Abstract
Context. Breast cancer (BC) requires a significant psychological adaptation once treatment is finished. There is growing evidence of how compassion training enhances psychological and physical well-being, however, there are very few studies analyzing the efficacy of compassion-based Interventions on BC survivors. Objective. To study the efficacy of the Cognitively-Based Compassion Training (CBCT) protocol in a BC survivor sample on quality of life, psychological well-being, fear of cancer recurrence, self-compassion, and compassion domains and mindfulness facets. Furthermore, enrollment, adherence, and satisfaction with the intervention were also analyzed. Methods. A randomized clinical trial was designed. Participants (n = 56) were randomly assigned to CBCT (n = 28) or a treatment-as-usual control group (TAU; n = 28). Pre-post intervention and 6-month follow-up measures took place to evaluate health-related quality of life, psychological well-being; psychological stress, coping strategies, and triggering cognitions; self-compassion and compassion; and mindfulness in both intervention and wait-list groups. Results. Accrual of eligible participants was high (77%), and the drop-out rate was 16%. Attendance to CBCT sessions was high and practice off sessions exceeded expectations). CBCT was effective in diminishing stress caused by FCR, fostering self-kindness and common humanity, and increasing overall self-compassion scores, mindful observation, and acting with awareness skillsets. Conclusion. CBCT could be considered a promising and potentially useful intervention to diminish stress caused by FCR and enhance self-kindness, common humanity, overall self-compassion, mindful observation, and acting with awareness skillsets. Nevertheless, future randomized trials are needed and a process of deeper cultural adaptation required.
Keywords: breast cancer, survivorship, compassion training, well-being, self-compassion, fear of cancer recurrence, contemplative training
Introduction
Breast cancer (BC) has been the second most common cancer in the world and the most frequent cancer among women, with an estimated 1.67 million new cancer cases diagnosed in 2012 (25% of all cancers).1 BC has been associated with a number of physical, social, and psychological impairments, such as problems of adaptation, difficulties in communication, or depressive and anxious symptoms.2-4 It has been observed how psychological and emotional stress increased the experience of pain in patients and reduced overall social performance and is a fundamental factor of suicidal ideation and suicide attempts.5,6
In addition to confronting intrusive medical procedures (chemotherapy and/or radiotherapy) and side effects,7 it has been reported how BC treatment requires a significant psychological adaptation.4 Furthermore, once treatment is finished, fear of cancer recurrence (FCR) occurred in around 70% of patients, which has been associated with long-term functional impairments.8,9 In nearly half of the survivors, intrusive thoughts about the disease and its treatment (unwanted thoughts, images and memories) occurred years after successful treatment.10 In such patients, it has been observed that even when the rates of depression decreased, overall well-being did not improve.11 Fatigue and sleep problems were also clinically significant in 60% of patients, which diminished quality of life (QoL).12,13
Nowadays, several psychological interventions have been shown to be beneficial for BC patients.14 Recently, interest in mindfulness-based interventions (MBIs) for BC patients has increased significantly,15,16 especially for those patients who have passed the initial malignancy and its treatment but had to deal with functional, behavioral, and persistent emotional difficulties, such as depression, fatigue, fear of illness recurrence, and cognitive impairments.17,18 A systematic review has shown that a specific MBI for cancer patients can be considered an effective coping strategy that diminishes anxiety, stress, fatigue, general mood, and sleep disturbances and enhances QoL.19
Compassion is a construct closely related to mindfulness20 and can be defined as the desire to alleviate the suffering and its causes in one’s self and those around us.21 When compassion is directed toward oneself, it is called self-compassion.22 This process involves kindness and understanding toward oneself in terms of pain or failure, instead of being self-judgmental; perceiving one’s difficulties as part of the human experience rather than experiencing them with a sense of isolation; and observing the thoughts and painful feelings with mindfulness instead of overidentifying with them.23
Like mindfulness, compassion can be trained using specific techniques and procedures (compassion-based interventions [CBIs]) designed to specifically generate cognitive and emotional compassionate habits.20 Some authors have argued that CBIs could provide useful skills to treat and prevent several psychological difficulties (resources for interpersonal relationships, reduction of depressive symptomatology, reduction of social anxiety, marital conflict, and anger management and deal with the difficulties of being a caregiver).24 In addition, evidence points out that CBI has been associated with decreased inflammatory responding to a psychosocial stressor.25
Different studies have shown how loving-kindness and compassion practices (included in CBIs) have been associated with less physical pain, lower anger, reduced feeling of loneliness, and increased positive emotions.26,27 Other authors have found an increase in positive emotions in everyday experiences after training in compassion, which, in turn, enhanced purpose in life, social connection, and decrease in disease symptoms.28
Today, there are several CBI protocols29-31: Zaragoza University’s Attachment-Based Compassion Therapy,32 Stanford University’s Compassion Cultivation Training,33 Compassion Focused Therapy,34 Mindfulness and Self-compassion,22 Cultivating Emotional Balance Training,35,36 and Cognitively-Based Compassion Training (CBCT).37 Although there are numerous studies on the efficacy of these interventions in healthy populations as well as in clinical settings,38,39 there is not much data of the benefits of CBIs in cancer patients.
CBCT is a secular protocol to teach compassion.21 CBCT has been shown to be effective in reducing hormone levels related to psychoimmunological stress systems as well as regulation of inflammatory processes in the adolescent population with early-life adverse events.25,40-44 Recently, Dodds et al17 found that CBCT, when compared with a wait-list control, resulted in improvements in depression features, functional impairments related to FCR, and avoidance related to traumatic stress and an increase in vitality in a sample of BC survivors (BCSs). Nevertheless, effects of CBCT on QoL have not been thoroughly explored to date in cancer survivors and require further study in other populations.
The main aim of this study was to analyze the efficacy of a CBCT protocol in a randomized clinical trial (RCT; NCT03305952 October 9 to November 2017) on a sample of BCSs. Our primary outcome measure for this study was health-related QoL (physical, social, emotional, and functional domains). Physical and psychological well-being (somatic, depressive, anxious symptomatology), psychological dimensions linked to FCR, mindfulness, self-compassion, and compassion were secondary outcome measures. Moreover, acceptance, adherence, and satisfaction with the intervention were also evaluated.
Methods
Study Design
This RCT compared the benefits of a CBCT intervention versus a treatment-as-usual control group (TAU). The study was approved by FIVO’s Clinical Research Ethics Committee (December 2015) and was conducted in compliance with the study protocol, following the CONSORT statement (Consolidated Standards of Reporting Trials), the Declaration of Helsinki, and good clinical practice. The trial was registered at ClinicalTrials.gov (NCT 03305952) on October 9, 2017.
Sample Size
Sample size was calculated a priori using the G*Power software.45 A total of 42 participants were estimated to be needed in the study to detect a moderate effect size (Cohen’s d = 0.50) on the primary and secondary outcomes, an α error of .05, and a statistical power of 0.80. A moderate effect size was expected taking into account the results of Dodds et al,17 where a compassion-based training in BCSs (compared with a wait-list) showed moderate effect size in QoL-related outcomes (depression, functional impairment, vitality/fatigue) at postintervention. Nevertheless, because we anticipated dropouts, 14 more participants were randomized.
