Abstract
To control their reproductive lives, women must have access to all contraceptive methods including the most effective reversible methods, intrauterine devices, and implants. The Contraceptive CHOICE Project, a study of 9,256 women in St. Louis, showed that when barriers to contraception are removed, many women choose intrauterine devices and implants, substantially reducing rates of unintended pregnancy and abortion. This article discusses strategies we learned from the CHOICE Project to improve uptake of the most effective contraceptive methods.
The Public Health Challenge of Unintended Pregnancy
The United States has the highest unintended pregnancy rates among developed nations: more than 45% of pregnancies are unintended nationally.1 In Missouri in 2010, 51% of all pregnancies were unintended with a public cost of $518 million. 1 Approximately one in three women will undergo an abortion during their lifetimes.2 Unintended and teen pregnancy can result in reduced educational or employment attainment as well as increased risk of poverty and poor health outcomes. Although the U.S. has made significant strides in reducing teen pregnancy, it still leads developed nations with a teen pregnancy rate of 52.4 pregnancies per 1,000 15–19 year-olds.3 In surveys, U.S. women report that their ideal family includes just two children,4 meaning that women spend nearly three decades of their reproductive lives trying to avoid or prevent pregnancy. Additionally, regardless of desired family size, most women and families report that timing and spacing of their pregnancies is important, citing a variety of medical, social, and economic reasons.5–7 The inconsistency between the actual rates of unintended pregnancy and women’s ideal reproductive life plans suggests that women are not receiving the contraceptive care they want and need.
Delivery of Contraceptive Care
The provision of contraceptive care has long been the role of the obstetrician-gynecologist and the family medicine practitioner. However, assessing family planning needs is the responsibility of all medical professionals, especially those treating reproductive-age women with chronic medical conditions. Historically, both women and clinicians have chosen oral contraceptive pills (OCPs), with little discussion about the appropriateness of the methods or discussion of other options. Because OCPs require daily compliance, the failure rate can be as high as 9% with typical use. In contrast, the most effective reversible methods, long-acting reversible contraceptives (LARCs), including intrauterine devices (IUDs) and the contraceptive implant, are “forgettable” and have typical use failure rates of less than 1%. Although use of LARCs has increased from 2.6% to 11.7% over the last few years, OCPs, female sterilization, and male condoms remain the most frequently used methods in the U.S. at 25.9%, 25.1%, and 15.3% respectively.8 Increased awareness about and access to LARCs can increase the use of these methods.
The Contraceptive CHOICE Project
The Contraceptive CHOICE Project, a prospective cohort study of 9,256 reproductive-age women in the St. Louis area, illustrated a model of contraceptive care that can help women achieve their reproductive life goals. The project was designed to evaluate the impact of eliminating common barriers such as education, access, and cost on the uptake of LARCs. The CHOICE Project enrolled a racially and economically diverse group of women aged 14–45. Participants underwent a standardized contraceptive counseling session with a trained non-clinician in which all available reversible methods were discussed in decreasing order of effectiveness (e.g., IUD and implants first and condoms last). Participants chose and received their desired method on the day of enrollment at no out-of-pocket cost. We followed participants for two to three years depending on the time of enrollment. Participants were allowed to switch methods if they were dissatisfied with their initial chosen method. Study outcomes included method choice, continuation, satisfaction, and rates of unintended pregnancy and abortion.
