Abstract
Purpose:
Despite the evidence, the availability since 2006, and strong recommendations from many professional organizations, the human papillomavirus (HPV) vaccine has had a low uptake rate nationally and these trends have been even lower in the state of Virginia.
Design and Methods:
We explored key stakeholders’ perspectives on factors influencing HPV vaccination in central and southern Virginia organized within the socio-ecological model (SEM) framework. We conducted semi-structured key informant interviews with 31 stakeholders involved in HPV vaccination or cancer prevention.
Results:
Stakeholders identified barriers at all SEM levels: Knowledge gaps and sexuality concerns (parent-child dyad level), time constraint and inconsistent recommendation (interpersonal level), lack of leadership and informational support (organizational and community level), and an ineffective mandate (policy level). Facilitators identified were realistic/receptive attitude (parent-child dyad level), provider’s strong recommendation and educational support (interpersonal level), team approach and useful data (organizational level), educational outreach and community resources (community level), and support from federal and professional organizations (policy level).
Conclusions:
The stakeholder analysis provided an environmental scan of the barriers and facilitators so that an effective HPV vaccination strategy can be planned and implemented in the Commonwealth of Virginia by public health nurses.
Keywords: HPV vaccines, barriers, facilitators, socio-ecological model, Virginia, stakeholders
Background
Every 20 minutes, someone in the United States is diagnosed with a human papillomavirus (HPV)-associated cancer, and most are acquired in young adulthood (Center for Disease Control and Prevention (CDC), 2014). With more than 79 million individuals infected and 14 million new cases each year, HPV infection is the most common sexually transmitted infection in the United States (Satterwhite, Torrone, Meites, Dunne, Mahajan, Ocfemia, & Weinstock, 2013). While most cases resolve spontaneously, persistent infections with HPV types 6, 11, 16 and 18 are most concerning because they lead to 26,000 new cancer cases annually and 90% of anogenital warts (CDC, 2012). The annual burden of HPV-related treatment for women is 3 million cases at a cost of $7 billion (CDC, 2015).
To counter this statistic, vaccines are available and recommended by the Advisory Committee on Immunization Practices (ACIP) for all young women ages 9 to 26, and to young men ages 9 to 21 (CDC, 2010; Centers for Disease Control and Prevention (CDC), 2007; Petrosky, Bocchini, Hariri, Chesson, Curtis, Saraiya, Markowitz, 2015). Despite endorsement by many professional organizations (AAFP, AAP, ACOG, ACP, CDC, 2014; Association of Women’s Health, 2010) and from the leading 69 National Cancer Institute-designated cancer centers (National Cancer Institute, 2016), the initiation and completion rate of HPV vaccination series nationally in 2016 is only at 65.1% and 49.5% for young women, 50.6% and 37.5% for young men respectively (Walker et al., 2017). In Virginia, the rate is lower at 53.6% for initiation and 39.2% completion for young women, and 56.4% initiation and 37.4% completion for young men (Walker et al., 2017). The completion rate nationally and in Virginia is far below The Healthy People 2020 goal of 80% for all three injections (United States Department of Health and Human Services, 2011) and many young men and women are still at risk for developing this highly preventive cancer and infection. Of note, in 2016 the HPV vaccination recommendation changed from three to two vaccines for those young men and women who initiate the series prior to the age of 15 (Walker et al., 2017).
Virginia is unique because, in 2008, it was the first state to mandate HPV vaccination for adolescent girls entering middle school (Keim-Malpass, Mitchell, DeGuzman, Stoler, & Kennedy, 2017). However, this legislation has faced numerous threats of appeal, and many experts have criticized its opt-out policy as being too generous because parents/caregivers can opt out for any reason, and the policy only excluded boys (Keim-Malpass et al., 2017; Pitts & Adams Tufts, 2013). Only one published study has assessed the policy context in Virginia and assessed parental response to the Virginia HPV vaccination mandate. Pitts and colleagues (2013) found that parents had less trust in the vaccine because of the mandate due to the perceived political involvement and general uncertainty of government vaccination mandates.
As may be the case in other states, the presence of rural and medically underserved communities in the Commonwealth of Virginia may contribute to problems with vaccine uptake. Many of the Virginia’s counties are designated as “rural” (46%) and “medically underserved” (72%) according to the Health Resources and Services Administration (HRSA, 2018). A study conducted in Kentucky found a 7-fold decrease in rural women versus urban women returning for a follow-up vaccine doses despite the vaccine being free of charge (Crosby, Casey, Vanderpool, Collins, & Moore, 2011).
Population-based research to date has identified several key factors contributing to the lagging HPV vaccination rate. The most common barriers were cost (Ferrer, Trotter, Hickman, & Audrey, 2014; Garcini, Galvan, & Barnack-Tavlaris, 2012), individual/parental barriers (Rambout, Tashkandi, Hopkins, L., & Tricco, 2014), lack of health care providers’ recommendations at the interpersonal level (Bartlett, & Peterson, 2011; Head, Vanderpool, & Mills, 2013; Kessels, Marshall, Watson, Braunack-Mayer, Reuzel, 2012), and health disparities (Gelman, Miller, Schwarz, Akers, Jeong, & Borrero, 2013). Strong facilitators of HPV vaccination included health care provider’s recommendations, free HPV vaccines, and positive vaccine attitudes held by parents and young adults (Holman et al., 2014). The interactions of the various levels of the socio-economical model showed that overall, women who live in the South (Rahman, M., Laz, 2013), have low-income (Jeudin, Liveright, Del Carmen,, & Perkins, 2014), and are of racial/ethnic minorities (Gelman, Miller, Schwarz, Akers, Jeong, & Borrero, 2013) were less likely to initiate and/or complete the vaccination series.