Participants, Recruitment, and Randomization
Eligible participants were recruited and randomized from January 2016 to May 2017. The eligibility criteria were as follows: (1) age between 18 and 75 years, (2) being able to read and write using the Spanish language, (3) history of treated BC within the past 15 years, (4) being free from oncological illness, (5) not receiving any kind of chemotherapy and/or radiotherapy treatment during study, and (6) being free from severe psychiatric disorders assessed with the Mini International Neuropsychiatric Interview (MINI)46 Spanish version.47 Eligible participants were contacted by their personal psychooncologist either by a telephone call or at a periodic psychooncology appointment visit where they were invited to an explanatory meeting of the study. Potential participants were excluded at the beginning of the study for active severe mental disorders (schizophrenia, bipolar disorder, eating disorders, and major depression), substance use disorders, cognitive impairment, or impaired medical condition. Past and current psychiatric and medical history was determined by clinician assessment with the MINI46 Spanish version.47
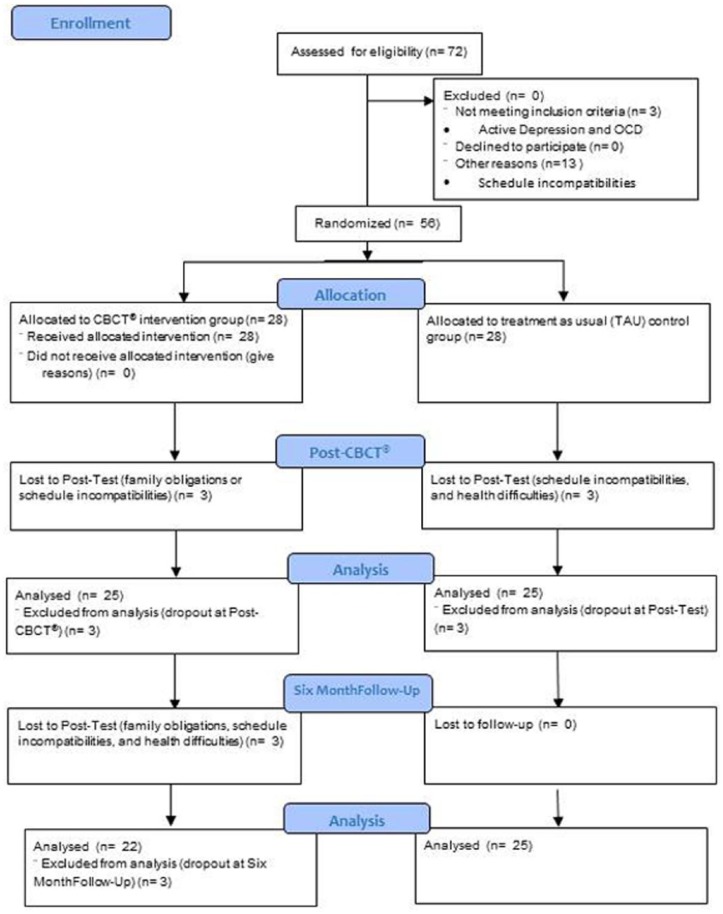
A total of 95 patients were invited to participate in the study, 72 showed interest and 56 met all the inclusion criteria. After signing the informed consent, participants were randomly assigned (by a list of random numbers generated by Research Randomizer software [http://www.randomizer.org]) to either 8 weeks of CBCT or TAU. TAU participants were offered the CBCT protocol at the end of research. Study participants were blinded to group assignment until completion of all baseline assessments. Moreover, outcome assessors, data analysts, and staff were blinded to the allocation at all times during study. Participants were evaluated before and after intervention and at the 6-month follow-up (see Figure 1).
Figure 1.
CONSORT 2010 flow diagram for randomized controlled trial of CBCT versus TAU condition.
Abbreviations: CBCT, Cognitively-Based Compassion Training; OCD, obsessive compulsive disorder.
Measures
Measures were obtained on all study participants (CBCT and TAU) at 3 time points: recruitment into the study pre-test), two months after baseline evaluation (posttest) and at 6 months (follow-up). Data were collected on satisfaction, acceptance, and adherence to the CBCT Program, demographic factors, and medical history.
Psychological variables were assessed using standardized and validated self-administered questionnaires. Primary outcome measures included health-related QoL in BC as measured by the Functional Assessment of Cancer Therapy–Breast Cancer (FACT-B+448; Spanish validation49) using the physical QoL, social/family, and social QoL; emotional QoL; functional QoL; and other concern measures. Secondary measurements included the following: somatic, emotional, and general well-being as measured by the Brief Symptom Inventory (BSI-18),50 Spanish version51; Cancer Recurrence Fear assessed with the Fear of Cancer Recurrence Inventory (FCRI)52; self-compassion evaluated with the Self-Compassion Scale–Short Form,53 Spanish version54; compassion as measured by the The Compassion Scale55; mindfulness facets measured with the Five Facets of Mindfulness Questionnaire–Short Form (FFMQ-SF),56 Spanish validation.57 Acceptance satisfaction and adherence was measured with the CBCT Evaluation Survey.58
Intervention
CBCT was delivered over 8 continuous weeks, in a 2-hour session format through didactics, class discussion, and guided meditation practice. CBCT is a CBI designed by study contemplative investigator Lobsang Tenzin Negi, Ph.D. Although secular in presentation, CBCT is derived from Tibetan Buddhist mind-training (Tibetan lojong) practices. These practices differ in important ways from the MBI practices; whereas MBI practices emphasize the development and maintenance of a nonjudgmental stance toward thought processes and emotional reactions, CBCT practices apply a cognitive, analytic approach. CBCT introduces participants to attentional and mindfulness-based techniques (modules 1-2) to improve attention and awareness before beginning specific compassion practices in training modules 3 to 6. The training protocol modules are sequential and iterative, such that once the 6 modules are completed, each student’s daily meditation practice (guided by audio recordings) begins with a brief period of shamatha to calm and focus the mind, followed by analytical practices designed to challenge unexamined assumptions regarding feelings and actions toward others with a focus on generating spontaneous empathy and compassion for themselves and others. A sequence of 8 sessions included didactic teaching combined with meditations designed to build a suite of skills. The CBCT instructor was a clinically trained psychologist, researcher, and experienced 18-year meditator fulfilling requirements for CBCT teacher certification of Emory University Center for Contemplative Science and Compassion-Based Ethics (CCSCBE). To ensure fidelity, 80% of classes taught were video recorded and reviewed by the CBCT training supervisor at CCSCBE. The supervisor reviewed CBCT class plans weekly. The CBCT teacher manual21 guided class content. CBCT components of each module were as described below.
Module I: Developing attentional stability and mental clarity. This component was delivered in week 1. The foundation for the practice of compassion is the cultivation of a basic degree of refined attention and mental stability. One of the basic skills trained in this module is the deliberate intention for cultivating a state of awareness, relaxation, stillness, and alertness.
Module II: Cultivating insight into the nature of mental experience. This module is trained through week 2. The stabilized mind is then used to gain insight into the nature of the inner world of thoughts, feelings, emotions, and reactions through nonjudgmental awareness and resulting in a mental state of nonreactivity and equanimity.
Module III: Cultivating self-compassion. Participants tune in their innate aspirations for happiness and well-being as well as those for freedom from unhappiness and dissatisfactions. This is progressively realizing which mental states contribute to well-being and which ones bring about anxiety, disappointment, and dissatisfaction. Afterward, participants learn to bring to mind the determination and skills to transcend the mental patterns and emotional states that promote distress. These mindsets and skillsets are covered in weeks 3 and 4.
Module IV: Developing equanimity and impartiality. This module focuses on creating balanced relationships with others promoting the initial mental and emotional conditions for constructive social connections through week 5. This is relevant because of the social disconnection that human beings experience when going through traumatic and stressful life events.
Module V: Developing appreciation, affection, and empathy for others. Social connection and gratitude is fostered through the emotional insight of interdependence. This prevents the feeling of isolation. Social connection and gratitude weakens self-centeredness and strengthens endearment and affection toward others, which serves as the catalyst for compassion. Endearment and affection foster a perception of the world based on kindness and not on threat. These emotional states were trained and fostered through week 6.
Module VI: Realizing engaged compassion. During weeks 7 and 8, patients were taught and invited to rest in a compassionate state of mind. The primary focus of this session was to cultivate the essential skillsets and mindsets for interacting in a proactive way with personal and social difficulties, preventing burnout and fostering a motivational readiness to act altruistically.
Each session included lecture, discussion, experiential exercises, and guided meditations. Over the intervention, participants were led through the entire series of integrated, cumulative meditations and provided with guided recordings for each module to support the systematic development of compassion. In between class sessions, participants were encouraged to meditate daily using the recorded meditations and to gradually increase both the length of time for an individual meditation session as well as the cumulative amount of practice time.
