Abstract
Bodybuilding has increasingly become popular between males since male body shape has become a subject of interest in the last decades. Bodybuilders have desired to gain more muscle and paid attention to their body shape. Based on this purpose, they have string rules that include restrictive eating and excessive exercise program. Recent research has demonstrated that desiring more muscular body shape exhibits eating behavior problems and body dissatisfaction issues in bodybuilders. Limited research exists on the relationship between body dissatisfaction and eating disorders in male bodybuilders. The aim of this study was to determine the relationship between body image disturbance and eating disorders in 120 male bodybuilders. The Eating Attitude Test (EAT-40) was used to determine eating disorders, the Muscle Dysmorphia Disorder Inventory was used to determine bigorexia symptoms, and Bodybuilder Image Grid-Original (BIG O) and Scaled (BIG S) forms were used to detect the factors associated with body dissatisfaction. There was a positive relationship between Eating Attitude Test and Muscle Dysmorphia Disorder Inventory total scores. Eating Attitude Test was positively correlated with both fat and muscle dissatisfaction. Our results indicated that eating disorder psychopathology is positively related to body dissatisfaction and body dysmorphic disorders in male bodybuilders.
Keywords: eating disorders, bodybuilders, body dissatisfaction
Male physique has risen in public interest in recent decades (Maier, Haeussinger, Hautzinger, Fallgatter, & Ehlis, 2017). Most men affected by this situation have started to practice excessive bodybuilding and many have experienced negative body image-related thoughts (Robert, Munroe-Chanler, & Gammage, 2009). Recent studies have focused on men due to the increasing prevalence of male body image disturbance, body dissatisfaction, and their effects on quality of life (Griffiths et al., 2016; Mitchison & Mond, 2015; Tod, Edwards, & Cranswick, 2016).
Muscle dysmorphia (MD) is defined as a type of body dysmorphic disorder (BDD) that is characterized by a preoccupation with a perceived defect in one’s physique that can lead to multiple problems (Fang & Wilhelm, 2015; Foster, Shorter, & Griffiths, 2015; Glashouwer, Bennik, de Jong, & Spruyt, 2018; Longobardi, Prino, Fabris, & Settanni, 2017; Mitchell et al., 2017), including the abuse of drugs (particularly anabolic androgenic steroids) (Davis & Scott-Robertson, 2000), prioritizing workout programs over time with family and friends (Emini & Bond, 2014), hiding their body, deterioration in their career (Celso Alves dos Santos, Patrícia Passarelli, Sergio Carlos, Stephen, & Angélica Medeiros, 2015), depression, and even suicide (Angelakis, Gooding, & Panagioti, 2016). Although MD is classified as a BDD, the classification of MD is disputed (Krebs, de la Cruz, & Mataix-Cols, 2017); some researchers have demonstrated that it could be classified as a type of eating disorder (Murray, Rieger, Touyz, & De la Garza Garcia Lic, 2010; Nieuwoudt, Zhou, Coutts, & Booker, 2012). It has been reported that eating disorders can occur in men as a consequence of body dissatisfaction (Nieuwoudt, Zhou, Coutts, & Booker, 2012; Olivardia, Pope, Borowiecki III, & Cohane, 2004). Studies reported that men with muscle dysmorphia have more disordered eating patterns than men without muscle dysmorphia (Murray, Griffiths, Mitchison, & Mond, 2017; Murray, Griffiths, & Mond, 2016). Although body image-related disorders have been recognized as a life-threatening problem, diagnosis is still controversy (Mitchison & Mond, 2015).
It is well known that eating disorders are more common in weight-sensitive sports such as gymnastics, figure skating, and synchronized swimming (De Bruin, Quedejans, & Bakker, 2007; Pietrowsky & Straub, 2008; Sundgot-Borgen et al., 2013). As body weight has quite effective on performance, the athletes have a huge fear of gaining weight, and generally this fear is the origin of body image and weight-related disorders (Quatromoni, 2017; Sundgot-Borgen et al., 2013). High performance sports such as team sports (football, basketball, or volleyball) (Galli, Petrie, & Chatterton, 2017; Prather et al., 2016), and elite athletes (Olympic athletes) have performed under pressure (e.g., own coach, teammates, or race partners) (Hagmar, Berglund, Brismar, & Hirshberg, 2013; Plateau, McDermott, Arcelus, & Meyer, 2014). It was reported that coaches have especially a strong impact on athletes’ eating behaviors (Byrne & McLean, 2002). Although performance is the key factor of most of sports, this may not always be so (Chapman & Woodman, 2016). Such as competitive bodybuilding is arguably quite different from other sports that their activity in not only about performance in a task, but rather literally about appearance (Lambert, Frank, & Evans, 2004). Therefore the main reason that caused eating and body image-related disorders is to have a preoccupation about appearance, not performance (Nieuwoudt, Zhou, Coutts, & Booker, 2015). Competitive or noncompetitive bodybuilders are particularly vulnerable to eating disorders and body image dissatisfaction as a consequence of the obsession that being more muscular and leaner (Cafri, Olivardia, & Thompson, 2008). Although, both competitive and noncompetitive bodybuilders carry out similar restrictive eating and exercise schedule, the main purpose is different from each other (Blouin & Goldfield, 1995). While competitive bodybuilders focus on body modification to be leaner and more muscular to became successful in competitions, noncompetitive bodybuilders desire to gain muscle for own appearance and self-satisfaction (Pickett, Lewis, & Cash, 2005). Mosley (2009) reported that MD symptoms are mainly seen in male bodybuilders. A recent systematic review on MD diagnostic criteria demonstrated that 47.05% of reviewed articles analyzed weightlifters and bodybuilders (Celso Alves dos Santos et al., 2015). Although body dissatisfaction and eating disorder-related problems in males cause life-threatening conditions (Dakanalis et al., 2015), studies have reported that the actual prevalence of body dysmorphic disorder, eating disorders, and muscle dysmorphia are underreported (Devrim, Bilgic, Aslantas, & Hongu, 2017; Stanford & Lemberg, 2012).
