Abstract
Hemodiafiltration combines diffusive and convective solute removal in a single therapy by ultrafiltering 20% or more of the blood volume processed using a high-flux hemodialyzer and maintaining fluid balance by infusing sterile nonpyrogenic replacement fluid directly into the patient’s blood. In online hemodiafiltration, the large volumes of replacement fluid required are obtained by online filtration of standard dialysate through a series of bacteria- and endotoxin-retaining filters. Currently available systems for online hemodiafiltration are on the basis of conventional dialysis machines with added features to safely prepare and infuse replacement fluid and closely control fluid balance. Hemodiafiltration provides greater removal of higher molecular weight uremic retention solutes than conventional high-flux hemodialysis, and recently completed randomized, controlled clinical trials suggest better patient survival with online hemodiafiltration compared with standard high-flux hemodialysis when a high convection volume is delivered. Hemodiafiltration is also associated with improvements in other clinical outcomes, such as a reduction in intradialytic hypotension, and it is now used routinely to treat >100,000 patients, mainly in Europe and Japan.
Keywords: Hemodiafiltration; Clinical outcomes; Technical requirements; Therapy prescription; Bacteria; Blood Volume; Convection; Dialysis Solutions; Endotoxins; Europe; Filtration; Humans; hypotension; Japan; Kidney Failure, Chronic; Kidneys, Artificial; Molecular Weight; renal dialysis; ultrafiltration; water-electrolyte balance
Introduction
The Kidney Health Initiative (KHI) is a public-private partnership between the American Society of Nephrology, the US Food and Drug Administration, and over 75 other organizations that was formed to promote introduction of new therapies for treating kidney-related problems in the United States (1). As part of that effort, the KHI established a workgroup to examine pathways for the approval of therapies already marketed in Europe and Canada. One such therapy is hemodiafiltration (HDF). This review examines the technical requirements for performing HDF, the prescription of HDF, and the clinical evidence that HDF might provide benefits beyond those obtained with conventional hemodialysis (HD). Regulatory barriers to implementing HDF in the United States are covered elsewhere (2).
HDF was conceived in the 1980s to address the limited middle molecule clearances associated with low-flux HD and the limited small molecule clearance provided by hemofiltration. Solute removal in HD occurs by diffusion, and because diffusion coefficients decrease rapidly with increasing molecular size (3), removal of larger uremic toxins is modest in HD. In contrast, because solute removal in hemofiltration occurs by convection, small solute removal in hemofiltration is modest, because it cannot exceed the ultrafiltration rate. Hemofiltration provides higher clearances of larger solutes than HD, however, because sieving coefficients, which together with ultrafiltration, determine convective clearance, decrease only gradually with increasing molecular size (4). By combining diffusion and convection in the same high-flux hemodialyzer, HDF provides both the high diffusive clearance of small molecules obtained in HD and the superior removal of larger molecules obtained with hemofiltration.
Online HDF uses a high-flux hemodialyzer with a membrane having an ultrafiltration coefficient >20 ml/h per 1 mm Hg per 1 m2 and a sieving coefficient for β2-microglobulin of >0.6 to deliver a convection volume of at least 20% of the total blood volume processed, and it maintains fluid balance by infusing a sterile, nonpyrogenic fluid into the patient’s blood (5).
HDF has been postulated to improve removal of middle molecular weight uremic toxins (6,7), reduce intradialytic hypotension (8), and reduce dialysis-related pathology, such as amyloidosis and accelerated atherosclerosis (9–11). HDF was used to routinely treat 70,000 patients in Europe in 2011 (12) and >30,000 patients in Japan in 2013 (13).
Technical Requirements for HDF
HDF Machines
After initially using prepackaged bags of substitution fluid, it became clear that online preparation was the only practical means of implementing HDF as a routine therapy (14). Online preparation of substitution fluid is made possible by adding three components to conventional HD machines: (1) a pump for delivering substitution fluid, (2) a series of specifically qualified sterilizing ultrafilters to produce sterile substitution fluid from dialysate, and (3) a system for controlling fluid exchange to achieve the desired convection volume and net fluid removal.
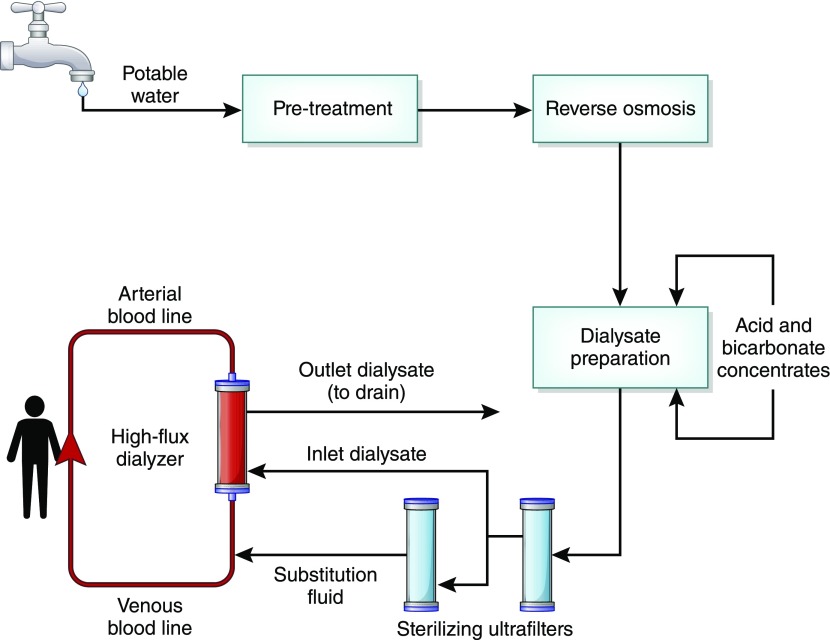
As in standard dialysis machines, HDF machines prepare dialysate from dialysis water and concentrates. That dialysate is then subjected to a process capable of producing sterile, nonpyrogenic substitution fluid for immediate infusion into the blood. Current HDF machines use a series of ultrafilters for this purpose (Figure 1). The sterilizing ultrafilters are incorporated in the dialysate pathway, disinfected with the machine, and replaced periodically according to the manufacturer’s instructions to ensure their ability to sterilize and remove endotoxin is sustained.
Figure 1.
Dialysate and substitution fluid are prepared using a purification cascade comprising reverse osmosis and two sterilizing ultrafilters. The high-flux dialyzer with polysulfone membranes acts as an additional endotoxin adsorber and provides additional microbial safety.