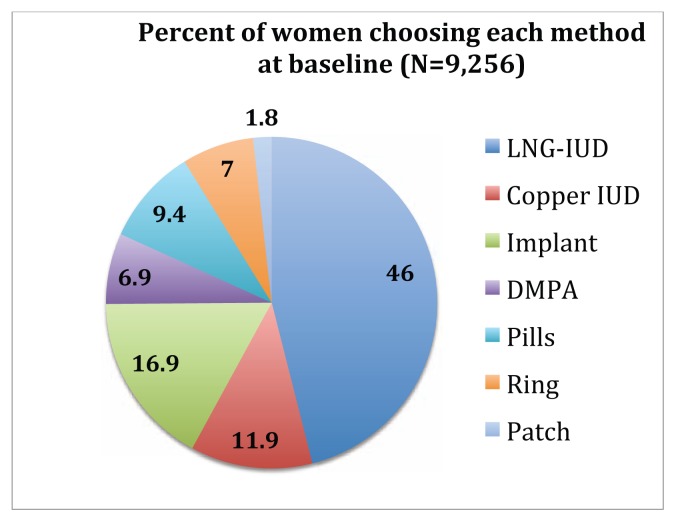
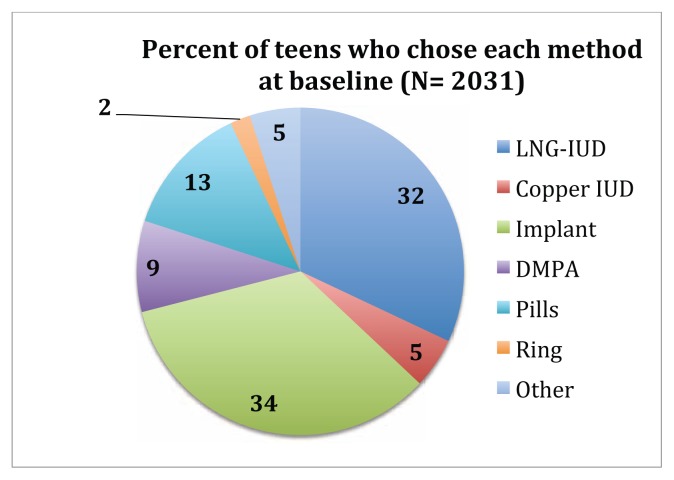
Among the 9,256 women enrolled, 75% chose a LARC method at enrollment; 46% of women chose the levonorgestrel IUD, 12% chose the copper IUD, and 17% chose the etonogestrel implant (see Figure 1).9 Women chose LARC methods at over 10 times the rate of the general U.S. population, and LARC users reported higher rates of continuation and satisfaction than non-LARC users.10 Additionally, similar to adult women in our cohort, more than 70% of adolescent girls chose a LARC method (see Figure 2), and their rates of continuation and satisfaction were similar to older women. 11,12 This finding should reassure clinicians that when young women choose a long-acting method, they are likely to be satisfied with and continue use of the method.
Figure 1.
Distribution of Contraceptive Method Choice at Baseline in the Contraceptive CHOICE Project.
DMPA, depot medroxyprogesterone acetate injection; IUD, intrauterine device; implant, levonorgestrel implant; pills, oral contraceptive pills; ring, vaginal ring
Figure 2.
Distribution of Contraceptive Method Choice at Baseline for Teen in the Contraceptive CHOICE Project.
The CHOICE Project validated the superior effectiveness of LARC; users of shorter-acting methods such as OCPs, the contraceptive patch, and the vaginal ring were 22 times more likely to experience an unintended pregnancy than IUD and implant users.13 Although we found no difference in unintended pregnancy by age among LARC users, we found that OCP, contraceptive patch, and vaginal ring users under the age of 21 were twice as likely as adult women to experience an unintended pregnancy.13
The potential population impacts of our inter vention are profound. We found that rates of abortion amongst CHOICE participants were less than half of the regional and national rates.9 These findings were consistent across age demographics. Most notably, compared to teens nationwide, CHOICE teens had 75% lower rates of pregnancy, birth, and abortion.11
Strategies to Improve Contraceptive Care
The CHOICE Project was designed to address multiple barriers to reversible contraception. We argue that many of the strategies from the CHOICE Project can be implemented or adapted to improve contraceptive care in every day practice. We highlight three key barriers to contraceptive care that CHOICE addressed: cost, education, and access.
