Abstract
Introduction
Designing, delivering, and evaluating high-performing primary health care services for complex and vulnerable subpopulations are challenging endeavors. However, there is a relative paucity of research evidence available to support such work.
Objective
To provide a case study using HealthConnection Clinic, a public primary care center located in Metropolitan Vancouver’s North Shore.
Methods
Developmental evaluation approach operationalizing the 10 Building Blocks of High-Performing Primary Care framework using qualitative and quantitative methods.
Results
The clinic provided valuable insights to policymakers and researchers related to development of the Building Blocks’ foundational elements, particularly engaged leadership, empanelment, and data-driven improvement. The study highlighted the key enablers, achievements, challenges, and barriers related to operationalizing each Building Block. The Building Blocks were a useful heuristic that enabled the development and evaluation of primary care for complex subpopulations. Particularly salient from a Canadian policy perspective was the demonstration that system integration was possible when highly engaged leaders from a Regional Health Authority and a Division of Family Practice shared a common vision and purpose. HealthConnection Clinic’s entrepreneurial spirit has enabled the development of innovative, evidence-based tools such as the AMPS complexity assessment tool (attachment, medical conditions, psychological/mental health/addictions challenges, and socioeconomic status), designed to identify and assess biopsychosocial complexity and needs. The study also highlighted the importance of incorporating community orientation and equity into developmental work.
Conclusion
The study demonstrates how the Building Blocks approach can be adapted to operationalize high-performing primary care standards in settings serving complex and vulnerable populations.
INTRODUCTION
HealthConnection Clinic, a primary care center located in Metropolitan Vancouver’s North Shore area, is part of Vancouver Coastal Health (VCH), the largest by population of 6 publicly funded Regional Health Authorities in British Columbia (BC), Canada. VCH serves more than 1 million ethnically and socioeconomically diverse subpopulations living across Canada’s wealthiest and poorest postal codes. For example, VCH covers both Vancouver’s Downtown Eastside (median household income of $17,051 in 2015) and West Vancouver (median household income of $145,481 in 2015).1
Although Vancouver’s North Shore is composed of some of Canada’s wealthiest municipalities, there exists a sizable minority of people who are poor, homeless, or at risk of homelessness.2 It has been estimated that the North Shore has more than 3000 high-needs people lacking regular access to primary care (Table 1).2 These vulnerable and diverse subpopulations often forgo medical care or resort to using hospital Emergency Departments (EDs) and primary care walk-in clinics, both of which are not designed to address complex biopsychosocial needs.
Table 1.
Vancouver North Shore key statistics on homelessness, 20162
| Statistic | Numbera |
|---|---|
| Homeless individuals receiving health and social services in Vancouver’s North Shore | 736 |
| Homeless individuals accessing multiple services | 124 |
| Homeless adults aged 25–54 years | 453 |
| Homeless youth under 24 years | 103 |
| Homeless seniors 55 years and older | 178 |
| Homeless or at-risk service recipients who reported domestic violence | 136 |
| Children accompanying homeless or at-risk parent or parents | 143 |
| Unique individuals who accessed homelessness services in 2016 and were considered at risk because of imminent risk of housing loss | 295 |
| Number (%) of the absolutely homeless population that accessed HealthConnection Clinic in 2016 | 366 (50) |
Unless otherwise indicated.
Founding and Development of HealthConnection Clinic
In 2011 to 2012, a group of general practitioners (GPs) who had launched the Division of Family Practice (DFP) on the North Shore, VCH Health Authority staff, and local community agencies identified the need to work together to address the issue of unmet primary care needs for North Shore’s most vulnerable and disenfranchised subpopulations.3 The working group prepared a business plan for the development of a high-needs clinic and engaged with community agencies and partners, homeless shelters, and community mental health associations to design and help staff the clinic.3
Despite asking for relatively few resources, the business plan initially had no traction with the Health Authority. The work group therefore leveraged unused funds from other initiatives and formed the clinic with borrowed underused space from the Health Authority, with no means of sustainable funding.3 The team worked carefully to brand the clinic and collaboratively developed a unique logo (Figure 1).
Figure 1.
Logo of HealthConnection Clinic.
HealthConnection Clinic Key Statistics.
Health care providers: Three GPs (0.6 FTE total), 3 NPs (2.5 FTEs total), a Social Services Support Coordinator (1.0 FTE), a chronic disease Nurse Coordinator (0.2 FTE), a half-time Team Lead, and 2 Medical Office Assistants (2.0 FTE total)
Number of unique clients marked as “active” in the EMR, with at least one care encounter: 948 (55.6% male; 43.8% female; 0.5% transgender; 0.1% unknown)
Mean age of “active” clients: 53 years (range = 0 to < 90 years)
Total visits: 10,337 (28% walk-in, 11% home visit, 25% consult, 1.1% outreach)a
Average visits per client: 8.75 (range = 1–159 visits)a
Opioid addiction: 2.1%a
Clients with 1 or more diagnoses of diabetes, COPD, or CHF: 13.6%a
Referrals to specialists: 1272 referrals for 377 unique clients (mean = 3.4 referrals per client, range = 1–26 referrals)a
Data from past 2 years, as of October 2017. Data sourced from Intrahealth Profile Electronic Medical Record (EMR; Intrahealth Systems Ltd, Vancouver, British Columbia, Canada). Note that there is a high possibility of underreporting figures because of coding issues.
CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; FTE = full-time equivalent; GP = general practitioner; NP = nurse practitioner.
In July 2013, the clinic opened as a drop-in service (weekday mornings), using space that was not designed for primary care. Although the layout of the clinic’s rooms was not ideal (eg, examination rooms did not have sinks), the space was in a storefront location that was accessible.3 Funding was available to equip each room with necessary infrastructure and equipment, and to install hand hygiene stations. The HealthConnection Clinic management visited an existing Health Authority clinic in Vancouver to better understand essential equipment, staffing, safety, and infection control requirements. (HealthConnection Clinic was accredited in 2016 and scored high on all areas.)
