Abstract
Brucella may cause testicular masses, which may be confused with a testicular tumour. We present the case of a man with fever and oedema in the scrotum. Ultrasound and colour Doppler ultrasound with a 6 to 15 MHz high-frequency linear-array transducer was performed, revealing bilateral scrotal wall oedema, heterogeneous echo texture and slightly increased vascularization of the right testis, with hypoechoic lesions characterized by hypervascular margins and no flow within them. These findings were compatible with testicular abscesses. Three blood cultures grew Brucella melitensis, so the patient received treatment with doxycycline and rifampin for 8 weeks, which resulted in disappearance of the testicular abscesses.
Keywords: Brucella melitensis, genitourinary brucellosis, testicular abscess, zoonosis, stuartii
Introduction
Brucellosis is the most frequent worldwide zoonosis caused by Brucella species. Because of the scarcity of the disease and the difficulties in yielding this microbe, brucellosis often goes underdiagnosed. We describe a man who presented with fever and testicular masses who was found to be infected with Brucella.
Case report
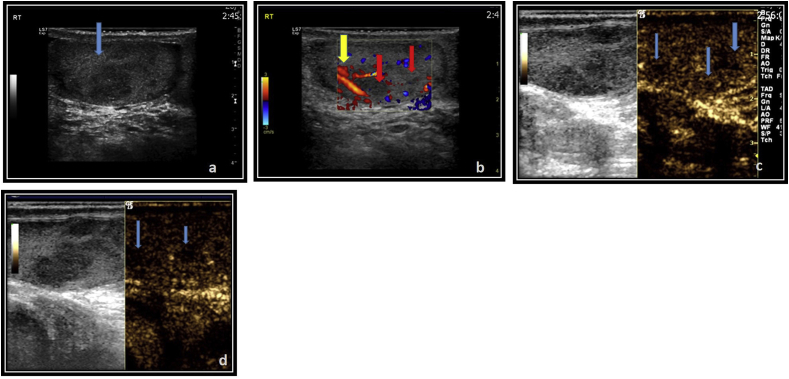
A 66-year-old man sought care at our hospital for fever (temperature 39°C) which had started 2 weeks before. He also reported oedema and pain in the scrotum together with weight loss. His medical history was unremarkable. Physical examination revealed oedema and tenderness in his right testis. Laboratory tests revealed anaemia (haematocrit 33.1%, haemoglobin 11.3 mg/dL), white blood cell count 5.150 cells/mm3, platelets 313 × 109 cells/mm3, erythrocyte sedimentation rate 45 mm/h and C-reactive protein 13.5 mg/dL (normal value, <0.5 mg/dL). Ultrasound, colour Doppler ultrasound with a 6 to 15 MHz high-frequency linear-array transducer and contrast-enhanced ultrasound (SonoVue) were used, which confirmed findings compatible with testicular abscesses (Fig. 1).
Fig. 1.
Right-sided orchitis with abscess formation. (a) Ultrasound revealed sharp heterogeneous echostructure of right testis. (b) Colour Doppler imaging revealed nonvascular hypoechoic areas (abscesses) and slightly hypervascular testis. (c, d) Contrast-enhanced ultrasound revealed focal absence of enhancement with peripheral rim of enhancement.
Because of the presence of abscesses in the testis and the reported consumption of unpasteurized milk, as well as his working in a farm with sheep and goats in an area where brucellosis is endemic, a diagnosis of Brucella infection was suspected, which was confirmed by a positive Wright-Coombs immunoglobulin G reaction at a titre of 1/10.240. Also, three blood cultures, which were drawn on three consecutive days, grew Brucella melitensis by the use BACTEC 9240 automated system. The patient was treated with doxycycline 100 mg twice daily and rifampin 600 mg once daily. Because three blood cultures were positive and a cardiac murmur was present, transthoracic and transesophageal cardiac ultrasounds were performed, which did not reveal any vegetation. Therefore, the presence of endocarditis was ruled out. However, because of the severity of the infection, and because the patient had suppurated lesions in the testis, he also received gentamicin 5 mg/kg daily for 8 days. An ultrasound of the testis performed after the completion of his treatment (i.e. after 8 weeks) was normal. It is noteworthy that no drainage of the testicular abscesses was performed at any time. Also, two blood cultures, which were drawn after 4 and 8 weeks of therapy, were negative.
