Abstract
Constipation is defined as the infrequent passage of stools or difficulty with evacuation of stools. Constipation can be classified as primary or secondary, and primary constipation can be further divided into slow transit constipation or outlet obstruction. The diagnostic workup involves focused lab tests and structural evaluation, followed by a therapeutic trial of fiber and laxatives, and finally, specialized tests. Treatment can consist of dietary changes, medications, physical therapy, and possibly surgery in refractory cases.
Constipation is a common and challenging complaint, but a systematic approach to evaluating patients with constipation can lead to effective treatments.
Background
Constipation is defined as infrequent passage of stools or difficulty with evacuation of stools. It is associated with various symptoms including hard stools, straining, sensation of anorectal blockage, incomplete evacuation, abdominal discomfort and bloating.1 The prevalence of constipation is 15% in the general population with a higher female to male ratio and a higher prevalence in the elderly especially over 65 years.2, 3 This disease poses a great economic burden related to direct health care costs and indirect costs.4
Etiology
Causes of constipation can be divided into primary (slow transit or outlet obstruction) or secondary causes. Secondary causes can include simple dehydration or inadequate fluid intake, metabolic disturbances, medications, neurological disorders, myopathic disorders and structural abnormalities (Table 1).
Table 1.
Secondary Causes of Constipation
| Secondary Causes of Constipation | |
| Metabolic disturbances | Diabetes, hypothyroidism, hypercalcemia, panhypopituitarism and pheochromocytoma.30–32 |
| Medications | Analgesics like opioids and nonsteroidal anti-inflammatory agents, anticholinergics including antidepressants and antipsychotics, anti-hypertensives like calcium channel blockers, diuretics and iron supplementation.32,33 |
| Neurological disorders | Parkinson’s disease, multiple sclerosis, dementia, Hirschprung’s disease and spinal cord lesions.32,34 |
| Myopathic diseases | Scleroderma, myotonic dystrophy and amyloidosis.32,35 |
| Structural disorder | Colon cancer, strictures and a large rectocele.36 |
When evaluating patients with constipation, secondary causes should be considered first and after secondary causes of constipation have been ruled out, the patient should be evaluated for primary or functional constipation. Risk factors for functional constipation include advanced age, low fiber diet, low socioeconomic status, immobility, abdominal or pelvic surgery and polypharmacy.5–7
Diagnosis of Functional Constipation
Since there are no specific tests to identify functional constipation, this diagnosis is based on criteria established by expert consensus called the Rome criteria.8 These have been sequentially refined over time and the Rome IV criteria define functional constipation as fulfilling at least 2 of the 6 criteria listed in Table 2. Functional constipation can be divided into 2 groups, slow transit constipation and outlet dysfunction.8 Slow transit constipation refers to delayed passage of fecal contents through the colon and is more common in women. The exact pathophysiology of slow transit constipation is unknown, however, it appears to involve a number of underlying causes including alterations in colonic muscle or nerve activity, enteric neurotransmitters and loss of interstitial cells of Cajal. The interstitial cells of Cajal are electrically active cells believed to act as the pacemakers for the intestines.7, 9. Studies have also found that excess methane production by colonic bacteria may be responsible for slow transit in some patients.10
Table 2.
ROME IV Criteria
| ROME IV criteria for functional constipation(must have at least 2 of 6): |
| • Fewer than 3 bowel movement per week |
| • Straining during >25% of the time |
| • Lumpy or hard stools > 25% of the time |
| • Sensation of anorectal obstruction > 25% of the time |
| • Sensation of incomplete evacuation > 25% of the time |
| • Manual maneuvers required to aid defecation > 25% of the time |
In addition to the above, the following three criteria should also be met to diagnose functional constipation: (1) Loose stools should rarely be present without the use of laxatives (2) Insufficient criteria for IBS (3) Present for at least 3 months during a period of 6 months.
Opioid-induced constipation is one of the most common side effects of opioid analgesic use in patients with cancer and non-cancer pain or chronic opiate use for other reasons. It is a common cause of slow transit constipations, and is thought to arise from increased non-propulsive segmental motility and decreased propulsive peristalsis due to μ-opioid receptor activation. The μ-opioid receptors are expressed in the myenteric and submucosal plexuses of the enteric nervous system in the gastrointestinal tract.
