Abstract
Background: Cancer ‘patients’ are increasingly using traditional indigenous and complementary medicines (T&CM) alongside conventional medical treatments to both cure and cope with their cancer diagnoses. To date T&CM use among Indigenous cancer patients from Australia, Canada, New Zealand, and the United States has not been systematically reviewed. Methods: We systematically searched bibliographic databases to identify original research published between January 2000 and October 2017 regarding T&CM use by Indigenous cancer patients in Australia, Canada, New Zealand, and the United States. Data from records meeting eligibility criteria were extracted and appraised for quality by 2 independent reviewers. Results: Twenty-one journal articles from 18 studies across all 4 countries met our inclusion criteria. T&CM use ranged from 19% to 57.7% (differing across countries). T&CM was mostly used concurrently with conventional cancer treatments to meet their spiritual, emotional, social, and cultural needs; however, bush, traditional, and herbal medicines were used in a minority of cases as an alternative. Conclusions: Our findings highlight the importance of T&CM use to Indigenous cancer patients across these 4 countries; we identified multiple perceived spiritual, emotional and cultural benefits to its use. The patient’s perception of their health professional’s attitudes toward T&CM in some cases hindered or encouraged the patient’s disclosure. Additional research is required to further explore the use and disclosure of T&CM among Indigenous cancer patients to help inform and ensure effective, safe, coordinated care for Indigenous cancer patients that relies on shared open decision making and communication across patients, communities, and providers.
Keywords: traditional medicine, complementary therapies, cancer, neoplasms, cancer care facilities, Indigenous population, Oceanic Ancestry Group, American Native Continental Ancestry Group
Introduction
It is well documented that Indigenous people in Australia, Canada, New Zealand, and the United States consistently experience substantial inequities in cancer outcomes in comparison with their non-Indigenous counterparts, in terms of increased incidence,1-3 poorer prospects of treatment,2-4 and higher mortality rates.1-3,5 Current evidence suggests that these disparities are attributable to a range of factors, including, but not limited to, later stage at diagnosis, lower treatment compliance, lower cancer screening rates, and social deprivation.3,6
Cancer ‘patients’ are increasingly using traditional and complementary medicine (T&CM) in addition to conventional medical treatments, such as chemotherapy or radiation therapy, to both cure and cope with their cancer diagnosis.7,8 A recent systematic review7 reported a combined prevalence of 40% for current complementary medicine (CM) use in 152 studies, from across 18 countries, which included more than 65 000 cancer patients. Horneber et al7 also reported that CM use had increased over time from approximately 25% in the 1970s to more than 32% in the 1990s and to 49% post-2000. Cancer patients’ disclosure of their use of T&CM to health care providers is important to assess any potential treatment interactions.9-12
Indigenous people tend to view health from a holistic perspective that incorporates physical, cultural and spiritual wellbeing and this underpins their care-seeking behaviors.6,13 The use of traditional medicine (TM) (eg, singing/chanting, bush medicine, traditional healers, and external remedies) is part of Indigenous culture, continuing traditions and lore.13 TM is often used to enhance overall well-being through reconnection to land, spiritual, and ancestral roots.6,13 Traditional healers provide spiritual and social support that is equally as important as the botanically based herbal remedies.13 To date there has been no comprehensive review of T&CM among Indigenous cancer patients and this manuscript aims to address this gap.
Methods
Eligibility Criteria
TM and CM14 include a broad range of practices, technologies, products, knowledge systems, and approaches to preventing and/or treating illness and/or promoting well-being, which are not historically associated with the conventional medical profession or medical curriculum.15 While TM refers to health care indigenous to the local culture of users (including examples such as herbal medicines and practices provided by traditional healers who are usually unregulated and operate outside the publicly funded health care system), CM refers to health care, both self-administered or practitioner-led, which is often exotic to the culture of users (examples include massage, chiropractic, and Western herbal medicine).14 As these definitions suggest there may well be temporal and geographical fluidity whereby the definition of a particular health care practice can be considered TM or CM depending on the context of use and users.16 However, despite these possible variations of context both TM and CM in the vast majority of cases are largely defined by their continuing provision and use beyond the routine focus of conventional medical practice.14
Indigenous populations eligible for inclusion in this review were from Australia (Aboriginal and Torres Strait Islander), Canada (Aboriginal, First Nations, Inuit, or Métis), New Zealand (Māori), or the United States (American Indian, Native American, Alaskan Native, American Samoan, Eskimo, and Native Hawaiian). These countries were included because of their shared history of colonization and disproportionally worse health in Indigenous populations.1,3 In this review, we respectfully refer to Indigenous people in these 4 countries as “Indigenous” while acknowledging that they comprise many diverse groups with distinct languages, beliefs, and cultural practices.
Search Strategy
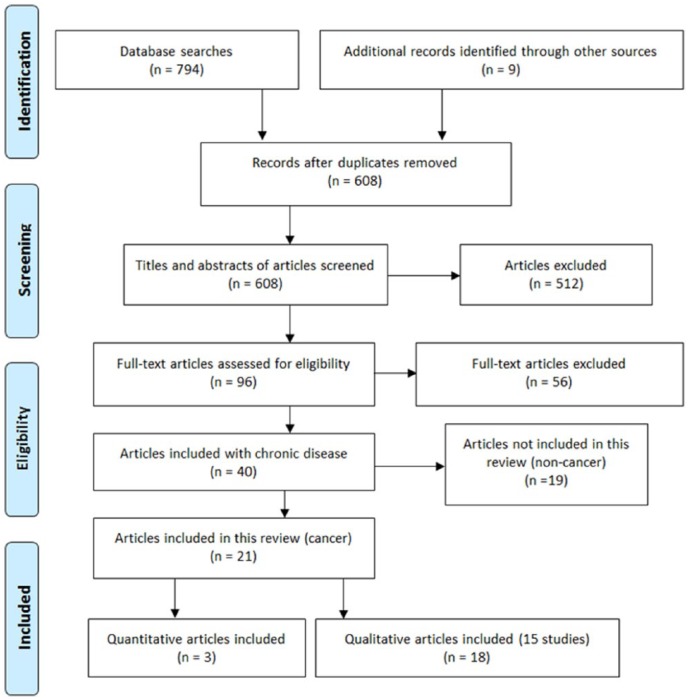
The search originally aimed to identify peer reviewed literature reporting new empirical data from qualitative or quantitative studies examining T&CM use for 1 of 5 chronic diseases (cancer, cardiovascular disease, kidney disease, diabetes type 2, or respiratory disease) in adult (18 years and older) Indigenous populations from Australia, Canada, New Zealand, and the United States. As approximately half of all records were unique to cancer at the end of our search, this review focuses on cancer only; however, the flowchart (Figure 1) and search terms (Table 1) depict the screening of studies for all 5 diseases. We required full records of original research that were published in a peer-reviewed journal from 2000 onward, excluding (a) books or book chapters, commentaries, literature reviews, editorials, poster abstracts, and dissertations; (b) published languages other than English; and (c) efficacy studies (as we are interested in T&CM use).
