Abstract
We aimed to assess the impact of timing of surgery in elderly patients with acute hip fracture on morbidity and mortality. We systematically searched MEDLINE, the Cochrane Library, Embase, PubMed, and trial registries from 01/1997 to 05/2017, as well as reference lists of relevant reviews, archives of orthopaedic conferences, and contacted experts. Eligible studies had to be randomised controlled trials (RCTs) or prospective cohort studies, including patients 60 years or older with acute hip fracture. Two authors independently assessed study eligibility, abstracted data, and critically appraised study quality. We conducted meta-analyses using the generic inverse variance model. We included 28 prospective observational studies reporting data of 31,242 patients. Patients operated on within 48 hours had a 20% lower risk of dying within 12 months (risk ratio (RR) 0.80, 95% confidence interval (CI) 0.66–0.97). No statistical significant different mortality risk was observed when comparing patients operated on within or after 24 hours (RR 0.82, 95% CI 0.67–1.01). Adjusted data demonstrated fewer complications (8% vs. 17%) in patients who had early surgery, and increasing risk for pressure ulcers with increased time of delay in another study. Early hip surgery within 48 hours was associated with lower mortality risk and fewer perioperative complications.
Introduction
Hip fractures in elderly populations are a major public health concern in Europe and the United States (US)1–3. The annual incidence of hip fractures rises with age. In the US, it ranges between 0.2% in women aged 60 to 64 years to 2.5% in women aged 85 years or older4. In Europe, the annual hip fracture incidence for elderly women aged 60 years or older ranges between 0.5% to 1.6% per year5–7. The risk for men is about half of that for women8.
Hip fractures in elderly patients are serious injuries that can lead to immobility and permanent dependence, negatively impacting patients’ quality of life and resulting in a financial burden for health systems and societies7–10. Hip fractures can also lead to death. Mortality rates among the elderly following hip fractures range between 14% to 36% within 1 year of the injury11–19. During the first three months after hip fracture, elderly patients have a 5- to 8-fold increased risk of dying20. The increased mortality risk persists up to ten years20. Because of a predicted increase in life expectancy in western countries over the next decades21–23, hip fractures and their consequences will have an even larger impact on health systems and societies in the future.
Factors that influence prognosis of elderly patients after hip fracture are age, gender, comorbidities, anticoagulation therapy, and general physical health status at the time of injury24. Furthermore, timing of surgery is thought to play an important role regarding survival. Although international clinical practice guidelines recommend surgical treatment of acute hip fracture within 24 to 48 hours after admission25–27, these recommendations are still discussed controversially28–30. Some researchers argue that early surgery can lead to an increased risk of perioperative complications, including pneumonia, deep venous thrombosis, bleeding, pulmonary embolism, urinary tract infections, and decubital ulcerations because clinicians do not have enough time to optimise patients’ medical conditions preoperatively29–31.
The most recent systematic review on this topic was published in 201032. Since then, many well-conducted studies have been published. To provide a comprehensive overview, it is necessary to systematically review the currently available evidence on the impact of timing of surgery in elderly patients with acute hip fracture. In contrast to former reviews that focused exclusively on mortality, we additionally aimed to assess other patient-relevant outcomes, such as perioperative complications, functional capacity, and quality of life. We also explored whether timing of surgery has different effects in different subgroups, e.g., in patients on anticoagulation treatment or patients with poor physical status.
Our systematic review aimed to answer the following questions:
In patients aged 60 years or older with an acute hip fracture, what is the impact of timing of surgery on beneficial and harmful outcomes such as mortality, functional capacity, quality of life, and perioperative complications?
Do beneficial or harmful treatment effects of timing of surgery vary by subgroups based on patient characteristics (age, sex), physical status (e.g., ASA Physical Status System), and common medical treatments (e.g., anticoagulation treatment)?
Methods
To answer our research questions, we conducted a systematic review that has been registered with the International Prospective Register of Systematic Reviews (PROSPERO), registration number: CRD4201705821633. The study protocol has been published previously34. We will summarise the most important methodological steps in the sections below.
Search Strategy and Criteria
An experienced information specialist searched MEDLINE (Ovid), PubMed (non-MEDLINE content), Embase.com, the Cochrane Library (Wiley), for the period of January 1997 to May 2017, using keywords and medical subject headings for hip fracture surgery, adult patients, and timing factors. To ensure finding all relevant studies on this topic a broad range of synonyms where used for the search (see Appendix 1 for the search strategy). In addition, we searched the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) and ClinicalTrials.gov, as well as reference lists of relevant publications, websites and conference proceedings of orthopaedic and traumatological societies (see Appendix 2).
Inclusion and Exclusion
Inclusion and exclusion criteria were predetermined in the published protocol35. Eligible study designs were randomised controlled trials (RCTs), non-randomised controlled trials, and prospective controlled cohort studies. The populations of interest were adults aged 60 years or older undergoing surgery for acute intra- and extracapsular hip fracture. We also included studies where only a small proportion (<5%) of patients were younger than 60 years. Studies were included only if they compared early and delayed surgery for hip fractures. The primary outcome was all-cause mortality. Secondary outcomes of interest were perioperative complications, functional capacity, and quality of life. Detailed eligibility criteria are presented in Table 1.
Table 1.
Eligibility criteria for included studies.
| Study characteristic | Inclusion | Exclusion |
|---|---|---|
| Population | • Studies including at least 95% adults aged 60 years or older who underwent surgery for acute hip fracture (intra- or extracapsular) | • Studies including 5% or more patients younger than 60 years • Studies on patients undergoing surgery for other reasons than hip fracture • Studies on patients with hip fracture not related to acute trauma, with pathological fractures, or with periprosthetic fractures |
| Intervention | • Early surgery for hip fracture as defined by authors in the primary study | • Studies that do not compare timing of surgery |
| Control intervention | • Delayed surgery for hip fracture as defined by authors in the primary study | |
| Outcomes | • All-cause mortality • Severe perioperative complications ○ Pulmonary embolism ○ Pneumonia ○ Deep vein thrombosis ○ Others Other perioperative complications: ○ Urinary tract infection ○ Pressure ulcer ○ Others • Functional capacity • Quality of life |
• Studies that do not include at least one of the outcomes listed under the inclusion criteria |
| Publication language | • English • German |
• All other languages |
| Geography | No limitation | No limitation |
| Study design | • Randomised controlled trials• Non-randomised trials• Prospective controlled cohort studies | • Case series • case reports • retrospective controlled cohort studies • case-control • studies studies without a control group |
| Publication type | Any publication reporting primary data | Publications not reporting primary data, or only available as abstracts |
| Publication date | Studies published from 1997 onwards | Studies published before 1997 |
Assessment of Study Quality and Certainty of Evidence
We used the Newcastle-Ottawa-Scale (NOS) to judge the risk of bias in included cohort studies36. Two authors independently assessed the risk of selection bias, comparability of groups, adequacy of outcome measurement, and reporting. We resolved disagreements by consensus or involvement of a third review author.
In addition, we assessed the certainty of evidence (CoE) across studies for important outcomes following recommendations of the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) working group37. Experts in the field of orthopaedics and traumatology ranked outcomes regarding clinical and patients’ relevance in a modified two-staged Delphi process. They agreed on mortality, quality of life, perioperative complications, and function/mobility as the most important outcomes. For these outcomes, we graded the certainty of evidence and classified it as “high,” “moderate,” “low,” or “very low.” High certainty means we are very confident that the true effect is close to the effect estimate. On the contrary, if the certainty is very low, we assume that the true effect is likely to be significantly different from the effect estimate37.
Data Collection and Abstraction
Two review authors independently reviewed abstracts and full-text articles in two consecutive steps. Disagreements were resolved by consensus or discussion with a third author. Two team members independently extracted relevant information on study design, methods, patient characteristics, intervention, control, and outcomes from included studies. In case information about relevant outcomes or study characteristics was missing or unclear, we contacted study authors.
