Highlights
-
•
We experienced a giant Peutz-Jeghers-type polyp in the stomach without features of Peutz-Jeghers syndrome.
-
•
Solitary Peutz-Jeghers-type polyps of the stomach are extremely rare.
-
•
We found only 10 reports describing solitary gastric PJ polyps.
-
•
We present the patient with a comprehensive literature review.
Keywords: Solitary peutz-jeghers-type polyps, Sporadic hamartomatous polyps, Stomach
Abstract
Introduction
Solitary Peutz-Jeghers-type polyps of the stomach are extremely rare. They are defined as unique polyps that are not associated with Peutz-Jeghers syndrome (PJS).
Presentation of Case
A 37-year-old woman presented at our hospital with anemia and epigastric discomfort. Esophagogastroduodenoscopy to determine the cause of anemia revealed a 5 × 6-cm pedunculated polypoid tumor at the greater curvature of the upper gastric body. Pathological examination of a biopsy specimen confirmed a Group 1 hyperplastic polyp. Computed tomography revealed neither lymph node swelling nor distant metastasis. A malignant component of the polypoid tumor was difficult to deny because of its size. The patient underwent local resection of the stomach. Her postoperative course was uneventful.
A pathological examination of the surgical specimen revealed a Peutz-Jeghers-type, hamartomatous polyp containing an enlarged crypt with hyperplastic foveolar epithelium and smooth muscle proliferating into the lamina propria. No atypical cells were found in the overlying epithelium. Based on these findings, we performed colonoscopy and capsule endoscopy of the intestine. No polyps were found in the intestine or colon. She had no family history of any type of tumor and no mucocutaneous pigmentation.
Discussion
There were only 10 reports of solitary gastric Peutz-Jeghers polyps published to date. Although most of them did not have atypical cells, one case has proliferative component. A few reports have described relationship with malignant tumor.
Conclusion
Solitary gastric PJ-type polyps are rare. Careful follow-up should be recommended and further studies are needed to evaluate cancer risk of solitary gastric PJ-type polyps.
1. Introduction
Peutz-Jeghers-type (PJ-type) polyps are histologically characterized by proliferation of the muscularis mucosae to form branching configurations covered by hypertrophic, but otherwise normal mucosa. Solitary PJ-type polyps lack the features of Peutz-Jeghers syndrome (PJS). This report describes a patient with a gastric PJ-type polyp who did not have a family history of PJS or associated mucocutaneous pigmentations or any other gastrointestinal polyps. This case report has been reported in line with the SCARE criteria [1].
2. Presentation of case
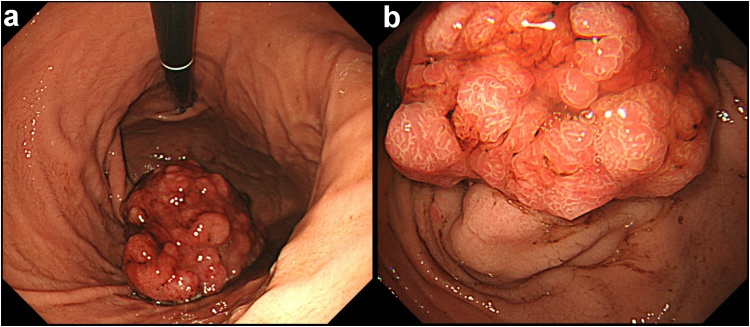
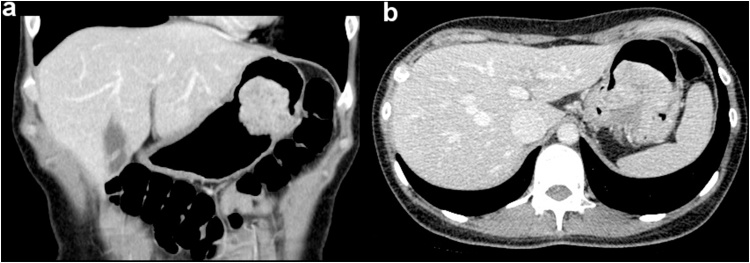
A 37-year-old woman was referred to us with epigastric discomfort. She had gone to a different hospital over a year before and had been taking iron supplementation for anemia ever since. Esophagogastroduodenoscopy showed a giant (5–6 cm), semi-pedunculated polypoid tumor located at the greater curvature of the upper gastric body (Fig. 1). There were no signs of H.pylori infection such as atrophic gastritis. Pathological examination of a biopsy specimen revealed that it was a Group 1, hyperplastic polyp of the stomach. H.pylori was negative. She had no mucocutaneous pigmentation and no family history of polyps. Laboratory findings showed a slightly depressed serum iron level. The tumor markers CEA and CA19-9 were within normal limits. Fluoroscopy confirmed that the tumor was located around the border of the fornix and the upper body of the stomach. Contrast CT showed a stalk-like structure at the root portion of the polyp (Fig. 2). Lymph node swelling and distant metastasis were not found.
