,000 children followed from 3 to 7 y of age for whom caries data are linked to available national registers and focused on socioeconomic factors, maternal health, and maternal health behaviors during pregnancy. We hypothesized that mothers’ socioeconomic disadvantage, poor health, and poor health behaviors would be significantly associated with dental caries in their offspring.
Materials and Methods
Study Population
This cross-sectional study was part of a register-based cohort study with dental caries–related data of children followed from 3 y to 7 y of age. Data came from the Public Health Care Administration in Stockholm, as well as from the national registers at the National Board of Health and Welfare and Statistics Sweden. The unique Swedish personal identity number was used to link this cohort to multiple health care and administrative registers, and linkage was performed by the board. Linkage was possible for all children with dental data and a personal identity number. The complete methodology was previously published (Brandquist et al. 2017), so we present only variables of interest for this study. The methods employed in this study are consistent with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for a human observational study.
Children born from 2000 to 2003 who resided in Stockholm County, Sweden, were eligible for inclusion. Initially examined at 3 y of age, the children were followed until 7 y of age. The subjects received regular dental check-ups at the Public Dental Service, with private practitioners, or at the Karolinska Institutet (Division of Pediatric Dentistry, Department of Dental Medicine). For cross-sectional study at 3 y of age, 73,658 children were included. For cross-sectional study at 7 y of age, 65,259 children were included (33,423 boys and 31,836 girls). The Regional Ethics Board in Stockholm and the Swedish Data Inspection Board, a national agency that serves as an institutional review board for studies using database linkage, approved the protocol for this study (Daybook 2010/1563-31/1).
Variables
We collected data on manifest caries lesions from clinical and radiographic examinations. The registration sheets for the 3- and 7-y-old children comprised the following caries indices: dt = decayed teeth, et = extracted teeth, and ft = filled teeth. Decayed teeth were defined as caries on smooth surfaces at the lowest level that can be verified as a cavity and detectable by probing or, in fissures, by a catch of the probe under slight pressure. Proximal manifest caries was diagnosed on bite-wing radiographs and defined as a lesion clearly extending into the dentin (Koch 1967). Not all children had a radiographic examination at a specific age, only those for whom it was indicated. Indications for bite-wing radiographs are mainly previous caries experience of several caries risk factors present. The decayed, extracted, and filled primary teeth (deft) index measured the severity of the caries experience in children at 3 and 7 y of age. We dichotomized the dependent variable as caries free (deft = 0) and caries experience (deft >0). No permanent teeth were included in data collection.
The Swedish National Board of Health and Welfare maintains the Swedish Medical Birth Register (MBR). We collected the following variables from the MBR: maternal age (25 to 34, <25, >34 y), marital status (cohabiting parents, single), maternal smoking habits during early pregnancy (no, yes), and the mother’s height and weight at the first visit to the public maternity health care clinic. The body mass index of the mother was calculated and classified as <25 or ≥25.
Statistics Sweden maintains the Total Population Register. From this register, we collected data on the mother’s number of children as well as country of birth and analyzed the latter in the statistical analyses as “mother born in well-developed countries” (North America, Nordic, Oceania, Western Europe, Soviet Union, Sweden, Southern Europe, Korea) or “mother born in underdeveloped countries” (Africa, India, China, other Asia, South America, Eastern Europe, Vietnam; Urquia et al. 2015). The Swedish National Tax Board sends summary statistics to Statistics Sweden, and from this register, we collected information regarding the family’s disposable income from the 2003 survey. Family income was divided into quintiles, with the highest-income quintile as reference. Family income included all reported sources of income from which taxes were deducted; thereafter, it was divided by consumer units in the household according to a formula developed by Statistics Sweden.
We obtained data on maternal education level from the Register of Education, which is updated each year in April. In the statistical analysis, we classified the variable “education level” according to the number of years of schooling in 2003: low (≤9 y), intermediate (10 to 12 y), and high (>12 y).