The TAU control group continued with their normal rehabilitation program, attendance at briefings given at FIVO, pharmacological treatment, and psychological counseling. TAU participants were offered the CBCT course at the end of research.
Data Analyses
Group differences at baseline on demographic characteristics and clinical variables were analyzed using independent-samples t-tests for continuous data and χ2 tests for categorical variables. Intent-to-treat mixed-models analyses without any ad hoc imputation were used to handle missing data.59 This approach is appropriate for RCTs with multiple time points and pre-to-post-only designs and does not assume that the last measurement is stable (the last observation carried forward assumption). This method is conducted using all available observations.60,61 For each outcome measure, a linear mixed model was implemented with Time (pre, post, and 6-month follow-up) as within-group factor and Group (CBCT and TAU) as between-group factor using the MIXED procedure with 1 random intercept per subject. An identity covariance structure was specified to model the covariance structure of the random intercept. Significant effects were followed up with pairwise comparisons. Effect sizes (Cohen’s d; 95% CI) were calculated for within- and between-group comparisons.62-65 All statistical analyses were performed using IBM SPSS version 23 for Windows.
Results
Participant Flow
The final sample was composed of 56 women between 39 and 70 years old (mean age = 52.13 years [SD = 6.96]; 100% female; see Figure 1). During the study, 3 of the 28 participants from the CBCT condition dropped out because of family obligations or schedule incompatibilities at posttest, and 3 more participants could not continue with the study at follow-up because of family obligations, schedule incompatibilities, and health difficulties. Regarding TAU condition, 3 of the 28 participants dropped out because of schedule incompatibilities and health difficulties at posttest. There were no dropouts at follow-up in the TAU group (for more details, please see Figure 1).
Baseline Data
Table 1 shows sociodemographic characteristics and Table 2 clinical features for the CBCT and TAU groups. There were no significant differences between groups in all demographic characteristics or outcome measures at baseline, except for clinical severity (oncological stage when first diagnosed) and Insight factor from the FCRI: F(1, 97.17) = 4.176; P < .05. As for clinical severity when first diagnosed, the CBCT group had a larger number of participants with oncological stage III when compared with the TAU group. The CBCT group also had larger scores for the Insight factor when compared with the TAU group.
Table 1.
Sociodemographic and Clinical Data in CBCT and WL Groups.
| Sociodemographic and Clinical Data | CBCT (n = 28) | WL (n = 28) | Student t/χ2 | P |
|---|---|---|---|---|
| Age (in years) | 51.64 (6.87) | 52.63 (7.16) | 0.52 | .60 |
| Time since first diagnosis (years) | 11.32 (1.44) | 10.46 (2.90) | −1.40 | .17 |
| Oncological stage at first diagnosis | 18.49 | .047 | ||
| I | 1 (3.6) | 3 (10.7) | ||
| II | 13 (46.4) | 18 (64.3) | ||
| III | 14 (50) | 7 (25) | ||
| IV | — | — | ||
| Breast cancer treatments | 41.48 | .21 | ||
| Partial mastectomy (removal of tumor along with some of the breast tissue around it) | 5 (17.9) | 7 (25) | ||
| Total mastectomy (removal of entire breast) | 17 (60.7) | 12 (42.9) | ||
| Radiotherapy | 19 (67.9) | 18 (64.3) | ||
| Chemotherapy | 25 (89.3) | 23 (82.1) | ||
| Other | 14 (50) | 18 (64.3) | ||
| Educational level | 2.12 | .55 | ||
| Elementary school or less | 7 (25) | 6 (21.40) | ||
| Middle school | 1 (3.6) | 1 (3.60) | ||
| High school | 7 (25) | 12 (42.9) | ||
| University studies or more | 13 (46.4) | 9 (32.1) | ||
| Employment status | 1.12 | .77 | ||
| Employed | 17 (60.7) | 18 (64.3) | ||
| Unemployed | 1 (3.6) | 0 (0) | ||
| Retired | 4 (14.3) | 5 (17.9) | ||
| Off work | 6 (21.4) | 5 (17.9) |
Table 2.
Participants’ Enrollment, Satisfaction, Adherence to Program, and Contemplative Practice Experience Data in the CBCT and TAU Groups.a
| Data Description | |
|---|---|
| Number of sessions attended | |
| 0 | 0 (0.00) |
| 1 | 1 (3.55) |
| 2 | 0 (0.00) |
| 3 | 0 (0.00) |
| 4 | 0 (0.00) |
| 5 | 3 (10.70) |
| 6 | 5 (17.90) |
| 7 | 9 (32.15) |
| 8 | 10 (35.70) |
| Mean time of practice after session (minutes) | |
| 0 | 2 (7.15) |
| 9 | 1 (3.55) |
| 12 | 3 (10.70) |
| 15 | 6 (21.40) |
| 18 | 4 (14.30) |
| More than 24 | 12 (42.90) |
| Percentage of home practice with meditation recordings | |
| 0% | 2 (7.15) |
| 10% | 1 (3.55) |
| 20% | 0 (0.00) |
| 30% | 0 (0.00) |
| 40% | 0 (0.00) |
| 50% | 0 (0.00) |
| 60% | 3 (10.70) |
| 70% | 0 (0.00) |
| 80% | 4 (14.30) |
| 90% | 2 (7.15) |
| 100% | 16 (57.15) |
| Frequency of practice (days) | |
| 0 | 2 (7.15) |
| 1 | 2 (7.15) |
| 2 | 5 (17.90) |
| 3 | 6 (21.40) |
| 4 | 4 (14.30) |
| 5 | 5 (17.90) |
| 6 | 2 (7.15) |
| 7 | 2 (7.15) |
| Intention to attend to future CBCT groups | |
| Yes | 25 (89.30) |
| No | 3 (10.70) |
| Intention to continue CBCT personal practice | |
| Yes | 25 (89.30) |
| No | 3 (10.70) |
| CBCT recommendation to others | |
| Yes | 26 (92.9) |
| No | 2 (7.10) |
| Satisfaction with instructor | |
| Yes | 26 (92.9) |
| No | 2 (7.10) |
Abbreviations: CBCT, Cognitively-Based Compassion Training; TAU, treatment-as-usual.
Percentage shown in parentheses.
Health-Related QoL in BC Survival
Even though, no Time × Group effect was observed in any of the health-related QoL subscales that compose FACT-B+4 (all P > .05), a Time × Group tendency was observed for social/family QoL [F(2, 94.758) = 2.710; P = .072], where participants allocated to the CBCT group scored somewhat higher than the TAU control group. Results from within-group comparisons revealed a significant pre-to-post change for emotional and general QoL in the CBCT group with moderate effect sizes (−0.56 and −0.46, respectively). No significant changes were found in TAU (Table 3).
Table 3.