Figure 1.
Study selection and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Reasons for exclusion: nonindigenous population; indigenous population outside Australia, Canada, New Zealand, and the United States; no traditional and complementary medicine (T&CM) use reported; relevant diseases not mentioned in their chronic form (cancer, cardiovascular disease, kidney disease, diabetes type 2, or respiratory disease); nonhuman records, for example, animals or plants; not an empirical article reporting original research in an IMRaD (Introduction, Methods, Results, and Discussion)–style manuscript; not peer-reviewed; no participants aged 18 years or older; pre-2000; non-English; no indigenous breakdown of results.
Table 1.
Free-Text Terms for All Databases and Controlled Vocabulary for CINAHL.
| Search Terms | |
|---|---|
| Indigenous population terms | [Title/Abstract search: Indigenous OR Aborigin* OR Torres Strait Islander* OR Māori* OR American Samoa* OR First Nation* OR Canadian Indian* OR Native American* OR American Indian* OR Inuit* OR Métis OR Eskimo* OR Alaska* Native* OR Aleut OR Native Hawaiian* CINAHL headings: Indigenous peoples OR American Samoa] |
| Chronic disease terms | [Title/Abstract search: cancer* OR neoplasm* OR heart disease* OR cardiovascular disease* OR kidney disease* OR renal disease* OR diabetes OR respiratory disease* OR lung disease* CINAHL headings: Neoplasms; Diabetes Mellitus; Cardiovascular Diseases; Kidney Diseases; Respiratory Tract Diseases] |
| CM and TM terms | [Title/Abstract search: complementary medicine* OR complementary therap* OR alternative medicine* OR alternative therap* OR natural medicine* OR natural therap* OR holistic medicine* OR holistic therap* OR Integrative medicine OR traditional medicine* OR bush medicine* OR traditional medicine practice* OR ethnomedicine* OR traditional healer* OR traditional practitioner* OR traditional health practice* OR native American medicine* OR Native American healing practice* OR spiritual treatment* OR medicine man OR medicine men OR native medicine* OR aboriginal healer* CINAHL headings: Alternative Health Personnel; Alternative Therapies] |
Abbreviations: CINAHL, Cumulative Index to Nursing and Allied Health Literature; CM, complementary medicine; TM, traditional medicine.
We searched AMED, AltHealthWatch, CINAHL, EMBASE, PsychINFO, and PubMed for records published between January 2000 and October 2017 (the year 2000 was chosen because of changes in complementary medicine and service systems that might limit the applicability of studies prior to this date). Keywords included using free-text terms representing (a) Indigenous populations from and residing in Australia, Canada, New Zealand, and the United States; (b) common chronic conditions among Indigenous populations (ie, cancer, diabetes, heart disease, kidney disease, respiratory disease); and (c) terms used previously for CM,9 which included TM terms (Table 1). In addition, we searched the reference lists of articles that had previously conducted systematic literature reviews on similar topics to ours.
Review Process
The systematic review process was guided by the Cochrane Collaboration17 and the Centre for Reviews and Dissemination18 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines19 as outlined in Figure 1.
After removing duplicates, AG and SL independently examined titles and abstracts using Covidence systematic review software.20 Articles not meeting eligibility criteria were excluded. All retrieved full-text articles were independently assessed by AG and SL and the reasons for excluding articles were documented and discrepancies were resolved by consensus. Extraction of data in qualitative studies was conducted via the Joanna Briggs Institute’s method of qualitative research synthesis (meta-aggregation) as it avoids reinterpreting data and attempts to accurately and reliably present the findings of included studies consistent with the intent of the original authors.21 AG and SL independently piloted this approach21 to achieve consensus on interpretation and data extraction. AG and SL then proceeded with double independent extraction of findings, categories and synthesised findings from qualitative studies. Extraction discrepancies were documented and discrepancies were resolved by consensus.
Quality Appraisal of Studies
The methodological quality of each publication was assessed by AG and SL using separate tools for quantitative and qualitative studies. Quality assessment for the quantitative studies was conducted using the Newcastle-Ottawa Scale (NOS) modified for prevalence studies22 and a 6-item critical appraisal tool was used for the qualitative studies developed by Kuper et al.23
The NOS scale authors report that the scale has face/content validity and interrater reliability.24 The modified NOS produce a rating out of 5. It assesses the representativeness of the sample, the sample size adequacy, nonresponse, measurement of variables and the quality of the descriptive statistics reporting. Consistent with Cochrane guidance,17 we made minor adaptions to the NOS to fit the specifics of our review question. Specifically, we altered the first NOS item to score studies on variability in remoteness, socioeconomic status, gender, and age. In addition, we modified the fourth NOS item to represent our topic of interest, T&CM, by keeping the validated measurement tool and adding the need for a T&CM definition.
The Kuper et al23 quality assessment tool for qualitative studies produces a rating out of 6. The 6 questions cover: sampling, data collection, data analysis, transferability, ethical issues, and reflexivity and the overall clarity of the study. AG and SL piloted the measures, introducing half marks for items that had 2-part questions and agreed upon a scoring system based on our research question. Furthermore, studies with no ethnic breakdown reported, received a reduced score, as we were unable to distinguish Indigenous from non-Indigenous participants.
Ethics
Ethical approval was not required for this systematic literature review.
Results
Of the 794 records retrieved, 195 duplicates were removed and 599 records were screened by title and abstract. An additional 9 records were identified through checking the reference lists. Of the 608 abstracts considered for inclusion, 96 full-text articles were assessed for eligibility, and 40 records were subsequently considered eligible for inclusion. Of these records, 21 were cancer-related, and as such other chronic conditions were excluded (see Figure 1).
Characteristics of the Included Articles
The 21 articles represented 18 individual studies: 3 were conducted in Australia,25-29 4 in Canada,30-33 3 in New Zealand,34-36 and 8 in the United States.37-45 Most were qualitative,26-33,35-42,44,45 (n = 15, 83%), including 2 case studies,32,38 and all 3 quantitative studies were cross-sectional.25,34,43 All quantitative studies assessed TM as a subset of CM, where the qualitative studies differed in their focus, with 10 (75%) exclusively examining TM and/or TM healers; 2 from Australia, 4 from the United States, 3 from Canada, and 1 from New Zealand.