Performance of the sterilizing ultrafilters is validated by the machine manufacturer in accordance with applicable regulations to produce a solution free from micro-organisms for their stated operating lifetime, including all foreseen disinfection cycles. Typically, filters are qualified to provide a Sterility Assurance Level of 10−6 (that is, a six-log reduction in the number of incoming bacteria in a challenge test using selected bacterial strains and defined exposure times) (15). HDF systems should include a mechanism for ensuring ultrafilter integrity before each treatment, such as a pressure holding test or bubble test performed automatically as the machine is prepared for use. Alternatively, safety can be secured by including a single-use ultrafilter in the disposable substitution fluid infusion tubing.
HDF machines include an infusion pump that can infuse substitution fluid into the blood at different points in the extracorporeal circuit, including the venous line (postdilution), the arterial line (predilution), and the blood compartment of the dialyzer (mid-dilution). These machines can achieve fluid balance with a precision of ±100 ml irrespective of the convection volume. Achieving the desired convection volume can be facilitated by using automated ultrafiltration control systems (16,17), which ensure a maximal tolerable filtration fraction regardless of the blood flow and targeted convection volume (17,18).
The safety of online production of substitution fluid for HDF has been shown in large clinical studies (19).
Dialysis Fluid Preparation
Dialysate used for online HDF must consistently meet stringent quality standards, because that fluid is used to prepare a large amount of substitution fluid (20). Practices used for water treatment and dialysate preparation must be sufficient to ensure that fluids entering the HDF machine routinely meet the quality requirements for which the online HDF system has been validated (2,21).
Prescription of HDF
Treatment Prescription
The treatment schedule for HDF (treatments per week and treatment time) does not need to be different from that of standard HD. HDF is not intended as a means of shortening treatment time, but rather, it is a way to enhance solute removal within currently prescribed treatment times. The composition of the dialysate, including use of citrate-containing dialysate (22), does not need to be different between HDF and HD. However, HDF can differ from HD with respect to dialyzer, blood and dialysate flow rates, administration of anticoagulant if low molecular weight heparin is used (23), and convection and substitution fluid volumes. The main features of the HDF prescription are summarized in Table 1.
Table 1.
Summary of the treatment prescription for hemodiafiltration
| Parameter | Target Range |
|---|---|
| Hemodialyzer | |
| Membrane | High flux, 1.6–2.2 m2 |
| Fiber internal diameter | ≥200 μm |
| Ultrafiltration coefficient | >20 ml/h per 1 mm Hg per 1 m2 |
| Sieving coefficient | >0.6 for β2-Microglobulin; <0.001 for albumin |
| Vascular access | |
| AVF or AVG; tunneled central venous catheter | Needles, 14–15 g |
| Blood flow rate | 350–450 ml/min |
| Dialysate flow rate | |
| Total (including substitution solution) | 600–1000 ml/min |
| Dialyzer | 500–600 ml/min |
| Convection volume | |
| Postdilution | 23 L per treatment or 26 L/1.73 m2 |
| Predilution | 46 L per treatment or 52 L/1.73 m2 |
| Mid-dilution or mixed dilution | 35 L per treatment or 40 L/1.73 m2 |
| Ultrafiltration control | |
| Manual | TMP<400 mm Hg, filtration fraction <0.25 |
| Automated | TMP=105–300 mm Hg |
| Anticoagulation | |
| Unfractionated heparin | No dose adjustment |
| Low molecular weight heparin | Dose and injection site adjustment |
| Dialysate composition | Adjusted according to patient need and convection volume |
AVF, arteriovenous fistula; AVG, arteriovenous graft; TMP, transmembrane pressure.
Hemodialyzers
In addition to selecting a hemodialyzer with membrane permeability characteristics that allow the benefits of combining diffusion and convection to be realized, hemodialyzer geometry and hollow fiber internal diameter should also be considered. Hemodialyzers favoring internal filtration (ultrafiltration and backfiltration) due to high internal blood flow resistance (e.g., reduced internal diameter and increased fiber length) and reduced fiber wall thickness are preferred for HD (24), whereas hemodialyzers with low internal blood flow resistance (e.g., slightly larger fiber internal diameter) are preferred for HDF to maximize the filtration fraction (25).
Blood and Dialysate Flows
The effective blood flow rate and treatment time are critical to achieving the prescribed convection volume. Blood volume processed per session represents the limiting factor for overall solute clearances. The ultrafiltration rate is limited to 25%–30% of the blood flow rate. Higher filtration fractions lead to excessive hematocrits in the dialyzer, resulting in high pressures, membrane fouling, increased albumin loss, and risk of clotting. Shear rate and shear stress per hollow fiber are critical factors for limiting the secondary protein layer that forms during forced ultrafiltration and that compromises both hydraulic and solute permeability of the membrane. To maintain an adequate shear rate and best use the effective membrane area of the hemodialyzer, the blood flow should be >200 ml/min per 1 m2.
In online HDF machines, the dialysate is divided into two streams—one flows through the dialysate compartment and allows solute removal by diffusion as in HD, whereas the other is infused into the patient’s blood (post- or predilution) as substitution fluid necessary for the convection volume associated with HDF (Figure 1). Overall dialysate production can be increased to compensate for the substitution fluid to preserve small molecule removal.
Substitution Fluid Flow
Prescription of HDF includes specification of the substitution fluid flow rate and treatment time to achieve the targeted convection volume. HDF sessions may be performed in manual or automatic control mode. In manual mode, substitution fluid flow and weight loss are set by the user. Substitution fluid flow is then kept constant at the expense of a steadily increasing transmembrane pressure. If the transmembrane pressure becomes too high, the substitution fluid flow is reduced to keep transmembrane pressure within a safe range at the expense of a reduced convection volume. In automatic mode, ultrafiltration flow is maximized and kept on a plateau by the HDF machine acting in an ultrafiltration-controlled mode (16,17).