The socio-ecological model (SEM) posits that complex interactions at the intrapersonal, interpersonal, organizational, community, and public policy levels shape health behavior (McLeroy, Bibeau, Steckler, & Glanz, 1988). For the adolescent, health care decision is often tied to the parent and labeled as “Parent-child dyad” at the intrapersonal level. Public policy, community support programs, and institutional processes further impact HPV vaccination. To better understand barriers and facilitators to HPV vaccination, the interactions between these levels are examined. The purpose of this study is to identify barriers and facilitators to HPV vaccination using the SEM model as a conceptual framework for improving HPV vaccination initiation and uptake in young men and women ages 9 to 26. The data from this study will provide an environmental scan so that future programs can be developed to improve the HPV vaccination rate and cancer prevention in Virginia.
Material and Methods
A descriptive qualitative study was initiated using a purposive sampling technique to identify stakeholders involved with aspects of care related directly to HPV vaccination (pediatrics, family medicine, women’s health, state Health Departments), policy, industry, research, or cancer outreach/community engagement. Individuals not involved in HPV vaccination or cancer outreach were excluded. Twenty-eight interviews with 31 stakeholders were conducted over the phone or in person. The interviews occurred individually or in a group setting. Stakeholders were identified as registered nurses or nurse practitioners (n=7), medical doctors (n=7; with specialty in pediatrics, family practice, gynecology, oncology, and pathology), pharmacy or industry (n=5), health department (n=5), community programs (n=6), and health research professors (n=4). Since stakeholders had multiple roles, the roles identified do not equal to 31. The stakeholders had an average of 12.5 years of experience, with a range of one month to 48 years of experience or in their current position. Stakeholders represented public and private institutions. Ten stakeholders provided direct patient care with regard to HPV administration and/or education.
After IRB approval, a primary investigator sent an email message to all stakeholders requesting that they email or schedule the interview. The email message contained information regarding the study, confidentiality and protection of identity, risks, benefits, and voluntary nature of the interview. We conducted the interview via phone or during a site visit using the key informant semi-structured questions. After consent for recording, a digital voice recorder was used to record the interview so that an accurate transcription could be done for later review and analysis. The interview recording was transcribed verbatim. The interviewer also took written notes to capture the key points of each interview. If the individual stakeholder did not agree to audio recording (n=2), we sent the typed interview summary to the stakeholder for review to ensure the accuracy of the information.
Qualitative methods were guided by conventional content analysis. Members of the research team applied codes to the qualitative interviews line-by-line using the a priori framework provided by the SEM model. Coded lines were grouped to form inductively derived themes. Final theme development was reached through consensus among the research team. Trustworthiness was addressed by the lead author reflecting on prior assumptions and beliefs about the topic and allowing for an open review and audit process among the research team.
Results
Several barriers and facilitators were identified at all levels of the SEM and are shown in Figure 1. Themes and exemplars for barriers are described in Table 1 and for facilitators in Table 2.
Figure 1. Barriers and facilitators identified by stakeholders outlined in the Socio-Ecological Model framework.
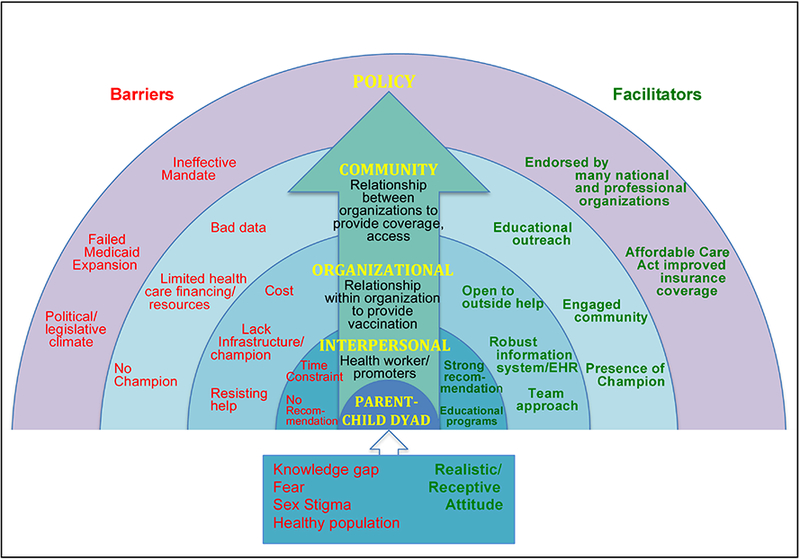
Table 1.