Most studies included participants from urban/accessible areas (n = 6; 33%), or rural areas (n = 8; 44%) and were conducted in a range of clinical and community settings. Most studies contained solely Indigenous participants (n = 13; 72%) and females (83.9%). Sample sizes varied extensively, with single clinical case studies, 126 in the largest qualitative study and 248 in the largest quantitative study; with both samples 100% Indigenous. For those studies that reported cancer type (n = 15; 83%), most included participants with breast cancer (40.5%), followed by digestive organ cancers (14.2%) and lung cancer (12.7%).
Of the quantitative studies, only the Australian study exclusively sampled an Indigenous population (from Queensland, a state of Australia), whereas the others sampled small (n = 26) and moderately sized (n = 129) Indigenous subgroups. Seven of 15 qualitative studies investigated TM and/or CM use exclusively, with 2 of these 7 being case studies. Four qualitative articles intentionally reported on TM and/or CM as a subset of a broader focus, often indicated by mention of these practices only in the abstract. Seven qualitative studies referred to TM and/or CM in a section of the results not devoted to their use.
Using the modified Newcastle-Ottawa scoring guide,24 the overall scores assigned to each quantitative study out of a possible score of 5 was 4.5, 3.5 and 0.5 (see Table 2). Using the quality assessment tool of Kuper et al23 for qualitative studies, we assigned the 15 studies scores ranging from 1 to 5.5 (mean = 3.41) out of 6 possible points (see Table 3).
Table 2.
Characteristics of Included Quantitative Studies.
| Authors (Year) | Setting | Study Design | Indigenous Sample Size (Indigenous % of Total Sample) | Sex for Indigenous Sample Only | Data Collection Method | T&CM Use for Indigenous Sample Only | Discussions Regarding T&CM Use With HP | Quality Assessment Score/5 |
|---|---|---|---|---|---|---|---|---|
| Australia—Aboriginal and Torres Strait Islander | ||||||||
| Adams et al (2015)25 | 62.9% urban, 37.1% outer regional outpatient clinics large public hospitals | Quantitative cross-sectional | 248 (100%) | 57% female | Structured questionnaire delivered face-to-face | 47 of 248 (18.7%) used T&CM | NR | 4.5 |
| New Zealand—Maori | ||||||||
| Chrystal et al (2003)34 | Outpatient clinics at a regional cancer treatment center unit | Quantitative cross-sectional | 26 (13%) | NIB | Self-administered postal questionnaire | 15 of 26 (57.7%) used T&CM | NIB | 0.5 |
| USA—Alaskan Native, Native American, and Native Hawaiian | ||||||||
| Maskarinec et al (2000)43 | State of Hawaii | Quantitative cross-sectional | 129 (12.9%) | NIB | Self-administered postal questionnaire | 45 of 129 (29.8%) used T&CM | NR | 3 |
Abbreviations: NIB, no Indigenous breakdown; NR, not reported; HP, health professional(s); T&CM, traditional and complementary medicine.
Table 3.
Characteristics of Included Qualitative Studies.
| Authors (Year) | Setting | Indigenous Sample size (Indigenous % of total sample) | Age (Years)/Sex of Indigenous Sample Only | Data Collection Method | Methodology | Extent of Use of Indigenous Sample Only | Discussions Regarding T&CM Use With HP | Quality Assessment Score/6 |
|---|---|---|---|---|---|---|---|---|
| Australia—Aboriginal and Torres Strait Islander | ||||||||
| Prior (2005)27/Prior (2009)26 | Women’s health clinics, mobile cancer screening venues, gynecology clinics and in the general community | 38 (100%) MS | NR/100% female | Face-to-face interviews, focus groups, and field notes | Interpretive ethnography | NR | Women in study feared disclosing TM preference due to potential ridicule | 2 and 5.5a |
| Shahid et al (2009)29/ Shahid et al (2010)28 | Primary or tertiary care, Aboriginal Health Services or other local support agencies in urban, rural and remote | 37 (100%) MS | 30-39 (n = 5) 40-49 (n = 19) 50-59 (n = 9) 60+ (n = 4)/78% female | Face-to-face interviews; observations and field notes | Social constructionist framework | 22 mentioned (59%) | NR | 5 and 5a |
| Canada—Aboriginal | ||||||||
| Barkwell (2005)31 | Hospital servicing a reserve community and the outskirts of the reserve | 18 (58%) MS | NR/NR | Open-ended face-to-face interviews loosely based on Kleinman’s explanatory model | Grounded theory | NR | NR | 3.5 |
| Clarke and Holstander (2010)32 | NR | 1 (100%) | NR/100% female | Observation (field notes) | Case study of Medicine Wheel teachings | 1 (100%) | NR but HP aware | 1 |
| Mehl-Madrona (2008)33 | NR | 47 (100%) | Age range from 20 to 89/NR | Face-to-face interviews | Schatzman’s 1991 grounded method | 100% (eligibility criteria) | NR | 3 |
| Poudrier and Mac-Lean (2008)30 | Aboriginal organizations, universities and cancer centers in cities, rural, and First Nations communities | 12 (100%) | 42-75/100% female | Interviews and photography | Photovoice and feminist epistemology | NR | NR | 4.5 |
| New Zealand—Maori | ||||||||
| Dew et al (2015)35 | Local community health services and hospitals | 19 (55.9%) | Maori M = 59/NIB | Semistructured Interviews | NR | 8 (42%), 4 no, but had considered | Yes, including conflict, % not reported | 3.5 |
| Walker et al (2008)36 | Cancer Society Centre (feedback session), residential facilities for cancer patients and whanau | 44 (100%) MS | Early-20s to mid-70s/NR | Face-to-face focus groups and interviews | Thematic data analysis incorporating feedback hui (member checking) | NR | NR | 2.5 |
| USA—Alaskan Native, Native American, and Native Hawaiian | ||||||||
| Arthur et al (2012)37 | University Medical Centre (teaching hospital) in small city | 1 (7%) | 66/100% female | Semistructured face-to-face interviews | Grounded theory | 1 (100%) | NIB | 1.5 |
| Bucher (2008)38 | Tertiary care hospital | 1 (100%) | 65/100% female | Observation (field notes) | Case study | 1 (100%) | NR but HP aware | 1 |
| Canales (2004)39 | NR | 6 (100%) 14 had no cancers | 39 to 75, M = 53/100% female | Open-ended face-to-face interviews | Grounded theory | NR | NR | 3 |
| Haozous et al (2011)40 | Regional cancer clinic servicing reservations | 10 (100%) | M = 54 years (range 31-75 years)/90% female | Face-to-face interviews and semistructured questionnaire using Brief Pain Inventory–Short Form | Lincoln and Guba’s criteria for methodological rigor in qualitative analysis (p. 405) | NR | NR | 5.5 |
| Hohl et al (2016)41 | Urban tribal clinics | 82 (100%) MS | NR but eligibility >21 years/69% female | Open-ended question interviews via phone or face-to-face | NR | 33% | Mixed, some reported and some did not—mixed responses when reported, both positive and negative | 4 |
| Itty et al (2014)42 | Community clinics and community centers | 126 (100%) MS | NR/70.6% female | Focus groups | Constructivist grounded theory | NR | Mixed reporting, many barriers identified to communication | 4 |
| Struthers and Eschiti (2004)44/Struthers and Eschiti (2005)45 | Participant homes, offices and 1 at their reservation | 4 (100%) | 49 to 61/75% female | Face-to-face interviews | Qualitative phenomenological methodology | 4 (100%) | One participant disclosed after doctors noted unusual improvement—felt they needed to educate the HPs | 3.5 and 3.5a |
Abbreviations: NIB, no Indigenous breakdown; NR, not reported; MS, mixed sample of cancer patients/survivors and caregivers; HP, health professional(s); T&CM, traditional and complementary medicine.