Eating and body image-related disorders are generally under-recognized due to the lack of doing structured diagnostic interviews with individuals, particularly men, with BDD (Veale, Akyuz, & Hodsoll, 2015). Given that body image dissatisfaction could cause unhealthy eating patterns and eating disorders, the aim of this study is to determine the relationship between eating and body image-related disorders. It is hypothesized that using the screening tools to point the occurrence of eating disorder, muscle dysmorphia and body image perception to health professionals could be effective in early detection the high symptomatology of eating disorders and muscle dysmorphic disorders in male bodybuilders.
Materials and Methods
Participants
Participants consisted of 120 (to detect a moderate effect size at the p < .05 level) bodybuilders (competitive, n = 62 (mean age 31.05 ± 10.60 years; mean FFMI scores 24.09 ± 3.05 kg/m2, and mean 362.0 ± 128.46 min a week) and noncompetitive, n = 58 (mean age 25.63 ± 6.67 years; mean FFMI scores 21.18 ± 1.93 kg/m2, and had been practicing bodybuilding from 342.6 ± 130.20 min a week) recruited from four bodybuilding gym centers in Ankara, Turkey. The effect size used in this study was approved from a previous study done by Mayo and George (2014). The informed consent form was signed by all participants before taking part in the study. The inclusion criteria for competitive bodybuilders were to have prepared for or competed in a bodybuilding competition in the previous year and to do strength training at least three times a week (at least 150 min), and for noncompetitive bodybuilders were to have done strength training at least three times a week (at least 150 min) and never participated in a bodybuilding competition. This project was approved by Hacettepe University Ethics Board and Commission (Declaration of Helsinki) (Research ethic project no: GO 16/162.
Personal Information Questionnaire, Eating Attitude Test (EAT-40), Muscle Dysmorphia Disorder Inventory (MDDI), and Bodybuilder Image Grid (BIG) (Both Original (BIG O) and Scaled (BIG S) Forms)
Personal information questionnaire, EAT-40, MDDI, and BIG (both BIG O and BIG S forms) were applied to all participants in this study. Personal information questionnaire was included anthropometric measures, a personal information questionnaire, a bodybuilding-related questionnaire.
EAT-40 is a 40-item scale used to detect eating disorder symptoms in both sexes and all age groups (Garner & Garfinkel, 1979) (see Appendix A). Although EAT-26 is a new form of the screening tool for eating disorders, it was preferred to use EAT-40 to analyze eating disorders symptomatology more in detail. The main score is calculated with a rating on a 5-point Likert-type scale. The cut-off point is 30, and >30 indicates having high pathology of an eating disorder.
MDDI is a 13-item, five item scale that is used to measure muscle dysmorphia symptoms (Hildebrandt, Langenbucher, & Schlundt, 2004) (see Appendix B). The questionnaire has three subscales: drive for size (DFS) (items 1, 3, 5, 6, 8), appearance intolerance (AI) (items 2, 4, 7, 9), and functional impairment (FI) (items 10, 11, 12, 13). The cut-off point is 39 (min 0 point, max 65 points), with higher scores reflecting high muscle dysmorphia symptoms.
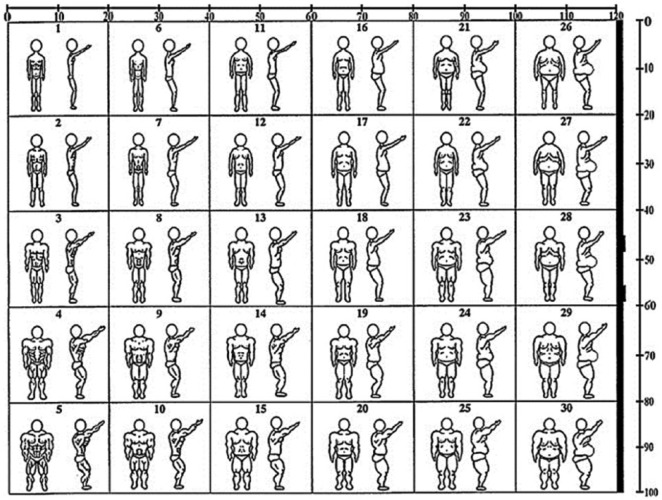
BIG is 30 silhouettes of male figures that are used to measure body image perceptions of male athletes, especially for bodybuilders (Hildebrandt et al., 2004) (see Appendix C). It has two self-perceived forms; BIG-Original (BIG O); and BIG Scaled (BIG S). In BIG O, their current body shape and ideal body shape figures are selected and scored based on two numerical scales along the top and right-hand side of the grid (between 0–120 for body fat score and 0–110 for body muscle mass score). In BIG S, participants select four self-perceived figures, which (a) represent their current body shape, (b) represent their ideal body shape, (c) represent the most attractive body shape, and (d) represent the most attractive body shape to the opposite sex. In the figure, body fat percentages increase from left to right and change between 3.5% and 36.0%. Fat Free Mass Index (FFMI) is used to calculate muscle mass in selected figures, increasing from left to right and changing between 15.5% and 29.0%.
Statistical Analysis
SPSS software v. 22.0 (IBM SPSS, Armonk, New York, USA) was used to perform statistical analyses. A p-value of less than .05 was considered to be statistically significant. First, the presence of eating disorders in both competitive and noncompetitive bodybuilders was determined. Then, differences between bodybuilders with eating disorders and non-eating disorders were assessed by t-tests. Correlations were determined by using analysis of Pearson and Spearman correlations. A multiple linear regression model was used to identify independent factors of EAT-40 scores.
Results
The descriptive features of bodybuilders are presented in Table 1. The FFMI of the bodybuilders was above normal value (>22.0 kg/m2).
Table 1.
Descriptive Features of Male Bodybuilders (N = 120).
| Male bodybuilders | |
|---|---|
| Mean (SD) | |
| Age (years) | 28.25 (9.17) |
| Body weight (kg) | 83.72 (12.97) |
| Height (cm) | 178.91 (6.36) |
| Body fat percentage (%) | 13.57 (4.00) |
| Fat Free Mass Index (kg/m2) | 22.58 (2.91) |
Note. SD = standard deviation.
To determine the effect of eating disorders on muscle dysmorphia and body dissatisfaction, all participants were first assessed according to EAT-40 scores. Participants who were above the cut-off point of EAT-40 were defined as having an eating disorder. The following analyses were performed to examine the differences in scores between the bodybuilders with and without eating disorders (Table 2).