Themes and Exemplars Regarding HPV Vaccination Barriers
| PARENT-CHILD DYAD |
Knowledge gap “I think the consumer education, the people who need to be educated, the parents who are resistant, or the young adult who are resistant…. sometimes their readiness to learn…if they don’t want to know, they may not be open to the information.”--Community program (1) “Perhaps lack of education, lack of information. Being unclear about how to get the vaccine, where to get the vaccine.”--Professor Fear “I hear a lot of people who are concerned about vaccinations in general.”--Community program (1) “For some people, it may be understanding and trusting that it’s beneficial.”--MD “Vaccine hurts. After they get the first one, they are a little timid on #2 and #3. That’s probably the biggest comment we get from the recipients.”--Pharmacy Sex Stigma “Well boys also, I mean. It’s interesting, it seems….and we looked at our data not too long ago..it seems that parents are more concerned about giving it to girls than they are boys. (chuckle). Boys are expected to stray I guess, (more chuckle), but they don’t seem to be that concerned.”--Health Dept “And I think one of the other main hesitation points that we hear from parents is that they don’t understand why their child need to be vaccinated against a disease that is sexually transmitted at such a young age when they believe or hope that their child won’t be sexually active until later on.”--RN Healthy Population “It focuses on adolescents who don’t have to come in to the doctor’s office as often maybe unless they are doing a school physicals or things like that.”--Health Dept “Most of the children at this age don’t go to the doctor regularly, they only go for sports or when they’re sick. So the fact that if it’s not part of the regular routine of booster, it’s easily fall of the radar.”--Community program (2) |
| INTERPERSONAL |
No Recommendation “Meaning that the physicians are not promoting the vaccine as good medicine to their patients. They have no problem promoting the other vaccines, but HPV vaccine stands alone, as you know being promoted. I think it’s a failure of physician leadership. Failure of physicians to being willing to say this is an unequivocally terrific medicine.”--MD “Immunization is not central to family medicine so they are not proactive and making strong recommendations toward all vaccines.” --Industry “The biggest barriers in my view are physicians are not recommending and not following through on vaccinations. But the problem is that the folks who need to do the vaccination are the pediatricians. Or family medicine. Most people don’t get their gyn exam until they are almost out of the window for vaccination.” --MD “They have been counseled by previous physicians in their local, rural area that they lived in. The physician advised against it. That was the barrier.”--RN Time Constraint “Providers are always difficult to reached because of their available time…. how do you reach people who are busy.”--Community program “I think that so much falls on the nurses that they don’t have the time to routinely go out their way to find these vaccine or what not.’’--Health Dept “A lot of the feedback that we got from physicians and nurses were that there wasn’t always times to talk about it and if the patient/parent didn’t bring it up, most of the time it didn’t get addressed.”--Community program (1) “One of the biggest challenges is, really has nothing to do with the vaccine itself, it’s just on top of everything else because we talk about vaccine every time - Making sure we address it, making sure one of us can do it notably our nurse who is being pulled in different directions. So our intentions are honorable. So the biggest challenge/barrier is making sure we include that in the visits as far as time.”--NP |
| ORGANIZATIONAL |
Cost “It’s expensive, but if you have insurance it’s covered. If you don’t have insurance and you are Medicaid or un-insured and you go to the VFC then it’s provided to you based on your inability to pay. So I don’t think so, but I don’t know. Maybe that’s unknown. Maybe people don’t know what access they have if they have limited resources.”—Pharmacy “One thing that I’ve noticed, a lot of the Ob offices are not carrying the HPV vaccine…”--Health dept “Cost is a barrier, but I don’t know how much of a barrier other than access. Is it cover by Medicaid or any of the children’s program?” -Community program (1) Lack infrastructure/Champion “So the alternative is to have the insurers and/or organizations make it a performance criteria.” -MD “Currently lack infrastructure to schedule that far out for a nursing visit, lack of infrastructure to determine how is behind in immunizations, VIIS not efficient). Currently: letting them schedule them own, low number that do.”--MD “Organizations don’t place immunization as high enough of priority; more focus on chronic illnesses.”--Industry Resisting Help “Access to organization --people won’t let you in the door because (1) perception with industry that collaborating is negative (2) time constraint - providers are overwhelm with managing changes to healthcare; perception of disruption to busy schedule (3) hard to get one-on-one time with providers/doctors- perception of distrust, that there is a catch. Providers do not realize that drug industry have changed too, more collaboration rather than selling.”--Industry “And then I guess a challenge off of that is also the lack of time that I noticed with providers saying, “Well, we don’t have time to go to another system to look up record.”--Health Dept |
| COMMUNITY |
Bad Data “One is my concern that we don’t have very good data on just how well or how badly we’re doing. A lot of it is guesstimates based on national data and or limited sources such as VIIS and the Vaccine For Kids program.”--Community program (1) “Because Virginia Immunization Information System is a voluntary system in Virginia, our rates still tend to be showing lower maybe than what the national average or what Virginia’s average are.”--Health Dept Limited Health Care Financing/Resources “Funding is definitely a challenge that changes from year to year… We also have a lot of trouble with transportation in this area. It’s very mountainous area so it’s difficult for people to get to where they need to get to.”--Health Dept “Well, we know that ethnic minorities tend to have more difficulty to access health care to begin with. [A]nd that (vaccine assistance programs) might actually promote access, but general speaking we know that low-income minorities tend to have more difficult barriers to health care both because some providers don’t take Medicaid.”--Professor No Champion “I would like to see the same amount of attention. I know it’s a little harder because the scope of it is a little bit different, but I think any attention it has gotten that way has been negative unfortunately. So basically having someone willing to fight back against that will be really nice.”--RN “I think you got to first, we live in an area with a strong, fundamental religious approach. And somehow, I think as well as nationwide this discussion of HPV has been about sex, where it should be about cancer. I think we get too many moral voices on this….I think the medical community needs to really step forward instead….”--Community program(2) |
| POLICY |
Ineffective mandate “Other barrier is that it’s not a school requirement vaccine in Virginia. So parents thinking, ‘Well if I don’t have to have it, then I don’t need to get it.’ And medical providers thinking also, ‘Well if it’s not required by schools…’ and so it’s being treated more as a optional vaccine…”--Health Dept “There’s not accountability for that requirement so that bring the message to parent and they seem to interpret it as that maybe this vaccine is not as important as some of the other school-required vaccines.”--RN “Currently the mandate is only for girls, not for boys. And while parents can opt out of the mandate, there’s no way to determine it in the data versus, in the tracking, if a parent opt out because they chose not to or were they not even asked about immunization for their child.”--Health Dept Failed Medicaid Expansion “Since the state of Virginia chose not to expand Medicaid under the Affordable Care Act, we have a lot of people kinda trapped. They’re making a little too much for Medicaid but they don’t make enough to be able to go into the health exchange of the Affordable Care Act”--Community program (2) “The big challenge is there are people who don’t have any healthcare at all or the people that fall through the crack because they don’t have Medicaid Expansion. Vaccinations are expensive.”--MD Political/Legislative Climate “I do think that the resistance to the mandate has been a problem and there has been numerous efforts over the years to get that off the book. So any attempt to do better legislatively risk losing what we got. I think that some of the conservative elements, and I don’t mean political conservative, but just very conservative religious conservative. What family should do, and not what society should do …that those are barriers we’re going to have to deal with in large part of the commonwealth and in this catchment area.”--Community program (2) |
Note: RN = Registered Nurse; NP = Nurse Practitioner; MD = Medical Doctor; VIIS = Virginia Immunization Information System
Table 2.