Substitution Mode
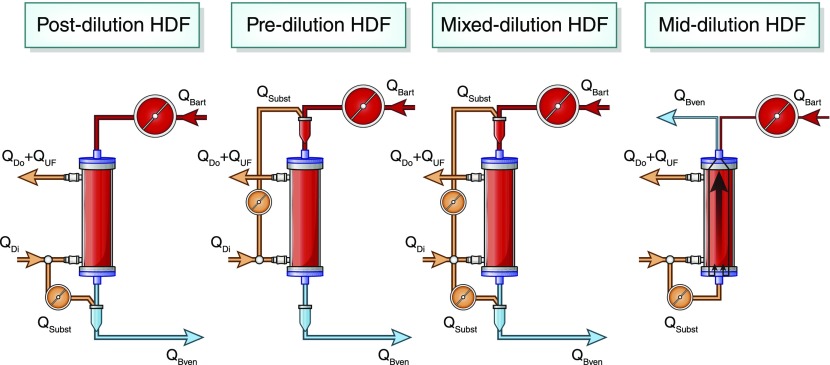
Fluid can be infused at different points in the blood circuit (Figure 2). Postdilution is the reference method. It provides the highest solute clearances for the lowest convection volume, and it is more cost effective. Predilution, mid-dilution, and mixed dilution can be used when the desired convection volume cannot be achieved in postdilution (26,27). Mid-dilution allows substitution fluid to be introduced directly into the dialyzer at the midpoint of the blood pathway, thus combining elements of both postdilution and predilution. Mixed dilution introduces substitution fluid both pre- and postdialyzer. The ratio of predilution to postdilution is adjusted automatically by the machine to maintain transmembrane pressure in the range of 150–300 mm Hg. These alternatives to postdilution are useful for increasing convective volume when facing a low extracorporeal blood flow or unfavorable hemorheologic conditions (high hematocrit, high protein concentration, or high viscosity).
Figure 2.
Different modalities of hemodiafiltration (HDF) are defined by the route of substitution fluid administration. QBart, arterial blood line to dialyzer; QBven, venous blood line to patient; QDi, inlet dialysate flow; QDo, outlet dialysate flow; QUF, ultrafiltrate flow; QSubst, substitution fluid flow.
All alternatives to postdilution involve dilution of solute concentrations in the blood reaching the hemodialyzer, leading to a reduction in solute clearances. To match the performance of postdilution HDF, that dilution should be compensated for by an additional convection volume, which translates to increasing the substitution fluid volume by a correction factor of two in predilution and close to 1.5 with mid-dilution and mixed dilution (5).
Convection Volume
The convection volume achieved per session is the sum of the substitution fluid volume and the net ultrafiltration volume required to correct the patient’s interdialytic weight gain, and it should be >20% of the total blood volume processed.
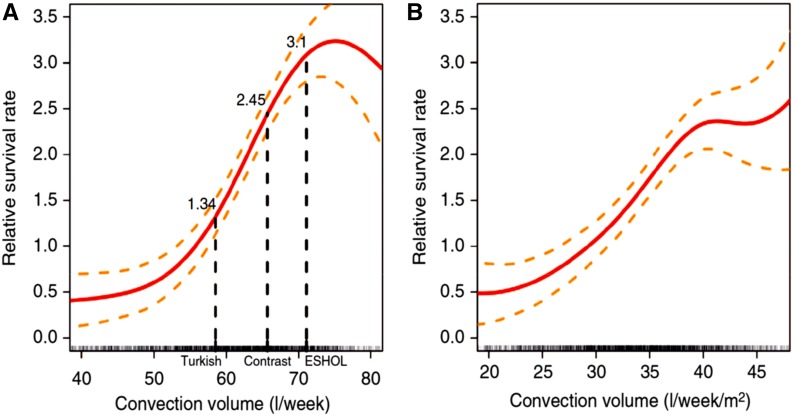
The optimal convection volume for improving patient outcomes needs further evaluation. Retrospective and prospective trials with postdilution HDF suggest that outcome depends on convection volume (28) (Figure 3), with analysis of pooled data from four randomized, controlled trials suggesting that only high-volume HDF (>66 L/wk) improves patient outcome (29). Moreover, convection volume might need to be scaled to patient anthropometric characteristics (30,31).
Figure 3.
The results of a series of clinical trials suggest that patient survival depends on using a high convection volume. (A) Relative survival as a function of convection volume (l/week). (B) Relative survival as a function of convection volume normalized to body surface area (l/week per 1 m2). Reprinted from ref. 31, with permission.
Potential Benefits of HDF
Patient Outcomes
Several retrospective cohort studies suggested that HDF had beneficial effects on patient survival (Supplemental Table 1). For example, the Dialysis Outcomes and Practice Patterns Study (DOPPS) suggested that patients treated with high-volume HDF (substitution fluid volume of 15–25 L per session) had a 35% lower mortality than those treated with low-flux HD. However, comparison of high-flux HD and low-volume HDF (<15 L per session) did not yield statistically significant results (32), and a more recent analysis of the DOPPS data failed to show that HDF was associated with a reduction in mortality (33).
Early results stimulated four European randomized, controlled trials, which are summarized in Tables 2 and 3. The primary analysis of two studies (the Convective Transport (CONTRAST) Study and the Turkish study) failed to show beneficial effects on all-cause or cardiovascular mortality, although post hoc analyses of both studies showed beneficial effects in patients with high convection volumes (>22 L per session) (34,35). The fact that 50%–66% of patients enrolled in the CONTRAST Study did not achieve the targeted convection volume could be considered a weakness of that study (36). Subsequently, the CONTRAST Study investigators reported that, after implementation of a targeted policy and nurse training, >80% of patients could achieve the threshold convection volume of 22 L per treatment (37,38), suggesting that failure to achieve the target convection volume was not inherent to HDF but was related to its clinical implementation.
Table 2.
Randomized, controlled trials comparing patient mortality with hemodiafiltration and hemodialysis
| Study Parameter | CONTRAST Study (34) | Turkish Study (35) | ESHOL Study (39) | FRENCHIE Study (40) |
|---|---|---|---|---|
| Comparison | LF-HD (n=358) versus HDF (n=356 | HF-HD (n=391) versus HDF (n=391) | HF-HD (n=450) versus HDF (n=456) | HF-HD (n=191) versus HDF (n=190) |
| Mean follow-up, yr | 3.04 | 1.89 | 1.91 | 1.64 |
| Target convection volume | 24 L per 4-h session | >15 L per session + net UF | >18 L per session + net UF | |
| Delivered convection volume | 20.7 L per session | 17.2 L per session + net UF | 22.9–23.9 L per session | 21 L per session |
| Primary outcome | All-cause mortality | All-cause mortality + nonfatal cardiovascular events | All-cause mortality | Intradialytic tolerance |
| HR for primary outcome [95% CI], HD=1.00 | 0.95 [0.75 to 1.20] | 0.82 [0.59 to 1.16] | 0.70 [0.53 to 0.92] | 0.94 [0.51 to 1.76] |
| Secondary outcomes | Fatal + nonfatal cardiovascular events (HR, 1.07; 95% CI, 0.83 to 1.39) | Cardiovascular and overall mortality (HR, 0.72; 95% CI, 0.45 to 1.13) | Cardiovascular mortality (HR, 0.67; 95% CI, 0.44 to 1.02); infection-related mortality (HR, 0.45; 95% CI, 0.21 to 0.96) | All-cause mortality (HR, 0.83; 95% CI, 0.52 to 1.33) |
| Potential limitations | Failure to deliver target convection volume | Underpowered (lower than anticipated event rate) | Underpowered (recruitment target not met) |
CONTRAST, Convective Transport; ESHOL, Estudio de Supervivencia de Hemodiafiltración On-Line; FRENCHIE, French Convective versus Hemodialysis in Elderly; LF-HD, low-flux hemodialysis; HDF, hemodiafiltration; HF-HD, high-flux hemodialysis; UF, ultrafiltration; HR, hazard ratio; 95% CI, 95% confidence interval; HD, hemodialysis.
