Abstract
Introduction
Link4Health, a cluster-RCT, demonstrated the effectiveness of a combination strategy targeting barriers at various HIV continuum steps on linkage to and retention in care; showing effectiveness in achieving linkage to HIV care within 1 month plus retention in care at 12 months after HIV testing for people living with HIV (RR 1.48, 95% CI 1.19–1.96, p = 0.002). In addition to standard of care, Link4Health included: 1) Point-of-care CD4+ count testing; 2) Accelerated ART initiation; 3) Mobile phone appointment reminders; 4) Care and prevention package including commodities and informational materials; and 5) Non-cash financial incentive. Our objective was to evaluate the cost-effectiveness of a scale-up of the Link4Health strategy in Swaziland.
Methods and findings
We incorporated the effects and costs of the Link4Health strategy into a computer simulation of the HIV epidemic in Swaziland, comparing a scenario where the strategy was scaled up to a scenario with no implementation. The simulation combined a deterministic compartmental model of HIV transmission with a stochastic microsimulation of HIV progression calibrated to Swaziland epidemiological data. It incorporated downstream health costs potentially saved and infections potentially prevented by improved linkage and treatment adherence. We assessed the incremental cost-effectiveness ratio of Link4Health compared to standard care from a health sector perspective reported in US$2015, a time horizon of 20 years, and a discount rate of 3% in accordance with WHO guidelines.[1] Our results suggest that scale-up of the Link4Health strategy would reduce new HIV infections over 20 years by 11,059 infections, a 7% reduction from the projected 169,019 cases and prevent 5,313 deaths, an 11% reduction from the projected 49,582 deaths. Link4Health resulted in an incremental cost per infection prevented of $13,310 and an incremental cost per QALY gained of $3,560/QALY from the health sector perspective.
Conclusions
Using a threshold of <3 x per capita GDP, the Link4Health strategy is likely to be a cost-effective strategy for responding to the HIV epidemic in Swaziland.
Introduction
Swaziland has the highest prevalence of HIV in the world. With a population of 1.1 million persons, Swaziland has an estimated adult (age 18–49 years) HIV prevalence of 31% and an estimated HIV incidence of 2.4%.[2–4] The country has made impressive strides to respond to the epidemic by increasing the number of HIV-positive adults on antiretroviral therapy (ART) from 72,402 in 2011 to 147,274 in 2015.[5] However, evidence shows that linkage to and retention in care after ART initiation remains suboptimal.[6, 7]
In order to garner the individual and societal benefits from ART, HIV-positive individuals must achieve all steps of the HIV care continuum.[8–11] The care continuum has been shown to be fragile with critical gaps reported from multiple studies conducted in sub-Saharan African countries including high attrition from testing to linkage to care and suboptimal retention in ongoing care.[12–20] Despite the interdependent nature of the steps in the HIV care continuum, most studies have only considered the effect of an individual intervention on one step in the HIV care continuum,[21–24] and few have studied a combination approach that targets multiple barriers along the continuum.[25]
The Link4Health Study, a cluster-randomized controlled trial that evaluated a combined multi-intervention strategy aimed at various steps in the HIV care continuum demonstrated significant improvement in the primary outcome of linkage to HIV care within 1 month of HIV testing plus retention in care at 12 months after HIV testing for people living with HIV (PLWH) in Swaziland (RR 1.48, 95% CI 1.19–1.96, p = 0.002).[26] The study compared standard of care alone with standard of care along with multiple evidence-based structural, biomedical, and behavioral interventions, including point of care CD4+ cell count testing, rapid ART initiation, SMS visit reminders, financial incentives, and provision of health packages to motivate linkage and retention. The study design was described previously.[26, 27]
Neither, the cost-effectiveness of the Link4health in Swaziland and similar contexts, nor other similar multi-component interventions, however, have been assessed. We aimed to evaluate the cost-effectiveness of this scale-up through use of a computer simulation of HIV progression and transmission, comparing a scenario in which the Link4Health strategy was scaled up with a counterfactual scenario with no implementation of the Link4Health strategy.
Methods
Analyses were performed using a combined stochastic natural history model and deterministic, compartment model of the HIV epidemic in Swaziland. A previously developed model of HIV progression and transmission for east Africa [28] was modified to be calibrated to Swaziland epidemiological data and parameterized with the observed effects and costs of the Link4Health strategy (Table 1). Using the simulation, the impact and cost-effectiveness of a nationwide scale-up of the Link4Health strategy in Swaziland was projected.
Table 1. Key input parameters.
| Description of parameter input | Value | References |
|---|---|---|
| Alcohol use | ||
| Prevalence of unhealthy alcohol use (Male/Female) | 9.7%/2% | [29] |
| Relative risk of unhealthy alcohol use on condom misuse or non-use | 1.29 | [30] |
| Relative risk of unhealthy alcohol use on non-HIV STIs | 1.72 | [30] |
| Relative risk of unhealthy alcohol use on non-adherence to ART | 2.33 | [30] |
| Sexual risk behaviors | ||
| Proportion abstinent (M/F) | 5%/10% | [31–34] |
| Proportion monogamous (M/F) | 31%/69% | [34–36] |
| Proportion in multiple, concurrent relationships (M/F) | 56%/17% | Assumption |
| Proportion who are clients of (men) or who are CSW (female) (M/F) | 8%/4% | [37, 38] |
| Frequency of sex acts (per year) | 104 | Assumption |
| Duration of relationship | 1y-30y | Assumption |
| Median number of concurrent partners- non CSW | 3 | [36] |
| Median number of concurrent partners- CSW | 10 | [36] |
| Probability of consistent condom use | 56.8% | [39] |
| Relative risk of unsafe sex (condom nonuse most or all of the time) if aware of HIV status | 0.47 | [40] |
| HIV epidemiology and transmission | ||
| Adult HIV prevalence (1997) | 20.9% | [41] |
| Probability of transmission per sex act | 0.00011–0.01243 | [42, 43] |
| Prevalence of circumcision among adult men | 20% | [39] |
| Modifier of male circumcision on F→M HIV transmission per sex act | RR 0.6 | [44] |
| Modifier of consistent condom use on HIV transmission per sex act | RR 0.2 | [45] |
| Untreated non-HIV STI prevalence | 6% | [46] |
| Probability of HIV testing | 40% | [39] |
| Probability of linkage to HIV care and treatment | 50.3% | [39] |
| Probability of adherence to ART regimen | 84% | [47] |
| Intervention effects and costs | ||
| Modifier of Intervention on Linkage and Retention | RR 1.48 | RCT |
| Outpatient care, per year, no ART (visits, SMS, BCPP, Financial incentives) | $324 | RCT |
| On Site CD4+ test available | $26 | RCT |
| Utilities | ||
| Decrease in utility with ART | 0.053 | [48] |
| Utility with CD4+ count < 50 cells/mm3 | 0.69 | [49, 50] |
| Utility with CD4+ count between 50 cells/mm3 and 199 cells/mm3 | 0.79 | [50] |
| Utility with CD4+ count ≥200 cells/mm3 | 0.83 | [50] |
| Other Costs (2015 US$) | ||
| Outpatient care, per year, without ART (non-intervention) | $278 | RCT |
| Hospitalization costs, per year | $464 | [51] |
| First-line ART, monthly | $13 | [52] |
| Second-line ART, monthly | $28 | [52] |
| Viral load test | $35 | [53] |
| CD4+ count test (non-intervention) | $11 | RCT |
Abbreviations: STI, Sexually transmitted infection; CSW, Commercial sex worker; SMS, text messaging; BCPP, Basic care and prevention package
Model overview
The simulation is composed of two modules. The first module is a Monte Carlo microsimulation of HIV progression that follows a cohort of HIV-positive individuals and predicts time until ART failure, accumulation of resistance mutations, and patient survival. Individuals progress to AIDS and AIDS-related deaths at varying rates depending on whether they adhere with ART and/or develop resistance to ART, based on viral load suppression and CD4+ cell count trajectory. This progression module provides data to inform the second module, a transmission model. This process is described in detail in the Supplementary Material.
