Abstract
Introduction
Transjugular liver biopsy (TJLB) is a minimally invasive procedure performed to obtain hepatic tissue in patients whom standard percutaneous liver biopsy is contraindicated due to abnormal coagulation profile and/or severe ascites. Additionally, it has the advantage of simultaneously measuring the hepatic venous pressures.
Case Presentation
61-year-old male with history of pulmonary fibrosis, cholecystectomy and Hepatitis C underwent transjugular liver biopsy (TJLB) as part of his lung transplant workup. Shortly after the procedure, the patient developed sharp right upper abdominal pain. Immediate CT of the abdomen and pelvis showed small foci of contrast and gas in the gallbladder fossa and porta hepatis indicating hepatic capsular penetration without perihepatic hematoma or other evidence of hemorrhage. Follow up CT of the abdomen and HIDA scan confirmed the presence of bile leak. Sphincterotomy and stent placement through ERCP was performed.
Conclusion
Bile leak after a TJLB is a rare, however, potential complication. ERCP and biliary stent seems an effective treatment for persistent symptomatic bile leak post TJLB.
Keywords: Liver, Biopsy, Transjugular, Bile leak
Introduction
Transjugular liver biopsy (TJLB) is a minimally invasive procedure performed to obtain hepatic tissue in patients whom standard percutaneous liver biopsy is contraindicated due to abnormal coagulation profile and/or severe ascites. Additionally, it has the advantage of simultaneously measuring the hepatic venous pressures.
Case presentation
A 61-year-old male with a history of pulmonary fibrosis, cholecystectomy, and Hepatitis C underwent TJLB as part of his lung transplant workup. The patient's coagulation profile before the procedure was; platelets: 158 K/mcL (normal 153-367 K/mcL), INR: 1.1 (normal 0.8-1.2), and PTT 27 seconds (normal value 24-33 seconds). Using the right internal jugular vein access and through the middle hepatic vein cannulation, the biopsy was performed by using Cook Quick-Core device (Fig. 1). Shortly after the procedure, the patient developed sharp right upper abdominal pain. Unenhanced computed tomography (CT) of the abdomen and pelvis obtained 2 hours after the biopsy due to persistent abdominal pain showed small foci of contrast and gas in the gallbladder fossa and porta hepatis indicating hepatic capsular penetration without perihepatic hematoma or other evidence of hemorrhage (Fig. 2). Patient's pain was controlled with oral pain medication and the patient was discharged later the same day. The patient was admitted overnight to an outside hospital with recurrent right upper abdominal pain and nausea and was transferred to our institution 3 days after the biopsy. The repeat CBC showed stable Hgb but liver function test showed increased total bilirubin level to 2.5 mg/dL compared to his normal level (1.0 mg/dL) 2 months before. Repeat CT abdomen and pelvis with intravenous and oral contrast showed increased fluid in the perihepatic region, around the duodenum, the transverse mesocolon, and in the pelvis, concerning for bile leak (Fig. 3). Subsequent, hepatobiliary scintigraphy confirmed the diagnosis of bile leak (Fig. 4). Total bilirubin levels rose to 6.3 mg/dL on day 4 after the biopsy. At this point, an endoscopic retrograde cholangio-pancreatography (ERCP) was performed and showed contrast extravasation from a right intrahepatic duct peripheral branch (Fig. 5). Sphincterotomy was made and a 10 Fr by 7 cm plastic stent with a single external pigtail was placed into the common bile duct (Fig 6A and B). At follow-up, total bilirubin level after 48 hours was 2.0 mg/dL and the patient was discharged home. Biopsy results showed chronic hepatitis C with mild activity and cirrhosis (grade 2, stage 4).
Fig. 1.
Select hepatic venogram image during transjugular liver biopsy through the right hepatic vein by using Cook Quick-Core device.
Fig. 2.
Unenhanced CT of the abdomen and pelvis 2 hours after the biopsy shows contrast (black asterisk) and foci of gas (white arrow) in the gallbladder fossa and porta hepatis indicating capsular penetration.
Fig. 3.
CT abdomen and pelvis with intravenous and oral contrast 3 days after the biopsy showed increased fluid in the perihepatic region (asterisk) concerning for bile leak.
Fig.– 4.
Hepatobiliary scintigraphy 3 days after the biopsy showed increased radiotracer uptake in the region of the gallbladder fossa, confirming the diagnosis of bile leak.
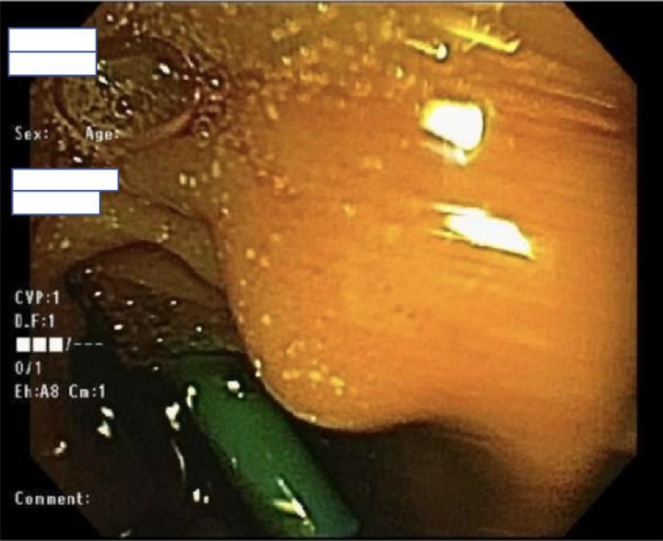
Fig. 5.
