Abstract
The objective of the current study was to quantify the behavioral intentions of young adult male sexual minorities (MSM) to initiate human papillomavirus (HPV) vaccination and test an integrative model of HPV vaccine decision making. Participants were 575 MSM who were residing in the United States and were between ages 18 and 26 years. Standard direct and indirect measures of attitudes, perceived norms, and perceived behavioral control were employed to explain variation in behavioral intention. Additional background factors—such as concealment of one’s sexual identity, suspicion of health care provider competence in LGBT health issues, perceived threat, and information orientation—were also included in the model. The final model fit the data well and identified a set of salient attitudinal and control beliefs as the strongest determinants of intention (R2 = .38). Perceived threat and information orientation were positively correlated with HPV-related beliefs. Perceived threat was higher among men infected with HIV and lower among men in monogamous relationships. Self-efficacy, as an indirect measure of perceived behavioral control, was inversely related to the general tendency to conceal aspects of one’s sexual orientation and a suspicion of health care providers. Bisexual identified men were more likely to conceal their sexual orientation and be more suspicious of health care providers. In this study, a number of modifiable determinants of HPV vaccine intentions—both psychosocial and environmental—were identified and have implications for targeted and tailored behavioral interventions to promote HPV vaccination among MSM.
Keywords: sexual identity, health education, health promotion and disease prevention, public health, sexually transmitted diseases/infections
Introduction
Targeted behavioral interventions are needed to increase uptake of human papillomavirus (HPV) vaccine among male sexual minorities (MSM) in the United States. This is a risk-based primary prevention strategy recommended by the Advisory Committee on Immunization Practices that prioritized routine vaccination of MSM up to age 26 with the quadrivalent or nonavalent HPV vaccine (Petrosky et al., 2015). The rationale for this recommendation is based on low vaccine coverage (22% in 2014) of adolescent males in the general population (Reagan-Steiner et al., 2015), evidence of considerably higher rates of anal cancer in MSM (Joseph et al., 2008; Machalek et al., 2012), as well as the cost-effectiveness of targeted vaccination (Kim, 2010). Despite this strong recommendation, uptake of this vaccine remains low. Estimates of MSM receiving at least one dose of the three-dose series were just 5% and 13% in 2011 and 2013, respectively (Meites, Markowitz, Paz-Bailey, & Oster, 2014; Reiter, McRee, Katz, & Paskett, 2015).
Lack of awareness about the availability and direct health benefits of HPV vaccination are likely reasons for low uptake among MSM (Nadarzynski, Smith, Richardson, Jones, & Llewellyn, 2014; Newman, Logie, Doukas, & Asakura, 2013). And while this population is believed to regularly utilize health care services at higher rates than other males (Meites, Krishna, Markowitz, & Oster, 2013), health care providers are not routinely recommending HPV vaccination during these visits (Reiter et al., 2015). With routine recommendations, existing behavioral research suggests that uptake among MSM would increase given their overall high acceptability of HPV vaccination (Nadarzynski et al., 2014); however, in concert with needed efforts to change health care provider behaviors regarding the recommendation of HPV vaccination, tailored community-based interventions for MSM are needed to increase awareness, foster positive attitudes and beliefs regarding HPV vaccination, and heighten individual intention to get vaccinated within a given time frame.
The current behavioral research in this area is of limited utility for program planning. No studies in the most recent systematic review of this literature developed or tested a theoretical model of HPV vaccine decision making specific to MSM (Nadarzynski et al., 2014). In fact, only 5 out of the 16 studies overtly applied behavioral theories. The resulting analyses ignored presumed causal priority among variables by simultaneously modeling all predictors with single multivariable models. In addition, measures were constructed without regard for combinatorial rules explicit in health behavior theories (Fishbein & Ajzen, 2010; Hochbaum, 1958). Without strong theoretically based research, the resulting body of evidence provides little information in how vaccine promotion programs targeting MSM would substantively differ from similar programs targeting other populations.
In order to develop a decision-making model focused on HPV vaccination of adult MSM, the integrative model of behavioral prediction (IM) was used to inform this study. This theoretical approach postulates that a set of population-specific salient beliefs underlies the formation of attitudes toward HPV vaccination, perceived norms in favor or against vaccination, and perceived control over one’s ability to get vaccinated if so desired. The effects of attitudes, norms, and perceived control on HPV vaccination are, in turn, mediated by an individual’s behavioral intention (Ajzen, 1991). The model also specifies that beliefs related to HPV vaccination are influenced by a variety of background factors inclusive of personal characteristics and experiences, sociocultural factors, and exposure to information (Fishbein, 2009). The structural relationships among these constructs provide valuable information regarding the decision-making process and were explored in this investigation.
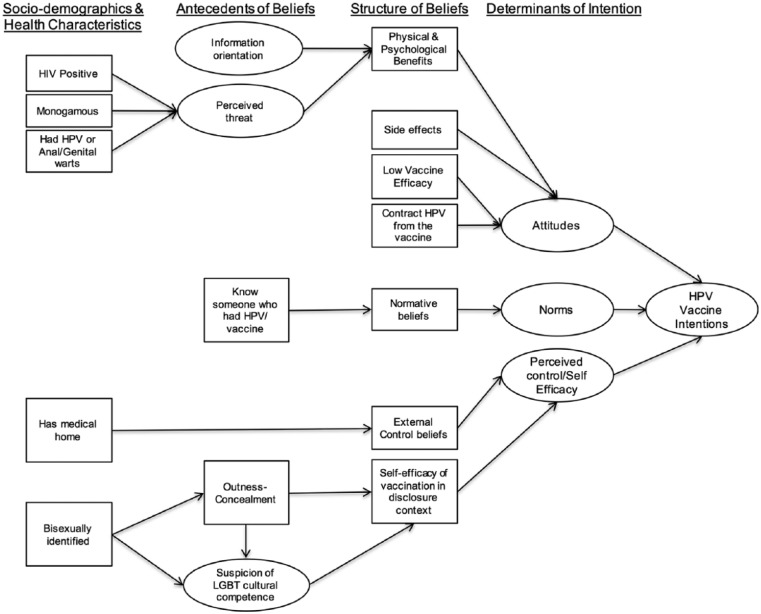
The primary aim of this study was to test and refine the theoretical model depicted in Figure 1 using structural equation modeling (SEM). This model was based on IM constructs and expanded through in-depth formative research with MSM between the ages of 18 and 26 years (Wheldon et al., 2016).