Meta-analysis Methodology
We used the generic inverse variance method to combine effects of individual observational studies that were adjusted for potential confounders and were rated as low or moderate risk of bias in meta-analyses. We pooled data only if at least three studies used comparable cut-offs for “early” and “delayed” surgery and reported the same outcome. In case the studies reported hazard ratios (HR) or odds ratios (OR), we converted them into risk ratio (RR) using the following formulas for HR: RR = 1 − e (HR* ln (1 − P0))/P032, and for OR: RR = OR/((1 − P0) + (P0 * OR))38; P0 means the event rate in the control group. For one study39, we were not able to calculate P0 because no crude numbers of events were reported, so we used the mean P0 from the other included studies to convert OR into RR. We added observational studies with unadjusted results, irrespective of their risk of bias judgment to meta-analyses for sensitivity analyses.
To assess statistical heterogeneity in effects between studies, we calculated the chi-squared statistic and the I2 statistic (the proportion of variation in study estimates attributable to heterogeneity rather than due to chance)40,41. Due to the limited number of studies included in meta-analyses, no funnel plots could be used to assess publication bias. We used RevMan Version 5.342 for all statistical analyses.
For outcomes for which no meta-analyses were possible, we summarise data narratively. If several studies reported the same outcome but meta-analyses were not possible because of high clinical heterogeneity or because the study was rated high risk of bias, we graphically display results in forest plots without pooled summary estimates.
Because data were not sufficient to conduct subgroup analyses, we summarise these results narratively.
Results
Study characteristics
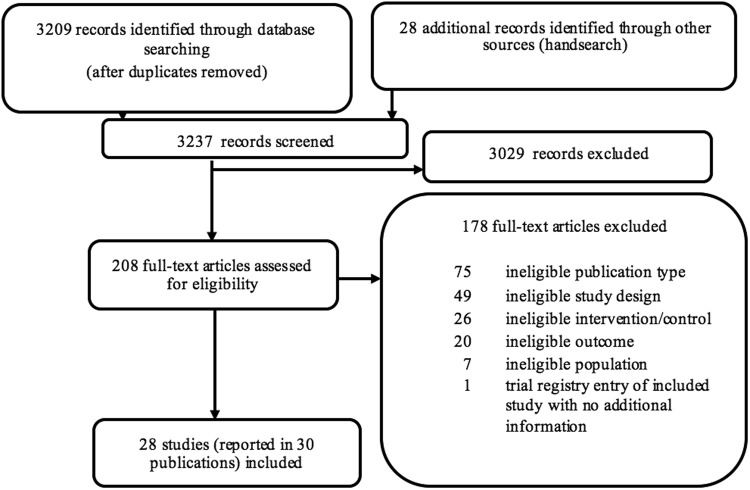
We included 28 prospective cohort studies13,29,31,39,43–67 (published in 30 articles) reporting results on 31,242 patients (see Fig. 1, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart). We could not detect any eligible RCTs.
Figure 1.
PRISMA flow chart.
Of the 28 included studies, 15 had a low29,46,53,57,62,68 or moderate13,31,39,45,47,52,55,64–66 risk of bias, and 13 studies were rated high risk of bias43,44,48–51,54,56,58–61,63. Most studies used a cut-off time for surgical delay of 48 or 24 hours; other studies used (additional) cut-offs at 6 hours, 12 hours, 18 hours, 36 hours, and 72 hours. Table 2 presents study and patient characteristics of included studies.
Table 2.
Characteristics of included studies.
| Author, year of publication, country | Follow-up | Number of patients analysed | Age, mean (SD or range) | Female | Fracture type | Comparison early/delayed surgery | Outcomes | Additional information from authors used | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|
| Al-Ani, 2008, Sweden62 | 4 months | 744 | 81 (9) | 73% | cervical 49%, trochanteric 43%, subtrochanteric 8% | ≤24 h vs. >24 h, ≤36 h vs. >36 h, ≤48 h vs. >48 h | - mortality within 4 months (adjusted for age, sex, prefracture walking ability,dementia, ASA score), - pressure ulcer (adjusted for age, prefracture walking ability, dementia, ASA score,duration of surgery) |
yes | low |
| Bretherton, 2015, United Kingdom53 | 12 months | 6638 | 82 (8) | 78% | intracapsular 58%, extracapsular 42% | ≤6 h vs. >6 h, ≤12 h vs. >12 h, ≤18 h vs. >18 h, ≤24 h vs. >24 h, ≤36 h vs. >36 h, ≤48 h vs. >48 h | - mortality within 1 month (adjusted for age, gender, pre-fracture mobility, Mini-Mental Test Score, fracture type, ASA grade,prefracture residence) | no | low |
| Butler, 2017, Ireland63 | 6 weeks | 51 | 82 (9) | 82% | intracapsular 57%, extracapsular 43% | >12 h & ≤36 h vs. >36 h | - functional capacity (Barthel Index) unadjusted | no | high |
| Crego–Vita, 2017, Spain44 | 24 months | 293 (mortality), 136 (function) | 83 (65-105) | 61% | intracapsular 100% | ≤24 h vs. >24 h (mortality) ≤24 h vs. >24 h & ≤72 h vs. >72 h (function) | - mortality within 6 months - mortality within 12 months - mortality within 24 months - functional capacity (FAC level, MBI) - u all outcomes: unadjusted |
yes | high |
| Dailiana, 2013, Greece39 | 12 months | 218 | 79 (7) | 64% | intertrochanteric 64%, subcapital 30%, subtrochanteric 6%, | ≤48 h vs. >48 h | - mortality within 1 month (adjusted for age,sex, Charlson index) - mortality within 12 months (adjusted for age, sex, Charlson index) |
no | moderate |
| Dorotka, 2003, Austria48 | 6 months | 181 (mortality, complications), 152 (function) | early group: 77 (12) delayed group: 79 (12) | 76% | Garden type I, II 10%, Garden type III, IV 30%, basocervial 3%, pertrochanteric stable 30%, pertrochanteric unstable 10%, per- and subtrochanteric 17% | ≤6 h vs. >6 h, ≤12 h vs. >12 h, >18 h vs. >18 h, ≤24 h vs. >24 h,≤36 h vs. >36 h | - mortality within 6 months perioperative complications (pneumonia) - functional capacity (mobility) - all outcomes: unadjusted |
no | high |
| Elliott, 2003, United Kingdom49 | 12 months | 1780 | <65 y:12%, 65-75 y: 17%, 75–84 y: 40%, over 85 y: 31% | 77% | NR | ≤24 h vs. >24 h | - mortality within 12 months (unadjusted) | no | high |
| Hapuarachchi, 2014, United Kingdom54 | 12 months | 146 | 93 (NR) | 84% | femoral neck fractures 100% | ≤24 h vs. >24 h, ≤48 h vs. >48 h | - Mortality within 1 months - Perioperative complications all outcomes: unadjusted |
no | high |
| Kelly-Pettersson, 2017, Sweden64 | 12 months | 561 | 82 (10) | 72% | femoral neck 54%, intertrochanteric 38%, subtrochanteric 8% | ≤24 h vs. >24 h | - Mortality within 12 months - Perioperative complications (pressure ulcer, pneumonia, pulmonary embolus, urinary tract infection) all outcomes: unadjusted |
yes (author provided data removing 16 patients younger than 60 years) | moderate |
| Kim, 2012, South Korea56 | 24 months | 415 | 75 (60–96) | 68% | femoral neck 56%, intertrochanteric 44% | ≤48 h vs. >48 h | - functional capacity | no | high |
| Lizaur-Utrilla, 2016, Spain13 | 12 months | 628 | 84 (7) | 74% | trochanteric 63%, cervical 37% | ≤48 h vs. >48 h | - mortality within 12 months (adjusted for age, gender, ASA, Charlson index,anticoagulation therapy, fracture type,prosthetic implant, complication,readmission, dementia, ADL, mobility, pre-nursing residence, nursing discharge) | yes | moderate |