Represents the quality assessment score for the 2 articles included in this column in the order that they appear.
Quantitative Study Findings
Three quantitative studies were conducted, one each in Australia,25 New Zealand,34 and the United States.43 Two studies focused exclusively on T&CM,34,43 and one reported T&CM use within a broader study not focused on T&CM use.25 One study included broad terms to assess T&CM use (eg, “traditional Indigenous practitioner,” “complementary medicine practitioner,” and “relaxation/meditation class”)25 while the other 2 assessed specific therapies.34,43 Across the 3 studies, T&CM use ranged from 19% to 57.7%—with Maori reporting the highest use and Indigenous Australians the lowest (note: we are only reporting on the Indigenous populations reported in these studies). Two studies did not provide reasons for T&CM use by Indigenous status.34,43 However, Adams and colleagues25 found all users employed T&CM for support with their cancer; however, the specific areas of support were not identified. This Australian study also identified those patients with an education level of high-school or above were more likely to consult a CM practitioner than those with education levels less than high school (P = .015).25
Qualitative Study Findings
Fifteen qualitative studies were conducted: 2 Australian,26-29 4 Canadian,30-33 2 New Zealand,35,36 and 7 United States studies.37-42,44,45 Following meta-aggregation, thematic analysis revealed 4 broad themes: (a) perceived efficacy and benefits of T&CM, (b) integrating T&CM with conventional treatments, (c) T&CM use as connection to culture, and (d) impact of health professionals’ views of T&CM (Table 4).
Table 4.
Findings Summary of Main Themes Identified via Meta-Aggregation.
| Themes | Key Findings | Example Quotes |
|---|---|---|
| Perceived efficacy and benefits of T&CM | Ambiguous terms to describe T&CM efficacy | “13 (93%) of the CAM users expressed belief in
CAM and/or valued CAM.” (Arthur et al)37(p235)
“I firmly believe that 75% of why I’m going to make it is going to be because of Indian medicine. Somehow or another it’s working. I don’t have the kind of faith in your medicine that I have in Indian medicine. I still give some credit to Western medicine and so, I have to give you guys [Western doctors] 25%.” (Struthers and Eschiti)44(p18) “All of the women interviewed shared the importance of balancing mind, body, and spirit in their efforts toward taking care of self and achieving a state of health and well-being.” (Canales)39(p422) “A connection to spirituality and holistic health worldview: Healing is mental, emotional and spiritual as well. For some participants the application of bush medicine was not only seen as relieving stress but was also seen as an enabler in maintaining their connections and beliefs on culture, ancestors and spirituality. The practice of bush medicines confirmed and supported participant’s cultural beliefs and attitudes that conformed to Aboriginal understandings and epistemologies of health and wellbeing as holistic.’ (Shahid et al)28(p4) “Linda developed pneumonia while undergoing chemotherapy and was hospitalized for 3 weeks. She lost 20 pounds. Family members contacted the medicine man, and Linda was given another herb to help stimulate her appetite.” (Bucher)38(p113) “He asked about alternative medicines. One relative who was in America had told him about a plant that could be used that was better than chemo and radiation and so he asked for information that could prove that, but he got no further information. Proof was particularly important as he had another relation who had died from cancer many years before after rejecting radiation and using an alternative approach in Mexico, so he concluded that “I’m afraid I’ve got no trust in them.” (Dew et al)35(p146) |
| Belief in T&CM | ||
| Holistic benefits of T&CM | ||
| T&CM used to reduce side-effects and assist in palliation | ||
| Lack of evidence about efficacy or risks of T&CM can reduce use | ||
| Integrating T&CM with conventional treatments | Integrated T&CM with conventional treatment | “CM users did not express a current or continued
dissatisfaction with their conventional cancer treatment.
Instead, they expressed satisfaction with the combination of
conventional treatment and CAM use, because they did not
want to limit themselves to conventional medicine alone.”
(Arthur et al)37(p236)
You have to use both [traditional and conventional]. But in terms of taking care of myself, obviously I’ve swung right back over toward [traditional] . . . but obviously a modern lab makes my Dim [dinomethyl], makes my Q-Co-10 [herbal remedy]. I’ll do whatever, but I grow my own burdock [for tea]. (Canales)39(p418) “Adverse reaction from biomedicine: Radiation and chemo nearly killed me. I know a couple of people who chose the bush medicine once they read up about chemotherapy and the two per cent of people that chemo cured, they took their chances with the bush medicine, and they are still going. It’s either the quality of life or being sick from the chemo, that’s what they weighed up. (Shahid et al)28(p6) “There are some Aboriginal people who use traditional medicine as an alternative to Western medicine. Both cancer patients and the family members felt some people get scared about the intensive procedures of common cancer treatments and their side-effects, influencing them to choose other options instead.” (Shahid et al)28(p6) |
| T&CM used for curative properties, coping or preventing recurrence | ||
| Rejection of conventional treatment and opt for TM only | ||
| Seeking TM after failure of conventional treatment | ||
| T&CM use as connection to culture | Indigenous holistic concept of health ways of healing | “They participated and took initiative in their
treatment because of the belief that wellbeing is holistic.