Within-Group Comparisons and Effect Sizes at Preintervention, Postintervention, and 6-Month Follow-up.a
| CBCT |
TAU |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Preintervention (n = 28) | Postintervention (n = 26) | Follow-up (n = 22) | Preintervention vs Postintervention, Mean Difference d [95% CI] | Preintervention vs FW, Mean Difference d [95% CI] | Preintervention (n =28) | Postintervention (n = 25) | Follow-up (n = 25) | Preintervention vs Postintervention, Mean Difference d [95% CI] | Preintervention vs FW, Mean Difference d [95% CI] | |
| FACTGP | 18.93 (5.70) | 21.50 (3.93) | 21.27 (4.09) | −2.24, −0.44 [−0.87, −0.01] | −2.20, −0.40 [−0.89, 0.09] | 17.57 (5.96) | 17.68 (6.16) | 17.52 (5.34) | −0.08, −0.02 [−0.24, 0.20] | 0.07, 0.01 [−0.35, 0.36] |
| FACTGS | 17.11 (6.05) | 19.23 (5.51) | 18.82 (5.79) | −1.81, −0.34 [−0.65, −0.03] | −1.12, −0.27 [−0.59, 0.04] | 17.56 (5.46) | 16.60 (5.39) | 16.40 (5.07) | 0.86, 0.17 [−0.07, 0.41] | 1.06, 0.21 [−0.14, 0.55] |
| FACTGE | 13.07 (5.26) | 16.12 (4.09) | 14.00 (4.69) | −2.84,** −0.56 [−0.92, −0.20] | −0.68, −0.17 [−0.56, 0.22] | 13.39 (4.94) | 14.72 (4.63) | 13.32 (5.32) | −1.33, −0.26 [−0.46, −0.07] | 0.07, 0.01 [−0.40, 0.43] |
| FACTGF | 15.75 (6.10) | 17.54 (3.20) | 17.64 (4.61) | −1.55, −0.29 [−0.72, 0.15] | −1.68, −0.30 [−0.76, 0.16] | 13.82 (5.68) | 15.40 (4.39) | 15.56 (4.81) | −1.41, −0.27 [−0.55, 0.01] | −1.57, −0.30 [−0.75, 0.16] |
| FACTGEN | 64.86 (20.04) | 74.38 (11.48) | 71.73 (15.45) | −8.45,* −0.46 [−0.82, −0.10] | −5.73, −0.33 [−0.73, 0.06] | 62.85 (15.86) | 64.40 (14.73) | 62.80 (17.63) | −1.60, −0.09 [−0.33, 0.14] | 0.00, 0.00 [−0.40, 0.41] |
| BSI SOM | 7.39 (5.87) | 4.88 (4.04) | 5.64 (4.18) | 2.00, 0.42 [0.11, 0.72] | 1.53, 0.29 [−0.16, 0.74] | 8.93 (5.47) | 8.64 (5.70) | 8.32 (5.03) | 0.31, 0.05 [−0.17, 0.27] | 0.63, 0.11 [−0.24, 0.46] |
| BSI DEP | 9.18 (7.13) | 5.65 (5.27) | 5.14 (5.19) | 2.91,* 0.49 [0.11, 0.87] | 3.55,* 0.55 [0.13, 0.97] | 9.36 (6.24) | 7.76 (6.54) | 8.56 (5.87) | 1.68, 0.25 [0.00, 0.50] | 0.88, 0.12 [−0.16, 0.41] |
| BSI ANX | 8.21 (5.93) | 6.15 (5.01) | 6.09 (5.38) | 1.69, 0.34 [−0.05, 0.73] | 1.96, 0.35 [−0.12, 0.81] | 9.00 (6.51) | 7.88 (5.94) | 7.56 (5.49) | 1.27, 0.17 [−0.02, 0.35] | 1.59, 0.21 [−0.10, 0.53] |
| GSI | 24.79 (17.55) | 16.69 (13.12) | 16.86 (13.12) | 6.51,* 0.45 [0.10, 0.79] | 6.98,* 0.44 [0.00, 0.88] | 27.29 (16.84) | 24.28 (16.74) | 24.44 (15.26) | 3.28, 0.17 [−0.03, 0.37] | 3.12, 0.16 [−0.14, 0.47] |
| FCRTRIG | 13.11 (9.30) | 13.04 (8.12) | 13.59 (9.28) | 0.00, 0.01 [−0.32, 0.33] | −0.49, 0.14 [−0.32] | 11.43 (8.81) | 12.32 (8.98) | 13.44 (7.42) | −1.08, −0.10 [−0.27, 0.08] | −2.20, −0.22 [−0.47, 0.03] |
| FCRPSTR | 8.39 (5.12) | 4.81 (3.43) | 5.95 (4.50) | 3.41,*** 0.68 [0.36, 1.00] | 2.34,* 0.46 [0.06, 0.86] | 7.93 (4.45) | 7.40 (3.96) | 8.16 (4.05) | 0.57, 0.12 [−0.14, 0.37] | −0.20, −0.05 [−0.41, 0.31] |
| FCRCOP | 22.11 (5.41) | 23.96 (3.84) | 21.36 (4.75) | −1.61, −0.33 [−0.89, 0.22] | 1.07, 0.13 [−0.27, 0.54] | 23.39 (5.69) | 23.72 (6.26) | 22.76 (4.56) | −0.08, −0.06 [−0.26, 0.15] | 0.88, 0.11 [−0.22, 0.44] |
| FCRINS | 7.18 (5.29) | 6.65 (4.91) | 6.95 (5.20) | 0.43, 0.10 [−0.11, 0.31] | 0.12, 0.04 [−0.14, 0.22] | 6.96 (5.05) | 7.00 (4.75) | 6.88 (3.52) | −0.04, −0.01 [−0.23, 0.22] | 0.08, −0.02 [−0.27, 0.30] |
| SCS_SK | 2.59 (1.11) | 3.27 (0.86) | 3.34 (0.78) | −0.63,* −0.60 [−1.08, −0.11] | −0.70,** −0.66 [−1.2, −0.11] | 2.79 (1.19) | 2.72 (1.19) | 2.42 (1.09) | 0.04, 0.06 [−0.20, 0.31] | 0.34, 0.30 [−0.10, 0.70] |
| SCS_SJ | 3.43 (1.26) | 2.79 (1.03) | 2.70 (1.01) | 0.57,* 0.49 [0.07, 0.92] | 0.72,** 0.56 [0.19, 0.93] | 3.34 (1.27) | 2.94 (1.42) | 3.28 (1.01) | 0.40, 0.31 [0.01, 0.60] | 0.06, 0.05 [−0.24, 0.33] |
| SCS_CH | 2.70 (1.02) | 3.27 (1.03) | 3.45 (0.82) | −0.54,* −0.54 [−1.01, −0.07] | −0.75,** −0.71 [−1.18, −0.25] | 3.16 (1.20) | 2.82 (1.00) | 2.84 (0.98) | 0.32, 0.28 [−0.20, 0.75] | 0.30, 0.26 [−0.18, 0.70] |
| SCS_I | 2.98 (1.21) | 2.62 (1.18) | 2.64 (1.13) | 0.29, 0.29 [−0.06, 0.64] | 0.31, 0.27 [−0.13, 0.67] | 3.02 (1.26) | 2.66 (1.26) | 3.06 (0.93) | 0.35, 0.28 [0.03, 0.52] | −0.49, −0.03 [−0.40, 0.34] |
| SCS_M | 2.82 (1.02) | 3.23 (0.82) | 3.20 (0.87) | −0.36, −0.39 [−0.87, 0.08] | −0.35, −0.36 [−0.81, 0.08] | 3.16 (1.11) | 3.10 (1.11) | 3.00 (0.90) | 0.07, 0.05 [−0.30, 0.41] | 0.17, 0.14 [−0.18, 0.46] |
| SCS_OI | 3.39 (1.17) | 2.75 (0.96) | 2.84 (0.99) | 0.60,* 0.53 [0.16, 0.90] | 0.52, 0.46 [0.14, 0.78] | 3.42 (1.17) | 3.18 (1.33) | 3.32 (1.07) | 0.27, 0.20 [−0.10, 0.50] | 0.13, 0.08 [−0.33, 0.50] |
| SCS_TOTAL | 2.71 (0.90) | 3.27 (0.76) | 3.30 (0.73) | −0.49,** −0.60 [−0.98, −0.23] | −0.55,** −0.64 [−1.00, −0.28] | 2.89 (0.91) | 2.98 (0.93) | 2.77 (0.69) | −0.10, −0.10 [−0.33, 0.14] | 0.11, 0.13 [−0.20, 0.45] |
| COMP_ TOTAL | 20.41 (2.89) | 22.01 (2.36) | 21.76 (2.75) | −1.53,* −0.54 [−0.95, −0.13] | −1.49, −0.45 [−0.90, −0.01] | 19.95 (2.68) | 20.87 (2.80) | 20.70 (3.15) | −0.88, −0.33 [−0.64, −0.03] | −0.71, −0.27 [−0.68, 0.14] |
| FFMQ_OB | 12.03 (2.85) | 14.54 (2.93) | 13.50 (2.81) | −2.41,*** −0.86 [−1.26, −0.45] | −1.25, −0.50 [−0.93, −0.07] | 12.89 (2.71) | 13.28 (3.82) | 12.20 (3.14) | −0.41, −0.14 [−0.34, 0.06] | 0.67, 0.25 [−0.07, 0.56] |
| FFMQ_D | 13.07 (4.45) | 13.62 (3.32) | 13.09 (4.02) | −0.37, −0.12 [−0.36, 0.12] | −0.13, 0.00 [−0.25, 0.24] | 13.25 (3.28) | 12.84 (3.39) | 13.20 (2.93) | 0.37, 0.12 [−0.18, 0.42] | 0.01, 0.01 [−0.39, 0.42] |
| FFMQ_AW | 11.68 (3.62) | 11.92 (3.31) | 11.82 (3.59) | −0.29, −0.06 [−0.40, 0.27] | −0.54, −0.04 [−0.45, 0.37] | 12.14 (3.57) | 11.88 (4.10) | 10.32 (2.87) | 0.14, 0.07 [−0.18, 0.32] | 1.70,* 0.50 [0.14, 0.85] |
