Abstract
Dorsal nasal gouty tophus are rare occurrences with limited documentation. Here we report a male patient who has a history of poorly controlled gouty arthritis. He had nasal obstruction with an enlarging mass over his left nasal ridge for the past three years. Image studies revealed a nasal bone defect underneath the nasal lesion. The firm mass was excised and confirmed to be of gouty origin. The nasal bone defect was repaired with a titanium mesh plate to prevent nasal depression. He has fully recovered with no more nasal obstruction or recurrence of nasal tophus. The case report illustrates a common illness, gout, with a rare clinical manifestation leading to a common symptom, nasal obstruction. It demonstrates the importance of a detailed history, a thorough physical examination and most important of all, an extensive differential diagnosis in our clinical practice.
Keywords: Nose, Gouty tophus, Bone
Gout is a well-known abnormality in the metabolism of uric acid, which leads to the undesired buildup of monosodium urate crystals primarily in the peripheral joints and soft tissues of our body. It has the highest prevalence of all inflammatory rheumatic diseases with a peak age incidence of 30–50-year-old, with men being affected five times greater than women [1]. This disease is promoted by a diet rich in purine and presents as an intermittent course of inflammatory joint manifestations with periods free of symptoms. Confirmation of diagnosis is typically made under polarized microscopes with the appearance of strong negative birefringent needle-like monosodium urate crystals [2].
Although gout is most frequently seen in joints of the extremities, such as the metatarsal-phalangeal joint at the base of the big toe, chronic tophaceous gout may develop as nodular lesions in all areas of the body from our toes to our head and neck region. Rarely, however, has there been cases reported that involved the nasal region. There are five cases of documented nasal gouty tophus, with two of them presenting as nasal obstruction, while the other three cases were identified as esthetic problems [3], [4], [5], [6], [7].
In this case study, we report a 39-year-old male who presented at our clinic due to nasal obstruction with a mass located in his left nasal ridge. A careful evaluation of the patient's history, along with a thorough physical examination and image studies allowed us to suspect the nasal mass to be of gouty origin. Reconstruction options for the patient's nasal bone defect are also discussed.
Case report
A 39-year-old man with a history of gouty arthritis presented to our clinic at Chang Gung Memorial Hospital, Linkou Branch, Taiwan, due to nasal obstruction and a progressively enlarging mass protruding from his left nasal ridge. He has a history of poorly controlled gouty arthropathy and had undergone two operations for the excisions of multiple tophi located on his elbow, wrist and heel regions within a six year time period. He denied any other systemic diseases such as hypertension or diabetes mellitus as well as a family history of gout or autoimmune illnesses.
The patient complained of an increase in difficulty of breathing, which coincided with the gradual growth of the dorsal nasal mass within the past three years. Upon examination, the protruding mass located on his left nasal ridge was firm, movable and slightly tender when compressed, with a diameter of approximately 2 cm [Fig. 1, arrow]. There were no other lesions such as an external fistula noted. He did not complain of any additional symptoms such as sleep apnea, rhinorrhea, epistaxis, purulence or foul odors. A history of nasal trauma or hyperlipidemia was also denied.
Fig. 1.
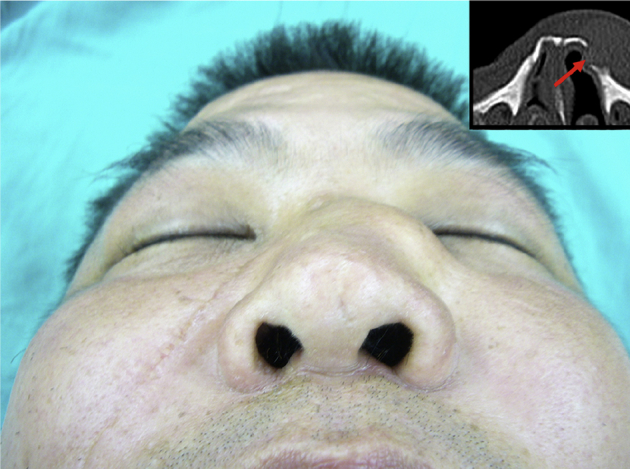
Preoperative view of the protruding nasal lesion; inset is the axial view of facial bone CT showing the protruding nasal lesion with bony destruction (arrow).