Themes and Exemplars Regarding HPV Vaccination Facilitators
| PARENT- CHILD DYAD |
Realistic and receptive attitude “I think our clinic, our families are receptive to it. They have realistic perceptions about adolescent sexual activity and want their kids protected. For the most part, our patient population at our teaching clinic are very open to vaccine.”--MD “For most people we tell them that they are due for vaccines and we have the VIIS information sheet. And they say, ‘Okay’”--NP |
| INTERPERSONAL |
Strong Recommendation “And that the provider will recommend it because, as oppose to our recommending it. The provider’s is one of the best predictor of whether patients would get the vaccine.”--Community program (1) Provider Education programs “So finding ways that will help families understand that this vaccine prevent cancer and you have to receive it before you become sexually active in order for it to provide the best protection. Somehow getting that message across in a positive way….”--RN “And so, physicians have to deal with these crazy schedules and the timing of these things. And so we just have to make it clear to them and provide them with the tools to deal with the patients that are coming to them.”--Health Dept “I think our outreach educations to providers in lecture format has been well received. People have said that they’ll change how they’re presenting the vaccine to their patients and families.”--MD |
| ORGANIZATIONAL |
Team Approach “Takes a multi-factorial, standardized approaches (patient education, provider education, reminder system, use of EMR). Use ideas from CDC.”--Industry “I know that for a fact when it first came out, we sat down with the criteria and the education available and went over it with the nurses. I myself met with the physicians prior to that meeting just to make sure they were on board with exactly we wanted to do as far as the age range.”--RN “No matter what they come for, we have their record and then we update it. And trying to get them scheduled before they leave.”--RN Robust Information System /EHR “What works well: (1) Electronic health record (EHR) set-up for reminder—this is a best practice; (2) put in hands of clinical staff through standing orders and standard practice; good system for call back; follow-up appointments for 2nd and 3rd shots before leaving.”--Industry Open to Outside Help “Because some of the states are further ahead than we are and their rates are better. There have been some really good webinars like the CDC webinar from Florida and Georgia where the rates were worse than Virginia, but these small practices have really revved how they educated their patients, how they challenged their doctors and I think we can all learn from their successes.”--Community program (2) |
| COMMUNITY |
Educational Outreach “…CDC recommends that we try to educate the providers to push it as of the regular vaccines, just like any other school requirement….I think as more vaccine education is being done on HPV, which there is a lot of resources out there, but just getting it to the people that really need it.” -Health Dept “ “[The Cancer Coalition of Virginia] did a number of initiatives related to HPV for the last 5 years and have generated a lot of interest in making certain that HPV stays top of minds in public health.”--Community program (2) “There definitely need to be consistent messaging across all sectors and then coordinated effort. We can’t have one group saying one thing and another group recommending something else. Consistent and coordinated.”--Health Dept Engaged Community “I think we have a really good health department. I think that anything they issue is very positive so we feel supported. I feel supported by them. There seems to be consistency in the message as compare to the family practice.”--NP “I think that it’s an engaged population more than other areas. I think the strengths is that we have the University and a lot of really great public health programs and resources for people to tap into.”-- Community program (2) “We (Women’s Health Virginia]) are also actively involved with the Cancer Action Coalition of Virginia and the cancer plan has a goal of increasing uptake of HPV vaccines.”--Community program(2) Presence of Champion “That’s one of the reasons we brought an Adolescent Coordinator on.”--Health Dept |
| POLICY |
Endorsed by Professional Organizations “It’s been promoted by the CDC. In the last year, CDC has had incredibly strong messaging. Every organizations that’s out there promote/say, ‘HPV vaccine…recommended for boys and girls, boys and girls.” There’s no medical organizations.there’s no organization in organized medicine that doesn’t recommend HPV vaccine.” --MD Affordable Care Act (ACA) “Immunization is important prevention. Affordable Care Act focuses on prevention so can improve vaccination rate, but it will be slow going.”--Industry “Clearly the ACA requires health insurance plans to offer screenings and vaccines and preventative services that are recommended by the US Preventive Services Task Force. And to the extent that any vaccine is recommended, then the ACA would provide coverage for that vaccine which could expand access to it.”--Professor |
Note: RN = Registered Nurse; NP = Nurse Practitioner; MD = Medical Doctor; VIIS = Virginia Immunization Information System
Parent-Child Dyad Level
Stakeholders identified knowledge gap, fear, sexuality belief, and healthy adolescents as barriers to care at the parent-child level. Often parents did not perceive the HPV vaccine as a routine part of adolescent care and did not schedule an appointment unless the child was sick or needed a sports physical. Once at the appointment, the parents frequently expressed concerns and fear regarding the vaccine safety, efficacy, side effects, and what they heard from social media. The adolescents also mentioned the fear of needles as a barrier to initiating and completing injections. Parents also articulated that they did not think their children needed the vaccine because of their religion, or because their children were not sexually active, or that the vaccine promoted promiscuity. A small group of parents were not interested in any vaccine or the government or doctors telling them what their child needed or did not need. Knowledge regarding the cost associated with the vaccine and the medical visit may also prohibit some parents or young adults from accessing care. Lack of knowledge regarding the need, how to, and when to return for subsequent injections also prevented many adolescents from receiving their second and third shots.