Table 2.
MDDI and EAT-40 Scores of Comparison of Bodybuilders With and without Eating Disorders.
| Bodybuilders with ED | Bodybuilders without ED | p | |
|---|---|---|---|
|
n = 81 Mean (SD) |
n = 39 Mean (SD) |
||
| EAT-40 score | 36.71 (6.48) | 17.53 (5.81) | <.001 |
| Total MDDI score | 39.53 (4.97) | 28.87 (6.01) | <.001 |
| Drive for size (DFS) | 16.51 (3.86) | 12.61 (4.21) | <.001 |
| Appearance intolerance (AI) | 8.33 (3.20) | 6.05 (2.58) | <.001 |
| Functional impairment (FI) | 14.77 (3.12) | 10.20 (3.54) | <.001 |
| Body checking |
Median (IQR)
9.2 (3.2–11.7) |
Median (IQR)
4.7 (2.4–5.2) |
<.001 |
Note. MDDI = Muscle Dysmorphia Disorder Inventory; EAT-40 = Eating Attitude Test; ED = eating disorder; SD = standard deviation; DFS = drive for size; AI = appearance intolerance; FI = functional impairment; IQR= interquartile range.
EAT-40
Of the 120 bodybuilders, 81 (67.5%) had EAT-40 scores above its cut-off point, indicating that potentially clinical levels of eating pathology. Thirty-nine percent of bodybuilders with eating disorders and 35% of bodybuilders without eating disorders reported that they planned their diet schedules and cooked for themselves, and there was no significant difference between competitive and noncompetitive bodybuilders (Mean EAT-40 scores of competitive and noncompetitive bodybuilders; respectively, p > .05).
BIG
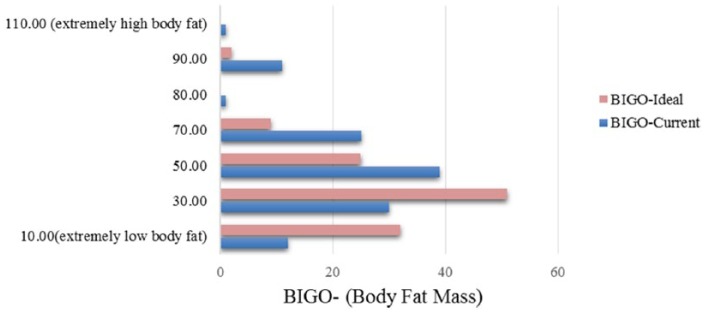
The results of BIG O provide bodybuilders’ current and ideal (desired) fat mass (Figure 1). For current and ideal body fat mass, the average BIG O body fat mass scores were 47.06 ± 22.32 and 28.96 ± 19.61, respectively. There was a statistically significant difference between current and ideal body fat mass scores (p < .01).
Figure 1.
Frequency graphs of bodybuilders’ figure selections of their current and ideal fat mass. BIG O = Bodybuilder Image Grid-Original.
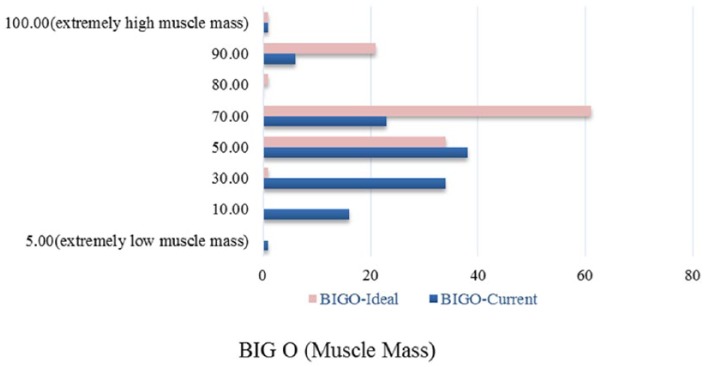
Figure 2 provides frequency graphs of BIG O muscle mass scores of bodybuilders. The average BIG O ideal muscle mass scores (72.24 ± 14.63) were observed to be significantly higher than BIG O current muscle mass scores (54.31 ± 20.09). The data indicated that bodybuilders want to be leaner (less fat) and more muscular. There was no difference in BIG O results between competitive and noncompetitive bodybuilders (data not reported).
Figure 2.
Frequency graphs of bodybuilders’ figure selections of their current and ideal muscle mass.
BIG O = Bodybuilder Image Grid-Original.
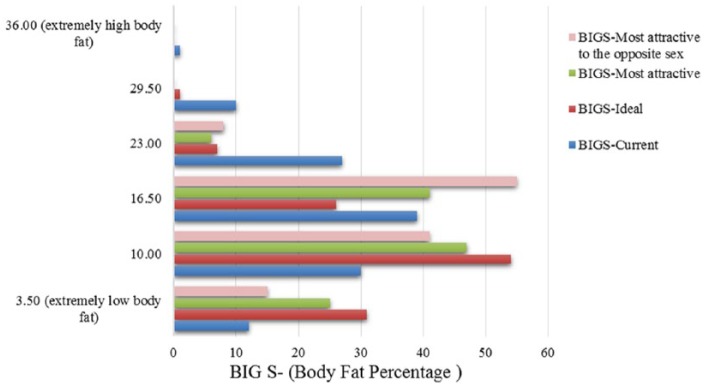
Figure 3 presents information about bodybuilders’ figure selections of their body fat percentage on BIG S. For their current body fat percentage, participants most commonly chose column 3, which indicated approximately 16.5% body fat. For their desired % body fat, they most commonly chose column 2, indicating approximately 10% body fat. They most frequently selected figures in column 2 (10% body fat) for the figures that they thought indicated the most attractive body fat mass. Participants most frequently selected column 3, indicative of 16.5% body fat, for the figures that they thought were most attractive according to the opposite sex. These differences indicated that bodybuilders chose leaner figures than what they thought the opposite sex found attractive.
Figure 3.
Frequency graphs of bodybuilders’ figure selections of BIG S. BIG S = Bodybuilder Image Grid-Scaled.
