Abstract
Purpose/Introduction
We explored whether the risk of hip, humerus and wrist fracture was associated with markers of inequality using data from Danish health registries.
Methods
All patients 50 years or older with a primary hip (ICD10: S720, S721, S722, and S729) humerus (ICD10: S422, S423, S424, S425, S426, and S427) or wrist (ICD10: S52) fracture were identified from 1/1/1995 to 31/12/2011. Fracture patients were matched 1:1 by age, sex and year of fracture, to a non-fracture control. Markers of inequality were: Income (fifths); marital status (married, divorced, widowed or unmarried); area of residence (remote, rural, intermediate or urban). Conditional logistic regression was used to investigate associations between these exposures, and risk of fracture, adjusting for covariates (smoking, alcohol and Charlson co-morbidity). Interactions were fitted between exposure and covariates where appropriate.
Results
A total of 189,838 fracture patients (37,500 hip; 45,602 humerus; and 106,736 wrist) and 189,838 controls were included. Mean age was 73.9 years (hip), 67.5 years (humerus), and 65.3 years (wrist). High income (5th quintile) was significantly associated with a lower odds ratio of all three fractures, compared to average income (3rd quintile). Married subjects had a significantly decreased odds ratio across all three fractures. However, no overall secular difference was observed regarding the influence of the markers of inequality.
Conclusion
In conclusion, we have demonstrated important, stable associations between social inequality, assessed using income, marital status, and area of residence, and fracture at the population level. These findings can inform approaches to healthcare, and suggest that much thought should be given to novel interventions aimed especially at those living alone, and ideally societal measures to reduce social inequality.
Keywords: Osteoporosis, epidemiology, fracture, inequality, social economic
Introduction
Osteoporotic fractures are a significant healthcare issue in developed countries, despite a decrease in incidence rates of hip fractures in the last decade in many such populations [1,2]. In Denmark, femoral neck fractures are the 14th most common cause of admission to hospital and account for 2% of all admissions [3]. Additionally, wrist fractures are the fifth most common reason for emergency room contacts and the seventh most common reason for an outpatient visit [3]. Osteoporotic fractures result in subsequent excess morbidity and mortality [4,5] and significantly affect the quality of life [6]. Whilst there is much information on clinical risk factors for fractures [7], there has been much less work directed at societal risk factors such as education and income.
The social determinants of health can be divided into societal-level influences and individual-level risk factors such as ethnicity, religion, socioeconomic status, and disability [8,9]. Social inequality appears to be increasing in many countries around the world, and this leads to unwanted differences in outcome of the same treatment strategy across strata of the population. The association between risk of fracture and different measures of socioeconomic status have been investigated predominantly in retrospective observational studies [10–13]. The results from these studies provide limited evidence for the association between outcome and exposures, and thus more research is needed to investigate whether measures of socioeconomic status could be used for future prevention strategies for osteoporotic fractures. Thus the aim of the current study was to investigate the association over time between the risk of hip, humerus and wrist fracture, and markers of inequality (area of residence, marital status, and income) in a population-based study.
Methods
Source of data and study population
We conducted a population-based case-control study with data obtained from the Danish health registries. The cases and controls were identified using the National Patient Register with complete coverage of inpatient contacts to the hospital since 1977 and outpatient contacts since 1994. The Danish health registries comprise all contacts with healthcare services both at public and private facilities for all 5.7 million citizens. The National Patient Register was the source of identification of cases for this study and includes complete registrations on the classification of diseases (ICD10 codes), surgical procedures (NCSP codes), and administrative variables (time and place of treatment). In Denmark, all citizens are provided with a personal identification number at birth or at occupancy in the country. This number is used for all contact with governmental agencies and hence also within the healthcare system and can thus be used to link information about citizens between different registers.
All patients aged 50 years or over with a primary hip fracture (ICD10 diagnosis codes S720, S721, S722, and S729), humerus fracture (ICD 10 diagnosis codes S422, S423, S424, S425, S426, and S427) or wrist fracture (ICD 10 diagnosis codes S52) were identified for the period January 1st, 1995 to December 31st, 2011. Fracture patients were matched 1:1 by age, sex and year of fracture to a non-fracture control.
