Highlights
-
•
The pathophysiology of the stroke-like episodes of MELAS has not completely been elucidated.
-
•
Here we report a case of stroke-like episodes, successfully treated with levetiracetam.
-
•
Neuronal hyperexcitability can be the underlying mechanism of stroke-like episodes in MELAS.
Keywords: MELAS, Stroke-like episodes, Hyperexcitability, Levetiracetam
Dear Editor,
Mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS) is a mitochondrial disorder characterized by fluctuating encephalopathy, migrainous headache, seizures, and stroke-like episodes. Stroke-like episodes are focal neurological deficits and one of the most common symptoms in MELAS patients, however their pathogenic mechanisms remain unknown. Here we report a case of stroke-like episodes in MELAS with a suggested association with neuronal hyperexcitability, one of the pathogenic theories.
1. Case report
A 53-year-old woman who had been diagnosed at the age of 36 with mitochondrial disease arising from m.3243A>G, suddenly felt walking instability ten days before admission. She complained of headache and writing difficulty from the day before admission. She had a past history of type 1 diabetes, Graves' disease, bilateral sensorineural deafness, end-stage renal failure on hemodialysis, chronic heart failure, coronary heart disease, peripheral artery disease, and hypertension, with a strong family history of m.3243A>G-related mitochondrial diseases.
She was of short stature (height 149.2 cm and weight 32 kg) and her blood pressure was 168/98 mmHg and pulse rate 106/min on admission. No other abnormality was found during a general physical examination. She was alert and her neurological examination showed right hemianopsia, bilateral deafness, and truncal ataxia. Brain computed tomography (CT) revealed calcification in the bilateral basal ganglia and atrophy of the bilateral cerebellar hemisphere. Brain magnetic resonance imaging (MRI) showed hyperintensity in the bilateral occipital lobe on DWI with reduction of the apparent diffusion coefficient (ADC). Cervical and intracranial magnetic resonance angiography (MRA) showed no stenotic lesions.
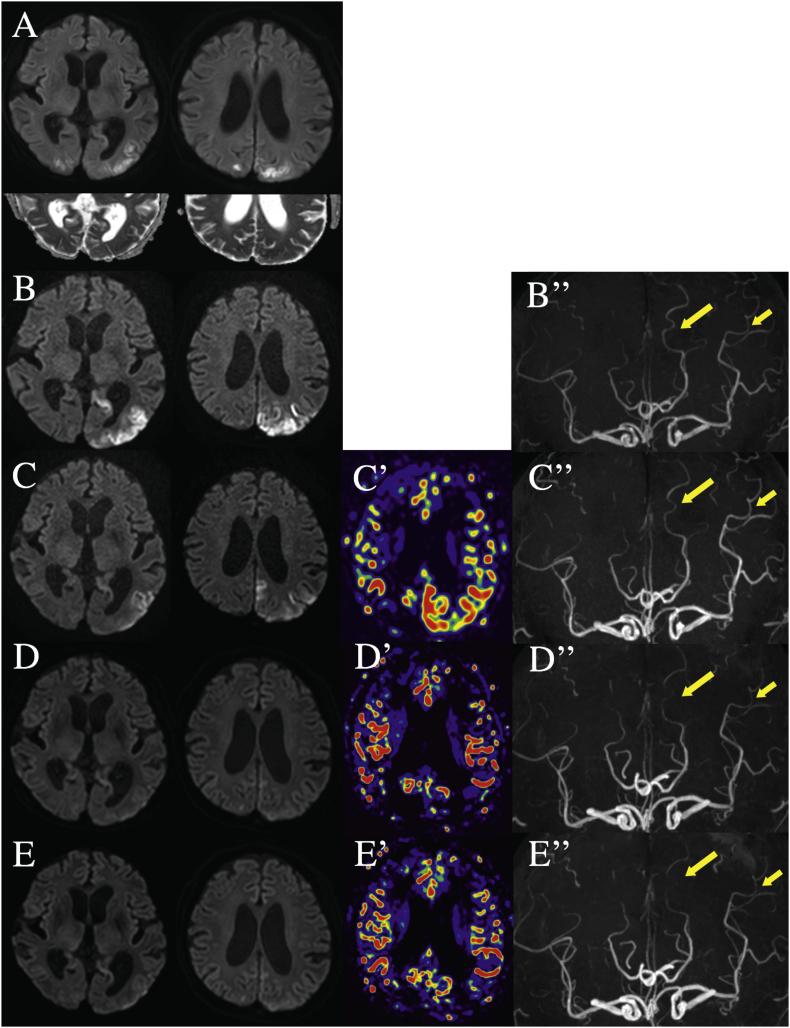
We initiated a continuous infusion of unfractionated heparin with the tentative diagnosis of acute ischemic stroke. However, this did not improve her neurological symptoms, with the DWI-positive and ADC-partial negative lesions expanding to the left parietal lobe beyond the vascular territory on the 3rd hospital day (HD) (Fig. 1A). In addition, because her serum levels of lactic and pyruvic acid were elevated (61.2 mg/dl and 2.6 mg/dl, respectively), we diagnosed her with stroke-like episodes associated with MELAS and started intravenous administration of L-arginine (16 g/day) (for 3 days followed by oral administration), instead of heparin infusion, on the 3rd HD. However, her neurological symptoms deteriorated with the additional development of pure alexia and Gerstmann's syndrome on the 4th HD. Electroencephalogram (EEG) showed an intermittent slow wave of 4–5 Hz