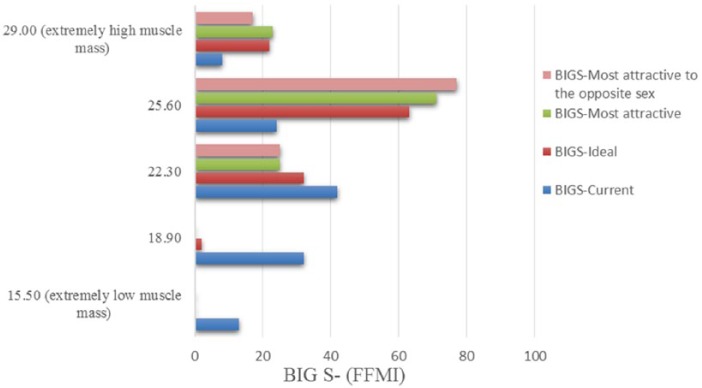
Bodybuilders’ selections on muscle attractiveness are presented in Figure 4. Bodybuilders most commonly (35.4%) selected row 3 to define what they thought about their current muscle mass (indicative of 22.3% FFMI), and 52.5% of bodybuilders selected row 4 to define what they thought about their ideal muscle mass (indicative of 23.6% FFMI). Bodybuilders commonly chose the same figures (row 4) (indicative 25.6% FFMI) when asked which figure they thought to be most attractive according to them (59.2%) and to the opposite sex (64.7%).
Figure 4.
Frequency graphs of bodybuilders’ figure selections of BIG S. BIG S = Bodybuilder Image Grid-Scaled; FFMI = Fat Free Mass Index.
MDDI
Of the 120 bodybuilders, 70 (58.3%) have higher MDDI scores (>39), indicating that they have high muscle dysmorphia symptoms. The average MDDI score was 36.06 ± 7.30.
BIG, EAT, and MDDI
The mean and standard deviation of MDDI and EAT-40 scores of eating disorders compared with non-eating disorders are given in Table 2. Total and all subscales of MDDI scores and body image/dissatisfaction scores according to BIG O and BIG S scales were significantly higher in bodybuilders with eating disorders (p < .05). EAT-40 was positively related with both percent body fat (rs = 0.453, p < .01) and percent muscle dissatisfaction according to results of MDDI (rs = 0.488, p < .01).
Correlation Analysis
There was a significant positive relationship between EAT-40 and MDDI total scores (r = 0.614, p < .001). FFMI scores were positively correlated with drive for size. The data showed that the more muscles participants had gained, the more they work for muscularity (Table 3). The average number of hours dedicated to improving muscularity was 6.03 ± 2.14 hr for competitive/professional and 5.71 ± 2.17 hr for noncompetitive bodybuilders.
Table 3.
Pearson Correlation Coefficients Between FFMI, EAT-40, MDDI Total Scores, and MDDI Subscales.
| A | B | C | D | E | F | G | |
|---|---|---|---|---|---|---|---|
| (A) EAT-40 | – | ||||||
| (B) FFMI | 0.109 | – | |||||
| (C) MDDI total score | 0.614** | −0.080 | – | ||||
| (D) DFS | 0.298** | −0.259** | 0.687** | – | |||
| (E) AI | 0.370** | −0.018 | 0.481** | −0.045 | – | ||
| (F) FI | 0.547** | 0.166 | 0.720** | 0.190* | 0.207* | – | |
| (G) Body fat percentage (%) | 0.054 | 0.049 | −0.013 | −0.147 | 0.340** | −0.146 | – |
Note. FFMI = Fat Free Mass Index; MDDI = Muscle Dysmorphia Disorder Inventory; EAT-40 = Eating Attitude Test; DFS = drive for size; AI = appearance intolerance; FI = functional impairment.
Regression Analysis
Table 4 provides the results of the regression analysis. A linear regression analysis predicting the eating disorder was mirrored with MDDI subscales and FFMI scores (R2 = .428).
Table 4.
Linear Regression Analyses of EAT-40 and MDDI Subscales and FFMI.
| Variable | B | SE | β | t | p |
|---|---|---|---|---|---|
| EAT-40 | −12.540 | 7.786 | −1.611 | .001 | |
| MDDI (DFS) | 0.419 | 0.190 | 0.262 | 3.454 | .001 |
| MDDI (AI) | 1.023 | 0.249 | 0.298 | 4.102 | .001 |
| MDDI (FI) | 1.173 | 0.214 | 0.416 | 5.489 | .001 |
| FFMI | 0.427 | 0.283 | 0.113 | 1.509 | .134 |
Note. EAT-40 = Eating Attitude Test; MDDI = Muscle Dysmorphia Disorder Inventory; DFS = drive for size; AI = appearance intolerance; FI = functional impairment.
This regression analysis indicates that EAT-40, FFMI, and subscales of MDDI (DFS, AI, and FI) reach statistical significance and that an eating disorder was a relative risk factor for muscle dysmorphia symptoms and muscle-related body dissatisfaction.
Discussion
This study aimed to investigate the relationship between eating disorders and body dissatisfaction in male bodybuilders. It was hypothesized that bodybuilders with eating disorders might have greater body dissatisfaction than bodybuilders without eating disorders. Individuals with EAT-40 scores >30 are considered to have high symptoms of eating disorders (Garner & Garfinkel, 1979), and those with MDDI scores >39 are considered to have high muscle dysmorphia symptoms and body dissatisfaction problems (Hildebrandt et al., 2004). In this study, 67.5% of bodybuilders scored >30 for EAT-40, and 58.3% of bodybuilders scored >39 for MDDI. This result indicates that bodybuilders have high symptomatology of both eating and muscle dysmorphic disorders.
Murray et al. (2017) determined a correlation between muscle dysmorphia symptoms and eating disorders in 21 muscle dysmorphia patients, 24 anorexia nervosa patients, and 15 recreationally gym-using controls. The anorexia and muscle dysmorphia patients were diagnosed by a clinical psychiatrist or psychologist, then to investigate the relationship between ED and MD, the screening tools of MD and ED were applied to both patients and recreationally gym-using controls. It was reported that both anorexia patients and muscle dysmorphia patients had symptomatic similarities and similar scores than gym-using controls. In this study, it was reported that there was a significantly positive relationship between MDDI and EAT-40 in both professional and recreational bodybuilders. These findings support that there was a significant positive correlation between body dissatisfaction and eating disorders in bodybuilders.