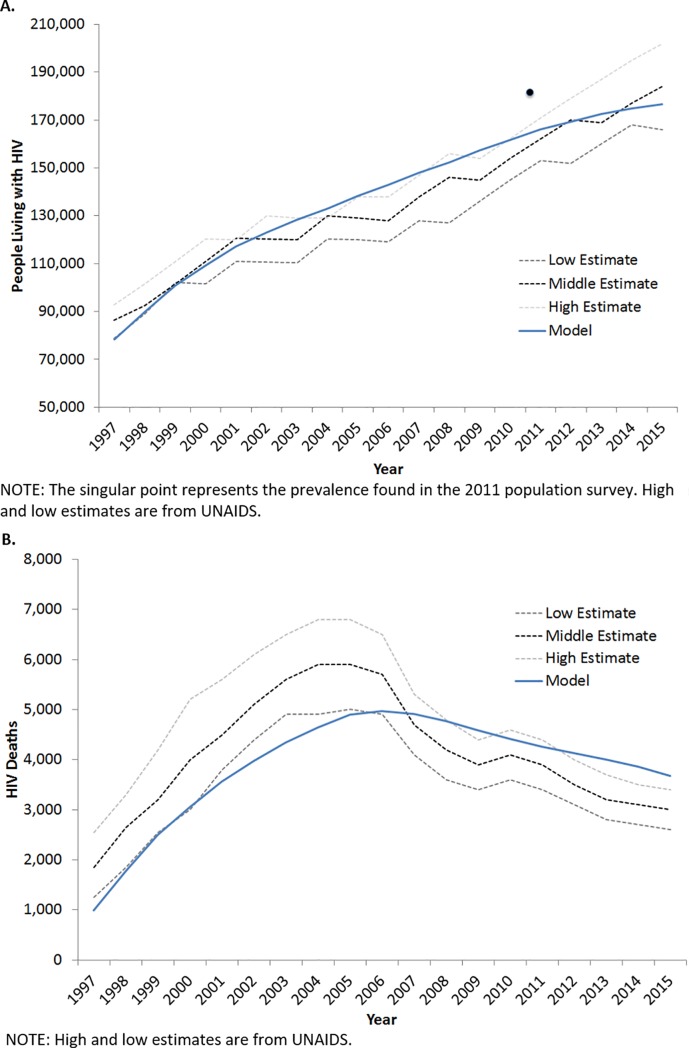
In the second module, the transmission of HIV through the Swaziland population is predicted by a compartmental model. In the transmission module segments of a hypothetical population can become HIV infected, have their infection detected, and access treatment, which can modify their infectivity. Segments of this population can also modify their risk of transmission by exhibiting behaviors including ART adherence, multiple sexual partnerships, failing to use condoms, and having STIs. For example, an intervention may lead to improved ART adherence, which lowers viral load and extends life expectancy in the progression module. The lowered viral load then decreases the risk of transmitting HIV in the transmission module. Transmission model compartments are stratified by age, sexual activity level, excessive alcohol use, HIV status, and if infected, viral load, CD4+ cell count, and ART resistance pattern. Model calibration did not prioritize individual parameters, but sought to minimize the least squares across the parameters as a whole. The design of the simulation, as well as its calibration and validation, is described in more detail in the Supplementary Material and elsewhere.[28] We used the calibrated simulation to evaluate the impact and value of the Link4Health strategy in Swaziland. The simulation was calibrated to Swaziland epidemiological data with the goal of replicating trends in Swaziland HIV prevalence, incidence, deaths, and PLWH from 1997 to 2015 (Fig 1).[41, 54, 55] Therefore, model inputs, such as HIV prevalence, reflect 1997 HIV data representing the start of the calibration period. The model inputs and the intervention effects are described in more detail in Table 1.
Fig 1.
Calibration (A) Number of persons living with HIV, (B) Number of HIV Deaths. A. NOTE: The singular point represents the prevalence found in the 2011 population survey. High and low estimates are from UNAIDS. B.NOTE: High and low estimates are from UNAIDS.
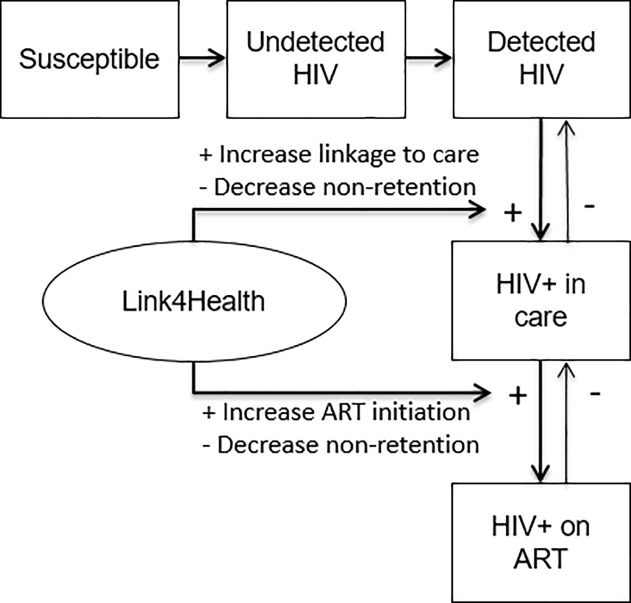
The Link4Health strategy was represented in the simulation by a specific set of HIV transmission “pathways” through which it could exert an effect, along with the corresponding target population (e.g. all HIV-positive adults), and an estimated cost per person per year. The effect of the Link4Health strategy (RR 1.48 for linkage to and retention in care) was represented in the transmission model as a multiplier that accelerated pathways for linkage to care and enhanced retention in treatment, in accord with the observed effect size in the study (Fig 2). The effect on linkage and retention was applied to current HIV patients and new HIV diagnoses continuously while the strategy was active. Link4Health also impacts QALYs gained by increasing linkage to and retention in care. The model applied the viral load decrement that is expected with care retention versus non-retention to influence that person’s HIV course (and, therefore, that person’s QALYs), as well as that person’s likelihood of transmitting HIV (and, therefore, other persons’ QALYs). We conservatively assumed that effects only persisted while the strategy was continued.