Table 3.
Hazard ratios relative to hemodialysis for mortality as a function of convection volume from post hoc analysis of data from randomized, controlled trials of hemodiafiltration
| Convection Volume, L per Session | Hazard Ratio Relative to Hemodialysis [95% Confidence Interval] |
|---|---|
| CONTRAST Study (34) | |
| <18 | 0.80 [0.52 to 1.24] |
| 18–22 | 0.84 [0.54 to 1.29] |
| >22 | 0.61 [0.38 to 0.98] |
| Turkish study (35) | |
| 18–20 | 1.10 [0.68 to 1.76] |
| >20.5 | 0.54 [0.33 to 0.88] |
| ESHOL Study (39) | |
| <23.1 | 0.90 [0.61 to 1.31] |
| 23.1–25.4 | 0.60 [0.39 to 0.90] |
| >25.4 | 0.55 [0.34 to 0.84] |
| FRENCHIE Study (40) | |
| 19–23 | 0.83 [0.43 to 1.60] |
| >23 | 0.86 [0.46 to 1.63] |
CONTRAST, Convective Transport; ESHOL, Estudio de Supervivencia de Hemodiafiltración On-Line; FRENCHIE, French Convective versus Hemodialysis in Elderly.
Primary analysis of the third study (the Estudio de Supervivencia de Hemodiafiltración On-Line (ESHOL) Study), which achieved a median convection volume of 22.9–23.9 L, showed that patients treated with HDF had a 30% lower risk of both all-cause and cardiovascular mortality than patients treated with high-flux HD. This study also found lower risk in patients on HDF of hypotensive episodes (28%), stroke (61%), and infection (55%) compared with in patients on HD (39).
The fourth study (the French Convective versus Hemodialysis in Elderly [FRENCHIE] Study) was performed in patients over 65 years old and focused on dialytic tolerance and patient-reported outcomes (40). The primary analysis showed that the proportion of patients experiencing at least one treatment-associated adverse event did not differ between HDF (84% of patients) and high-flux HD (85% of patients). Secondary analyses showed a significantly lower occurrence of intradialytic symptomatic hypotension and muscle cramps in the HDF-treated group, but no difference in health-related quality of life, morbidity, or mortality.
The magnitude of the convection volume that should be delivered remains a critical question. The CONTRAST Study was designed to deliver 24 L of convection volume for a 4-hour treatment, but it achieved a median volume of only 19.8 L (34). Post hoc analysis showed that survival was significantly higher in the tertile of patients treated with the highest convection volume: >21.95 L (34). In the Turkish study, a substitution fluid volume of at least 15 L was targeted, and a median substitution fluid volume of 17.2 L was achieved (35). Again, post hoc analysis indicated that convection volumes of >19.9 L (17.4 L substitution fluid volume +2.5 L net ultrafiltration) were associated with better survival (35). The results of the post hoc analyses from these two randomized, controlled trials were confirmed by post hoc analysis of the ESHOL Study, which showed that a convection volume exceeding 23.1 L per session was associated with better survival compared with that in patients treated with high-flux HD (39).
That a positive outcome might depend on convection volume is supported by results of secondary analyses of individual patient data pooled from the four European randomized, controlled trials (the CONTRAST Study, the Turkish study, the ESHOL Study, and the FRENCHIE Study) (29,30). The results of these analyses are presented in Table 4. In aggregate, after a median follow-up of 2.5 years, 769 of 2793 patients had died, with 292 of the deaths being cardiovascular. Patients on HDF were divided into tertiles on the basis of delivered convection volume and all-cause and cardiovascular mortality compared with those on HD using hazard ratios calculated using Cox proportional hazard regression models (29,30). In the first analysis, HDF was associated with a reduction in relative risk of mortality for patients in the highest tertile of convection volume, although results varied depending on how convection volume was standardized to body size (30). The relative risk of all-cause mortality in the tertile receiving the highest convection volumes was reduced when the convection volume was not standardized or was standardized to body surface area or total body water (hazard ratios of 0.66 [95% confidence interval, 0.52 to 0.83], 0.71 [95% confidence interval, 0.57 to 0.90], and 0.71 [95% confidence interval, 0.57 to 0.89], respectively); however, no reduction was found for standardization to body weight or body mass index. These results were confirmed in a second analysis, where online HDF was shown to reduce the relative risk of all-cause mortality by 14% and cardiovascular mortality by 23% compared with HD (29). There was no evidence for a differential effect in predetermined subgroups, and again, the greatest benefit was for patients receiving the highest delivered convection volume (>23 L or 26 L/1.73 m2 body surface area per treatment).
Table 4.
| Convection Volume, L/1.73 m2 per Session | Hazard Ratio [95% Confidence Interval] | |
|---|---|---|
| Hemodialysis, n=1369 | HDF, n=1367 | |
| All-cause mortality | ||
| All | 1.0 | 0.86 [0.75 to 0.99] |
| <19 | 1.0 | 0.83 [0.66 to 1.03] |
| 19–23 | 1.0 | 0.93 [0.75 to 1.16] |
| >23 | 1.0 | 0.78 [0.62 to 0.98] |
| Cardiovascular mortality | ||
| All | 1.0 | 0.77 [0.61 to 0.97] |
| <19 | 1.0 | 0.92 [0.65 to 1.30] |
| 19–23 | 1.0 | 0.71 [0.49 to 1.03] |
| >23 | 1.0 | 0.69 [0.47 to 1.00] |
HDF, hemodiafiltration.