Information about maternal diseases before and during pregnancy came from the National Patient Register and MBR. These registers collect information regarding inpatient care and outpatient visits from private and public caregivers in Sweden. Diseases were classified according ICD-10 codes (10th Revision of the International Statistical Classification of Diseases and Related Health Problems; http://www.socialstyrelsen.se/klassificeringochkoder/diagnoskodericd-10). We included all ICD-10 diagnoses from A00-O9A: some infectious and parasitic diseases; neoplasms (tumors); diseases of the blood and the hematopoietic organs and some immune disorders; endocrine, nutritional and metabolic diseases; mental and behavioral disorders; diseases of the nervous system; diseases of the eye and attachments; diseases of the ear and the mastoid process; diseases of the circulatory system; diseases of the respiratory tract; diseases of the digestive system; skin and subcutaneous tissue disorders; osteomuscular and connective tissue diseases; diseases of the genitourinary system and pregnancy, childbirth and the puerperium. Mothers diagnosed with ≥1 disease were characterized as not healthy.
Statistical Analysis
Data management and statistical analyses were performed with SPSS 22.0 (IBM) and STATA 14.0 (StataCorp LP). Data analysis employed frequency tables for description and assessed differences among categorical variables with a chi-square test.
Forward stepwise binary logistic regression analyzed the predictors of caries experience among 3- and 7-y-old children. We dichotomized the dependent variable as caries free and caries experience at 3 or 7 y of age. The univariate logistic regression model (crude) included as independent variables all those with a P value <0.05 in the chi-square test; for the regression model, we considered odds ratios (ORs) with 95% CIs and all P values <0.05 to be significant, based on 2-tailed tests. In the bivariate logistic regression model (adjusted), we tested 3 models: model 1, which included only the block of socioeconomic variables; model 2, which included only the block of maternal health variables; and model 3, in which both blocks were tested simultaneously. The factors that remained statistically significant in the multivariate analysis were the factors that simultaneously best explained the dependent variable. We used the fitted model 3 to estimate the impact of risk factors and calculated cumulative risk based on the logistic regression analysis.
Results
The data in this study came from children who underwent dental examinations at 3 and 7 y old. The sample consisted of 65,259 children. Table 1 shows the characteristics of the study participants.
Table 1.
Characteristics of the Study Population.
| Variables | n | % |
|---|---|---|
| Family income (quintile) | ||
| 1st (lowest) | 14,599 | 20 |
| 2nd | 14,636 | 20 |
| 3rd | 14,613 | 20 |
| 4th | 14,612 | 20 |
| 5th (highest) | 14,607 | 20 |
| Maternal country at birth | ||
| Well developed | 59,633 | 81 |
| Underdeveloped | 14,025 | 19 |
| Parity | ||
| 1 child | 34,377 | 47 |
| ≥2 children | 39,281 | 53 |
| Maternal education level, y | ||
| ≤9 | 6,747 | 9 |
| 10 to 12 | 28,929 | 40 |
| ≥13 | 37,537 | 51 |
| Marital status | ||
| Cohabiting parents | 58,915 | 80 |
| Single | 14,743 | 20 |
| Maternal age at delivery, y | ||
| <25 | 10,551 | 14 |
| 25 to 34 | 45,741 | 62 |
| >34 | 17,366 | 24 |
| Smoking during pregnancy | ||
| No | 60,535 | 92 |
| Yes | 5,336 | 8 |
| Obesity | ||
| No | 55,100 | 93 |
| Yes | 4,388 | 7 |
| Maternal health condition | ||
| Healthy | 63,209 | 87 |
| Not healthy | 9,849 | 13 |
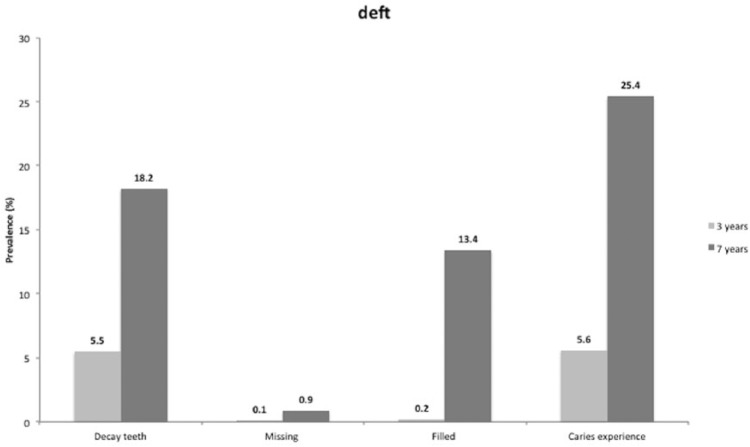
As Figure 1 shows, 5.5% of the children had caries lesions at age 3 y, increasing to 18% at age 7 y.