Figure 1.
Proposed model of human papillomavirus (HPV) vaccine intentions among vaccine-eligible male sexual minorities.
Method
This was a cross-sectional Internet-based study. Formative qualitative research with members of the priority population helped explicate antecedent beliefs and subpopulations important when considering HPV vaccination among MSM (Wheldon et al., 2016).
Participants and Procedures
To be included in this study participants needed to be English-speaking men 18 to 26 years of age, residing in the United States, identified as gay, bisexual, and/or have ever had sexual contact with another male, and who have not initiated the HPV vaccine series. Participants were recruited using snowball sampling and paid advertisements through social media and a sexual networking mobile application. All participants were referred to the study website where they provided informed consent and completed the web-based survey. A lottery incentive was offered for 1 of 10 $25 gift cards. The protocol for this research was reviewed and approved by the corresponding authors’ institutional review board.
Measures
Intentions
Three items measured vaccine intentions (α = .90). These items assess intention to “find out more information about HPV,” “make an appointment to talk to a doctor or health care provider about the HPV vaccine,” and to “get your first HPV shot.” Each item specified a time frame “within the next 12 months.” Responses were recorded on a 5-point bipolar scale (unlikely–likely).
Attitudes, Perceived Norms, and Perceived Behavioral Control
Direct measures of attitude, perceived norms, and perceived behavioral control were used according to standard measurement procedures (Fishbein & Ajzen, 2010). Attitudes toward HPV vaccination were measured using a 5-point semantic differential scale (α = .86) including the following adjectives: not worth it/worthwhile, harmful/beneficial, a bad thing for me/a good thing for me, unimportant/important, ineffective/effective. Three items were used to measure perceived norm (α = .70) on a 5-point bipolar scale (disagree–agree). Two items assessed subjective norms (e.g., “In general, people who are important to me would encourage me to receive the HPV vaccine”) and one item assessed descriptive norms (e.g., “Most of my gay/bisexual male friends would get the HPV vaccine if it were offered to them free of charge”). Three items were used to measure perceived behavioral control (α = .70) on a 5-point bipolar scale (disagree–agree). One item measured self-efficacy (“I am confident that I can get the HPV vaccine in the next 12 months”) and two items measured controllability (e.g., “There are factors beyond my control that would prevent me from getting the HPV vaccine in the next 12 months”) and were reverse coded; thus, higher values represent more positive attitudes, supportive norms, and perceived control.
Indirect Measures
The expectancy-value framework was employed to measure indirect attitudes, norms, and control by creating an index of beliefs weighted by their evaluation (Fishbein & Ajzen, 2010). For example, a behavioral belief of strength bi was weighted by a measure of the relevance or importance of that specific outcome ei. The cross product of these two variables is the expectancy-value score (biei) for that specific belief ranging from 1 (lowest) to 25 (highest). These scores were summed to represent an index of the salient beliefs (Σbiei). The same procedure was used for normative beliefs (weighted by motivation to comply; nimi) and control beliefs (weighted by perceived power; cipi). Higher scores represent beliefs in favor of HPV vaccination.
Behavioral Beliefs
Ten behavioral beliefs (see Table 1) were measured representing physical advantages (3 items), psychological advantages (3 items), and disadvantages/concerns associated with HPV vaccination (4 items). Low Efficacy of the vaccine was measured by two items (e.g., “not being completely protected”) that were averaged (α = .71). A single item was used to measure the belief that “I will contract HPV from the vaccine itself.” Perceived advantages were combined (α = .90) for SEM because of high interitem correlation. Outcome evaluations (ei; unimportant–important) and belief strengths (bi; unlikely–likely) were recorded on 5-point bipolar scales.
Table 1.
Behavioral Beliefs Associated With Human Papillomavirus (HPV) Vaccination and Correlations With HPV Vaccine Attitudes.
| Behavioral beliefs | Belief strength (bi) |
Outcome evaluation (ei) |
biei
|
Correlation biei with attitude | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| Physical advantages | |||||||
| It would make me healthier | 3.29 | 1.02 | 4.34 | 0.70 | 14.48 | 5.54 | .42* |
| It would prevent me from getting genital and anal warts | 3.86 | 1.00 | 4.31 | 0.86 | 16.84 | 5.86 | .40* |
| It would prevent me from getting anal cancer | 3.66 | 1.04 | 4.40 | 0.86 | 16.31 | 5.97 | .39* |
| Psychological advantages | |||||||
| Feel protected from HPV | 4.11 | 0.85 | 3.73 | 1.00 | 15.64 | 5.88 | .51* |
| Feel like there is one less thing to worry about | 3.89 | 1.06 | 3.98 | 1.00 | 15.90 | 6.56 | .47* |
| Less likely to spread HPV to future sex partner(s) | 4.22 | 0.86 | 4.11 | 0.94 | 17.64 | 5.90 | .39* |
| Expectancy-value index (Σbiei) | 96.76 | 29.34 | .53* | ||||
| Disadvantages | |||||||
| I will contract HPV from the vaccinea | 1.98 | 1.11 | — | — | — | — | −.17* |
| Not completely protected from future HPV infectionsa | 2.80 | 1.06 | — | — | — | — | −.22* |
| The vaccine may not work for mea | 2.54 | 0.99 | — | — | — | — | −.26* |
| I would have side effects | 2.69 | 1.00 | 2.79 | 0.92 | 7.83 | 4.34 | −.25* |
Note. N = 575. Belief strength and outcome evaluation were measured on a 5-point bipolar scales. biei Ranges from 1 to 25 with higher values indicating likely and important beliefs. Σbiei Ranges from 1 to 150.
Outcome evaluation was not assessed. Correlation coefficient represents correlation with belief strength and at3titude.
p < .05.