predominantly in the left parieto-occipital lobe on the 5th HD. On the 8th HD, the DWI-positive lesions further expanded (Fig. 1B) with hyperperfusion in the left parieto-occipital lobes as evaluated by single photon emission computed tomography (SPECT). Thus, we started the additional administration of LEV (1000 mg/day) on the 10th HD. Her symptoms gradually improved with decreases in lactic and pyruvic acid in both blood and cerebrospinal fluid. The DWI hyperintensities gradually disappeared with normalization of cerebral blood flow in the left parieto-occipital lobes, as assessed by arterial spin labeling (ASL) (Fig. 1C–E, C′–E′). Consistently, the follow-up SPECT showed normo-hypoperfusion in the left parieto-occipital lobes on the 30th HD. The caliber of the left middle cerebral artery (MCA) and the posterior cerebral artery (PCA) gradually normalized on intracranial MRA (Fig. 1B″–E″). Her neurological symptoms gradually improved with mild agraphia, visual abnormality, and truncal ataxia remaining on the 40th HD when she was transferred to a rehabilitation ward.
Fig. 1.
Temporal profile of DWI, ASL, and MRA. DWI-positive lesions continue to expand beyond the major cerebral artery territories with ADC reduction until the 8th HD (A, B). After the administration of LEV on 10th HD, the DWI-positive lesions started to improve (C–E). ASL shows hyperperfusion in the DWI-positive areas (C′). Intracranial MRA suggest dilatation (= increased blood flow) of the left middle and posterior cerebral arteries, compared to those of the right side (B″–C″). The vasodilatation shown on MRA seems to disappear along with the improvement of DWI-positive lesions (D′–E′, D″–E″).
2. Discussion
Here we have reported stroke-like episodes associated with MELAS, which were drastically improved by the administration of LEV.
There are some proposed theories on the development of stroke-like episodes in MELAS, such as the ischemic vascular theory, neuronal metabolic theory, and neuronal hyperexcitability theory. In the ischemic vascular theory, abnormal mitochondria are assumed to accumulate in endothelial cells and smooth muscle, and cause impaired dilated responses of the cerebral vessels, resulting in hypoperfusion and ultimately ischemia [1]. Based on this theory, administration of L-arginine, the substrate of endothelial nitric oxide synthase, is used for vasodilatation in the acute phase of stroke-like episodes in MELAS [2,3]. Although there have been some reports demonstrating the neuroprotective effects of L-arginine [2,3], others suggest that the efficiency of L-arginine depends on sufficient intravenous administration in the early phase (within 2 h) of stroke-like episodes or its efficacy may be restricted [4,5]. Thus, it is possible that the lack of efficacy of L-arginine in the present case may be due to its delayed administration. However, the fact that the DWI-positive areas responsible for the current neurological symptoms were accompanied by hyperperfusion may not always support the ischemic theory, at least in the present case.