A holistic view of well-being meant that the conventional
treatment plan was only part of their solution.” (Arthur et
al)37(p236)
“Making connections with community and family provided important coping for a population that is economically, socially, and physically isolated . . . There’s traditional medicine, I believe in it, too. Because all your relatives come together. I really like the environment when everybody comes as one, and it makes you feel real good. It makes you feel just uplifted. While participants referenced different spiritual foundations to their prayer, the common theme in these interviews was the power of spirituality to bring people together.” (Haozous et al)40(p408) “Generally the women in this study had a good knowledge of environmental and biological causes of cancer but they also believed in the spiritual forces of ‘bad spirits’ aroused as ‘payback’ to inflict the victim with a serious disease like cancer. Such beliefs added to the difficulty of the patients who may be reluctant to talk about their disease for fear of bringing shame to their family. But an important aspect of this view that cancer was a result of ‘payback’ were the beliefs that traditional medicine and Aboriginal healers were essential to the health care of the sick person, either with or maybe instead of, conventional medical treatment.” (Prior)27(p9) “She respects the fact that her family has decided to follow Christian ways; however, she wants her passing to be marked in traditional ways. This means that certain ceremonies must take place for her to have a peaceful transition to the spirit world.” (Clarke and Holtslander)32(p34) “Shelley, who identified as a Métis woman and had recently re-connected to her family’s cultural values and traditional practices, took a photo of her family sweat lodge explaining that it was a salient part of her recovery from breast cancer. For her, it was a source of connection to traditional values and family and a source of strength. The sweat lodge was also seen as a safe place for healing—a place free of racism.” (Poudrier and Mac-Lean)30(p311) The sweat lodge ceremony is a big part of my life and that’s where I did most of my healing . . . Anything and everything in there is safe. Everything in there is equal because when that door is closed its black. So nobody, there’s no color. There’s no racism in there. There is nothing in there. It’s really like a positive experience. (Poudrier and Mac-Lean)30(p312) |
| T&CM use to counter spiritual forces/payback | ||
| Family and community encouraged use | ||
| Fits with cultural values and beliefs | ||
| Opposed to conventional medicine | ||
| Connection to family (bridges isolation gap) | ||
| Didn’t want to be far away from home/family | ||
| Impact of health professionals’ views of T&CM | Lack of knowledge of T&CM by health providers | “Service providers need to acknowledge and
understand the existence of Aboriginal knowledge
(epistemology) and accept that traditional healing can be an
important addition to an Aboriginal person’s healing
complementing Western medical treatment regimes.” (Shahid et
al)28(p1)
“She didn’t trust the Western medical system because in her view it belittled Maori medicine and people were still dying under western medical treatment.” (Dew et al)35(p146) |
| Health professionals dismissive of TM | ||
| Health professionals’ lack of respect for TM hinders communication | ||
| Patients unlikely to disclosure T&CM usage due to negative responses of health professionals | ||
| “The women in this study recalled their apprehension about
declaring preferences for traditional approaches to
treatment because they feared being ridiculed by the
hospital staff. The culturally appropriate mantra of cancer
control misses the point unless there is a deeper engagement
of Aboriginal people in their own health care, so that real
choices are possible and the significance of culture is
understood and respected.” (Prior)26(p285)
“Though most respondents who discussed the use of traditional medicine with their care providers were met with support, some participants were either reluctant to share this information with care providers or felt disregarded, such as this survivor who reported: I tried to (discuss traditional medicine with providers). It was kind of one of those things where they didn’t want to hear it. They didn’t want to discuss it . . . They didn’t take the things I said seriously. They treated me like I was a complete idiot, and that was really, really difficult.” (Hohl et al)41(p2441) “The data suggest that when conventional providers respect native beliefs and traditions, are knowledgeable about natural practices, and recognize the influence of traditional world views on Native women’s health and health care decisions, Native women are more open to, and trusting of, the conventional health care system.” (Canales)39(p433) |
Abbreviation: T&CM, traditional and complementary medicine.
Perceived Efficacy and Benefits of T&CM
The terms used to describe efficacy and benefits of T&CM are often ambiguous, such as believing in it,40 healing,30,33,40,45 and protection.41 Three studies reported patients’ belief in T&CM as a cancer treatment,35,44,45 with 2 studies reporting patients’ belief that efficacy depends on the strength of their confidence in T&CM.28,29 The reported benefits of T&CM included: helping to cope; stress relief; cleansing and strengthening the body; increasing strength, energy, healing and recovery; and improving well-being.26-29,33,38,40,41,44,45
. . . it’s a bush or root that you boil it up, but there is something in it that is good for insides, just as a cleanser. Makes all your body organs healthy and strong, it gets rid of all your internal stress28
The exclusive use of TM during palliation was associated with “reconnection to land, ancestral and spiritual roots that enhanced the person’s overall well-being”; TM was used to reduce side effects of chemotherapy, including weight and appetite loss.38 For many patients, TM was described as a highly valued Indigenous way of healing that was attributed to health improvements.28,30,40,44 TM was said to work best when patients are diagnosed early, believe in the value of TM, and have a strong desire to fight cancer.44 Some participants had safety concerns about TM—citing the paucity of evidence relating to efficacy, the lack of prescription information and previous experiences of allergic reactions or interactions with other medications.28,35
Integrating T&CM With Conventional Treatments
Most participants used T&CM alongside conventional cancer treatments,28,35-39,42,44 while a minority replaced conventional treatments with TM.28 Some participants used TM for curing their cancer,28,30,44 some for healing and coping, and others to prevent recurrence,39 while some used it only as a last resort.28,35 One participant speaks of fully integrating the 2:
In between having my surgery, convalescing, and coming back home, they had done ceremonies to heal me.44
One participant explains why some people rely solely on TM:
I know a couple of people who chose the bush medicine once they read up about chemotherapy . . . they took their chances with the bush medicine, and they are still going. It’s either the quality of life or being sick from the chemo, that’s what they weighed up.28
Integrating TM and conventional medicine was common for some participants and this flowed naturally into their cancer treatment.28,39,44 Some participants used T&CM on recommendation from community members or after seeing others benefit.28 Some decided against using conventional treatments in order to stay with family and community or due to their care responsibilities.28
T&CM Use as Connection to Culture
Evidence that Indigenous cancer patients employ alternative health paradigms when using TM is consistent with Indigenous holistic conceptions of health.28,36,37,39,42,44 TM was associated with spirituality in all Indigenous cultures and the practice of TM with holistic healing.28,36,37,39,42,44 Prior and colleagues argued that TM usage is an active choice that fits with Indigenous cultural values26 and offers Indigenous patients a safe place for healing that is free of racism.30 Some participants expressed distrust and opposition to conventional treatment:
I said, “No, I’m not going that way. I’m going to stay with the rongoa”. The Māori herbal way.35
The role of TM in maintaining family and community connections was an important coping mechanism for participants; particularly given the common shame and stigma associated with a cancer diagnosis.28,40,42 The communal nature of many TM therapies encourage connection between patients, family, and community.26,28,30,35,38,40,42,44 Many participants desired to use TM,28,35,42,44 however, reported barriers facing urban participants included distance from traditional healers who are predominantly in remote and rural areas,28,35,42,44 uncertainty about accessing TM,28,35 lack of connection to Indigenous culture, and a preference for conventional medicines.