Figure 1.
Decayed, extracted, and filled teeth in children at 3 and 7 y of age.
We classified variables into 2 main groups: socioeconomic factors and maternal health behaviors. In a univariate analysis, we evaluated the association between “dental caries experience” and the various independent variables. The analysis showed associations between each variable studied and caries experience (deft > 0) at 3 and 7 y of age (Appendix Table). In a comparison of childhood caries prevalence based on the various studied variables, mothers having children with caries at 3 y of age were younger (9% caries prevalence vs. 5%), born in a low-income country (6% vs. 3%), had >1 child (7% vs. 4%), had low family income (11% vs. 3%), smoked during pregnancy (10% vs. 5%), were obese (9% vs. 5%), and were more likely to have a diagnosed health condition (6% vs. 5%).
Tables 2 and 3 present the results of multivariate logistic regression analyses at ages 3 and 7 y, respectively. Based on univariate logistic regression, all variables were included in the adjusted model for predicting caries experience at 3 and 7 y of age.
Table 2.
Multivariate Analysis Based on Logistic Regression of Variables Associated with Caries Experience in Children Aged 3 y (dmft).
| Crude Model | Adjusted Model 1a | Adjusted Model 2b | Adjusted Model 3c | |||||
|---|---|---|---|---|---|---|---|---|
| Variable: Category | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value |
| Family income (quintile) | ||||||||
| 1st (lowest) | 4.43(3.93 to 4.98) | <0.001 | 1.98(1.71 to 2.38) | <0.001 | 1.95(1.72 to 2.34) | <0.001 | ||
| 2nd | 2.21(1.95 to 2.51) | <0.001 | 1.43(1.28 to 1.63) | <0.001 | 1.50(1.33 to 1.74) | <0.001 | ||
| 3rd | 1.63(1.42 to 1.86) | <0.001 | 1.22(1.06 to 1.44) | 0.004 | 1.25(1.12 to 1.53) | 0.005 | ||
| 4th | 1.43(1.25 to 1.64) | <0.001 | 1.25(1.11 to 1.44) | 0.001 | 1.28(1.11 to 1.53) | 0.002 | ||
| 5th (highest) | 1 | 1 | 1 | |||||
| Maternal country at birth | ||||||||
| Well developed | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Underdeveloped | 5.02(4.69 to 5.38) | 3.38(3.13 to 3.63) | 3.36(3.10 to 3.72) | |||||
| Parity | ||||||||
| 1 child | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| ≥2 children | 1.67(1.56 to 1.79) | 1.43(1.33 to 1.53) | 1.47(1.31 to 1.63) | |||||
| Maternal education level, y | ||||||||
| ≤9 | 4.56(4.15 to 5.00) | <0.001 | 1.99(1.79 to 2.22) | <0.001 | 1.78(1.64 to 2.01) | <0.001 | ||
| 10 to 12 | 1.86(4.15 to 5.01) | <0.001 | 1.45(1.32 to 1.61) | <0.001 | 1.39(1.31 to 1.52) | <0.001 | ||
| ≥13 | 1 | 1 | 1 | |||||
| Marital status | ||||||||
| Cohabiting parents | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Single | 1.65(1.53 to 1.78) | 1.55(1.42 to 1.71) | 1.42(1.34 to 1.62) | |||||
| Maternal age at delivery, y | ||||||||
| 25 to 34 | 1 | 1 | 1 | |||||
| <25 | 2.06(1.89 to 2.24) | <0.001 | 1.92(1.75 to 2.12) | <0.001 | 1.30(1.23 to 1.51) | <0.001 | ||
| >34 | 1.26(1.16 to 1.36) | <0.001 | 1.26(1.15 to 1.38) | <0.001 | 1.27(1.17 to 1.38) | <0.001 | ||
| Smoking during pregnancy | ||||||||
| No | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Yes | 1.94(1.75 to 2.16) | 1.67(1.49 to 1.88) | 1.58(1.39 to 1.79) | |||||
| Obesity | ||||||||
| No | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Yes | 1.77(1.57 to 1.99) | 1.70(1.50 to 1.91) | 1.28(1.13 to 1.45) | |||||
| Maternal health condition | ||||||||
| Healthy | 1 | 0.008 | 1 | 0.140 | 1 | 0.497 | ||
| Not healthy | 1.13(1.03 to 1.25) | 1.08(0.97 to 1.20) | 0.96(0.87 to 1.08) | |||||
Bold indicates P < 0.05.
