Abstract
Idelalisib, a selective PI3Kδ inhibitor, has been approved by the FDA for chronic lymphocytic leukemia/small lymphocytic lymphoma treatment and for follicular lymphoma treatment when combined with rituximab. However, the mechanisms of effective action of idelalisib in hepatocellular carcinoma (HCC) remain unclear. In the current study, we aimed to investigate how idelalisib inhibits the growth of HCC cells and enhances the effects of other chemotherapeutic drugs. Our results show that idelalisib treatment promotes Bim induction in HCC via the FoxO3a pathway following PI3K/AKT inactivation. Moreover, our results show that Bim is required for idelalisib-mediated apoptosis in HCC. Idelalisib also synergizes with sorafenib or doxorubicin to induce significant apoptosis in HCC, and Bim is also necessary for the induction of apoptosis by cotreatment. Furthermore, a xenograft experiment reveals that the Bim deficiency abolishes apoptosis and antitumor effects of idelalisib in vivo. In summary, our results indicate a key role of Bim in mediating the antitumor effects of idelalisib in HCC. Our results also support the clinical significance of the drug.
Introduction
Hepatocellular carcinoma (HCC) represents the second leading cause of cancer-related deaths worldwide, especially in developing countries1,2. The incidence of HCC in developed countries is on the rise due to the progress of hepatitis C viral (HCV) infection in the elderly, as well as to alcohol consumption, the prevalence of obesity and the nonalcoholic fatty liver disease related to the metabolic syndrome2,3. Over the past few decades, the treatment of HCC has undergone significant changes, such as an introduction of liver transplantation, liver resection, systemic therapy and hepatic artery-targeted chemotherapy4,5.
Idelalisib (CAL-101 or GS-1101) belongs to a class of inhibitors of phosphatidylinositol 3 kinase delta (PI3Kδ), a cytosolic tyrosine kinase participating in various signaling pathways in B-cells6,7. Idelalisib is approved by FDA as monotherapy, or in combination with rituximab (Rituxan, for the treatment of small lymphocytic lymphoma, recurrent chronic lymphocytic leukemia (CLL) and follicular lymphoma8. However, idelalisib has side effects, such as colitis, diarrhea, severe hepatotoxicity, and intestinal perforation9,10. Idelalisib has also been found to be effective in p53-mutated CLL patients with high-risk genetic traits, which suggests the treatment of p53 deletion/mutant patients should involve screening for idelalisib11,12. However, the mechanism of autonomous effects of idelalisib, such as cell killing in solid tumors, is unclear.
Apoptosis, a process of programmed cell death, occurs in multicellular organisms and is regulated by both proapoptotic and anti-apoptotic proteins13,14. The proapoptotic protein Bim (Bcl2L11) is a Bcl-2 family member and has three major isoforms (Bim-EL, Bim-L, and Bim-S), which can be produced by alternative mRNA splicing15. Together with other proapoptotic proteins, such as Bad, Bax, PUMA, and anti-apoptotic proteins, such as Bcl-2, Bcl-XL, and Mcl-1, Bim regulates the homeostasis that is essential for normal cell death and survival15,16. Precise regulation of Bim expression has been shown to be essential for normal development17. Decreasing Bim expression can disrupt tumor suppression, accelerate tumorigenesis, and induce autoimmunity18,19.
In the current study, our results indicate that idelalisib induces Bim activation via the AKT/FoxO3a pathway, which plays a key role in therapeutic response to idelalisib in HCC.
Materials and Methods
Cell culture and drug treatment
The HCC cell lines, Hep G2, Hep3B, SNU-398, PLHC-1 and embryonic kidney 293T cells were obtained from American Type Culture Collection (ATCC, Manassas, VA, USA). HuH-7 cell line was got from Japanese Collection of Research Bioresources (JCRB), normal hepatocyte cell line HL-7702 was got from Institute of Biochemistry and Cell Biology (SIBS, CAS, Shanghai, China). All HCC cells were cultured in DMEM medium supplemented with 10% fetal bovine serum (FBS), 100 µg/mL streptomycin and 100 units/mL penicillin (Invitrogen, Carlsbad, CA, USA). The drugs, including idelalisib, sorafenib, doxorubicin (Selleckchem, Houston, TX, USA), were diluted with DMSO. Constitutively active AKT was obtained from Addgene (Cambridge, MA, USA).
CRISPR-Cas9-mediated Bim Knockout
To generate Bim knockout cells, two gRNA sequences targeting Bim were selected (5′-GACAATTGCAGCCTGCGGAG-3′; 5′-GCCCAAGAGTTGCGGCGTAT-3′). Single-stranded complementary oligos with BsmBI overhangs were generated. The LentiCRISPR v2 lentiviral vector (Addgene, Cambridge, MA, USA) was digested using FastDigest BsmBI obtained from Fermentas. The digested product was purified using the QIAquick Gel Extraction Kit (Qiagen, Germantown, MD, USA), followed by elution in EB buffer. Phosphorylation as well as annealing of the oligos was carried out using T4 polynucleotide kinase in T4 ligation Buffer (NEB, Ipswich, MA, USA). The reaction was incubated at 37 °C for 30 min, followed by 90 °C for 5 min, and finally cooled to 25 °C at a rate of 5 °C/min. The ligation reaction was carried out by mixing the oligos to be annealed, the digested LentiCRISPR v2 vector, and the Quick Ligase enzyme included in the Quick Ligase Buffer, before transformation into Stbl3 bacteria. Human 293T cells (2 × 106) were seeded on tissue culture plates (60 mm) 24 h prior to transfection. Subsequently, 1 µg of lentiviral products was mixed with pMD2G and psPAX plasmids, as well as the PolyJet agent in serum-free media. After 15-min incubation at room temperature, the mixture was slowly added to the cells. Medium containing lentiviral particles was obtained after 2 days of transfection. For lentivirus infection, 6-well plates were seeded with HepG2 cells (4–5 × 104 per well). The infected cells were selected with puromycin at a concentration of 2 µg/mL after 1 day of infection and then incubated at 37 °C and 5% CO2. For selecting a single clone, the surviving cells were seeded on a 96-well plate. Western blotting was used to confirm the knockout cells.
