Panniculitis is defined as inflammation of the subcutaneous tissue. Two well-known variants, morphea profunda (MP) and lupus erythematosus panniculitis (LEP), can be difficult to distinguish clinically and histologically. MP typically affects the legs, forearms, and trunk and is characterized by a bound-down inflammatory plaque or nodule with an overlying brown-red color with peau d'orange change.1 Homogenized collagen is seen throughout the dermis. LEP is characterized clinically by crops of tender, subcutaneous nodules involving the proximal extremities, trunk, face, and scalp.2 The resolved disease leaves depressed, atrophic plaques with overlying scar-like changes. Histopathologically, LEP shows extensive involvement of the dermis and subcutaneous fat with extensive periseptal and lobular lymphocytic infiltrate, hyaline necrosis, calcification, and a vacuolar interface reaction with pigment incontinence.2 Despite the epidermal involvement histopathologically, discoid lupus erythematosus (DLE) or DLE-like lesions are less commonly seen overlying LEP but may be seen at other sites.3 A major distinction of LEP from MP is the hyaline necrosis of the adipose tissue and the positive direct immunofluorescence.
We report a case of systemic scleroderma or systemic sclerosis (SSc) with LEP and distinctive DLE-like lesions. We review the literature on this rare co-occurrence and delineate some common clinical findings.
Case report
A 33-year-old Japanese man with a 7-year history of diffuse cutaneous SSc (2013 American College of Rheumatology/European League Against Rheumatism criteria for SSc4) presented with a 1.5-year history of multiple tender, indurated, subcutaneous nodules and plaques. On physical examination, there were multiple bound-down nodules and plaques with overlying mottled erythema and reticulated hyper- and hypopigmentation (Fig 1). The lesions were located over the scalp, face, chest, and trunk. Tightening of the skin was evident over the face and upper extremities.
Fig 1.
Our patient before the initiation of hydroxychloroquine.
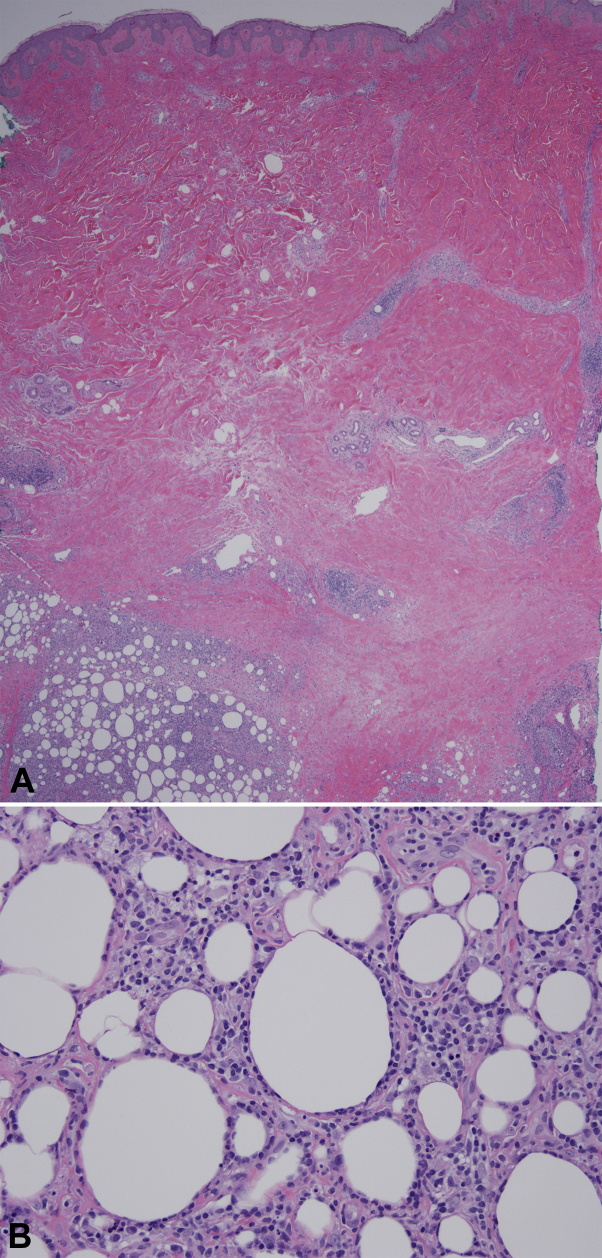
Multiple deep punch biopsy specimens were obtained for histologic and immunofluorescence studies (Fig 2, A). There was panniculitis with prominent hyaline necrosis and focal lymphoplasmacytic inflammation (Fig 2, B). The vacuolar interface changes were mild to absent in the specimens with the most prominent changes along the infundibulum of the hair follicle. While one biopsy specimen showed hyaline changes of the adipose, the other specimen showed a dense, lobular lymphocytic infiltrate with prominent rimming of adipocytes. The predominant cells were CD4+ and βF1+, and the T cell gene rearrangement was negative. There were aggregates of CD20+ cells.