OR, odds ratio.
Model 1: sociodemographic factors.
Model 2: maternal health factors.
Model 3: sociodemographic factors + maternal health factors.
Table 3.
Multivariate Analysis Based on Logistic Regression of Variables Associated with Caries Experience in Children Aged 7 y (dmft).
| Crude Model | Adjusted Model 1a | Adjusted Model 2b | Adjusted Model 3c | |||||
|---|---|---|---|---|---|---|---|---|
| Variable: Category | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value |
| Family income (quintile) | ||||||||
| 1st (lowest) | 3.44(3.26 to 3.64) | <0.001 | 1.82(1.72 to 1.92) | <0.001 | 1.73(1.65 to 1.80) | <0.001 | ||
| 2nd | 1.89(1.79 to 2.00) | <0.001 | 1.34(1.29 to 1.45) | <0.001 | 1.27(1.21 to 1.38) | <0.001 | ||
| 3rd | 1.45(1.37 to 1.54) | <0.001 | 1.17(1.14 to 1.23) | <0.001 | 1.15(1.10 to 1.23) | <0.001 | ||
| 4th | 1.19(1.12 to 1.26) | <0.001 | 1.07(1.01 to 1.13) | 0.034 | 1.04(0.98 to 1.13) | 0.212 | ||
| 5th (highest) | 1 | 1 | 1 | |||||
| Maternal country at birth | ||||||||
| Well developed | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Underdeveloped | 4.12(4.00 to 4.30) | 2.89(2.80 to 3.01) | 2.96(2.82 to 3.15) | |||||
| Parity | ||||||||
| 1 child | 1 | <0.001 | 1 | 1 | <0.001 | |||
| ≥2 children | 1.52(1.47 to 1.57) | 1.37(1.32 to 1.43) | <0.001 | 1.45(1.41 to 1.54) | ||||
| Maternal education level, y | ||||||||
| ≤9 | 4.22(3.99 to 4.45) | <0.001 | 2.22(2.13 to 2.32) | <0.001 | 1.85(1.71 to 2.16) | <0.001 | ||
| 10 to 12 | 1.79(1.72 to 1.85) | <0.001 | 1.49(1.43 to 1.50) | <0.001 | 1.38(1.33 to 1.41) | <0.001 | ||
| ≥13 | 1 | 1 | 1 | |||||
| Marital status | ||||||||
| Cohabiting parents | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Single | 1.57(1.51 to 1.63) | 1.46(1.40 to 1.51) | 1.37(1.31 to 1.42) | |||||
| Maternal age at delivery, y | ||||||||
| 25 to 34 | 1 | 1 | 1 | |||||
| <25 | 2.13(2.04 to 2.23) | <0.001 | 1.99(1.89 to 2.01) | <0.001 | 1.41(1.31 to 1.53) | <0.001 | ||
| >34 | 1.12(1.07 to 1.17) | <0.001 | 1.11(1.06 to 1.17) | <0.001 | 1.17(1.06 to 1.16) | <0.001 | ||
| Smoking during pregnancy | ||||||||
| No | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Yes | 2.01(1.90 to 2.13) | 1.73(1.63 to 1.85) | 1.56(1.42 to 1.63) | |||||
| Obesity | ||||||||
| No | 1 | <0.001 | 1 | <0.001 | 1 | <0.001 | ||
| Yes | 1.58(1.48 to 1.69) | 1.52(1.42 to 1.63) | 1.18(1.12 to 1.31) | |||||
| Maternal health condition | ||||||||
| Healthy | 1 | 0.005 | 1 | 0.420 | 1 | 0.440 | ||
| Not healthy | 1.07(1.02 to 1.12) | 1.02(0.97 to 1.08) | 0.92(0.94 to 1.09) | |||||
Bold indicates P < 0.05.
OR, odds ratio.
Model 1: sociodemographic factors.
Model 2: maternal health factors.
Model 3: sociodemographic factors + maternal health factors.
With regard to socioeconomic factors, model 3 found that children of mothers born in low-income countries had a higher risk of having a child with caries experience at 3 y (OR, 3.4) and 7 y (OR, 3.0) of age. As compared with the mothers in the highest quintile, those born in the lowest quintile of family income had a higher risk for having caries experience at 3 y (OR, 1.9) and 7 y (OR, 1.7). Mothers with an educational level <9 y were 1.8 times more likely to have children with caries experience at both ages. The risk of caries experience in children was 1.4 times higher among mothers who had >2 children.