Data for the study was supplied anonymized by Statistics Denmark Division of Research Services (project reference number: 703381) and subject to control by the Danish Data Protection Agency. Ethics committee approval is not required for epidemiology studies in Denmark.
Exposures
Income is recorded as the amount of DKK (kroner) each person earned as registered in the latest annual tax return before fracture. All incomes were adjusted for differential timing to 2011 prices using the consumer price index from Statistics Denmark and converted to € at the rate 1€ = 7.46 DKK. Income was grouped into fifths for analysis.
As the regional government reimburses the healthcare provider whenever a patient is treated, this allows registration on the area of residence via the National Patient Register, from which data for this study were retrieved. The classification of the area of residence, which we obtained from the Civic Person Register, is based on a previous categorization by the Ministry for Food, Agriculture, and Fisheries of Denmark, where municipalities are grouped as remote, rural, intermediate or urban [14]. Hence, within-country variations can be investigated.
The type of municipality is determined using fourteen indicator variables, which divides the 98 Danish municipalities into four classes: remote, rural, intermediate or urban. Remote and rural municipalities are primarily associated with migration to urban areas and higher unemployment. Intermediate and urban municipalities have a younger population and lower unemployment rates.
Remote areas (n=16 municipalities) are characterised as areas where more than half of the inhabitants live outside cities with more than 3000 inhabitants and where there is more than 30 minutes’ drive to a major city.
Rural areas (n=29 municipalities) are characterised as areas where more than half of the inhabitants live outside cities with more than 3000 inhabitants but where there is less than 30 minutes’ drive to a major city.
Intermediate areas (n=18 municipalities) are characterised as areas where at least half of the inhabitants live in cities with more than 3000 inhabitants but where there is more than 30 minutes’ drive to a major city.
Urban areas (n=35 municipalities) are characterised as areas where at least half of the inhabitants live in cities with more than 3000 inhabitants but where there is less than 30 minutes’ drive to a major city.
Marital status is registered in the Civil Registration System for all citizens and is in this study defined as married, divorced, widowed or unmarried, as according to the classification from Statistics Denmark. Both cases and controls had to have a valid registration of income, area of residence, and marital status to be included in the study. Hence, if either one had a missing value, the pair was excluded from further analysis.
Covariates
Patients were classified as smokers (current vs. former status is unknown) or non-smokers through either a chronic obstructive pulmonary disease (COPD) diagnosis, a prescription for bronchodilator/corticosteroids or smoking cessation drug (ATC: N07BA01) [15]. Excess alcohol consumption was defined as either an alcohol-related diagnosis (ICD-10: F10) or treatment with medications exclusively used in management of alcohol dependence (Disulfiram ATC: N07BB01 or Acamprosate N07BB03). The classifications of both smoking and excess alcohol consumption will only capture those individuals with treatment requirements or complications from this addiction but served as the only method to control for these known clinical risk factors in this register-based design. The previous use of anti-osteoporotic medication (ATC: G03XC01, H05AA02, H05BA, M05BX04) in the year leading up to fracture was additionally registered. The degree of co-morbidity was classified for each patient by using the Charlson Comorbidity Index [16]. Diagnostic data from across all diagnostic fields was used to create a weighted score, and an ordinal variable was created (none: Co-morbidity Index Score 0; mild: Co-morbidity Index Score 1; moderate: Co-morbidity Index Score 2; severe: Co-morbidity Index Score 3 or more). The confounding effects of age, sex and year of fracture are balanced by design through matching.
Statistical methods
The outcome is a binary variable of whether or not a patient sustained a fracture, i.e. case or control. Conditional logistic regression modeling was used to describe the association of income, area of residence, and marital status on risk of hip, humerus and wrist fractures, adjusting for covariates. For hip, humerus, and wrist fractures, the model included interactions where appropriate; i.e., between two covariates (income and marital status) and Charlson Comorbidity Index. Furthermore, secular trends were investigated by combining results from subgroups classified as 1995-2000, 2001-2006 or 2007-2011 for the year of fracture. All data management was carried out within the closed-circuit research server provided by Statistics Denmark and analyzed using Stata 14 (StataCorp, College Station, TX, USA).