Normative Beliefs
Four referents (mother, father, gay male friends, and straight friends) were used to assess normative beliefs. Participants reported on the degree to which each referent would be disapproving–approving of him getting the HPV vaccine (ni). Participants could choose “not applicable” in cases where this person/group was not present. “Not applicable” was recoded to represent the neutral midpoint of the scale so that a scale index could be calculated for each participant. Motivation to comply was measured with this question: “When deciding whether or not to get the HPV vaccine, would you seriously consider the advice/opinion of . . . ” Responses were recorded on a 5-point bipolar scale (unlikely–likely).
Control Beliefs
Four control beliefs (ci) were used to assess the degree to which external factors would make it “more difficult” or “much easier” for respondents to “get the HPV vaccine in the next 12 months” by weighting ci measured on a 5-point bipolar scale (disagree–agree) with a 5-point bipolar perceived power scale (pi; more difficult–much easier).
Self-Efficacy
Two items were used to assess the degree of confidence in getting the HPV vaccine in the event that “you had to talk to your doctor or health care provider about your sexual orientation (e.g., that you are gay or bisexual)” and “your sexual behaviors (e.g., your sexual history).” Responses were recorded on a 5-point unipolar scale (not at all confident–extremely confident). Reponses were averaged to form a self-efficacy score (α = .90).
Perceived Threat
Four indicators of perceived threat were measured (threat of warts on the penis or scrotum, anal warts, anal cancer, and HPV infection). The indictor variables were created from the product of perceived susceptibility (e.g., “Without the HPV vaccine, what do you think the likelihood is that you be infected with HPV?”) with a corresponding measure of severity (e.g., “How serious would it be for you if you became infected with HPV?”). Responses were recorded on 5-point bipolar scales (unlikely–likely and not at all serious–extremely serious). Each composite indicator had a theoretical range from 1 to 25 with higher values indicating greater perceptions of a likely and serious threat. A threat index was created to use in bivariate analyses by averaging all four composite scores (α = .96).
Health Information Orientation
Three items were used to assess health information orientation, which was defined as intrinsic motivation to seek out relevant health information and to process that information (Dutta-Bergman, 2009). These items were adapted from a validated health information orientation scale representing a single latent factor (Dutta-Bergman, 2009). The items used in the current study were (a) “When I take medicine, I try to get as much information as possible about its benefits and side effects”; (b) “Before making a decision about my health, I find out everything I can about the issue”; and (c) “It’s important to be informed about health issues affecting gay and bisexual men.” Responses were recorded on a 5-point bipolar scale. A scale score was calculated by taking the average of the three items (α = .80). Higher values indicate a greater degree of orientation toward relevant health information.
Suspicion of LGBT Cultural Competence
Four items (α = .71) were used to assess suspicion of lesbian, gay, bisexual, transgender (LGBT) cultural competence, which was defined as having previously received lower quality health care as a result of sexual orientation, expressing discomfort talking to a doctor about sexual orientation or sexual behaviors, expressing a preference that a doctor or health care provider not know one’s sexual orientation, and expressing a belief that sexual orientation is not relevant to medical care. Responses were recorded on a 5-point bipolar scale (disagree–agree).
Nebraska Outness Scale–Concealment (NOS-C)
The concealment subscale of the NOS was used to measure the frequency at which an individual conceals his sexual orientation across multiple domains (Meidlinger & Hope, 2014). Responses were recorded on a ratio scale ranging from never (0%) to always (100%). In previous research, the NOS-C demonstrated good internal reliability, as well as discriminant, convergent, and predictive validity (Meidlinger & Hope, 2014). Reliability was acceptable in the current study (α = .71). No existing research has investigated the factor structure of the NOS, so it was included as a measured variable in the structural equation models.
Analysis
A total of 806 respondents met inclusion criteria. Of those, 225 (28%) participants exited the survey before completion. The majority of noncompleters withdrew from participation prior to the midpoint of the survey and were excluded from analyses. An additional six cases were removed because they had more than 20% of missing data. The final analytic sample consisted of 575 respondents.
The SAS statistical software version 9.1 (SAS Institute, Cary, NC) was used to conduct univariate and bivariate analysis. All of the variables violated assumptions of univariate normality; however, the magnitudes of the sample skewness and kurtosis were small, and none surpassed an absolute value of 2 (Tabachnick & Fidell, 2007). The sample size is large enough to assume that the distributional assumptions were met for parametric tests. Nonparametric tests were also conducted for each analysis to check for concordance of results.
Mplus version 7 (Muthén & Muthén, 2007) was used to conduct SEM. SEM is useful in testing theoretical models as it allows for the estimation of the associations among latent and measured variables and attempts to remove measurement error from these estimates. This allows the complete propositional structure of a theory to be tested, including direct and indirect effects. The maximum likelihood estimator with robust standard errors was used to estimate parameters that are robust to nonnormality (Buhi, Goodson, & Neilands, 2007, 2008). A two-step approach (Anderson & Gerbing, 1988) was used to build the models starting with estimating the measurement model and then the structural paths. Although there is no universal agreement regarding fit indices or acceptable model fit (Marsh, Hau, & Wen, 2004), the authors followed the recommendations of Hu and Bentler (1999). Model fit was evaluated using the following indices: the chi-square test of goodness-of-fit index, the comparative fit index (CFI values greater than .95 indicate good fit), the standardized root mean square residual (SRMR values less than .10 are considered favorable), and the root mean square error of approximation (RMSEA values less than .06 indicate good fit; Hu & Bentler, 1999).
Results
Participants were on average 22 years old (SD = 2.43). They were primarily White (n = 363, 63%), college students (n = 329, 58%), with health insurance (n = 476, 83%), and had a place they usually go to for “routine medical care” (n = 426, 74%). The majority identified as gay (n = 431, 75%), but a significant proportion identified as bisexual (n = 127, 22%). Fifty-three (9%) respondents reported no previous male partners, but identified as gay or bisexual. Most were HIV-negative (n = 383, 67%); however, over a quarter reported never being tested (n = 156, 27%). Among those who received an HIV test, 132 (32%) were not tested within the previous year. Twenty-three (4%) reported a previous diagnosis of genital or anal warts.