Analyzing maternal health behavior in model 3, we found that pregnancy before age 25 y increased the chance of having caries by 1.3 times at 3 y and 1.4 at 7 y. Maternal obesity increased the child’s caries risk by 1.3 times at 3 y and 1.2 at 7 y old. The OR for caries risk among children of mothers who smoked during pregnancy was 1.6 at both ages.
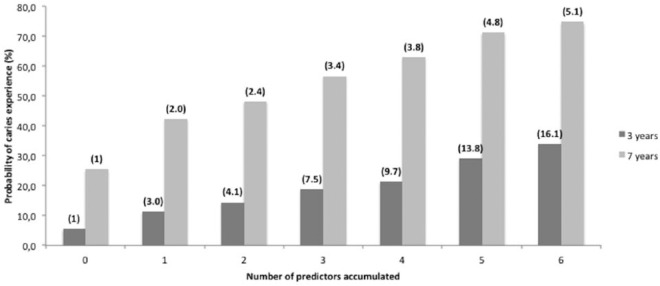
Model-based fitted cumulative risk factors estimated the probability of developing caries. The estimated probability of having caries experience at age 3 y was 5.6% when none of the risk factors were present; when all risk factors were present, the cumulative probability was 33.9% (Fig. 2). For children with all risk factors, the relative risk of developing dental caries was 16.1 times higher than for children with none of the risk factors present. When we analyzed children at 7 y of age, the cumulative probability of caries experience was 74.7% with all risk factors present. The relative risk of these children developing caries was 5.1 times higher than for children with none of the risk factors present.
Figure 2.
Cumulative percentage probability of caries experience at 3 and 7 y of age. The multivariate cumulative risk is in parentheses at the top of each column. When none of predictors was used, relative risk = 1. Predictors: 1 = mother’s nationality, 2 = mother’s nationality + parity, 3 = mother’s nationality + parity + family income, 4 = mother’s nationality + parity + family income + mother’s age, 5 = mother’s nationality + parity + family income + mother’s age + smoking, 6 = mother’s nationality + parity + family income + mother’s age + smoking + obesity.
Discussion
The results of this study show that socioeconomic and maternal health behaviors during pregnancy are important determinants of oral health among preschool children. The cumulative probability of being diagnosed with caries experience at 7 y was 75% for children with all the risk factors that we identified. This study also showed that maternal obesity and smoking during early pregnancy were predictors of caries experience among preschool children.
In a multivariate logistic regression analysis, country of birth, low maternal educational level, low family income, and family situation were factors significantly associated with caries experience. Children with parents born in low-income counties have consistently shown to be at high risk for caries development (Grindefjord et al. 1996; Braun et al. 2016). Social inequalities persist, and they have a profound effect on the general and oral health of the individual (Marmot 2017; Schwendicke et al. 2018;). Low maternal educational level, low family income, and single-parent families were found to be associated with high caries risk among preschool children (Marcenes et al. 2013). Parental practices, such as positive involvement, encouragement, and problem-solving skills, are important indicators of children’s oral health. Lower socioeconomic levels have also been linked to lower dental self-efficacy (parents’ confidence in their ability to engage in healthy oral health practices for their child), a more external locus of control, and poor parenting practices (Duijster et al. 2015).
Of course, some children and families may have less need of intervention because they have the personal, financial, and social resources that allow them to incorporate knowledge about caries prevention in a healthy lifestyle and adequate preventive measures (Watt 2007). Health behaviors are arguably a consequence of the social condition and environment in which people are born and grow up (Marmot et al. 2008). Preventive measures should take a more holistic approach and not focus only on individual behavioral factors (Watt and Sheiham 2012; Chi et al. 2017). There is need to examine ways to change the conditions that cause poor capacity to benefit from preventive programs. Evidence indicates that health coaches who support high-risk families over time can increase self-efficacy (Boyd et al. 2006).
The finding that having more siblings was associated with high caries prevalence is interesting. This association has been reported before (Christensen et al. 2010). Additional children in the family may dilute available parental time and resources, which reduce the time that parents spend reading to, teaching, or playing with each child, which could affect cognitive development (Downey 2001) and may make it harder for parents to attend to their children’s health care needs (Case and Paxson 2001; Chen and Escarce 2008).