Results
Study population
From the dataset, 671,958 fracture patients were identified, and after exclusion based on predefined characteristics and matching to a non-fracture control, 702,758 individuals (351,379 cases and equivalent number of controls) were included for further analysis. Information on income, marital status, and area of residence was only available from Statistics Denmark for a subset of patients, mainly due to substantial lack of income data. The eligible population differed from the included population on some clinically relevant parameters, as the included population was a little younger (4-6 year), more likely to be male (1.5-3.6 percentage points) and included for analysis in later years. For more details between the two populations, see Supplementary Table 1. The final analyses included 189,838 fracture cases and an equivalent number of control subjects. Demographics of fracture patients and controls are as described in Table 1. As expected, patients with a wrist fracture were on average youngest and hip fracture patients on average were oldest. The majority of individuals included for analysis were women (68.9-79.5% of women vs 20.5-31.2% men). Furthermore, individuals who sustained a fracture were more likely to smoke, drink excess alcohol and have higher Charlson Comorbidity Index scores compared to the matched controls (Table 1). The exposure variables were also significantly different distributed between fracture and controls with fracture patients having both lower income, living in urban communities and more often living alone (Table 1). The three fracture types investigated (Table 2) exhibited a similar overall tendency in terms of the association with income, where it appeared that high income is a significant protective factor for risk for fracture. This was most pronounced for hip fractures and least for wrist fracture. People living alone had a significantly increased risk for fracture; unmarried individuals had the highest likelihood of fracture followed by divorced and widowed individuals. People living in urban areas were more likely to sustain a humerus and wrist fracture, whereas people living in remote areas were more likely to sustain a hip fracture.
Table 1.
Demographics
| Hip fracture | Humerus fracture | Wrist fracture | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | |||||||
| N | 37,500 | 37,500 | 45,602 | 45,602 | 106,736 | 106,736 | ||||||
| Matching variables | ||||||||||||
| Age; mean (s.d.) | 73.9 | (9.5) | 73.9 | (9.5) | 67.5 | (10.1) | 67.5 | (10.1) | 65.3 | (9.6) | 65.3 | (9.6) |
| Gender | ||||||||||||
| Male; n (%) | 11,680 | (31.2%) | 11,680 | (31.2%) | 11,968 | (26.2%) | 11,968 | (26.2%) | 21,845 | (20.5) | 21,845 | (20.5) |
| Female; n (%) | 25,820 | (68.8%) | 25,820 | (68.8%) | 33,634 | (73.8%) | 33,634 | (73.8%) | 84,891 | (79.5) | 84,891 | (79.5) |
| Year of fracture | ||||||||||||
| 1995 to 2000; n (%) | 4,108 | (11.0) | 4,108 | (11.0) | 7,980 | (17.5) | 7,980 | (17.5) | 26,497 | (24.8) | 26,497 | (24.8) |
| 2001 to 2006; n (%) | 14,072 | (37.5) | 14,072 | (37.5) | 17,351 | (38.1) | 17,351 | (38.1) | 40,172 | (37.6) | 40,172 | (37.6) |