In inception, HealthConnection Clinic was able to access one-time-only funding for GP fees and a Medical Office Assistant and was able to redeploy the one community nurse practitioner (NP) doing community outreach to the clinic. Community agencies were also approached to staff the clinic with social work and outreach supports. Physicians are funded through sessional payments, whereas NPs and other allied health staff are on salary from the Health Authority.
In 2015, a provincial initiative supported by the DFP provided grants to enable the clinic to open in the afternoons, to employ more GP time, and to hire a Social Services Support Coordinator. Sustainable operational funding to support clinical and administrative staffing was secured in 2016 to 2017 ($435,000), although access to the clinic space remains uncertain. This funding was supplemented by NP funding that came from the provincial government’s Nurse Practitioners for BC (NP4BC) initiative. This NP divides her time between HealthConnection Clinic (0.8 full-time equivalent [FTE]) and 2 newly developed primary care clinics, modeled in part on HealthConnection Clinic, in 2 First Nations communities on the North Shore (0.2 FTE).
Population and Service Delivery Model
HealthConnection Clinic is officially mandated to serve its jurisdiction’s unattached clients (ie, clients not rostered to or without regular access to a primary care clinic or clinician) who have complex biopsychosocial needs. In the early days of operation, nearly half of all clients came from homeless shelters and nongovernmental organizations, resulting from the broad and inclusive engagement strategy with community partners.3 HealthConnection Clinic worked with the shelter’s outreach and community mental health workers, who would accompany clients to the clinic, giving a warm handoff. This enabled clinic staff to garner a more holistic understanding of clients’ needs and backgrounds, and to engage with them in a way that enabled longitudinal relationships. Physicians in the ED also started referring clients, as they found the clinic to be an accessible and appropriate service delivery model.
To ensure the clinic was serving the right population, HealthConnection Clinic created the “AMPS tool” to assess clients’ biopsychosocial complexity profile; AMPS stands for Attachment, Medical conditions, Psychological/mental health/addictions challenges, and Socioeconomic status.4–6 The AMPS tool was based on the Minnesota Complexity Assessment Method and was integrated into the Health Authority’s electronic medical record (EMR), providing a standard that enables clinicians to assess patient complexity and develop individualized care plans.4
To suit the clinic’s context, there is a heavy focus on psychiatric, mental health, addiction, and social domains. The “attachment” component aligns to national and provincial policies related to rostering patients with primary care clinicians, which is particularly important for complex subpopulations.7 It should be noted that AMPS items are meant to function interdependently of each other, to enable a contextualized approach to care delivery. The AMPS tool and user guide is freely available for download online.4–6
To integrate the social determinants of health and to enable intersectoral coordination, HealthConnection Clinic recruited a former outreach worker at a nongovernmental organization to fill the Social Services Support Coordinator position.3 Additionally, the clinic provides home visits to unattached housebound clients as well as outreach services to homeless clients.2
HealthConnection Clinic benchmarks 30-minute visits per client per primary care clinician and up to 60 minutes per social services support worker. Very-complex-needs clients can be booked for appointments that exceed an hour with a primary care clinician. The BC Practice Support Program was leveraged to establish standardized clinic processes and workflows. Some descriptive statistics of the population and service delivery model are highlighted in the Sidebar: HealthConnection Clinic Key Statistics.
Aligning with the Broader Policy Context
From its inception, HealthConnection Clinic designed and conducted evaluations to assess its performance and to enable quality improvement, using the Triple Aim framework.8 As of April 2016, the clinic received sustainable funding from the Health Authority, with the continued proviso of evaluating results.3 Furthermore, HealthConnection Clinic is part of a primary care network (PCN), a BC provincial initiative that aims to integrate primary care and home and community care services for complex subpopulations.9 Being part of a PCN enables the clinic to engage with other patient medical homes in the community, to optimize and align planning and strategy functions, share resources, and to participate in quality improvement initiatives.
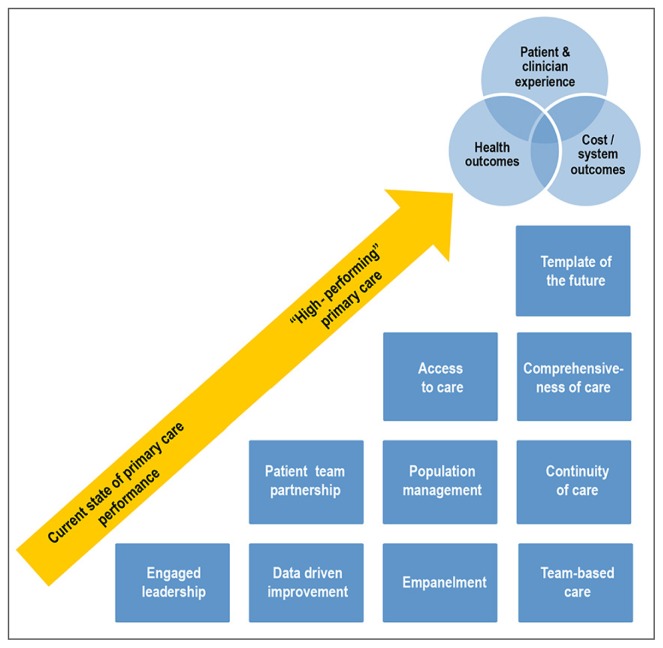
HealthConnection Clinic is guiding its ongoing development using the University of California, San Francisco’s 10 Building Blocks of High-Performing Primary Care approach, which provides a useful heuristic enabling a systematic approach to the ongoing development and evaluation of the clinic as a primary care home.9,10 Figure 2 illustrates the use of the Building Blocks as a heuristic guiding the clinic’s developmental transition, toward manifesting high-performing primary care and achievement of the Triple Aim.10
Figure 2.
