Abstract
The clinical presentation and diagnostic workup in pediatric cervical spine injuries (CSI) are different from adults owing to the unique anatomy and relative immaturity. The current article reviews the existing literature regarding the uniqueness of these injuries and discusses the current guidelines of radiological evaluation. A PubMed search was conducted using keywords “paediatric cervical spine injuries” or “paediatric cervical spine trauma.” Six hundred and ninety two articles were available in total. Three hundred and forty three articles were considered for the review after eliminating unrelated and duplicate articles. Further screening was performed and 67 articles (original articles and review articles only) related to pediatric CSI were finally included. All articles were reviewed for details regarding epidemiology, injury patterns, anatomic considerations, clinical, and radiological evaluation protocols. CSIs are the most common level (60%–80%) for pediatric Spinal Injuries (SI). Children suffer from atlantoaxial injuries 2.5 times more often than adults. Children's unique anatomical features (large head size and highly flexible spine) predispose them to such a peculiar presentation. The role of National Emergency X-Ray Utilization Study, United State (NEXUS) and Canadian Cervical Spine Rule criteria in excluding pediatric cervical injury is questionable but cannot be ruled out completely. The minimum radiological examination includes 2- or 3-view cervical X-rays (anteroposterior, lateral ± open-mouth odontoid views). Additional radiological evaluations, including computerized tomography (CT) and magnetic resonance imaging (MRI) are obtained in situations of abnormal physical examination, abnormal X-rays, inability to obtain adequate X-rays, or to assess cord/soft-tissue status. The clinical criteria for cervical spine injury clearance can generally be applied to children older than 2 years of age. Nevertheless, adequate caution should be exercised before applying these rules in younger children. Initial radiographic investigation should be always adequate plain radiographs of cervical spine. CT and MRI scans should only be performed in an appropriate group of pediatric patients.
Keywords: Anatomical features, Clinical Decision Rules, pediatric cervical spine injuries, spinal cord injury without radiological anomaly
MeSH terms: Pediatrics, cervical vertebrae, spinal cord injuries, anatomy
Introduction
Pediatric spinal trauma is uncommon and accounts for only 1%–10% of all reported spinal injuries. Nevertheless, these injuries contribute to a significant proportion of morbidity and mortality in them.1 The overall incidence of spinal injuries in children in the United States has been reported to be 7.41/100,000.2 It has also been observed that 1300 new cases of pediatric spinal cord injuries (SCI) occur every year.2 Data involving Indian population reveal an incidence of pediatric spinal trauma among overall spinal injuries around 1%–11%.3 The incidence of spinal cord injury without radiological anomaly (SCIWORA) in Indian population is also reported to be approximately 4.5%–35%.3
The cervical spine injuries (CSIs) in children present differently when compared to adults.4 The current article comprehensively reviews the existing literature on pediatric CSIs and discusses the uniqueness of presentation and current guidelines of radiological evaluation.
Materials and Methods
A PubMed search was conducted using the keywords “paediatric cervical spine injuries,” “paediatric cervical spine trauma,” “pediatric sub-axial spine injuries”, “cervical spine injury child,” “atlantoaxial injury in children,” “fractures of atlas,” or “fractures of dens.” A total of 692 articles were available [Flowchart 1]. Three hundred and forty three articles were considered for the review after eliminating unrelated (non-pediatric injuries, non-cervical spine injuries, non-trauma cases, pediatric infections, tumors and other pathologies) and duplicate articles. Only original articles involving human case series and review articles were included. Case reports, letters to the editor, articles published in languages other than English and non-relevant materials (not discussing the diagnostic evaluations of pediatric CSIs; or articles discussing issues on cervical SI not revlevant to the topics of discussion included in the current review) were excluded from the study. A total of 67 articles were finally included for the review of literature of pediatric cervical spine trauma. All the articles were reviewed for the epidemiology, injury patterns, special anatomical considerations, intricacies of clinical and radiological evaluation.
Flowchart 1.
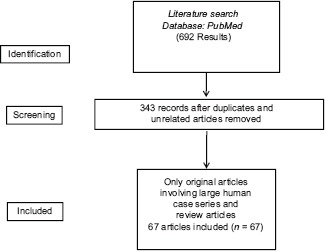
Flowchart depicting study methodology
Results
There was a significantly greater proportion of available articles on upper cervical injuries (51/67 studies) when compared with the subaxial (16/67 studies) cervical trauma. Among the articles on upper CSI, seven articles were focused on atlas or Jefferson's (C1 burst) injuries, 15 were focused on axial or odontoid injuries, 19 were on traumatic atlantoaxial (AA) rotatory injuries or other C1/C2 injuries and 10 articles on general upper cervical injuries, including occipitoatlantal injuries. Seven of these articles were review articles.