| Maggi, 2010, Italy65 | 6 months | 2428 | 82 (9) | 79% | femur neck/head: 56%, intertrochanteric: 37%, subtrochanteric 7% | ≤48 h vs. >48 h | - mortality within 6 months (unadjusted, based only on complete follow-up, n = 2,010) | no | moderate |
| Mariconda, 2015, Italy52 | 12 months | 552 (mortality), 568 (complication) | 78 (50–105) | 77% | femoral neck 42%, trochanteric 55%, subtrochanteric 3% | <72 h vs. ≥72 h | - mortality within 1 month (unadjusted) mortality within 12 months (unadjusted) - perioperative complications within 4 months (adjusted for Mini-Mental State,ASA grade) |
yes | moderate |
| Moran, 2005, United Kingdom47 | 12 months | 2537 (mortality), 2354 (complications) | 80 (17–103) | 76% | femoral neck 100% | ≤24 h vs. >24 h | - mortality within 1 months - perioperative complications (embolism) all outcomes: unadjusted |
no | moderate |
| Muhm, 2013, Germany51 | 12 months | 257 | 84 (NR) | 86% | femoral neck 38%, trochanteric 62% | ≤48 h vs. >48h–168h | - mortality within 12 months (unadjusted) | yes | high |
| Orosz, 2004, United States29 | 6 months | 1178 | 82 | 80.6% | femoral neck 48% | ≤24 h vs. >24 h | - mortality within 6 months (adjusted for age,sex, nursing home residence, independence,function, comorbidities, fracture type,hospitalization within 6 months,hospital site, day and time of admission,abnormal clinical findings) - perioperative complications - functional capacity (FIM) (propensity score matched) |
no | low |
| Öztürk, 2010, Turkey59 | 12 months | 74 | 78 (8) | 70% | NR | ≤48 h vs. >48 h | - mortality within 12 months (unadjusted) | no | high |
| Pajulammi, 2016, Finland66,67,69 | 12 months | 1400 (mortality), 611 (function) | 84 (65–105) | 75% | neck of femur 62%, intertrochanteric 32%, subtrochanteric 6% | ≤24 h vs. >24 h | - mortality within 12 months - functional capacity (mobility) all outcomes: unadjusted |
yes | moderate |
| Pioli, 2012, Italy57,68 | 12 months | 806 | 86 (6) | 76% | intracapsular 47%, trochanteric 46%, subtrochanteric 7% | ≤48 h vs. >48 h | - mortality within 12 months (adjusted for age, sex, ADL, Charlson index) - functional capacity (mobility, ADL; unadjusted) |
yes | low |
| Poh, 2013, Singapore55 | in-hospital (mean 15 days) | 242 | 78 (10) | 70% | femoral neck 53%, pertrochanteric 47% | ≤48 h vs. >48 h | - perioperative complications (unadjusted) | no | moderate |
| Rae, 2007, Australia45 | 18 months | 222 | 79 (51–95) | 72% | femoral neck 100% | ≤24 h vs. >24h–≤48 h | - mortality within 1 months (adjusted for preoperative length of stay, ASA score,procedure, age, theatre cancellations, sex) | no | moderate |
| Siegmeth, 2005, United Kingdom46 | 12 months | 3628 | 81 (8) | 81% | intracapsular 59%, extracapsular 41% | ≤48 h vs. >48 h | - mortality within 12 months (unadjusted) | no | low |
| Smektala, 2000, Germany50 | 12 months | 161 | 84 (NR) | 93% | femoral neck NR%, intertrochanteric NR% | ≤24 h vs. >24 h | - mortality during hospital stay (unadjusted) | no | high |
| Smektala, 2008, Germany31 | 12 months | 1993 (mortality) 2916 (complications) | 82 (7) | 80% | femoral neck 50%, pertrochanteric femoral 50% | ≤12 h vs. >12h–≤36 h (mortality)≤36 h vs. >36 h (complications) | - mortality within 12 months (adjusted for age, sex, time from fracture to surgery,ASA, MBI, comorbidities, post-operative complications) - perioperative complications (pneumonia, embolism, UTI, pressure ulcer; unadjusted) |
no | moderate |
| Trpeski, 2013, Macedonia43 | 6 months | 120 | 74 (10) | 78% | inter- and pertrochanteric NR%, subtrochanteric NR% | ≤48 h vs. >48 h | - mortality within 1 months - mortality within 6 months all outcomes: unadjusted |
no | high |
| Vertelis, 2009, Lithuania60 | 12 months | 265 | women 77 (9), men 72 (14) | 68% | femoral neck fracture Garden ¾ 100% | ≤7 h vs. >7 h | - mortality within 12 months (adjusted for sex, age, osteosynthesis, arrival to hospital) | no | high |
| Vidán, 2011, Spain58 | in-hospital (median 10 days) | 1240 (mortality) 2249 (complications) | 84 (7) | 82% | femoral neck 41%, intertrochanteric 48%; subtrochanteric 6%; 5% other | ≤48 h vs. >48 h (mortality)≤48 h vs. >48 h (complications) | - mortality during hospital stay (adjusted for age, dementia, comorbidities, ADL) - perioperative complications (unadjusted) |
yes | high |
| Yonezawa, 2009, Japan61 | in-hospital (average 39.1 days) | 536 (mortality), 347 (function) | 83 (9) | 83% | trochanteric femoral 52%, femoral neck 48% | ≤24 h vs. >24 h | - mortality during hospital stay - functional capacity (mobility) all outcomes: unadjusted |
no | high |
Abbreviations: ADL, activities of daily living; ASA, American Society of Anaesthesiologists; FAC, Functional Ambulation Categories; FIM, Functional Independence Measure; h, hour; MBI: Modified Barthel Index; NR, not reported; UTI, urinary tract infection; vs., versus.
Mortality
Overall, 25 studies reported on all-cause mortality: nine studies (14,863 patients) provided adjusted hazard ratios (HR) or odds ratios (OR) for mortality13,29,31,39,45,53,57,58,62, adjusting at least for age, sex, and patient’s health status; 16 studies43,44,46–52,54,59–61,64–66 (14,654 patients) reported unadjusted effect estimates on mortality.
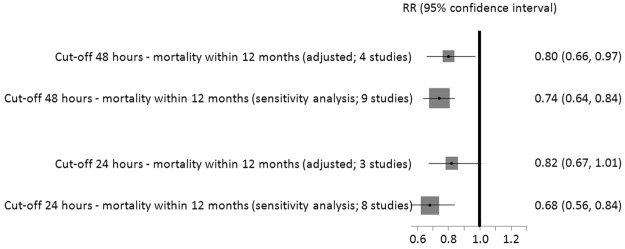
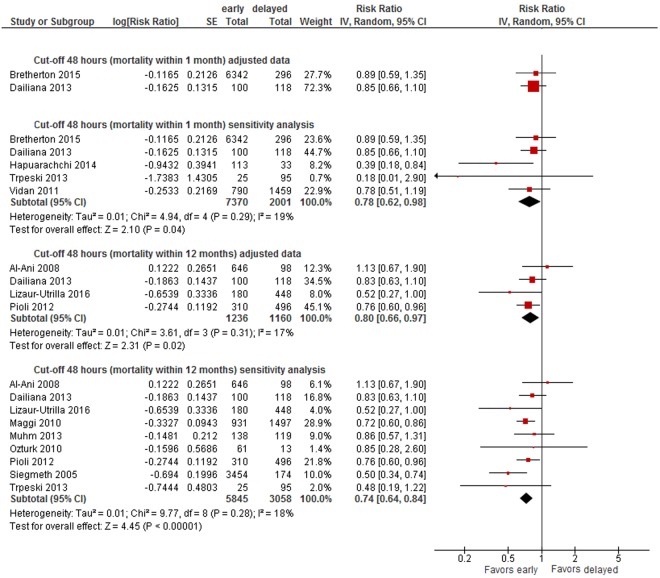
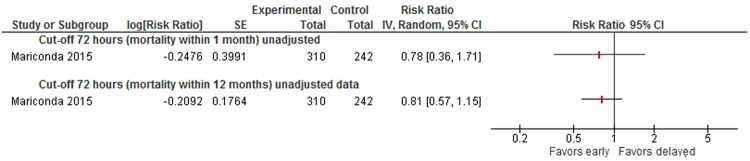
Cut-off 48 hours
Based on a meta-analysis of adjusted data from four studies13,39,62,68 the absolute risk of dying within 12 months was 21% in patients who had surgery after 48 hours and 17% in patients who had surgery within 48 hours resulting in a 20% smaller long-term mortality risk in patients operated on within 48 hours (RR 0.80, 95% CI 0.66-0.97, 2,396 patients, see Fig. 2). We graded the CoE for this outcome as low. We also conducted sensitivity analyses by adding unadjusted data on mortality from the remaining studies to the meta-analysis, irrespective of their bias risk. Adding the non-adjusted data did not alter the results for long-term mortality (RR 0.74, 95% CI 0.64-0.84, 8,903 patients)13,39,43,46,51,57,59,62,65,68 (see Fig. 2). No statistically significant differences were observed in two studies presenting adjusted data on short-term mortality (within 1 months) (RR 0.89, 95% CI 0.59-1.35, 6,638 patients; RR 0.85, 95% CI 0.66-1.10, 218 patients; CoE: very low)39,53. In sensitivity analyses, including unadjusted data, surgery within 48 hours was associated with a statistical significant benefit on short-term mortality (RR 0.78, 95% CI 0.62-0.98, 9,371 patients)39,43,53,54,58 (see Appendix 3, Fig. 5).