Fig 2. Link4Health impact on model pathways.
Outcomes measured included total quality-adjusted life years (QALYs), incremental cost effectiveness ratios (ICERs), number and proportion of new HIV infections prevented and incremental cost per infection averted. Incremental outcomes compared standard of care to standard of care plus the Link4Health intervention. Link4Health cost data was collected prospectively at the time of the trial and represent actual in-trial costs for standard of care and the Link4Health intervention, including the cost of training staff implementing the Link4Health intervention (Table 2). Uncertainty ranges around trial costs were unavailable as all study sites were Ministry of Health (MoH) health facilities with MoH funded staff with defined salaries, and all lab testing were done on a pre-determined schedule based on national guidelines and performed either at the facility or the national laboratory. Consequently, there was little to no variation in treatment costs across study sites. Research-specific costs, such as material development, were not included in the analysis. Non-trial specific costs, including treatment and hospitalization costs were derived from the literature (Table 1). Trial costs were converted from Swazi lilangeni into US dollars and along with cost data collected from the literature were converted into 2015 US dollars using the consumer price index.[56] Costs and effects were discounted at 3%, our time horizon was 20 years, and costs were assessed from a health sector perspective using 2015 US dollars. Other than specifying a finite time horizon, all other aspects of the cost-effectiveness analysis were conducted in line with recommendations by the Panel on Cost-Effectiveness in Health and Medicine.[57] We chose a 20-year rather than infinite time horizon because we found that it was the longest time horizon viewed as credible by stakeholders. A population of 1,098,575 was simulated representing the population of Swaziland at the start of the calibration period in 1997.
Table 2. In trial costs per patient and component descriptions.
| Item | Step targeted in HIV care continuum | SOC | Link4Health | |||
|---|---|---|---|---|---|---|
| Component Description and Cost Assumptions | Cost per patient | Component Description and Cost Assumptions | Cost per patient | |||
| Point-of-care CD4+ count testing | Linkage, ART initiation | • Standard CD4+ test after initial HIV diagnosis • Turnaround time approximately 2 weeks • 1 additional clinic visit required to return lab results to patient (15 min staff time of nurse) |
$11.40 | • Point-of-care CD4 assays at the HIV testing site at the time of HIV testing • Turnaround time immediate • Accelerated ART initiation for patients with point-of-care CD4+ count ≤ 350 cells/mm3 within 1 week from testing • On site CD4+ test. No staff time for duration of test processing included as routine counseling occurs during processing time; testing supplies; 5 mins for blood draw |
$25.80 | |
| Outpatient care | $278 | $324 | ||||
| Outpatient visit | - | Average cost for standard appointment for ART patients and pre-ART patients, not including treatment | $266.50 | Average cost for standard appointment for ART patients and pre-ART patients, not including treatment | $266.50 | |
| Point-of-care CD4+ count testing | Linkage, ART initiation | • Standard CD4+ test after initial HIV diagnosis • Turnaround time approximately 2 weeks • 1 additional clinic visit required to return lab results to patient (15 min staff time of nurse) |
$11.40 | • Point-of-care CD4 assays at the HIV testing site at the time of HIV testing • Turnaround time immediate • Accelerated ART initiation for patients with point-of-care CD4+ count ≤ 350 cells/mm3 within 1 week from testing • On site CD4+ test. No staff time for duration of test processing included as routine counseling occurs during processing time; testing supplies; 5 mins for blood draw |
$25.80 | |
| Cell phone visit reminders | Linkage, retention | - | - | • SMS visit reminders 3 days prior to each scheduled visit • SMS reminder within 7 days after a missed visit |
$0.90 | |
| Care and Prevention Bags | Retention | - | - | • A health education package every 3 mo. at visits. Included condoms, soap, cotrimoxazole, a pill box, and pictorial education about use of materials and HIV Includes training, materials, staff time |
$2.01 | |
| Financial incentives | Linkage, retention | - | - | • Mobile phone credit for those linked to care within 1 month and those completing HIV care clinic visits at 6 and 12 mo. of HIV testing • Mobile phone credit, staff time |
$29.14 | |
Abbreviations: ART, antiretroviral therapy; SMS, short message service
Link4Health intervention
The Link4Health study was a cluster randomized controlled trial performed from 2013 to 2015 in Swaziland that compared standard of care (N = 1,101) to the Link4Health combination strategy plus standard of care (N = 1,096).[26] As noted above, the Link4Health strategy incorporated multiple evidence-based structural, biomedical, and behavioral interventions to improve linkage to and retention in care among adults with HIV in Swaziland. In addition to standard of care, the five interventions combined as package in the Link4Health strategy included: 1) Point-of-care CD4+ count testing. 2) Accelerated ART initiation for eligible participants (CD4+ count ≤ 350 cells/mm3 or WHO Stage III/VI) to enable ART initiation within 1 week of diagnosis. 3) Mobile phone appointment reminders. 4) Basic care and prevention package including commodities and informational materials. 5) Non-cash financial incentive for who linked to care within 1 month of HIV testing and those who completed HIV care clinic visits at 6 and 12 months after HIV testing (Table 2). Swazi decision makers were involved at each step of the Link4Health trial and cost-effectiveness analysis and provided guidance to ensure the Link4Health strategy and its analyses were relevant to the Swazi HIV program goals.