Discussion
Epidemiology
Cervical spine is the most common level (60%–80%) for pediatric spinal injury (PSI).2 In fact, a large majority of fatal spinal injuries in children involve cervical spine.1 Based on the existing literature on pediatric cervical spine trauma, 25%-44% of injuries have been reported to involve ligamentous disruptions.5,6,7,8 Henry et al.8 reported 78% incidence of ligamentous injuries following inflicted trauma, as against 46% incidence in children with accidental trauma. Majority of the pediatric cervical spine injuries (CSIs) occur between the skull and C4 vertebra; and around 10.8% to 38.7% of these injuries involve C1 and C2 vertebrae.1,9,10,11 Children suffer from atlanto-axial injuries 2.5 times more often than adults.12 As per available western data, the most common variable (in 67.7%) associated with pediatric CSIs includes noncompliance with seat belt.12 Patterns of CSIs among various pediatric age groups have been described elaborately.13,14 Literature reports that around 11%-61.9% of CSIs occur secondary to motor vehicle accidents (MVA).6,7,9,14,15 Birth-associated injuries are uniquely associated with infants.16,17 Aggressive delivery techniques and breech presentations are significantly associated with CSIs.18 In toddlers of walking age, falls from ground level constitute a significant mode of injury.6,9 In older, school-going children, sports-related injuries are common (overall incidence reportedly varying between 11.3% and 49%).6,15,18,19,20 Large case series involving children with inflicted injuries (or child abuse) report around 5.6% -13% incidence of CSIs in such scenarios.4,7,21,22
Embryological consideration
The ossification centers in a growing spine are separated by synchondrosis. A knowledge of this anatomy is of utmost importance, as they can be erroneously identified as fracture.23,24 Atlas vertebra develops from three ossification centers: one for anterior arch and two for lateral masses. These ossification centers appear at 1 year and fuse by 7 years. Axis develops an ossification center for centrum, two for posterior arches, and two for odontoid process. The two ossification centers for dens fuse with each other before birth and further unite with the centrum at 5–7 years of age. This persistent synchondrosis can be mistaken for a fracture. The main differentiating feature for persistent synchondrosis is its location below the level of C1–C2 facet joint.23 Ossiculum terminale or ossification center for the tip of odontoid process appears at 7 years and fuses to the rest of dens by 12 years of age. All other cervical vertebrae develop from one ossification center for vertebral body, two for lateral masses, and one for posterior arch.24 These ossification centers unite in midline between 2 and 4 years while neurocentral synchondroses fuse at 3–6 years. The immature spines therefore potentially fail at physes, more often than osseous or ligamentous or intradiscal disruptions.23,24
Pathophysiology and anatomical considerations
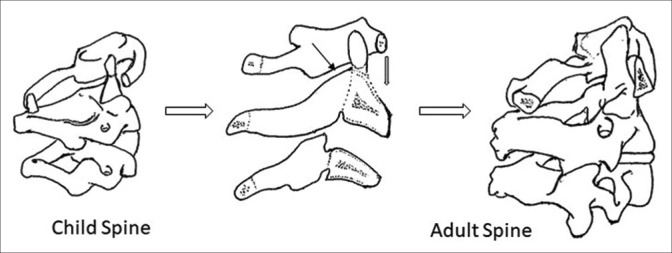
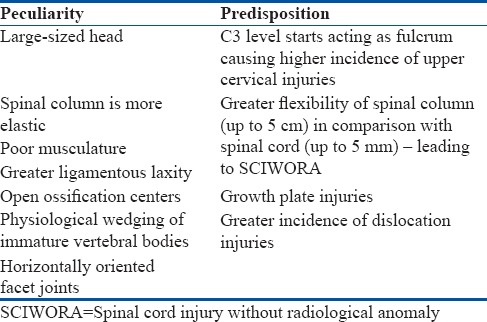
Children's unique anatomic features predispose them to the risk of SCIs and peculiar presentation.1 Large head size and highly flexible spine are fundamental attributes in this context. Pediatric cervical spine, owing to increased flexibility, has greater tolerability to motion. Such enhanced mobility also predisposes to the kind of injuries they sustain. Poor musculature, greater ligamentous laxity, open ossification centers, physiological wedging of immature vertebral bodies and horizontally oriented facet joints [Figure 1] enhance this flexibility and put cervical spine at a greater risk for dislocation injury or growth plate injuries.25,26 Shear forces during rapid deceleration and hyperflexion extension mechanisms can commonly inflict injuries at synchondroses between dens and C2 body [Figure 2]. The spinal column is more elastic than spinal cord (vertebral column can tolerate up to 5 cm of distraction, in comparison to significant cord damage following a mere 5 mm distraction) leading to SCIWORA (spinal cord injury with intact spinal column).27
Figure 1.