A computed tomographic (CT) scan of his face revealed a huge nasal mass with destruction of the nasal bone [Fig. 1, arrow]. Due to this finding and his past history of chronic tophi developments, nasal gouty tophus was highly suspected to be the etiology of the mass and cause of nasal obstruction symptoms. As a result of this tentative diagnosis, surgical removal was suggested.
In the operating room, the nasal lesion could be clearly seen to protrude from his left nasal ridge. A diagonal incision was made along the lines of the nasal fold for better cosmetic purposes and after careful dissection, a well defined, encapsulated mass measuring approximately 2 × 2 × 1.5 cm was exposed. The mass was removed in its entirety and no further tophi were identified in the region. Following removal of the tophi, bony defect of the nasal bone was revealed. The defect was then repaired with one piece of titanium mesh plate and fixed with one microscrew to prevent the nasal depression. After the wound was irrigated extensively, the wound was closed in the usual fashion. The operating scar was prudently hidden in the patient's nasal fold for cosmetic appeal.
Final pathologic reports confirmed the initial diagnosis of nasal gouty tophus. Under a magnification power of 400× the original, eosinophilic tophaceous deposits surrounded by chronically inflammatory cells, including multinucleate histiocytes was seen.
The patient was followed up for two years with no more breathing difficulties as well as no recurrences of chronic tophi in the nasal region or other parts of his face or body [Fig. 2]. His repaired nasal bone defect has not caused any new symptoms, discomforts or cosmetic dissatisfactions.
Fig. 2.

Images of the patient two years post operation show no nasal or facial recurrences of chronic tophi. No functional or cosmetic discomforts were noted.
Discussion
Out of the five previously reported cases of nasal gouty tophus, three cases presented as a dorsal nasal mass with cosmetic appeal as the primary surgical indication. Two other cases, along with the patient we reported here, suffered from nasal obstruction symptoms caused by nasal tophus [3], [4], [5], [6], [7]. All previous five cases received surgical treatment for their nasal gouty tophus. Their chief complaints, whether it was cosmetic appeal, diplopia or nasal obstruction, were improved post operation. Similar to our case report, there were no recurrences of nasal gouty tophus mentioned upon follow up.
The patient described in this case is the first one reported to have bone destruction at the site of a growing nasal tophus with subsequent nasal bone defect. The enlarging tophus significantly deformed the upper lateral nasal ridge while eroding the nasal bone underneath. This resulted in a diminished airway patency and thus led to symptoms of nasal obstructions. Reconstruction of the nasal bone defect using bone or cartilage grafts, nasal prosthesis or metal plates was discussed with the patient thoroughly. A simple titanium mesh plate was decided for the repair due to cosmetic reasons and the simplicity of the deformity. Overlying skin was not compromised so skin grafts or tissue flaps were not required. Upon follow up at one year, the patient no longer suffers from breathing difficulties and there have been no reoccurrences of nasal tophi noted.
Despite the low incidence of such a rare clinical manifestation, we are able to find prevalent similarities between the patients of these six cases. A history of gouty arthropathy, poorly controlled despite medication therapy, seems to be the prevailing underlying disease. All six cases involved middle-aged men with ages ranging from 39-years-old to 69-years-old. Future research and case-series analysis are recommended before any conclusions can be made.
Although gout is commonly described as an inflammatory crystal-induced arthropathy that predominantly afflicts the peripheral joints, it has been reported that environmental exposures, medications, genetic mutations and certain patient populations can affect the pathophysiology of uric acid, thus predisposing patients to both typical and atypical manifestations of gout [8]. In addition, gout can often mimic malignancy, infection or other unrelated disease processes as numerous reports have described gout deposition in unusual parts of the body, further complicating the diagnostic process [9].
