Abstract
Background:
Supracondylar humerus fracture is the most common fracture around elbow in children. Closed reduction and percutaneous Kirschner wire (pin) fixation is the standard method of managing displaced extension type (Gartland Type II and Type III) supracondylar humerus fractures. The configuration of wires is debatable. Although two crossed K-wires are mechanically stable, there is an inherent risk of ulnar nerve injury. Lateral K-wires – parallel or divergent – are good alternative. This study was aimed at identifying the best configuration for the lateral wires.
Materials and Methods:
Patients with Gartland type 3 supracondylar humerus fractures were randomized by envelope method to receive closed reduction and K-wire fixation in either a parallel or divergent fashion. The patients were followed up at 3 weeks for wire removal and at 6 weeks and 3 months after surgery. Baumann's angle, functional outcome as per Flynn's criteria, and range of motion were recorded in each visit. Effect of delay in surgery was also evaluated as a secondary outcome.
Results:
Nineteen patients received fixation with parallel wires and 11 patients had divergent fixation. No loss of reduction was seen in any patient at 3 months. No statistically significant difference was seen in the Baumann's angles and outcome according to Flynn's criteria irrespective of the wire configuration (divergent or parallel). Furthermore, the delay in surgery was also found not to have a significant effect on the functional outcome.
Conclusions:
Both parallel and divergent K-wire configurations provide satisfactory stability when accurate reduction and adequate fixation of the fracture has been done. Based on the limited number of patients in this study, one configuration cannot be judged to be superior to the other.
Keywords: Baumann's angle, closed reduction, Flynn's criteria, Gartland's Type 3, supracondylar humerus fracture
MeSH terms: Pediatrics, humerus, humeral fractures
Introduction
Supracondylar humerus fractures being the most common pediatric fracture around the elbow account for nearly three-fourth of all upper-extremity fractures.1,2,3 Closed reduction and percutaneous Kirschner wire (pin) fixation is the standard method of managing displaced extension type (Gartland Type II and Type III) supracondylar humerus fractures. Many investigators have used two crossed pins: one introduced medially and one laterally.4,5,6 Few have used two or three lateral pins without any medial pin.7 The optimal configuration of percutaneous pin fixation is however debatable. Biomechanically, a crossed pin configuration (one medial and one lateral) provides increased stability but carries the risk of iatrogenic ulnar nerve injury during insertion of the medial pin.8,9,10 Conversely, lateral pin fixation avoids the danger of iatrogenic ulnar nerve injury but has been proven to be mechanically less stable compared to crossed pin configuration.11,12,13,14,15 There are studies which have proven that lateral-only fixation is good enough for maintaining reduction while simultaneously avoiding injury to the ulnar nerve.16 However, except for the study by Lee et al.,17 not much discussion or brainstorming has been done on the configuration of pins when using lateral-only pins, i.e. whether to use the pins in parallel or divergent configuration. The present study compares the radiological and functional outcomes of lateral-only pin fixation in parallel and divergent configuration for Gartland Type III supracondylar humerus fractures in terms of loss of reduction, late deformity, and functional outcome. In addition, the effect of delay in surgery on the final Baumann's angle and the functional outcome was also evaluated.
Materials and Methods
This was a single-center prospective randomized study conducted between April 2014 and September 2015 after approval by the Institutional Ethics Committee. Children with Type III Gartland supracondylar fractures between the ages of 2 and 12 years were included. Children presenting up to 7 days of injury were considered for inclusion. Children with vascular injuries, open fractures, transphyseal injuries, with blisters, with established compartment syndrome at presentation, and those who would eventually require an open reduction due to inadequate closed reduction were planned to be excluded from the study. The children were randomized into two groups using the opaque sealed envelope technique for fixation with parallel or divergent pins. A written informed consent was obtained from the parents/legal guardians of each patient before proceeding for operative fixation. The details were recorded on Microsoft Excel Sheet and statistical analysis was done using SPSS version 20 (IBM Corporation, New York, USA).