Salient HPV-Related Beliefs
Behavioral Beliefs
Behavioral beliefs are presented in Table 1. Protecting sex partners from HPV was the belief with the highest expectancy value (biei). The disadvantages of vaccination were generally rated as unlikely to occur and had lower correlations with attitudes (see Table 1; correlations biei with attitude). On average, participants indicated little concern regarding vaccine-related side effects (i.e., belief means in “unlikely” range). As expected, perceived advantages positively correlated and perceived disadvantages negatively correlated with a favorable attitude toward vaccination.
Normative Beliefs
The normative referents regarding HPV vaccination are reported in Table 2. All of the referents were perceived as being supportive of vaccination; however, their influence with regard to this decision was low (see mean values for mi). The degree of social influence is represented by the expectancy-value indicators (nimi). Values greater than 9 (the midpoint) indicated influence supportive of vaccination. The modal referent group was gay male friends, who appear to have some influence over HPV vaccine perceptions. The least influential referents were fathers; however, all normative referents contributed positively toward perceived norms.
Table 2.
Normative Beliefs Associated With Human Papillomavirus Vaccination and Correlations With Perceived Norms.
| Normative beliefs | N | Belief strength (ni) |
Motivation to comply (mi) |
nimi
|
Correlation nimi with norm | |||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| Mother | 513 | 3.91 | 1.32 | 3.19 | 1.66 | 13.29 | 8.72 | .40* |
| Father | 445 | 3.48 | 1.39 | 2.57 | 1.59 | 9.83 | 8.10 | .33* |
| Gay male friends | 521 | 4.19 | 0.99 | 3.57 | 1.43 | 15.35 | 7.58 | .39* |
| Straight friends | 531 | 3.86 | 1.14 | 2.95 | 1.44 | 12.00 | 7.55 | .35* |
| Expectancy-value index (Σnimi) | 48.65 | 22.96 | .45* | |||||
Note. N = 575. Belief strength and motivation to comply were measured on a 5-point bipolar scale. nimi Ranges from 1 to 25 with higher values indicating supportive referents. Statistics are calculated only if referent was mentioned and participant did not indicate “not applicable.” Values of 3 (neutral midpoint of scales) were imputed for participants who chose “not applicable” in calculations of Σnimi.
p < .05.
Control Beliefs
Salient control beliefs are reported in Table 3. These beliefs represent a set of perceived facilitators of HPV vaccination. An examination of the expectancy-value indicators (cipi) identifies that health insurance is the strongest perceived facilitator of vaccination followed by the ability to get vaccinated at locations that offer HIV testing. All of the control beliefs exhibited small to moderate correlations with perceived behavioral control (Table 3; correlations cipi with PBC). Participants expressed a moderate degree of self-efficacy in getting vaccinated if they had to discuss their sexual orientation with a health care provider. Self-efficacy was also positively associated with perceived behavioral control.
Table 3.
Control Beliefs Associated With Human Papillomavirus Vaccination and Correlations With Perceived Behavioral Control (PBC).
| Control beliefs | Belief strength (ci) |
Perceived power (pi) |
cipi
|
Correlation cipi with PBC | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| Find out where to get vaccinated | 3.85 | 1.01 | 4.09 | 1.07 | 15.79 | 6.10 | .37* |
| Have health insurance | 4.20 | 1.02 | 4.02 | 1.21 | 18.97 | 6.45 | .44* |
| Do not need an appointment | 3.13 | 1.10 | 4.44 | 1.02 | 12.44 | 5.90 | .22* |
| Available at HIV testing location | 3.87 | 1.13 | 4.04 | 1.23 | 16.21 | 7.24 | .18* |
| Expectancy-value index (Σcipi) | 63.15 | 0.85 | .42* | ||||
| Perceived self-efficacy | 3.42 | 1.26 | .42* | ||||
Note. N = 575. Belief strength and outcome evaluation were measured on a 5-point bipolar scale. cipi Ranges from 1 to 25 with higher values indicating stronger control beliefs that can help facilitate HPV vaccination.
p < .05.
Descriptive and Bivariate Statistics
Means, standard deviations, and zero-order correlations for all variables are presented in Table 4. Overall, participants expressed positive attitudes toward vaccination (M = 4.23, SD = 0.80; range = 1-5), supportive norms (M = 3.75, SD = 0.79; range = 1-5), and perceived control over their decision to get vaccinated (M = 3.76, SD = 0.85; range = 1-5). More than half (57%) of participants indicated they were “likely/very likely” to initiate HPV vaccination as indicated by the vaccine intention scale (M = 3.26, SD = 1.08; range = 1-5). Zero-order correlations (Table 4) provided initial support for the proposed relationships presented in Figure 1.
Table 4.