Figure 2.
Effects of early and delayed surgery on short- and long-term mortality using 48 hours and 24 hours as cut-offs (summary of results of random-effects meta-analyses and sensitivity analysis).
Figure 5.
Cut-off 48 hours - short- and long-term mortality adjusted and sensitivity analyses incl. unadjusted data.
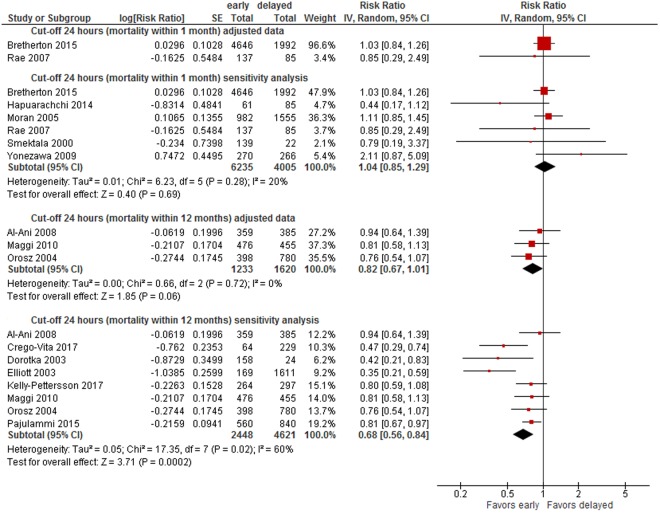
Cut-off 24 hours
A meta-analysis of three trials29,62,65(2,853 patients) rendered an 18% lower risk of long-term mortality in patients operated on within 24 hours (within 12 months: RR 0.82, 95% CI 0.67-1.01, CoE: low, absolute mortality risk early surgery: 17%, delayed: 14%) (see Fig. 2). When adding unadjusted data in sensitivity analyses, the difference between surgery within and after 24 hours was statistically significant (RR 0.68, 95% CI 0.56-0.84, 7,069 patients)29,44,48,49,62,64,65,69 (see Fig. 2). No statistically significant differences were observed in two studies presenting adjusted data on short-term mortality (RR 1.03, 95% CI 0.84-1.26, 6,638 patients; RR 0.85, 95% CI 0.29 to 2.49, 222 patients; CoE: very low)45,53, as well as in sensitivity analyses (RR 1.04, 95% CI 0.85-1.29)31,45,47,53,54,61 (see Appendix 3, Fig. 7).
Figure 7.
Cut-off 24 hours - short- and long-term mortality adjusted and sensitivity analyses incl. unadjusted data.
Figure 2 summarises results of meta-analyses on long-term mortality and corresponding sensitivity analyses.
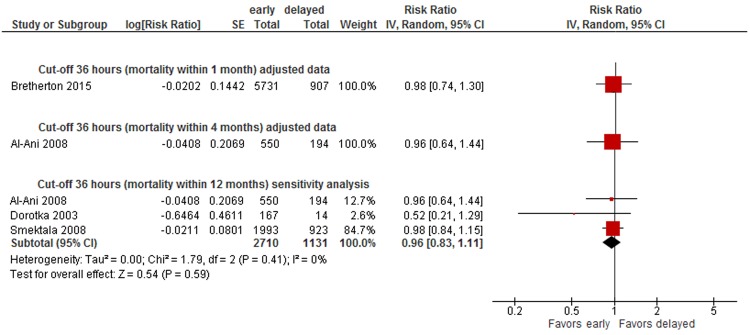
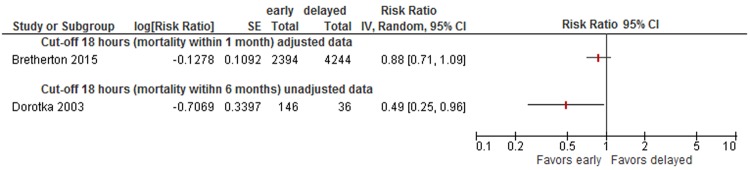
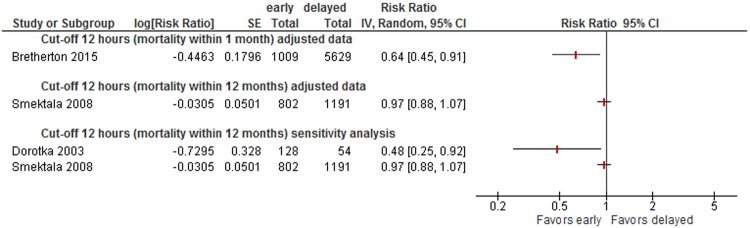
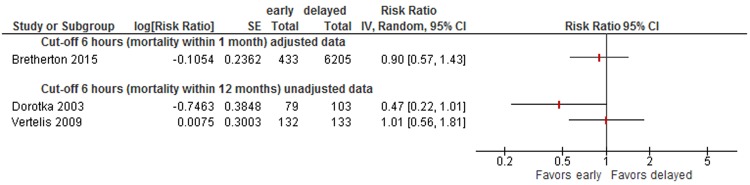
Data were insufficient to conduct meta-analyses for other cut-offs (6, 12, 18, 36, 72 hours) of timing of surgery. However, to illustrate the results on mortality of all studies, we present forest plots for each cut-off in Appendix 3 (48 hours: see Fig. 5, 36 hours: see Fig. 6, 24 hours: see Fig. 7, 18 hours: see Fig. 8, 12 hours: see Figs 9, 6 hours: see Fig. 10, 72 hours: see Fig. 11).
Figure 6.
Cut-off 36 hours - short- and long-term mortality adjusted and sensitivity analyses incl. unadjusted data.
Figure 8.
Cut-off 18 hours - short- and long-term mortality adjusted and unadjusted data (not pooled).
Figure 9.
Cut-off 12 hours - short- and long-term mortality adjusted and unadjusted data (not pooled).
Figure 10.
Cut-off 6 hours - short- and long-term mortality adjusted and unadjusted data.
Figure 11.
Cut-off 72 hours - short- and long-term mortality adjusted and unadjusted data.
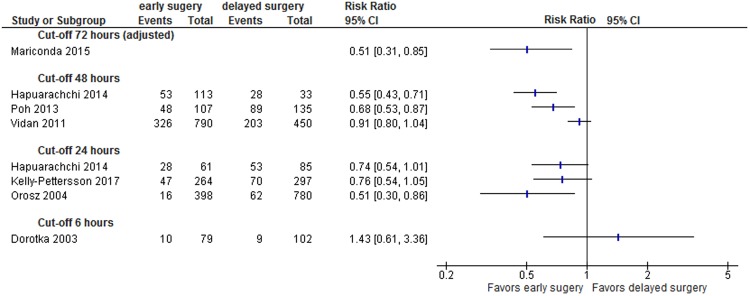
Perioperative Complications
Two studies with low62 and medium52 risk of bias reported adjusted data on general perioperative complications or pressure ulcers, respectively. Mariconda et al. reported data on 568 patients and showed that surgery within 72 hours was associated with decreased odds of general complications such as pressure ulcers, urinary tract infection, deep vein thrombosis/embolism, or stroke (absolute risk of complications: 17% vs. 8%; OR 0.51, 95% CI 0.31-0.85, see Fig. 3)52.