Solomon-Kraus et al. (2017) reported that determining the self-perceived approximation of their current and ideal body images has been used to realize the perception of body dissatisfaction in bodybuilders. BIG O and BIG S scales complemented these findings by revealing bodybuilders’ body image perceptions. Mayo and George (2014) reported that for both body muscle mass and body fat, males chose the figures which they thought someone found themselves attractive. In this study, bodybuilders selected the same figures as being the most attractive body muscle mass according to them and to the opposite sex; however, for their desired body fat percentage, they desired to have a leaner body shape even if they thought the opposite sex found that less attractive. It is emphasized that the bodybuilders in this study give more attention on their own thoughts even partners don’t desire it.
Cafri et al. (2005) indicated that the desired muscular body ideal for the purposes of self-satisfaction and/or sports performance has become a major issue in males. The increased concern about being more muscular had health-threatening problems has caused to increase the prevalence of disordered eating pathology and body dissatisfaction symptomatology, both the clinical and subclinical levels (Chapman & Woodman, 2016). Bodybuilder Image Grid regarded as a perceptional measure that represents the discrepancy between current and desired percent of body fat and body mass (Hildebrandt, Langenbucher, & Schlundt, 2004) (Figure 5). There are limited data discussing the association between body image perception and disordered eating behaviors in male bodybuilders. In this study, according to the correlation between the BIG and EAT-40, it was identified that higher scores for eating disorders indicated a desire for more muscle mass.
Figure 5.
Bodybuilder Image Grid. *BIG S: use scales and remove numbers above figures. *BIG O use numbers above figures and remove scales (Hildebrandt, Langenbucher, & Schlundt, 2004).
The frequency of body dissatisfaction in athletes with eating disorders is influenced by the type of sports they participate in. Anderson, Reilly, Gorrell, and Anderson (2016) conducted a study with adult runners, which is one of weight-sensitive sports. They reported that disordered eating symptoms of female runners were significantly related with image-related body dissatisfaction, and this relationship was not demonstrated in male runners. Athletes from aesthetic sports has more disordered eating symptoms then nonathletic populations due to environment pressure, as Krentz and Warchburger (2011) found in 96 elite athletes from aesthetic sports and 96 sex-matched non-athletes. In weight-dependence sports, such as wrestling, judo, rowing, the athletes purposed to obtain the lowest possible body weight to get advantage in sports performance. The purpose caused abnormal eating behaviors (Currie, 2010). On the other side, bodybuilding is directly an appearance-based sport that focuses on building muscles. Research on bodybuilding identified that appearance intolerance could be the main reason that caused eating and muscle dysmorphic disorders. Pickett et al. (2005) demonstrated that bodybuilders had higher self-reported disordered eating symptoms than control groups. Hallsworth, Wade, and Tiggemann (2005) examined the levels of self-objectification in bodybuilders, weightlifters and nonathletic controls. It was reported that bodybuilders had significantly higher levels of self-objectification than weightlifters and nonathletic controls, and the self-objectification mainly based on appearance anxiety. A research on eating disorders, and muscle dysmorphic disorders performed by Santarnecchi and Dettore (2012) identified that competitive bodybuilders had higher muscle dysmorphia symptoms than noncompetitive and nonathletic controls, and the correlation between MDDI scores were statistically positively correlated with BIG S scores. The results from this study indicated that 53.7% of bodybuilders had body dissatisfaction, and this result correlated significantly with eating disorder scores (according to EAT-40) (r = .614, p < .01).
Treatment of eating psychopathology requires a multidisciplinary approach in collaboration with dietitians, psychiatrist, and psychologist. Turton, Goodwin, and Meyer (2017) mentioned to be aware of the symptoms of the disorder by closely monitoring compulsive exercise and eating behaviors for early diagnosis and reversing its effects on body and sport performance. In this study, it was identified that the combined use of three screening tools could provide useful information to health-care professionals for early detection of eating and body image-related problems in male bodybuilders.
Conclusion
Males with eating disorders desire to have a more muscular shape, particularly in body weight-related sports, such as bodybuilding, wrestling, and weightlifting. This study used three assessment tools to identify eating disorders, addressing emotional and behavioral aspects of the body condition, and body satisfaction in bodybuilders. Each tool has advantages and limitations, but this study confirmed that two assessment tools, EAT-40 and MDDI, could be used to predict early symptoms. Because eating disorders, especially in men, may not be diagnosed at an early stage, the screening tools could provide early detection of eating disorders and muscle dysmorphia symptoms for athletes and health professionals. All of these screening tools are available in Appendices of this article as tests for men who may have eating disorders and muscle dysmorphia symptoms.
Given the correlative nature of the study design, one limitation of this study is its inability to speculate causality. Although this study demonstrated significant correlation of eating disorders and body dissatisfaction, the study was not able to determine whether such a trend can be generalized to athletes of all sexes.
The findings of this study endorse the need for research and informed prevention strategies, risk assessments, and intervention approaches for nutrition, psychiatry, psychology, and sports professionals and athletic departments.
Appendices
A. Personal Information Questionnaire
Name:
Age (year):
Height (cm):
Weight (kg):
Body fat percentage (%):
FFMI (kg/m2):
- How many times a week do you work out strength training?
- (a) 1–2 times [ ] (b) 2–4 times [ ] (c) 4–6 times [ ] (d) More than 6 times [ ]
- How long do you work out strength training?
- (a) <30 min [ ] (b) 30–45 min [ ] (c) 45–60 min [ ] (d) More than 60 min [ ]
- Do you participate in a bodybuilding competition?
- (a) No (b)Yes
- Have you ever participated in a bodybuilding competition before?