Fig 2.
A, Abdomen biopsy specimen showing no vacuolar interface reaction, dense and thickened collagen bundles, and prominent lymphoplasmacytic infiltrate of the subcutaneous adipose. B, Abdomen biopsy specimen showing dense lymphoplasmacytic infiltrate with rimming. (Hematoxylin–eosin stain; original magnification: A, ×20; B, ×200.)
Direct immunofluorescence showed a strong granular basement membrane deposition of immunoglobulin M and complement component 3. Laboratory studies were positive for serum antinuclear antibodies, Scl70, and ds-DNA. A diagnosis of LEP in the setting of SSc was made. The patient did not meet the American College of Rheumatology diagnostic criteria for systemic lupus erythematosus. Hydroxychloroquine was initiated at 400 mg/day and resulted in a dramatic improvement within 3 months. The mottled hyper- and hypopigmentation persisted but there was a near total resolution of the subcutaneous nodules. The patient's SSc remained stable throughout the LEP flare.
Methods
A review of the published literature was performed using OVID Medline from 1946 to December 31, 2016 without language restrictions (keywords are listed in Supplemental Table I). The search found 237 references when the publication type was limited to case reports. The title and abstracts were reviewed for all 237 reports; 21 articles were fully reviewed. Of these, 1 was a case of SSc with underlying LEP and was included. Three additional case reports from the Japanese literature were referenced in the single case report and were translated into English for review.
All Mayo Clinic patients were searched from 1983 to September 2016 for the dual diagnoses of panniculitis and either morphea or scleroderma as determined by International Classification of Diseases, 9th revision codes 729.3 and 701.0 or 710.1. The search returned 280 possible cases; after chart review, only 1 case was included.
Discussion
SSc with LEP has rarely been reported in the literature. A total of 5 cases, including this case, have been reported with concomitant SSc and LEP (Table I)5, 6, 7, 8; a thorough search of the Mayo Clinic patient database did not return any additional cases. The mean age was 33 years (range 16-40 years) and the female to male ratio was 3:2. All patients were Japanese and had a similar clinical presentation with hyperpigmented plaques without atrophy or depression of the lesions. Four of 5 patients had a positive direct immunofluorescence for immunoglobulin M and complement component 3. One case reported had features of MP and LEP.8 However, this case lacked hyaline necrosis, had a lobular lymphocytic infiltrate with fibrosis, a positive direct immunofluorescence, and showed an interface reaction with hyalinization of superficial collagen. Taken together, this case is most fitting with LEP.
Table I.
Scleroderma and lupus panniculitis
| Reference | Sex | Age, y | Anatomic localization | Histology | DIF | Treatment | Evolution |
|---|---|---|---|---|---|---|---|
| Takahashi5 | F | 32 | Forearms, forehead, and left preauricular area | SSc and LEP | + IgM and C3 | SC | N/A |
| Arai et al6 | F | 16 | Left face and scalp | SSc and LEP | N/A | SC | Some improvement |
| Ohashi et al7 | F | 40 | Right buttocks | SSc and LEP | + IgM and C3 | Vitamin E, oral prostaglandins, and TC | No changes in skin lesion |
| Oka et al8 | M | 33 | Left buttock and left back | SSc and mixed picture of MP and LEP | + IgM and C3 | No treatment | No change over 1-year follow-up |
| Current case | M | 34 | Scalp, face, chest, and trunk | SSc and LEP | + IgM and C3 | HCQ | Near complete response |
C3, Complement component 3; F, female; HCQ, hydroxychloroquine; IgM, immunoglobulin M; LEP, lupus erythematosus panniculitis; M, male; N/A, not applicable; SC, systemic corticosteroids; SSc, systemic sclerosis; TC, topical corticosteroid.
Interestingly, all reported cases of SSc with LEP are reported in Japanese individuals. This suggests a possible genetic component to this unique phenotype. The absence of central depression likely caused by the sclerotic changes of the skin—which leads to both skin rigidity and localized ischemia because of poor vascularization—and the overlying DLE-like changes are likely related to the vacuolar interface reaction.
