Abstract
Background:
It is uncertain whether single bone fixation is comparable to both bone fixation in the treatment of unstable both bone forearm fractures in children.
Materials and Methods:
A systematic review using PubMed, Embase, and Cochrane Library database searches was performed on October 1, 2015 on English language scientific literature only. Clinical study designs comparing single bone fixation with both bone fixation of pediatric both bone forearm fractures were included. Studies of only one treatment modality were excluded from the study. Studies eligible for inclusion were assessed using the risk of bias tool for nonrandomized studies.
Results:
Metaanalysis points to no significant differences in re-angulation, loss of rotation, union time and complications between single bone and both bone fixation. However, the published research lacks quality.
Conclusions:
Despite scattered evidence and small sample sizes, the metaanalysis suggests single bone fixation can be considered a suitable alternative for both bone forearm fractures in children, as it carries less time in surgery and less cost without compromise in final functional outcome compared to double-bone fixation.
Keywords: Children, forearm fractures, single bone fixation, both bone fixation
MeSH terms: Pediatrics, forearm, fracture fixation
Introduction
Radius and ulna fractures, also known as both bone forearm fractures, are the third most common injuries in children.1,2 Given the excellent remodeling potential, most cases can be successfully treated with closed reduction and casting.3,4 A well thought out casting technique potential for tension banding, residual intact periosteum, and accurate reduction can be performed for most children with forearm fractures. However, surgical intervention is recommended when an acceptable reduction cannot be achieved by nonoperative means.5,6 Various methods of treatment are available to achieve near anatomical reduction, such as compression plating, intramedullary nailing, external fixation, or K-wires incorporated with a plaster or synthetic cast.7,8,9,10,11 Each modality has its advantages and disadvantages. Whatever the method chosen, standard treatments entail fixation of both the radius and ulna, but several studies have reported that single bone fixation alone is often enough to obtain a satisfactory outcome in pediatric patients.12,13,14,15,16 There is still controversy as to whether fixation of the ulna or radius alone is adequate to restore and maintain stability in fractures of both bones of the forearm, and whether it has comparable complication rates.17,18 This study was designed (1) as an overview of the efficacy of treating unstable both bone fractures using either single bone fixation or both bone fixation, (2) to compare treatment outcomes and identify patient groups most likely to benefit from single bone fixation, and (3) to investigate the source of heterogeneity among the studies.
Materials and Methods
Search strategy
The literature search was conducted for studies concerning surgical intervention of pediatric patients with both bone forearm fractures. The search was performed through the following electronic bibliographic databases: PubMed MEDLINE (Medical Literature Analysis and Retrieval System Online), EMBASE (Excerpta Medica dataBASE), and Cochrane Library. The combination of medical subject headings or keywords used included as follows: “children,” “forearm fractures,” “single bone fixation,” and “double bone fixation.” The initial electronic search yielded 126 articles.
Criteria for eligibility
Studies selected for analysis were original studies meeting the following eligibility criteria: (1) assessed primary management of both bone forearm fractures in children with single bone fixation using a both bone fixation group as a control; (2) published in English language; (3) evaluated more than 10 patients; (4) provided enough data for statistical analysis (mean, standard deviation [SD], or interquartile range [IQR], and sample size); and (5) published between January 1960 and October 2015.
Studies that investigated patients with both bone forearm fractures treated by single bone fixation (either ulna or radius) alone, studies that involved re-fractures, case reports, reviews, or studies with incomplete data were excluded from the study.
Review procedure and study quality
After being selected, studies were screened independently by authors (BY and ZY). The only randomized clinical trial found was included in the systematic review, but it was not analyzed in the metaanalysis.18 Nonrandomized studies were assessed using the Risk of Bias Assessment Tool for Nonrandomized Studies (RoBANS),19 which considers similar bias domains to the one produced by Cochrane but is adapted for nonrandomized study designs. Both tools assess the risk of bias in each domain as “high,” “low,” or “unknown.” Reviewers were not blinded to authors and journal. Rather, a study was included for analysis as long as both screeners agreed that it met our inclusion criteria. No authors were contacted.