Operative procedure
General anesthesia was used in all patients. Intravenous cephalosporin was given at the time of induction. Traction was applied with the elbow flexed to about 20°. Next, varus and valgus angular alignment was corrected by movement of the forearm. Medial and lateral fragment translation was corrected with direct movement of the distal fragment by the surgeon's thumb with image confirmation. The elbow was slowly flexed while anterior pressure was applied to the olecranon with the thumb. The limb was flexed in pronation or supination depending on the initial displacement of the distal fragment. Reduction was checked by Jones view and by oblique views to assess the reduction of medial and lateral pillars. Lateral view was obtained by moving the image intensifier and not by moving the limb. Continuity of the medial and lateral pillars on oblique views with reformed tear drop and the anterior humeral line crossing the capitellum on lateral view were taken as the signs of having obtained reasonable reduction. Once the reduction was judged to be appropriate, the position was maintained using an elastic bandage.
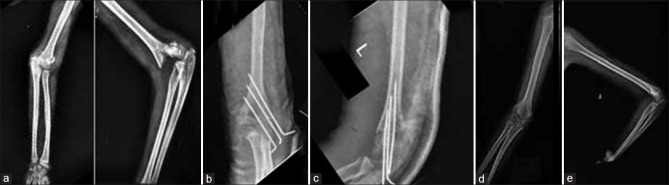
One K-wire (1.6 mm) was placed against the lateral condyle and the position was checked under image intensifier. It was advanced initially by hand and then after getting some purchase, with a wire driver through the fracture site to engage the opposite cortex. The first wire was aimed to pass through the olecranon fossa, thereby providing purchase in four cortices and provide room for placing one more wire on either side. One K-wire (1.6 mm) each on lateral and medial side of the first K-wire was then inserted under image intensifier control, well separated at the fracture site in parallel or divergent manner depending on the preoperative randomization. To ensure adequate divergent placement of the wires within the bone, they were crossed by the same amount outside the skin [Figure 1]. After insertion of all the wires, stability of the fixation was assessed by applying varus and valgus stress and by putting the limb into maximum permissible flexion and extension movements. Image intensifier images were used to assess any loss of reduction after stressing the fixation. The wires were left protruding from the skin for easy removal in the outpatient clinic. The intraoperative Bauman's angle was recorded.
Figure 1.

Intraoperative image showing a trick for achieving divergence inside the arm. the K-wires should cross each other outside for diverging inside
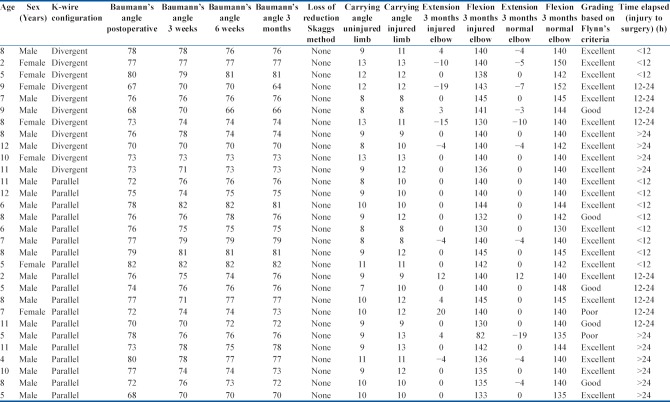
Postoperatively, the limb was immobilized for 3 weeks in an above-elbow plaster slab. The wires were removed at first follow-up visit i.e at 3 weeks. After removal of the wires, physiotherapy was started for regaining the range of motion under the supervision of a physiotherapist. Aggressive stretching was always avoided. Follow-up evaluations were done at 6 weeks, and 3 months from the day of surgery. Loss of reduction was assessed by the method described by Skaggs et al.16 by measuring the Baumann's angle on radiographs obtained in peri-operative period and at 3 months after surgery. The maintenance of reduction was also assessed on lateral view by drawing the anterior humeral line. At the third followup (3 months after surgery), range of motion of both the injured and normal elbows was measured, along with the carrying angles, and the functional outcome was assessed based on Flynn's criteria [Figures 2 and 3].
Figure 2.
X-ray of elbow joint with arm and forearm showing (a) Preoperative radiograph with Gartland III supracondylar fracture (b and c) Immediate postoperative radiograph with divergent K-wire configuration. (d and e) Anteroposterior and lateral views after removal of K-wires 3 months postoperatively
Figure 3.