Outlet dysfunction is characterized by impaired rectal evacuation from inadequate rectal propulsive forces or increased resistance to evacuation or both.1, 8 Dyssynergic defecation is a form of outlet dysfunction and is defined by the inadequate relaxation or paradoxical contraction of the anorectal muscles while attempting to pass a bowel movement. Its pathophysiology is incompletely understood, however anxiety, psychological stress, and chronicity of constipation can contribute to the development of dyssynergic defecation.8, 11
Diagnosis
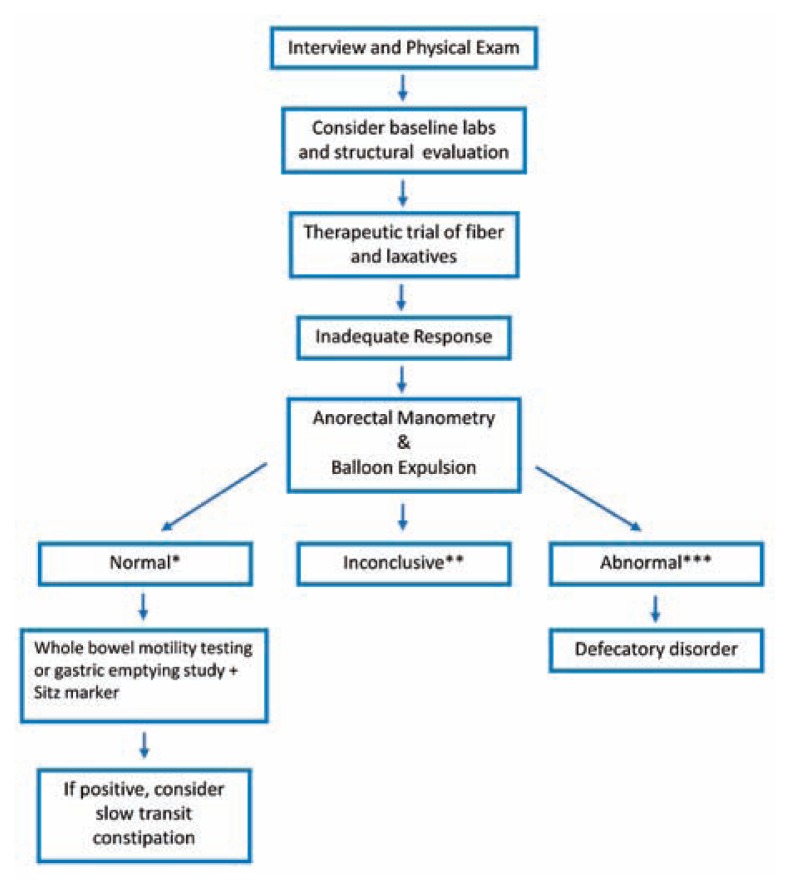
During evaluation of constipation, a careful history and physical examination should be conducted. Performing a complete digital rectal exam (DRE) is an important part of the clinical evaluation that includes squeeze and push maneuvers.12 An overview of the diagnostic algorithm is shown in Figure 1. After the initial history and physical examination, a set of focused tests should be obtained to assess disorders that are either treatable (like hypothyroidism) or important to diagnose early (like colon cancer). Guidelines agree that a complete blood cell count should be performed, however, further testing should be chosen based on history and physical.13 Although metabolic tests (thyroid-stimulating hormone, serum glucose, creatinine, and calcium) are often performed when evaluating patients with constipation, their diagnostic utility and cost-effectiveness have not been demonstrated. A structural evaluation of the colon may be beneficial, especially if the patient has alarm symptoms (weight loss, abdominal pain and hematochezia), has abrupt onset of constipation or is older than the recommended screening age for colonoscopy and has not undergone previous screening for colorectal cancer.1
Figure 1.