Interpersonal Level
Time constraint and inconsistent or lack of recommendation by the health care provider (HCP) are barriers at the Interpersonal level. Gynecologists and oncologists involved with treating HPV-related cancers strongly recommended the vaccines and cannot understand why the vaccination rate is not higher. One stakeholder said that pediatricians and family practice providers are not making the strong recommendation for the vaccine and organizations are not holding them accountable. OB/GYN providers may not offer the vaccine because they typically don’t see the younger range of the recommended age group and when they do, it’s often after sexual activity has been initiated. Providers acknowledged that it may be difficult for young adults to locate a healthcare provider who will accept and file insurance for the vaccinations. Another barrier HCPs reported is that they have a difficult time getting adolescents to their appointment because they are usually healthy, and the parents don’t seek wellness appointments for them. Many providers reported addressing vaccination only at wellness visits; however, a few providers were trying to address it at all visits to avoid “missed opportunities.” Time constraint and the need to prioritize care, however, can limit how much is covered during an acute care visit. Family practice providers reported too many competing priorities, such as the requirement for depression screening, that even though they have the intention of recommending the vaccine, they lose track and forget to do it. Moreover, stakeholders reported having to have the “sex talk” versus cancer prevention talk with parents of adolescents regarding the vaccine, which can be difficult and take extra time. Even within the same practice, not all health care providers made the same recommendation, and some did not make the recommendation at all. Other stakeholders reported that there were providers who would not “push” the vaccine for fear of losing the patient from the practice. They also reported that there are providers who “don’t believe” in the vaccine. Furthermore, inconsistent messaging from support staff in the practice can downplay a licensed provider’s strong recommendation.
On the whole, stakeholders reported that providers are making more of an effort to make the recommendation for vaccination, and they have used educational programs from the community, the CDC, and their professional organizations to help them learn “how to” talk effectively with parents and adolescents about the vaccine. Providers who treat the HPV vaccine like other vaccines are more likely to help with vaccination consent. Providers who have support staff to help with education and reminders are also more effective with making the strong recommendation.
Organizational Level
Cost, lack of infrastructure/champion, and resistant to outside resources are barriers at the organizational level. The cost of having a program in place for vaccination, to provide storage and administration of the vaccine may prove to be too much for some organizations that provide free or reduced health care services. Organizations that are not familiar with health insurance plans and assistance programs, such as Vaccine for Children, limit what they can offer to their patients. Stakeholders cited inconsistent practices between clinics and within clinics, lack of training, and not holding physicians/providers accountable for “substandard” care as additional barriers. Other major hindrances include having a medical record system that does not provide alerts, inability to pull vaccination reports for measuring progress, reaching out to patients who are due for vaccination, and helping with reminders. Finally, organizations that are resistance to resources from industry and the community are likely to have less or no insight regarding available resources and how to incorporate best practices to improve HPV vaccination efforts.
Organizations that do well with HPV vaccination have a streamlined, team approach with a robust information system. These clinics all have similar processes and strategies such as treating vaccination as routine with established standing orders or pre-orders; and follow-up appointments and/or reminder systems. From check-ins to checkouts, clear, consistent messaging on vaccination is addressed at all visits. Having an information system that allows stakeholders to pull reports, track progress, and reach out to the patients with alerts and reminder-recalls are cited as key facilitators.
Community Level
Bad data, lack of an HPV vaccination champion, and limited health care financing capacity/resources were found to be barriers at the community level. Stakeholders shared various community efforts to improve cancer care and prevention; however, no one is leading the charge to promote adolescent vaccination. Efforts to reach specific groups or regions are limited because there is not robust data sources to show which areas are doing well and which areas are not doing as well. The Virginia Immunization Information System (VIIS), a web-based system, is one effort the state health department hopes to use to track all immunizations given within the state; however, use is considered voluntary and data are not able to be analyzed on the county-level. While the system can pull reports and has reminder-recalls feature, individual clinics and users are not taking advantage of this feature because it’s yet another system that they have to learn and use. Furthermore, VIIS is not set-up for clinics within larger medical center to extract a report at their clinic specific level. Even within these organizations’ electronic health record (EHR), many stakeholders said that they have a hard time getting immunization reports.
In rural communities, many stakeholders cited lack of transportation, poverty, geographical isolation, and limited health resources as barriers. Many individuals are unemployed or underinsured and cannot afford health care. Health clinics are sparse, and transportation is limited thus getting to appointments can be problematic especially since HPV vaccination requires three visits (three vaccines were required at the time this study was conducted prior to the recommendation change). While cancer support outreach is available, there is limited outreach to promote HPV vaccination.
Stakeholders described a few facilitators at the community level: educational outreach, presence of a champion, and engaged community. Firstly, community programs, such as the Cancer Action Coalition of Virginia and the Women’s Health Virginia, provided educational outreach and resources to providers/nurses and some patients regarding HPV vaccination. Individuals who are leading these program are champions; however, their reach is limited, and there is no data available to track improvement in HPV vaccination rate. Secondly, the Virginia Department of Health is working to improve resources to stakeholders at all levels by making VIIS more robust and hiring a new Adolescent Immunization Coordinator. The individual in this position will collaborate with the Cancer Coalitions and other partnerships to develop a state strategic plan to improve adolescent immunizations. Finally, stakeholders are proud of the community they serve and cited various strengths and resources that may be helpful. Some stakeholders, for example, talked about engaging with school nurses to help with the vaccine registry and education.