MTS assay
Indicated cell lines were seeded in 96-well plates at a density of 1 × 104 cells/well. After overnight incubation, various concentrations of idelalisib were added into wells and incubated for additional 72 h. The 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay was performed using the MTS assay kit (Promega, Durham, NC, USA) according to the manufacturer’s instructions. Luminescence was measured with a Wallac Victor 1420 Multilabel Counter (Perkin Elmer, Akron, OH, USA). Each assay was conducted in triplicate and repeated three times.
RNA extraction and real-time reverse transcriptase (RT) PCR
Total RNA was extracted using the TRIzol RNA Kit (Invitrogen, Carlsbad, USA) according to the manufacturer’s protocol. One µg of total RNA was used to generate cDNA using SuperScript II reverse transcriptase (Invitrogen, Carlsbad, USA). PCR was performed in triplicate using SsoFasrTM Probes Supermix (Bio-Rad) in a final reaction volume of 20 μL with gene-specific primer/probe sets, and a standard thermal cycling procedure (35 cycles) in a Bio-Rad CFX96TM real-time PCR system. Bim and β-actin levels were assessed using TaqMan Gene Expression Real-Time PCR assays. The results were expressed as the threshold cycles (Ct). The relative quantification of the target transcripts was determined by the comparative Ct method (ΔΔCt) according to the manufacturer’s protocol. The 2−ΔΔCt method was used to analyze the relative changes in gene expression. Control experiments were conducted without reverse transcription to confirm that the total RNA was not contaminated with genomic DNA. β-actin was used as an internal control gene for normalization.
Western blotting
Proteins were extracted and western blotting was performed as described previously20, with antibodies against AKT (9272, 1:1000), phospho-AKT (5012, 1:1000), Bid (2002, 1:2000), cleaved-caspase 3 (9661, 1:1000), cleaved-caspase 9 (9505, 1:1000), phospho-FoxO3a (9466, 1:1000), Bak (6947, 1:1000), FoxO3a (2497, 1:1000), cytochrome oxidase subunit IV (Cox IV) (4850, 1:2000) (Cell Signaling Technology, Beverly, CA, USA), E2F1 (sc-193, 1:1000), Egr-1 (sc-110, 1:1000), cytochrome c (sc-8385, 1:1000), β-actin (sc-1615, 1:1000), Bim (sc-11425, 1:1000) (Santa Cruz Biotechnology, Santa Cruz, CA, USA), Mcl-1 (559027, 1:1000), Bcl-2 (551097, 1:1000) and Bcl-XL (610746, 1:1000) (BD, San Jose, CA, USA).
Apoptosis assays
Apoptosis was analyzed by nuclear staining with Hoechst 33258 (Invitrogen, Carlsbad, CA, USA). Apoptosis was assessed through microscopic visualization of condensed chromatin and micronucleation. At least three independent experiments were carried out for each condition, and a minimum of 300 cells were counted in each measurement. Annexin V/propidium iodide (PI) staining was performed using annexin-Alexa 488 (Invitrogen, Carlsbad, CA, USA) and PI. For analysis of cytochrome c release, cytosolic fractions were isolated by differential centrifugation and probed by western blotting for cytochrome c. For colony formation assays, the treated cells were plated in 12-well plates at appropriate dilutions and allowed to grow for 2 weeks, followed by crystal violet staining of cell colonies.
Transfection and siRNA
Cells were transfected with Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. The knockdown experiment was performed 24 h prior to the treatment with idelalisib with 200 pmol siRNA. The scrambled siRNA and siRNA for human FoxO3a (sc-37887) were from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Chromatin immunoprecipitation (ChIP)
ChIP with FoxO3a antibody was performed using the Chromatin Immunoprecipitation Assay Kit (EMD Millipore, Burlington, MA, USA) according to the manufacturer’s instructions. The precipitates were analyzed by PCR using primers 5′-TGCCACCAAAGATCTCTACC-3′ and 5′-GCATTTCCTCACAGAGTTGG-3′ to amplify a Bim promoter fragment containing putative FoxO3a sites.
Xenograft
All animal experiments were conducted according to the relevant ethical regulations of China Medical University. WT and Bim-KO HepG2 cells were collected, and 4 × 106 cells in 0.2 mL of medium were subcutaneously implanted into the back of athymic nude female mice. After 7 days of tumor growth, mice were treated with idelalisib 30 mg/kg daily for 10 consecutive days through the oral gavage. Tumor growth was monitored with a caliper and tumor volumes were calculated according to the formula ½ × length × width2. Mice were killed when tumors reached ~1.0 cm3 in size. Tumors were dissected and fixed in 10% formalin and embedded in paraffin. TUNEL and active caspase 3 staining were performed on 5-µM paraffin-embedded tumor sections, by using an AlexaFluor 488-conjugated secondary antibody (Invitrogen, Carlsbad, USA) for signal detection. TUNEL and active caspase 3-positive cells were counted and plotted.
Statistical analysis
GraphPad Prism IV software was carried out for statistical analyses. Student’s t test was used to identify the significance of difference of two groups, and one-way analysis of variance (ANOVA) was used for multiple groups. *p < 0.05 was considered to be statistically significant. The means ± SD are shown in the figures.