Conversely, the neuronal metabolic theory attributes the neuronal death to a lack of intracellular ATP production due to mutation-related defective oxidative phosphorylation [6]. The neuronal hyperexcitability theory primarily supposes astrocytic dysfunction due to ATP deficiency as the underlying mechanism: astrocytic dysfunction causes defective uptake of glutamate through glutamate transporters and of potassium through Na+/ K+ ATPase into astrocytes and the elevation of glutamate and potassium concentration in the synaptic clefts that can induce not only vasodilatation in small vessels [7,8] but also neuronal death by excitotoxicity [9]. Considering the expansion of the lesions beyond the arterial territory, accompanied by hyperperfusion, we speculate that stroke-like episodes are more likely attributable to the neuronal hyperexcitability theory than the ischemic vascular theory. This may also be supported by the fact that the anticonvulsant LEV was effective against the stroke-like episodes in the present case. LEV regulates neurotransmission by binding to the synaptic vesicle glycoprotein 2A at the presynapse and inhibiting N-type Ca2+ channels. In addition, LEV not only improves synaptic plasticity but also elevates ATP levels [10], with low toxic potential to mitochondria [11]. It has also been reported that continuous infusion of midazolam [5] and administration of phenytoin [12] or lamotrigine [4] were effective against stroke-like episodes in MELAS. Thus, neurotransmitter regulation by anticonvulsants may be useful for the treatment of stroke-like episodes in MELAS.
3. Ethical standards
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflicts of interest
The authors declare that they have no competing interests.
Acknowledgments
Wendy Brooks, PhD, from Edanz Group (www.edanzediting.com/ac) provided English language editing assistance for a draft of this manuscript.
Contributor Information
Shota Sakai, Email: shoooo0725@gmail.com.
Tetsuro Ago, Email: agou@intmed2.med.kyushu-u.ac.jp.
Takanari Kitazono, Email: kitazono@intmed2.med.kyushu-u.ac.jp.
References
- 1.Ohama E., Ohara S., Ikuta F. Mitochondrial angiopathy in cerebral blood vessels of mitochondrial encephalomyopathy. Acta Neuropathol. 1987;74:226–233. doi: 10.1007/BF00688185. [DOI] [PubMed] [Google Scholar]
- 2.Koga Y., Ishibashi M., Ueki I. Effects of L-arginine on the acute phase of strokes in three patients with MELAS. Neurology. 2002;58:827–828. doi: 10.1212/wnl.58.5.827. [DOI] [PubMed] [Google Scholar]
- 3.Koga Y., Akita Y., Junko N. Endothelial dysfunction in MELAS improved by l-arginine supplementation. Neurology. 2006;66:1766–1769. doi: 10.1212/01.wnl.0000220197.36849.1e. [DOI] [PubMed] [Google Scholar]
- 4.Kai T., Masuda S., Tokunaga H. A case of mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS) with treatment-resistant status epilepticus that was effectively treated with lamotrigine. Clin. Neurol. 2013;53:809–813. doi: 10.5692/clinicalneurol.53.809. [DOI] [PubMed] [Google Scholar]
- 5.Tsujikawa K., Yokoi S., Yasui K. Effectiveness of midazolam for L-arginine-resistant headaches during stroke-like episodes in MELAS: a case report. Clin. Neurol. 2014;54:882–887. doi: 10.5692/clinicalneurol.54.882. [DOI] [PubMed] [Google Scholar]
- 6.Mukoyama M., Kazui H., Sunohara N. Mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes with acanthocytosis: a clinicopathological study of a unique case. J. Neurol. 1986;233:228–232. doi: 10.1007/BF00314025. [DOI] [PubMed] [Google Scholar]
- 7.Iizuka T., Sakai F. Pathogenesis of stroke-like episodes in MELAS: analysis of neurovascular cellular mechanisms. Curr. Neurovasc. Res. 2005;2:29–45. doi: 10.2174/1567202052773544. [DOI] [PubMed] [Google Scholar]
- 8.Iizuka T., Sakai F. Pathophysiology of stroke-like episodes in MELAS: neuron-astrocyte uncoupling in neuronal hyperexcitability. Future Neurol. 2010;5:61–83. [Google Scholar]
- 9.Attwell D., Buchan A.M., Charpak S. Glial and neuronal control of brain blood flow. Nature. 2010;468:232–243. doi: 10.1038/nature09613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stockburger C., Miano D., Baeumlisberger M. A Mitochondrial role of SV2a protein in aging and Alzheimer's disease: studies with levetiracetam. J. Alzheimers Dis. 2016;50:201–215. doi: 10.3233/JAD-150687. [DOI] [PubMed] [Google Scholar]
- 11.Finsterer J., Scorza F.A. Effects of antiepileptic drugs on mitochondrial functions, morphology, kinetics, biogenesis, and survival. Epilepsy Res. 2017;136:5–11. doi: 10.1016/j.eplepsyres.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Iizuka T., Sakai F., Kan S. Slowly progressive spread of the stroke-like lesions in MELAS. Neurology. 2003;61:1238–1244. doi: 10.1212/01.wnl.0000091888.26232.fe. [DOI] [PubMed] [Google Scholar]