Policy Level
Barriers at the policy level include an ineffective mandate, a failed Medicaid expansion, and the current political climate. First, the current mandate has a generous opt-out policy so many parents and providers treat the HPV vaccines as different and optional. There is no documentation needed for parents who declined the vaccine for their child. A few stakeholders were not even aware of the mandate. Furthermore, the current mandate only covers girls, thus many people are unaware of the benefits to boys. And because of the bad publicity from the mandate, many stakeholders still feel the backlash from it. Second, the failed Medicaid Expansion still leaves some individuals vulnerable to the cost of co-pays and general access to the health care system. Finally, the current political climate of a failed mandate, conservatism, and anti-government rhetoric may make it harder for any changes to occur legislatively.
Nevertheless, important facilitators exist on the policy level, including the, endorsement of HPV vaccination by many professional organizations and the Affordable Care Act (ACA). Since the ACA focuses on prevention, coverage for vaccines is expected to improve although uptake may be slow. The CDC’s “You are the Key” campaign and toolkit provided incredibly strong messaging and tools for the providers to give the strong recommendation. Professional organizations, such as the American Academy of Pediatrics (AAP), for example, have also provided resources and strategies for members to improve HPV vaccination effort.
Discussion
To our knowledge, this study is the first to explore the barriers and facilitators from stakeholders from various levels and positions involved with HPV vaccination and cancer prevention in Virginia. Virginia is a unique environment because it was the first state to endorse a school-based mandate for adolescent girls. This study endorses the CDC’s findings (Stokley, Jeyarajah, Yankey, Cano, Gee, Roark, & Markowitz, 2014) that knowledge gap and sexuality concerns at the parent-child dyad level and lack of provider’s recommendation at the interpersonal level are barriers to HPV vaccination. Most providers in this study stated that they are making the recommendations to vaccinate; however, they are constrained by time and have a hard time getting adolescents to the appointments. Any programs to help bridge the knowledge gap at the parent-child dyad and to help providers communicate the strong recommendation can facilitate HPV vaccination efforts. More thorough research is needed to explore the adolescent/parents’ perspective for this region, the reasons for provider’s hesitancy, and what implementation and communication strategy is effective for improving vaccination uptake.
Fear is a barrier that stands out in this study and is a component of vaccine hesitancy. According to the Strategic Advisory Group of Experts (SAGE) on Immunization of the World Health Organization [30, p.7], vaccine hesitancy is the “delay in acceptance or refusal of vaccines despite availability of the vaccination services.” Fear can promote learning, but it can impede readiness to learn. Depending on the types of fear and the level of fear, it can lead to inactions and/or trust issues. Fear of needles from the adolescent and fear of sexual promiscuity from the parent, for example, are mentioned as barriers for the initiation and completion of the HPV vaccine. On the other hand, fear of cancer facilitates vaccination, and many stakeholders recommend this approach. Stakeholders also noted that parents were afraid of the vaccine from what they are learning on social media, especially from anti-vaccine groups. Instilling fear and distrust of the vaccine is a strategy of anti-vaccine groups (Kata, 2012).
More research is needed on the relationships between social media influence, the antivaccine movement, and vaccine hesitancy and how to counter these barriers where the primary goal is to establish trust (Leask, 2015). To this end, Henrikson et al (2015) conducted a randomized, interventional study to train doctors and other health care providers to better address parents’ concerns regarding vaccination. They found no improvement in vaccination uptake and that parents who were hesitant to vaccinate their children had very strong feelings or distrust of vaccines in general(Henrikson, Opel, Grothaus, Nelson, Scrol, Dunn, Grossman, 2015). This supports the notion that there are core values that brief information doesn’t change and more research on strategies to overcome trust issues is needed. The Strategic Advisory Group of Experts (SAGE) Working Group on Vaccine Hesitancy , for example, suggests that use of commercial and social marketing practices and principles may foster vaccine acceptance (Nowak, Gellin, MacDonald, Butler, 2015). Furthermore, recent systematic review recommends multicomponent and dialogue-based interventions because they are most effective (Jarrett, Wilson, O’Leary, Eckersberger, Larson, 2015). However, they stress the importance of tailoring the strategies to the target population, i.e., their reasons for hesitancy and the specific community/cultural context.
While cost was cited as a prominent barrier in the literature at the parent-child dyad level and interpersonal level, Virginian stakeholders identify cost as less of a barrier. This study explains that sometimes when cost is noted to be a barrier, the true issue may in fact, be a knowledge gap on the part of the parents, health care providers, or administrators regarding the various insurance programs, the impact of the Affordable Care Act, and vaccine assistance programs. In rural communities, at the level of the parent-child dyad, stakeholders indicate it is the indirect costs associated with getting the vaccine that may make it prohibitive. For example, the young adult or parents of adolescents may not be able to afford to take the time off from work, or they may not have the transportation means to get to the appointment. Cost is cited as an issue at the organizational level because it takes manpower, systems, and processes to provide vaccination services especially if these processes never before existed.