Diagnostic algorithm for constipation
*Normal or negative manometry study is normal balloon expulsion with no paradoxical contraction
**Inconclusive manometry is normal balloon expulsion and paradoxical contraction OR abnormal balloon expulsion and no paradoxical contraction
***Abnormal or positive manometry is abnormal balloon expulsion and paradoxical contraction
If this evaluation reveals a secondary cause for constipation, the appropriate treatment can be offered. The patient’s medications should be adjusted when possible to limit those with constipating effects.
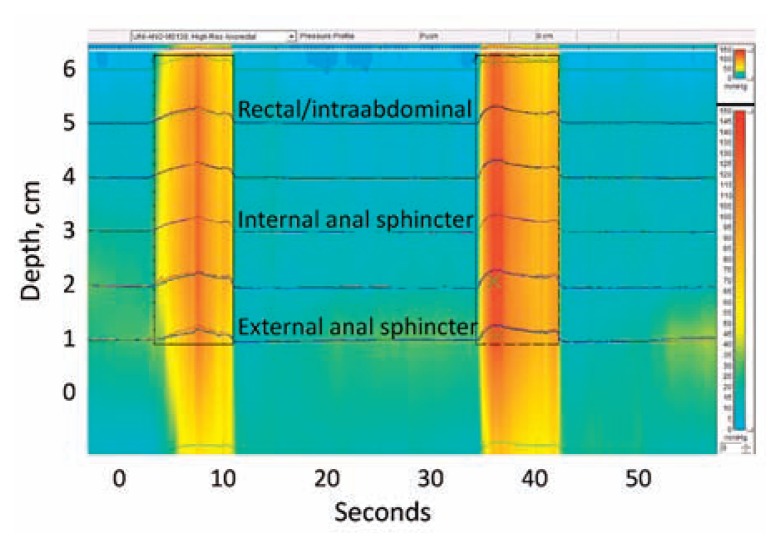
Those patients who do not respond to initial treatment with laxatives should undergo anorectal testing for evaluation of possible outlet dysfunction.1 Anorectal manometry measures the rectal and anal pressure at rest and during attempted defecation (Figure 2). It is also able to assess rectal sensation, recto-anal reflexes and rectal compliance. During the maneuver, when a patient mimics defecation, or tries to bear down, there should be a rise in the rectal pressure along with relaxation of the internal and external anal sphincters. The inability to relax the external anal sphincter and/or the puborectalis (Figure 2 is an example), along with inability to expel a 50cc water-filled balloon within one minute, is diagnostic of dyssynergic defecation.14
Figure 2.
High resolution anorectal manometry. A catheter with multiple pressure transducers is introduced through the anal canal and into the rectum and provides real-time pressure measurements at the external anal sphincter, internal anal sphincter and within the rectum. The patient is asked to try to expel the catheter by increasing intraabdominal pressure and relaxing the external sphincter. as shown in this example, two attempts to expel the catheter (from 3 to 11 seconds and 34 to 42 seconds) resulted in appropriately increased intraabdominal pressure but dyssynergic contraction of the external sphincter and no relaxation of the internal sphincter. The color pressure scale is shown on the right from low pressure (blue) to high pressure (red).
A balloon expulsion test can be done during anorectal manometry or as an independent test. It involves filling a balloon with 50cc of saline and asking the patient to expel it. Patients with normal defecation are able to expel the balloon within 1 minute. If the patient has difficulty expelling the balloon in this time frame, dyssynergic defecation should be suspected.15
After excluding outlet dysfunction with anorectal manometry and balloon expulsion, colonic transit should be evaluated using radiopaque markers (sitzmark study) or a wireless motility capsule.16, 17 A sitzmark study can measure colonic transit time by administering 24 radiopaque markers and obtaining a plain abdominal x-ray on day 5. A prolonged colonic transit time is identified when there are more than 20% of the markers or more than 5 markers remaining in the colon on day 5.16 The wireless motility capsule is a wireless capsule which measures pH, temperature and pressure throughout the entirety of the gastrointestinal tract, therefore providing gastric, small bowel and colonic transit time without radiation exposure.17 Defecography and Magnetic Resonance Defecography are additional tests that can be obtained. These record the pelvic anatomy of the patient during attempted defecation and are useful for evaluating conditions like rectocele or sigmoidocele, intussusception, rectal prolapse, and megarectum.8
Treatment
Once secondary causes of constipation are excluded, patients should be advised to increase their fiber and fluid intake, engage in regular physical activity and conduct timed toilet training.18
Most patients with constipation require the use of laxatives at some point in their course. For chronic use, bulk laxatives (fiber) and polyethylene glycol 3350 (“PEG,” e.g., Miralax) are tolerated best. Bulk laxatives include psyllium (Metamucil) and methylcellulose (Citrucel). Stimulant laxatives like senna and bisacodyl (Dulcolax) can produce excessive cramping and should therefore be used sparingly. Emollient stool softeners such as docusate (e.g., Colace) are best used for short-term prophylaxis, for example, in the post-operative setting.19 Osmotic agents include polyethylene glycol (PEG)-based solutions, magnesium citrate–based products, sodium phosphate–based products (e.g., Fleets), and non-absorbable carbohydrates (e.g., sorbitol). These hypertonic products work by the osmotic effect, retaining water in the colon.