Cost-effectiveness analysis
As a base case analysis we conducted simulations where the Link4Health strategy was activated and calculated the health benefits, costs, and cost-effectiveness ratios of each over the twenty year time horizon. These simulations were compared to a scenario where no additional interventions were implemented. As a sensitivity analysis we varied both intervention efficacy and cost independently across plausible ranges and evaluated their impact on cost-effectiveness. Plausible ranges were determined using trial 95% confidence intervals for effectiveness. It was technically infeasible to do a probabilistic sensitivity analysis as the simulation involves information exchange between a compartmental model and a microsimulation and the run times would be prohibitively long. Between 2013 and 2018 the economic discount rate established by the Central Bank of Swaziland has ranged from 5% to 7.25%.[58] The economic discount rate has been suggested as a surrogate for the social discount rate in developing countries,[59] therefore to encapsulate alternate discount rates that are relevant to Swazi decision making, we also performed sensitivity analyses ranging the discount rate from 5 to 8%. Additionally, in line with evolving ART initiation recommendations, we performed a secondary analysis to simulate the effectiveness of the strategy under the scenario of universal ART adoption, thus eliminating CD4+ testing costs and starting all HIV-positive individuals on ART immediately. We then simulated the Link4Health strategy and calculated the ICERs of the intervention. ICERs measure the additive benefit of each strategy compared with its next best alternative, and interpret this benefit together with its additive cost. A cost per QALY gained value less than three times the per capita GPD (~$9,840) was considered likely to have favorable cost effectiveness, and values equivalent to the per capita GDP ($3,280) were considered favorably cost effective.[60]
Results
Base case outcomes
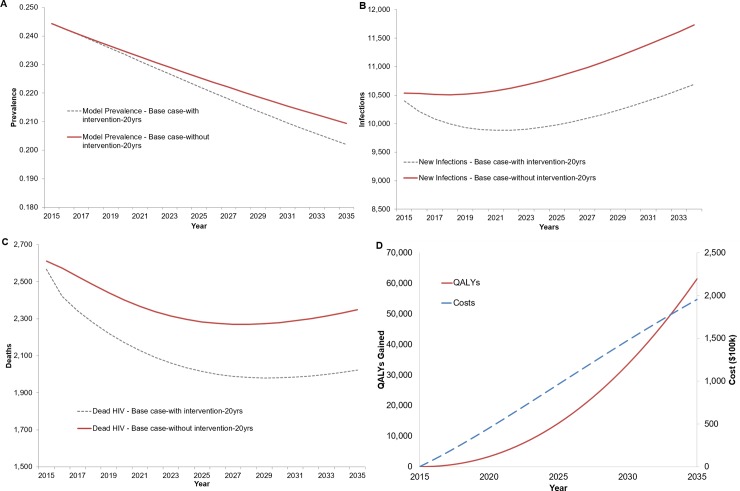
In the base case analysis, the Link4Health strategy reduced the number of new HIV infections over 20 years by 11,059 (6.5%) for total of 157,961 versus 169,019 new infections in Swaziland (Fig 3A) and the HIV prevalence in adults decreased by 0.7% from 20.9% to 20.2% (Fig 3B). The number of HIV-related deaths over 20 years was reduced by 5,313 from 49,582 to 44,270 deaths (Fig 3C).
Fig 3.
Undiscounted change in (A) HIV Prevalence, (B) Number of new infections, (C) Number of HIV-related Deaths, and (D) Undiscounted cost and undiscounted QALYs gained.
Cost effectiveness
When implemented using a health sector perspective, the Link4Health strategy resulted in a total additional cost of $195,700,677 (Fig 2D) and a total discounted additional cost of $147,197,723 over 20 years. Over 20 years the discounted cost per HIV infection prevented was $13,310. Over a 20-year time horizon, the discounted cost per QALY gained was $3,560. Using time horizons of 10 years and 5 years rather than 20 years increased the discounted incremental cost-effectiveness ratio of the Link4Health strategy to $7,195/QALY and $14,122/QALY, respectively, (Table 3) as the costs were mostly borne early whereas the benefits (lengthened life and reduced transmission) mostly occurred later. The discounted cost-effectiveness of Link4Health strategy over 20 years at the highest and lowest range of the 95% confidence interval of intervention effectiveness was $5,572/QALY and $2,911/QALY, respectively.
Table 3. Cost-effectiveness by time horizon.
| Total Costs (Discounted) | Total Discounted QALYs | Cost Change | QALYS Gained (Discounted) | ICER ($/QALY) | |
|---|---|---|---|---|---|
| 20 Yr. Horizon | |||||
| Standard Care | $1,263,589,463 | 19,314,636 | - | - | - |
| Link4Health | $1,410,787,186 | 19,355,978 | $147,197,723 | 38,597 | $3,919 |
| 10 Yr. Horizon | |||||
| Standard Care | $711,420,043 | 10,529,352 | - | - | - |
| Link4Health | $794,361,248 | 10,540,879 | $82,941,205 | 10,904 | $7,686 |
| 5 Yr. Horizon | |||||
| Standard Care | $379,390,695 | 5,540,162 | - | - | - |
| Link4Health | $421,639,679 | 5,543,153 | $42,248,984 | 2,894 | $14,626 |
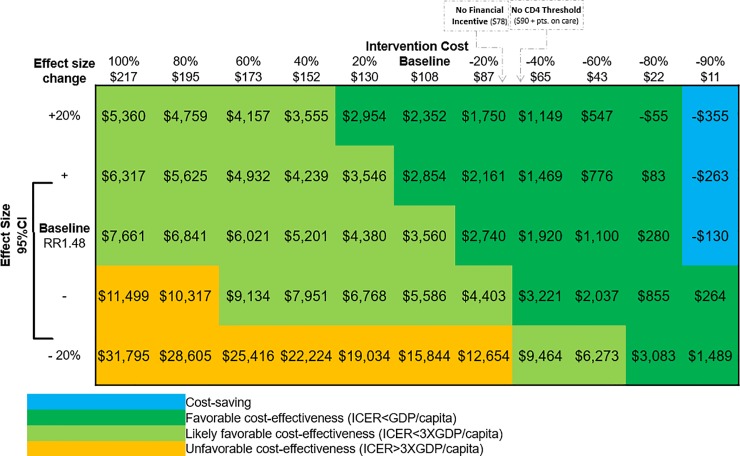
Sensitivity analyses
In one-way and multi-way sensitivity analyses, results regarding costs and benefits were highly stable, with the Link4Health strategy remaining cost effective and improving health across a range of assumptions. In sensitivity analyses to determine the threshold at which Link4Health is no longer cost-effective, reducing the per-patient cost of the Link4Health strategy by 7% (-$8) from baseline ($108) decreased the ICER to make the intervention very cost effective ($/QALY<GPD/Capita) (Fig 4). Reducing the cost by 87% (-$94) made the Link4Health strategy cost-saving (Fig 4). Increasing the strategy cost by 154% (+$166) made the strategy not cost-effective ($/QALY>3xGPD/Capita). The model results were more sensitive to programmatic costs than the cost of care and treatment. Similarly, decreasing strategy effectiveness by 15% decreased new infections averted to 872 infections and HIV deaths to 3,277, decreased discounted QALYs gained to 19,014 QALYs, and made the strategy no longer cost-effective. Increasing the strategy effect size by 4% increased infections averted to 12,603 infections and HIV deaths to 6,055, increased discounted QALYs gained to 44,751 QALYs, and made the strategy very cost-effective (Fig 4). Universal ART decreased the discounted ICER to $2,211/QALY. Increasing the discount rate to 5% and 8% resulted in an ICER of $3,832/QALY and $4,286/QALY, respectively.
Fig 4. Discounted cost-effectiveness sensitivity analysis.