| FFMQ_NJ | 11.93 (3.83) | 12.38 (3.68) | 13.00 (4.07) | −0.42, −0.11 [−0.47, 0.24] | −0.93, −0.27 [−0.62, 0.07] | 10.96 (4.26) | 12.20 (4.62) | 11.04 (4.17) | −1.12, −0.28 [−0.52, −0.05] | 0.05, −0.02 [−0.36, 0.32] |
| FFMQ_NR | 11.54 (2.50) | 12.12 (2.49) | 12.27 (2.96) | −0.51, −0.23 [−0.68, 0.23] | −0.59, −0.28 [−0.67, 0.10] | 11.54 (2.47) | 11.76 (2.37) | 10.92 (2.84) | −0.15, −0.09 [−0.50, 0.32] | 0.69, 0.24 [−0.12, 0.60] |
Abbreviations: CBCT = Cognitively-Based Compassion Training; TAU, treatment as usual control group; FW, 6-month follow-up; FACTGP, Physical quality of life; FACTGS, Social/Family quality of life; FACTGE, Emotional quality of life; FACTGF, Functional quality of life; FACTGEN, General quality of life; BSI Som, Brief Symptom Inventory somatic symptoms; BSI Dep, BSI depressive symptoms; BSI Anx, BSI anxiety symptoms; GSI, General Symptom Index; FCRTRIG, Fear of Cancer Recurrence triggers; FCRPSTR, FCR psychological stress; FCRCOP, FCR coping strategies; FCRINS, FCR insight; SCS_SK, Self-Compassion Scale self-kindness; SCS_SJ, SCS self-judgment; SCS_CH, common humanity; SCS_I, SCS isolation; SCS_M, SCS mindfulness; SCS_OI, SCS overidentification; SCS_Total, SCS total; COMP_ TOTAL, Total Compassion Score; FFMQ_OB, Five Facets of Mindfulness Questionnaire observe; FFMQ_D, FFMQ describe; FFMQ_AW, FFMQ awareness; FFMQ_NJ, FFMQ nonjudgmental; FFMQ_NR, FFMQ NONREACTIVITY.
Means and SDs are represented; d: Cohen’s d; *P < .05, **P < .01, ***P < .001.
Somatic, Emotional, and General Well-being
In relation to our secondary outcomes, no significant Time × Group effect was observed for any of the BSI-18 factors. However, within-group comparisons revealed significant pre-to-post and pre-to-follow-up improvements for depressive and general distress symptomatology in the CBCT group, with moderate effect sizes (Cohen’s d ranging from 0.44 to 0.55, respectively); no significant changes were observed in the TAU group (Table 3).
Cancer Recurrence Fear
Psychological Stress factor from the FCRI showed significant Time × Group interaction: F(2, 96.863) = 3.521; P < .05. No significant interaction effects were found for any other of the FCRI factors (all P > .05). Within-group comparisons showed significant pre-post and pre-to-follow-up changes for psychological stress in the CBCT group, with effects sizes of 0.68 and 0.49, respectively. No significant changes were found in the TAU group (Table 3).
Self-compassion
A significant Time × Group interaction was seen for self-kindness [F(2, 97.453) = 5.769; P < .01], common humanity [F(2, 98.323) = 6.161; P < .01], and Self-compassion Scale overall score [F (2, 96.277) = 5.423; P < .01]. Overall, participants scored higher on those measures at post- and follow-up time compared with TAU, although no significant differences were found except for self-kindness, indicating that CBCT scored significantly higher compared with TAU at the 6-month follow-up (P < .05; Cohen’s d = 0.94; 95% CI = [0.34, 1.55]).Within-group analyses showed significant pre-to-post changes for self-kindness, self-judgment, common humanity, over identification, and self-compassion overall scores in the CBCT group (Table 3). These changes were maintained at follow-up for all those outcomes, except for the overidentification subscale. In the TAU group, nonsignificant changes were found.
Compassion
Results showed no significant Time × Group effect. Within-group comparisons revealed a significant pre-to-post change in the CBCT group with moderate effect size (d = 0.75) and nonsignificant change in the TAU group (Table 3).
Mindfulness Facets
Results showed a significant interaction of Time × Group for observing (F[2, 96.052] = 4.709; P < .05) and awareness facets (F[2, 98.598] = 3.444; P < .05) from FFMQ. Participants in the CBCT scored significantly higher than those in the TAU group for observing at postintervention (P < .05; d = 0.37; 95% CI [−0.19, 0.92]) and follow-up (P < .05; d = 0.43; 95% CI [−0.15, 1.01]) as well as for awareness at follow-up (P < .05; d = 0.45; 95% CI [−0.12, 1.04]). Within-group comparisons revealed a significant pre-post change for observing in CBCT, with large effect size (−0.86), and a significant preintervention to follow-up change for awareness in TAU, with moderate effect size (0.50; Table 3).
Acceptance Satisfaction and Adherence
In the CBCT group, 27 participants (96.4%) attended 5 or more of the 8 sessions of the program. In all, 25 (89.30%) participants practiced at home from 12 to 24 or more minutes in total, across all 8 weeks; 25 (89.30%) participants practiced on their own with the meditation recordings, and 9 (32.15%) of the 28 participants used the prerecorded meditation between 60% and 90% of the time (for more details see Table 2); and 13 (46.50%) participants practiced from 4 to 7 days a week. A total of 25 participants (89.30%) indicated that they would participate in future CBCT courses if offered and that they would continue to practice after the course program ended; 26 (92.90%) said that they were satisfied with the program and that they would recommend CBCT to other participants, and confirmed that they felt satisfied with the instructor’s ability to facilitate the course sessions.
Discussion
The present article aimed to analyze the efficacy of a CBCT program to improve variables associated with health-related QoL (physical, social, emotional, and functional dimensions); somatic, depressive, and anxious symptomatology; psychological dimensions linked to FCR; and self-compassion, compassion, and mindfulness trait in a BCS clinical sample compared with a TAU control group after the intervention and a 6-month follow-up. Feasibility, acceptance, and satisfaction of this program was also evaluated.