Results
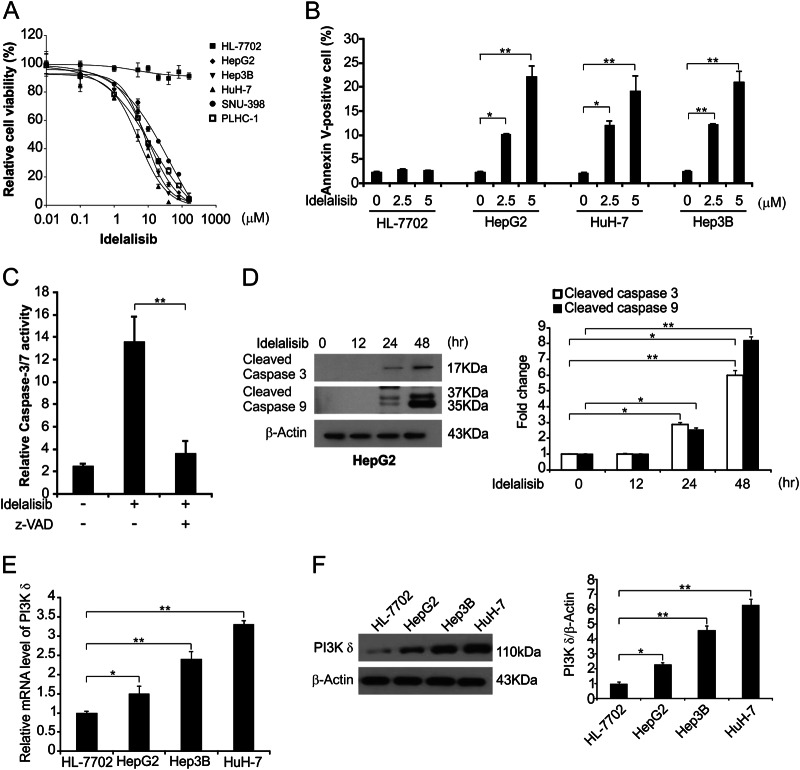
Idelalisib promotes growth inhibition and induces apoptosis in HCC cells
To investigate the effects of idelalisib on HCC, HCC cell lines were treated with increasing concentrations of idelalisib for 72 h, and cell growth was examined by the MTS assay. As shown in Fig. 1a, MTS results demonstrated that idelalisib effectively reduced viability of the HCC cell lines. We next investigated the mechanism of idelalisib-induced HCC growth inhibition in the following experiments. In apoptotic assays, we found that idelalisib upregulated the Annexin V-positive populations (Annexin V+/PI− and Annexin+/PI+) of HepG2, HuH-7, and Hep3B cells as detected by flow cytometry, but not in HL-7702 cells (Fig. 1b and Supplementary Fig. S1A). Our results also indicated that idelalisib negatively affected Annexin V−/PI+ population in these cells (Fig. 1b and Supplementary Fig. S1A). Moreover, our results indicated that idelalisib induced activation of caspases 3/7 in HepG2 cells (Fig. 1c). It was also found that the apoptotic response was blocked upon pretreatment with z-VAD-fmk, a pan-caspase inhibitor (Fig. 1c), indicating that idelalisib induced caspase-dependent apoptosis. Furthermore, idelalisib treatment also promoted activation of caspase 3 and 9 in HepG2 and Hep3B cells, but not in HL-7702 cells (Fig. 1d and Supplementary Fig. S1B and C). In addition, the expression of PI3K δ was found higher in HCC cells than HL-7702 cells (Fig. 1e and Supplementary Fig. S1D). These findings suggest that idelalisib decreased cell growth and induced caspase-dependent apoptosis in HCC.
Fig. 1. Idelalisib induces apoptosis in HCC.
a The indicated cell lines were treated with increasing concentrations of idelalisib for 72 h. Cell viability was determined by MTS assay. b The indicated cell lines were treated with idelalisib for 24 h at indicated concentrations. Apoptosis was analyzed by Annexin V/PI staining followed by flow cytometry. The results were expressed as the means ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). c HepG2 cells were treated with 5 μmol/L idelalisib with or without z-VAD-fmk, and caspase 3/7 activity was determined by fluorogenic analysis. The results were expressed as the means ± SD of three independent experiments. **P < 0.01 (Student’s t test). d HepG2 cells were treated with 5μmol/L idelalisib at indicated time point. Cleaved-caspase 3 and 9 were analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). e The expression of PI3Kδ was analyzed by real-time PCR in indicated cell lines. The results were expressed as the means ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). f The expression of PI3Kδ was analyzed by Western blotting in indicated cell lines and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test)
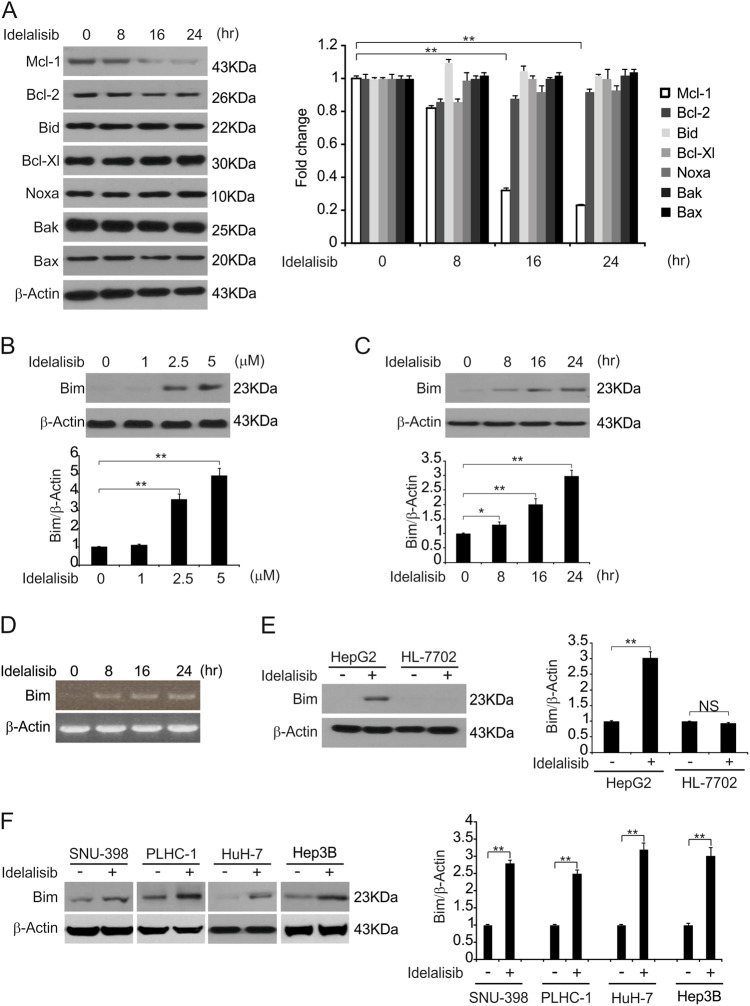
Idelalisib promotes Bim induction in HCC cells