Discussion
We provide projections of the impact and cost-effectiveness of a scale up of a combination strategy of multiple interventions targeting barriers at various HIV continuum steps for linkage to and retention in care among HIV-positive individuals in Swaziland. Few studies have evaluated a combination approach that includes multiple interventions bundled into a coherent strategy that would target numerous barriers along the HIV care continuum,[23, 25, 27, 61] and the cost-effectiveness of such an approach has not previously been evaluated.[62] Our analyses suggest that from a health sector perspective, a scale-up of the Link4Health combination strategy is likely to be cost-effective. Our findings were robust over a range of assumptions regarding cost and effectiveness and the strategy was found to remain cost-effective at shorter time horizons such as 10 years. Examining a range of time horizons demonstrated the potential to underestimate the cost-effectiveness of HIV interventions when only considering shorter horizons due to the frequent longer-term health and cost implications of diseases like HIV/AIDS.
The Link4Health study represents the first study that evaluated multiple interventions packaged in one strategy on both linkage to care and retention in care. Previous studies have found individual elements that increase linkage and retention in care to be cost-effective in other low- and middle- income nations in Africa.[63–65] The cost-effectiveness of the Link4Health strategy falls within the range observed in these single intervention studies, being more cost effective than point of care testing alone ($4,468/DALY),[63] but not quite as cost effective as text messaging alone ($1,024/QALY [adjusted to USD2015]) if DALYs are considered a surrogate for QALYs.[65] This demonstrates the potential benefits of a multicomponent strategy for achieving a greater and more cost-effective impact on the care continuum than implementing standalone interventions. With the potential to further decrease the Link4Health strategy costs, the multicomponent strategy may prove to be the dominant choice for HIV care continuum interventions. A decline in HIV prevalence is projected in Swaziland, even with standard of care, and Link4Health magnifies this decline, which is in large part attributable to the increasing population of Swaziland and low incidence of HIV in new births. Prior to the Link4Health study, there was substantial reluctance to rapidly initiate ART. The Link4Health study, however, has already had a strong influence on the adoption of rapid initiation of ART by the Swazi National AIDs Control Program, thus indicating the interest from stakeholders in incorporating Link4Health-like strategies into the Swazi HIV program. Despite interest in the program and its cost effectiveness as a care continuum intervention, a wide-scale implementation of the Link4health strategy may not be feasible until Swaziland has achieved universal ART coverage at the CD4+ count ≤ 500 cells/mm3 threshold. While Swaziland has achieved universal ART coverage under the 2010 WHO guidelines (CD4+ count ≤ 350 cells/mm3), it has not achieved universal ART coverage at the CD4+ count ≤ 500 cells/mm3 threshold.[66] Therefore, HIV funds may not be available as they are diverted to the more cost effective implementation of universal ART coverage at the CD4+ count ≤ 500 cells/mm3 threshold ($245 to $1,746/DALY [adjusted to USD2015]).[67]
The largest portion of program costs was incurred through ART treatment costs, followed by outpatient care, and the cost of CD4+ count testing. Therefore, there is potential to reduce the cost of the HIV treatment program through reductions in the cost of outpatient care and CD4+ count testing as HIV programs shift to differentiated models of care in which stable HIV patients on ART may decrease the number and or frequency of clinic visits and universal ART initiation replacing the need for CD4+ count testing. For example, in some resource-limited settings, patients who achieve viral suppression and are clinically stable receive ongoing HIV care, including medications, in community adherence clubs, which decrease the number of clinic visits.[68, 69] The 2015 Swaziland HIV strategy supports the development of HIV support groups, however universal test and treat, while under consideration, is not part of current HIV guidelines.[66] Further reductions in program costs are likely feasible because, while financial incentives have shown promise in increasing HIV treatment in some interventions,[70] a comparable level of effectiveness to that in the Link4Health study was found in a trial performed in Mozambique of a similar intervention that did not include the financial incentive component.[71] Removing the financial incentives from the Link4Health strategy has the potential to decrease the strategy cost by nearly 30% and result in an even more favorable cost-effectiveness at <1 times the GDP. The adoption of “treat-all” WHO recommendations in Swaziland may eliminate the need for CD4+ count testing, reducing programmatic costs by nearly 25% and improving potential cost-effectiveness to $2,211/QALY (Fig 4).[72]
Our analysis has a number of limitations. First, because of the compartmental nature of the transmission model, the effect on retention in care was represented through improvement of ART adherence and does not account for the other potential benefits gained such as access to other clinical assessments and health counselling. As a result, our analyses may underestimate the total health benefits generated by the Link4Health strategy. Second, the analysis included the same strategy costs for all individuals enrolled in the study, including those that did not ultimately receive the full intervention. This, however, likely overestimates the total cost of implementation as individuals not in HIV care would not incur the full strategy cost. Similarly, we assumed that HIV care visit costs would be the same for patients both on ART and those not on ART. In practice, however, these costs may differ due to factors such as the professional level of the healthcare worker. These differences in visit costs, however, are likely to be negligible when the cost ART treatment is considered. Third, not all model inputs were available for a Swazi-specific setting, which may impact cost-effectiveness. During model validation, the model was permitted to fit some indicators better than others in order to avoid overfitting to a particular data source. The robust cost-effectiveness results across sensitivity analyses, however, indicate that minor variations in these inputs are unlikely to substantially affect the results. Fourth, the Link4Health strategy was carried out in a population that has high prevalence of HIV compared to other countries in the world. Consequently, our results may not be applicable to other populations. Further testing is needed to investigate the Link4Health strategy’s effectiveness in populations outside of high HIV prevalence countries and contexts. Fifth, the nature of the Link4Health trial, which examined the implementation of a package of interventions together and did not isolate the impact of each component separately, made this analysis unable to estimate how each component individually affects the cost-effectiveness of the combined strategy. Similarly, due to the model structure it is not technically feasible to separate how annuals costs will accrue for each relevant budget holder. Finally, it is worth noting that the use of a cost-effectiveness threshold of <3 x per capita GDP, while transparent and easily applied, is insufficient to determine whether an intervention should be implemented. The more relevant cost-effectiveness threshold would be the incremental cost-effectiveness ratio of simultaneously resource constrained interventions, as the health gained from any additional funds allocated towards on Link4Health would likely exceed the health lost from removing funds from other interventions.
Conclusion
The scale-up of the Link4Health strategy would substantially reduce HIV-related deaths and avert new HIV infections. With a favorable value over a 10 year timeframe or longer, using a threshold of <3 x per capita GDP, the Link4Health strategy could be a cost-effective strategy for confronting the HIV epidemic in Swaziland and other low-income countries with a generalized HIV epidemic. Efforts to strategically reduce strategy costs could lead to Link4Health being a highly cost-effective HIV intervention.
Supporting information
(DOCX)
Acknowledgments
Human subjects: No human subjects were involved in this research project. Secondary data only was used in the performance of this cost effectiveness analysis and all data were fully anonymized prior to accessing them for this study. The NYU School of Medicine IRB determined the study to be non-human subjects and did not require informed consent. The original Link4Health study was performed separately and was approved by the Columbia University IRB.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This manuscript was funded by NIH Award Number: R01AI100059. The funder had no role in the in the writing of the manuscript or the decision to submit it for publication.