Indigenous Australians spoke of cancer being caused by spiritual forces associated with “payback”28 and TM was seen as essential in countering such forces.28 For some, TM ensured a peaceful passage into the afterlife.32,38 Shahid and colleagues28 stated that many Aboriginal Australians were brought up on missions with strong Christian beliefs that associated TM with paganism:
We didn’t use traditional medicine or anything like that. Because we are not traditional Aboriginal, and our family was Christian based, and so . . . We put our trust on God.28
Impact of Health Professionals’ Views of T&CM
When conventional healthcare providers respected and had knowledge of TM, Indigenous patients’ satisfaction reportedly increased,28,39,41 and they had confidence and trust in conventional medical services.28,39 Participants who used CM and/or TM were reportedly more actively engaged in their treatment plans.26,37
Most studies found that health professionals had little understanding of traditional beliefs and values of Indigenous cultures,26-30,36,39,41,44 which negatively affected communication and patients satisfaction.29,36 Some authors argue that culture and spirituality is central to healing and argue that TM could improve cancer outcomes.28,44 Health professionals need to counter “white man’s authority”27 in health care and better “negotiate a balance between the different cultural paradigms.”26 TM use had variable support from health professionals and there was a perceived lack of respect for TM, which arguably hinders patient-provider communication, reducing the likelihood of patients disclosing their T&CM use. Some participants felt belittled in their choice to use TM,35,39,41 as one participant describes:
I tried to (discuss traditional medicine with providers). They didn’t take the things I said seriously.41
While a minority of health professionals were openly accepting of TM, some participants reported some of their health care providers were personally interested in TM, but reluctant to openly discuss it, as it is generally disapproved of in conventional healthcare settings.41
Discussion
This systematic review reports on the use of T&CM by Indigenous cancer patients in Australia, Canada, New Zealand, and the United States. We identified 21 journal articles25-45 from 18 studies that inform understandings of usage of T&CM across all 4 countries.
Most of the articles in this review were qualitative, with 7 investigating T&CM use exclusively.28,32,33,37,38,44,45 Two32,38 of these were case studies; 4 articles reported TM and/or CM use as a component of a broader study (eg, a study on quality of life)29,35,39,40; and the remainder made some reference to T&CM use within their results.26,27,30,31,36,41,42
The number of quantitative studies was small. All explicitly focused on TM and/or CM use, but only 1 Australian study exclusively sampled an Indigenous population (Queensland, a state of Australia),25 whereas the others sampled34,43 Indigenous people as a subgroup. The estimated extent of T&CM use in the quantitative articles varied from 19% in Indigenous Australians,25 58% in Maori in NZ34 and 29.8% in Native Hawaiians.43 The Australian study may have produced the lowest estimate because of the limitations of having only 5 options for reporting the type of T&CM used in a structured questionnaire, which would miss some types of T&CM. In contrast, the US study43 and the NZ study34 collected much more detailed T&CM information asking 21 and 19 questions, respectively. The estimate of T&CM in Native Hawaiians may be lower relative to the New Zealand study as the study collected data pre-2000, which yields lower estimates relative to studies conducted in the year 2000 or after.7 It is known that restricting CM use to certain categories or treatments reduces estimates,7 and makes comparisons difficult. Therefore, the use of consistent definitions and measurements are recommended using standardized and validated tools such as the International Complementary and Alternative Medicine Questionnaire (I-CAM-Q).46 While standardization is critical improving overall understanding of the types and prevalence of T&CM use among Indigenous people, the validity of such tools to measure the diversity of TM is often questioned.47 It has been previously reported that when evaluating CM use in ethnically diverse populations, ethnic-specific modalities should be recognized7; this should also include TM.
High heterogeneity was observed in the quantitative studies, which is consistent with the 2012 systematic review and meta-analysis of CM use in non-Indigenous cancer patients that reported estimates ranging between nine and 88%.7 These disparate estimates speak to the importance of consistency in survey methods. In light of this, we advocate following the recommendations of Horneber and colleagues’ review7 to improve the relevance, reliability, validity, and reporting of future surveys assessing CM use in cancer patients. These recommendations relate to improvements in the conduct and reporting of future surveys of CM use in cancer patients, and specify 10 quality criteria, with recommendations on how these criteria should be fulfilled and reported.
It is evident from the current thematic analysis that Indigenous populations perceive T&CM as more than just a treatment for physical symptoms, and a cure for cancer. Indigenous people who use T&CM also do so as intrinsic to their wider belief system as a means of maintaining connections with family and community.13 Similarly, Iwasaki et al48 found that Indigenous people in Canada used T&CM as a means to impart spirituality, which they see as sacred and fundamental to their lives; in particular to their ability to cope and heal from their diabetes.48 It is important that health professionals recognize this and be respectful when engaging in conversations about T&CM use. This also speaks to the importance of creating safe spaces in health services to make patients feel comfortable discussing T&CM and disclosing its use. The importance of open and effective patient-clinician communication is paramount to assessing the potential risks and benefits associated with the use of T&CM in the cancer setting.49,50 Indeed, effective, safe, and coordinated care for Indigenous cancer patients relies on shared open decision making and communication across patients, communities, and health care providers. Therefore, it is important for health professionals and policymakers to ensure that the care afforded to Indigenous cancer patients is culturally relevant, safe, effective, and optimal wherever and as much as possible.