Developmental transition of HealthConnection Clinic.a
a Equity is a cross-cutting domain (ie, across the 10 Building Blocks and the Triple Aim).
Despite growing policy and research interest, there has been relatively little attention or resources devoted to operationalizing and evaluating the Building Blocks and the patient-centered medical home (PCMH) models in public community health center settings.11–16 Such research is particularly salient in light of recent proposals for major expansions of community health centers (CHCs) in the US.17
This article contributes to such desired knowledge, by providing a contextual narrative of the development of HealthConnection Clinic and a systematic descriptive evaluation of its content (ie, structures and processes) using the Building Blocks as a framework.10 Together, the content and context will provide useful and meaningful insights for policymakers, administrators, providers, and academics interested in operationalizing and evaluating primary care serving complex subpopulations. The level of detail provided offers useful information for stakeholders involved in the design and evaluation of CHCs—a blueprint of mechanics (ie, structures and processes) as well as a synthesis of key innovations and challenges.18 We hope that this article will fill a major gap in the health services research literature.
METHODS
The study was based on a developmental evaluation approach, with the VCH Regional Primary Care Evaluator embedded as part of the HealthConnection Clinic team, from March to December 2017. The developmental evaluation was underpinned and guided by the University of California, San Francisco’s Center for Excellence framework in Primary Care’s 10 Building Blocks of High-Performing Primary Care.10
The framework was operationalized using both qualitative and quantitative data. Qualitative data were gathered using participative observation, document analysis, emails, and a series of meetings and iterative analytical processes with clinic team members. Quantitative data regarding the clinic’s client population and health care utilization were derived from the primary care EMR (Intrahealth Profile EMR, Intrahealth Systems Ltd, Vancouver, British Columbia, Canada), the Patient Automated Records Information Systems (PARIS Home and Community Care EMR), and hospital administrative databases. These databases were queried by VCH’s Decision Support Team and Practice Support Program, to generate simple descriptive statistics (Tables 2, 3, and 4). Quantitative patient experience data were derived using VCH’s client experience survey tool, which was developed using the BC PREMS (Patient Reported Experience Measures) Steering Committee’s indicator bank.
Table 2.
AMPS complexity score breakdown by age rangea
| Active patients with complexity score in last 12 months (December 2017) | AMPS complexity score (maximum possible points) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, years | Male | Female | Total | Total (33) | A: Attachment (3) | M: Medical (6) | P: Psychiatric-mental health-addictions (12) | S: Social support (12) | |||||
| Mean | Median | Mean | Median | Mean | Median | Mean | Median | Mean | Median | ||||
| Total | 73 | 55 | 128 | 14.38 | 14 | 1.84 | 2 | 2.78 | 3 | 5.36 | 5 | 4.40 | 4 |
| 0–20 | 0 | 1 | 1 | 3 | 3 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 20–29 | 10 | 5 | 15 | 13.67 | 15 | 2 | 1 | 1.20 | 0 | 6.40 | 7 | 4.13 | 4 |
| 30–39 | 7 | 10 | 17 | 12.71 | 13 | 1.88 | 2 | 1.53 | 1 | 5.12 | 5 | 4.18 | 4 |
| 40–49 | 19 | 8 | 27 | 16.00 | 14 | 1.59 | 1 | 2.89 | 3 | 6.52 | 6 | 5.00 | 5 |
| 50–59 | 15 | 12 | 27 | 14.89 | 15 | 1.93 | 2 | 3.30 | 4 | 5.63 | 5 | 4.04 | 4 |
| 60–69 | 15 | 11 | 26 | 15.62 | 14.50 | 1.88 | 2.50 | 3.35 | 3.50 | 5.12 | 5 | 5.27 | 5 |
| ≥ 70 | 7 | 8 | 15 | 11.73 | 11 | 1.80 | 2 | 3.87 | 4 | 2.80 | 3 | 3.27 | 3 |
Source: Intrahealth Profile electronic medical record (EMR; Intrahealth Systems Ltd, Vancouver, British Columbia, Canada).
Table 3.
AMPS complexity score breakdown by sexa
| Sex | AMPS complexity score (maximum points possible) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (33) | A: Attachment (3) | M: Medical (6) | P: Psychiatric-mental health-addictions (12) | S: Social support (12) | ||||||
| Mean | Median | Mean | Median | Mean | Median | Mean | Median | Mean | Median | |
| Total (N = 128) | 14.38 | 14 | 1.84 | 2 | 2.78 | 3 | 5.36 | 5 | 4.40 | 4 |
| Male (n = 73) | 15.67 | 9 | 1.86 | 2 | 2.89 | 3 | 5.82 | 3 | 5.1 | 5 |
| Female (n = 55) | 12.65 | 14 | 1.8 | 2 | 2.64 | 3 | 4.75 | 5 | 3.47 | 3 |
Source: Intrahealth Profile electronic medical record (EMR; Intrahealth Systems Ltd, Vancouver, British Columbia, Canada).
Table 4.
Health care utilization indicators for HealthConnection Clinic clients
| Utilization indicator | % change in 2017 vs 2016 |
|---|---|
| Home health/home support visits (case management, nursing, occupational therapy, and physiotherapy) | +48.7 |
| Emergency Department (ED) visits | −2.9 |
| ED visits with admission (Canadian Triage and Acuity Scale 4 and 5) | −13.5 |
| Hospital admissions | −12.7 |
| Average length of stay per admission | −11.8 |
Themes and data were organized and synthesized according to the key primary care system domains of the 10 Building Blocks framework, using thematic content analysis where appropriate. Data were input and updated into a central document, and were triangulated by each team member using the track changes feature of a word processing program (MS Word, Microsoft, Redmond, WA). The final draft was reviewed by the clinic’s team for accuracy and completeness.