References
- 1.Walker DG, Hutubessy R, Beutels P. WHO Guide for standardisation of economic evaluations of immunization programmes. Vaccine. 2010;28(11):2356–9. 10.1016/j.vaccine.2009.06.035 [DOI] [PubMed] [Google Scholar]
- 2.Bicego GT, Nkambule R, Peterson I, Reed J, Donnell D, Ginindza H, et al. Recent patterns in population-based HIV prevalence in Swaziland. PLoS One. 2013;8(10):e77101 Epub 2013/10/22. 10.1371/journal.pone.0077101 ; PubMed Central PMCID: PMCPMC3797108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Justman J, Reed JB, Bicego G, Donnell D, Li K, Bock N, et al. Swaziland HIV Incidence Measurement Survey (SHIMS): a prospective national cohort study. The Lancet HIV. 10.1016/S2352-3018(16)30190-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control. CDC in Swaziland: Factsheet 2013 [january 12, 2017]. Available from: https://www.cdc.gov/globalhealth/countries/swaziland/pdf/swaziland_2013.pdf.
- 5.Kingdom of Swaziland Ministry of Health. Annual HIV Programs Report, 2015. In: Monitoring & Evaluation Unit: Strategic Information Department, editor. 2015.
- 6.Auld AF, Kamiru H, Azih C, Baughman AL, Nuwagaba-Biribonwoha H, Ehrenkranz P, et al. Implementation and Operational Research: Evaluation of Swaziland's Hub-and-Spoke Model for Decentralizing Access to Antiretroviral Therapy Services. J Acquir Immune Defic Syndr. 2015;69(1):e1–12. Epub 2015/05/06. 10.1097/QAI.0000000000000547 . [DOI] [PubMed] [Google Scholar]
- 7.Auld AF, Agolory SG, Shiraishi RW, Wabwire-Mangen F, Kwesigabo G, Mulenga M, et al. Antiretroviral therapy enrollment characteristics and outcomes among HIV-infected adolescents and young adults compared with older adults—seven African countries, 2004–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1097–103. Epub 2014/11/27. . [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Vital signs: HIV prevention through care and treatment—United States. MMWR Morb Mortal Wkly Rep. 2011;60(47):1618 [PubMed] [Google Scholar]
- 9.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. Epub 2011/03/04. doi: ciq243 [pii] 10.1093/cid/ciq243 ; PubMed Central PMCID: PMC3106261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. Epub 2011/07/20. 10.1056/NEJMoa1105243 ; PubMed Central PMCID: PMCPmc3200068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. Aids. 2012;26(14):1735–8. Epub 2012/05/23. 10.1097/QAD.0b013e328355d67b . [DOI] [PubMed] [Google Scholar]
- 12.Fairall LR, Bachmann MO, Louwagie GM, van Vuuren C, Chikobvu P, Steyn D, et al. Effectiveness of antiretroviral treatment in a South African program: a cohort study. Arch Intern Med. 2008;168(1):86–93. Epub 2008/01/16. 10.1001/archinternmed.2007.10 . [DOI] [PubMed] [Google Scholar]
- 13.McGrath N, Glynn JR, Saul J, Kranzer K, Jahn A, Mwaungulu F, et al. What happens to ART-eligible patients who do not start ART? Dropout between screening and ART initiation: a cohort study in Karonga, Malawi. BMC Public Health. 2010;10:601 Epub 2010/10/14. 10.1186/1471-2458-10-601 ; PubMed Central PMCID: PMCPMC2964626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawn SD, Wood R. How can earlier entry of patients into antiretroviral programs in low-income countries be promoted? Clin Infect Dis. 2006;42(3):431–2; author reply 2–3. Epub 2006/01/05. 10.1086/499527 . [DOI] [PubMed] [Google Scholar]
- 15.Bisson GP, Gaolathe T, Gross R, Rollins C, Bellamy S, Mogorosi M, et al. Overestimates of survival after HAART: implications for global scale-up efforts. PLoS One. 2008;3(3):e1725 Epub 2008/03/06. 10.1371/journal.pone.0001725 ; PubMed Central PMCID: PMCPMC2254493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brinkhof MW, Pujades-Rodriguez M, Egger M. Mortality of patients lost to follow-up in antiretroviral treatment programmes in resource-limited settings: systematic review and meta-analysis. PLoS One. 2009;4(6):e5790 10.1371/journal.pone.0005790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalal RP, Macphail C, Mqhayi M, Wing J, Feldman C, Chersich MF, et al. Characteristics and outcomes of adult patients lost to follow-up at an antiretroviral treatment clinic in johannesburg, South Africa. J Acquir Immune Defic Syndr. 2008;47(1):101–7. Epub 2007/11/01. 10.1097/QAI.0b013e31815b833a . [DOI] [PubMed] [Google Scholar]
- 18.Krebs DW, Chi BH, Mulenga Y, Morris M, Cantrell RA, Mulenga L, et al. Community-based follow-up for late patients enrolled in a district-wide programme for antiretroviral therapy in Lusaka, Zambia. AIDS Care. 2008;20(3):311–7. Epub 2008/03/21. 10.1080/09540120701594776 . [DOI] [PubMed] [Google Scholar]
- 19.Maskew M, MacPhail P, Menezes C, Rubel D. Lost to follow up: contributing factors and challenges in South African patients on antiretroviral therapy. S Afr Med J. 2007;97(9):853–7. Epub 2007/11/07. . [PubMed] [Google Scholar]
- 20.Yu JK, Chen SC, Wang KY, Chang CS, Makombe SD, Schouten EJ, et al. True outcomes for patients on antiretroviral therapy who are "lost to follow-up" in Malawi. Bull World Health Organ. 2007;85(7):550–4. Epub 2007/09/05. 10.2471/BLT.06.037739 ; PubMed Central PMCID: PMCPMC2636367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox MP, Rosen S, Geldsetzer P, Barnighausen T, Negussie E, Beanland R. Interventions to improve the rate or timing of initiation of antiretroviral therapy for HIV in sub-Saharan Africa: meta-analyses of effectiveness. J Int AIDS Soc. 2016;19(1):20888 Epub 2016/08/11. 10.7448/IAS.19.1.20888 ; PubMed Central PMCID: PMCPMC4978859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Govindasamy D, Meghij J, Kebede Negussi E, Clare Baggaley R, Ford N, Kranzer K. Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low- and middle-income settings—a systematic review. J Int AIDS Soc. 2014;17:19032 Epub 2014/08/07. 10.7448/IAS.17.1.19032 ; PubMed Central PMCID: PMCPMC4122816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amanyire G, Semitala FC, Namusobya J, Katuramu R, Kampiire L, Wallenta J, et al. Effects of a multicomponent intervention to streamline initiation of antiretroviral therapy in Africa: a stepped-wedge cluster-randomised trial. Lancet HIV. 2016;3(11):e539–e48. Epub 2016/10/30. 