Definitions
Stability was defined as no loss of reduction when the forearm was screened using fluoroscopy through the full range of pronation.20,21
Angulation was defined as abnormal angle or bend revealing the alignment of long bones that have been affected by injury. Loss of rotation was defined as pronation or supination ranges of motion with the forearm.
Extraction of data
Data from the published papers that met our inclusion criteria were carefully extracted and computerized on the following variables: (1) Corresponding authors’ names (2) publication year (3) study design (4) number of patients in each group (5) instrument used (6) gender; (7) age (8) estimated surgical time (9) casting time (10) complications (11) loss of rotation (12) re-angulation and (13) fracture healing time.
Statistical analysis
Pooled means, SD, and sample size were either identified or calculated from the results of each study. Odds ratios (ORs) with 95% confidence intervals (CIs) were used to evaluate associations. Heterogeneity was quantified by Cochran's Q test with statistical significance set at P < 0.50 and I2 with P < 0.01 interpreted as significant heterogenicity. We used the random-effects model. Where heterogeneity was found, sensitivity analysis was performed by omitting a single study, each, in turn, to see whether a particular omission influenced the overall estimate. All the above analyses were carried out using Review Manager 5.2 software (Cochrane Collaboration, Oxford, UK).
Results
Literature search
The search identified 142 articles, including 16 duplicates which we removed. Of the remaining 126 articles, 120 studies were excluded as including case reports, reviews, nonEnglish articles, and articles that did not match inclusion criteria. This left a total of just 6 studies. Meta-analyses were performed on outcomes from 5 studies that met inclusion criteria [Figure 1]. Three studies evaluated the loss of rotation rates. Three studies reported fracture union time. Four studies listed complications. One published Cochrane study protocol failed to meet the authors’ study inclusion criteria. There were 5 retrospective level-III studies with control groups17,20,21,22,23,24 and one prospective randomized control trial (RCT) [Table 1].18
Figure 1.
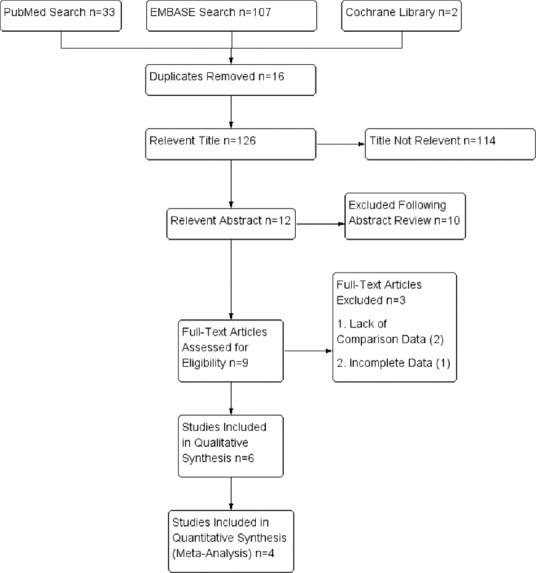
Eligibility selection; process flowchart
Table 1.
Characteristics of the included studies
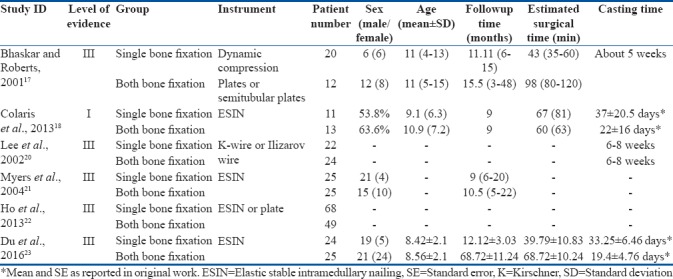
Study characteristics
The RCT18 was a multi-center trial (four Dutch medical centers) in which pediatric patients with diaphyseal forearm fractures of the radius and ulna were randomized to either single bone fixation or both bone fixation. Primary outcome measures were a range of motion, fracture healing time, and complications. In total, 24 fractures were randomized, which was the number determined by a prior power analysis designed to give an 80% chance of detecting a 15° limitation of forearm rotation in the primary outcome measure between the two groups [Table 1].