Our findings suggest that an 8-week CBCT protocol is efficacious in reducing psychological stress related to FCR and increasing self-kindness, common humanity, general self-compassion, observation, and acting with awareness mindfulness skills. Regarding QoL, CBCT was not shown to be efficacious compared with TAU; however, in the pre-post analysis, it shows effects on emotional and general factors. Regarding symptoms, participants allocated to the CBCT intervention did show reductions in depressive and general distress symptomatology compared with those in the TAU group; however, improvements in pre-post analysis in the CBCT group were observed in depressive and general symptomatology after intervention and at 6-month-follow-up. Growing literature has validated interventions with active mindfulness components to be effective for diminishing depression and increasing general psychological well-being in oncological survivorship.66 More specifically, previous studies with CBCT have also been validated as a promising intervention for depressive symptomatology in the healthy population67 and specific clinical oncological settings.17
It is widely known how once the physical threat of cancer is surpassed, FCR is one of the most significant sources of distress in BCSs.68-71 Previous studies showed how implementing a contemplative practice in daily life resulted in significant reductions in FCR which, in turn, mediated significant reductions in perceived stress and anxiety.72 CBCT has shown hints of significant improvements in functional impairment associated with fear of recurrence.17 In the present study, CBCT has proved to be efficacious in facilitating motivational, attentional, cognitive, and emotional resources and enables BCSs to cope with the distress that evokes thoughts, images, or memories related to FCR.
In relation to self-compassion domains, CBCT proved to improve the ability to be kind in the face of one’s own inadequacies and vulnerabilities, not feel alienated when experiencing difficulties (self-kindness and common humanity, self-compassion traits), and aid overall self-compassion. These self-compassion dimensions have been strongly related to well-being, happiness, and resilience in different studies.15,36,73-78 According to Neff and colleagues,53,79 the constituents of self-compassion that have been highlighted in their studies are central to fostering a self-compassionate mindset when coping with one’s own inadequacies, personal failures, and external circumstances that are hard to bear. This perspective realizes imperfection as part of the shared human condition, so that one’s weaknesses are seen from a broad, inclusive perspective. Similarly, difficult life circumstances are framed in light of the shared human experience, fostering connection instead of disconnection and isolation when experiencing suffering. In this sense, when assuming a non–self-compassionate outlook, people tend to feel isolated, harsh, and emotionally reactive when considering personal flaws, weaknesses, or hardship.
CBCT was not seen to be efficacious compared with TAU in the increase of compassion scores; however, data show significant improvements in compassion at posttest for the CBCT group with medium effect size, and no significant improvements for TAU. These findings are in line with previous results in compassion measures related to CBIs.80,81 These results could be explained by several factors, such as the length of the intervention; other CBCT studies have been done with an extended format.67 This extension is relevant given the complex and numerous psychosocial and physiological impairments in survivorship when trying to adapt CBCT in future studies. Furthermore, more efforts should be focused on adapting the CBCT program to Latin-Mediterranean-Catholic cultural contexts. In these contexts, compassion as proposed by CBIs is relatively new and needs a longer time to be integrated into the individual and collective schema.
Regarding mindfulness facets, data reveal that CBCT is an effective intervention that fosters abilities to observe external and internal phenomena or stimuli with awareness (mindful observation factor, FFMQ trait) and act mindfully in daily activities (acting with awareness scores, FFMQ trait). Although CBCT is a protocol that uses meditation to generate mindsets and skillsets related to well-being, no other interaction in mindfulness facets were reported as significant in this study. This may be a result of the orientation of this program, which pays special attention and care to the cognitive strategies and techniques that have been tested to enhance well-being.* However, efforts to accurately assess mindfulness facets are highly needed in contemplative training programs that include analytical approaches that enhance well-being.84-87 We think that this point is relevant because of the importance of the cognitive constituents that have been highlighted as central in compassion mind training.88,89
To sum up, results from this RCT study also suggest that CBCT is a feasible and highly satisfactory 8-week intervention among BCSs. Moreover, the adherence rate was higher than in previous studies with CBCT and BCSs.17 In this previous study, adherence was assessed in 2 ways: logged home practice time between participant and attendance at weekly classes as recorded by the teacher. In the present study, data suggest that CBCT has high rates of attendance, high rates of adherence to home practice, and high scores in minutes of practice between sessions. Moreover, most of the participants had a high rate of practice frequency a day after finishing each session. A high percentage of these participants wish to continue with CBCT training if offered and would recommend CBCT to other patients. Data confirm a high level of satisfaction with the program. Finally, most of the participants intend to continue practicing CBCT on a daily basis.
Several limitations and methodological issues with this study should be mentioned: (1) The results might be influenced by participants’ contemplative experience prior to the study, and this is one variable that should be taken into account in future studies; (2) considering that this is the first CBCT study conducted outside an Anglo-Saxon context, refinement in the adaptation process to Latin-Mediterranean-Catholic cultural contexts must be examined. This will be included in future analyses with samples of Spanish BCSs and CBCT.
However, caution must be exercised when considering the effects of compassion training in this study; results suggest that CBCT could be considered as a promising protocol that aids BCSs in coping with the stress evoked by FCR, fosters self-compassion facets that promote well-being and resilience, and nurtures mindful abilities.
This research is another call for deepening scientific knowledge and paying more attention to the mechanisms and implications of training in compassion. One of the main goals of compassion programs is to cultivate skills to cope with internal (feelings, thoughts, sensations, memories, self-criticism, etc) and external (lost, sickness, death, criticism) difficulties and turn them into opportunities for growth from the basis of a selflessness perspective. According to a theoretical construct discussed by some authors,90,91 the abilities embedded in CBIs offer a selflessness perspective that cultivate conative, attentional, cognitive, and affective abilities that enhance authentic and lasting well-being.92 Moreover, as far as we know, this is one of the first studies to evaluate the effects of a CBI in an oncological survivor sample and the first study to measure the efficacy of CBCT in a Latin-Mediterranean-Catholic setting.
Acknowledgments
For their crucial predisposition and help we extend our deepest gratitude to the breast cancer survivors who participated in this study; to Sally E. Dodds, PhD, and Thaddeus W. W. Pace, PhD, of the College of Nursing at University of Arizona; and Carol Beck and Timothy Harrison of the Emory University Center for Contemplative Science and Compassion-Based Ethics. Thanks also to the IVO for their support with facilities and to the Barcelona EsMindfulness Institute for its help. CiberObn is an initiate of the ISCIII.