- (a) No (b) Yes (……times)
B. EAT-40
Instruction: Please place an (X) under the column, which applies best to each of the numbered statements. All of the results will be strictly confidential. Most of the questions directly relate to food or eating, although other types of questions have been included. Please answer each question carefully. Thank you.
| 1. Like eating with other people | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 2. Prepare foods for others but do not eat what I cook | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 3. Become anxious prior to eating | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 4. Am terrified about being overweight | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 5. Avoid eating when I am hungry | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 6. Find myself preoccupied with food | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 7. Have gone on eating binges where I feel that I may not be able to stop | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 8. Cut my food into small pieces | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 9. Aware of the calorie content of the foods that I eat | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 10. Particularly avoid foods with a high carbohydrate content (e.g., bread, potatoes, rice) |
( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 11. Feel bloated after meals | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 12. Feel that others would prefer if I ate more | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 13. Vomit after I have eaten | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 14. Feel extremely guilty after eating | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 15. Am preoccupied with a desire to be thinner | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 16. Exercise strenuously to burn off calories | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 17. Weight myself several times a day | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 18. Like my clothes to fit tightly | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 19. Enjoy eating meat | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 20. Wake up early in the morning | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 21. Eat the same foods day after day | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 22. Think about burning up calories when I exercise | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 23. Have regular menstrual periods | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 24. Other people think that I am too thin | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 25. Am preoccupied with the thought of having fat on my body | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 26. Take longer than others to eat my meals | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 27. Enjoy eating at restaurants | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 28. Take laxatives | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 29. Avoid foods with sugar in them | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 30. Eat diet foods | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 31. Feel that food controls my life | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 32. Display self-control around food | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 33. Feel that others pressure me to eat | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 34. Give too much time and thought to food | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 35. Suffer from constipation | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 36. Feel uncomfortable after eating sweets | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 37. Engage in dieting behavior | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 38. Like my stomach to be empty | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 39. Enjoy trying new rich foods | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
| 40. Have the impulse to vomit after meals | ( ) | ( ) | ( ) | ( ) | ( ) | ( ) |
C. MDDI
Instruction:
Please rate the following statements to best indicate how you typically think, feel, or behave on a scale from 1 to 5 (1: never, 5: always)
| 1. I think my body is too small | |
| 2. I wear loose clothing so that people can’t see my body | |
| 3. I hate my body | |
| 4. I wish I could get bigger | |
| 5. I think my chest is too small | |
| 6. I think my legs are too thin | |
| 7. I feel like I have too much body fat | |
| 8. I wish my arms were bigger | |
| 9. I am very shy about letting people see me with my shirt off | |
| 10. I feel anxious when I miss one or more workout days | |
| 11. I pass up social activities with friends because of my workout schedule | |
| 12. I feel depressed when I miss one or more workout days | |
| 13. I pass up chances to meet new people because of my workout schedule |
C.1 Bodybuilder Image Grid-Original
On the following page, you will find a grid of male figures. Look at them closely. Please recognize that these bodies may not be completely accurate representations of you personally or bodies you think to be attractive. You will see two numerical scales along the top and right-hand side of the grid: (a) the Body Fat scale on the top that ranges from extremely low body fat (0) to extremely high body fat (120), and (b) the Muscle Mass scale along the right-hand side that ranges from extremely low muscle mass (0) to extremely high muscle mass (100). For each of the following questions, you will be asked to choose where on these scales the male body asked about falls. You will indicate for each the desired body fat score (on the scale of 0–120 as marked on the grid), and desired muscle mass score (on a scale of 0–100 as marked on the grid) that correspond to the “ideal” figure as requested.
- What do you think is the best approximation of your CURRENT body (assume figure has your height)?Body Fat Scale Score: _________Muscle Mass Scale Score: ______
- What do you think is the best approximation of your IDEAL body?Body Fat Scale Score: ________Muscle Mass Scale Score: _____
C.2. Bodybuilder Image Grid-Scaled (BIG S)
The Bodybuilder Image Grid was designed to measure the perceptual body image disturbance in males and perceived attractiveness of the male body to both men and women. The figures used in the BIG vary along dimensions of muscularity and body fat. Directions for males instruct individuals to make four choices: (a) the figure they think best represents their current body type, (b) the figure they think best represents their ideal body type, (c) the body type that is most attractive, and (d) the body type that is most attractive to the opposite sex. The scale is intended to be used for males with any sexual preference; by asking for ratings of most attractive and most attractive to the opposite sex, individuals make ratings of attractiveness independent of their sexual preference. The BIG O grid has two scales analogous to the measurement of longitude (body fat columns) and latitude (muscle mass rows). The top left figure represents the column with the least body fat, and row with the least muscle mass. From left to right the columns increase in body fat from 1: extremely low body fat to 6: extremely high body fat.