The PEG and electrolyte lavage solutions used for colonic cleansing before procedures are typically not used for chronic constipation and are iso-osmotic with plasma; bowel evacuation is achieved with these by high-volume lavage rather than an osmotic effect.20
Newer medications include lubiprostone, an agent that activates chloride channels much like the cholera toxin and increases luminal fluid secretion. It has been shown to decrease stool transit time and improve symptoms of chronic idiopathic constipation.21 Linaclotide, a guanylin analog, works by stimulating the guanylyl cyclase-C receptor to increase chloride secretion like the enterotoxin from E. coli, and has been shown in studies to have neuromodulatory benefits in patients with IBS-C as well as decrease stool transit time.22 Plecanatide is another agent that also stimulates the guanylyl cyclase inhibitor and causes increased chloride and bicarbonate entry into the lumen via the activation of the cystic fibrosis transmembrane conductance regulator (CFTR) ion channel. Tegaserod is a serotonin type 4 (5-HT4) receptor partial agonist that is thought to trigger a peristaltic reflex via 5-HT4 activation, which enhances motor activity and normalizes impaired GI motility.23
Colchicine, which is a cytotoxin used to treat gout, is not usually recommended for regular clinical use for constipation because of its side effect profile, particularly when renal function is impaired. However small studies have shown that it may be useful in a subset of patients with chronic constipation who are refractory to medical management.24 Misoprostol is a prostaglandin E1 analogue that increases intraluminal fluid and bicarbonate secretion, effects that have been exploited to reduce the severity of refractory chronic constipation in small studies.25, 26
For patients with functional outlet obstruction, biofeedback has been shown to be very helpful. Trials have demonstrated that biofeedback is extremely useful in patients with dyssynergia, and is superior to standard therapy alone.27
First-line treatment for opioid-induced constipation typically involves a combination of pharmacological and non-pharmacological interventions such as laxatives and increased dietary fiber. A more targeted pharmacological approach to the treatment of refractory opioid-induced constipation is the development of peripherally acting μ-opioid receptor antagonists (PAMORAs), which aim to reverse opioid-induced constipation by selectively blocking opioid actions at peripheral μ-opioid receptors, including those in the enteric nervous system, without affecting analgesia in the CNS.28, 29 Drugs in this class currently approved for the treatment of opioid-induced constipation include naloxegol, methylnaltrexone, alvimopan and naldemidine. These agents should be avoided if bowel obstruction is suspected.
Surgical options, such as colectomy, should be a last resort for those patients who have failed medical management.