To investigate the role of Bcl-2 family proteins in idelalisib-induced apoptosis, we treated HCC cells with idelalisib and found that it did not promote Bid, Bax and Noxa protein upregulation but did reduce the level of the anti-apoptotic proteins, such as Bcl-2 and Mcl-1 (Fig. 2a). Treating HepG2 cells with idelalisib significantly induced mRNA and protein levels of Bim in a time- and dose-dependent manner (Figs. 2b–d). Then, we investigated the effect of idelalisib on primary human liver HL-7702 cells and found that idelalisib had little effect on the growth of HL-7702 cells, and no Bim induction was detected in the cells (Figs. 1a and 2e). Moreover, Idelalisib treatment induced Bim upregulation in other HCC cell lines, including SNU-398, PLHC-1, Hep3B and HuH-7 cell lines (Fig. 2f). Our results suggest that idelalisib-induced Bim expression and Bim may contribute to the anticancer effects of idelalisib.
Fig. 2. Idelalisib enhances Bim induction in HCC.
a HepG2 cells were treated with 5 μmol/L idelalisib at indicated time points. The expression of indicated Bcl-2 family members was analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). b HepG2 cells were treated with idelalisib at indicated concentrations for 24 h. Bim expression was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). c HepG2 cells were treated with 5 μmol/L idelalisib at indicated time points. Bim expression was analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). d HepG2 cells were treated with 5 μmol/L idelalisib at indicated time points. Total RNA was extracted, and Bim mRNA expression was analyzed by semiquantitative reverse transcription PCR (RT-PCR). β-actin was used as a control. (e) HepG2 and HL-7702 cells were treated with 5 μmol/L idelalisib for 24 h. Bim expression was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01 (Student’s t-test). f Indicated HCC cell lines were treated with 5 μmol/L idelalisib for 24 h. Bim expression was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01 (Student’s t-test)
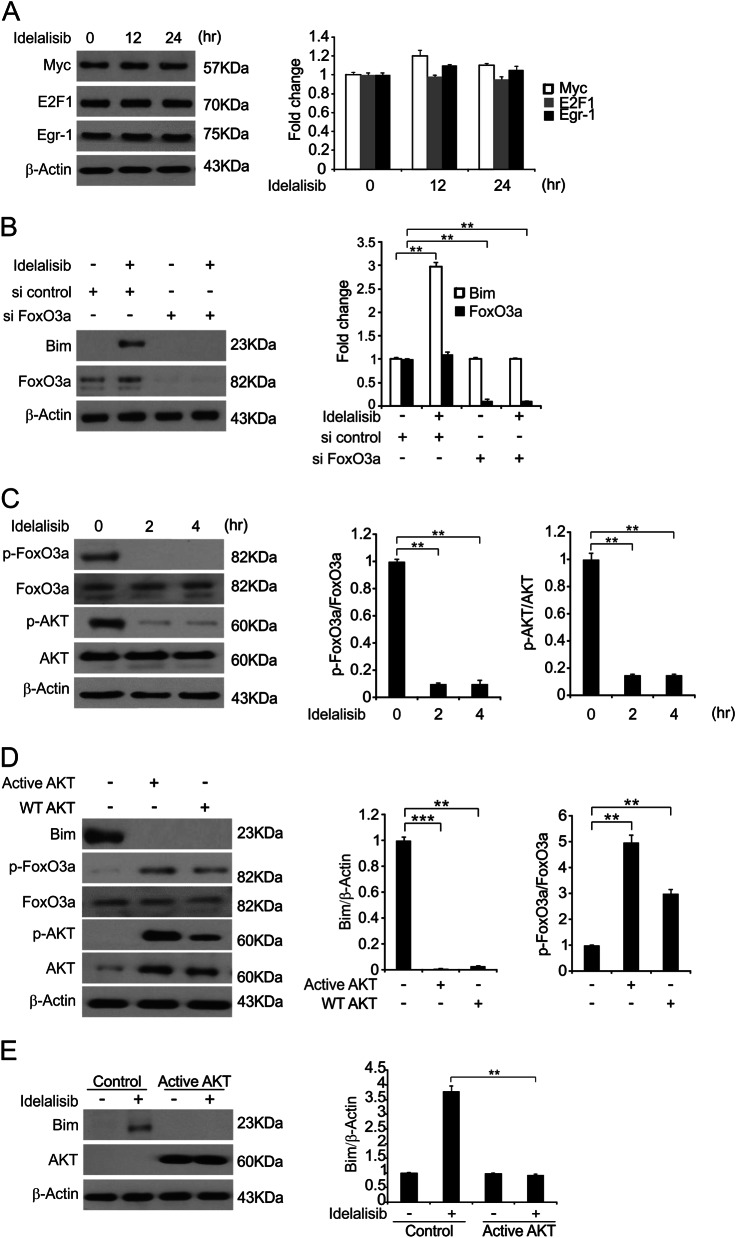
FoxO3a-mediated idelalisib-induced Bim expression
Next, we identified the Bim induction mechanism in response to idelalisib. Transcription factors, such as E2F1, Egr-1 and myc, were not involved as seen from their unchanged expression following idelalisib treatment (Fig. 3a). Previous studies showed that the transcription factor FoxO3a regulates Bim expression in response to many stimuli21,22. In addition, idelalisib inhibited AKT, which phosphorylates FoxO3a and blocks its nuclear localization. Therefore, we examined whether FoxO3a and AKT are involved in idelalisib-induced Bim expression. As shown in Fig. 3b, siRNA-mediated FoxO3a depletion in HepG2 cells abrogated Bim induction by idelalisib, suggesting that FoxO3a is required for the induction of Bim following kinase inhibition. To further test whether FoxO3a directly activates the Bim promoter, ChIP with the FoxO3a antibody was used. After treatment with idelalisib, FoxO3a binding to the Bim promoter was significantly enhanced (Supplementary Figure S2A).
Fig. 3. FoxO3a mediates idelalisib induced Bim induction.