Figure 3.
Perioperative complications (adjusted and unadjusted data); Mariconda 2015: effect estimate presented is odds ratio (OR) not RR and based on adjusted data so no event rates displayed; Abbreviations: CI: confidence interval.
Six studies reported unadjusted data for perioperative complications29,48,54,55,58,64. Figure 3 presents unadjusted effect estimates of individual studies. While a cut-off of 6 hours did not show significantly different rates of complications, patients who had surgery within 24 or 48 hours suffered from complications less frequently than those with late surgery.
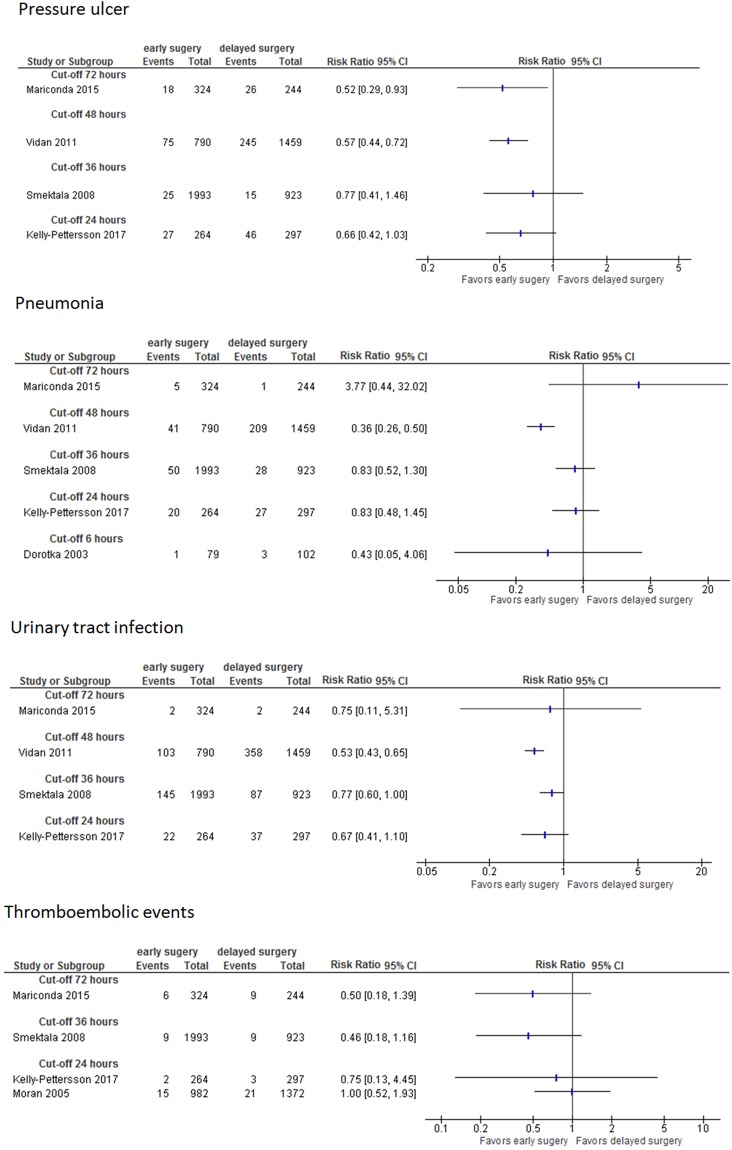
One study on 744 patients used three different cut-offs (24, 36, 48 hours) for “delayed surgery” and presented adjusted data for pressure ulcers. The odds of developing pressure ulcers increased with the time of delay (>24 hours: OR 2.19, 95% CI 1.21-3.96; >36 hours: OR 3.42, 95% CI 1.94-6.04; >48 hours: OR 4.34, 95% CI 2.34-8.04)62. In studies reporting unadjusted data the risk for developing pressure ulcers, pneumonia, urinary tract infections, or thromboembolic events was either smaller for patients who had early surgery or similar between both groups; it was not higher in any study for patients who had early surgery (see Fig. 4). CoE for perioperative complications was very low.
Figure 4.
Pneumonia, pressure ulcers, urinary tract infection, thromboembolic events (unadjusted data); Abbreviations: CI: confidence interval.
Quality of life
None of the included studies reported how timing of surgery affects the patients’ quality of life.
Functional capacity
Measuring of mobility and functional capacity was different among eight studies29,44,48,56,57,61,63,66 and data are summarised in Table 3. Patients who had early surgery had similar or slightly better functional capacity compared to those operated on later (CoE: very low).
Table 3.
Functional capacity outcomes.
| Study, year | Function/Mobility outcome | Cut-off | Outcome in patients operated on early | Outcome in patients operated on delayed | ||
|---|---|---|---|---|---|---|
| Continuous outcome measure | Mean score (measure of dispersion) | N | Mean score (measure of dispersion) | N | ||
| Crego-Vita, 201744 | FAC* (functional ambulation category) at 6 months | ≤24 h vs. >24 h–≤72 h | 4 (NR) | 64 | 3 (NR) | 72 |
| Crego-Vita, 201744 | FAC* (functional ambulation category) at 12 months | ≤24 h vs. >24 h–≤72 h | 4 (NR) | 64 | 4 (NR) | 72 |
| Crego-Vita, 201744 | FAC* (functional ambulation category) at 2 years | ≤24 h vs. >24 h–≤72 h | 3 (NR) | 64 | 3 (NR) | 72 |
| Crego-Vita, 201744 | MBI** (Modified Barthel Index) at 6 months | ≤24 h vs. >24 h–≤72 h | 60 (NR) | 64 | 48 (NR) | 72 |
| Crego-Vita, 201744 | MBI** (Modified Barthel Index) at 12 months | ≤24 h vs. >24 h–≤72 h | 71 (NR) | 64 | 58 (NR) | 72 |
| Crego-Vita, 201744 | MBI** (Modified Barthel Index) at 2 years | ≤24 h vs. >24 h–≤72 h | 69 (NR) | 64 | 55 (NR) | 72 |
| Orosz, 200629 | FIM*** (Functional independence measure) locomotion (range 2–14) at 6 months (propensity score matched, 296 pairs) | 24 h | 9.4 (NR) | 398 | 9.3 (NR) | 780 |
| Orosz, 200629 | FIM*** (Functional independence measure) self-care (range 6–42) at 6 months (propensity score matched, 299 pairs) | 24 h | 32.3 (NR) | 398 | 33.4 (NR) | 780 |
| Orosz, 200629 | FIM*** (Functional independence measure) transferring (range 3–21) at 6 months (propensity score matched, 302 pairs) | 24 h | 14.4 (NR) | 398 | 14.9 (NR) | 780 |
| Butler, 201763 | Barthel Index** (mean decrease) | 36 h | 10 (IQR 0–19) | 30 | 30 (IQR 25–40) | 21 |
| Pioli, 201257 | ADL**** (activities of daily living) at 6th months | 48 h | 3.1 (SD ± 2.1) | 310 | 3.4 (SD ± 2.2) | 496 |
| Dichotomous outcome measure | Proportion | N | Proportion | N | ||
| Dorotka, 200348 | Mobility at 6 months (no walking aids needed) | 6 h | 33% (NR) | 71 | 23% (NR) | 81 |
| Pajulammi, 201566 | Same or better mobility level at 1 year | 24 h | 65% (NR) | 258 | 60% (NR) | 353 |
| Yonezawa, 200861 | Mobility in those independent before injury | 24 h | 52% (NR) | 173 | 41% (NR) | 174 |
| Pioli, 201257 | Independent walking at 6 months | 48 h | 42% (NR) | 310 | 39% (NR) | 496 |
| Kim, 201256 | Recovery to former functional capacity (2 years after surgery) | 48 h | 45% (NR) | 174 | 34% (NR) | 241 |
Abbreviations: ADL, activities of daily living; FAC, Functional Ambulation Categories; FIM, Functional Independence Measure; h, hour; IQR, interquartile range; MBI: Modified Barthel Index; N, total number of patients in this group; NR, not reported; SD, standard deviation.