| 2007 to 2011; n (%) | 19,320 | (51.5) | 19,320 | (51.5) | 20,271 | (44.5) | 20,271 | (44.5) | 40,067 | (37.5) | 40,067 | (37.5) |
| Exposures | ||||||||||||
| Income, € in thousands | ||||||||||||
| 1st Quintile; mean [IQR] | 14.8 | [0;18] | 14.6 | [0;18] | 14.6 | [0;19] | 14.5 | [0;19] | 14.4 | [0;18] | 14.3 | [0;18] |
| 2nd Quintile; mean [IQR] | 20.9 | [18;23] | 20.9 | [18;23] | 21.5 | [19;24] | 21.4 | [19;23] | 21.5 | [18;24] | 21.5 | [18;24] |
| 3rd Quintile; mean [IQR] | 24.5 | [23;26] | 24.4 | [23;26] | 25.3 | [24;28] | 25.3 | [24;28] | 25.7 | [24;28] | 25.7 | [24;28] |
| 4th Quintile; mean [IQR] | 29.5 | [26;35] | 29.7 | [26;35] | 32.0 | [28;38] | 32.2 | [28;38] | 33.6 | [28;40] | 33.8 | [28;40] |
| 5th Quintile; mean [IQR] | 53.7 | [35;3,423] | 57.2 | [35;6,938] | 61.3 | [38;3,423] | 62.3 | [38;2,749] | 63.3 | [40;3,444] | 65.0 | [40;8,809] |
| Marital status | ||||||||||||
| Married; n (%) | 12,819 | (34.2) | 16,372 | (43.7) | 19,016 | (41.7) | 23,665 | (51.9) | 51,740 | (48.5) | 56,956 | (53.3) |
| Widowed; n (%) | 5,965 | (42.6) | 15,351 | (40.9) | 14,194 | (31.1) | 13,616 | (29.9) | 30,579 | (28.7) | 29,613 | (27.7) |
| Divorced; n (%) | 5,428 | (14.5) | 3,778 | (10.1) | 8,165 | (17.9) | 5,530 | (12.1) | 16,609 | (15.6) | 13,683 | (12.8) |
| Unmarried; n (%) | 3,288 | (8.8) | 1,999 | (5.3) | 4,227 | (9.3) | 2,791 | (6.1) | 7,808 | (7.3) | 6,484 | (6.1) |
| Urban | ||||||||||||
| Remote | 4,185 | (11.2) | 4,208 | (11.2) | 4,362 | (9.6) | 4,955 | (10.9) | 11,263 | (10.6) | 11,467 | (10.7) |
| Rural | 10,971 | (29.3) | 11,307 | (30.2) | 12,160 | (26.7) | 13,849 | (30.4) | 30,300 | (28.4) | 32,290 | (30.3) |
| Intermediate | 5,857 | (15.6) | 5,885 | (15.7) | 6,826 | (15.0) | 7,361 | (16.1) | 16,628 | (15.6) | 17,128 | (16.1) |
| Urban | 16,487 | (44.0) | 16,100 | (42.9) | 22,254 | (48.8) | 19,437 | (42.6) | 48,545 | (45.5) | 45,851 | (43.0) |
| Covariates | ||||||||||||
| Smoking (imputed) | ||||||||||||
| Non-smoker; n (%) | 30,176 | (80.5) | 33,412 | (89.1) | 39,031 | (85.6) | 41,397 | (90.8) | 95,181 | (89.2) | 97,537 | (91.4) |
| Smoker; n (%) | 7,324 | (19.5) | 4,088 | (10.9) | 6,571 | (14.4) | 4,205 | (9.2) | 11,555 | (10.8) | 9,199 | (8.6) |
| Alcohol (imputed) | ||||||||||||
| Non-drinker; n (%) | 33,794 | (90.1) | 36,653 | (97.7) | 39,137 | (85.8) | 44,316 | (97.2) | 98,583 | (92.4) | 103,691 | (97.1) |
| Drinker; n (%) | 3,706 | (9.9) | 847 | (2.3) | 6,465 | (14.2) | 1,286 | (2.8) | 8,153 | (7.6) | 3,045 | (2.9) |
| Charlson comorbidity index | ||||||||||||
| None; n (%) | 9,040 | (24.1) | 15,669 | (41.8) | 17,355 | (38.1) | 23,181 | (50.8) | 52,707 | (49.4) | 56,811 | (53.2) |
| Mild; n (%) | 7,854 | (20.9) | 6,945 | (18.5) | 8,641 | (19.0) | 7,536 | (16.5) | 18,323 | (17.2) | 17,212 | (16.1) |
| Moderate; n (%) | 7,068 | (18.9) | 6,315 | (16.8) | 7,419 | (16.3) | 6,690 | (14.7) | 15,866 | (14.9) | 15,125 | (14.2) |
| Severe; n (%) | 13,538 | (36.1) | 8,571 | (22.9) | 12,187 | (26.7) | 8,195 | (18.0) | 19,840 | (18.6) | 17,588 | (16.5) |
| Previous OP medication | 3,187 | (8.5) | 1,514 | (4.0) | 89 | (0.2) | 40 | (0.1) | 114 | (0.1) | 65 | (0.1) |
OP=osteoporosis
Table 2.