a HepG2 cells were treated with 5 μmol/L idelalisib at indicated time point. E2F1, Egr-1 and myc expression was analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. b HepG2 cells were transfected with either a control scrambled siRNA or a FoxO3a siRNA for 24 h, and then treated with 5 μmol/L idelalisib for 24 h. FoxO3a and Bim expression was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). c HepG2 cells were treated with 5 μmol/L idelalisib for 24 h. Indicated protein expression was analyzed by western blotting and p-FoxO3a normalized to FoxO3a, p-AKT normalized to AKT. The data represent the mean ± SD of three independent experiments. **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). d HepG2 cells were transfected with WT or Active AKT plasmid for 8 h. Indicated protein expression was analyzed by western blotting and Bim was normalized to β-actin, p-FoxO3a was normalized to FoxO3a. The data represent the mean ± SD of three independent experiments. ***P < 0.001; **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). e HepG2 cells were transfected with Active AKT plasmid for 8 h, and then treated with 5 μmol/L idelalisib for 24 h. Indicated protein expression was analyzed by western blotting and Bim was normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01 (Student’s t-test)
Next, we examined whether the PI3K/AKT signaling pathway is involved in the action of idelalisib on Bim expression. Idelalisib treatment markedly inhibited AKT phosphorylation at S473 while reducing FoxO3a phosphorylation (Fig. 3c), which is known to prevent its nuclear translocation and subsequent transactivation. In contrast, transfection with WT or constitutively active AKT induced FoxO3a phosphorylation, suppressed basal Bim expression (Fig. 3d), and thus overcame the induction of Bim by idelalisib (Fig. 3e). Therefore, AKT inhibition is involved in FoxO3a-mediated Bim induction following idelalisib treatment.
Bim is required for idelalisib-induced apoptosis
To determine the functional role of Bim, we generated Bim knockout cells in HepG2 cells using CRISPR-Cas9 system (Fig. 4a). Idelalisib treatment significantly induced apoptosis in WT cells, which was significantly reduced in Bim-KO HepG2 cells (Fig. 4b). Annexin V/PI staining results confirmed that the deficiency of Bim expression in HepG2 cells abrogated idelalisib-induced apoptosis (Fig. 4c and Supplementary Figure S3A). Idelalisib treatment increased activation of caspases 3 and 9, as well as the release of cytochrome c in WT, but not Bim-KO cells (Fig. 4d, e). Moreover, after idelalisib treatment, Bim-KO cells had better survival rates than WT HepG2 cells in a long-term clonogenic assay (Fig. 4f). In addition, Bim was upregulated post idelalisib treatment in Hep3B and HuH-7 cells, and Bim is required for idelalisib-induced apoptosis in both of these cells (Supplementary Figure S3B–E). These results show that Bim is essential for the apoptotic effect of idelalisib in HCC.
Fig. 4. Bim mediates the antitumor effects of idelalisib through the mitochondrial pathway.