X-ray of elbow joint with arm and forearm showing (a) Gartland type III supracondylar fracture. (b and c) Immediate postoperative radiograph with parallel K-wire configuration. (d and e) Anteroposterior and lateral views after removal of K-wires 3 months postoperatively
Results
Thirty patients who fulfilled inclusion and exclusion criteria were included in the study. The average age was 7.6 years (range 2-12 years). Twenty three patients (77%) were male and 7 (23%) were female. Left side was involved in 19 and right side in 11 patients. Seventeen patients had posterolateral displacement, whereas 13 had posteromedial displacement. Four patients had radial nerve paresis at presentation, whereas two had anterior interosseous nerve palsy. There was no iatrogenic nerve injury. All the six patients with preoperatively diagnosed nerve injuries recovered within 3 months. Radial pulse was not palpable at the time of presentation in nine patients. Pulses returned in four patients immediately after reduction and fixation. However, five patients did not have palpable radial pulse even after reduction and fixation. Of these, four had pink pulseless hand and were kept under observation and one patient underwent thrombectomy by vascular surgeon. However, at 3 months, radial pulse had returned in all the patients.
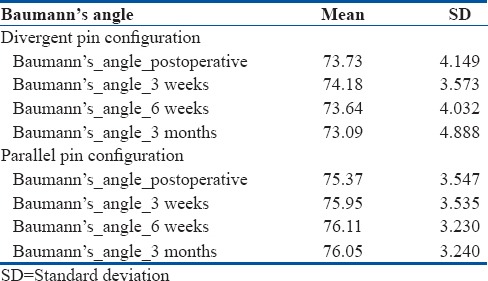
Nineteen (63%) patients were treated with three parallel K-wire fixation and 11 (37%) were treated with three divergent K-wire fixation [Table 1]. Based on the method described by Skaggs et al.,16 no loss of reduction was found in any patient (i.e., in none of them, Baumann's angle changed more than 6°) at follow up. Using ANOVA for intragroup Baumann's angle change, no statistically significant difference was found in Baumann's angle values measured at immediate postoperative period, at 3 weeks, 6 weeks, and at 3 months with either divergent or parallel stabilization configuration (P = 0.720 and 0.395, respectively). The mean Baumann's angles at different followups are presented in Table 2. Thus, both the configurations of K-wires were stable, and no significant loss of reduction was found in either of them at 3 months post fixation. All the fractures eventually healed by 3 months and no case of nonunion or delayed union was identified.
Table 1.
Clinical details of patients
Table 2.
The mean and standard deviation of Baumann's angles at different followups in the two groups of patients
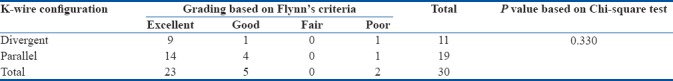
The shortest time between injury and surgical intervention was 5 h and the longest was 136 h. Median delay from injury to surgery was 15 hours. While patients with delayed presentation had somewhat greater degree of swelling around the elbow in comparison to those who presented early, there was no significant difficulty in achieving reduction and fixation. The issue of nonreducible fractures was not encountered. When the patients were compared in terms of time elapsed between injury and surgery and loss of reduction using the Baumann's angle values, no significant difference was found on Friedman ANOVA in Baumann's angle values measured at immediate postoperative period, at 3 weeks, 6 weeks, and 3 months after surgery, whether the surgery was done within 12 h, 12–24 h, or after more than 24 h of sustaining the fracture (P = 0.370, 0.536, and 0.543, respectively). Functional outcome was assessed using Flynn's criteria6 3 months after the surgery. Out of all the thirty patients, 22 had excellent functional outcome, 6 had good outcome, and 2 had poor outcome. The functional outcome as per Flynn's criteria of the two groups (divergent and parallel) is presented in Table 3. There was no significant difference in functional outcomes between the two-wire configurations on Chi-square test.
Table 3.
K-wire configuration (divergent or convergent) and its relation to functional grading by Flynn's criteria
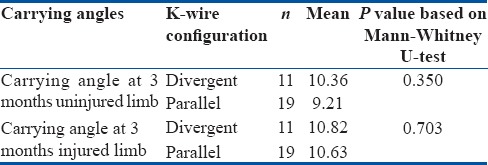
Chi-square test showed no significant difference in functional outcomes (as per the Flynn criteria) and time of surgical intervention from injury [Table 4]. Carrying angles were measured for the injured as well as uninjured limbs at 3 months for evaluating a clinically evident varus or valgus deformity at elbow. No significant difference was found in the carrying angles of the two limbs in either of the two groups [Table 5]. While the detailed data on the range of motion of the injured and uninjured elbows are presented in Table 1, statistical analysis to look for any significant difference in the maximum possible extension and flexion between the elbows of the two groups showed no statistically significant difference on independent samples Mann–Whitney U-test.