The 5 retrospective studies17,19,20,21,22,23 accounted for 294 (92.5%) of published cases available for analysis. There was substantial heterogeneity between the retrospective studies in terms of populations studied and interventions used. One study included proximal, shaft and distal forearm fractures as well as Monteggia fractures (the data on Monteggia fractures was excluded from the study). The remaining four studies dealt exclusively with pediatric patients presenting diaphyseal fractures. Each study reported on a range of internal techniques using multiple devices, including plates (3.5-mm dynamic compression plates, Stratec Medical, Hertfordshire, UK), wires (Kirschner wire or Ilizarov wires), stainless steel or titanium elastic stable intramedullary nails (C-nail, McKinnon Medical, Doddington, UK). Some patients treated with open reduction and internal fixation also received iliac crest bone grafting or artificial bone substitute [Table 1].
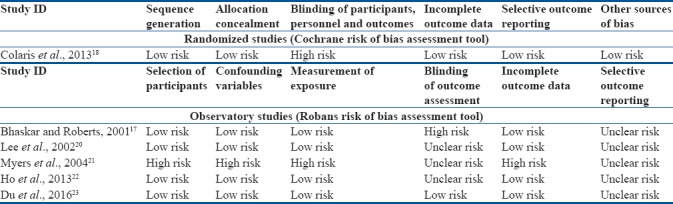
Study quality
The RCT18 was assessed as being at low risk of bias across most domains, although there was no blinding of patients or personnel and the protocol was not published before recruitment commenced [Tables 2 and 3]. There were protocol-to-publication differences, but intention-to-treat analysis and per-protocol analysis were used. The orthopedic surgeon examined all children after the initial trauma, the radiographs were measured without masking, and patients and parents were not blinded. The study was judged at high risk due to the failure of blinding participants, personnel and outcomes.
Table 2.
Outcomes of the included studies
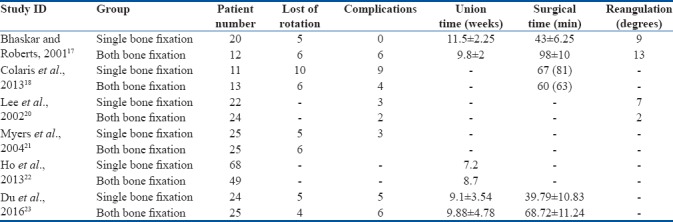
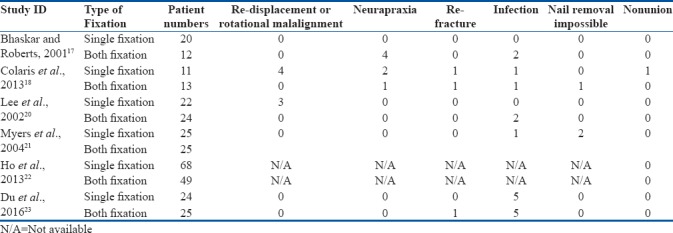
Table 3.