Preventive programs often focus on mothers of first-born children, with early information in maternity clinics and follow-up (Dobloug and Grytten 2016). Maternal age <25 y and >35 y were both associated with higher child caries prevalence. Children of young mothers were particularly at risk, in agreement with previous studies (Julihn et al. 2009; Dobloug and Grytten 2016). Young mothers often have lower education and income and more often live in a single household (Mattila et al. 2000).
An important finding in this study was that maternal obesity and maternal smoking during pregnancy were both associated with caries development in children aged 3 to 7 y. The association between obesity and caries experience among preschool children could be mediated by factors such as unhealthy eating habits and a sedentary lifestyle. Wigen and Wang (2011) showed that obese mothers consume a diet containing more fat and sugar than recommended. Children born to obese mothers are themselves at higher risk of becoming obese and being diagnosed with chronic inflammatory disease (Tapanainen et al. 2001). An association between childhood obesity and dental caries has also been suggested (Willershausen et al. 2004), and it is likely that the 2 conditions share common risk factors, related to socioeconomic status and diet (Marshall et al. 2007).
Children whose mothers smoked during pregnancy were at higher risk to develop caries at 3 and 7 y. Tanaka et al. (2015) showed that exposure to tobacco smoke, pre- and postnatally, was associated with increased caries prevalence among preschool children. Prenatal exposure to tobacco smoke was also reported by Julihn et al. (2009) to be a predictor of caries development. This association can be explained in several ways. Nicotine inhibits matrix synthesis and mineralization by ameloblasts and odontoblasts, interfering in enamel mineralization (Dong et al. 2011). However, there is an inverse correlation between cotinine levels and serum vitamin D concentration (Manavi et al. 2015). Lower maternal 25-hydroxy vitamin D levels in serum were associated with dental caries in children (Schroth et al. 2014). Smoking during pregnancy is also associated with adverse effects on the cellular function of immune system–modifying fetal T-helper 1 and 2 cells (Macaubas et al. 2003).
This study has several strengths. Our sample size was large, >65,000 children, as provided by the public health care administration in Stockholm, reducing the possibility of selection bias and increasing the generalization of the results. The publicly funded standardized oral health care system with local guidelines for diagnosis and treatment should limit residual confounding and provide high internal validity. However, there are some limitations. We did not have access to data on diet or oral hygiene factors during the first years of life. Another limitation is the retrospective nature of the study, which does not allow answering cause-and-effect relationships. Dentists performing the examinations of children were not calibrated for this specific study, which may have generated a measurement bias. Likewise, the fact that only a certain proportion of children have bite radiographs may have generated the same bias. However, random errors decrease with increasing study size and are reduced to zero if a study becomes infinitely large (Rothman 2002). Finally, the last limitation is that data regarding the family income were collected at a single time point, which presumes that income remained the same at the point when children were 3 and 7 y old.
Our study provides conclusive evidence that socioeconomic factors and maternal health behavior during pregnancy are predictors of caries experience in children. Education, income, and other socioeconomic factors are difficult to modify in the short term. Therefore, strategies must be developed to increase parental motivation and self-efficacy to give parents the determination, knowledge, and tools for prevention.
Author Contributions
A. Julihn, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; F.C. Soares, contributed to data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; A. Hjern, G. Dahllöf, contributed to design and data interpretation, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_2380084418788066 for Socioeconomic Determinants, Maternal Health, and Caries in Young Children by A. Julihn, F.C. Soares, A. Hjern and G. Dahllöf in JDR Clinical & Translational Research
Footnotes
A supplemental appendix to this article is available online.