a The Bim expression in Bim-KO cells were analyzed by western blotting. b WT and Bim-KO HepG2 cells were treated with idelalisib at indicated concentration for 24 h. Apoptosis was analyzed by a nuclear fragmentation assay. The results were expressed as the means ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). c WT and Bim-KO HepG2 cells were treated with 5 μmol/L idelalisib for 24 h. Apoptosis was analyzed by annexin V/PI staining followed by flow cytometry. The results were expressed as the means ± SD of three independent experiments. **P < 0.01 (one-way ANOVA with Tukey’s post hoc test). d WT and Bim-KO HepG2 cells were treated with 5 μmol/L idelalisib for 24 h. Cleaved caspase 3 and 9 expression was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. *P < 0.05 (Student’s t-test). (e) The cytoplasm and mitochondria were fractionated from WT and Bim-KO HepG2 treated with 5 μmol/L idelalisib for 24 h. The distribution of cytochrome c was analyzed by western blotting and normalized to β-actin. Data represent the mean ± SD of three independent experiments. *P < 0.05 (Student’s t test). β-actin and cytochrome oxidase subunit IV (Cox IV) were analyzed as the control for loading and fractionation. f WT and Bim-KO HepG2 cells were treated with 5 μmol/L idelalisib for 24 h. Colony formation assay was done by seeding an equal number of treated cells in 12-well plates, and then staining attached cells with crystal violet 14 days later. Left, representative pictures of colonies; Right, quantification of colony numbers. The results were expressed as the means ± SD of three independent experiments. **P < 0.01 (Student’s t-test)
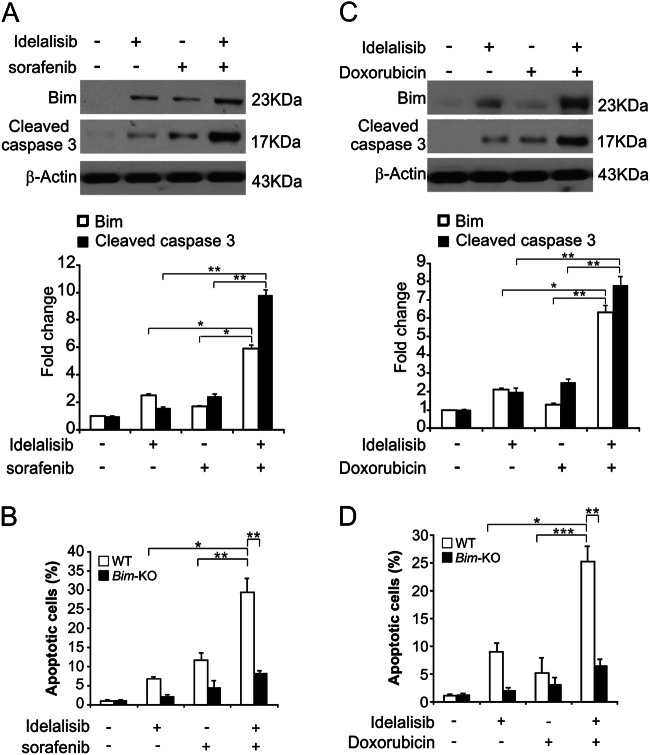
The chemosensitization effects of idelalisib is mediated by Bim
Because both idelalisib and sorafenib induce Bim-dependent apoptosis23, we checked whether chemosensitization by idelalisib is due to Bim induction. The combination of idelalisib and sorafenib induced higher levels of Bim in HepG2 cells, compared to the idelalisib or sorafenib single treatments (Fig. 5A). Moreover, the combination treatment also markedly enhanced apoptosis and cleaved-caspase 3 in WT cells (Fig. 5a, b). However, in the Bim-KO cells, the combination treatment-induced apoptosis was greatly decreased (Fig. 5b), indicating that Bim mediates its chemosensitization effect. In addition, Bim-dependent sensitization effect was also found in the cells treated with idelalisib in combination with doxorubicin (Fig. 5c). We also found that higher level of apoptosis and caspase 3 activation followed the combination treatment in WT HepG2 cells. However, the loss of Bim in HepG2 cells abolished the combination treatment-induced apoptosis and caspase 3 activation (Fig. 5c, d). These findings suggest that Bim plays a role in the chemosensitization effects of idelalisib in HCC.
Fig. 5. Idelalisib synergizes with sorafenib or doxorubicin to induce apoptosis via Bim in HCC.
a HepG2 cells were treated with 2.5 μmol/L idelalisib, 5 μmol/L sorafenib, or their combination for 24 h. Bim and Cleaved-caspase 3 expression were analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). b WT and Bim-KO HepG2 cells were treated 2.5 μmol/L idelalisib, 10 μmol/L sorafenib, or their combination for 24 h. Apoptosis was analyzed by a nuclear fragmentation assay. The results were expressed as the means ± SD of three independent experiments. **P < 0.01; *P < 0.05 (Two-way ANOVA with Tukey’s post hoc test). c HepG2 cells were treated with 2.5 μmol/L idelalisib, 5 μmol/L doxorubicin, or their combination for 24 h. Bim and Cleaved-caspase 3 expression were analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (one-way ANOVA with Tukey’s post hoc test). d WT and Bim-KO HepG2 cells were treated 2.5 μmol/L idelalisib, 5 μmol/L doxorubicin, or their combination for 24 h. Apoptosis was analyzed by a nuclear fragmentation assay. The results were expressed as the means ± SD of three independent experiments. ***P < 0.001**P < 0.01; *P < 0.05 (Two-way ANOVA with Tukey’s post hoc test)
Bim contributes to the anticancer effect of idelalisib in vivo
To determine whether Bim-mediated apoptosis is required for the anti-tumor activation of idelalisib in vivo, we established xenograft tumors in nude mice with WT and Bim-KO HepG2 cells. Tumor-bearing mice were then treated with idelalisib at 30 mg/kg or the vehicle for 10 days by oral gavage, and tumor volume was measured every 2 days. WT and Bim-KO tumors growing in the vehicle treatment group were not obviously different (Fig. 6a, b). WT tumor growth was suppressed by 70–80% following idelalisib treatment (Fig. 6a, b). However, compared with WT tumors, Bim-KO tumors were significantly insensitive to idelalisib treatment (Fig. 6a, b), suggesting that depletion of Bim abrogated the antitumor effect of idelalisib. FoxO3a phosphorylation and Bim expression were upregulated by idelalisib (Fig. 6c). As shown in Fig. 6d, e, TUNEL and cleaved-caspase 3 staining results indicated significant induction of apoptosis in idelalisib-treated parental tumors. However, in the idelalisib-treated Bim-KO tumors, weaker TUNEL and cleaved-caspase 3 stainings were detected. Furthermore, to evaluate the toxicity effects of idelalisib on mice, we detected ALT and AST upon treatment. We found that idelalisib did not influence the level of ALT or AST in serum samples (Supplementary Figure S4A and B). Therefore, the above data suggest that Bim plays a key role in the antitumor and apoptotic activity of idelalisib in vivo.