Fig. 1.
Esophagogastroduodenoscopy findings. Images show a semi-pedunculated, 5 × 6-cm polypoid tumor in the greater curvature of the upper gastric body (a, b).
Fig. 2.
Computed tomography findings. Images show tumor located around the border of fornix and upper body of stomach (a), and stalk-like structure at root of the polyp (b).
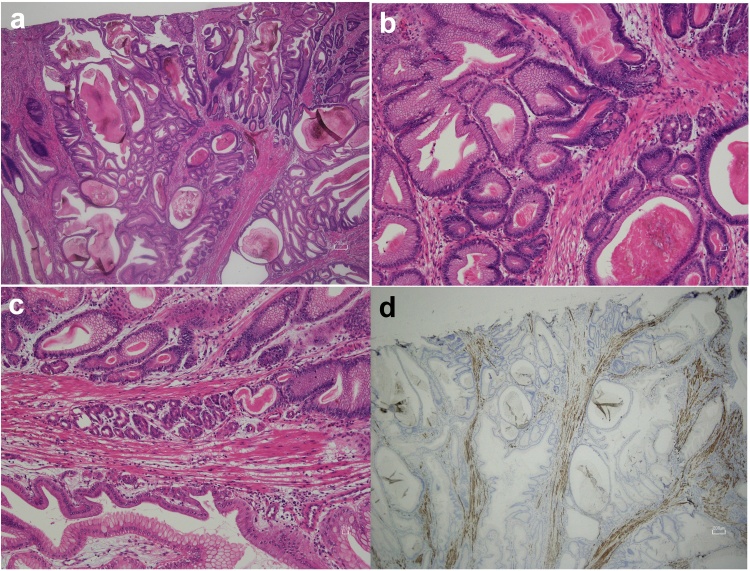
An excisional biopsy of the tumor was required to rule out malignant components and the stomach was locally resected. The serosal surfaces of the tumor were indented. The tumor was nodular and a stalk was evident at the root of the tumor. Histopathological assessment revealed foveolar hyperplasia on the surface of the polyp and cystically dilated glands (Fig. 3a and b), with cells at the base that resembled those in the fundic glands (Fig. 3c). Desmin staining showed arborizing smooth muscle bundles extending up to the superficial lamina propria (Fig. 3d). Only the neck of enlarged glands was immunostained for Ki 67 like normal glands. All of these features supported a differential diagnosis as a PJ hamartomatous polyp. The overlying epithelium did not contain any atypical cells (Fig. 3a, b and c).
Fig. 3.
Pathological findings. Foveolar hyperplasia on polyp surface (a; magnification ×20) and cystically dilated glands (b, magnification ×40). Cells at the base of glands are similar to those in fundic glands (c). Desmin staining shows arborizing smooth muscle bundles extending up to the superficial lamina propria (d).
The postoperative course was uneventful and the patient was discharged after six days. Colonoscopy and capsule endoscopy of the intestine proceeded considering the histological judgement, but neither the intestine nor the colon contained any polyps.
3. Discussion
Digestive hamartomatous polyps are rare, and can be solitary or multiple. The latter type is often associated with familial or non-familial polyposis syndromes such as PJS, juvenile polyposis, Cowden disease, and Cronkhite-Canada syndrome. If a family history or clinical symptoms are not found, they are called “solitary” or “sporadic” hamartomatous polyps. Solitary hamartomatous polyps are thought to comprise PJ and juvenile types [2].
Macroscopically, PJ-type polyps usually have a lobulated or convoluted surface, whereas the juvenile type is often spherical, with a non-lobulated surface. However, the two types considerably differ histologically in that the muscularis mucosae are involved in PJ-type polyps. An arborizing framework of smooth muscle originating from the muscularis mucosae is a distinctive feature of PJ polyps. The crypts or pits as well as the deeper glands are often elongated, and the overlying epithelium is normal.
Peutz-Jeghers syndrome is an autosomal-dominant familial disorder that is diagnosed based on the presence of any two of three diagnostic criteria consisting of a family history, mucocutaneous pigmentation, and intestinal hamartomatosis with typical PJ-type histology [3,4]. As our patient did not meet any of the other criteria for a diagnosis of PJS, the diagnosis was a solitary PJ-type polyp.
A search of case reports in the English PubMed database up to January 2017 using the terms “solitary hamartomatous PJ polyp” or “sporadic PJ polyp” identified 37 reports describing a total of 55 PJ-type hamartomatous polyps located in the duodenum (n = 20), stomach (n = 8), small bowel (n = 13), colon (n = 11), and rectum (n = 3). In contrast, polyps associated with PJS can be found throughout the gastrointestinal tract, mostly in the small bowel (60%–90%), stomach (15%–30%), and colon (50%–64%) [5].