Discussion
Brucellosis, although uncommon in the United States, northern Europe and Eastern Asia, is common in the Middle East, southern Europe and South America [1]. Human brucellosis is a potentially life-threatening multisystem disease which requires combined and prolonged treatment with antimicrobial agents because it has the potential for recurrence. Genitourinary system involvement occurs in 2% to 20% of patients with brucellosis and includes prostatitis, epididymo-orchitis, cystitis, pyelonephritis, interstitial nephritis, exudative glomerulonephritis and renal abscesses. Because of the nonspecific symptoms, infections of the urinary tract due to Brucella species often remain underdiagnosed [2]. Epididymitis due to Brucella species may cause serious complications if left untreated, such as necrotizing orchitis, aspermia or oligospermia [3], [4].
Epididymo-orchitis occurs in 6% to 20% of cases of Brucella infection, is usually unilateral and most frequently presents in young men [5], [6]. The main differential diagnosis of testicular brucellar abscess is a necrotic tumour. Failure to appropriately diagnose the abscess can lead to unnecessary orchiectomy [5], [6]. The ultrasound findings of hypervascularization of the testis and the epididymis were crucial in this setting [6]. Although testicular abscesses due to B. melitensis are a rare manifestation of the disease, they should be considered in the differential diagnosis of a testicular mass in highly endemic areas, such as the Mediterranean region [7], [8].
Conflict of interest
None declared.
References
- 1.Pappas G., Akritidis N., Bosilkovski M., Tsianos E. Brucellosis N Engl J Med. 2005;352:2325–2336. doi: 10.1056/NEJMra050570. [DOI] [PubMed] [Google Scholar]
- 2.Khan M.S., Humayoon M.S., Al-Manee M.S. Epididymo-orchitis and brucellosis. Br J Urol. 1989;63:87–89. doi: 10.1111/j.1464-410x.1989.tb05131.x. [DOI] [PubMed] [Google Scholar]
- 3.Akinci E., Bodur H., Cevik M.A., Erbay A., Eren S.S., Ziraman I. A complication of brucellosis: epididymoorchitis. Int J Infect Dis. 2006;10:171–177. doi: 10.1016/j.ijid.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Erdem H., Elaldi N., Ak O., Gulsun S., Tekin R., Ulug M. Genitourinary brucellosis: results of a multicentric study. Clin Microbiol Infect. 2014;20:847–853. doi: 10.1111/1469-0691.12680. [DOI] [PubMed] [Google Scholar]
- 5.Savasci U., Zor M., Karakas A., Aydin E., Kocaaslan R., Oren N.C. Brucellar epididymo-orchitis: a retrospective multicenter study of 28 cases and review of the literature. Travel Med Infect Dis. 2014;12:667–672. doi: 10.1016/j.tmaid.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Kaya F., Kocyigit A., Kaya C., Turkcuer I., Serinken M., Karabulut N. Brucellar testicular abscess presenting as a testicular mass: can color Doppler sonography be used in differentiation? Turk J Emerg Med. 2015;15:43–46. doi: 10.5505/1304.7361.2014.82698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yemisen M., Karakas E., Ozdemir I., Karakas O. Brucellar testicular abscess: a rare cause of testicular mass. J Infect Chemother. 2012;18:760–763. doi: 10.1007/s10156-011-0354-7. [DOI] [PubMed] [Google Scholar]
- 8.Kocak I., Dündar M., Culhaci N., Unsal A. Relapse of brucellosis simulating testis tumor. Int J Urol. 2004;11:683–685. doi: 10.1111/j.1442-2042.2004.00862.x. [DOI] [PubMed] [Google Scholar]