Cost
The CHOICE Project eliminated the cost of the contraceptive method by providing all methods free of charge to participants. The public health community, including the Institute of Medicine, the Centers for Disease Control and Prevention (CDC), and the American College of Obstetricians and Gynecologists, have identified contraception as an essential part of preventive care. As such, these institutions have advocated for contraception to be a covered benefit of all health insurance without cost sharing. Although the Affordable Care Act included this provision, implementation has become entangled in political discourse. As a result, many women still struggle to secure affordable access to their desired contraceptive method. The CHOICE Project team continues to advocate on the local, regional, and national levels for equitable and affordable access to contraceptive care for all women.
Education
Early in the CHOICE Project, we found that most women had limited knowledge about available methods; participants generally underestimated the effectiveness of LARC and overestimated the effectiveness of OCPs, the patch, and the ring.14 To address this knowledge gap effectively, we delivered education on all reversible methods in a standardized fashion beginning with the most effective methods.15 This structured approach to counseling may allow women to more accurately consider the risk of method failure while deciding which method is best for them. In addition, the CHOICE model used trained non-clinician educators. This helped remove the time constraints of a clinician’s schedule and allowed the patient adequate time for counseling. Other practice setting have adapted this model and trained medical assistants or nurses for this role.
Education barriers are not limited to patients, and many myths surrounding LARC still exist amongst practicing clinicians. To best serve our patients and their contraceptive needs, we must be vigilant in providing evidence-based care.
Access – Same-day Initiation
One of the most important ways that the CHOICE Project reduced barriers to contraception, particularly LARC methods, was by providing same-day initiation when medically appropriate. Data from other studies clearly demonstrate that any delay in delivery of a desired method increases the patient burden, increases the risk that the woman will become pregnant before returning for care, and decreases the likelihood that the patient will actually receive a contraceptive method.16,17 LARC methods are often not inserted on the same day they are chosen for a multitude of reasons. One of the most common reasons cited is concern about the possibility of a luteal-phase pregnancy. To reasonably rule out a pregnancy, clinicians can make use of the simple checklist provided by the CDC Selected Practice Recommendations18 (see Table 1). In the CHOICE Project, only 0.5% of women were diagnosed with a luteal-phase pregnancy following enrollment, suggesting that the overall risk is very low.19 Another reason some providers are unwilling to place a same-day LARC method is concern about infection. The CDC’s Medical Eligibility Criteria for Contraceptive Use provides evidence-based indications for contraceptive use.20 The most recent publication supports following CDC recommendations for Chlamydia trachomatis and Neisseria gonorrhea screening and placing the LARC method, including IUDs, at the time of screening. Women with positive tests should be treated as soon as possible but do not need to have their IUDs removed. Although other sexually transmitted infections are not a contraindication to LARC placement, a history of pelvic inflammatory disease and post-partum or post-abortion endometritis within the past three months is a contraindication to IUD insertion.
Table 1.
How to be reasonably certain a woman is not pregnant
| How to be reasonably certain a woman is not pregnant |
If a patient has no symptoms or signs of pregnancy and meets any one of the following criteria:
|
Adapted from CDC Select Practice Recommendations. http://www.cdc.gov/reproductivehealth/contraception/usspr.htm
A final potential barrier to same-day LARC insertion is the concern that an unscheduled insertion will delay clinic flow. Health centers can use several strategies to help maximize the efficiency of visits, keeping in mind that every visit should be viewed as an opportunity to address a woman’s reproductive life plan and thus an opportunity to reassess contraceptive use. First, if all members of the health care team are knowledgeable about contraception, including LARC methods, they can counsel patients, thereby freeing up clinician time. Second, use of decision aids or informational videos in the waiting room can help patients identify factors that are important to them in choosing a contraceptive method. Finally, creating instrument packs containing all required supplies for LARC insertion can help streamline procedures.