Means, Standard Deviations, and Zero-Order Correlations for Indices and Scales.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Intention | — | |||||||||||||||
| 2. Attitude | .47* | — | ||||||||||||||
| 3. PHY advantages | .47* | .46* | — | |||||||||||||
| 4. PSY advantages | .54* | .50* | .68* | — | ||||||||||||
| 5. Low efficacy | −.19* | −.27* | −.19* | −.21* | — | |||||||||||
| 6. Contract HPV | .00 | −.17* | .03 | .01 | .51* | — | ||||||||||
| 7. Side effects | −.06 | −.25* | −.02 | −.01 | .45* | .51* | — | |||||||||
| 8. Norms | .43* | .39* | .49* | .54* | −.14* | −.01 | −.01 | — | ||||||||
| 9. Normative beliefs | .26* | .18* | .31* | .38* | −.12* | .06 | −.04 | .45* | — | |||||||
| 10. PBC | .27* | .16* | .14* | .20* | −.16* | −.14* | −.16* | .17* | .13* | — | ||||||
| 11. Control beliefs | .35* | .30* | .33* | .38* | −.16* | −.10* | −.03* | .30* | .32* | .42* | — | |||||
| 12. Self-efficacy | .14* | .11* | .22* | .17* | −.09* | −.02 | −.03* | .16* | .20* | .24* | .23* | — | ||||
| 13. Threat | .28* | .27* | .33* | .35* | −.08 | .07 | .08 | .27* | .24* | .07* | .18* | .04 | — | |||
| 14. Information-O | .26* | .12* | .26* | .32* | .09* | −.05 | .06 | .23* | .21* | .18* | .35* | .23* | .08* | — | ||
| 15. LGBT-SUS | −.02 | .00 | .02 | .02 | .06 | .16* | .13* | −.01 | −.10* | −.13* | −.10* | −.51* | .01 | −.16* | — | |
| 16. Concealment | −.04 | .04 | −.04 | −.00 | −.01 | −.12* | −.01 | −.12* | −.02 | −.04 | .01 | −.23* | .03 | −.03 | .22* | — |
| Mean | 3.26 | 4.23 | 47.57 | 49.19 | 2.67 | 1.97 | 7.84 | 3.75 | 48.66 | 3.76 | 63.15 | 3.42 | 9.51 | 4.24 | 2.49 | 45.66 |
| Standard deviation | 1.07 | 0.80 | 15.20 | 16.82 | 0.90 | 1.11 | 4.34 | 0.79 | 22.96 | 0.85 | 18.06 | 1.26 | 4.99 | 0.69 | 0.86 | 26.08 |
Note. N = 575. PHY = physical; PSY = psychological; low efficacy = concerns about the efficacy of HPV vaccination; contract HPV = concern that one can contract human papillomavirus from the vaccine; PBC = perceived behavioral control; information-O = information orientation; LGBT-SUS = Suspicion of LGBT Cultural Competence Scale; Concealment = Nebraska Outness Scale–Concealment subscale.
p < .05.
Test of an Integrative Model of HPV Vaccine Decision Making
Measurement Model
Confirmatory factor analysis of the measurement model reported poor absolute fit of the data to the latent factors, χ2 (df) = 428.76 (254), p < .001; however, the chi-square test is highly sensitive to sample size so additional fit indices were examined. All three fit indices suggested the measurement model fit the data well (RMSEA = .04, 90% CI [.03, .04]; CFI = .97; SRMR = .04). All items significantly loaded on their respective factor (results not reported). No modifications to the measurement model were warranted.
Structural Model
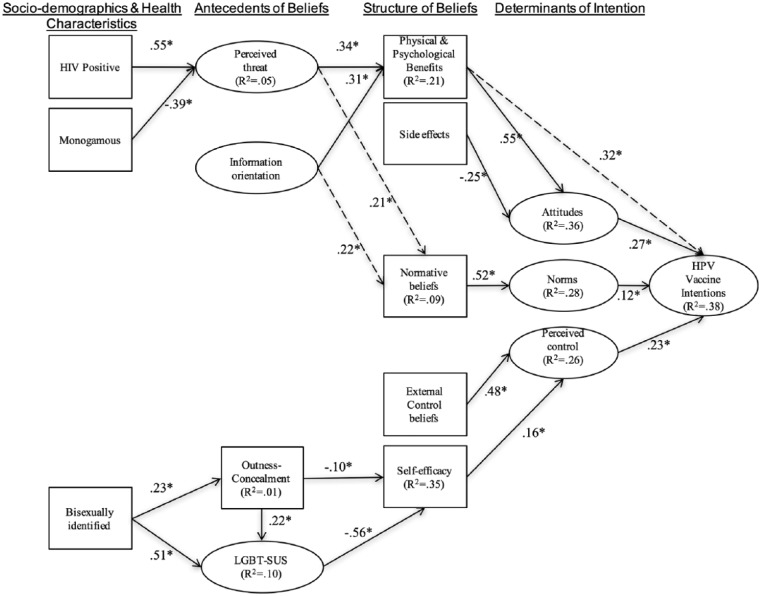
The initial structural model tested 28 structural relationships. This model had poor fit among all but one of the indices examined: χ2 (df) = 1808.28 (640), p < .001; RMSEA = .06, 90% CI [.05, .06]; CFI = .85; SRMR = .10. Nonsignificant pathways were removed from the model one at a time starting with the weakest relationships (indicated by lower β values). The revised model (Model 2) approximated acceptable fit: χ2 (df) = 1132.22 (503), p < .001; RMSEA = .05, 90% CI [.04, .05]; CFI = .91; SRMR = .10. Modification indices were examined to determine if any theoretically relevant paths could be added to the model in order to increase fit. Based on this information, three additional paths were added (see Figure 2 dotted lines). In addition, control beliefs were allowed to covary with Physical/Psychological benefits and normative beliefs. This final model (Model 3; see Figure 2) exhibited adequate fit: χ2 (df) = 1265.48 (507), p < .001; RMSEA = .05; 90% CI [.05, .06]; CFI = .91; SRMR = .09.
Figure 2.
Structural model of human papillomavirus (HPV) vaccine intentions among vaccine-eligible male sexual minorities.
Note. N = 568 (7 cases were removed for listwise deletion); dotted lines indicate post hoc paths; parameter estimates are standardized regression (β) weights. Model fit statistics: χ2 (df) = 1265.48 (507), p < .001; root mean square error of approximation = .05, 90% CI [.04, .05]; comparative fit index = .91; standardized root mean square residual = .09.
*p < .05.
Determinants of intention
Standardized parameter estimates for the final model are depicted in Figure 2. Results are presented here moving from the right side elements of Figure 2 to the left side elements. The largest direct effects on intentions were from Physical/Psychological benefits (β = 0.32, Β = 0.01; 95% CI [0.01, 0.01]) and attitudes (β = 0.27, Β = 0.25; 95% CI [0.17, 0.34]). Norms had a smaller association with intention (β = 0.12, Β = 0.12; 95% CI [0.02, 0.20]). Perceived control had a moderately strong association with intentions (β = 0.23, Β = 0.31; 95% CI [0.20, 0.44]). Thirty-eight percent of the variation in intentions was explained by the model.