ERCP image 4 days after the biopsy shows contrast extravasation from a right intrahepatic duct peripheral branch (white arrow).
Fig. 6.
(A) A photograph during ERCP after performing sphincterotomy. (B) A photograph during ERCP after common bile duct stent placement.
The internal biliary stent removed after 4 weeks and patient was asymptomatic at 2 months follow-up.
Discussion
Several studies reviewed various major and minor complications following TJLB, namely intraperitoneal hematoma, pseudoaneurysm formation, ventricular arrhythmia, or high-grade fever [2,3,4,5]; however, data regarding bile leak after TJLB and its management is scarce [1]. One advantage of TJLB over percutaneous liver biopsy is to avoid capsular perforation which can lead to intraperitoneal hemorrhage particularly in coagulopathic patients which leads to increased morbidity or mortality. The correlation between number of passes and rate of complication is still debated [7], [8]. Delayed symptoms are consistent with prior reports and could be masked temporarily by the effects of analgesic medications [3], [6], [7].
Persistent bile leak following transjugular liver biopsy is an unusual complication rarely described in the literature [1].
In this patient, the middle hepatic vein was selected, which anatomically is a less favorable access for obtaining hepatic needle biopsy compared to right hepatic vein. The right hepatic vein is most favorable venous access for TJLBx due to its deep anatomic location within the right hepatic lobe parenchyma away from the liver capsule, which improves the chance of obtaining better tissue core samples while decreasing risk of liver capsular penetration by the biopsy needle. Additionally, empty gallbladder fossa in the setting of cholecystectomy, although not been described before, appears to add an extra risk for persistent symptomatic intraperitoneal bile leak should the capsular penetration occur during the biopsy.
When bile leak occurs, pressure gradient between the bile duct and duodenum develops. Endoscopic procedures have been performed to treat bile leaks, sphincterotomy alone, biliary stenting with or without sphincterotomy, and nasobiliary drainage with or without sphincterotomy.
The treatment goal is to abolish the pressure gradient to allow bile to flow to the duodenum instead through the leak. Eventually, the defect in the bile duct will heal with absence of flow through it.
Conclusion
Bile leak is a rare potential complication after TJLB. ERCP and biliary stent seem an effective treatment for persistent symptomatic bile leak post TJLB.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2018.07.026.
Contributor Information
Omar Alharthi, Email: omar.alharthi@umm.edu, dralharthi.o@gmail.com.
Vahid Etezadi, Email: ete100@gmail.com.
Appendix. Supplementary materials
References
- 1.Fricker Z, Levy E, Kleiner D, Taylor JG, 6th, Koh C, Holland SM. Case series: biliary leak after transjugular liver biopsy. Am J Gastroenterol. 2013;108:145–147. doi: 10.1038/ajg.2012.352. [DOI] [PubMed] [Google Scholar]
- 2.Mammen T1, Keshava SN, Eapen CE, Raghuram L, Moses V, Gopi K. Transjugular liver biopsy: a retrospective analysis of 601 cases. J Vasc Interv Radiol. 2008;19(3):351–358. doi: 10.1016/j.jvir.2007.09.002. Mar. [DOI] [PubMed] [Google Scholar]
- 3.Dohan A, Guerrache Y, Dautry R, Boudiaf M, Ledref O, Sirol M. Major complications due to transjugular liver biopsy: Incidence, management and outcome. Diagn Interv Imaging. 2015;96(6):571–577. doi: 10.1016/j.diii.2015.02.006. Jun. [DOI] [PubMed] [Google Scholar]
- 4.Gamble P, Colapinto RD, Stronell RD, Colman JC, Blendis L. Transjugular liver biopsy: a review of 461 biopsies. Radiology. 1985;157:589–593. doi: 10.1148/radiology.157.3.4059543. [DOI] [PubMed] [Google Scholar]
- 5.Shin JL, Teitel J, Swain MG, Bain VG, Adams PC, Croitoru K. A Canadian multicenter retrospective study evaluating transjugular liver biopsy in patients with congenital bleeding disorders and hepatitis C: is it safe and useful. Am J Hematol. 2005;78:85–93. doi: 10.1002/ajh.20263. [DOI] [PubMed] [Google Scholar]
- 6.Dillon BJ, Alomari AI. Delayed formation and rupture of a pseudoaneurysm after transjugular liver biopsy in a pediatric bone marrow transplant patient: imaging and endovascular treatment. Cardiovasc Intervent Radiol. 2009;32(2):377–380. doi: 10.1007/s00270-008-9444-z. [DOI] [PubMed] [Google Scholar]
- 7.Lebrec D, Goldfarb G, Degott C, Rueff B, Benhamou JP. Transvenous liver biopsy: an experience based on 1000 hepatic tissue samplings with this procedure. Gastroenterology. 1982;83(2):338–340. Aug. [PubMed] [Google Scholar]
- 8.Cholongitas E, Burroughs AK. Liver: transjugular liver biopsy yields high-quality samples. Nat Rev Gastroenterol Hepatol. 2012;9(9):491–492. doi: 10.1038/nrgastro.2012.146. Sep. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.