From top to bottom the figures increase in muscle mass from 1: extremely low muscle mass to 5: extremely high muscle mass.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Aslı Devrim  https://orcid.org/0000-0002-4267-9950
https://orcid.org/0000-0002-4267-9950
Pelin Bilgic  https://orcid.org/0000-0002-8177-0300
https://orcid.org/0000-0002-8177-0300
Nobuko Hongu  https://orcid.org/0000-0001-8365-5253
https://orcid.org/0000-0001-8365-5253
References
- Anderson L. M., Reilly E. E., Gorrell S., Anderson D. A. (2016). Running to win or to be thin? An evaluation of body dissatisfaction and eating disorder symptoms among adult runners. Body Image, 17, 43–47. doi: 10.1016/j.bodyim.2016.02.003 [DOI] [PubMed] [Google Scholar]
- Angelakis I., Gooding P. A., Panagioti M. (2016). Suicidality in Body Dysmorphic Disorder (BDD): A systematic review with meta-analysis. Clinical Psychology Review, 49, 55–66. doi: 10.1016/j.cpr.2016.08.002 [DOI] [PubMed] [Google Scholar]
- Blouin A. G., Goldfield G. S. (1995). Body image and steroid use in male bodybuilders. International Journal of Eating Disorders, 18, 159–165. [DOI] [PubMed] [Google Scholar]
- Byrne S., McLean N. (2002). Elite athletes: Effects of the pressure to be thin. Journal of Science and Medicine in Sport, 5, 80–94. [DOI] [PubMed] [Google Scholar]
- Cafri G., Olivardia R., Thompson J. K. (2008). Symptom characteristics and psychiatric comorbidity among males with muscle dysmorphia. Comprehensive Psychiatry, 49(4), 374–379. doi: 10.1016/j.comppsych.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Cafri G., Thompson J. K., Ricciardelli L., McCabe M., Smolak L., Yesalis C. (2005). Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clinical Psychology Review, 25(2), 215–239. [DOI] [PubMed] [Google Scholar]
- Celso Alves dos Santos F., Patrícia Passarelli T., Sergio Carlos S., Stephen W. T., Angélica Medeiros C. (2015). Systematic review of the diagnostic category muscle dysmorphia. Australian & New Zealand Journal of Psychiatry, 50(4), 322–333. doi: 10.1177/0004867415614106 [DOI] [PubMed] [Google Scholar]
- Chapman J., Woodman T. (2016). Disordered eating in male athletes: A meta-analysis. Journal of Sports Sciences, 34(2), 101–109. [DOI] [PubMed] [Google Scholar]
- Currie A. (2010). Sport and eating disorders-understanding and managing the risks. Asian Journal of Sports Medicine, 1(2), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakanalis A., Zanetti A. M., Riva G., Colmegna F., Volpato C., Madeddu F., Clerici M. (2015). Male body dissatisfaction and eating disorder symptomatology: Moderating variables among men. Journal of Health Psychology, 20(1), 80–90. [DOI] [PubMed] [Google Scholar]
- Davis C., Scott-Robertson L. (2000). A psychological comparison of females with anorexia nervosa and competitive male bodybuilders: Body shape ideals in the extreme. Eating Behaviors, 1(1), 33–46. [DOI] [PubMed] [Google Scholar]
- De Bruin A. P., Oudejans R. R. D., Bakker F. C. (2007). Dieting and body image in aesthetic sports: A comparison of Dutch female gymnasts and non-aesthetic sport participations. Psychology of Sport and Exercise, 8, 507–520. [Google Scholar]
- Devrim A., Bilgic P., Aslantas B., Hongu N. (2017). Relationship between muscularity concerns and body checking behaviors in Turkish bodybuilders. The FASEB Journal, 31(Suppl 1), 436.27799346 [Google Scholar]
- Emini N. N., Bond M. J. (2014). Motivational and psychological correlates of bodybuilding dependence. Journal of Behavioral Addictions, 3(3), 182–188. doi: 10.1556/JBA.3.2014.3.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang A., Wilhelm S. (2015). Clinical features, cognitive biases, and treatment of body dysmorphic disorder. Annual Review of Clinical Psychology, 11, 187–212. [DOI] [PubMed] [Google Scholar]
- Foster A. C., Shorter G. W., Griffiths M. D. (2015). Muscle dysmorphia: Could it be classified as an addiction to body image? Journal of Behavioral Addictions, 4(1), 1–5. doi: 10.1556/jba.3.2014.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli N., Petrie T., Chatterton J. (2017). Team weigh-ins and self-weighing: Relations to body-related perceptions and disordered eating in collegiate male athletes. Psychology of Sport and Exercise, 29, 51–55. [Google Scholar]
- Garner D. M., Garfinkel P. E. (1979). The eating attitudes test: An index of the symptoms of anorexia nervosa. Psychology Medicine, 9(2), 273. doi: 10.1017/s0033291700030762 [DOI] [PubMed] [Google Scholar]
- Glashouwer K. A., Bennik E. C., de Jong P. J., Spruyt A. (2018). Implicit measures of actual versus ideal body image: Relations with self-reported body dissatisfaction and dieting behaviors. Cognitive Therapy and Research, 42, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths S., Hay P., Mitchison D., Mond J. M., McLean S. A., Rodgers B., Paxton S. J. (2016). Sex differences in the relationships between body dissatisfaction, quality of life and psychological distress. Australian & New Zealand Journal of Public Health, 40(6), 518–522. doi: 10.1111/1753-6405.12538 [DOI] [PubMed] [Google Scholar]
- Hagmar M., Berglund B., Brismar K., Hirshberg A. L. (2013). Body composition and endocrine profile of male Olympic athletes striving for leanness. Clinical Journal of Sport Medicine, 23, 197–201. [DOI] [PubMed] [Google Scholar]
- Hallsworth L., Wade T., Tiggemann M. (2005). Individual differences in male body-image: An examination of self-objectification in recreational body builders. British Journal of Health Psychology, 10(3), 453–465. [DOI] [PubMed] [Google Scholar]
- Hildebrandt T., Langenbucher J., Schlundt D. G. (2004). Muscularity concerns among men: Development of attitudinal and perceptual measures. Body Image, 1(2), 169–181. doi: 10.1016/j.bodyim.2004.01.001 [DOI] [PubMed] [Google Scholar]
- Krebs G., de la Cruz L. F., Mataix-Cols D. (2017). Recent advances in understanding and managing body dysmorphic disorder. Evidence-Based Mental Health, 20(3), 71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krentz E. M., Warschburger P. (2011). Sports-related correlates of disordered eating in aesthetic sports. Psychology of Sport and Exercise, 12(4), 375–382. [Google Scholar]
- Lambert C. P., Frank L. L., Evans W. J. (2004). Macronutrient considerations for the sport of bodybuilding. Sports Medicine, 34(5), 317–327. [DOI] [PubMed] [Google Scholar]