Structure of beliefs
There were five key characteristics of HPV-related beliefs that underscore the main determinants of intention. This included beliefs regarding the physical/psychological benefits of vaccination, which was strongly correlated with positive attitudes (β = 0.55, Β = 0.02; 95% CI [0.01, 0.02]). Concern about potential side effects was negatively associated with attitudes (β = −0.25, Β = −0.05; 95% CI [−0.06, −0.03]). As was expected, normative, control, and efficacy beliefs were each positively associated with their respective determinant.
Antecedents of beliefs
The strongest antecedents of HPV-related beliefs were perceived threat, suspicions of LGBT cultural competence, and information orientation. The higher perceptions of threat correlated with higher perceived benefits from vaccination (β = 0.34, Β = 2.27; 95% CI [1.82, 2.75]). In addition, the perceived benefits of vaccination were higher among those with higher levels of health information orientation (β = 0.31, Β = 12.79; 95% CI [8.90, 16.36]). There was also a strong negative association between those expressing suspicion of LGBT cultural competence and self-efficacy (β = −0.56, Β = −1.63; 95% CI [−2.05, −1.32]).
Sociodemographic targets
HIV positive men had higher levels of perceived threat (β = 0.55, Β = 2.34; 95% CI [0.74, 3.83]). Inversely, men in monogamous relationships reported lower levels of threat (β = −.39, Β = −1.67; 95% CI [−2.25, −1.04]). Bisexual identification was positively associated with both Outness–concealment (β = 0.23, Β = 5.91; 95% CI [1.46, 10.37]) and suspicions of LGBT cultural competence (β = 0.51, Β = 0.23; 95% CI [0.14, 0.31]).
Indirect effects
The indirect effects were relatively small (results not reported). The most theoretically meaningful indirect effects were from the salient belief measures to intentions, mediated by the main determinants of behavior (i.e., attitudes, norms, perceived control/efficacy). All of these indirect paths were statistically significant and among the largest indirect paths identified in the model.
Discussion
Existing research on the psychology of HPV vaccine decision making among MSM relies primarily on standard theoretical constructs to explain readiness or motivation to initiate vaccination (Nadarzynski et al., 2014; Newman et al., 2013). These models are therefore limited to the most proximate determinants of intention, acceptability, or willingness. Tailoring health education interventions for this population requires the identification of modifiable beliefs salient to MSM when making decisions about HPV vaccination. Insights into how to change HPV-related beliefs come from the identification of their antecedents. The model identified in this study provides a rich source of information for targeting and tailoring vaccine promotion programs for young MSM by explicating these beliefs and antecedents.
The strongest determinant of behavioral intention was attitude. According to this model, HPV-related attitudes can be changed by increasing beliefs in physical and psychological benefits of vaccination and decreasing concerns about side effects. Some of the beliefs most strongly associated with attitude toward HPV vaccination were experiential (e.g., feeling protected from HPV and allaying the worry associated with sexual activity). These findings are consistent with in-depth qualitative research with MSM that reported infection with HPV—even in the absence of diseases such as anogenital warts or cancer—can be anxiety provoking (Wheldon et al., 2016). The vaccine therefore becomes a method of reducing anxiety by increasing a sense of protection.
Perceived threat and information orientation serve as the key motivational factors related to perceived advantages of vaccination. The antecedent role of perceived threat in HPV vaccine decision making was identified in a previous study of young MSM (Wheldon, Buhi, & Daley, 2013). This relationship implies that the motivation to process health information (e.g., information about the advantages of vaccination) varies as a function of perceived threat (Chen & Chaiken, 1999; Wheldon et al., 2013). As such, this theoretical model predicts that messages regarding the advantages of HPV vaccination are more likely to be systematically processed if a threat stimulus is present (Das, de Wit, & Stroebe, 2003). Threat messages should focus on the social, emotional, and physical consequences of HPV infection and utilize a combination of communication channels in to reach individuals with varying health information orientations (Dutta-Bergman, 2009).
Perceived behavioral control was a moderate predictor of vaccine intentions and was a function of external control beliefs, as well as perceived self-efficacy to disclose one’s sexual orientation. Men who believed that their health insurance covered the vaccine had higher perceived control and higher intentions to get vaccinated. The Affordable Care Act mandates that health plans must provide coverage for HPV vaccinations that are determined by Advisory Committee on Immunization Practices to be for routine use (Kaiser Family Foundation, 2015). Therefore, health plans should cover HPV vaccination for MSM up to age 26 without cost-sharing. This information should be included in promotion messages to minimize concerns over cost among men with health insurance. For uninsured men, programs created to control hepatitis in MSM through education and vaccination can serve as models for targeted HPV vaccine promotion (Mast et al., 2006). This approach is especially suited to this population given the finding that they would be more likely to get vaccinated if they could do so during their regular HIV testing visits. In addition, bundling services like HPV vaccination with other recommended vaccinations, STI screening, and HIV prevention (e.g., preexposure prophylaxis) for MSM may increase the uptake of these services (van den Berg, Larson, Zimet, & Lally, 2014). Research is needed to determine what services should be bundled and what training is required for providers to ensure comprehensive care to MSM.
Self-efficacy was inversely related to a general tendency to conceal aspects of one’s sexual orientation and a suspicion of health care providers. Both of these relationships have important implications for patient–provider interactions. The likelihood of sexual orientation disclosure will increase if providers can demonstrate that they care about and are knowledgeable about the unique health issues and concerns of LGBT populations. This would improve patient–provider interactions and allow for more opportunities to recommend preventive services like HPV vaccination.
Normative influence was less important to HPV vaccine intentions relative to attitudes and perceived behavioral control. This construct has not be modeled in most studies of vaccine decision making in MSM; however, in two previous studies, neither injunctive nor descriptive norms were correlated with intentions (Reiter, Brewer, McRee, Gilbert, & Smith, 2010; Wheldon, Daley, Buhi, Nyitray, & Giuliano, 2011). The current findings are in contrast to previous research that demonstrated the strong influence of perceived norms on HPV vaccine acceptability among adult heterosexual males (Gerend & Barley, 2009) and females (Kahn, Rosenthal, Hamann, & Bernstein, 2003). Lower normative influence among MSM may result from a desire to keep issues related to their sexuality private, which has been described in the qualitative literature (Gutierrez et al., 2013; Wheldon et al., 2016). This was also reflected by normative beliefs that valued gay male peers as more influential in HPV vaccine decisions than heterosexual friends or parents.