Future research in this area would benefit from addressing some of the questions not addressed in the current review. In particular, studies looking at predictors of T&CM use in Indigenous populations. For instance, does the use of T&CM have an impact on the time taken to seek Western medical treatments for cancer? What are Indigenous people’s perceptions and beliefs regarding the ability for T&CM to prevent or cure cancer; does this impact or prompt T&CM use? Its questions like these that will help to form a clearer understanding about the potential motivations and predictors of T&CM use in Indigenous populations. Furthermore, there is a clear lack of research focused on determining the actual percentages of Indigenous people from Australia, Canada, New Zealand, and the United States that are using T&CM either alongside or instead of conventional cancer treatments. Without accurate quantitative data in this area, we are not able to show the significance of this phenomenon.
Conclusion
The current review identified wide variations in the estimates of T&CM use among Indigenous cancer patients, perhaps due to methodological variety across studies. This review highlights the importance of understanding the cultural beliefs of Indigenous people with cancer about the effectiveness and safety of T&CM, and in providing clinical information known about the T&CM treatments to enable Indigenous people to make informed choices. These findings are also a reminder of the importance of reflexivity when working with Indigenous populations, to recognise and set aside health professionals’ own backgrounds, positions, perspectives, paradigms, experiences, and biases, which have an impact on attitudes to T&CM use and patient-practitioner relations. The review results highlight a critical need for further research investigating T&CM use, decision-making and information seeking among Indigenous cancer patients, to help inform health practitioners and policy makers on how to create culturally relevant, safe, effective, and optimal care for Indigenous cancer patients wherever and as much as possible.
Acknowledgments
We would like to acknowledge the contributions of Abbey Diaz, Bronwyn Morris, Lisa Whop, and Suzanne Moore, who provided support and guidance throughout the research process to Alana Gall.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was undertaken under the auspices of the Centre of Research Excellence in Discovering Indigenous Strategies to improve Cancer Outcomes Via Engagement, Research Translation and Training (DISCOVER-TT CRE, funded by the National Health and Medical Research Council #1041111), and the Strategic Research Partnership to improve Cancer control for Indigenous Australians (STREP Ca-CIndA, funded through Cancer Council NSW (SRP 13-01) with supplementary funding from Cancer Council WA). We also acknowledge the ongoing support of the Lowitja Institute, Australia’s National Institute for Aboriginal and Torres Strait Islander Health Research. GG was supported by an NHMRC Early Career Fellowship (#1105399). JA was supported by an ARC Professorial Future Fellowship (#FT140100195). The views expressed in this publication are those of the authors and do not necessarily reflect the views of the funding agencies.
ORCID iDs: Alana Gall  https://orcid.org/0000-0002-2503-2696
https://orcid.org/0000-0002-2503-2696
Stuart Leske  https://orcid.org/0000-0002-4279-1053
https://orcid.org/0000-0002-4279-1053
Jon Adams  https://orcid.org/0000-0002-9901-5717
https://orcid.org/0000-0002-9901-5717
Veronica Matthews  https://orcid.org/0000-0002-1319-257X
https://orcid.org/0000-0002-1319-257X
Kate Anderson  https://orcid.org/0000-0002-1214-2001
https://orcid.org/0000-0002-1214-2001
Sheleigh Lawler  https://orcid.org/0000-0002-5771-0551
https://orcid.org/0000-0002-5771-0551
Gail Garvey  https://orcid.org/0000-0001-5065-5716
https://orcid.org/0000-0001-5065-5716
References
- 1. Teng AM, Atkinson J, Disney G, et al. Ethnic inequalities in cancer incidence and mortality: census-linked cohort studies with 87 million years of person-time follow-up. BMC Cancer. 2016;16:755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Australian Institute of Health and Welfare. Cancer in Australia 2017. Cancer Series No. 101. Cat. No. CAN 100.Canberra, Australia: Australian Institute of Health and Welfare; 2017. [Google Scholar]
- 3. Moore SP, Antoni S, Colquhoun A, et al. Cancer incidence in indigenous people in Australia, New Zealand, Canada, and the USA: a comparative population-based study. Lancet Oncol.2015;16:1483-1492. [DOI] [PubMed] [Google Scholar]
- 4. Guadagnolo BA, Petereit DG, Coleman CN. Cancer care access and outcomes for American Indian populations in the United States: challenges and models for progress. Semin Radiat Oncol. 2017;27:143-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nishri ED, Sheppard AJ, Withrow DR, Marrett LD. Cancer survival among First Nations people of Ontario, Canada (1968-2007). Int J Cancer. 2015;136:639-645. [DOI] [PubMed] [Google Scholar]
- 6. Shahid S, Thompson SC. An overview of cancer and beliefs about the disease in indigenous people of Australia, Canada, New Zealand and the US. Aust N Z J Public Health. 2009;33:109-118. [DOI] [PubMed] [Google Scholar]
- 7. Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11:187-203. [DOI] [PubMed] [Google Scholar]
- 8. Reid R, Steel A, Wardle J, Trubody A, Adams J. Complementary medicine use by the Australian population: a critical mixed studies systematic review of utilisation, perceptions and factors associated with use. BMC Complement Altern Med.2016;16:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fønnebø V, Grimsgaard S, Walach H, et al. Researching complementary and alternative treatments—the gatekeepers are not at home. BMC Med Res Methodol. 2007;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buchanan DR, White JD, O’Mara AM, Kelaghan JW, Smith WB, Minasian LM. Research-design issues in cancer-symptom–management trials using complementary and alternative medicine: lessons from the National Cancer Institute Community Clinical Oncology Program experience. J Clin Oncol. 2005;23:6682-6689. [DOI] [PubMed] [Google Scholar]
- 11. Miller FG, Emanuel EJ, Rosenstein DL, Straus SE. Ethical issues concerning research in complementary and alternative medicine. JAMA. 2004;291:599-604. [DOI] [PubMed] [Google Scholar]
- 12. Robotin MC, Penman AG. Integrating complementary therapies into mainstream cancer care: which way forward? Med J Aust. 2006;185:377-379. [DOI] [PubMed] [Google Scholar]
- 13. Oliver SJ. The role of traditional medicine practice in primary health care within Aboriginal Australia: a review of the literature. J Ethnobiol Ethnomed. 2013;9:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Adams J, Andrews G, Barnes J, Broom A, Magin P. Traditional, Complementary and Integrative Medicine: An International Reader. Basingstoke, England: Palgrave MacMillan; 2012. [Google Scholar]
- 15. Adams J, Barbery G, Lui CW. Complementary and alternative medicine use for headache and migraine: a critical review of the literature. Headache. 2013;53:459-473. [DOI] [PubMed] [Google Scholar]
- 16. Andrews G, Adams J, Segrott J. Complementary and alternative medicine (CAM): production, consumption, research. In: Brown T, McLafferty S, Moon G. eds. A Companion to Health and Medical Geography. West Sussex, England: Blackwell; 2010:587-603. [Google Scholar]
- 17. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). http://www.handbook.cochrane.org. Accessed April 23, 2018.