In addition, we searched reference lists of published articles and found 10 reports describing solitary gastric PJ polyps (Table 1). Although the incidence of the solitary type is unknown, the incidence of PJ polyps among gastric polyps is 0.18% [6] and most of those polyps were with PJS. Therefore, solitary gastric PJ polyps are extremely rare.
Table 1.
Publications describing solitary gastric Peutz–Jeghers polyps.
| No. | Author | Year | Country | Size (mm) | Age (y) | Sex | Locus | Symptoms |
|---|---|---|---|---|---|---|---|---|
| 1 | Kuwano | 1989 | Japan | 20 | 17 | M | Gastric body, Gre/Post | Epigastralgia with diarrhea |
| 2 | Grisendi | 1990 | Italy | 20 | 53 | F | – | – |
| 3 | Hunt | 1996 | Australia | 80 × 50 × 45 | 27 | F | Lower (antrum?) | Vomiting, weight loss, bleeding (melena) |
| 4 | Sakadamis | 2001 | Greece | 75 × 50 | 47 | F | Antrum, Ant | Epigastric pain, nausea, melena |
| 5 | O’Loughlin | 2002 | USA | 70 × 40 | 38 | F | Antrum | Epigastric discomfort, abdominal fullness, nausea, regurgitation |
| 6 | Oncel | 2002 | USA | 5 | 78 | M | – | Dyspepsia |
| 7 | Harbaum | 2009 | Austria | 10 | 61 | M | Oxyntic-type mucosa | – |
| 8 | Jin | 2012 | China | 40 × 30 | 71 | F | Antrum | Epigastric pain, weight loss |
| 9 | Sorinel Lunca | 2014 | Romania | 150 × 70 × 50 | 43 | F | Below ECJ | Bleeding, abdominal discomfort, weight and appetite loss, fatigability |
| 10 | LeiShi | 2014 | China | 25 | 67 | M | Antrum, Ant | Abdominal pain and distension |
| 11 | Present case | 2016 | Japan | 65 × 60 × 35 | 37 | F | Fornix, Gre/Post | Epigastric discomfort |
According to the 10 cases, solitary gastric PJ polyps have been found in various places, such as in Europe, North America, Asia, and Australia. Women are more frequently affected and the median age is 47 (IQR, 37–64) years. In contrast, 30% and 60% of PJS is diagnosed during the first, and during the second or third decades, respectively. Polyps can arise anywhere in the stomach, but might be more prevalent in the lower part. Polyps were found in the oxyntic-type mucosa of one patient described in the literature [7] and in our patient. None of the reports mention H. pylori or atrophic gastritis.
Common symptoms are abdominal pain, digestive bleeding, and anemia. Hamartomatous polyps have a highly vascular stroma, which explains their tendency to bleed.
Biopsy specimens of polyps collected only from a surface layer using endoscopic forceps are often diagnosed as being hyperplastic. Moderate dysplasia may be diagnosed [8], because the fragile superficial area is prone to inflammatory erosion. Two patients had swollen lymph nodes [8,9] that were finally diagnosed as reactive hyperplasia without tumor metastasis. Reactive lymph-node swelling is probably due to inflammatory changes on the surfaces of polyps. Thus, total polypectomy or an excisional biopsy is mandatory for complete diagnosis. A small gastric polyp can be endoscopically resected, but large polypoid tumors require gastrectomy with consideration for the possibility of a malignant component such as carcinoma in adenoma.
When choosing the surgical approach, we considered that the tumor was located very close to the esophagogastric junction (EGJ) on the posterior wall. The laparoscopic gastric local resection using linear stapler was impossible because the resection line involves EGJ. Meanwhile, for the purpose of histological biopsy, proximal or total gastrectomy that significantly impair QOL are not acceptable. In order to minimize the extent of gastrectomy, it was necessary to hollow out the stomach wall manually around the tumor. Since the laparoscopic and endoscopic cooperative surgery (LECS) [10] for this size tumor in this part of the stomach is very difficult, we chose to perform a small laparotomy.
Whether PJ-type polyps represent an incomplete form of PJS or a different entity remains unknown. The STK11/LKB1 gene is mutated in 30%–80% of patients with PJS. Patients with PJS are at an increased risk of developing carcinomas of many organs with a cumulative lifetime risk for cancer of 93% [11]. The STK11/LKB1 gene mutation was undetectable in two patients each with a solitary PJ polyp [7,12]. We were unable to genotype the PJ polyp from our patient. Whether solitary PJ-type polyps carry a risk for cancer and whether patients with these polyps are at risk for carcinoma of other organs like PJS patients are also unknown. Many patients do not have atypical cells. However some reports describe adenomatous transformation, dysplasia [7,13,14], and an adenocarcinomatous component [15]. In 10 gastric PJ polyps, only one case had proliferative component with low grade atypia. Cancers of other organs have also coincided in patients with PJ polyps [16]. Therefore, more information needs to be gathered from more patients.