The exogenous variables in the model identified three subpopulations of MSM who may benefit from targeted health education interventions. HIV-infected individuals exhibited higher perceived threat of HPV. It may be that MSM infected with HIV have different experiences with the health care system (Meites et al., 2013) and are motivated to process information about HPV in significantly different ways given their increased risk of cancer (Burkhalter et al., 2011). Messages focusing on anal cancer prevention may be particularly effective for HIV-infected MSM.
In previous research, bisexual identity has been unrelated to HPV vaccine intentions (Wheldon et al., 2011) or initiation (Reiter et al., 2015); however, in the current study, bisexual identity was indirectly associated with intentions through lower self-efficacy resulting from higher concealment of sexual orientation and suspicion of health care providers. This model suggests that—and is supported by previous research (Durso & Meyer, 2013)—bisexual identified men may be less likely to ask about HPV vaccination if they have to discuss their sexual behaviors. Lack of trust in patient–provider interactions among bisexual men may in turn result in fewer opportunities for vaccination. Additional research is needed to identify ways to increase patient–provider communication among this subpopulation of MSM.
Men in monogamous relationships exhibited lower levels of perceived threat. This relationship supports finding in previous qualitative research where MSM described low levels of perceived HPV threat as a result of being in a monogamous, or semimonogamous, relationships (Wheldon et al., 2016). Further research is needed to identify the specific targets of behavioral interventions for this unique subpopulation.
The final model reported here represents the set of beliefs, experiences, and expectations associated with HPV vaccination that were described by MSM through in-depth qualitative interviews (Wheldon et al., 2016) and quantitatively tested in the current investigation. This model was simplified by removing weak associations unlikely to represent causal relationships, while maintaining the complexity that represents the decision-making process unique to this population. Three additional propositions were added to the model that were empirically based but raise important theoretical implications for further research. Specially, the authors identified that attitudes did not fully account for the association between perceived benefits and intention, and that there are normative processes involved in the formation of personalized risk and health information seeking.
Study Limitations
The conceptual population for this study is based on stigmatized sexual identities and behaviors that are often concealed or “hidden.” Therefore, constructing sampling frames that closely approximate these types of conceptual populations is inherently flawed, which results in biased samples. In addition to the use of nonprobability sampling techniques, cross-sectional data and proxy measures for vaccine initiation (e.g., intention to vaccinate) limits the degree to which the IM could be fully tested. Longitudinal research is needed to model vaccine uptake directly. Also, the current study comprised adult MSM (i.e., 18-26 years old). Future research would benefit by sampling younger MSM who likely have unique barriers to HPV vaccination.
Conclusion
Despite these methodological limitations, this study makes a unique contribution to the behavioral HPV vaccination literature by explicating a theoretical model of vaccine decision making specific to vaccine-eligible adult MSM. In this model, a number of modifiable determinants of HPV vaccine intentions—both psychosocial and environmental—were identified. These determinants can be used to target and tailor behavioral interventions for this priority population and inform the content of patient–provider conversations about this vaccine. Such interventions are critically needed in the prevention of anal and other HPV-related cancers, as well as to mitigate HPV-related disparities among MSM in the United States.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the University of South Florida Department of Community and Family Health Student Research Award and by the National Cancer Institute under the Ruth L. Kirschstein National Research Service Award (5F31CA168015-02)
References
- Ajzen I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179-211. [Google Scholar]
- Anderson J. C., Gerbing D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103, 411-423. [Google Scholar]
- Buhi E. R., Goodson P., Neilands T. B. (2007). Structural equation modeling: A primer for health behavior researchers. American Journal of Health Behavior, 31, 74-85. doi: 10.5993/AJHB.31.1.8 [DOI] [PubMed] [Google Scholar]
- Buhi E. R., Goodson P., Neilands T. B. (2008). Out of sight, not out of mind: Strategies for handling missing data. American Journal of Health Behavior, 32, 83-92. doi: 10.5555/ajhb.2008.32.1.83 [DOI] [PubMed] [Google Scholar]
- Burkhalter J. E., Hay J. L., Coups E., Warren B., Li Y., Ostroff J. S. (2011). Perceived risk for cancer in an urban sexual minority. Journal of Behavioral Medicine, 34, 157-169. doi: 10.1007/s10865-010-9296-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Chaiken S. (1999). The heuristic-systematic model in its broader context. In Chaiken S., Troppe Y. (Eds.), Dual-process theories in social psychology (1st ed., pp. 73-96). New York, NY: Guilford Press. doi: 10.4319/lo.2013.58.2.0489 [DOI] [Google Scholar]
- Das E., de Wit J., Stroebe W. (2003). Fear appeals motivate acceptance of action recommendations: Evidence for a positive bias in the processing of persuasive messages. Personality and Social Psychology Bulletin, 29, 650-664. doi: 10.1177/0146167203029005009 [DOI] [PubMed] [Google Scholar]
- Durso L. E., Meyer I. H. (2013). Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sexuality Research and Social Policy, 10(1), 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta-Bergman M. J. (2009). Primary sources of health information: Comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Communication, 16, 273-288. doi: 10.1207/S15327027HC1603 [DOI] [PubMed] [Google Scholar]