Fig. 6. Bim mediates the antitumor effects of idelalisib in vivo.
a Nude mice were injected s.c. with 5 × 106 WT and Bim-KO HepG2 cells. After 1 week, mice were treated with 30 mg/kg idelalisib or buffer for 10 consecutive days. Tumor volume at indicated time points after treatment was calculated and plotted (n = 6 in each group), **P < 0.01; *P < 0.05 (Student’s t-test). Arrows indicate idelalisib injection. b Representative tumors at the end of the experiment in (a). c WT HepG2 xenograft tumors were treated with 30 mg/kg idelalisib or the control buffer as in (a) for 4 consecutive days. Phosphor-FoxO3a and Bim in representative tumors were analyzed by western blotting and normalized to β-actin. The data represent the mean ± SD of three independent experiments. **P < 0.01; *P < 0.05 (Student’s t-test). d Paraffin-embedded sections of tumor tissues from mice treated as in (a) were analyzed by TUNEL staining. Left, representative TUNEL staining pictures; Right, TUNEL-positive cells were counted and plotted. e Tissue sections from (D) were analyzed by active caspase 3 staining. Left, representative staining pictures; Right, active caspase 3-positive cells were counted and plotted. The results of (d) and (e) were expressed as the means ± SD of 3 independent experiments. **P < 0.01 (Student’s t-test). Scale bars: 25 μm
Discussion
Idelalisib is the first in a class of delta isoform-specific, PI3-kinase inhibitors. Idelalisib targets malignant B-cell migration, survival, proliferation and homing to lymphoid tissues through a variety of mechanisms7. Our findings provide a new mechanism for the antitumor action of idelalisib. Previous studies have focused on the impact of idelalisib on cell cycle checkpoint, which is widely recognized as the primary mode of antitumor therapy24. Previous reports indicate that idelalisib enhances apoptosis through the intrinsic apoptotic pathway12,25. However, the exact mechanism of this activity is still not well-understood, and the role of apoptosis in the therapeutic response to idelalisib is still speculative. In the present study, we examined the effect of idelalisib on HCC. Our findings suggest that the therapeutic effect of idelalisib is mediated at least in part by apoptosis-induced autophagic processes that inhibit PI3K/AKT activation, which activates FoxO3a and results in the development of Bim-induced and mitochondria-dependent apoptosis. In addition, besides the Bim induction, downregulation of Bcl-2 and Mcl-1 is an early event following idelalisib treatment, which may also contribute to induction of apoptosis.
Bim is one of the Bcl-2 homology 3 (BH3-only) proteins with the ability to bind all anti-apoptotic Bcl-2 proteins with high affinity to trigger cell death26. In addition to its intrinsic toxicity, alternative splicing produces a variety of Bim isoforms with different toxicities and regulatory forms27. Among them, Bim-EL, Bim-L and Bim-S have different effects on the proapoptotic activity and have been widely studied28,29. After the discovery that Bim inhibition promotes tumor cell metastasis and chemoresistance, a large body of research has focused on its use as a cell death inducer, which is a potential target for oncology treatments.
In the current study, we found that idelalisib promotes Bim induction via AKT/FoxO3a pathway and initiates apoptosis of the HCC via the intrinsic apoptosis pathway. Bim induction plays a key role in apoptosis in response to a variety of chemotherapeutic agents and may be a useful indicator of chemosensitivity. In addition, recent studies showed that the response of isolated mitochondria from tumor cells to a peptide containing the BH3-domain of Bim is associated with chemotherapy response in patients26,28,30. Our results suggest that Bim expression can be used as a biomarker for the prediction of the antitumor effect of idelalisib in HCC.
In summary, our findings demonstrate a novel antitumor mechanism of idelalisib through Bim-mediated apoptosis. Idelalisib-induced Bim upregulation may serve as a biomarker for the clinical trials and may provide important implications for the future development and application.
Electronic supplementary material
Acknowledgements
We thank our lab members for critical reading of the manuscript. This study was supported by National Natural Science Foundation of China (81771753).
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
This article has been retracted. Please see the retraction notice for more detail:https://doi.org/10.1038/s41419-024-07162-y
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by M. Agostini
Change history
10/24/2024
This article has been retracted. Please see the Retraction Notice for more detail: 10.1038/s41419-024-07162-y
Electronic supplementary material
Supplementary Information accompanies this paper at (10.1038/s41419-018-0960-8).