Meta-analyses and/or systematic reviews comparing HDF with standard HD have reported conflicting results (41–43). Unfortunately, some of these meta-analyses aggregated several different convection-based methods under the umbrella of “convective therapies” (i.e., hemofiltration, acetate-free biofiltration, and low-volume HDF).
Enhanced Solute Removal and Other Clinical Benefits of HDF
HDF provides enhanced clearance of β2-microglobulin compared with HD (30%–40% higher with HDF than with high-flux HD) (6), and several large cohort studies indicate that the use of convective therapies has a beneficial effect on the development of β2-microglobulin amyloidosis, reducing the incidence of carpal tunnel syndrome and other related manifestations (9,10). This beneficial effect probably results from use of ultrapure fluids and biocompatible materials reducing inflammation combined with convective transport that enhances β2-microglobulin removal.
Whether HDF removes more phosphate than high-flux HD is unclear, with two studies on the basis of direct quantitation of dialysate phosphate yielding contradictory results. In one study, the mass of phosphate removed with postdilution HDF was 15%–20% greater than that with high-flux HD (44), whereas in the second study, no difference was found (45). Furthermore, in the CONTRAST Study, predialysis serum phosphate levels reduced by 6%, and the percentage of patients reaching target pretreatment serum phosphorus levels increased from 64% to 74% (46), whereas no difference was found in serum phosphate levels in the ESHOL Study and the Turkish study (35,39).
HDF provides higher clearances of other solutes, including complement factor D (a proinflammatory mediator), leptin (involved in loss of appetite), fibroblast growth factor 23 (implicated in metabolic bone disorders and vascular calcification), various cytokines, and circulating advanced glycation end products and advanced glycation end product precursors (6,47–49). Other prospective studies have shown HDF to be associated with lower levels of C-reactive protein and other sensitive biomarkers of inflammation (e.g., IL-6) and/or proinflammatory cells, such as CD14+ and CD16+ (50,51). The clinical relevance of these findings is currently unknown.
It remains unclear if HDF is of benefit in anemia management. Erythropoiesis-stimulating agent dose could be reduced in several clinical studies with HDF, the benefit being attributed to the combined effects of the higher removal of middle-sized uremic toxins (erythropoietic inhibitor substances) and use of higher-quality water and dialysate reducing inflammation (52,53). No effect on erythropoiesis-stimulating agent resistance was found in a preplanned secondary analysis of the CONTRAST Study data (54) and a recent meta-analysis combining various convective therapies (55), whereas a significant decrease was observed in a large observational study for incident patients treated with erythropoietin who received a high convective volume (56).
A significant reduction in episodes of intradialytic hypotension in HDF compared with conventional HD has been observed in some (39,40,57) but not all (35) studies, and it has been ascribed to negative thermal balance due to infusion of relatively cool substitution fluid, a slightly positive sodium mass balance due to generation of hyponatremic ultrafiltrate secondary to the Gibbs–Donnan effect, and/or removal of mediators of vasodilation (58).
A recent prospective study showed that, compared with high-flux HD, high-dose HDF was associated with preservation of muscle mass, increased protein intake, and reduced inflammation, suggesting that HDF could help prevent protein-energy wasting (59).
Conclusion
Online HDF can no longer be considered an experimental treatment but has matured to an RRT used daily to sustain life in >70,000 patients in Europe (12) and 30,000 patients in Japan (13). The technology for the realization of online HDF has proven to be safe and sustainable.
Online HDF offers efficient removal of uremic retention solutes over a wide spectrum of molecular weights. Several short- and medium-term clinical studies have proven both its safety and efficacy. Recent randomized, controlled trials support the superiority of online HDF compared with standard HD when a high convection volume is delivered.
Further clinical trials should examine both the superiority of HDF compared with high-flux HD and the optimal convective dose in different clinical settings.
Disclosures
B.C. is an employee of Fresenius Medical Care, and R.A.W. is a consultant for Baxter Healthcare. The other authors have no relevant financial arrangements to report.
Supplementary Material
Acknowledgments
This work was supported by the Kidney Health Initiative (KHI), a public-private partnership between the American Society of Nephrology, the US Food and Drug Administration, and >75 member organizations and companies, to enhance patient safety and foster innovation in kidney disease. The KHI funds were used to defray costs incurred during the conduct of the project, including project management support. There was no honorarium or other financial support provided to the KHI workgroup members.
The authors of this paper had final review authority, and they are fully responsible for its content. The KHI makes every effort to avoid actual, potential, or perceived conflicts of interest that may arise from industry relationships or personal interests among the members of the workgroup. More information on the KHI, the workgroup, and the conflict of interest policy can be found at www.kidneyhealthinitiative.org. The views and opinions expressed in this publication are those of the authors and do not necessarily reflect the official policies of any KHI member organization, the US Department of Veterans Affairs, or the US Department of Health and Human Services, and the mention of any trade names, commercial practices, or organizations does not imply endorsement by the US Government.
Members of the KHI hemodiafiltration workgroup were B.C., J.V., S.A., R.A.W., Greg Collins (Nephros, Inc.), William Fissell (Vanderbilt University), Gema Gonzalez (Centers for Devices and Radiological Health, FDA), Shani Haugen (Center for Drug Evaluation and Research, FDA), Robert Kossmann (Fresenius Medical Care - North America), Carolyn Y. Neuland (Centers for Devices and Radiological Health, FDA), Douglas M. Silverstein (Centers for Devices and Radiological Health, FDA), Todd Snell (NxStage Medical, Inc.), Jim Summerton (Nephros, Inc.), and Shen Xiao (Center for Devices and Radiological Health, FDA).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.12631117/-/DCSupplemental.