Access – Immediate Postpartum LARC Placement
Another strategy to increase access to LARC methods is to provide IUDs and implants in the immediate postpartum setting, as recommended by the American College of Obstetricians and Gynecologists.21 This is important because up to 45% of women report having unprotected intercourse before the routine six-week postpartum visit, putting them at risk for rapid repeat pregnancy.22 Provision of LARC methods in the immediate postpartum period can reduce this risk, and there are few contraindications to providing these methods in this setting. Twenty-one state Medicaid programs, including Missouri’s, reimburse for IUDs and implants in the postpartum hospital setting. Although rates of IUD expulsion are higher after immediate postpartum insertion than at other times (10–27% vs. 2–10%),23 this risk is likely offset by the low rates of postpartum follow-up among women at highest risk for rapid repeat pregnancy.
Access – Special Populations
We highlight four populations in which LARC methods are often not used but in which use could increase. First, women receiving emergency contraception most commonly receive oral levonorgestrel or ulipristal acetate. However, the copper IUD has been shown to be the most effective form of emergency contraception, greater than 99% effective within 120 hours of unprotected sexual intercourse. The copper IUD has the added benefit of providing “forgettable” contraception, thus nearly eliminating the chance that a woman will need emergency contraception again. Second, LARC methods are appropriate for and acceptable to adolescents. Although some providers have been reluctant to provide LARC methods to teens, this practice is supported by both the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists.24, 25 Third, with the increasing epidemic of obesity, consideration of effectiveness of methods in women of varying body mass index is relevant. Importantly, data from CHOICE demonstrated that LARC methods are equally effective regardless of body mass index.26 Finally, women who have been using the 52 mg letonorgestrel-IUD or the etonogestrel implant for their FDA-approved durations can continue to use these methods for at least one more year without fearing any loss of effectiveness.27–28
Thoughts and Conclusion
The contraceptive and family planning needs of our patients are diverse, but with attention to reducing barriers to the most highly effective contraceptive methods, we can better help women plan and space their pregnancies. Preventing unintended pregnancy is an important way to reduce maternal and neonatal morbidity and mortality and help our patients reach their education, career, and life goals.
Biography
Colleen McNicholas, DO, MSCI, (left), Assistant Professor, Division of Family Planning, and Tessa Madden, MD, MPH, (right), Associate Professor, Director, Division of Family Planning; both in the Department of Obstetrics and Gynecology, Washington University School of Medicine.
Contact: mcnicholasc@wudosis.wustl.edu


Footnotes
Disclosure
None reported.
References
- 1.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. New England Journal of Medicine. 2016;374(9):843–852. doi: 10.1056/NEJMsa1506575. http://nejm.org/doi/full/10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones RK, Kavanaugh M. Changes in Abortion Rates Between 2000 and 2008 and Lifetime Incidence of Abortion. Obstet Gynecol. 2011;117(6):1358–1366. doi: 10.1097/AOG.0b013e31821c405e. [DOI] [PubMed] [Google Scholar]
- 3.Kost K, Maddow-Zimet I. U.S. Teenage Pregnancies, Births and Abortions, 2011: State Trends by Age, Race and Ethnicity. New York: Guttmacher Institute; 2016. http://www.guttmacher.org/report/us-teen-pregnancy-state-trends-2011. [Google Scholar]
- 4.Institute TG. Fulfilling the Promise: Public Policy and U.S. Family Planning Clinics. New York: Guttmacher Institute; 2000. [Google Scholar]
- 5.Mayer JP. Unintended childbearing, maternal beliefs, and delay of prenatal care. Birth. 1997;24(4):247–252. doi: 10.1111/j.1523-536x.1997.tb00598.x. [DOI] [PubMed] [Google Scholar]
- 6.Barber JS, Axinn WG, Thornton A. Unwanted childbearing, health, and mother-child relationships. J Health Soc Behav. 1999;40(3):231–257. [PubMed] [Google Scholar]