Multivariate conditional logistic regression model to describe association of socioeconomic predictors on risk of fracture.
| Hip fracture Odds Ratio (95% CI) |
Humerus fracture Odds Ratio (95% CI) |
Wrist fracture Odds Ratio (95% CI) |
|
|---|---|---|---|
| Income | |||
| 1st Quintile | 1.01 (0.92; 1.12) | 0.98 (0.91; 1.06) | 0.97 (0.93; 1.01) |
| 2nd Quintile | 0.94 (0.86; 1.04) | 1.00 (0.93; 1.08) | 0.95 (0.91; 0.99) |
| 3rd Quintile | Ref | Ref | Ref |
| 4th Quintile | 0.97 (0.89; 1.06) | 0.96 (0.89; 1.03) | 1.01 (0.97; 1.05) |
| 5th Quintile | 0.78 (0.72; 0.85) | 0.85 (0.80; 0.91) | 0.95 (0.91; 0.99) |
| Marital status | |||
| Married | Ref | Ref | Ref |
| Widowed | 1.53 (1.42; 1.65) | 1.26 (1.19; 1.34) | 1.13 (1.09; 1.17) |
| Divorced | 1.60 (1.45; 1.77) | 1.35 (1.26; 1.44) | 1.18 (1.14; 1.23) |
| Unmarried | 2.24 (2.01; 2.49) | 1.68 (1.55; 1.82) | 1.20 (1.14; 1.26) |
| Area of residence | |||
| Remote | Ref | Ref | Ref |
| Rural | 0.95 (0.90; 1.00) | 0.98 (0.94; 1.04) | 0.95 (0.92; 0.98) |
| Intermediate | 0.96 (0.90; 1.02) | 1.03 (0.97; 1.09) | 0.98 (0.94; 1.01) |
| Urban | 0.94 (0.90; 0.99) | 1.22 (1.16; 1.28) | 1.04 (1.01; 1.07) |
| Smoking1 | 1.29 (1.23; 1.35) | 1.12 (1.07; 1.18) | 1.12 (1.09; 1.16) |
| Alcoholism1 | 3.60 (3.31; 3.92) | 4.65 (4.34; 4.98) | 2.60 (2.48; 2.72) |
| Previous OP medication | 2.06 (1.92; 2.21) | 1.88 (1.27; 2.79) | 1.63 (1.20; 2.23) |
| Charlson comorbidity index | |||
| None | Ref | Ref | Ref |
| Mild | 1.89 (1.66; 2.15) | 1.40 (1.25; 1.56) | 1.08 (1.01; 1.16) |
| Moderate | 1.80 (1.58; 2.16) | 1.42 (1.27; 1.60) | 1.12 (1.04; 1.20) |
| Severe | 2.93 (2.60; 3.31) | 2.02 (1.82; 2.24) | 1.24 (1.16; 1.32) |
Please see methods section for how these exposed were imputed
Note: table represents single multivariate model
OP=osteoporosis
Socioeconomic status and hip fracture risk
Reduced odds of hip fracture was observed for the highest fifth of income compared to third (average) group (Odds ratio (OR): 0.78, 95% CI 0.72; 0.85), Table 2. The likelihood of hip fracture was highest in unmarried individuals (OR: 2.25, 95% CI 2.02-2.51), compared with married individuals. The likelihood of hip fracture was also significantly higher for widowed and divorced individuals compared to married. The odds of hip fracture were significantly decreased for both rural (OR: 0.95, 95% CI 0.90-0.99) and urban (OR: 0.94, 95% CI 0.89-0.99) residents compared to those individuals living in remote areas. Table 2 summarizes these findings.
Socioeconomic status and humerus fracture risk
Similarly, reduced odds of humerus fracture was observed for the highest fifth of income compared to third (average) group (OR: 0.85, 95% CI 0.80; 0.91), Table 2. The likelihood of humerus fracture was highest in unmarried individuals (OR: 1.68, 95% CI 1.55-1.82), compared with married individuals. Humerus fracture was also significantly more likely for widowed and divorced individuals compared to married. The odds of humerus fracture were significantly increased for urban residents (OR: 1.22, 95% CI 1.16-1.28) compared to those individuals living in remote areas. These results are again summarized in Table 2.