Complications of included studies
The risk of bias assessment using the RoBANS tool23 on the 6 retrospective studies found 4 studies to be at low risk of selection bias17,20,22,23,25,26 and one study to be at high risk as patients with radial neck or Monteggia/Galeazzi variants were also included.16 Only one study23 stated that patients attending their last followup visit were assessed by a clinical researcher not involved in their treatment. Another study clearly showed that the doctor who performed the surgeries was also collecting the data, putting this study at high risk of failure for blinding the outcome assessment, which also relied on subjective assessment by a single unblinded assessor.17 The other four studies did not explicitly report blinding of the outcome assessors and were found to be at unclear risk of detection bias. Similarly, the risk of reporting bias (selective outcome reporting) was unclear for all of the retrospective studies. One study was at high risk of attrition bias (incomplete outcome data) as a case was lost to followup (1/25).21 The rest were judged to be at low risk of attrition bias. The majority of studies included addressed known confounders by reporting the patient characteristics of each group and were all judged at low risk of confounding factors. As stated earlier, one study specifically included patients with both fractures and dislocations,20 and is therefore at high risk of confounding variables. The retrospective nature of these studies means additional confounders (either unreported or unidentified) are likely to exist, so conclusions from all five retrospective studies should be treated with caution [Table 4].
Table 4.
Risk of bias assessment
Healing time at cast removal
Four studies reported healing time at cast removal, but two studies reported this factor for their series as a whole, without distinguishing between the two treatment groups. One study only presented data with a median and IQR, making it difficult to pool its results findings with the remaining study.18 However, in one single bone fixation group, cast immobilization was longer (mean days in cast ± SD 33.25 ± 6.46 vs. 19.4 ± 4.761, median days in cast 37.0 [IQR 20.5] vs. 22.0 [IQR 16.0] days).
Radiographic outcome
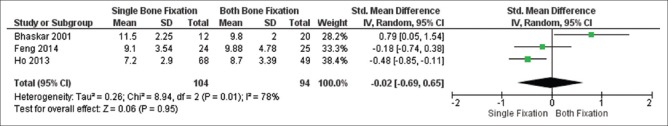
Only three studies reported time to radiographic union.17,22,23 One study showed longer union time for single bone fixation than both bone fixation,17 yet two other studies reached the opposite conclusion.22,23 Pooling the results of these three studies suggests that bone healing time is not statistically different between single bone and both bone fixation (mean difference − 0.02, 95% CI − 0.69–0.65, P = 0.95) [Figure 2].
Figure 2.
Bone healing time after single bone fixation and both bone fixation
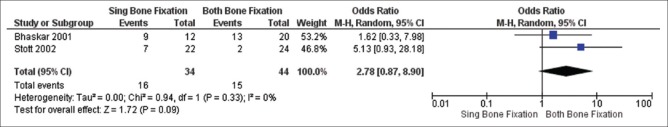
Two studies (78 fractures) assessed angular deformity,17,20 and both considered radial or ulnar angulation >10° as unacceptable. The single bone fixation patients exhibited a trend toward higher angulation which might have reached significance with a greater sample size (OR 2.78, 95% CI 0.87–8.90, P = 0.09) [Figure 3].
Figure 3.
Angular deformity after single bone fixation and both bone fixation
Function outcomes
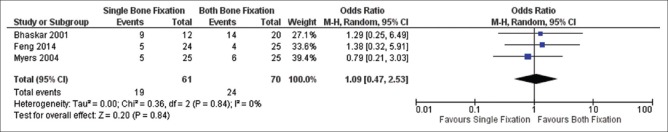
Five studies reported functional outcomes,17,18,20,21,23 although one reported a loss of rotation for the patient group as a whole, without distinguishing between the two treatment groups.20 Although one study18 found that the single bone fixation group had a statistically lower rotation of the forearm, this finding did not hold after pooling the results (OR 1.52, 95% CI 0.60–3.82, P = 0.38) [Figure 4]. Followup time across all included studies also varied hugely, ranging from 9 to 68.7 months.
Figure 4.