References
- 1.Archdeacon P, Shaffer RN, Winkelmayer WC, Falk RJ, Roy-Chaudhury P: Fostering innovation, advancing patient safety: The kidney health initiative. Clin J Am Soc Nephrol 8: 1609–1617, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward RA, Vienken J, Silverstein DM, Ash S, Canaud B: Regulatory considerations for hemodiafiltration in the United States. Clin J Am Soc Nephrol 13: 1444–1449, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farrell PC, Babb AL: Estimation of the permeability of cellulosic membranes from solute dimensions and diffusivities. J Biomed Mater Res 7: 275–300, 1973 [DOI] [PubMed] [Google Scholar]
- 4.Wendt RP, Klein E, Bresler EH, Holland FF, Serino RM, Villa H: Sieving properties of hemodialysis membranes. J Membr Sci 5: 23–49, 1979 [Google Scholar]
- 5.Tattersall JE, Ward RA; EUDIAL group: Online haemodiafiltration: Definition, dose quantification and safety revisited. Nephrol Dial Transplant 28: 542–550, 2013 [DOI] [PubMed] [Google Scholar]
- 6.Ward RA, Schmidt B, Hullin J, Hillebrand GF, Samtleben W: A comparison of on-line hemodiafiltration and high-flux hemodialysis: A prospective clinical study. J Am Soc Nephrol 11: 2344–2350, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Maduell F, Navarro V, Cruz MC, Torregrosa E, Garcia D, Simon V, Ferrero JA: Osteocalcin and myoglobin removal in on-line hemodiafiltration versus low- and high-flux hemodialysis. Am J Kidney Dis 40: 582–589, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Donauer J, Schweiger C, Rumberger B, Krumme B, Böhler J: Reduction of hypotensive side effects during online-haemodiafiltration and low temperature haemodialysis. Nephrol Dial Transplant 18: 1616–1622, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Nakai S, Iseki K, Tabei K, Kubo K, Masakane I, Fushimi K, Kikuchi K, Shinzato T, Sanaka T, Akiba T: Outcomes of hemodiafiltration based on Japanese dialysis patient registry. Am J Kidney Dis 38[Suppl 1]: S212–S216, 2001 [DOI] [PubMed] [Google Scholar]
- 10.Locatelli F, Marcelli D, Conte F, Limido A, Malberti F, Spotti D: Comparison of mortality in ESRD patients on convective and diffusive extracorporeal treatments. The Registro Lombardo Dialisi E Trapianto. Kidney Int 55: 286–293, 1999 [DOI] [PubMed] [Google Scholar]
- 11.Ohtake T, Oka M, Ishioka K, Honda K, Mochida Y, Maesato K, Moriya H, Hidaka S, Kobayashi S: Cardiovascular protective effects of on-line hemodiafiltration: Comparison with conventional hemodialysis. Ther Apher Dial 16: 181–188, 2012 [DOI] [PubMed] [Google Scholar]
- 12.Sichart JM, Moeller S: Utilization of hemodiafiltration as treatment modality in renal replacement therapy for end-stage renal disease patients--a global perspective. Contrib Nephrol 175: 163–169, 2011 [DOI] [PubMed] [Google Scholar]
- 13.Akizawa T, Koiwa F: Clinical expectation of online hemodiafiltration: A Japanese perspective. Blood Purif 40[Suppl 1]: 12–16, 2015 [DOI] [PubMed] [Google Scholar]
- 14.Canaud B, N’Guyen QV, Lagarde C, Stec F, Polaschegg HD, Mion C: Clinical evaluation of a multipurpose dialysis system adequate for hemodialysis or for postdilution hemofiltration/hemodiafiltration with on-line preparation of substitution fluid from dialysate. Contrib Nephrol 46: 184–186, 1985 [DOI] [PubMed] [Google Scholar]
- 15.Ledebo I: On-line hemodiafiltration: Technique and therapy. Adv Ren Replace Ther 6: 195–208, 1999 [DOI] [PubMed] [Google Scholar]
- 16.Joyeux V, Sijpkens Y, Haddj-Elmrabet A, Bijvoet AJ, Nilsson L-G: Optimized convective transport with automated pressure control in on-line postdilution hemodiafiltration. Int J Artif Organs 31: 928–936, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Marcelli D, Scholz C, Ponce P, Sousa T, Kopperschmidt P, Grassmann A, Pinto B, Canaud B: High-volume postdilution hemodiafiltration is a feasible option in routine clinical practice. Artif Organs 39: 142–149, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panichi V, De Ferrari G, Saffioti S, Sidoti A, Biagioli M, Bianchi S, Imperiali P, Gabbrielli C, Conti P, Patrone P, Falqui V, Rombolà G, Mura C, Icardi A, Mulas D, Rosati A, Santori F, Mannarino A, Tomei V, Bertucci A, Steckiph D, Palla R: Divert to ULTRA: Differences in infused volumes and clearance in two on-line hemodiafiltration treatments. Int J Artif Organs 35: 435–443, 2012 [DOI] [PubMed] [Google Scholar]
- 19.Penne EL, Visser L, van den Dorpel MA, van der Weerd NC, Mazairac AH, van Jaarsveld BC, Koopman MG, Vos P, Feith GW, Kremer Hovinga TK, van Hamersvelt HW, Wauters IM, Bots ML, Nubé MJ, Ter Wee PM, Blankestijn PJ, Grooteman MP: Microbiological quality and quality control of purified water and ultrapure dialysis fluids for online hemodiafiltration in routine clinical practice. Kidney Int 76: 665–672, 2009 [DOI] [PubMed] [Google Scholar]
- 20.International Organization for Standardization: Quality of Dialysis Fluid for Haemodialysis and Related Therapies (ISO 11663:2014), Geneva, Switzerland, International Organization for Standardization, 2014 [Google Scholar]
- 21.International Organization for Standardization: Guidance for the Preparation and Quality Management of Fluids for Haemodialysis and Related Therapies (ISO 23500:2014), Geneva, Switzerland, International Organization for Standardization, 2014 [Google Scholar]
- 22.Schmitz M, Loke O, Fach B, Kalb K, Heering PJ, Meinke D, Rawer P, Galle J, Kozik-Jaromin J: Effects of citrate dialysate in chronic dialysis: A multicentre randomized crossover study. Nephrol Dial Transplant 31: 1327–1334, 2016 [DOI] [PubMed] [Google Scholar]
- 23.Dhondt A, Pauwels R, Devreese K, Eloot S, Glorieux G, Vanholder R: Where and when to inject low molecular weight heparin in hemodiafiltration? A crossover randomised trial. PLoS One 10: e0128634, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ward RA: Do clinical outcomes in chronic hemodialysis depend on the choice of a dialyzer? Semin Dial 24: 65–71, 2011 [DOI] [PubMed] [Google Scholar]