Socioeconomic status and wrist fracture risk
Consistent with the findings for hip and humerus fracture, reduced odds of wrist fracture was observed for the highest fifth of income compared to third (average) group (OR: 0.95, 95% CI 0.91; 0.99), Table 2. The odds of wrist fracture was highest in unmarried individuals (OR: 1.04, 95% CI 1.01-1.07), compared with married individuals. Furthermore, the odds of wrist fracture was significantly lower for people residing in rural areas. The likelihood of wrist fracture was also significantly higher for individuals living alone compared to married (all summarized in Table 2).
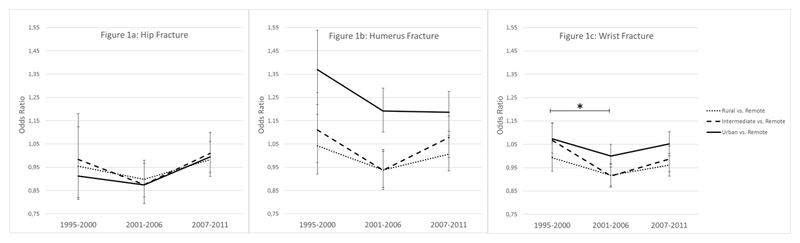
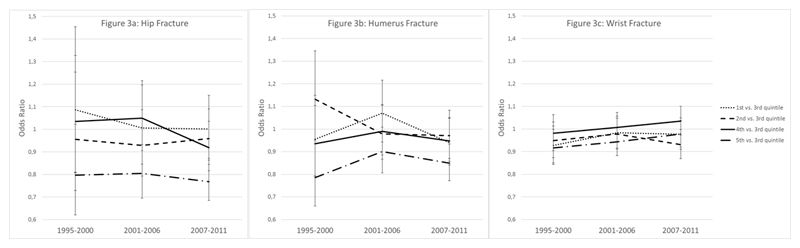
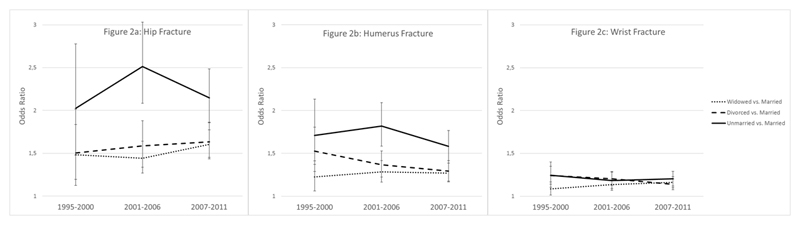
Secular trends of socioeconomic status (Figures 1 to 3)
Figure 1.
Secular trends of association between area of residence (urbanisation) and risk of fracture for three time intervals. Star (*) indicates statistically significant difference for intermediate vs remote residence; p-value<0.0001.
Figure 3.
Secular trends of association between income and risk of fracture for three time intervals.
There was no overall significant difference across the three fracture groups in terms of any secular trends between social determinants (marital status, area of residence or income) and risk of fracture. The only significant observation was observed for intermediate vs remote residence between 1995-2000 and 2001-2006; p<0.0001 (Figure 1).
Discussion
The results from the present study provide evidence that social determinants (marital status, area of residence and income) are strongly associated with the risk of osteoporotic fractures and there is no trend that the influence of socioeconomics has been diminishing over time. The association between living alone and risk of any fracture was particularly pronounced, and almost as marked as the risk associated with health covariates (smoking, increased alcohol intake and severe comorbidities). This emphasizes the need for future preventions strategies to address the social inequality observed within these patient groups. Furthermore, the association between social determinants and risk of fracture was independent of time over a fifteen year period, indicating that there is no sign of the impact of social inequality diminishing despite improvements in osteoporosis diagnosis and decreasing costs of the main osteoporosis treatments, which have been available as generics for several years. The latter would be expected to have significant impact on treatment uptake in countries such as Denmark where a significant part of medication costs are carried by the patients themselves unless covered by a private health insurance policy. Introduction of generics also likely affect treatment uptake in healthcare systems where there is no co-payment for medications, though here the change takes place at the level of insurers and health services through adjustments to prescription guidelines and through changes to the willingness of payers to cover such treatment.