Table 4.
Relation between the time elapsed from injury to surgery and the functional status based on Flynn's criteria
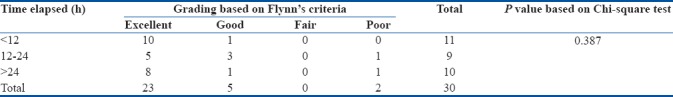
Table 5.
The mean carrying angles at 3 months of the uninjured and injured limbs in both the divergent and parallel configuration groups
We did not encounter any patient with medial comminution though we closely evaluated the preoperative as well as the intraoperative image intensifier images. In addition, aborting the procedure of closed reduction and pinning was not required in any patient. There was no vascular injury in any of the patients during either reduction or fixation. One patient suffered from compartment syndrome of forearm postoperatively and was managed with fasciotomy and secondary closure. The course of followup and duration of retention of pins were not changed as the fracture was found to be healing well. Secondary pin loosening, superficial or deep infections, and pin migration were not seen in any patient.
Discussion
Closed reduction and percutaneous pin fixation for the management of pediatric supracondylar humerus fractures is widely accepted and practiced, but the optimal pin configuration is still controversial.1,2,18,19 Chakraborty et al.20 and Balakumar and Madhuri21 found crossed (medial/lateral) pinning to be superior than two parallel lateral pin fixations. However, many studies have reinforced the observation that both lateral-entry pin fixation and crossed pin configuration are effective in the management of Type III Gartland supracondylar fractures in children.19,22,23 Skaggs et al.16 concluded that lateral-only pins provide adequate stability without endangering the ulnar nerve for fixation of both Type II and III supracondylar humerus fractures. They also advised avoiding the regular use of crossed pins in the treatment of pediatric supracondylar humerus fractures.16
Sapkota et al.24 suggested lateral pinning with 2 or 3 K-wires for proper stabilization and ideal configuration to be divergent to hold medial and lateral columns as the treatment of supracondylar fracture without risk of iatrogenic ulnar nerve injury. Guy et al.25 recommended the use of three pins on the lateral side with no evidence of loss of reduction and no iatrogenic nerve injury in their study. Lee et al.17 were the first one to address the question of ideal lateral-entry pin configuration. In their series, there were a total of 61 patients; 24 with Gartland II fractures and the rest 37 with Gartland III fractures. Forty-one patients had divergent pins and twenty had parallel pins. They found the lateral-entry pins to be adequate for Gartland II and III fractures. In the present study, all the fractures were treated with closed reduction and lateral fixation only.
Guy et al.25 used three divergent pins; 21 patients had an excellent outcome, three patients had good outcome, and 1 achieved poor outcome due to loss of movement alone. They attributed delayed presentation due to neglect over 48 h after injury and gross swelling requiring traction and elevation to be the main factors contributing for less than ideal outcome. However, no statistically significant difference was found in our study on functional outcomes (based on Flynn's criteria) in any of the patients, whether the surgery was performed before 12 h of sustaining the fracture, within 12–24 h, or after 24 h of the injury. Thus, the time elapsed from between injury and surgery has little effect on the functional outcomes, provided a satisfactory reduction has been achieved.
To summarize, the present study found that both configurations of lateral-entry pins are equally stable with similar functional outcomes and there is no loss of reduction in the short term if appropriate reduction is done. It thus supports the other available literature that lateral-entry pins only fixation can be safely used in displaced supracondylar fractures. Delay between injury and surgery too was found not to affect the overall outcome with the prerequisite of a successful closed reduction before pinning.
There are few important limitations of the present study. A major limiting factor is small sample size and short duration of followup. We believe that studies with participation of more patients and more centers need to be carried out with longer followup to clarify whether three parallel lateral pins or three divergent lateral pins should be used for fixing Gartland 3 supracondylar humerus fractures in children.