RESULTS
Leadership and Governance
Although officially designated as a Health Authority clinic, the HealthConnection Clinic originated as, and remains, a formal collaboration between the North Shore DFP and VCH. The joint governance is operationalized through the Collaborative Services Committee, in which the senior leadership of both groups meet to collaboratively address key issues.
At an organizational level, a Health Authority Manager and DFP physician were the key players in the original design, implementation, and ongoing management of the clinic. Whereas HealthConnection Clinic is accountable for staffing, financials, safety, and client relations to the Health Authority, the GP component is accountable to the DFP. A Health Authority Manager and half-time (0.5 FTE) Team Lead oversee the clinic operations in consultation with a Medical Director from the DFP. Staff at HealthConnection Clinic address standardization of practices, use of the EMR’s components, billing procedures, and administrative office processes on a quality improvement basis. Clinical leadership and governance is provided by a DFP physician and the clinic’s NPs.
Community governance is central to the clinic, with community partners formally engaged from the outset in relation to the design, organization, staffing, and delivery of services. A Patient Advisory Committee provides feedback, used to improve clinic operations.
Team-Based Care
Services at the clinic are delivered by a multidisciplinary team, as mentioned in the Sidebar: “HealthConnection Clinic Key Statistics.” The Social Services Support Coordinator is frequently the first person seen by clients, which opens a window of opportunity to encourage clients to receive care from the GP or NP, who subsequently engage the required allied professionals.
The multidisciplinary team is designed to be person-oriented, and is therefore oriented around problems and needs rather than functions or roles. The team structure is flexible and inclusive, encouraging collaboration, sharing of ideas, and utilization of all staff. Team members work to full scope (eg, NPs are able to prescribe controlled drugs such as analgesics or buprenorphine-naloxone [Suboxone]), and they collaborate to consolidate extremely complex medical histories and to design appropriate care plans.19 A strength deployment inventory (half-day session consisting of a professional facilitator and brief standardized assessment tools) was used to help the team understand the value and contribution of each member and to explore optimal mechanisms of teamwork and collaboration. Also, HealthConnection Clinic plans to use its EMR data (eg, length and type of visit; AMPS scores) to rigorously optimize staffing ratios and teamwork relative to patient complexity.
As a prototype PCN, HealthConnection Clinic has home-visiting NPs collaborate with a multidisciplinary team of home and community care providers who include nursing support, occupational therapists, physiotherapists, a social worker, a dietitian, a pharmacist, and a program assistant.
The Panel
Attaching people to primary care is a pan-Canadian priority and is particularly important for complex and vulnerable subpopulations.17–21 HealthConnection Clinic supports this priority by providing supportive, low-barrier primary care for unattached residents with complex needs. Identifying and attaching such patients to primary care is particularly challenging because of the chaotic nature of these patients’ lives, along with the transitory nature of their housing situations.
HealthConnection Clinic designed the AMPS tool to accurately assess and address the complex biopsychosocial needs of the subpopulations it serves.4 The AMPS scores help inform clinical judgment regarding which individuals to consider as having appropriately complex needs for the clinic (a total score of at least 13 of 33 is generally perceived to be a threshold for attachment) and to enable care planning functions and evaluation.6 Tables 2 and 3 show disaggregated descriptive statistics of AMPS scores for active clinic patients.
Attachment is ultimately enabled through empanelment, which is one of the 10 Building Blocks of Primary Care and a prerequisite for basic functions related to population health needs planning, performance assessment, and quality improvement.10,22 The Health Authority is currently in the process of developing standards for empanelment, for example, assigning most responsible clinician (referred to as Most Responsible Provider [MRP] in Intrahealth EMR) and point of service in the EMR. Assigning point of service is challenging because the EMR is shared across all the Health Authority’s owned and operated primary care clinics (eg, transient clients may use multiple services by different clinicians at different Health Authority clinics). Assigning MRP is also challenging because nonclinical staff (eg, the Social Services Support Coordinator) are often the de facto MRP for patients with highly complex needs who are averse to or refuse medical care.
Data-Driven Improvement and Population Management
Data sources to inform data-driven improvement include Intrahealth Profile EMR, PARIS, and hospital databases. Substantial attention and resources are being devoted toward standardizing EMR data entry rules and evidence-based clinical workflow processes. The EMR and administrative data sources, along with standardized organizational, health care team, and patient experience surveys are being used to operationalize a Triple Aim-oriented evaluation framework. Results from an inaugural VCH patient experience survey are undergoing evaluation for quality improvement purposes. The commitment to rigorous, comprehensive, and standardized evaluation is supported by the sustainable funding that was obtained as of 2016. The Health Authority is currently in discussions with the Doctors of BC to explore the possibility of adapting the provincial patient medical home Self-Assessment Tool (BC’s version of the University of California, San Francisco’s Building Blocks of Primary Care Self-Assessment Tool), to better suit the unique context of public CHCs.
The Health Authority is also developing standardized workflows for high-priority clinical conditions such as HIV, hepatitis C, type 2 diabetes, chronic obstructive pulmonary disease, depression, and psychosis. Currently, HealthConnection Clinic is in the early stages of developing standards around opioids and addiction, and is anticipating introduction of opioid agonist therapy as a maintenance service to patients over the coming months.
Access
HealthConnection Clinic has designed its service delivery model with specific attention to cross-cutting dimensions of access.20 The storefront location clinic is accessible to those with disabilities and is open weekdays. The mornings are for walk-ins, whereas appointments are available during afternoons. The clinic is close to the local hospital and is in the downtown area, close to public transit and police. Waiting rooms have magazines, adult coloring books, food, coffee, and water. During special seasons such as Christmas, cards and other games and activities are made available.
If the clinic is busy in the mornings, clients are triaged and offered appointments that afternoon or the next day. Two afternoons a month are reserved for staff meetings and administrative purposes. Because of a lack of funding, no after-hours, weekends, or holiday services are available; however, the clinic has opened during statutory holidays for half-days on occasion to reduce ED utilization surges.