- 25.Bowry SK, Canaud B: Achieving high convective volumes in on-line hemodiafiltration. Blood Purif 35[Suppl 1]: 23–28, 2013 [DOI] [PubMed] [Google Scholar]
- 26.Canaud B, Lévesque R, Krieter D, Desmeules S, Chalabi L, Moragués H, Morena M, Cristol JP: On-line hemodiafiltration as routine treatment of end-stage renal failure: Why pre- or mixed dilution mode is necessary in on-line hemodiafiltration today? Blood Purif 22[Suppl 2]: 40–48, 2004 [DOI] [PubMed] [Google Scholar]
- 27.Krieter DH, Falkenhain S, Chalabi L, Collins G, Lemke HD, Canaud B: Clinical cross-over comparison of mid-dilution hemodiafiltration using a novel dialyzer concept and post-dilution hemodiafiltration. Kidney Int 67: 349–356, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Canaud B, Bowry SK: Emerging clinical evidence on online hemodiafiltration: Does volume of ultrafiltration matter? Blood Purif 35: 55–62, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Peters SA, Bots ML, Canaud B, Davenport A, Grooteman MP, Kircelli F, Locatelli F, Maduell F, Morena M, Nubé MJ, Ok E, Torres F, Woodward M, Blankestijn PJ; HDF Pooling Project Investigators: Haemodiafiltration and mortality in end-stage kidney disease patients: A pooled individual participant data analysis from four randomized controlled trials. Nephrol Dial Transplant 31: 978–984, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Davenport A, Peters SAE, Bots ML, Canaud B, Grooteman MPC, Asci G, Locatelli F, Maduell F, Morena M, Nubé MJ, Ok E, Torres F, Woodward M, Blankestijn PJ; HDF Pooling Project Investigators: Higher convection volume exchange with online hemodiafiltration is associated with survival advantage for dialysis patients: The effect of adjustment for body size. Kidney Int 89: 193–199, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Canaud B, Barbieri C, Marcelli D, Bellocchio F, Bowry S, Mari F, Amato C, Gatti E: Optimal convection volume for improving patient outcomes in an international incident dialysis cohort treated with online hemodiafiltration. Kidney Int 88: 1108–1116, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Canaud B, Bragg-Gresham JL, Marshall MR, Desmeules S, Gillespie BW, Depner T, Klassen P, Port FK: Mortality risk for patients receiving hemodiafiltration versus hemodialysis: European results from the DOPPS. Kidney Int 69: 2087–2093, 2006 [DOI] [PubMed] [Google Scholar]
- 33.Locatelli F, Karaboyas A, Pisoni RL, Robinson BM, Fort J, Vanholder R, Rayner HC, Kleophas W, Jacobson SH, Combe C, Port FK, Tentori F: Mortality risk in patients on hemodiafiltration versus hemodialysis: A ‘real-world’ comparison from the DOPPS [published online ahead of print October 11, 2017]. Nephrol Dial Transplant doi:10.1093/ndt/gfx277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grooteman MP, van den Dorpel MA, Bots ML, Penne EL, van der Weerd NC, Mazairac AH, den Hoedt CH, van der Tweel I, Lévesque R, Nubé MJ, ter Wee PM, Blankestijn PJ; CONTRAST Investigators: Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J Am Soc Nephrol 23: 1087–1096, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ok E, Asci G, Toz H, Ok ES, Kircelli F, Yilmaz M, Hur E, Demirci MS, Demirci C, Duman S, Basci A, Adam SM, Isik IO, Zengin M, Suleymanlar G, Yilmaz ME, Ozkahya M; Turkish Online Haemodiafiltration Study: Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: Results from the Turkish OL-HDF Study. Nephrol Dial Transplant 28: 192–202, 2013 [DOI] [PubMed] [Google Scholar]
- 36.Penne EL, van der Weerd NC, Bots ML, van den Dorpel MA, Grooteman MP, Lévesque R, Nubé MJ, Ter Wee PM, Blankestijn PJ; CONTRAST investigators: Patient- and treatment-related determinants of convective volume in post-dilution haemodiafiltration in clinical practice. Nephrol Dial Transplant 24: 3493–3499, 2009 [DOI] [PubMed] [Google Scholar]
- 37.Chapdelaine I, Mostovaya IM, Blankestijn PJ, Bots ML, van den Dorpel MA, Lévesque R, Nubé MJ, ter Wee PM, Grooteman MP; CONTRAST investigators: Treatment policy rather than patient characteristics determines convection volume in online post-dilution hemodiafiltration. Blood Purif 37: 229–237, 2014 [DOI] [PubMed] [Google Scholar]
- 38.de Roij van Zuijdewijn CLM, Chapdelaine I, Nubé MJ, Blankestijn PJ, Bots ML, Konings CJAM, Kremer Hovinga TK, Molenaar FM, van der Weerd NC, Grooteman MPC: Achieving high convection volumes in postdilution online hemodiafiltration: A prospective multicenter study. Clin Kidney J 10: 804–812, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maduell F, Moreso F, Pons M, Ramos R, Mora-Macià J, Carreras J, Soler J, Torres F, Campistol V, Martinez-Castelao A; ESHOL Study Group: High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J Am Soc Nephrol 24: 487–497, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morena M, Jaussent A, Chalabi L, Leray-Moragues H, Chenine L, Debure A, Thibaudin D, Azzouz L, Patrier L, Maurice F, Nicoud P, Durand C, Seigneuric B, Dupuy AM, Picot MC, Cristol JP, Canaud B; FRENCHIE Study Investigators: Treatment tolerance and patient-reported outcomes favor online hemodiafiltration compared to high-flux hemodialysis in the elderly. Kidney Int 91: 1495–1509, 2017 [DOI] [PubMed] [Google Scholar]
- 41.Nistor I, Palmer SC, Craig JC, Saglimbene V, Vecchio M, Covic A, Strippoli GF: Convective versus diffusive dialysis therapies for chronic kidney failure: An updated systematic review of randomized controlled trials. Am J Kidney Dis 63: 954–967, 2014 [DOI] [PubMed] [Google Scholar]