- 7.Orr ST, Miller CA, James SA, Babones S. Unintended pregnancy and preterm birth. Paediatr Perinat Epidemiol. 2000;14(4):309–313. doi: 10.1046/j.1365-3016.2000.00289.x. [DOI] [PubMed] [Google Scholar]
- 8.Kavanaugh M, Jerman J, Finer L. Changes in the use of long-acting reversible contraceptive methods among US women, 2009–2012. Obstet Gynecol. 2015;126(5):917–25. doi: 10.1097/AOG.0000000000001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–1297. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117(5):1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014;371(14):1316–1323. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120(6):1298–1305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 14.Eisenberg DL, Secura GM, Madden TE, Allsworth JE, Zhao Q, Peipert JF. Knowledge of contraceptive effectiveness. Am J Obstet Gynecol. 2012;206(6):479 e471–479. doi: 10.1016/j.ajog.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88(2):243–249. doi: 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tocce K, Sheeder J, Python J, Teal SB. Long acting reversible contraception in postpartum adolescents: early initiation of etonogestrel implant is superior to IUDs in the outpatient setting. J Pediatr Adolesc Gynecol. 2012;25(1):59–63. doi: 10.1016/j.jpag.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Bergin A, Tristan S, Terplan M, Gilliam ML, Whitaker AK. A missed opportunity for care: two-visit IUD insertion protocols inhibit placement. Contraception. 2012;86(6):694–697. doi: 10.1016/j.contraception.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Division of Reproductive Health NCfCDP, Health Promotion CfDC, Prevention. U.S. Selected Practice Recommendations for Contraceptive Use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. MMWR Recomm Rep. 2013;62(RR-05):1–60. [PubMed] [Google Scholar]
- 19.Min J, Buckel C, Secura GM, Peipert JF, Madden T. Performance of a checklist to exclude pregnancy at the time of contraceptive initiation among women with a negative urine pregnancy test. Contraception. 2015;91(1):80–84. doi: 10.1016/j.contraception.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65(3):1–103. doi: 10.15585/mmwr.rr6503a1. [DOI] [PubMed] [Google Scholar]
- 21.Committee Opinion 670. Immediate Postpartum Long-Acting Reversible Contraception. Obstet Gynecol. 2016;128(2):e32–37. doi: 10.1097/AOG.0000000000001587. [DOI] [PubMed] [Google Scholar]
- 22.Brito MB, Ferriani RA, Quintana SM, Yazlle ME, Silva de Sa MF, Vieira CS. Safety of the etonogestrel-releasing implant during the immediate postpartum period: a pilot study. Contraception. 2009;80(6):519–526. doi: 10.1016/j.contraception.2009.05.124. [DOI] [PubMed] [Google Scholar]
- 23.Lopez LM, Bernholc A, Hubacher D, Stuart G, Van Vliet HA. Immediate postpartum insertion of intrauterine device for contraception. Cochrane Database Syst Rev. 2015;(6):CD003036. doi: 10.1002/14651858.CD003036.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adolescents and long-acting reversible contraception: implants and intrauterine devices. Committee Opinion No. 539. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120:983–8. doi: 10.1097/AOG.0b013e3182723b7d. [DOI] [PubMed] [Google Scholar]
- 25.Contracpetion for Adolescents. American Academy of Pediatrics Policy Statement. Pediatrics. 2014;134(4) [Google Scholar]
- 26.Xu H, Wade JA, Peipert JF, Zhao Q, Madden T, Secura GM. Contraceptive failure rates of etonogestrel subdermal implants in overweight and obese women. Obstet Gynecol. 2012;120(1):21–26. doi: 10.1097/AOG.0b013e318259565a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNicholas C, Maddipati R, Zhao Q, Swor E, Peipert JF. Use of the etonogestrel implant and levonorgestrel intrauterine device beyond the U.S. Food and Drug Administration-approved duration. Obstet Gynecol. 2015;125(3):599–604. doi: 10.1097/AOG.0000000000000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ali M, Akin A, Bahamondes L, et al. Extended use up to 5 years of the etonogestrel-releasing subdermal contraceptive implant: comparison to levonorgestrel-releasing subdermal implant. Hum Reprod. 2016 doi: 10.1093/humrep/dew222. [DOI] [PMC free article] [PubMed] [Google Scholar]