References
- 1.Waller, L. P., Deshpande, V. & Pyrsopoulos, N. Hepatocellular carcinoma: a comprehensive review. World J. Hepatol.7, 2648–2663 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghouri, Y. A., Mian, I. & Rowe, J. H. Review of hepatocellular carcinoma: epidemiology, etiology, and carcinogenesis. J. Carcinog.16, 1 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Llovet, J. M. et al. Hepatocellular carcinoma. Nat. Rev. Dis. Prim.2, 16018 (2016). [DOI] [PubMed] [Google Scholar]
- 4.Raza, A. & Sood, G. K. Hepatocellular carcinoma review: current treatment, and evidence-based medicine. World J. Gastroenterol.20, 4115–4127 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsoulfas, G., Agorastou, P., Tooulias, A. & Marakis, G. N. Current and future challenges in the surgical treatment of hepatocellular carcinoma: a review. Int. Surg.99, 779–786 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrientos, J. C. Idelalisib for the treatment of indolent non-Hodgkin lymphoma: a review of its clinical potential. Onco. Targets Ther.9, 2945–2953 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheah, C. Y. & Fowler, N. H. Idelalisib in the management of lymphoma. Blood128, 331–336 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furman, R. R. et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N. Engl. J. Med.370, 997–1007 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weidner, A. S. et al. Idelalisib-associated Colitis: Histologic Findings in 14 Patients. Am. J. Surg. Pathol.39, 1661–1667 (2015). [DOI] [PubMed] [Google Scholar]
- 10.Lampson, B. L. et al. Idelalisib given front-line for treatment of chronic lymphocytic leukemia causes frequent immune-mediated hepatotoxicity. Blood128, 195–203 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang, Q., Modi, P., Newcomb, T., Queva, C. & Gandhi, V. Idelalisib: first-in-class PI3K delta inhibitor for the treatment of chronic lymphocytic leukemia, small lymphocytic leukemia, and follicular lymphoma. Clin. Cancer Res.21, 1537–1542 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang, S., Zhu, Z., Zhang, X., Zhang, N. & Yao, Z. Idelalisib induces PUMA-dependent apoptosis in colon cancer cells. Oncotarget8, 6102–6113 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ouyang, L. et al. Programmed cell death pathways in cancer: a review of apoptosis, autophagy and programmed necrosis. Cell Prolif.45, 487–498 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang, X., Chen, Y., Jenkins, L. W., Kochanek, P. M. & Clark, R. S. Bench-to-bedside review: apoptosis/programmed cell death triggered by traumatic brain injury. Crit. Care.9, 66–75 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koenig, M. N. et al. Pro-apoptotic BIM is an essential initiator of physiological endothelial cell death independent of regulation by FOXO3. Cell Death Differ.21, 1687–1695 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shamas-Din, A., Kale, J., Leber, B. & Andrews, D. W. Mechanisms of action of Bcl-2 family proteins. Cold Spring Harb. Perspect. Biol.5, a008714 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Opferman, J. T. & Kothari, A. Anti-apoptotic BCL-2 family members in development. Cell Death Differ.25, 37–45 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes, P., Bouillet, P. & Strasser, A. Role of Bim and other Bcl-2 family members in autoimmune and degenerative diseases. Curr. Dir. Autoimmun.9, 74–94 (2006). [DOI] [PubMed] [Google Scholar]
- 19.Chen, M., Huang, L. & Wang, J. Deficiency of Bim in dendritic cells contributes to overactivation of lymphocytes and autoimmunity. Blood109, 4360–4367 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li, Y. et al. Enhanced therapeutic effects against murine colon carcinoma induced by a Colon 26/Ag85A-CD226 tumor cell vaccine. Oncol. Rep.34, 1795–1804 (2015). [DOI] [PubMed] [Google Scholar]
- 21.Sunters, A. et al. FoxO3a transcriptional regulation of Bim controls apoptosis in paclitaxel-treated breast cancer cell lines. J. Biol. Chem.278, 49795–49805 (2003). [DOI] [PubMed] [Google Scholar]
- 22.Essafi, A. et al. Direct transcriptional regulation of Bim by FoxO3a mediates STI571-induced apoptosis in Bcr-Abl-expressing cells. Oncogene24, 2317–2329 (2005). [DOI] [PubMed] [Google Scholar]
- 23.Zhang, W. et al. Sorafenib induces apoptosis of AML cells via Bim-mediated activation of the intrinsic apoptotic pathway. Leukemia22, 808–818 (2008). [DOI] [PubMed] [Google Scholar]
- 24.Chen, Y. et al. Idelalisib induces G1 arrest and apoptosis in chronic myeloid leukemia K562 cells. Oncol. Rep.36, 3643–3650 (2016). [DOI] [PubMed] [Google Scholar]
- 25.Park, G. B., Hur, D. Y. & Kim, D. Combining CAL-101 with celecoxib enhances apoptosis of EBV-transformed B-Cells through MAPK-induced ER stress. Anticancer Res.35, 2699–2708 (2015). [PubMed] [Google Scholar]
- 26.Shukla, S., Saxena, S., Singh, B. K. & Kakkar, P. BH3-only protein BIM: An emerging target in chemotherapy. Eur. J. Cell Biol.96, 728–738 (2017). [DOI] [PubMed] [Google Scholar]
- 27.Zhang, L. N., Li, J. Y. & Xu, W. A review of the role of Puma, Noxa and Bim in the tumorigenesis, therapy and drug resistance of chronic lymphocytic leukemia. Cancer Gene. Ther.20, 1–7 (2013). [DOI] [PubMed] [Google Scholar]
- 28.Ruppert, S. M. et al. The major isoforms of Bim contribute to distinct biological activities that govern the processes of autophagy and apoptosis in interleukin-7 dependent lymphocytes. Biochim. Biophys. Acta1823, 1877–1893 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sionov, R. V., Vlahopoulos, S. A. & Granot, Z. Regulation of Bim in health and disease. Oncotarget6, 23058–23134 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tu, Y. S. et al. The imipridone ONC201 induces apoptosis and overcomes chemotherapy resistance by upregulation of Bim in multiple myeloma. Neoplasia19, 772–780 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.