Loss of rotation after single bone fixation and both bone fixation
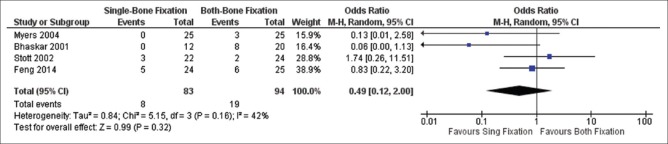
Complications
Complications described in the studies included as follows: re-displacement or rotational malalignment of the fractures, neurapraxias (transient and permanent), re-fracturing, excoriations of the skin, infections (superficial and deep), unremovable nails, and nonunions. All 6 studies consistently showed that both bone fixation had a higher infection rate.17,18,19,20,21,22,23,24 Only the RCT study18 reported that re-displacement rate was significantly higher in the single bone fixation group (36.6% vs 0), but regardless of whether this study was included, our metaanalysis found that incidence of complications as a whole was not different between the two method groups (OR 0.85, 95% CI 0.17–4.16, P = 0.84) [Figure 5]. However, due to the relatively low number of heterogeneous complications identified (38 out of 318 patients; 11.9%), it was not possible to discuss them separately [Tables 2 and 3].
Figure 5.
Complications after single bone fixation and both bone fixation
Discussion
A few studies have directly compared single bone fixation with both bone fixation for the treatment of pediatric both bone forearm fractures. This systematic review and meta-analysis found 6 such studies, most of which were poor quality retrospective case series except one RCT with detection bias and outcome assessment problems. There was substantial heterogeneity both in methods of intervention and reported outcomes. In addition, the retrospective studies, which accounted for the majority of cases available for analysis (88.1%), were at high risk of bias caused by confounding variables. Studies included in this systematic review suggest that single bone fixation might be a suitable treatment alternative for both bone forearm fractures in children. Compared with the both bone procedure, single bone fixation reduced surgical insult, operative times, and fluoroscopy radiation exposures, all of which equate to potential cost savings. Although it is reported that single bone fixation for treating both bone forearm fractures in children might have a higher risk of re-displacement, it is unclear whether this ultimately affects the radiographic and functional outcome.18
Pooled data from these studies suggest that patients managed with single bone fixation are at greater risk of re-displacement. Other complications had comparable rates between the two groups. These 6 included studies failed to show other statistically significant differences across a range of outcomes between single bone and both bone fixation. There is further uncertainty surrounding the complication profile of the two procedures. The proportion of patients with ulna/radius angular deformity and loss of rotation appeared to favor both bone fixation, but the advantage was not statistically significant.
Among the 6 included studies, one based on physical examination and X-ray gave the definition of “stability” after reduction. However, Tillotson and Glouchester24 reviewed 53 cases of pediatric diaphyseal forearm fractures and concluded that no single radiological criterion is predictive of fracture stability.24 The technique of reduction relies on the presence of an intact periosteum on the opposite cortex and uses it as a hinge. However, a surgeon cannot judge the periosteum and the interosseous membrane status using X-ray. Other methods like ultrasound might be useful to determine whether the restored fracture is stable. Authors of work included in the present analysis recommended casting if just one bone is to be fixed.
Angulation in the plane of joint movement is most likely to improve with growth and remodeling. However, rotational deformity and loss of normal interosseous space cannot be expected to improve with growth and remodeling, even in very young patients.25 We cannot firmly conclude whether both bone fixation helps to improve alignment and maintain the interosseous membrane, as the sample sizes of the included studies are too small.
The main limitation of this metaanalysis is that only a few studies compared single bone fixation and both bone fixation in the treatment of pediatric forearm fractures. Another important limitation of all these studies is that followup duration was relatively short. Loss of rotation is an important long term complication of forearm fractures, but small numbers of reangulation cases, short followup, and inconsistent reporting make it difficult to rely on the reported rates of bone reangulation and need for second surgery using these studies. Similarly, review of followup radiographs for evidence of bone healing relied on the subjective interpretation of nonblinded assessors. Although there are few short term functional differences between children undergoing single bone fixation or both bone fixation, the long term impact on forearm rotation remains unknown.