Previous studies investigating these associations have generated inconsistent results [11–13,17]. This may be a result of different definitions of variables investigated and hence lead to non-comparable groups across study populations. For example, the categorization of income may be quarters, other pre-defined groups, or by presence/absence of private health insurance. In a population-based study, Curtis and colleagues showed that area of residence, ethnicity and socioeconomic status (measured as deprivation) significantly influenced the fracture risk [18]. The association between risk of fracture and area of residence was in some areas more than 30% higher than the referent (London). These results are however not directly comparable to the results of this present study as the areas of residence categorization cannot be directly compared between studies.
Although the lack of universal definitions of socioeconomic indices may at least partly explain the variation across previous findings, even when the same definitions are used across countries it can be difficult to compare results, as the purchasing power per unit income may be different. Furthermore, access to health services will differ depending on the organization of the healthcare system. For example, access to healthcare in systems based on insurance, such as the US, is likely to be much more dependent on societal factors than access to systems based on universal provision free at the point of care, such as in the UK and Denmark.
The question then becomes who is responsible for this inequality- either patients themselves as they attribute different values on health depending on their societal position and wealth, or the society as a whole, as for example Danish legislation promulgates health equity for all [19]. In regards to social determinants, ethnicity and socioeconomic status are of specific interest to fracture patients, as studies have shown that morbidity is associated with these attributes [20–22]. Within the Danish population the vast majority is Caucasian (Statistics Denmark), and hence ethnicity was not considered further in this study.
The strengths of this study are that it includes a substantial number of individuals from the whole population included for analysis, with robustly collected information on fractures and socioeconomic variables due to the use of registries [23], allowing selection bias in recruitment to largely avoided. Personal income was not imputed from area of residence but available at individual patient level. However, there are some limitations which should be considered in the interpretation of our results. Firstly, the use of income as an indicator of socioeconomic status may be less relevant to the older population, mostly in relation to the risk of hip fracture, as they are usually retired, with current income possibly lower than reflecting true societal status, which likely depends more on lifetime earnings and savings than on present income. Secondly, we lacked direct quantitative measures for alcohol consumption and smoking. However, the approach taken has been successfully documented in previous studies using registry data[15]. Thirdly, we were unable to directly capture information on all potentially relevant factors which might have changed over the study period, for example, body mass index, smoking, or alcohol. These variables have previously been shown to influence the risk of fracture[7]. Though a substantial part of the eligible population was excluded due to missing data, the characteristics of the included and excluded populations were similar, suggesting that the results are likely to be representative for the entire population (see supplementary table 1). Finally, it is likely that low income and single living is more likely in persons with chronic comorbid conditions that are not fully captured by a hospital contacts based Charlson Comorbidity Index calculation. Indeed, living alone or in remote locations could decrease the likelihood of comorbid conditions coming to the attention of the health services.
In conclusion, we have demonstrated important associations between social inequality, assessed using marital status, area of residence and income, and fracture at the population level. These findings, and the observation that such differences have persisted over recent decades, can inform approaches to healthcare, and suggest that much thought should be given to novel interventions aimed at those of lower income and living alone, and ideally societal measures to reduce social inequality.
Supplementary Material
Summary.
We examined links between markers of social inequality and fracture risk in the Danish population, demonstrating that high income and being married are associated with a significantly lower risk.
Figure 2.
Secular trends of association between marital status and risk of fracture for three time intervals.
Footnotes
Disclosures
Louise Hansen, Andrew Judge, M Kassim Javaid, Cyrus Cooper, Peter Vestergaard, Nicholas C Harvey declare that they have no conflicts of interest. Bo Abrahamsen has institutional research grants from UCB and Novartis with funds paid to the institution.