Homebound patients are seen by an NP, the Social Services Support Coordinator, and the PCN team as needed; furthermore, NPs, the Social Services Support Coordinator, and community agency outreach workers visit areas where homeless people are located.
Comprehensiveness
HealthConnection Clinic provides comprehensive primary care services addressing the complex biopsychosocial needs and challenges of their clients (ie, housing, food security, nutrition, addictions, social isolation), supported by the multidisciplinary composition of the team. The clinic offers standard health promotion and illness prevention services, primary care for minor or episodic illnesses, primary reproductive care, chronic disease management, mental health and substance use services, and coordination and access to rehabilitation, as well as support for hospital, home, and long-term facility care and support for terminally ill individuals. HealthConnection Clinic is commencing a formal partnership with the Health Authority’s Mental Health and Substance Use Program to integrate mental health services on-site for clients (eg, opioid agonist therapy).
Also, HealthConnection Clinic accesses local community-based chronic disease management and public health services. Some chronic disease management services have also coordinated with the clinic so they can arrange to see clients on-site. This removes access barriers and enables clients to receive these services in a familiar, trusted, and safe setting.
Coordination
Coordination of care is a challenging yet critical function of the clinic. Clients with extremely complex and continuously changing biopsychosocial problems receive care from a large number of multidisciplinary clinicians cutting across oft-siloed sectors. The BC Provincial eHealth Viewer, CareConnect, which is embedded in the EMR system, is potentially especially useful, because it enables clinicians to understand health care utilization of patients. CareConnect could enable better coordination of care across sectors, because it is an online portal that provides authorized caregivers a secure, view-only access to integrated clinical information from various sources, including provincial laboratory results), diagnostic imaging, hospital encounters, community summaries (PARIS), and PharmaNet (the provincial drug information and claims processing system that links all community pharmacies in BC).
HealthConnection Clinic continues to strengthen processes related to coordination with hospitals (eg, discharge planning, medication reconciliation); community-based programs (eg, use of PARIS, PCN initiative, and the “Care Conferencing” function); mental health and substance use programs (ie, integration with outreach teams for clients with addictions); public health services (eg, harm reduction, naloxone programs); community agencies and nongovernmental organizations; and other CHCs and private-community GPs.
Continuity
Maintaining continuity of care for clients with highly complex needs is extremely important and challenging.23 Many of the clinic’s clients are transient and receive different services from different clinicians across the Health Authority (and even other Regional Health Authorities). HealthConnection Clinic has processes in place to ensure routine follow-up with the vulnerable subpopulations it serves, such as homebound and homeless individuals. Systematic and routine follow-ups are performed for critical planned care functions for patients with hepatitis C and HIV. The Health Authority is currently developing standards for empanelment, which will enhance continuity of care.
Patient-Team Partnership
Patient engagement, let alone activation and empowerment, is difficult for many of the clinic’s patients. For many patients, traditional goal-setting approaches are not realistic, appropriate, or desirable. HealthConnection Clinic promotes the use of approaches that are sensitive to the contexts of patients’ lives, which are often chaotic and precarious. For example, the clinic does have a chronic conditions nurse who has the ability to provide self-management guidance and supports; however, these functions are often not appropriate for clients with highly complex needs. Enabling patient adherence and compliance is a challenge, often achieved by having clients come in almost daily for medications (eg, pain) or to do certain tests (eg, urinalysis). After-visit summaries are provided to patients verbally and are printed out if requested. Longitudinal relationships with the NP have enabled successful chronic disease management for some patients.
In addition, the clinic holds inclusive group and self-help activities (eg, for pain) that aim to indirectly support the patient-team partnership. There have also been a number of fun events around holidays, which pull people together in an intentional community. The team also prepares meals for clients, helps create activities for clients to engage in when waiting in the waiting room, and most recently has invited a small group of regular clients to have a meal with the team. The clinic has a Patient Advisory Committee, conducts patient experience surveys and interviews, and has a suggestion box.
Health Care Utilization (System Outcomes)
The VCH Decision Support Team provides access to updated statistics of the utilization of HealthConnection Clinic’s clients of home and community care and hospital (ED and inpatient) services, by querying the respective hospital administrative databases. These metrics are useful proxy indicators of the profile of patients and the potential impact of primary care services over time. Indicators that are routinely reported are volumes and intensity of home health services by discipline (eg, case management, nursing, social work, occupational therapy, physiotherapy); ED visits (eg, disaggregated by admission status, Canadian Triage and Acuity Scale, Chief Complaint, Family Practice Sensitive Conditions), and hospital admissions indicators (eg, alternate level of care, length of stay), as shown in Table 4.
DISCUSSION
This study demonstrates how the 10 Building Blocks of High-Performing Primary Care can be adapted to inform the development and evaluation of primary care for complex subpopulations. Vancouver’s HealthConnection Clinic is reaching a mature state of primary care development and provides valuable insights related to the development of foundational elements of the Building Blocks framework, particularly engaged leadership, empanelment, and data-driven improvement.10
Engaged Leadership
HealthConnection Clinic represents what is possible when highly engaged leadership from a Health Authority and DFP share a common vision and purpose.3 The clinic highlights an alternative to the generic problems that Canadian policymakers, administrators, and clinicians face when attempting to integrate multisectoral services cutting across differing governance, funding, and accountability streams.24 It demonstrates that a satisfactory degree of integrated person-oriented primary care can be achieved within the confines and limitations of the current system.
Unlike the common practice of most shared governance endeavors, the leadership of both the Health Authority and DFP purposefully chose to delay a formal memorandum of understanding. Rather than basing their partnership understanding in a bureaucratic or legal document, they relied on mutual trust, honest communication, and a profound respect for one another. Although the leadership team recognized that a memorandum of understanding is useful to limit liability, the leaders recognized that successful integration would only be truly possible if they were willing to take a certain degree of risk. The risk was tempered by a high level of trust and a mutual understanding of institutional and regulatory requirements and boundaries.