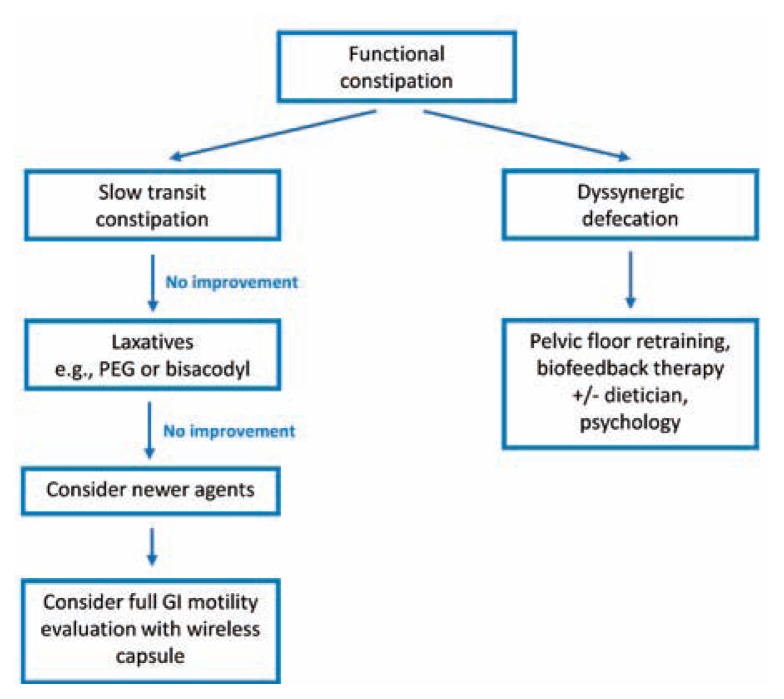
An algorithm for treatment decisions in functional constipation is shown in Figure 3.
Figure 3.
Treatment algorithm for functional constipation. Once secondary constipation has been excluded and functional constipation has been characterized, treatment can be focused on the underlying disorders.
Conclusion
Constipation is a very common complaint, especially in older adults, with a significant impact on healthcare costs. A careful history, physical examination and blood tests can help exclude secondary causes of constipation. Management of chronic constipation includes patient education, behavior modification, dietary changes, and laxative therapy.
Biography
Bhairvi Jani, MD, (left), is a Fellow and Elizabeth Marsicano, MD, (right), is an Assistant Professor of Internal Medicine in the Division of Gastroenterology and Hepatology, Saint Louis University School of Medicine, St. Louis, Mo.
Contact: Elizabeth.Marsicano@health.slu.edu


Footnotes
Disclosures
None reported.
References
- 1.American Gastroenterological A. Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013;144:211–217. doi: 10.1053/j.gastro.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 2.Mehendale AW, Goldman MP, Mehendale RP. Opioid overuse pain syndrome (OOPS): the story of opioids, prometheus unbound. J Opioid Manag. 2013;9:421–438. doi: 10.5055/jom.2013.0185. [DOI] [PubMed] [Google Scholar]
- 3.Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750–759. doi: 10.1111/j.1572-0241.2004.04114.x. [DOI] [PubMed] [Google Scholar]
- 4.Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, et al. Opioid epidemic in the United States. Pain physician. 2012;15:Es9–38. [PubMed] [Google Scholar]
- 5.Talley NJ, Jones M, Nuyts G, Dubois D. Risk factors for chronic constipation based on a general practice sample. Am J Gastroenterol. 2003;98:1107–1111. doi: 10.1111/j.1572-0241.2003.07465.x. [DOI] [PubMed] [Google Scholar]
- 6.McCrea GL, Miaskowski C, Stotts NA, Macera L, Varma MG. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manage. 2009;37:737–745. doi: 10.1016/j.jpainsymman.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastrointest Endosc Clin N Am. 2009;19:117–139. vii. doi: 10.1016/j.giec.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Drossman DA. Functional gastrointestinal disorders: Histor y, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016 doi: 10.1053/j.gastro.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349:1360–1368. doi: 10.1056/NEJMra020995. [DOI] [PubMed] [Google Scholar]
- 10.Pyleris E, Giamarellos-Bourboulis EJ, Tzivras D, Koussoulas V, Barbatzas C, Pimentel M. The prevalence of overgrowth by aerobic bacteria in the small intestine by small bowel culture: relationship with irritable bowel syndrome. Dig Dis Sci. 2012;57:1321–1329. doi: 10.1007/s10620-012-2033-7. [DOI] [PubMed] [Google Scholar]
- 11.Rao SS, Seaton K, Miller MJ, Schulze K, Brown CK, Paulson J, et al. Psychological profiles and quality of life differ between patients with dyssynergia and those with slow transit constipation. J Psychosom Res. 2007;63:441–449. doi: 10.1016/j.jpsychores.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 12.Tantiphlachiva K, Rao P, Attaluri A, Rao SS. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clin Gastroenterol Hepatol. 2010;8:955–960. doi: 10.1016/j.cgh.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 13.Wald A. Etiology and evaluation of chronic constipation in adults. In: Talley NJ, editor. UpToDate. Waltham, MA: UpToDate; 2017. [Google Scholar]