*FAC scale from 1–5; higher score indicates independence.
**MBI scale from 0–100; higher score indicates independence.
***FIM, range of scale depends on subscale; higher score indicates independence.
****Higher score indicates independence.
Impact of timing of surgery in subgroups
Due to insufficient data, we were not able to conduct subgroup analyses to assess different effects of timing of surgery between age groups, sex, patients’ physical status, and anticoagulation. However, six studies assessed the effects of timing of surgery in different subgroups29,47,54,57,58,61. Below we present results narratively.
Age
In two studies, timing of surgery (before or after 24 hours) showed no significant difference in mortality rates in different age groups. Yonezawa et al. showed that there was no statistically significant difference in mortality in patients 85 years and older, whether they had surgery within 24 hours or later (early: 10/136; 7% vs. delayed: 5/117; 4%; p = 0.301), as well as in patients younger than 85 years (early: 5/134; 4% vs. delayed: 2/149; 1%; p = 0.363)61. Vidán et al. also reported that time to surgery and age showed no interaction (p = 0.500)58.
Sex
In male patients, early surgery (within 24 hours) was associated with higher mortality (6/40; 15% vs. 1/51; 2%; p = 0.040), in females it was not (9/230; 4% vs. 6/215; 3%; p = 0.512)61. However, event rates are very small, and the observed differences could be chance findings.
Physical status
Timing of surgery (before or after 24 hours) was associated with similar mortality rates in dependently (early: 6/173; 4% vs. delayed: 3/174; 2%; p = 0.494) and independently living patients (early: 9/96; 9% vs. delayed: 4/90; 4%; p = 0.188). Patients with comorbidities benefited more often from surgery within 24 hours (early: 3/196; 7% vs. delayed 5/200; 3%; p = 0.048). In medically fit patients without comorbidities no statistically significant difference between early and delayed was detected61. Again, the low number of events makes chance findings inevitable.
Another study divided patients into two groups, either fit or unfit for immediate surgery, depending on their physical status. In the group of patients considered fit for surgery, no statistically significant difference between early (within 24 hours) and delayed surgery was observed regarding 30-day mortality (85/982; 9% vs. 85/1166; 7%; p = 0.510)47. In the group of patients with acute medical comorbidities, there was no significant relationship between timing of the surgery and mortality at 30 days, 90 days, or one year (HR 0.68, 95% CI 0.34-1.39; p = 0.290; HR 1.16, 95% CI 0.72-1.86; p = 0.540; HR 1.03, 95% CI 0.68-1.58; p = 0.880, respectively). A delay of more than one day from injury to presentation was associated with higher mortality in this group of patients (HR 2.1, 95% CI 1.01-4.2; p = 0.048)47.
Hapuarachchi et al. included 146 patients at the age of 90 or older54 and stratified patients according to the orthopaedic POSSUM (The Physiological and Operative Severity Score for enUmeration of Mortality and morbidity) score. Mortality was statistically significant higher in patients with POSSUM scores of ≥42 and delayed surgery (after 48 hours) as compared with early surgery (within 48 hours): early: 7% vs. delayed: 50%; p = 0.009. In patients with lower POSSUM scores no difference in mortality between early (within 48 hours) and delayed surgery was reported (POSSUM score 37-40: early: 8% vs. delayed: 11%, p = 0.500; POSSUM score ≤ 36: early: 24% vs. delayed: 50%, p = 0.310).
Pioli et al. hypothesised that timing of surgery is more important for frail elderly patients than for older people without functional impairment. Therefore, they divided patients into three groups according to their IADL (Instrumental Activities of Daily Living) score. One-year mortality in group 1 (dependent) and group 2 (intermediate level) relatively increased by 14% and 21%, respectively, per day of surgical delay (HR 1.14; 95% CI 1.06-1.22, p < 0.001 and HR 1.21; 95% CI 1.09-1.34, p < 0.001), but not in group 3 (high independence; HR 1.05; 95% CI 0.79-1.41, p = 0.706)57.
In a prospective cohort study including 1,206 patients, those with abnormal clinical findings or the need for further preoperative evaluation were excluded to form a restricted cohort of medically fit patients. In this group, early surgery within 24 hours had no association with functional outcomes or mortality, but was associated with reduced major postoperative complications (p = 0.041)29.
Anticoagulation treatment
In most of the studies, anticoagulants were more common in the delayed group and frequently caused surgical delay13,39,48,51. However, we did not identify any study reporting on differences between early and delayed surgery in patients with and without anticoagulation treatment.
Discussion
To the best of our knowledge, this is the first systematic review critically assessing all relevant prospective studies on this topic since 2010. We identified 20 new studies that had not been considered in the previous reviews32,70,71. Our findings agree with previous systematic reviews. Simunovic et al. showed that early surgery (within 24 to 72 hours) can reduce the risk of all-cause mortality in patients aged 60 or older by 19% (risk ratio (RR) 0.81, 95% confidence interval (CI) 0.68–0.96)32. Early surgery was also associated with a reduction of pressure ulcers and postoperative pneumonia (RR 0.48, 95% CI 0.34-0.69)32. Another systematic review including prospective and retrospective observational studies also demonstrated that a delay in surgery beyond 48 hours was associated with an increased 1-year-mortality and 30-day mortality risk (odds ratio (OR) 1.32, 95% CI 1.21-1.43; 30-day mortality: OR 1.41, 95% CI 1.29–1.54)70.
In contrast to other systematic reviews we looked at the effect of different cut-offs for “early” and “delayed” surgery separately and found that early surgery within 48 hours was associated with decreased long-term mortality in elderly patients after hip fractures. Single studies using other cut-offs (6, 12, 18, 24 or 36 hours) did not demonstrate significant differences in mortality between early and delayed surgery. However, these studies were probably underpowered and it is important to note that no study demonstrated a beneficial effect of delayed surgery on mortality.
Although findings of this review strengthen existing guidelines recommending surgery within 48 hours, in clinical practice, delay of surgery of hip fractures is quite common. In situations where patients need medical optimisation due to poor health status or long-term medication72, delays cannot be avoided. However, the reasons for delayed surgery are also often limited capacity of operating rooms and personnel, or weekend and holiday administration32,58,73,74. Cha et al. showed that hospital factors are accountable for three-fourths of the surgical delays74. In the interest of high quality care, organisational and structural improvements, such as better availability of operating rooms and staff, are necessary to enable early surgery. There is also general agreement that rapidly correctable comorbidities such as anaemia, hypovolemia, electrolyte imbalance, and correctable cardiac arrhythmias should not delay the operation27.
Only six of the included studies reported the effects of time to surgery in our predefined subgroups. In healthy, independent patients, delayed surgery was not as problematic as in patients with comorbidities. In most of these studies, the event rate was very small. Hence, the results could be chance findings. Moreover, the studies presented only unadjusted data. It should be emphasised that conclusions based on this data must be drawn carefully. Nevertheless, if availability of staff and operation room is limited, comorbid patients could be prioritised and have early surgery, presupposing that they do not have clear contraindications for surgery.
Our study has some limitations. We graded the certainty of evidence for all outcomes low or very low, which means that our confidence in the findings is limited. One reason for the low certainty of evidence is that we only identified prospective cohort studies but no RCTs. Results of observational studies must be interpreted with caution since confounding could distort the findings. It is possible that non-organisational reasons for delay of surgery such as need for medical optimisation also increased the risk of dying, independently, or in addition to timing of surgery. To minimise the distortion through confounding we included for our main analysis only data from adjusted analyses where at least the most important confounders such as age, gender, ASA score, fracture type and comorbidities had been considered. However, due to lack of randomisation, confounding cannot be completely eliminated.
The studies identified used different cut-offs to define early and delayed surgery. We combined only data from studies using very similar cut-offs. This allowed us to include only a small number of the included studies into meta-analyses. However, presenting the evidence for different cut-offs separately is relevant to inform clinical practice about the optimal timing of surgery.