The treatment of SSc and LEP has been inconsistently reported. Our case showed a dramatic response to hydroxychloroquine. Two cases were treated with oral prednisolone and only 1 of the cases had clinical follow-up and showed slow improvement.5, 6 One patient was treated with topical corticosteroids for her LEP and oral prostaglandins for her SSc without improvement.7
We recommend treating LEP occurring in the setting of SSc with traditional treatments for LEP. Hydroxychloroquine is considered a first-line treatment of LEP with a near 70% response rate.3 Typical dosing is ≤5.0 mg/kg/day based on real body weight or 400 mg max daily dose.9 Chloroquine may be used as an alternative at a dose ≤2.3 mg/kg/day real body weight, around 250 mg daily. These medications are slow acting and may require up to 3 months to see improvement. Quinacrine 100 mg daily can be added to either of the above medications for recalcitrant cases.10 The addition of topical or systemic corticosteroids can be considered based on severity and morbidity. Additional immunosuppressive options can be considered in antimalarial refractory cases.
In conclusion, SSc with LEP is a rare entity that has only been described in Japanese individuals. In these cases, first-line treatment of LEP with antimalarial drugs should be considered.
Acknowledgments
We thank Cynthia A. Heltne for her library and search support and Shiori Ito for the Japanese language translation.
Footnotes
Funding sources: None.
Dr Mangold is an investigator for Pfizer and is on an advisory board for Genentech.
Presented at the 51st Annual Meeting of the American Society of Dermatopathology, Chicago, IL, November 6-9, 2014.
Appendix
Supplemental Table I.
Methods search terms
| MeSH Terms | Keywords |
|---|---|
| Scleroderma, localized | Local∗ scleroderma |
| Scleroderma, systemic | System∗ scleroderma |
| Panniculitis, lupus erythematosus | Morphea |
| Panniculitis | Scleroderma |
| Lupus erythematosus, discoid | Lupus erythematosus panniculitis |
| Lupus erythematosus, systemic | Lupus panniculitis |
| Panniculitis, nodular nonsuppurative | Panniculitis |
| Lupus profundus | |
| Discoid lupus erythematosus | |
| Systemic lupus erythematosus | |
| Nodular nonsuppurative panniculitis |
MeSH, Medical subject headings.
Indicates truncated word.
References
- 1.Onajin O., Wieland C.N., Peters M.S., Lohse C.M., Lehman J.S. Clinicopathologic and immunophenotypic features of eosinophilic fasciitis and morphea profunda: a comparative study of 27 cases. J Am Acad Dermatol. 2018;78:121–128. doi: 10.1016/j.jaad.2017.06.148. [DOI] [PubMed] [Google Scholar]
- 2.Fraga J., Garcia-Diez A. Lupus erythematosus panniculitis. Dermatol Clin. 2008;26:453–463. doi: 10.1016/j.det.2008.06.002. vi. [DOI] [PubMed] [Google Scholar]
- 3.Martens P.B., Moder K.G., Ahmed I. Lupus panniculitis: clinical perspectives from a case series. J Rheumatol. 1999;26:68–72. [PubMed] [Google Scholar]
- 4.van den Hoogen F., Khanna D., Fransen J. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2013;65:2737–2747. doi: 10.1002/art.38098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takahashi T. Lupus erythematosus profundus. Rinsho Derma (Tokyo) 1991;33:1651–1656. [in Japanese] [Google Scholar]
- 6.Arai S., Hashimoto A., Eto H., Sakaeda T. Lupus profundus observed in systemic sclerosis. Pract Dermatol. 1996;18:1011–1014. [in Japanese] [Google Scholar]
- 7.Ohashi T., Taniuchi K., Sakai H., Tsutsui K., Takehara K. Systemic scleroderma with discoid lupus erythematosus and lupus erythematosus. Rinsho Derma (Tokyo) 1997;39:1821–1824. [in Japanese] [Google Scholar]
- 8.Oka H., Tanikawa A., Matsuda F., Tanaka M., Nishikawa T. Systemic sclerosis with unusual panniculitis and overlying discoid lupus erythematosus-like lesions. J Dtsch Dermatol Ges. 2005;3:627–629. doi: 10.1111/j.1610-0387.2005.05727.x. [DOI] [PubMed] [Google Scholar]
- 9.Melles R.B., Marmor M.F. The risk of toxic retinopathy in patients on long-term hydroxychloroquine therapy. JAMA Ophthalmol. 2014;132:1453–1460. doi: 10.1001/jamaophthalmol.2014.3459. [DOI] [PubMed] [Google Scholar]
- 10.Chang A.Y., Piette E.W., Foering K.P., Tenhave T.R., Okawa J., Werth V.P. Response to antimalarial agents in cutaneous lupus erythematosus: a prospective analysis. Arch Dermatol. 2011;147:1261–1267. doi: 10.1001/archdermatol.2011.191. [DOI] [PMC free article] [PubMed] [Google Scholar]