Rather than being risk-averse, the archetypal attribute of bureaucratic governance, the leadership team exhibited classic attributes of entrepreneurialism: A willingness to take risk, goal orientation, creativity, resourcefulness, confidence, flexibility, adaptability, self-reflexivity, learning, inclusivity, and an interest in promoting and marketing the HealthConnection Clinic brand (Figure 2).
The leadership team shared a clear purpose and vision relating to effectively addressing the unmet biopsychosocial needs of highly complex, vulnerable, and marginalized subpopulations. They recognized the need to think outside the box; they were therefore keen on leveraging and adapting available resources, and engaging and coordinating with diverse multisectoral and local community partners. This study provides an example of how the PCMH can be operationalized as a community-based strategy.25 Evaluation, continuous reflection, and learning were, and remain, cornerstones of the evidence-based development of the clinic.
The Panel: Identifying and Assessing Biopsychosocial Complexity and Needs
The entrepreneurial attributes of the leadership team were underpinned by a genuine drive to meet the needs of their clientele—their panel. It was therefore critical to develop effective and efficient mechanisms to identify appropriate clients, encourage their enrollment, and to comprehensively and accurately understand their complex biopsychosocial needs.
Vulnerable populations are often the hardest to find and identify; therefore, the clinic was designed to operationalize low barriers to accessibility. It is within walking distance of the local hospital, which has enabled ED physicians to make effective referrals. The leadership engaged with homeless shelters and nongovernmental organizations, whose workers would accompany clients to the clinic. This personalized approach enabled clinicians to garner a holistic understanding of clients’ needs, to develop longitudinal relationships, and to coordinate with other service providers.
Understanding the nature of the clinic panel’s needs remains a priority of the clinic. Assessing patients’ biopsychosocial complexity using a standardized and consistent approach is critical in HealthConnection Clinic, because it serves a population labeled as highly complex, often with a history of challenging patient-clinician relationships (eg, the difficult patient who has been recently “fired” by his/her GP). Such patients are often described as overserviced but underserved. However, it is important to note that it is perceived that many clients presenting at the clinic are both underserved and underserviced.
After reviewing the scientific literature on the measurement and assessment of patient complexity, the leadership team found that published research to be scant. The leadership team decided to adapt the Minnesota Complexity Assessment Method to suit HealthConnection Clinic’s needs, resulting in the development of the AMPS tool.4,6,26 The AMPS tool is now embedded as a standardized form in the Health Authority’s EMR system and is being tested across its clinics. Composite and disaggregated AMPS complexity scores are used to assess service utilization and to inform evaluation, planning, and design functions.
Rostering and Empanelment
The AMPS complexity scores can also inform the formal processes of EMR rostering and empanelment. The Health Authority’s empanelment work is building on the guidance of BC’s Practice Support Program, the University of California’s Center for Health Quality and Innovation and Center for Excellence in Primary Care (“Tools for Transformation”), and the Safety Net Medical Home Initiative empanelment resources.24–28 The Health Authority has also leveraged empanelment research by the Ontario Association of Health Centers.29,30 The recent attention to empanelment by the Federally Qualified Community Health Centers has yielded valuable insights and is encouraging.22
Like the Ontario Association of Health Centers, the Health Authority has learned that empanelment processes for its system of public primary care clinics are more complicated than for community GP settings.22 First, the Health Authority must consider the transient nature of patients with highly complex needs. These patients are often difficult to follow-up with and may access several of the Health Authority’s clinics. Although this is a positive sign of low-barrier care, it renders aspects of continuity and “longitudinality” of care (continuity over time) challenging. The lack of integration with the community GPs’ EMRs also makes it difficult, if not impossible, to accurately assess utilization to inform empanelment decisions.
The experience of HealthConnection Clinic also challenges the notion of having to designate an MRP, which is found in much of the contemporary primary care literature. Designations of MRP in the clinic can be rather arbitrary, because the whole of the team supports clients. Furthermore, nonclinical staff may be the de facto MRPs; for example, the Social Services Support Coordinator often has the most comprehensive relationship with clients who are either reluctant to receive medical care or refuse it outright.
The concept of MRP within the context of CHCs serving complex subpopulations warrants further research and policy attention. Studies have demonstrated that CHC patients receive higher quality care when they have a regular provider and that continuity with the CHC and with a specific clinician is associated with increased levels of appropriate preventive ambulatory care.31–33
Data-Driven Improvement
The clinic and Health Authority in general are focusing on the development and testing of data and measurement standards to systematically assess primary care performance. The priorities are to 1) develop EMR standards for panel management and data input and output; 2) standardize the measurement of patient experiences, caregiver/family experiences, and clinician experiences; 3) standardize organizational surveys; and 4) standardize the measurement of patient-reported outcomes. The focus will be on testing possible tools and ensuring alignment across Health Authority, provincial, and national standards.
Currently, HealthConnection Clinic is piloting the development and testing of evaluation tools, to inform decisions related to broader rollout across the Health Authority. This evaluation work also has broader national and international implications because it will inform the development of tools specifically tailored to meet the needs of CHCs serving marginalized, vulnerable, and highly complex subpopulations.
Reflections on the Building Blocks Developmental Approach
The 10 Building Blocks approach is proving to be a valuable and practical heuristic that enables systematic assessment of the current state of primary care development.10 Using the approach with diverse stakeholders involved in the development of primary care has enabled recursiveness and self-reflection, thereby promoting a culture of evaluation and a synthesis of diverse worldviews. The approach provides a common framework that enables different stakeholders to reflect on and evaluate their activities with a wider contextual lens.