No study conducted subgroup analysis with tests for interaction. However, some analysed the effect of timing of surgery in separate strata, allowing us to draw some conclusions about different effects in subgroups. Moreover, often the number of events was very small, making chance findings very likely. The results on subgroups therefore have to be interpreted with caution.
Despite our comprehensive search, it is possible that not all studies conducted on this topic have been detected (e.g., studies published in languages other than English or German). Publication bias cannot be ruled out, and we were not able to assess potential publication bias with a funnel plot. However, we contacted experts in the field, searched trial registries, and ultimately found 20 new studies that have not been included in former systematic reviews.
To overcome the limitation of observational studies, RCTs on this topic are needed. Although experts often argue, that this is unethical and not possible to implement, a RCT on timing of surgery in hip fracture patients is on the way. The HIP-ATTACK trial (HIP fracture Accelerated surgical TreaTment And Care tracK) will compare the effect of accelerated surgery and standard surgical care on perioperative complications and mortality75. A total of 1,200 patients older than 45 with low-energy hip fracture will be included in the study. The results of this trial will inform clinical practice and for the first time control adequately for known and unknown confounders.
Conclusion
In elderly patients sustaining hip fracture, early surgery is associated with reduced mortality and perioperative complications. Patients operated on within 48 hours had a 20% lower 1-year mortality.
However, timing of surgery for patients with hip fractures remains a challenge, as it requires multidisciplinary coordination between different occupational groups and the availability of appropriate surgical capacity with competent staff and proper equipment. No study demonstrated a survival benefit with delayed surgery. Future studies should investigate the effect of early surgery in subgroups of patients (e.g. patients with greater co-morbidities or anticoagulation treatment) and include data on patient-relevant outcomes, such as quality of life measurements. Furthermore, randomised controlled trials are needed to rule out potential confounding.
Electronic supplementary material
Acknowledgements
We thank Sandra Hummel and Sabine Siebenhandl for administrative support throughout the project and Emma Persad for proof reading.
Author Contributions
I.K. conducted systematic literature searches. T.K., C.S., C.R., B.W., B.N., G.W. reviewed records for inclusion, abstracted data, contacted authors, and assessed the risk of bias of included studies. B.N., G.G., and G.W. conducted meta-analyses. T.K., C.S., C.R., B.N., G.W., I.K. drafted the manuscript. G.G., S.N., M.L. critically revised the manuscript. All authors approved the final version of the manuscript.
Data Availability
The datasets generated during the study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-32098-7.
References
- 1.Langley J, Samaranayaka A, Davie G, Campbell AJ. Age, cohort and period effects on hip fracture incidence: analysis and predictions from New Zealand data 1974–2007. Osteoporos Int. 2010;22:105–111. doi: 10.1007/s00198-010-1205-6. [DOI] [PubMed] [Google Scholar]
- 2.Maalouf G, et al. Epidemiology of hip fractures in Lebanon: A nationwide survey. Orthopaedics & Traumatology: Surgery & Research. 2013;99:675–680. doi: 10.1016/j.otsr.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Lewiecki, M. E. et al. Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int22, 465 (2017). [DOI] [PubMed]
- 4.Ettinger B, Black DM, Dawson-Hughes B, Pressman AR, Melton LJ. Updated fracture incidence rates for the US version of FRAX. Osteoporos Int. 2010;21:25–33. doi: 10.1007/s00198-009-1032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abrahamsen B, Vestergaard P. Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997-2006. Osteoporos Int. 2010;21:373–380. doi: 10.1007/s00198-009-0957-3. [DOI] [PubMed] [Google Scholar]
- 6.Karacić TP, Kopjar B. Hip fracture incidence in Croatia in patients aged 65 years and more. Lijec Vjesn. 2009;131:9–13. [PubMed] [Google Scholar]
- 7.Leal J, et al. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 2015;27:549–558. doi: 10.1007/s00198-015-3277-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanis JA, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239–2256. doi: 10.1007/s00198-012-1964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marques, A., Lourenço, Ó., da Silva, J. A. P. & Portugal, O. B. O. T. P. W. G. F. T. S. O. T. B. O. H. F. I. The burden of osteoporotic hip fractures in Portugal: costs, health related quality of life and mortality. Osteoporos Int26, 2623–2630 (1BC). [DOI] [PubMed]
- 10.Tan LT, Wong SJ, Kwek EB. Inpatient cost for hip fracture patients managed with an orthogeriatric care model in Singapore. smedj. 2017;58:139–144. doi: 10.11622/smedj.2016065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyons, A. R. Clinical outcomes and treatment of hip fractures. Am. J. Med. 103, 51S–63S– discussion 63S–64S (1997). [DOI] [PubMed]
- 12.Panula J, et al. Mortality and cause of death in hip fracture patients aged 65 or older - a population-based study. BMC Musculoskeletal Disorders. 2011;12:105. doi: 10.1186/1471-2474-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lizaur-Utrilla A, et al. Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury. 2016;47:1530–1535. doi: 10.1016/j.injury.2016.04.040. [DOI] [PubMed] [Google Scholar]
- 14.Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1:6–14. doi: 10.1177/2151458510378105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 16.Morrison RS, Chassin MR, Siu AL. The medical consultant’s role in caring for patients with hip fracture. Ann. Intern. Med. 1998;128:1010–1020. doi: 10.7326/0003-4819-128-12_Part_1-199806150-00010. [DOI] [PubMed] [Google Scholar]
- 17.Parker M, Johansen A. Hip fracture. BMJ. 2006;333:27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury. 2008;39:1157–1163. doi: 10.1016/j.injury.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 19.Tolppanen A-M, Taipale H, Tanskanen A, Tiihonen J, Hartikainen S. Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer’s disease - exposure-matched cohort study. BMC Geriatr. 2016;16:204. doi: 10.1186/s12877-016-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haentjens P, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann. Intern. Med. 2010;152:380–390. doi: 10.7326/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silvia Andueza Robustillo, V., Juchno, P., Marcui, M. & Wronsk, A. Eurostat Demography Report - Short Analytical Web Note 3/2015. 2015.
- 22.Xu, J., Murphy, S., Kenneth, D., Kochanek, M. & Arias, E. Mortality in the United States, 2015. NCHS Data Brief, No 267. 2016. [PubMed]
- 23.OECD. Health at a Glance 2015: OECD Indicators. 1–220 (2015).
- 24.Carpintero P. Complications of hip fractures: A review. WJO. 2014;5:402–11. doi: 10.5312/wjo.v5.i4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23:131–137. doi: 10.5435/JAAOS-D-14-00432. [DOI] [PubMed] [Google Scholar]
- 26.National Guideline C. American Academy of Orthopaedic Surgeons clinical practice guideline on management of hip fractures in the elderly. 2014.
- 27.NICE. Hip fracture: management, Clinical guideline [CG124]. 2014.
- 28.Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med. 2017;377:2053–2062. doi: 10.1056/NEJMcp1611090. [DOI] [PubMed] [Google Scholar]
- 29.Orosz GM, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291:1738–1743. doi: 10.1001/jama.291.14.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parker MJ, Pryor GA. The timing of surgery for proximal femoral fractures. J Bone Joint Surg Br. 1992;74:203–205. doi: 10.1302/0301-620X.74B2.1544952. [DOI] [PubMed] [Google Scholar]
- 31.Smektala R, et al. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskeletal Disorders. 2008;9:387–9. doi: 10.1186/1471-2474-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simunovic, N. et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. 182, 1609–1616 (2010). [DOI] [PMC free article] [PubMed]
- 33.Klestil, T. et al. Immediate versus delayed surgery for hip fractures in the geriatric population. Available at: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017058216. (Accessed: 29 January 2018).
- 34.Klestil T, et al. Immediate versus delayed surgery for hip fractures in the elderly patients: a protocol for a systematic review and meta-analysis. Syst Rev. 2017;6:164. doi: 10.1186/s13643-017-0559-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klestil, T. et al. Immediate versus delayed surgery for hip fractures in the elderly patients: a protocol for a systematic review and meta-analysis. 1–7, 10.1186/s13643-017-0559-7 (2017). [DOI] [PMC free article] [PubMed]
- 36.Wells, G. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. (Accessed: 14 June 2018).