- 14.Rao SS, Azpiroz F, Diamant N, Enck P, Tougas G, Wald A. Minimum standards of anorectal manometry. Neurogastroenterol Motil. 2002;14:553–559. doi: 10.1046/j.1365-2982.2002.00352.x. [DOI] [PubMed] [Google Scholar]
- 15.Minguez M, Herreros B, Sanchiz V, Hernandez V, Almela P, Anon R, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology. 2004;126:57–62. doi: 10.1053/j.gastro.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 16.Rao SS, Kuo B, McCallum RW, Chey WD, DiBaise JK, Hasler WL, et al. Investigation of colonic and whole-gut transit with wireless motility capsule and radiopaque markers in constipation. Clin Gastroenterol Hepatol. 2009;7:537–544. doi: 10.1016/j.cgh.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 17.Camilleri M, Thorne NK, Ringel Y, Hasler WL, Kuo B, Esfandyari T, et al. Wireless pH-motility capsule for colonic transit: prospective comparison with radiopaque markers in chronic constipation. Neurogastroenterol Motil. 2010;22:874–882. e233. doi: 10.1111/j.1365-2982.2010.01517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao SS, PPH, McCallum RW. Handbook of gastrointestinal motility and functional disorders. Thorofare, NJ: Slack Incorporated; 2015. [Google Scholar]
- 19.Sweetser S, ACJ, SOA . DDSEP eight. 2016. pp. 294–295. [Google Scholar]
- 20.Bharucha AE, Pemberton JH, Locke GR., 3rd American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218–238. doi: 10.1053/j.gastro.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lacy BE, Levy LC. Lubiprostone: a novel treatment for chronic constipation. Clin Interv Aging. 2008;3:357–364. doi: 10.2147/cia.s2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lembo AJ, Schneier HA, Shiff SJ, Kurtz CB, MacDougall JE, Jia XD, et al. Two randomized trials of linaclotide for chronic constipation. N Engl J Med. 2011;365:527–536. doi: 10.1056/NEJMoa1010863. [DOI] [PubMed] [Google Scholar]
- 23.Hussain ZH, Everhart K, Lacy BE. Treatment of chronic constipation: Prescription medications and surgical therapies. Gastroenterol Hepatol (N Y) 2015;11:104–114. [PMC free article] [PubMed] [Google Scholar]
- 24.Verne GN, Davis RH, Robinson ME, Gordon JM, Eaker EY, Sninksy CA. Treatment of chronic constipation with colchicine: randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol. 2003;98:1112–1116. doi: 10.1111/j.1572-0241.2003.07417.x. [DOI] [PubMed] [Google Scholar]
- 25.Bosshard W, Dreher R, Schnegg JF, Bula CJ. The treatment of chronic constipation in elderly people: an update. Drugs Aging. 2004;21:911–930. doi: 10.2165/00002512-200421140-00002. [DOI] [PubMed] [Google Scholar]
- 26.Soffer EE, Metcalf A, Launspach J. Misoprostol is effective treatment for patients with severe chronic constipation. Dig Dis Sci. 1994;39:929–933. doi: 10.1007/BF02087539. [DOI] [PubMed] [Google Scholar]
- 27.Rao SS. Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am. 2008;37:569–586. viii. doi: 10.1016/j.gtc.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26:1386–1395. doi: 10.1111/nmo.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hale M, Wild J, Reddy J, Yamada T, Arjona Ferreira JC. Naldemedine versus placebo for opioid-induced constipation (COMPOSE-1 and COMPOSE-2): two multicentre, phase 3, double-blind, randomised, parallel-group trials. Lancet Gastroenterol Hepatol. 2017;2:555–564. doi: 10.1016/S2468-1253(17)30105-X. [DOI] [PubMed] [Google Scholar]