Prompt diagnosis and proper management of gouty tophi are essential for the patients' quality of life as these chronic tophaceous lesions play a major role in the development of structural joint damage and an increase in the mortality risk in people suffering from gout [10]. Gaviria et al. further supports the notion that chronic gouty lesions may present in various atypical locations such as the sclera, nose, ears, heart valves, breast, abdominal striae, gouty panniculitis, which increases morbidities as well as deformities caused by the disease [11]. As a result, patients with persistent hyperuricemia should receive regular medication to lower their serum urate concentration to an optimal level in order to prevent acute gouty attacks or the formation of gouty tophi. When medical compliance is insufficient, however, tophi lesions should be surgically removed upon identification to limit joint or structural damage or for cosmetic reasons. Management options regarding the reconstruction of nasal bone is dependent on the extent of the defect as well as the desire of the patient.
Conclusions
This case study describes a rare etiology for a prevalent clinical presentation, nasal hump and obstruction. Not only does this report depict the importance of a thorough history, evaluation process and extensive differential diagnosis, it also acts as a reminder that extraordinary etiologies may present in everyday practice. Both medication and surgical treatment plans should be individualized to meet the need of each patient.
Disclosure
None of the authors has any commercial associations or financial disclosures that might pose or create conflicts of interest with anything discussed in this article. Each author has contributed original work to the article and adhered to the ethical requirements as outlined by the journal.
Patient consent
The patient provided written consent for the use of his images.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Monu J., Pope T.L. Gout: a clinical and radiologic review. Radiol Clin North Am. 2004;42:169–184. doi: 10.1016/S0033-8389(03)00158-1. [DOI] [PubMed] [Google Scholar]
- 2.Grass W., De Angelis R. Clinical features of gout. Reumatismo. 2012;63:238–245. doi: 10.4081/reumatismo.2011.238. [DOI] [PubMed] [Google Scholar]
- 3.Rask M.R., Kopf E.H. Nasal gouty tophus. JAMA. 1978;240:636. [PubMed] [Google Scholar]
- 4.Bergamaschi J.A., Costa Huve F., Von Holleben I., Bauer J.A., Deutsch K.M., Piltcher O. Nasal gouty tophus presenting as nasal obstruction: a case report. Int Arch Otorhinolaryngol. 2014;18:a2260. [Google Scholar]
- 5.Kwak P.E., Gorman B.K., Olson K.L. Nasal gout presenting as nasal obstruction. JAMA Otolaryngol Head Neck Surg. 2013;139:411–413. doi: 10.1001/jamaoto.2013.220. [DOI] [PubMed] [Google Scholar]
- 6.Parodi P.C., De Biasio F., Nadalig B., Ricci S. Tophaceous lesion of the middle third of the nose. Dermatol Surg. 2006;32:556–557. doi: 10.1111/j.1524-4725.2006.32113.x. [DOI] [PubMed] [Google Scholar]
- 7.Hughes J.P., Di Palma S., Rowe-Jones J. Tophaceous gout presenting as a dorsal nasal lump. J Laryngol Otol. 2005;119:492–494. doi: 10.1258/0022215054273160. [DOI] [PubMed] [Google Scholar]
- 8.Ning T.C., Keenan R.T. Unusual clinical presentations of gout. Curr Opin Rheumatol. 2010;22:181–187. doi: 10.1097/BOR.0b013e3283361ac0. [DOI] [PubMed] [Google Scholar]
- 9.Forbess L.J., Fields T.R. The broad spectrum of urate crystal deposition: unusual presentations of gouty tophi. Semin Arthritis Rheum. 2012;42:146–154. doi: 10.1016/j.semarthrit.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Chhana A., Dalbeth N. The gouty tophus: a review. Curr Rheumatol Rep. 2015;17:19. doi: 10.1007/s11926-014-0492-x. [DOI] [PubMed] [Google Scholar]
- 11.Gaviria J.L., Ortega V.G., Gaona J., Motta A., Medina Barragán O.J. Unusual dematological manifestations of gout: review of literature and a case report. Plastic Reconstr Surg Glob Open. 2015;3:e455. doi: 10.1097/GOX.0000000000000420. [DOI] [PMC free article] [PubMed] [Google Scholar]