References
- [1].Hansen L, Petersen KD, Eriksen Sa, et al. Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int. 2014;26:513–519. doi: 10.1007/s00198-014-2875-2. [DOI] [PubMed] [Google Scholar]
- [2].Omsland TK, Holvik K, Meyer HE, et al. Hip fractures in Norway 1999–2008: time trends in total incidence and second hip fracture rates. A NOREPOS study. Eur J Epidemiol. 2012;27:807–814. doi: 10.1007/s10654-012-9711-9. [DOI] [PubMed] [Google Scholar]
- [3].Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ryg J, Rejnmark L, Overgaard S, et al. Hip Fracture Patients at Risk of Second Hip Fracture: A Nationwide Population-Based Cohort Study of 169,145 Cases During 1977–2001. J Bone Min Res. 2009;24:1299–1307. doi: 10.1359/jbmr.090207. [DOI] [PubMed] [Google Scholar]
- [5].Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–21. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- [6].Si L, Winzenberg TM, de Graaff B, et al. A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int. 2014;25:1987–1997. doi: 10.1007/s00198-014-2636-2. [DOI] [PubMed] [Google Scholar]
- [7].Abrahamsen B, Brask-Lindemann D, Rubin KH, et al. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. Bonekey Rep. 2014;3:574. doi: 10.1038/bonekey.2014.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q. 2004;82:101–124. doi: 10.1111/j.0887-378X.2004.00303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Baker E, Metzler M, Galea S. Addressing Social Determinants of Health Disparities: Learning From Doing. Am J Public Health. 2005;95:553–556. doi: 10.2105/AJPH.2005.061812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Omsland TK, Eisman Ja, Naess Ø, et al. Educational Inequalities in Post-Hip Fracture Mortality: A NOREPOS Studys. J bone Miner Res. 2015;30:2221–2228. doi: 10.1002/jbmr.2579. [DOI] [PubMed] [Google Scholar]
- [11].Vestergaard P, Rejnmark L, Mosekilde L. Socioeconomic aspects of fractures within universal public healthcare: a nationwide case-control study from Denmark. Scand J Public Health. 2006;34:371–377. doi: 10.1080/14034940500441223. [DOI] [PubMed] [Google Scholar]
- [12].Farahmand P, Persson PG, Michaelsson K, et al. Socioeconomic Status, Marital Status and Hip Fracture Risk : A Population-Based Case-Control Study. Osteoporos Int. 2000;11:803–808. doi: 10.1007/s001980070060. [DOI] [PubMed] [Google Scholar]
- [13].Peel NM, McClure RJ, Hendrikz JK. Psychosocial factors associated with fall-related hip fractures. Age Ageing. 2007;36:145–151. doi: 10.1093/ageing/afl167. [DOI] [PubMed] [Google Scholar]
- [14].Velfærdsministeriet, Ministeriet for Fødevarer Landbrug og Fiskeri. Landdistriktsredegørelse 2009. København K: 2009. [Google Scholar]
- [15].Thvilum M, Brandt F, Almind D, et al. Excess mortality in patients diagnosed with hypothyroidism: a nationwide cohort study of singletons and twins. J Clin Endocrinol Metab. 2013;98:1069–1075. doi: 10.1210/jc.2012-3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- [17].Wilson RT, Chase Ga, Chrischilles Ea, et al. Hip fracture risk among community-dwelling elderly people in the United States: A prospective study of physical, cognitive, and socioeconomic indicators. Am J Public Health. 2006;96:1210–1218. doi: 10.2105/AJPH.2005.077479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Curtis EM, van der Velde R, Moon RJ, et al. Epidemiology of fractures in the United Kingdom 1988-2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19–26. doi: 10.1016/j.bone.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Brazier J, Ratcliffe J, Salomon JA, et al. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford University Press; 2007. [Google Scholar]
- [20].Dawson-Hughes B, Tosteson ANA, Melton LJ, et al. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–458. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- [21].Curtis JR, McClure LA, Delzell E, et al. Population-Based Fracture Risk Assessment and Osteoporosis Treatment Disparities by Race and Gender. J Gen Intern Med. 2009;24:956–962. doi: 10.1007/s11606-009-1031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Brennan SL, Pasco Ja, Urquhart DM, et al. The association between socioeconomic status and osteoporotic fracture in population-based adults: A systematic review. Osteoporos Int. 2009;20:1487–1497. doi: 10.1007/s00198-008-0822-9. [DOI] [PubMed] [Google Scholar]
- [23].Thygesen LC, Ersbøll AK. When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol. 2014:1–8. doi: 10.1007/s10654-013-9873-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.