- Fishbein M. (2009). An integrative model for behavioral prediction and its application to health promotion. In DiClemente R. J., Crosby R. A., Kegler M. C. (Eds.), Emerging theories in health promotion practice and research (pp. 215-234). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Fishbein M., Ajzen I. (2010). Predicting and changing behavior. New York, NY: Psychology Press. [Google Scholar]
- Gerend M. A., Barley J. (2009). Human papillomavirus vaccine acceptability among young adult men. Sexually Transmitted Diseases, 36, 58-62. doi: 10.1097/OLQ.0b013e31818606fc [DOI] [PubMed] [Google Scholar]
- Gutierrez B., Leung A., Jones K. T., Smith P., Silverman R., Frank I., Leader A. E. (2013). Acceptability of the human papillomavirus vaccine among urban adolescent males. American Journal of Men’s Health, 7, 27-36. doi: 10.1177/1557988312456697 [DOI] [PubMed] [Google Scholar]
- Hochbaum G. (1958). Public participation in medical screening programs: A sociopsychological study. Washington, DC: Public Health Service. [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1-55. [Google Scholar]
- Joseph D. A., Miller J. W., Wu X., Chen V. W., Morris C. R., Goodman M. T., . . . Cress R. D. (2008). Understanding the burden of human papillomavirus-associated anal cancers in the US. Cancer, 113(Suppl. 10), 2892-2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn J. A., Rosenthal S. L., Hamann T., Bernstein D. I. (2003). Attitudes about human papillomavirus vaccine in young women. International Journal of STD & AIDS, 14, 300-306. doi: 10.1258/095646203321605486 [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2015). Preventive services covered by private health plans under the Affordable Care Act. Retrieved from http://kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans/
- Kim J. J. (2010). Targeted human papillomavirus vaccination of men who have sex with men in the USA: A cost-effectiveness modelling analysis. Lancet Infectious Diseases, 10, 845-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machalek D. A., Poynten M., Jin F., Fairley C. K., Farnsworth A., Garland S. M., . . . Grulich A. E. (2012). Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men : A systematic review and meta-analysis. Lancet Oncology, 13, 487-500. doi: 10.1016/S1470-2045(12)70080-3 [DOI] [PubMed] [Google Scholar]
- Marsh H. W., Hau K., Wen Z. (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizaing Hu and Benter’s (1999) findings. Structural Equation Modeling, 11, 452-483. doi: 10.1207/s15328007sem1103 [DOI] [Google Scholar]
- Mast E. E., Weinbaum C. M., Fiore A. E., Alter M. J., Bell B. P., Finelli L., . . . Ward J. W. (2006). A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States. Morbidity and Mortality Weekly Report, 55(16), 1-25. [PubMed] [Google Scholar]
- Meidlinger P. C., Hope D. A. (2014). Differentiating disclosure and concealment in measurement of outness for sexual minorities : The Nebraska Outness Scale. Psychology of Sexual Orientation and Gender Diversity, 1, 489-497. [Google Scholar]
- Meites E., Krishna N. K., Markowitz L. E., Oster A. M. (2013). Health care use and opportunities for human papillomavirus vaccination among young men who have sex with men. Sexually Transmitted Diseases, 40, 154-157. doi: 10.1097/OLQ.0b013e31827b9e89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meites E., Markowitz L. E., Paz-Bailey G., Oster A. M. (2014). HPV vaccine coverage among men who have sex with men: National HIV Behavioral Surveillance System, United States, 2011. Vaccine, 32, 6356-6359. doi: 10.1016/j.vaccine.2014.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., Muthén B. (2007). Mplus user’s guide (Version 7.0). Los Angeles, CA: Author. [Google Scholar]
- Nadarzynski T., Smith H., Richardson D., Jones C. J., Llewellyn C. D. (2014). Human papillomavirus and vaccine-related perceptions among men who have sex with men: A systematic review. Sexually Transmitted Infections, 90, 515-523. doi: 10.1136/sextrans-2013-051357 [DOI] [PubMed] [Google Scholar]
- Newman P. A., Logie C. H., Doukas N., Asakura K. (2013). HPV vaccine acceptability among men: A systematic review and meta-analysis. Sexually Transmitted Infections, 89, 568-574. doi: 10.1136/sextrans-2012-050980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosky E., Bocchini J. A., Hariri S., Chesson H., Curtis R., Saraiya M., . . . Markowitz L. E. (2015). Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. Morbidity and Mortality Weekly Report, 64(11), 300-304. [PMC free article] [PubMed] [Google Scholar]
- Reagan-Steiner S., Yankey D., Jeyarajah J., Elam-Evans L. D., Singleton J. A., Curtis C. R., . . . Stokley S. (2015). National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years—United States, 2014. Morbidity and Mortality Weekly Report, 64(29), 784-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter P. L., Brewer N. T., McRee A., Gilbert P., Smith J. S. (2010). Acceptability of HPV vaccine among a national sample of gay and bisexual men. Sexually Transmitted Diseases, 37, 197-203. doi: 10.1097/OLQ.0b013e3181bf542c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter P. L., McRee A., Katz M. L., Paskett E. D. (2015). Human papillomavirus vaccination among young adult gay and bisexual men in the United States. American Journal of Public Health, 105(1), 96-102. doi: 10.2105/AJPH.2014.302095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2007). Using multivariate statistics (5th ed.). Boston, MA: Pearson/Allyn and Bacon. doi: 10.1037/022267 [DOI] [Google Scholar]
- van den Berg J. J., Larson H. E., Zimet G. D., Lally M. A. (2014). Bundling human papillomavirus vaccination and rapid human immunodeficiency virus testing for young gay and bisexual men. LGBT Health, 1, 233-237. doi: 10.1089/lgbt.2014.0028 [DOI] [PubMed] [Google Scholar]
- Wheldon C. W., Buhi E. R., Daley E. M. (2013). Gay and bisexual men’s human papillomavirus vaccine intentions: A theory-based structural equation analysis. Journal of Health Psychology, 18, 1177-1186. doi: 10.1177/1359105312459875 [DOI] [PubMed] [Google Scholar]
- Wheldon C. W., Daley E. M., Buhi E. R., Baldwin J. A., Nyitray A. G., Giuliano A. R. (2016). HPV vaccine decision-making among young men who have sex with men. Health Education Journal, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheldon C. W., Daley E. M., Buhi E. R., Nyitray A. G., Giuliano A. R. (2011). Health beliefs and attitudes associated with HPV vaccine intention among young gay and bisexual men in the southeastern United States. Vaccine, 29, 8060-8065. doi: 10.1016/j.vaccine.2011.08.045 [DOI] [PubMed] [Google Scholar]