An important emphasis of this study is that the interactions of the various barriers and facilitators impact other SEM levels. Stakeholders talk about the lack of leadership and information system support at the organizational and community level as important barriers to the vaccination process at the interpersonal/provider level. Moreover, many stakeholders see the HPV vaccination mandate as ineffective; because of the failed mandate and the generous opt-out, the vaccine is treated differently than other vaccines and many parents see the vaccine as optional. Some of the stakeholders are not even aware of the mandate. Of the eight factors identified by Colgrove, Abiola, and Mello (2010) as barriers to HPV mandate, stakeholders agree that the newness of the vaccine, the sexually transmitted nature of HPV, and early legislative mandate of the vaccine contribute to parental distrust of the vaccine (Colgrove, Abiola, & Mello, 2010). Other factors identified by stakeholders include resistance to governmental coercion, the influence of anti-vaccination activism, and social and religious conservatism as great challenges to the political environment.
Stakeholders identify a need for a communication campaign at the larger organizational or community level to help counter the negative media and improve knowledge regarding the vaccines. Stakeholders also want timesaving strategies, such as team approach and effective immunization system or electronic health record (EHR) that will allow them to work more efficiently and to track progress with HPV initiatives. In short, multi-level approaches are needed to improve HPV vaccination efforts within the state.
Strengths and Limitations
This study gathers information that is unique to Virginia regarding the barriers and facilitators to HPV vaccination. It provides information that can inform future efforts to develop and expand applied research and programs to increase HPV vaccination uptake. These results are specific to the geographic area surveyed, and while not necessarily generalizable may be helpful to other regions intending to reduce barriers to HPV vaccination.
While a concerted effort has been made to select a representative sample of stakeholders to provide information, the possibility exists that important stakeholders were omitted or failed to participate in these interviews.
Implications for Pediatric Nurses
Understanding these factors can help stakeholders plan and implement an effective HPV vaccination strategy in Virginia. Based on this study, the three most important things that the Commonwealth should consider are: to jointly work with cancer prevention and immunization stakeholders to incorporate HPV vaccination in the state cancer plan and initiatives to include policy change; to provide a comprehensive communication campaign, and to support health care providers with a robust immunization information system; and provide strategies to educate key clinical and administrative staff about the importance of timely HPV vaccination. Pediatric nurses must cultivate and implement state-specific action plans to accelerate collaboration within the state to increase access and uptake of HPV vaccination.
Conclusion
In summary, the stakeholders identified unique barriers and echoed the latest CDC’s recommendation for multifaceted approaches to improve HPV vaccination efforts (Reagan-Steiner et al., 2015). These efforts include (a) incorporating HPV vaccination in cancer control plans; (b) joint initiatives with cancer prevention and immunization stakeholders; (c) public communication campaigns; (d) immunization information system-based reminder/recall; (e) assessment and feedback activities (including clinician-to-clinician education sessions emphasizing providing strong recommendations at ages 11–12 years); practice-focused strategies to educate staff and provide input on how to improve routine HPV vaccination within the practice; and (f) using all opportunities to educate clinicians and parents about the importance of on-time HPV vaccination. Additionally, stakeholders from this study identified the need for policy change. Stakeholders shared some of the initiatives underway in their clinics, in their organizations, and within the communities; however, these efforts are not strategic and coordinated. The Virginia Department of Health recognizes this and has hired a new Adolescent Immunization Coordinator. With this new position, improvement in VIIS functionality, and support from key stakeholders, the Virginia Department of Health is poised to help lead the change.
Highlights.
Chief barriers to HPV vaccination are knowledge gaps, fear, and sexuality concerns at the parent- child dyad level; time constraint and inconsistent recommendation at the interpersonal level, lack of leadership and informational support at the organizational and community level, and ineffective mandate at the policy level.
Pediatric nurses are critical in implementing effective state-based HPV vaccination strategies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- AAFP, AAP, ACOG, ACP, CDC, I. (2014). Give a strong recommendation for HPV vaccine to increase uptake. Retrieved from http://www2.aap.org/immunization/illnesses/hpv/HPV_letter_color_12114.pdf
- Association of Women’s Health, O. & N. N. (2010). HPV vaccination for the prevention of cervical cancer. JOGNN - Journal of Obstetric, Gynecologic, & Neonatal Nursing, 39(1), 129–130. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1111/j.1552-6909.2009.01097.x [DOI] [PubMed] [Google Scholar]
- Bartlett JA, & Peterson JA (2011). The uptake of human papillomavirus (HPV) vaccine among adolescent females in the United States: A review of the literature. Journal of School Nursing, 27(6), 434–446. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1177/1059840511415861 [DOI] [PubMed] [Google Scholar]
- CDC. (2010). FDA licensure of bivalent human papillomavirus (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report, 59(20), 626–629. [PubMed] [Google Scholar]
- CDC. (2012). Human papillomavirus-associated cancers-United States, 2004–2008. Morbidity and Mortality Weekly Report, 61(15), 258–261. [PubMed] [Google Scholar]
- CDC. (2015). You are the key to cancer prevention: Webinar #2: CDC’s clinician engagement initiative. Retrieved from https://www.youtube.com/watch?v=C1vEnHXQWbg
- Center for Disease Control and Prevention (CDC). (2014). CDC Telebriefing on national immunization survey—Teen results and HPV vaccination coverage among adolescents [Press Release]. Retrieved from http://www.cdc.gov/media/releases/2014/t0724-hpv-vaccination.html