4. Conclusion
Solitary gastric PJ-type polyps are rare. Although a genetic abnormality similar to that associated with PJS has not been identified, a few reports have described the malignant transformation of polyps and cancers of other organs. Thus, careful follow-up should be recommended. However, further studies are needed to evaluate cancer risk in more patients.
Consent
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned, externally peer-reviewed
Acknowledgements
The authors greatly appreciate Dr. Seiichiroh Shimizu (Department of Pathology, Showa General Hospital) for his pathological diagnosis.
References
- 1.Agha R.A., Fowler A.J., Saeta A. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Cauchin E., Touchefeu Y., Matysiak-Budnik T. Hamartomatous Tumors in the Gastrointestinal Tract. Gastrointest. Tumors. 2015;2:65–74. doi: 10.1159/000437175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calva D., Howe J.R. Hamartomatous polyposis syndromes. Surg. Clin. North Am. 2008;88:779–817. doi: 10.1016/j.suc.2008.05.002. vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zbuk K.M., Eng C. Hamartomatous polyposis syndromes. Nat. Clin. Pract. Gastroenterol. Hepatol. 2007;4:492–502. doi: 10.1038/ncpgasthep0902. [DOI] [PubMed] [Google Scholar]
- 5.Utsunomiya J., Gocho H., Miyanaga T. Peutz-Jeghers syndrome: its natural course and management. Johns Hopkins Med. J. 1975;136:71–82. [PubMed] [Google Scholar]
- 6.Sotnikov V.N., Dubinskaia T.K., Sotnikov A.V. 2007. Polyposis of the Stomach. Endoscopic Treatment or Follow-up?]. Khirurgiia (Mosk) pp. 38–42. [PubMed] [Google Scholar]
- 7.Harbaum L., Geigl J.B., Volkholz H. Sporadic gastric Peutz-Jeghers polyp with intraepithelial neoplasia. APMIS. 2009;117:941–943. doi: 10.1111/j.1600-0463.2009.02549.x. [DOI] [PubMed] [Google Scholar]
- 8.Jin J.S., Yu J.K., Tsao T.Y., Lin L.F. Solitary gastric Peutz-Jeghers type stomach polyp mimicking a malignant gastric tumor. World J. Gastroenterol. 2012;18:1845–1848. doi: 10.3748/wjg.v18.i15.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lunca S., Porumb V., Velenciuc N. Giant solitary gastric Peutz-Jeghers polyp mimicking a malignant gastric tumor: the largest described in literature. J. Gastrointestin. Liver Dis. 2014;23:321–324. doi: 10.15403/jgld.2014.1121.233.vpb2. [DOI] [PubMed] [Google Scholar]
- 10.Hiki N., Yamamoto Y., Fukunaga T. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg. Endosc. 2008;22:1729–1735. doi: 10.1007/s00464-007-9696-8. [DOI] [PubMed] [Google Scholar]
- 11.Giardiello F.M., Welsh S.B., Hamilton S.R. Increased risk of cancer in the Peutz-Jeghers syndrome. N. Engl. J. Med. 1987;316:1511–1514. doi: 10.1056/NEJM198706113162404. [DOI] [PubMed] [Google Scholar]
- 12.Kitaoka F., Shiogama T., Mizutani A. A solitary Peutz-Jeghers-type hamartomatous polyp in the duodenum. A case report including results of mutation analysis. Digestion. 2004;69:79–82. doi: 10.1159/000077392. [DOI] [PubMed] [Google Scholar]
- 13.Jamaludin A.Z., Telisinghe P.U., Yapp S.K., Chong V.H. Solitary duodenal hamartomatous polyp with malignant transformation: report of a case. Surg. Today. 2009;39:527–532. doi: 10.1007/s00595-008-3873-9. [DOI] [PubMed] [Google Scholar]
- 14.Limaiem F., Bouraoui S., Lahmar A. Adenomatous transformation in a giant solitary Peutz-Jeghers-type hamartomatous polyp. Pathologica. 2011;103:346–349. [PubMed] [Google Scholar]
- 15.Ichiyoshi Y., Yao T., Nagasaki S., Sugimachi K. Solitary Peutz-Jeghers type polyp of the duodenum containing a focus of adenocarcinoma. Ital. J. Gastroenterol. 1996;28:95–97. [PubMed] [Google Scholar]
- 16.Oncel M., Remzi F.H., Church J.M. Course and follow-up of solitary Peutz-Jeghers polyps: a case series. Int. J. Colorectal Dis. 2003;18:33–35. doi: 10.1007/s00384-002-0411-x. [DOI] [PubMed] [Google Scholar]