10.1016/S2352-3018(16)30090-X ; PubMed Central PMCID: PMCPMC5408866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koenig SP, Dorvil N, Devieux JG, Hedt-Gauthier BL, Riviere C, Faustin M, et al. Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial. PLoS Med. 2017;14(7):e1002357 Epub 2017/07/26. 10.1371/journal.pmed.1002357 ; PubMed Central PMCID: PMCPMC5526526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elul B, Lahuerta M, Abacassamo F, Lamb MR, Ahoua L, McNairy ML, et al. A combination strategy for enhancing linkage to and retention in HIV care among adults newly diagnosed with HIV in Mozambique: study protocol for a site-randomized implementation science study. BMC Infect Dis. 2014;14:549 Epub 2014/10/15. 10.1186/s12879-014-0549-5 ; PubMed Central PMCID: PMCPMC4210581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McNairy ML, Lamb MR, Gachuhi AB, Nuwagaba-Biribonwoha H, Burke S, Mazibuko S, et al. Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial. PLoS Med. 2017;14(11):e1002420 Epub 2017/11/08. 10.1371/journal.pmed.1002420 ; PubMed Central PMCID: PMCPMC5675376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNairy ML, Gachuhi AB, Lamb MR, Nuwagaba-Biribonwoha H, Burke S, Ehrenkranz P, et al. The Link4Health study to evaluate the effectiveness of a combination intervention strategy for linkage to and retention in HIV care in Swaziland: protocol for a cluster randomized trial. Implement Sci. 2015;10:101 Epub 2015/07/21. 10.1186/s13012-015-0291-4 ; PubMed Central PMCID: PMCPMC4506770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braithwaite RS, Nucifora KA, Yiannoutsos CT, Musick B, Kimaiyo S, Diero L, et al. Alternative antiretroviral monitoring strategies for HIV-infected patients in east Africa: opportunities to save more lives? J Int AIDS Soc. 2011;14:38 Epub 2011/08/02. 10.1186/1758-2652-14-38 ; PubMed Central PMCID: PMCPmc3163507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Organization WH. Swaziland, Alcohol Consumption: Levels and Patterns 2014 [January 9, 2017]. Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/swz.pdf?ua=1.
- 30.Braithwaite RS, Nucifora KA, Kessler J, Toohey C, Mentor SM, Uhler LM, et al. Impact of Interventions Targeting Unhealthy Alcohol Use in Kenya on HIV Transmission and AIDS-Related Deaths. Alcohol Clin Exp Res. 2014;38(4):1059–67. Epub 2014/01/17. 10.1111/acer.12332 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kapiga SH, Sam NE, Mlay J, Aboud S, Ballard RC, Shao JF, et al. The epidemiology of HIV-1 infection in northern Tanzania: results from a community-based study. AIDS Care. 2006;18(4):379–87. Epub 2006/07/01. 10.1080/09540120500465012 . [DOI] [PubMed] [Google Scholar]
- 32.Ao TT, Sam NE, Masenga EJ, Seage GR 3rd, Kapiga SH. Human immunodeficiency virus type 1 among bar and hotel workers in northern Tanzania: the role of alcohol, sexual behavior, and herpes simplex virus type 2. Sex Transm Dis. 2006;33(3):163–9. 10.1097/01.olq.0000187204.57006.b3 [DOI] [PubMed] [Google Scholar]
- 33.Mbizvo MT, Machekano R, McFarland W, Ray S, Bassett M, Latif A, et al. HIV seroincidence and correlates of seroconversion in a cohort of male factory workers in Harare, Zimbabwe. Aids. 1996;10(8):895–901. Epub 1996/07/01. . [DOI] [PubMed] [Google Scholar]
- 34.Quigley M, Munguti K, Grosskurth H, Todd J, Mosha F, Senkoro K, et al. Sexual behaviour patterns and other risk factors for HIV infection in rural Tanzania: a case-control study. Aids. 1997;11(2):237–48. Epub 1997/02/01. . [DOI] [PubMed] [Google Scholar]
- 35.Mishra V, Bignami-Van Assche S. Concurrent Sexual Partnerships and HIV Infection: Evidence from National Population-Based Surveys. DHS Working Papers No. 62. 2009. [Google Scholar]
- 36.Volle J, Foreit J, Letsatsi T, Tan A. A baseline survey of multiple and concurrent sexual partnerships among Basotho men in Lesotho Washington (DC): C-Change/Academy for Educational Development; 2009. [Google Scholar]
- 37.UNAIDS. Global Report-UNAIDS report on the global AIDS epidemic 2013. 2013 [May 5, 2014]. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf.
- 38.Vandepitte J, Lyerla R, Dallabetta G, Crabbe F, Alary M, Buve A. Estimates of the number of female sex workers in different regions of the world. Sex Transm Infect. 2006;82 Suppl 3:iii18–25. Epub 2006/06/01. 10.1136/sti.2006.020081 ; PubMed Central PMCID: PMCPMC2576726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.UNAIDS. Swaziland Global AIDS Response Progress Reporting 2014 2014 [January 10, 2017]. Available from: http://www.unaids.org/sites/default/files/country/documents/SWZ_narrative_report_2014.pdf.
- 40.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-Analysis of High-Risk Sexual Behavior in Persons Aware and Unaware They are Infected With HIV in the United States: Implications for HIV Prevention Programs. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2005;39(4):446–53. PubMed PMID: 00126334-200508010-00013. [DOI] [PubMed] [Google Scholar]
- 41.UNAIDS. AIDSinfo 2016 [January 10, 2017]. Available from: http://aidsinfo.unaids.org/.
- 42.Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. Aids. 2009;23(11):1397–404. Epub 2009/04/22. 10.1097/QAD.0b013e32832b7dca . [DOI] [PubMed] [Google Scholar]
- 43.Boily MC, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. The Lancet infectious diseases. 2009;9(2):118–29. 10.1016/S1473-3099(09)70021-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siegfried N, Muller M, Deeks JJ, Volmink J. Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane Database Syst Rev. 2009;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weller SC D-BK. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database of Systematic Reviews. 2002;(1). [DOI] [PubMed] [Google Scholar]
- 46.World Health Organization. Global Prevalence and Incidence of Selected Curable Sexually Transmitted Infections Overview and Estimates. Geneva: 2001.