The framework also enables systematic, efficient, and effective cross-learning. A simple descriptive evaluation outlining the core content (ie, standard structures and processes) of each PCMH should be considered basic good practice because this would enable effective communication and comprehensive understanding between clinical sites and regions. The Building Blocks could enable alignment in relation to the development of primary care standards for CHCs in Health Authorities as well as provincially and internationally.11,13–15,23 This study also highlights the importance of incorporating community orientation and equity within the Building Blocks and PCMH approaches.14,25
CONCLUSION
There is growing research and policy interest in relation to operationalizing the attributes of high-performing primary care in community health settings.11,13 This study demonstrates how the framework and tools of the 10 Building Blocks of High-Performing Primary Care are enabling the development and evaluation of primary care services for vulnerable and complex subpopulations. This study provides valuable insights related to the development of foundational elements, particularly engaged leadership, empanelment, and data-driven improvement. HealthConnection Clinic demonstrates what is possible when highly engaged leadership share a common vision and purpose, and it highlights the importance and effectiveness of entrepreneurialism and innovation. The clinic’s innovative evaluation work will inform the development of evidence-based tools specifically tailored to meet the needs of public primary care clinics serving highly complex and marginalized subpopulations.
Know Life As It Is
It is a happy sign of the times when medical men understand that they must study sociology, that they must appreciate economic conditions, that they must face the facts and know life as it is, and not as their wishes would have it to be.
— Denslow Lewis, MD, 1856-1913, American physician and author
Acknowledgments
The authors would like to thank the following colleagues for their kind contributions: Julie Zimmerman, MA, and Ann Sarte, PBD, MA, for providing data from Intrahealth Profile EMR and for reviewing and providing feedback and input on the content of drafts; Brian Lane, BScPT, for providing complexity data from Intrahealth Profile EMR; and Rachael McKendry, MA, for providing patient experience data. The authors also thank Niek Klazinga, MD, PhD, for reviewing and providing feedback on the framework and content of several drafts.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Author Contributions
Ali Rafik Shukor, MSc, is the developmental evaluator who conceptualized the article and collected and synthesized data. Ali Rafik Shukor, MSc; Sandra Edelman, MA; Dean Brown, MD; and Cheryl Rivard, MA, jointly analyzed and interpreted data, and drafted the content of the article.
References
- 1.Statistics Canada. Income highlight tables, 2016 census [Internet] Ottawa, Ontario, Canada: Statistics Canada; 2017. Sep 11, [cited 2017 Dec 15] Available from: www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/inc-rev/Table.cfm?Lang=Eng&T=107&S=88&O=A. [Google Scholar]
- 2.Eguchi L North Shore Homelessness Task Force. North Shore homelessness data report: 2016 service use data [Internet] Vancouver, British Columbia, Canada: North Shore Homelessness Task Force; 2017. Sep 27, [cited 2018 May 16]. Available from: https://northshorehomelessness.files.wordpress.com/2017/09/north-shore-homelessness-data-report.pdf. [Google Scholar]
- 3.Canadian Foundation for Healthcare Improvement. Using Canadian case studies to improve healthcare for inner city and marginalized populations [Internet] Ottawa, Ontario, Canada: Canadian Foundation for Healthcare Improvement; 2017. May 31, [cited 2017 Dec 15]. Available from: www.cfhi-fcass.ca/WhatWeDo/on-call/using-canadian-case-studies-to-improve-healthcare. [Google Scholar]
- 4.Brown D HealthConnection. HealthConnection clinic complexity assessment tool (AMPS): An introduction [Internet] North Vancouver, British Columbia, Canada: HealthConnection; updated 2014 Jun 11 [cited 2018 May 7]. Available from: www.cfhi-fcass.ca/sf-docs/default-source/on-call/complexity-assessment-introduction-may31-2017.pdf?sfvrsn=4. [Google Scholar]
- 5.Brown D HealthConnection. HealthConnection clinic complexity assessment tool (AMPS) [Internet] North Vancouver, British Columbia, Canada: HealthConnection; updated 2016 Feb 18 [cited 2018 May 7]. Available from: www.cfhi-fcass.ca/sf-docs/default-source/on-call/complexity-tool-may31-2017.pdf?sfvrsn=2. [Google Scholar]
- 6.Brown D HealthConnection. HealthConnection clinic complexity assessment tool (AMPS): User guide [Internet] North Vancouver, British Columbia, Canada: HealthConnection; updated 2014 Sep 23 [cited 2018 May 7]. Available from: www.cfhi-fcass.ca/sf-docs/default-source/on-call/complexity-tool-user-guide-may31-2017.pdf?sfvrsn=2. [Google Scholar]
- 7.Innovation in primary care: Caring for unattached and marginalized patients [Internet] Mississauga, Ontario, Canada: The College of Family Physicians Canada; 2018. Mar, [cited 2018 May 7]. Available from: www.cfpc.ca/uploadedFiles/Health_Policy/IPC_Unattached_Marginalized.pdf. [Google Scholar]
- 8.Bodenheimer T, Sinsky C.From triple to quadruple aim: Care of the patient requires care of the provider Ann Fam Med 2014. November-December126573–6. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.What we do: Patient medical homes (PMH) and primary care networks (PCN) [Internet] Vancouver, British Columbia, Canada: General Practice Services Committee; c2015. [cited 2017 Dec 15]. Available from: www.gpscbc.ca/what-we-do/primary-care-bc. [Google Scholar]