The data available from this systematic review also fails to clarify which bone should be fixed if using a single bone fixation method, and which bone should be fixed first if using the both bone fixation method. Restoration of the radial bow is thought to play an important role in preserving forearm rotations,26 whereas intramedullary single bone fixation of the ulna is associated with high rates of re-displacement of the associated radial fracture.16 Although the study by Dietz et al.16 and the study by Schemitsch and Richards26 could not be included in the metaanalysis due to incomplete data, single bone fixation of the radius appears to be the preferable option when fixing only one bone.16,26 However, studies comparing single bone fixation of the radius against single bone fixation of the ulna would be greatly informative.
Assessing the stability of the unfixed bone during the operation may be as important as the fixation method or choice of bone. We believe that the second bone can be left unfixed only if the fixation of the first bone achieves good reduction and stability.
Conclusions
Single bone fixation is an effective procedure that appears to have as good results as both bone fixation for treating unstable forearm both bone fractures in children. Based on metaanalysis, there appears to be no significant difference in loss of rotation, union time, or complications between single bone and both bone fixation. On the other hand, patients treated by single bone fixation exhibited a trend toward re-angulation. However, the small study populations and poor quality of the evidence currently available mean there is a pressing need for high quality RCTs to evaluate the treatment protocol for pediatric both bone fracture. The protocol has to be more specific with respect to stratification of the bone age of patients, and has to include a very reproducible definition of “stability.” Pediatric orthopedics needs to better define the bone age specific ranges for reliable remodeling of an array of combinations of fracture angulation and location in the forearm (i.e., size and metadiaphyseal, diaphyseal, or metaphyseal location). These parameters affect the long term consequences of residual angulation for patients undergoing nonoperative treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19:344–50. [PubMed] [Google Scholar]
- 2.Jones K, Weiner DS. The management of forearm fractures in children: A plea for conservatism. J Pediatr Orthop. 1999;19:811–5. [PubMed] [Google Scholar]
- 3.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop. 2005;25:507–12. doi: 10.1097/01.bpo.0000158005.53671.c4. [DOI] [PubMed] [Google Scholar]
- 4.Franklin CC, Robinson J, Noonan K, Flynn JM. Evidence-based medicine: Management of pediatric forearm fractures. J Pediatr Orthop. 2012;32(Suppl 2):S131–4. doi: 10.1097/BPO.0b013e318259543b. [DOI] [PubMed] [Google Scholar]
- 5.Ali AM, Abdelaziz M, El-Lakanney MR. Intramedullary nailing for diaphyseal forearm fractures in children after failed conservative treatment. J Orthop Surg (Hong Kong) 2010;18:328–31. doi: 10.1177/230949901001800314. [DOI] [PubMed] [Google Scholar]
- 6.Vopat ML, Kane PM, Christino MA, Truntzer J, McClure P, Katarincic J, et al. Treatment of diaphyseal forearm fractures in children. Orthop Rev (Pavia) 2014;6:5325. doi: 10.4081/or.2014.5325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson GH, Wilber JH, Marcus RE. Internal fixation of fractures in children and adolescents. A comparative analysis. Clin Orthop Relat Res. 1984;188:10–20. [PubMed] [Google Scholar]
- 8.Amit Y, Salai M, Chechik A, Blankstein A, Horoszowski H. Closing intramedullary nailing for the treatment of diaphyseal forearm fractures in adolescence: A preliminary report. J Pediatr Orthop. 1985;5:143–6. [PubMed] [Google Scholar]