- Centers for Disease Control and Prevention (CDC). (2007). Quadrivalent human papillomavirus vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report, 56(RR-2). [PubMed] [Google Scholar]
- Colgrove J, Abiola S, & Mello MM (2010). HPV vaccination mandates--lawmaking amid political and scientific controversy. New England Journal of Medicine, 363(8), 785–791. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1056/NEJMsr1003547 [DOI] [PubMed] [Google Scholar]
- Crosby RA, Casey BR, Vanderpool R, Collins T, & Moore GR (2011). Uptake of free HPV vaccination among young women: A comparison of rural versus urban rates. Journal of Rural Health, 27(4), 380–384. 10.1111/j.1748-0361.2010.00354.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer HB, Trotter C, Hickman M, & Audrey S (2014). Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health, 14(1), 700 10.1186/1471-2458-14-700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcini LM, Galvan T, & Barnack-Tavlaris JL (2012). The study of human papillomavirus (HPV) vaccine uptake from a parental perspective: A systematic review of observational studies in the united states. Vaccine, 30(31), 4588–4595. 10.1016/j.vaccine.2012.04.096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A, Miller E, Schwarz EB, Akers AY, Jeong K, & Borrero S (2013). Racial disparities in human papillomavirus vaccination: Does access matter? Journal of Adolescent Health, 53(6), 756–762. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1016/j.jadohealth.2013.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head KJ, Vanderpool RC, & Mills LA (2013). Health care providers’ perspectives on low HPV vaccine uptake and adherence in Kentucky. Public Health Nursing, 30(4), 351–360. 10.1111/phn.12044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrikson NB, Opel DJ, Grothaus L, Nelson J, Scrol A, Dunn J, . . . Grossman DC (2015). Physician communication training and parental vaccine hesitancy: A randomized trial. Pediatrics, 136(1), 70–79. [DOI] [PubMed] [Google Scholar]
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, & Stokley S (2014). Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatrics, 168(1), 76–82. 10.1001/jamapediatrics.2013.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HRSA. (2018). Defining rural population. Retrieved March 22, 2018, from https://www.hrsa.gov/rural-health/about-us/definition/index.html
- Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, & S. W. G. on V. H. (2015). Strategies for addressing vaccine hesitancy - A systematic review. Vaccine, 33(34), 4180–4190. [DOI] [PubMed] [Google Scholar]
- Jeudin P, Liveright E, Del Carmen MG, & Perkins RB (2014). Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clinical Therapeutics, 36(1), 24–37. 10.1016/j.clinthera.2013.11.001 [DOI] [PubMed] [Google Scholar]
- Kata A (2012). Anti-vaccine activists, Web 2.0, and the postmodern paradigm - An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine, 30(25), 3778–3789. 10.1016/j.vaccine.2011.11.112 [DOI] [PubMed] [Google Scholar]
- Keim-Malpass J, Mitchell EM, DeGuzman PB, Stoler MH, & Kennedy C (2017). Legislative activity related to the human papillomavirus (HPV) vaccine in the United States (2006–2015): a need for evidence-based policy. Risk Management and Healthcare Policy, Volume 10, 29–32. 10.2147/RMHP.S128247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, & T. R. L. (2012). Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine, 30(24), 3546–3556. Retrieved from http://dx.doi.org.proxy.its.virginia.edu/10.1016/j.vaccine.2012.03.063 [DOI] [PubMed] [Google Scholar]
- Leask J (2015). Should we do battle with antivaccination activists? Public Health Research & Practice, 25(2), e252151 https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.17061/phrp2521515 [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2016). NCI-Designated Cancer Centers Urge HPV Vaccination for the Prevention of Cancer. Retrieved July 31, 2016, from https://www.mdanderson.org/content/dam/mdanderson/documents/prevention-and-screening/NCI_HPV_Consensus_Statement_012716.pdf
- Nowak GJ, Gellin BG, MacDonald NE, Butler R, & S. W. G. on V. H. (2015). Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine, 33(34), 4202–4211. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1016/j.vaccine.2015.04.039 [DOI] [PubMed] [Google Scholar]
- Petrosky E, Bocchini JA, Hariri S, Chesson H, Curtis CR, Saraiya, … Markowitz LE (2015). Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR - Morbidity & Mortality Weekly Report, 64(11), 300–304. Retrieved from http://ovidsp.ovid.com.proxy.its.virginia.edu/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=prem&AN=25811679 [PMC free article] [PubMed] [Google Scholar]
- Pitts MJ, & Adams Tufts K (2013). Implications of the Virginia human papillomavirus vaccine mandate for parental vaccine acceptance. Qualitative Health Research, 23(5), 605–17. 10.1177/1049732312470871 [DOI] [PubMed] [Google Scholar]
- Rahman M, Laz TH, & B. A. B. (2013). Geographic variation in human papillomavirus vaccination uptake among young adult women in the United States during 2008–2010. Vaccine, 31(47), 5495–5499. https://doi.org/http://dx.doi.org.proxy.its.virginia.edu/10.1016/j.vaccine.2013.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rambout L, Tashkandi M, Hopkins L, & Tricco AC (2014). Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: A systematic review. Preventative Medicine, (58), 22–32. 10.1016/j.ypmed.2013.10.009 [DOI] [PubMed] [Google Scholar]
- Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans L, Singleton J, Curtis C, … Stokley S (2015). National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2014. MMWR. Morbidity and Mortality Weekly Report, 64(29), 784–792. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/26225479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, & Weinstock H (2013). Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sexually Transmitted Diseases, 40(3), 187–193. 10.1097/OLQ.0b013e318286bb53 [DOI] [PubMed] [Google Scholar]
- Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J,G, Roark J, & Markowitz L (2014). Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014 -United States. Morbidity and Mortality Weekly Report, 63(29), 620–624. [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. (2011). Immunizations and Infectious Diseases; Sexually transmitted diseases. Retrieved June 7, 2017, from https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
- Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, … Stokley S (2017). National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2016. MMWR. Morbidity and Mortality Weekly Report, 66(33), 874–882. https://doi.org/10.15585/mmwr.mm6633a2 [DOI] [PMC free article] [PubMed] [Google Scholar]