Footnotes
Authors’ Note: Trial registration: Clinicaltrials.gov: NCT03305952. Trial registration date October 9, 2017.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [DOI] [PubMed] [Google Scholar]
- 2. Nasser M, Baistow K, Treasure J. The Female Body in Mind: The Interface Between the Female Body and Mental Health. New York, NY: Routledge; 2007. [Google Scholar]
- 3. Moorey S, Greer S. Cognitive Behaviour Therapy for People With Cancer. New York, NY: Oxford University Press; 2002. [Google Scholar]
- 4. Bellver A, Sánchez-Cánovas J, Santaballa A, Munárriz B, Pérez-Fidalgo JA, Montalar J. Mujeres con cáncer de mama: evaluación del afecto positivo y negativo y valoración de un programa de intervención psicológica en el ámbito hospitalario. Psicooncología. 2009;6:139-154. [Google Scholar]
- 5. Rosenfeld B, Krivo S, Breitbart W, Chochinov HM. Suicide, assisted suicide, and euthanasia in the terminally ill. In: Chochinov HM, Breitbart W. eds. Handbook of Psychiatry in Palliative Medicine. New York, NY: Oxford University Press; 2000:51-62. [Google Scholar]
- 6. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19-28. [DOI] [PubMed] [Google Scholar]
- 7. Buick DL, Petrie KJ, Booth R, Probert J, Benjamin C, Harvey V. Emotional and functional impact of radiotherapy and chemotherapy on patients with primary breast cancer. J Psychosoc Oncol. 2000;18:39-62. [Google Scholar]
- 8. Thewes B, Brebach R, Dzidowska M, Rhodes P, Sharpe L, Butow P. Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psychooncology. 2014;23:390-396. [DOI] [PubMed] [Google Scholar]
- 9. Thewes B, Butow P, Bell M, et al. ; FCR Study Advisory Committee. Fear of cancer recurrence in young women with a history of early-stage breast cancer: a cross-sectional study of prevalence and association with health behaviours. Support Care Cancer. 2012;20:2651-2659. [DOI] [PubMed] [Google Scholar]
- 10. Bleiker EM, Pouwer F, van der Ploeg HM, Leer JH, Adèr HJ. Psychological distress two years after diagnosis of breast cancer: frequency and prediction. Patient Educ Couns. 2000;40:209-217. [DOI] [PubMed] [Google Scholar]
- 11. Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ. 2005;330:702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bower JE, Ganz PA, Desmond KA, Rowland JH, Meyerowitz BE, Belin TR. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743-753. [DOI] [PubMed] [Google Scholar]
- 13. Rosedale M. Survivor loneliness of women following breast cancer. Oncol Nurs Forum. 2009;36:175-183. [DOI] [PubMed] [Google Scholar]
- 14. Matthews H, Grunfeld EA, Turner A. The efficacy of interventions to improve psychosocial outcomes following surgical treatment for breast cancer: a systematic review and meta-analysis. Psychooncology. 2017;26:593-607. [DOI] [PubMed] [Google Scholar]
- 15. Baer RA, Lykins ELB, Peters JR. Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. J Posit Psychol. 2012;7:230-238. [Google Scholar]
- 16. Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21:1038-1049. [DOI] [PubMed] [Google Scholar]
- 17. Dodds SE, Pace TW, Bell ML, et al. Feasibility of Cognitively-Based Compassion Training (CBCT) for breast cancer survivors: a randomized, wait list controlled pilot study. Support Care Cancer. 2015;23:3599-3608. [DOI] [PubMed] [Google Scholar]
- 18. Huang H, He M, Wang H, Zhou M. A meta-analysis of the benefits of mindfulness-based stress reduction (MBSR) on psychological function among breast cancer (BC) survivors. Breast Cancer. 2016;23:568-576. [DOI] [PubMed] [Google Scholar]
- 19. Bartley T. Mindfulness-Based Cognitive Therapy for Cancer. Malden, MA: John Wiley & Sons; 2011. [Google Scholar]
- 20. Cebolla A, Campos D, Galiana L, et al. Exploring relations among mindfulness facets and various meditation practices: do they work in different ways? Conscious Cogn. 2017;49:172-180. [DOI] [PubMed] [Google Scholar]
- 21. Negi LT. Emory Compassion Meditation Protocol: Cognitively-Based Compassion Training Manual. Atlanta, GA: Emory University; 2013. [Google Scholar]
- 22. Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013;69:28-44. [DOI] [PubMed] [Google Scholar]
- 23. Neff K, Germer C. Being kind to yourself: the science of self-compassion. In: Singer T, Bolz M. eds. Compassion: Bridging Theory and Practice. Munich, Germany: Max Plank Society; 2013:291-312. [Google Scholar]
- 24. Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev. 2011;31:1126-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pace T, Negi LT, Adame DD, et al. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009;34:87-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kok BE, Coffey KA, Cohn MA, et al. How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci. 2013;24:1123-1132. [DOI] [PubMed] [Google Scholar]
- 27. Carson JW, Keefe FJ, Lynch TR, et al. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs. 2005;23:287-304. [DOI] [PubMed] [Google Scholar]
- 28. Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol. 2008;95:1045-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kirby JN, Tellegen CL, Steindl SR. A meta-analysis of compassion-based interventions: current state of knowledge and future directions. Behav Ther. 2017;48:778-792. [DOI] [PubMed] [Google Scholar]
- 30. García-Campayo J, Cebolla A, Demarzo M. La ciencia de la compasión: más allá de Mindfulness. Madrid, Spain: Alianza; 2016. [Google Scholar]
- 31. Brito G. Secular compassion training: an empirical review. J Transpers Res. 2014;6:61-71. [Google Scholar]
- 32. García-Campayo J, Navarro-Gil M, Demarzo M. Attachment-based compassion therapy. Mindfulness Compassion. 2016;1:68-74. [Google Scholar]
- 33. Jazaieri H, McGonigal K, Jinpa T, Doty JR, Gross JJ, Goldin PR. A randomized controlled trial of compassion cultivation training: effects on mindfulness, affect, and emotion regulation. Motiv Emot. 2014;38:23-35. [Google Scholar]
- 34. Gilbert P. Introducing compassion-focused therapy. Adv Psychiatr Treat. 2009;15:199-208. [Google Scholar]
- 35. Jennings PA, Foltz C, Snowberg KE, Sim H, Kemeny ME. The influence of mindfulness and emotion skills training on teachers’ classrooms: the effects of the cultivating emotional balance training. http://files.eric.ed.gov/fulltext/ED518584.pdf. Published April 18, 2011. Accessed February 9, 2017.
- 36. Sansó N, Galiana L, Cebolla A, Oliver A, Benito E, Ekman E. Cultivating emotional balance in professional caregivers: a pilot intervention. Mindfulness. 2017;8:1319-1327. [Google Scholar]
- 37. Desbordes G, Negi LT, Pace T, Wallace BA, Raison CL, Schwartz EL. Effects of mindful-attention and compassion meditation training on amygdala response to emotional stimuli in an ordinary, non-meditative state. Front Hum Neurosci. 2012;6:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kirby J. Cultivating compassion: a systematic review and meta-analysis of compassion-based interventions. PROSPERO 2015 CRD42015024576. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42015024576. Accessed October 9, 2016.
- 39. Kirby JN. Compassion interventions: the programmes, the evidence, and implications for research and practice. Psychol Psychother. 2017;90:432-455. [DOI] [PubMed] [Google Scholar]
- 40. Pace T, Negi L, Donaldson-Lavelle B, et al. Cognitively-Based Compassion Training reduces peripheral inflammation in adolescents in foster care with high rates of early life adversity. BMC Complement Altern Med. 2012;12(suppl 1):175.23039061 [Google Scholar]
- 41. Pace T, Negi L, Dodson-Lavelle B, et al. Engagement with Cognitively-Based Compassion Training is associated with reduced salivary C-reactive protein from before to after training in foster care program adolescents. Psychoneuroendocrinology. 2013;38:294-299. [DOI] [PubMed] [Google Scholar]
- 42. Pace T, Mletzko TC, Alagbe O, et al. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry. 2006;163:1630-1633. [DOI] [PubMed] [Google Scholar]
- 43. Pace TW, Negi LT, Sivilli TI, et al. Innate immune, neuroendocrine and behavioral responses to psychosocial stress do not predict subsequent compassion meditation practice time. Psychoneuroendocrinology. 2010;35:310-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mascaro JS, Pace TWW, Raison CL. Mind your hormones! The endocrinology of compassion. In: Singer T, Bolz M. eds. Compassion: Bridging Theory and Practice. Munich, Germany: Max Plank Society; 2013:230-250. [Google Scholar]
- 45. Faul F, Erdfelder E, Lang A, Buchner A. G* power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191. [DOI] [PubMed] [Google Scholar]
- 46. Lecrubier Y, Sheehan DV, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12:224-231. [Google Scholar]