- 10.Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K.The 10 building blocks of high-performing primary care Ann Fam Med 2014. March-April122166–71. 10.1370/afm.1616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Timbie JW, Setodji CM, Kress A, et al. Implementation of medical homes in federally qualified health centers. N Engl J Med. 2017 Jul 20;377(3):246–56. doi: 10.1056/NEJMsa1616041. [DOI] [PubMed] [Google Scholar]
- 12.Clarke RM, Tseng CH, Brook RH, Brown AF. Tool used to assess how well community health centers function as medical homes may be flawed. Health Aff (Millwood) 2012 Mar;31(3):627–35. doi: 10.1377/hlthaff.2011.0908. [DOI] [PubMed] [Google Scholar]
- 13.Sugarman JR, Phillips KE, Wagner EH, Coleman K, Abrams MK. The safety net medical home initiative: Transforming care for vulnerable populations. Med Care. 2014 Nov;52(11 Suppl 4):S1–10. doi: 10.1097/mlr.0000000000000207. [DOI] [PubMed] [Google Scholar]
- 14.Anderson DR, Olayiwola JN. Community health centers and the patient-centered medical home: Challenges and opportunities to reduce health care disparities in America. J Health Care Poor Underserved. 2012 Aug;23(3):949–57. doi: 10.1353/hpu.2012.0099. [DOI] [PubMed] [Google Scholar]
- 15.Quinn MT, Gunter KE, Nocon RS, et al. Undergoing transformation to the patient centered medical home in safety net health centers: Perspectives from the front lines. Ethn Dis. 2013 Summer;23(3):356–62. [PMC free article] [PubMed] [Google Scholar]
- 16.Shin P, Sharac J, Rosenbaum S. Community health centers and Medicaid at 50: An enduring relationship essential for health system transformation. Health Aff (Millwood) 2015 Jul;34(7):1096–104. doi: 10.1377/hlthaff.2015.0099. [DOI] [PubMed] [Google Scholar]
- 17.Rieselbach RE, Epperly T, Friedman A, et al. A new community health center/academic medicine partnership for Medicaid cost control, powered by the mega teaching health center. Acad Med. 2018 Mar;93(3):406–13. doi: 10.1097/ACM.0000000000001901. [DOI] [PubMed] [Google Scholar]
- 18.Frigon A, Salverda D South Okanagan Similkameen, Division of Family Practice. Martin Street Outreach Centre: Innovative partnerships at one-stop mental health & substance use clinic [Internet] Vancouver, British Columbia, Canada: Divisions of Family Practice; 2018. [cited 2018 May 7]. Available from: https://qualityforum.ca/qf2018/wp-content/uploads/2017/11/A5-RF-Martin-Street-Outreach-Centre-Innovative-Partnerships-at-One-Stop-Mental-Health-Substance-Use-Clinic-v2.pdf. [Google Scholar]
- 19.VCH News. Problem solving is hard-wired in for nurse practitioners at HealthConnection Clinic [Internet] Vancouver, British Columbia, Canada: Vancouver Coastal Health; 2017. Aug 22, [cited 2018 Apr 4]; Available from: http://vchnews.ca/news-coastal/2017/08/22/problem-solving-hard-wired/ [Google Scholar]
- 20.Richard L, Furler J, Densley K, et al. Equity of access to primary healthcare for vulnerable populations: The IMPACT international online survey of innovations. Int J Equity Health. 2016 Apr 12;15:64. doi: 10.1186/s12939-016-0351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haj-Ali W, Hutchison B Primary Care Performance Measurement Steering Committee. Establishing a primary care performance measurement framework for Ontario. Healthc Policy. 2017 Feb;12(3):66–79. DOI: https://doi.org/10.12927/hcpol.2017.25026. [PMC free article] [PubMed] [Google Scholar]
- 22.Christiansen E, Hampton MD, Sullivan M. Patient empanelment: A strategy to improve continuity and quality of patient care. J Am Assoc Nurse Pract. 2016 Aug;28(8):423–8. doi: 10.1002/2327-6924.12341. [DOI] [PubMed] [Google Scholar]
- 23.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: A multidisciplinary review. BMJ. 2003 Nov 22;327(7425):1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marchildon GP, Hutchison B. Primary care in Ontario, Canada: New proposals after 15 years of reform. Health Policy. 2016 Jul;120(7):732–8. doi: 10.1016/j.healthpol.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Franz BA, Murphy JW. The patient-centered medical home as a community-based strategy. Perm J. 2017;21:17–002. doi: 10.7812/TPP/17-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mount JK, Massanari RM, Teachman J. Patient care complexity as perceived by primary care physicians. Fam Syst Health. 2015 Jun;33(2):137–45. doi: 10.1037/fsh0000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Safety Net Medical Home Initiative. Empanelment [Internet] Seattle, WA: Qualis Health; 2013. May, [cited 2017 Dec 15]. Available from: www.safetynetmedicalhome.org/change-concepts/empanelment. [Google Scholar]
- 28.UCSF Center for Excellence in Primary Care. Panel management [Internet] San Francisco, CA: University of California, San Francisco; 2013. [cited 2017 Dec 15]. Available from: https://cepc.ucsf.edu/panel-management. [Google Scholar]
- 29.Martin-Misener R, Kilpatrick K, Donald F, et al. Nurse practitioner caseload in primary health care: Scoping review. Int J Nurs Stud. 2016 Oct;62:170–82. doi: 10.1016/j.ijnurstu.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 30.Muldoon L, Rayner J, Dahrouge S. Patient poverty and workload in primary care: Study of prescription drug benefit recipients in community health centres. Can Fam Physician. 2013 Apr;59(4):384–90. Erratum in: Can Fam Physician 2013 Jun;59(6):612. [PMC free article] [PubMed] [Google Scholar]
- 31.O’Malley AS, Forrest CB. Continuity of care and delivery of ambulatory services to children in community health clinics. J Community Health. 1996 Jun;21(3):159–73. doi: 10.1007/bf01557996. [DOI] [PubMed] [Google Scholar]
- 32.Lewin ME, Baxter RJ. America’s health care safety net: Revisiting the 2000 IOM report. Health Aff (Millwood) 2007 Sep-Oct;26(5):1490–4. doi: 10.1377/hlthaff.26.5.1490. [DOI] [PubMed] [Google Scholar]
- 33.Beal A, Hernandez S. Patient reports of the quality of care in community health centers: The importance of having a regular provider. J Health Care Poor Underserved. 2010 May;21(2):591–605. doi: 10.1353/hpu.0.0305. [DOI] [PubMed] [Google Scholar]