This study was supported by grants from the Swedish Patent Revenue Research Fund.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
ORCID iD: F.C. Soares  https://orcid.org/0000-0001-6465-3164
https://orcid.org/0000-0001-6465-3164
References
- Anderson M, Dahllöf G, Twetman S, Jansson L, Bergenlid AC, Grindefjord M. 2016. Effectiveness of early preventive intervention with semiannual fluoride varnish application in toddlers living in high-risk areas: a stratified cluster-randomized controlled trial. Caries Res. 50(1):17–23. [DOI] [PubMed] [Google Scholar]
- Armfield JM, Spencer AJ, Stewart JF. 2006. Dental fear in Australia: who’s afraid of the dentist? Aust Dent J. 51(1):78–85. [DOI] [PubMed] [Google Scholar]
- Bagramian RA, Garcia-Godoy F, Volpe AR. 2009. The global increase in dental caries. Am J Dent. 22(1):3–8. [PubMed] [Google Scholar]
- Boyd RC, Diamond GS, Bourjolly JN. 2006. Developing a family-based depression prevention program in urban community mental health clinics: a qualitative investigation. Fam Process. 45(2):187–203. [DOI] [PubMed] [Google Scholar]
- Brandquist E, Dahllöf G, Hjern A, Julihn A. 2017. Caesarean section does not increase the risk of caries in Swedish children. JDR Clin Trans Res. 2(4):386–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun PA, Quissell DO, Henderson WG, Bryant LL, Gregorich SE, George C, Toledo N, Cudeii D, Smith V, Johs N, et al. 2016. A cluster-randomized, community-based, tribally delivered oral health promotion trial in Navajo Head Start children. J Dent Res. 95(11):1237–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Paxson C. 2001. Mothers and others: who invests in children’s health? J Health Econ. 20(3):301–328. [DOI] [PubMed] [Google Scholar]
- Chen AY, Escarce JJ. 2008. Family structure and the treatment of childhood asthma. Med Care. 46(2):174–184. [DOI] [PubMed] [Google Scholar]
- Chi DL, Luu M, Chu F. 2017. A scoping review of epidemiologic risk factors for pediatric obesity: implications for future childhood obesity and dental caries prevention research. J Public Health Dent. 77 Suppl 1:S8–S31. [DOI] [PubMed] [Google Scholar]
- Christensen LB, Twetman S, Sundby A. 2010. Oral health in children and adolescents with different socio-cultural and socio-economic backgrounds. Acta Odontol Scand. 68(1):34–42. [DOI] [PubMed] [Google Scholar]
- Dobloug A, Grytten J. 2016. Correlation between siblings in caries in Norway: a quantitative study. Community Dent Oral Epidemiol. 44(5):416–425. [DOI] [PubMed] [Google Scholar]
- Dong Q, Wu H, Dong G, Lou B, Yang L, Zhang L. 2011. The morphology and mineralization of dental hard tissue in the offspring of passive smoking rats. Arch Oral Biol. 56(10):1005–1013. [DOI] [PubMed] [Google Scholar]
- Downey DB. 2001. Number of siblings and intellectual development: the resource dilution explanation. Am Psychol. 56(6–7):497–504. [DOI] [PubMed] [Google Scholar]
- Duijster D, De Jong-Lenters M, De Ruiter C, Thijssen J, Van Loveren C, Verrips E. 2015. Parental and family-related influences on dental caries in children of Dutch, Moroccan and Turkish origin. Community Dent Oral Epidemiol. 43(2):152–162. [DOI] [PubMed] [Google Scholar]
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, Eke PI, Beltran-Aguilar ED, Horowitz AM, Li C-H. 2007. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat. 11(248):1–92. [PubMed] [Google Scholar]
- Grindefjord M, Dahllöf G, Nilsson B, Modéer T. 1996. Stepwise prediction of dental caries in children up to 3.5 years of age. Caries Res. 30(4):256–266. [DOI] [PubMed] [Google Scholar]
- Julihn A, Ekbom A, Modéer T. 2009. Maternal overweight and smoking: prenatal risk factors for caries development in offspring during the teenage period. Eur J Epidemiol. 24(12):753–762. [DOI] [PubMed] [Google Scholar]
- Koch G. 1967. Effect of sodium fluoride in dentifrice and mouthwash on incidence of dental caries in schoolchildren. Odontol Rev. 18 Suppl 12:4. [Google Scholar]
- Li M, Fallin MD, Riley A, Landa R, Walker SO, Silverstein M, Caruso D, Pearson C, Kiang S, Dahm JL, et al. 2016. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 137(2):e20152206–e20152206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macaubas C, de Klerk NH, Holt BJ, Wee C, Kendall G, Firth M, Sly PD, Holt PG. 2003. Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet. 362(9391):1192–1197. [DOI] [PubMed] [Google Scholar]