- 37.Falck-Ytter Y, Schünemann H, Guyatt G. AHRQ series commentary 1: rating the evidence in comparative effectiveness reviews. Journal of Clinical Epidemiology. 2010;63:474–475. doi: 10.1016/j.jclinepi.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 38.Zhang J, Yu K. What’s the Relative Risk? JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 39.Dailiana, Z. et al. Surgical treatment of hip fractures: factors influencing mortality. 1–6 (2017). [PMC free article] [PubMed]
- 40.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 42.Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- 43.Trpeski S, Kaftandziev I, Kjaev A. The effects of time-to-surgery on mortality in elderly patients following hip fractures. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2013;34:115–121. [PubMed] [Google Scholar]
- 44.Crego-Vita D, Sanchez-Perez C, Gomez-Rico JAO, de Arriba CC. Intracapsular hip fractures in the elderly. Do we know what is important? Injury. 2017;48:695–700. doi: 10.1016/j.injury.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 45.Rae HC, Harris IA, McEvoy L, Todorova T. Delay to surgery and mortality after hip fracture. ANZ J Surg. 2007;77:889–891. doi: 10.1111/j.1445-2197.2007.04267.x. [DOI] [PubMed] [Google Scholar]
- 46.Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123–1126. doi: 10.1302/0301-620X.87B8.16357. [DOI] [PubMed] [Google Scholar]
- 47.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? The Journal of Bone and Joint Surgery. 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 48.Dorotka R, Schoechtner H, Buchinger W. The influence of immediate surgical treatment of proximal femoral fractures on mortality and quality of life. The Journal of Bone and Joint Surgery. 2003;85:1107–1113. doi: 10.1302/0301-620X.85B8.14282. [DOI] [PubMed] [Google Scholar]
- 49.Elliott J, et al. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. Journal of Clinical Epidemiology. 2003;56:788–795. doi: 10.1016/S0895-4356(03)00129-X. [DOI] [PubMed] [Google Scholar]
- 50.Smektala R, Wenning M, Luka M. Early surgery after hip para-articular femoral fracture. Results of a prospective study of surgical timing in 161 elderly patients. Zentralbl Chir. 2000;125:744–749. doi: 10.1055/s-2000-10657. [DOI] [PubMed] [Google Scholar]
- 51.Muhm M, Arend G, Ruffing T, Winkler H. Mortality and quality of life after proximal femur fracture—effect of time until surgery and reasons for delay. Eur J Trauma Emerg Surg. 2013;39:267–275. doi: 10.1007/s00068-013-0267-5. [DOI] [PubMed] [Google Scholar]
- 52.Mariconda M, et al. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint J. 2015;97-B:383–390. doi: 10.1302/0301-620X.97B3.34504. [DOI] [PubMed] [Google Scholar]
- 53.Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Joint J. 2015;97-B:104–108. doi: 10.1302/0301-620X.97B1.35041. [DOI] [PubMed] [Google Scholar]
- 54.Hapuarachchi KS, Ahluwalia RS, Bowditch MG. Neck of femur fractures in the over 90s: a select group of patients who require prompt surgical intervention for optimal results. J Orthopaed Traumatol. 2013;15:13–19. doi: 10.1007/s10195-013-0248-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Poh KS, Lingaraj K. Complications and their risk factors following hip fracture surgery. J Orthop Surg (Hong Kong) 2013;21:154–157. doi: 10.1177/230949901302100207. [DOI] [PubMed] [Google Scholar]
- 56.Kim S-M, et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012;50:1343–1350. doi: 10.1016/j.bone.2012.02.633. [DOI] [PubMed] [Google Scholar]
- 57.Pioli G, et al. Older People With Hip Fracture and IADL Disability Require EarlierSurgery. The Journals of Gerontology Series A: Biological Sciences and Medical Science. 2012;67:1272–1277. doi: 10.1093/gerona/gls097. [DOI] [PubMed] [Google Scholar]
- 58.Vidán MT, et al. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann. Intern. Med. 2011;155:226–233. doi: 10.7326/0003-4819-155-4-201108160-00006. [DOI] [PubMed] [Google Scholar]
- 59.Oztürk A, et al. The risk factors for mortality in elderly patients with hip fractures: postoperative one-year results. smedj. 2010;51:137–143. [PubMed] [Google Scholar]
- 60.Vertelis A, Robertsson O, Tarasevicius S, Wingstrand H. Delayed hospitalization increases mortality in displaced femoral neck fracture patients. Acta Orthopaedica. 2009;80:683–686. doi: 10.3109/17453670903506666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yonezawa T, Yamazaki K, Atsumi T, Obara S. Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. Journal of Orthopaedic Science. 2009;14:566–573. doi: 10.1007/s00776-009-1380-5. [DOI] [PubMed] [Google Scholar]
- 62.Al-Ani AN, et al. Early Operation on Patients with a Hip Fracture Improved the Ability to Return to Independent Living. The Journal of Bone and Joint Surgery. 2008;90:1436–1442. doi: 10.2106/JBJS.G.00890. [DOI] [PubMed] [Google Scholar]
- 63.Butler A, Hahessy S, Condon F. The effect of time to surgery on functional ability at six weeks in a hip fracture population in Mid-West Ireland. International Journal of Orthopaedic and Trauma Nursing. 2017;26:36–42. doi: 10.1016/j.ijotn.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 64.Kelly-Pettersson P, et al. Waiting time to surgery is correlated with an increased risk of serious adverse events during hospital stay in patients with hip-fracture: A cohort study. International Journal of Nursing Studies. 2017;69:91–97. doi: 10.1016/j.ijnurstu.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 65.Maggi S, et al. A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int. 2010;21:223–231. doi: 10.1007/s00198-009-0936-8. [DOI] [PubMed] [Google Scholar]
- 66.Pajulammi HM, Pihlajamäki HK, Luukkaala TH, Nuotio MS. Pre- and perioperative predictors of changes in mobility and living arrangements after hip fracture—A population-based study. Archives of Gerontology and Geriatrics. 2015;61:182–189. doi: 10.1016/j.archger.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 67.Pajulammi, H. M., Luukkaala, T. H., Pihlajamäki, H. K. & Nuotio, M. S. Decreased glomerular filtration rate estimated by 2009 CKD-EPI equation predicts mortality in older hip fracture population. Injury 1–7, 10.1016/j.injury.2016.04.028 (2016). [DOI] [PubMed]
- 68.Pioli G, et al. Time to surgery and rehabilitation resources affect outcomes in orthogeriatric units. Archives of Gerontology and Geriatrics. 2011;55:316–322. doi: 10.1016/j.archger.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 69.Pajulammi, H. M. et al. The Effect of an In-Hospital Comprehensive Geriatric Assessment on Short-Term Mortality During Orthogeriatric Hip Fracture Program—Which Patients Benefit the Most? 8, 183–191 (2017). [DOI] [PMC free article] [PubMed]
- 70.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 71.Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: A systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40:692–697. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 72.Lawrence JE, Fountain DM, Cundall-Curry DJ, Carrothers AD. Do Patients Taking Warfarin Experience Delays to Theatre, Longer Hospital Stay, and Poorer Survival After Hip Fracture? Clin Orthop Relat Res. 2016;475:273–279. doi: 10.1007/s11999-016-5056-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Muhm, M. et al. Length of hospital stay for patients with proximal femoral fractures. 119, 560–569 (2014). [DOI] [PubMed]
- 74.Cha Y-H, et al. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Archives of Orthopaedic and Trauma Surgery. 2017;137:625–630. doi: 10.1007/s00402-017-2674-2. [DOI] [PubMed] [Google Scholar]
- 75.Hip Fracture Accelerated Surgical Treatment and Care Track (HIP ATTACK) Investigators Accelerated care versus standard care among patients with hip fracture: the HIP ATTACK pilot trial. CMAJ. 2014;186:E52–60. doi: 10.1503/cmaj.130901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during the study are available from the corresponding author on reasonable request.