- Longobardi C., Prino L. E., Fabris M. A., Settanni M. (2017). Muscle dysmorphia and psychopathology: Findings from an Italian sample of male bodybuilders. Psychiatry Research, 256, 231–236. doi: 10.1016/j.psychres.2017.06.065 [DOI] [PubMed] [Google Scholar]
- Maier M. J., Haeussinger F. B., Hautzinger M., Fallgatter A. J., Ehlis A. C. (2017). Excessive bodybuilding as pathology? A first neurophysiological classification. World Journal of Biological Psychiatry, 18, 1–11. doi: 10.1080/15622975.2017.1395070 [DOI] [PubMed] [Google Scholar]
- Mayo C., George V. (2014). Eating disorder risk and body dissatisfaction based on muscularity and body fat in male university students. Journal of American College Health, 62(6), 407–415. doi: 10.1080/07448481.2014.917649 [DOI] [PubMed] [Google Scholar]
- Mitchell L., Murray S. B., Hoon M., Hackett D., Prvan T., O’Connor H. (2017). Correlates of muscle dysmorphia symptomatology in natural bodybuilders: Distinguishing factors in the pursuit of hyper-muscularity. Body Image, 22, 1–5. doi: 10.1016/j.bodyim.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Mitchison D., Mond J. (2015). Epidemiology of eating disorders, eating disordered behaviour, and body image disturbance in males: A narrative review. Journal of Eating Disorders, 3, 20. doi: 10.1186/s40337-015-0058-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosley P. E. (2009). Bigorexia: Bodybuilding and muscle dysmorphia. European Eating Disorder Review, 17(3), 191–198. doi: 10.1002/erv.897 [DOI] [PubMed] [Google Scholar]
- Murray S. B., Griffiths S., Mitchison D., Mond J. M. (2017). The transition from thinness-oriented to muscularity-oriented disordered eating in adolescent males: A clinical observation. Journal of Adolescent Health, 60(3), 353–355. doi: 10.1016/j.jadohealth.2016.10.014 [DOI] [PubMed] [Google Scholar]
- Murray S. B., Griffiths S., Mond J. M. (2016). Evolving eating disorder psychopathology: Conceptualising muscularity-oriented disordered eating. British Journal of Psychiatry, 208(5), 414–415. doi: 10.1192/bjp.bp.115.168427 [DOI] [PubMed] [Google Scholar]
- Murray S. B., Rieger E., Touyz S. W., De la Garza Garcia Lic Y. (2010). Muscle dysmorphia and the DSM-V conundrum: Where does it belong? A review paper. International Journal of Eating Disorders, 43(6), 483–491. doi: 10.1002/eat.20828 [DOI] [PubMed] [Google Scholar]
- Nieuwoudt J. E., Zhou S., Coutts R. A., Booker R. (2012). Muscle dysmorphia: Current research and potential classification as a disorder. Psychology of Sport and Exercise, 13(5), 569–577. doi: 10.1016/j.psychsport.2012.03.006 [DOI] [Google Scholar]
- Nieuwoudt J. E., Zhou S., Coutts R. A., Booker R. (2015). Symptoms of muscle dysmorphia, body dysmorphic disorder, and eating disorders in a nonclinical population of adult male weightlifters in Australia. The Journal of Strength & Conditioning Research, 29(5), 1406–1414. [DOI] [PubMed] [Google Scholar]
- Olivardia R., Pope H. G., Borowiecki J. J., III, Cohane G. H. (2004). Biceps and body image: The relationship between muscularity and self-esteem, depression, and eating disorder symptoms. Psychology of Men & Masculinity, 5(2), 112–120. doi: 10.1037/1524-9220.5.2.112 [DOI] [Google Scholar]
- Pickett T. C., Lewis R. J., Cash T. F. (2005). Men, muscles, and body image: Comparisons of competitive bodybuilders, weight trainers, and athletically active controls. British Journal of Sports Medicine, 39(4), 217–222. doi: 10.1136/bjsm.2004.012013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrowsky R., Straub K. (2008). Body dissatisfaction and restrained eating in male juvenile and adult athletes. Eating and Weight Disorders, 13, 14–21. [DOI] [PubMed] [Google Scholar]
- Plateau C. R., McDermott H. J., Arcelus J., Meyer C. (2014). Identifying and preventing disordered eating among athletes: Perceptions of track and field coaches. Psychology of Sport and Exercise, 15(6), 721–728. doi: 10.1016/j.psychsport.2013.11.004 [DOI] [Google Scholar]
- Prather H., Hunt D., McKeon K., Simpson S., Meyer E. B., Yemm T., Brophy R. (2016). Are elite female soccer athletes at risk for disordered eating attitudes, menstrual dysfunction, and stress fractures? American Journal of Physical Medicine and Rehabilitation, 8(3), 208–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quatromoni P. A. (2017). A tale of two runners: A case report of athletes’ experiences with eating disorders in college. Journal of the Academy of Nutrition and Dietetics, 117(1), 21–31. doi: 10.1016/j.jand.2016.09.032 [DOI] [PubMed] [Google Scholar]
- Robert C. A., Munroe-Chandler K. J., Gammage K. L. (2009). The relationship between the drive for muscularity and muscle dysmorphia in male and female weight trainers. The Journal of Strength & Conditioning Research, 23(6), 1656–1662. [DOI] [PubMed] [Google Scholar]
- Santarnecchi E., Dèttore D. (2012). Muscle dysmorphia in different degrees of bodybuilding activities: Validation of the Italian version of muscle dysmorphia disorder inventory and bodybuilder image grid. Body Image, 9(3), 396–403. [DOI] [PubMed] [Google Scholar]
- Solomon-Krakus S., Sabiston C. M., Brunet J., Castonguay A. L., Maximova K., Henderson M. (2017). Body image self-discrepancy and depressive symptoms among early adolescents. Journal of Adolescent Health, 60(1), 38–43. doi: 10.1016/j.jadohealth.2016.08.024 [DOI] [PubMed] [Google Scholar]
- Sotiriadou P., De Bosscher V. (2018). Managing high-performance sport: Introduction to past, present and future considerations. European Sport Management Quarterly, 18(1), 1–7. [Google Scholar]
- Stanford S. C., Lemberg R. (2012). A clinical comparison of men and women on the Eating Disorder Inventory-3 (EDI-3) and the Eating Disorder Assessment for Men (EDAM). Eating Disorders, 20(5), 379–394. [DOI] [PubMed] [Google Scholar]
- Sundgot-Borgen J., Meyer N. L., Lohman T. G., Ackland T. R., Maughan R. J., Stewart A. D., Müller W. (2013). How to minimise the health risks to athletes who compete in weight-sensitive sports review and position statement on behalf of the ad hoc research working group on body composition, health and performance, under the auspices of the IOC medical commission. British Journal of Sports Medicine, 47(16), 1012–1022. [DOI] [PubMed] [Google Scholar]
- Tod D., Edwards C., Cranswick I. (2016). Muscle dysmorphia: Current insights. Psychology Research and Behavior Management, 9, 179–188. doi: 10.2147/PRBM.S97404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turton R., Goodwin H., Meyer C. (2017). Athletic identity, compulsive exercise and eating psychopathology in long-distance runners. Eating Behaviors, 26, 129–132. doi: 10.1016/j.eatbeh.2017.03.001 [DOI] [PubMed] [Google Scholar]
- Veale D., Akyuz E. U., Hodsoll J. (2015). Prevalence of body dysmorphic disorder on a psychiatric inpatient ward and the value of a screening question. Psychiatry Research, 230(2), 383–386. doi: 10.1016/j.psychres.2015.09.023 [DOI] [PubMed] [Google Scholar]