- 9.Yung SH, Lam CY, Choi KY, Ng KW, Maffulli N, Cheng JC, et al. Percutaneous intramedullary Kirschner wiring for displaced diaphyseal forearm fractures in children. J Bone Joint Surg Br. 1998;80:91–4. doi: 10.1302/0301-620x.80b1.8110. [DOI] [PubMed] [Google Scholar]
- 10.Schranz PJ, Gultekin C, Colton CL. External fixation of fractures in children. Injury. 1992;23:80–2. doi: 10.1016/0020-1383(92)90036-r. [DOI] [PubMed] [Google Scholar]
- 11.Voto SJ, Weiner DS, Leighley B. Use of pins and plaster in the treatment of unstable pediatric forearm fractures. J Pediatr Orthop. 1990;10:85–9. [PubMed] [Google Scholar]
- 12.Flynn JM, Waters PM. Single-bone fixation of both-bone forearm fractures. J Pediatr Orthop. 1996;16:655–9. doi: 10.1097/00004694-199609000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Kirkos JM, Beslikas T, Kapras EA, Papavasiliou VA. Surgical treatment of unstable diaphyseal both-bone forearm fractures in children with single fixation of the radius. Injury. 2000;31:591–6. doi: 10.1016/s0020-1383(00)00057-7. [DOI] [PubMed] [Google Scholar]
- 14.Houshian S, Bajaj SK. Forearm fractures in children. Single bone fixation with elastic stable intramedullary nailing in 20 cases. Injury. 2005;36:1421–6. doi: 10.1016/j.injury.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Bader M, Sanz L, Waseem M. Forearm fractures in children: Single bone fixation with elastic stable intramedullary nailing in 20 cases. Injury. 2006;37:923–4. doi: 10.1016/j.injury.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Dietz JF, Bae DS, Reiff E, Zurakowski D, Waters PM. Single bone intramedullary fixation of the ulna in pediatric both bone forearm fractures: Analysis of short-term clinical and radiographic results. J Pediatr Orthop. 2010;30:420–4. doi: 10.1097/BPO.0b013e3181e00c44. [DOI] [PubMed] [Google Scholar]
- 17.Bhaskar AR, Roberts JA. Treatment of unstable fractures of the forearm in children. Is plating of a single bone adequate? J Bone Joint Surg Br. 2001;83:253–8. doi: 10.1302/0301-620x.83b2.10955. [DOI] [PubMed] [Google Scholar]
- 18.Colaris J, Reijman M, Allema JH, Kraan G, van Winterswijk P, de Vries M, et al. Single-bone intramedullary fixation of unstable both-bone diaphyseal forearm fractures in children leads to increased re-displacement: A multicentre randomised controlled trial. Arch Orthop Trauma Surg. 2013;133:1079–87. doi: 10.1007/s00402-013-1763-0. [DOI] [PubMed] [Google Scholar]
- 19.Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408–14. doi: 10.1016/j.jclinepi.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Lee S, Nicol RO, Stott NS. Intramedullary fixation for pediatric unstable forearm fractures. Clin Orthop Relat Res. 2002;402:245–50. doi: 10.1097/00003086-200209000-00024. [DOI] [PubMed] [Google Scholar]
- 21.Myers GJ, Gibbons PJ, Glithero PR. Nancy nailing of diaphyseal forearm fractures. Single bone fixation for fractures of both bones. J Bone Joint Surg Br. 2004;86:581–4. [PubMed] [Google Scholar]
- 22.Ho CA, Jarvis DL, Phelps JR, Wilson PL. Delayed union in internal fixation of pediatric both-bone forearm fractures. J Pediatr Orthop B. 2013;22:383–7. doi: 10.1097/BPB.0b013e328361c7ea. [DOI] [PubMed] [Google Scholar]
- 23.Du SH, Feng YZ, Huang YX, Guo XS, Xia DD. Comparison of pediatric forearm fracture fixation between single- and double-elastic stable intramedullary nailing. Am J Ther. 2016;23:e730–6. doi: 10.1097/MJT.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 24.Tillotson L, Glouchester R. Radiographic predictors of instability in pediatric diaphyseal forearm fractures. Inj Extra. 2011;42:95–169. [Google Scholar]
- 25.Bowman EN, Mehlman CT, Lindsell CJ, Tamai J. Nonoperative treatment of both-bone forearm shaft fractures in children: Predictors of early radiographic failure. J Pediatr Orthop. 2011;31:23–32. doi: 10.1097/BPO.0b013e318203205b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74:1068–78. [PubMed] [Google Scholar]