- 42.Wang AY, Ninomiya T, Al-Kahwa A, Perkovic V, Gallagher MP, Hawley C, Jardine MJ: Effect of hemodiafiltration or hemofiltration compared with hemodialysis on mortality and cardiovascular disease in chronic kidney failure: A systematic review and meta-analysis of randomized trials. Am J Kidney Dis 63: 968–978, 2014 [DOI] [PubMed] [Google Scholar]
- 43.Mostovaya IM, Blankestijn PJ, Bots ML, Covic A, Davenport A, Grooteman MP, Hegbrant J, Locatelli F, Vanholder R, Nubé MJ; EUDIAL1 – an official ERA-EDTA Working Group: Clinical evidence on hemodiafiltration: A systematic review and a meta-analysis. Semin Dial 27: 119–127, 2014 [DOI] [PubMed] [Google Scholar]
- 44.Lornoy W, De Meester J, Becaus I, Billiouw JM, Van Malderen PA, Van Pottelberge M: Impact of convective flow on phosphorus removal in maintenance hemodialysis patients. J Ren Nutr 16: 47–53, 2006 [DOI] [PubMed] [Google Scholar]
- 45.Cornelis T, van der Sande FM, Eloot S, Cardinaels E, Bekers O, Damoiseaux J, Leunissen KM, Kooman JP: Acute hemodynamic response and uremic toxin removal in conventional and extended hemodialysis and hemodiafiltration: A randomized crossover study. Am J Kidney Dis 64: 247–256, 2014 [DOI] [PubMed] [Google Scholar]
- 46.Penne EL, van der Weerd NC, van den Dorpel MA, Grooteman MP, Lévesque R, Nubé MJ, Bots ML, Blankestijn PJ, ter Wee PM; CONTRAST Investigators: Short-term effects of online hemodiafiltration on phosphate control: A result from the randomized controlled Convective Transport Study (CONTRAST). Am J Kidney Dis 55: 77–87, 2010 [DOI] [PubMed] [Google Scholar]
- 47.Lin CL, Huang CC, Yu CC, Yang HY, Chuang FR, Yang CW: Reduction of advanced glycation end product levels by on-line hemodiafiltration in long-term hemodialysis patients. Am J Kidney Dis 42: 524–531, 2003 [DOI] [PubMed] [Google Scholar]
- 48.Mandolfo S, Borlandelli S, Imbasciati E: Leptin and beta2-microglobulin kinetics with three different dialysis modalities. Int J Artif Organs 29: 949–955, 2006 [DOI] [PubMed] [Google Scholar]
- 49.Patrier L, Dupuy AM, Granger Vallée A, Chalabi L, Morena M, Canaud B, Cristol JP: FGF-23 removal is improved by on-line high-efficiency hemodiafiltration compared to conventional high flux hemodialysis. J Nephrol 26: 342–349, 2013 [DOI] [PubMed] [Google Scholar]
- 50.Panichi V, Rizza GM, Paoletti S, Bigazzi R, Aloisi M, Barsotti G, Rindi P, Donati G, Antonelli A, Panicucci E, Tripepi G, Tetta C, Palla R; RISCAVID Study Group: Chronic inflammation and mortality in haemodialysis: Effect of different renal replacement therapies. Results from the RISCAVID study. Nephrol Dial Transplant 23: 2337–2343, 2008 [DOI] [PubMed] [Google Scholar]
- 51.Carracedo J, Merino A, Nogueras S, Carretero D, Berdud I, Ramírez R, Tetta C, Rodríguez M, Martín-Malo A, Aljama P: On-line hemodiafiltration reduces the proinflammatory CD14+CD16+ monocyte-derived dendritic cells: A prospective, crossover study. J Am Soc Nephrol 17: 2315–2321, 2006 [DOI] [PubMed] [Google Scholar]
- 52.Panichi V, Rosati A, Bigazzi R, Paoletti S, Mantuano E, Beati S, Marchetti V, Bernabini G, Grazi G, Rizza GM, Migliori M, Giusti R, Lippi A, Casani A, Barsotti G, Tetta C; RISCAVID Study Group: Anaemia and resistance to erythropoiesis-stimulating agents as prognostic factors in haemodialysis patients: Results from the RISCAVID study. Nephrol Dial Transplant 26: 2641–2648, 2011 [DOI] [PubMed] [Google Scholar]
- 53.Panichi V, Scatena A, Rosati A, Giusti R, Ferro G, Malagnino E, Capitanini A, Piluso A, Conti P, Bernabini G, Migliori M, Caiani D, Tetta C, Casani A, Betti G, Pizzarelli F: High-volume online haemodiafiltration improves erythropoiesis-stimulating agent (ESA) resistance in comparison with low-flux bicarbonate dialysis: Results of the REDERT study. Nephrol Dial Transplant 30: 682–689, 2015 [DOI] [PubMed] [Google Scholar]
- 54.van der Weerd NC, Den Hoedt CH, Blankestijn PJ, Bots ML, van den Dorpel MA, Lévesque R, Mazairac AH, Nubé MJ, Penne EL, ter Wee PM, Grooteman MP; CONTRAST Investigators: Resistance to erythropoiesis stimulating agents in patients treated with online hemodiafiltration and ultrapure low-flux hemodialysis: Results from a randomized controlled trial (CONTRAST). PLoS One 9: e94434, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Susantitaphong P, Siribamrungwong M, Jaber BL: Convective therapies versus low-flux hemodialysis for chronic kidney failure: A meta-analysis of randomized controlled trials. Nephrol Dial Transplant 28: 2859–2874, 2013 [DOI] [PubMed] [Google Scholar]
- 56.Marcelli D, Bayh I, Merello JI, Ponce P, Heaton A, Kircelli F, Chazot C, Di Benedetto A, Marelli C, Ladanyi E, Kroczak M, Stuard S, Grassmann A, Scatizzi L, Brand K, Canaud B: Dynamics of the erythropoiesis stimulating agent resistance index in incident hemodiafiltration and high-flux hemodialysis patients. Kidney Int 90: 192–202, 2016 [DOI] [PubMed] [Google Scholar]
- 57.Locatelli F, Altieri P, Andrulli S, Bolasco P, Sau G, Pedrini LA, Basile C, David S, Feriani M, Montagna G, Di Iorio BR, Memoli B, Cravero R, Battaglia G, Zoccali C: Hemofiltration and hemodiafiltration reduce intradialytic hypotension in ESRD. J Am Soc Nephrol 21: 1798–1807, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van der Sande FM, Kooman JP, Konings CJ, Leunissen KM: Thermal effects and blood pressure response during postdilution hemodiafiltration and hemodialysis: The effect of amount of replacement fluid and dialysate temperature. J Am Soc Nephrol 12: 1916–1920, 2001 [DOI] [PubMed] [Google Scholar]
- 59.Molina P, Vizcaíno B, Molina MD, Beltrán S, Gonzáles-Moya M, Mora A, Castro-Alonso C, Kanter J, Ávila AI, Górriz JL, Estañ N, Pallardó LM, Fouque D, Carrero JJ: The effect of high-volume online haemodiafiltration on nutritional status and body composition: The ProtEin Stores prEservaTion study [published online ahead of print January 22, 2018]. Nephrol Dial Transplant doi:10.1093/ndt/gfx342 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.