- 47. Lobo A, Saz P, Marcos G, et al. Revalidación y normalización del mini-examen cognoscitivo (primera versión en castellano del mini-mental status examination) en la población general geriátrica. Med Clin (Barc). 1999;112:767-774. [PubMed] [Google Scholar]
- 48. Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15:974-986. [DOI] [PubMed] [Google Scholar]
- 49. Martinez RB, Boronat OG, Badia MS, Latiesas JS, Navarro EM, Fores MF. Functional assessment of cancer therapy questionnaire for breast cancer (FACT-B+4). Spanish version validation [in Spanish]. Med Clin (Barc). 2011;137:685-688. [DOI] [PubMed] [Google Scholar]
- 50. Derogatis LR. BSI 18, Brief Symptom Inventory 18: Administration, Scoring and Procedures Manual. Minneapolis, MN: NCS Pearson, Inc; 2001. [Google Scholar]
- 51. Andreu Y, Galdón MJ, Dura E, et al. Psychometric properties of the Brief Symptoms Inventory-18 (Bsi-18) in a Spanish sample of outpatients with psychiatric disorders. Psicothema. 2008;20:844-850. [PubMed] [Google Scholar]
- 52. Simard S, Savard J. Fear of Cancer Recurrence Inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2009;17:241-251. [DOI] [PubMed] [Google Scholar]
- 53. Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18:250-255. [DOI] [PubMed] [Google Scholar]
- 54. Garcia-Campayo J Navarro-Gil M Andrés E Montero-Marin J López-Artal L Demarzo MMP. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion Scale (SCS). Health Qual Life Outcomes. 2014;12:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pommier EA. The Compassion Scale, PhD [dissertation]. Austin, TX: University of Texas at Austin; 2010. [Google Scholar]
- 56. Tran US, Glück TM, Nader IW. Investigating the Five Facet Mindfulness Questionnaire (FFMQ): construction of a short form and evidence of a two-factor higher order structure of mindfulness. J Clin Psychol. 2013;69:951-965. [DOI] [PubMed] [Google Scholar]
- 57. Cebolla A, García-Palacios A, Soler J, Guillen V, Baños R, Botella C. Psychometric properties of the Spanish validation of the Five Facets of Mindfulness Questionnaire (FFMQ). Eur J Psychiatry. 2012;26:118-126. [Google Scholar]
- 58. Emory-Tibet Partnership. CBCT Evaluation Survey. Atlanta, GA: Emory University; 2014:1-20. [Google Scholar]
- 59. Chakraborty H, Gu H. A Mixed Model Approach for Intent-to-Treat Analysis in Longitudinal Clinical Trials With Missing Values. Research Triangle Park, NC: RTI Press; 2009:1-10. https://www.rti.org/rti-press-publication/mixed-model-approach-intent-treat-analysis-longitudinal-clinical-trials. Accessed April 3, 2018. [PubMed] [Google Scholar]
- 60. Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the archives of general psychiatry. Arch Gen Psychiatry. 2004;61:310-317. [DOI] [PubMed] [Google Scholar]
- 61. Salim A, Mackinnon A, Christensen H, Griffiths K. Comparison of data analysis strategies for intent-to-treat analysis in pre-test–post-test designs with substantial dropout rates. Psychiatry Res. 2008;160:335-345. [DOI] [PubMed] [Google Scholar]
- 62. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Mahwah, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 63. Cumming G, Calin-Jageman R. Introduction to the New Statistics: Estimation, Open Science, and Beyond. New York, NY: Routledge; 2016. [Google Scholar]
- 64. Cumming G. The new statistics: a how-to guide. Aust Psychol. 2013;48:161-170. [Google Scholar]
- 65. Ausina JB, Meca JS. Meta-análisis en ciencias sociales y de la salud. Madrid, Spain: Síntesis; 2015. [Google Scholar]
- 66. Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psychooncology. 2013;22:1457-1465. [DOI] [PubMed] [Google Scholar]
- 67. Mascaro JS, Kelley S, Darcher A, et al. Meditation buffers medical student compassion from the deleterious effects of depression. J Posit Psychol. 2016;13:133-142. [Google Scholar]
- 68. van den Beuken-van Everdingen MH, Peters ML, de Rijke JM, Schouten HC, van Kleef M, Patijn J. Concerns of former breast cancer patients about disease recurrence: a validation and prevalence study. Psychooncology. 2008;17:1137-1145. [DOI] [PubMed] [Google Scholar]
- 69. Mast ME. Survivors of breast cancer: illness uncertainty, positive reappraisal, and emotional distress. Oncol Nurs Forum. 1998;25:555-562. [PubMed] [Google Scholar]
- 70. Ferrell BR, Grant MM, Funk BM, Otis-Green SA, Garcia NJ. Quality of life in breast cancer survivors: implications for developing support services. Oncol Nurs Forum. 1998;25:887-895. [PubMed] [Google Scholar]
- 71. Cohee AA, Adams RN, Johns SA, et al. Long-term fear of recurrence in young breast cancer survivors and partners. Psychooncology. 2017;26:22-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lengacher CA, Shelton MM, Reich RR, et al. Mindfulness based stress reduction (MBSR (BC)) in breast cancer: evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). J Behav Med. 2014;37:185-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Neely ME, Schallert DL, Mohammed SS, Roberts RM, Chen Y. Self-kindness when facing stress: the role of self-compassion, goal regulation, and support in college students’ well-being. Motiv Emot. 2009;33:88-97. [Google Scholar]
- 74. Van Dam NT, Sheppard SC, Forsyth JP, Earleywine M. Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J Anxiety Disord. 2011;25:123-130. [DOI] [PubMed] [Google Scholar]
- 75. Campos D, Cebolla A, Quero S, et al. Meditation and happiness: mindfulness and self-compassion may mediate the meditation–happiness relationship. Pers Individ Dif. 2016;93:80-85. [Google Scholar]
- 76. Neff KD, Vonk R. Self-compassion versus global self-esteem: two different ways of relating to oneself. J Pers. 2009;77:23-50. [DOI] [PubMed] [Google Scholar]
- 77. Neff KD. Self-compassion, self-esteem, and well-being. Soc Personal Psychol Compass. 2011;5:1-12. [Google Scholar]
- 78. Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self Identity. 2010;9:225-240. [Google Scholar]
- 79. Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2:223-250. [Google Scholar]
- 80. Penberthy JK, Williams S, Hook JN, et al. Impact of a Tibetan Buddhist meditation course and application of related modern contemplative practices on college students’ psychological well-being: a pilot study. Mindfulness. 2017;8:911-919. [Google Scholar]
- 81. Brito G, Campos D, Cebolla A. Implicit or explicit compassion? Efficacy of a compassion-based intervention and comparison with mindfulness-based stress reduction intervention on empathy and compassion. Mindfulness. In press. [Google Scholar]
- 82. Reddy SD, Negi LT, Dodson-Lavelle B, et al. Cognitive-Based Compassion Training: a promising prevention strategy for at-risk adolescents. J Child Fam Stud. 2013;22:219-230. [Google Scholar]
- 83. Mascaro J, Rilling JK, Negi LT, Raison CL. Compassion meditation enhances empathic accuracy and related neural activity. Soc Cogn Affect Neurosci. 2013;8:48-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re) invention of mindfulness: comment on Brown et al (2011). Psychol Assess. 2011;23:1034-1046. [DOI] [PubMed] [Google Scholar]
- 85. Ozawa-de Silva BR, Dodson-Lavelle B, Raison CL, Negi LT. Compassion and ethics: scientific and practical approaches to the cultivation of compassion as a foundation for ethical subjectivity and well-being. J Healthcare Sci Hum. 2012;2:145-161. [Google Scholar]
- 86. Grossman P. Kindness and compassion as integral to mindfulness—experiencing the knowable in a special way. In: Singer T, Bolz M. eds. Compassion: Bridging Theory and Practice. Munich, Germany: Max Plank Society; 2013:192-207. [Google Scholar]
- 87. Grossman P, Van Dam NT. Mindfulness, by any other name . . . : trials and tribulations of sati in Western psychology and science. Contemp Buddhism. 2011;12:219-239. [Google Scholar]
- 88. Dahl CJ, Lutz A, Davidson RJ. Cognitive processes are central in compassion meditation. Trends Cogn Sci. 2016;20:161-162. [DOI] [PubMed] [Google Scholar]
- 89. Dahl CJ, Lutz A, Davidson RJ. Reconstructing and deconstructing the self: cognitive mechanisms in meditation practice. Trends Cogn Sci. 2015;19:515-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Dambrun M, Ricard M. Self-centeredness and selflessness: a theory of self-based psychological functioning and its consequences for happiness. Rev Gen Psychol. 2011;15:138-157. [Google Scholar]
- 91. Dambrun M, Ricard M, Després G, et al. Measuring happiness: from fluctuating happiness to authentic-durable happiness. Front Psychol. 2012;3:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wayment HA, Bauer JJ, Sylaska K. The Quiet Ego Scale: measuring the compassionate self-identity. J Happiness Stud. 2015;16:999-1033. [Google Scholar]