- 18. Centre for Reviews and Dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York, England: Centre for Reviews and Dissemination/University of York; 2009. [Google Scholar]
- 19. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Veritas Health Innovation. Covidence Systematic Review Software [computer program] . Melbourne, Victoria Australia: Veritas Health Innovation; 2016-2017. [Google Scholar]
- 21. Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13:179-187. [DOI] [PubMed] [Google Scholar]
- 22. Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314:2373-2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008;337:a1035. [DOI] [PubMed] [Google Scholar]
- 24. Wells G, Shea B, O’Connell D, et al. , et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2017. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed April 23, 2018.
- 25. Adams J, Valery PC, Sibbritt D, Bernardes CM, Broom A, Garvey G. Use of traditional indigenous medicine and complementary medicine among Indigenous cancer patients in Queensland, Australia. Integr Cancer Ther. 2015;14:359-365. [DOI] [PubMed] [Google Scholar]
- 26. Prior D. The meaning of cancer for Australian Aboriginal women; changing the focus of cancer nursing. Eur J Oncol Nurs. 2009;13:280-286. [DOI] [PubMed] [Google Scholar]
- 27. Prior D. Don’t mention the ‘C’ word: Aboriginal women’s view of cancer. Aborig Isl Health Work J. 2005;29:7-10. [Google Scholar]
- 28. Shahid S, Bleam R, Bessarab D, Thompson SC. “If you don’t believe it, it won’t help you”: use of bush medicine in treating cancer among Aboriginal people in Western Australia. J Ethnobiol Ethnomed. 2010;6:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shahid S, Finn L, Bessarab D, Thompson SC. Understanding, beliefs and perspectives of Aboriginal people in Western Australia about cancer and its impact on access to cancer services. BMC Health Serv Res. 2009;9:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Poudrier J, Mac-Lean RT. ‘We’ve fallen into the cracks’: Aboriginal women’s experiences with breast cancer through photovoice. Nurs Inq. 2009;16:306-317. [DOI] [PubMed] [Google Scholar]
- 31. Barkwell D. Cancer pain: voices of the Ojibway people. J Pain Symptom Manage. 2005;30:454-464. [DOI] [PubMed] [Google Scholar]
- 32. Clarke V, Holtslander LF. Finding a balanced approach: incorporating medicine wheel teachings in the care of Aboriginal people at the end of life. J Palliat Care. 2010;26:34-36. [PubMed] [Google Scholar]
- 33. Mehl-Madrona L. Narratives of exceptional survivors who work with Aboriginal healers. J Altern Complement Med. 2008;14:497-504. [DOI] [PubMed] [Google Scholar]
- 34. Chrystal K, Allan S, Forgeson G, Isaacs R. The use of complementary/alternative medicine by cancer patients in a New Zealand regional cancer treatment centre. N Z Med J. 2003;116:U296. [PubMed] [Google Scholar]
- 35. Dew K, Signal L, Davies C, et al. Dissonant roles: the experience of Māori in cancer care. Soc Sci Med. 2015;138:144-151. [DOI] [PubMed] [Google Scholar]
- 36. Walker T, Signal L, Russell M, Smiler K, Tuhiwai-Ruru R. The road we travel: Maori experience of cancer. N Z Med J. 2008;121:27-35. [PubMed] [Google Scholar]
- 37. Arthur K, Belliard JC, Hardin SB, Knecht K, Chen CS, Montgomery S. Practices, attitudes, and beliefs associated with complementary and alternative medicine (CAM) use among cancer patients. Integr Cancer Ther. 2012;11:232-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bucher DR. Cultural competence: scholarly nature of clinical practice of nursing. Clin Scholars Rev. 2008;1:110-113. [Google Scholar]
- 39. Canales M. Taking care of self: health care decision making of American Indian women. Health Care Women Int. 2004;25:411-435. [DOI] [PubMed] [Google Scholar]
- 40. Haozous EA, Knobf MT, Brant JM. Understanding the cancer pain experience in American Indians of the Northern Plains. Psychooncology. 2011;20:404-410. [DOI] [PubMed] [Google Scholar]
- 41. Hohl S, Molina Y, Koepl L, et al. Satisfaction with cancer care among American Indian and Alaska Natives in Oregon and Washington state: a qualitative study of survivor and caregiver perspectives. Support Care Cancer. 2016;24:2437-2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Itty TL, Hodge FS, Martinez F. Shared and unshared barriers to cancer symptom management among urban and rural American Indians. J Rural Health. 2014;30:206-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Maskarinec G, Shumay DM, Kakai H, Gotay CC. Ethnic differences in complementary and alternative medicine use among cancer patients. J Altern Complement Med. 2000;6:531-538. [DOI] [PubMed] [Google Scholar]
- 44. Struthers R, Eschiti VS. The experience of indigenous traditional healing and cancer. Integr Cancer Ther. 2004;3:13-23. [DOI] [PubMed] [Google Scholar]
- 45. Struthers R, Eschiti VS. Being healed by an indigenous traditional healer: sacred healing stories of Native Americans.Part II. Complement Ther Clin Pract. 2005;11:78-86. [DOI] [PubMed] [Google Scholar]
- 46. Quandt SA, Verhoef MJ, Arcury TA, et al. Development of an international questionnaire to measure use of complementary and alternative medicine (I-CAM-Q). J Altern Complement Med. 2009;15:331-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Edwards P, Clarke M, DiGuiseppi C, Pratap S, Roberts I, Wentz R. Identification of randomized controlled trials in systematic reviews: accuracy and reliability of screening records. Stat Med. 2002;21:1635-1640. [DOI] [PubMed] [Google Scholar]
- 48. Iwasaki Y, Bartlett J, O’Neil J. Coping with stress among Aboriginal women and men with diabetes in Winnipeg, Canada. Soc Sci Med. 2005;60:977-988. [DOI] [PubMed] [Google Scholar]
- 49. Broom A, Adams J. Oncology clinicians’ accounts of discussing complementary and alternative medicine with their patients. Health (London). 2009;13:317-336. [DOI] [PubMed] [Google Scholar]
- 50. Meiklejohn JA, Adams J, Valery PC, et al. Health professional’s perspectives of the barriers and enablers to cancer care for Indigenous Australians. Eur J Cancer Care (Engl). 2016;25:254-261. [DOI] [PubMed] [Google Scholar]