- 47.Jobanputra K, Parker LA, Azih C, Okello V, Maphalala G, Kershberger B, et al. Factors associated with virological failure and suppression after enhanced adherence counselling, in children, adolescents and adults on antiretroviral therapy for HIV in Swaziland. PLoS One. 2015;10(2):e0116144 Epub 2015/02/20. 10.1371/journal.pone.0116144 ; PubMed Central PMCID: PMCPMC4335028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Braithwaite RS, Goulet J, Kudel I, Tsevat J, Justice AC. Quantifying the decrement in utility from perceived side effects of combination antiretroviral therapies in patients with HIV. Value Health. 2008;11(5):975–9. Epub 2008/01/30. 10.1111/j.1524-4733.2007.00315.x ; PubMed Central PMCID: PMC3121315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Louwagie GM, Bachmann MO, Meyer K, Booysen Fle R, Fairall LR, Heunis C. Highly active antiretroviral treatment and health related quality of life in South African adults with human immunodeficiency virus infection: A cross-sectional analytical study. BMC Public Health. 2007;7:244 Epub 2007/09/15. 10.1186/1471-2458-7-244 ; PubMed Central PMCID: PMCPMC2194770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mafirakureva N, Dzingirai B, Postma MJ, van Hulst M, Khoza S. Health-related quality of life in HIV/AIDS patients on antiretroviral therapy at a tertiary care facility in Zimbabwe. AIDS Care. 2016;28(7):904–12. Epub 2016/04/22. 10.1080/09540121.2016.1173639 . [DOI] [PubMed] [Google Scholar]
- 51.Adam T, Evans DB, Murray CJ. Econometric estimation of country-specific hospital costs. Cost Effectiveness and Resource Allocation. 2003;1(1):3 10.1186/1478-7547-1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.World Health Organization. HIV/AIDS: Global Price Reporting Mechnism [January 10, 2017]. Available from: http://apps.who.int/hiv/amds/price/hdd/.
- 53.Jobanputra K, Parker LA, Azih C, Okello V, Maphalala G, Jouquet G, et al. Impact and programmatic implications of routine viral load monitoring in Swaziland. J Acquir Immune Defic Syndr. 2014;67(1):45–51. Epub 2014/05/30. 10.1097/QAI.0000000000000224 ; PubMed Central PMCID: PMCPMC4149657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization. Life tables by country: Swaziland 2017 [August 16, 2017]. Available from: http://apps.who.int/gho/data/?theme=main&vid=61590.
- 55.Justman J, Reed JB, Bicego G, Donnell D, Li K, Bock N, et al. Swaziland HIV Incidence Measurement Survey (SHIMS): a prospective national cohort study. The lancet HIV. 2017;4(2):e83–e92. 10.1016/S2352-3018(16)30190-4 PubMed PMID: PMC5291824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bureau of Labor Statistics. Consumer Price Index Online: United States Department of Labor; 2017 [August 4, 2017]. Available from: https://www.bls.gov/cpi/tables/detailed-reports/home.htm.
- 57.Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316(10):1093–103. Epub 2016/09/14. 10.1001/jama.2016.12195 . [DOI] [PubMed] [Google Scholar]
- 58.Central Bank of eSwatini. Monthly Statistical Releases 2018 [August 16, 2018]. Available from: http://www.centralbank.org.sz/monetarypolicy/statistics/.
- 59.Warusawitharana M. The Social Discount Rate in Developing Countries. FEDS Notes. 2014;Oct. 9.
- 60.World Health Organization. Making choices in health: WHO guide to cost-effectiveness analysis. Geneva: WHO, 2003. [Google Scholar]
- 61.Elul B, Lamb MR, Lahuerta M, Abacassamo F, Ahoua L, Kujawski SA, et al. A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: A cluster-randomized study. PLoS Med. 2017;14(11):e1002433 10.1371/journal.pmed.1002433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harripersaud K, Abrams E, McNary M, Ahmed S, Thirumurthy H, El-Sadr W. Management of HIV/AIDS and Co-Morbidities in Children and Adults: Cost-Effectiveness Considerations in Disease Control Priorities, Third Edition Volume 6, Major Infectious Diseases. Edited by Holmes K.K., Bertozzi S., Bloom B.R., Jha P., and Nugent R. Washington, DC: World Bank; 2017. Available from: http://dcp-3.org/volume/aids-tb-and-malaria/chapter/1/hivaids-and-other-sexually-transmitted-infections. [Google Scholar]
- 63.Heffernan A, Barber E, Thomas R, Fraser C, Pickles M, Cori A. Impact and Cost-Effectiveness of Point-Of-Care CD4 Testing on the HIV Epidemic in South Africa. PLoS One. 2016;11(7):e0158303 Epub 2016/07/09. 10.1371/journal.pone.0158303 ; PubMed Central PMCID: PMCPMC4938542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hyle EP, Jani IV, Lehe J, Su AE, Wood R, Quevedo J, et al. The clinical and economic impact of point-of-care CD4 testing in mozambique and other resource-limited settings: a cost-effectiveness analysis. PLoS Med. 2014;11(9):e1001725 Epub 2014/09/17. 10.1371/journal.pmed.1001725 ; PubMed Central PMCID: PMCPMC4165752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patel AR, Kessler J, Braithwaite RS, Nucifora KA, Thirumurthy H, Zhou Q, et al. Economic evaluation of mobile phone text message interventions to improve adherence to HIV therapy in Kenya. Medicine (Baltimore). 2017;96(7):e6078 Epub 2017/02/17. 10.1097/md.0000000000006078 ; PubMed Central PMCID: PMCPMC5319505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Organization WH. Swaziland Integrated HIV Management Guidelines 2015 [June 18, 2018]. Available from: https://www.infocenter.nercha.org.sz/sites/default/files/Swaziland%20Integrated%20HIV%20Management%20Guidelines_0.pdf.
- 67.Eaton JW, Menzies NA, Stover J, Cambiano V, Chindelevitch L, Cori A, et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a combined analysis of 12 mathematical models. The Lancet Global Health. 2014;2(1):e23–e34. 10.1016/S2214-109X(13)70172-4 [DOI] [PubMed] [Google Scholar]
- 68.Naslund JA, Dionne-Odom J, Junior Destine C, Jogerst KM, Renold Senecharles R, Jean Louis M, et al. Adapting and Implementing a Community Program to Improve Retention in Care among Patients with HIV in Southern Haiti: "Group of 6". AIDS research and treatment. 2014;2014:137545 10.1155/2014/137545 ; PubMed Central PMCID: PMC4274858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grimsrud A, Sharp J, Kalombo C, Bekker LG, Myer L. Implementation of community-based adherence clubs for stable antiretroviral therapy patients in Cape Town, South Africa. J Int AIDS Soc. 2015;18:19984 10.7448/IAS.18.1.19984 ; PubMed Central PMCID: PMC4444752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bassett IV, Wilson D, Taaffe J, Freedberg KA. Financial incentives to improve progression through the HIV treatment cascade. Current opinion in HIV and AIDS. 2015;10(6):451–63. 10.1097/COH.0000000000000196 PubMed PMID: PMC4699403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Elul B, Lamb M, Lahuerta M, F A, L A, S K, et al. A Combination Intervention Strategy for HIV Linkage and Retention in Mozambique. CROI; Seattle, WA2017. [Google Scholar]
- 72.World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV: World Health Organization; 2015. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.