- Manavi KR, Alston-Mills BP, Thompson MP, Allen JC. 2015. Effect of serum cotinine on vitamin D serum concentrations among american females with different ethnic backgrounds. Anticancer Res. 35(2):1211–1218. [PubMed] [Google Scholar]
- Marcenes W, Kassebaum NJ, Bernabe E, Flaxman A, Naghavi M, Lopez A, Murray CJ. 2013. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 92(7):592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. 2017. Social justice, epidemiology and health inequalities. Eur J Epidemiol. 32(7):537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S, Hlt CSD. 2008. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 372(9650):1661–1669. [DOI] [PubMed] [Google Scholar]
- Marshall TA, Eichenberger-Gilmore JM, Broffitt BA, Warren JJ, Levy SM. 2007. Dental caries and childhood obesity: roles of diet and socioeconomic status. Community Dent Oral Epidemiol. 35(6):449–458. [DOI] [PubMed] [Google Scholar]
- Mattila ML, Rautava P, Sillanpää M, Paunio P. 2000. Caries in five-year-old children and associations with family-related factors. J Dent Res. 79(3):875–881. [DOI] [PubMed] [Google Scholar]
- Rothman KJ. 2002. Biases in study design. In: Epidemiology: an introduction. New York (NY): Oxford University Press; p. 94–112. [Google Scholar]
- Schroth RJ, Lavelle C, Tate R, Bruce S, Billings RJ, Moffatt MEK. 2014. Prenatal vitamin D and dental caries in infants. Pediatrics. 133(5):e1277–e1284. [DOI] [PubMed] [Google Scholar]
- Schwendicke F, Splieth CH, Thomson WM, Reda S, Stolpe M, Foster Page L. 2018. Cost-effectiveness of caries-preventive fluoride varnish applications in clinic settings among patients of low, moderate and high risk. Community Dent Oral Epidemiol. 46(1):8–16 [DOI] [PubMed] [Google Scholar]
- Starfield B, Robertson J, Riley AW. 2002. Social class gradients and health in childhood. Ambul Pediatr. 2(4):238–246. [DOI] [PubMed] [Google Scholar]
- Tanaka K, Miyake Y, Nagata C, Furukawa S, Arakawa M. 2015. Association of prenatal exposure to maternal smoking and postnatal exposure to household smoking with dental caries in 3-year-old Japanese children. Environ Res. 143:148–153. [DOI] [PubMed] [Google Scholar]
- Tapanainen P, Leinonen E, Ruokonen A, Knip M. 2001. Leptin concentrations are elevated in newborn infants of diabetic mothers. Horm Res. 55(4):185–90. [DOI] [PubMed] [Google Scholar]
- Urquia ML, Qiao Y, Ray JG, Liu C, Hjern A. 2015. Birth outcomes of foreign-born, native-born, and mixed couples in Sweden. Paediatr Perinat Epidemiol. 29(2):123–130. [DOI] [PubMed] [Google Scholar]
- Villamor E, Tedroff K, Peterson M, Johansson S, Neovius M, Petersson G, Cnattingius S. 2017. Association between maternal body mass index in early pregnancy and incidence of cerebral palsy. JAMA. 317(9):925–936. [DOI] [PubMed] [Google Scholar]
- Watanabe M, Wang DH, Ijichi A, Shirai C, Zou Y, Kubo M, Takemoto K, Masatomi C, Ogino K. 2014. The influence of lifestyle on the incidence of dental caries among 3-year-old Japanese children. Int J Environ Res Public Health. 11(12):12611–12622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt RG. 2007. From victim blaming to upstream actions: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 35(1):1–11. [DOI] [PubMed] [Google Scholar]
- Watt RG, Sheiham A. 2012. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol. 40(4):289–296. [DOI] [PubMed] [Google Scholar]
- Wigen TI, Wang NJ. 2011. Maternal health and lifestyle, and caries experience in preschool children: a longitudinal study from pregnancy to age 5 yr. Eur J Oral Sci. 119(6):463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willershausen B, Haas G, Krummenauer F, Hohenfellner K. 2004. Relationship between high weight and caries frequency in German elementary school children. Eur J Med Res. 9(8):400–404. [PubMed] [Google Scholar]
- Zhou S, Rosenthal D, Sherman S, Zelikoff J. 2014. Physical, behavioral, and cognitive effects of prenatal tobacco and postnatal secondhand smoke exposure. Curr Probl Pediatr Adolesc Health Care. 44(8):219–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_2380084418788066 for Socioeconomic Determinants, Maternal Health, and Caries in Young Children by A. Julihn, F.C. Soares, A. Hjern and G. Dahllöf in JDR Clinical & Translational Research