Conclusions
As the fixation remained stable in both parallel and divergent lateral-entry K-wire configurations at every followup visit, with no loss of reduction or disparity in the functional outcomes, it can be concluded that closed reduction and fixation of Gartland type III supracondylar fractures with lateral-entry K-wires is safe and effective irrespective of the wire (divergent or parallel) configuration selected.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients’ guardians have given their consent for their children's images and other clinical information to be reported in the journal. The patients’ guardians understand that their children's names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Beaty JH, Kasser JR. Fractures about the elbow. Instr Course Lect. 1995;44:199–215. [PubMed] [Google Scholar]
- 3.Boyd HB, Altenberg AR. Fractures about the elbow in children. Arch Surg. 1944;49:213. [Google Scholar]
- 4.Swenson AL. The treatment of supracondylar fractures of the humerus by Kirschner-wire transfixion. J Bone Joint Surg Am. 1948;30A:993–7. [PubMed] [Google Scholar]
- 5.Casiano E. Reduction and fixation by pinning “banderillero” style-fractures of the humerus at the elbow in children. Mil Med. 1960;125:262–4. [PubMed] [Google Scholar]
- 6.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long term followup. J Bone Joint Surg Am. 1974;56:263–72. [PubMed] [Google Scholar]
- 7.Ariño VL, Lluch EE, Ramirez AM, Ferrer J, Rodriguez L, Baixauli F, et al. Percutaneous fixation of supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1977;59:914–6. [PubMed] [Google Scholar]
- 8.Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT, et al. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83-A:735–40. [PubMed] [Google Scholar]
- 9.Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children's elbows. J Pediatr Orthop. 1998;18:43–5. [PubMed] [Google Scholar]
- 10.Rasool MN. Ulnar nerve injury after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1998;18:686–90. doi: 10.1097/00004694-199809000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Gordon JE, Patton CM, Luhmann SJ, Bassett GS, Schoenecker PL. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J Pediatr Orthop. 2001;21:313–8. [PubMed] [Google Scholar]
- 12.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22:440–3. [PubMed] [Google Scholar]
- 13.Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76:253–6. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Kallio PE, Foster BK, Paterson DC. Difficult supracondylar elbow fractures in children: Analysis of percutaneous pinning technique. J Pediatr Orthop. 1992;12:11–5. [PubMed] [Google Scholar]
- 15.Davis RT, Gorczyca JT, Pugh K. Supracondylar humerus fractures in children. Comparison of operative treatment methods. Clin Orthop Relat Res. 2000;376:49–55. [PubMed] [Google Scholar]
- 16.Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86-A:702–7. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lee YH, Lee SK, Kim BS, Chung MS, Baek GH, Gong HS, et al. Three lateral divergent or parallel pin fixations for the treatment of displaced supracondylar humerus fractures in children. J Pediatr Orthop. 2008;28:417–22. doi: 10.1097/BPO.0b013e318173e13d. [DOI] [PubMed] [Google Scholar]
- 18.Oztürkmen Y, Karamehmetoğlu M, Azboy I. Closed reduction and percutaneous lateral pin fixation in the treatment of displaced supracondylar fractures of the humerus in children. Acta Orthop Traumatol Turc. 2005;39:396–403. [PubMed] [Google Scholar]
- 19.Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong) 2004;12:76–82. doi: 10.1177/230949900401200114. [DOI] [PubMed] [Google Scholar]
- 20.Chakraborty MK, Onta PR, Sathian B. Displaced supracondylar fracture of humerus in children treated with crossed pin versus lateral pin: A hospital based study. J Clin Diagn Res. 2011;5:1260–3. [Google Scholar]
- 21.Balakumar B, Madhuri V. A retrospective analysis of loss of reduction in operated supracondylar humerus fractures. Indian J Orthop. 2012;46:690–7. doi: 10.4103/0019-5413.104219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yen YM, Kocher MS. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2(Pt 1)):20–30. doi: 10.2106/JBJS.G.01337. [DOI] [PubMed] [Google Scholar]
- 23.Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. 2012;7:6. doi: 10.1186/1749-799X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sapkota K, Shrestha B. Study of supracondylar fracture of distal humerus in children and its management with lateral k- wire fixation. Nepal J Med Sci. 2014;3:38–43. [Google Scholar]
- 25.Guy SP, Ponnuru RR, Gella S, Tulwa N. Lateral entry fixation using three divergent pins for displaced paediatric supracondylar humeral fractures. ISRN Orthop 2011. 2011:137372. doi: 10.5402/2011/137372. [DOI] [PMC free article] [PubMed] [Google Scholar]