Diagrammatic representation of lateral cervical spine radiograph showing a comparison between pediatric and adult cervical vertebral bodies. Open ossification centers, physiological wedging of immature vertebral bodies and horizontally oriented facet joints enhance flexibility of the spine and augment risk for dislocation injury or growth plate fractures
Figure 2.
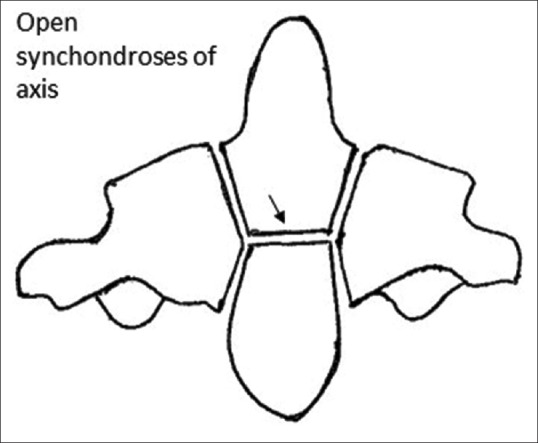
Diagrammatic representation of anteroposterior radiograph depicting open synchondrosis between dens and C2 body. This anatomical peculiarity should not be confused for an odontoid fracture
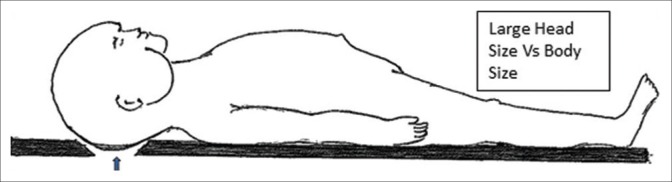
Pediatric spines are also at risk for “fulcrum effect.”28 This phenomenon is secondary to a large-sized head overlying a totally flexible cervical spine. In very young children, this fixes the fulcrum of cervical motion at C2/C3 leading to high levels of cervical injury. Nevertheless, as the child's spine matures and grows accompanied by a relative reduction in head size, the fulcrum gradually shifts caudally leading to a more distal location of fractures [Figure 3 and Table 1].28
Figure 3.
Diagrammatic representation of the relative size of head of a child in comparison with body size. This peculiarity of pediatric spine fixes the fulcrum of cervical motion at C2/C3 in younger patients and predispose them to high levels of cervical injury
Table 1.
Peculiarities of pediatric cervical spine and predisposition to different injury pattern
When to suspect cervical spine injuries in children?
The suspicion regarding CSI should be based on history (nature of trauma, mode of injury and symptoms, even if transient).29,30,31 Any child with associated high-risk injuries (head injuries or multisystem trauma) or conditions predisposing to SI (syndromes with ligamentous laxity and cervical instability or rheumatoid disorders), need to be considered to have CSI until proven otherwise.32
In children <3 years of age, injury should be suspected on the basis of injury mechanism and imaging should be obtained in all suspected patients, irrespective of time since injury. In older children, in addition to the above-mentioned, postinjury symptoms should be given equal importance while evaluation. Transient symptoms do not warrant imaging in older children presenting after 4 days of injury provided the child is asymptomatic at the time of presentation. However, in patients with persistent symptoms, imaging needs to be performed immediately, irrespective of the day of presentation.33
The classic triad of symptoms includes pain, muscle spasm, and restricted neck movements, which may be accompanied by varying degrees of neurological symptoms.33,34 A significant proportion of pediatric CSI patients may be asymptomatic. In a study by Browne et al. (2017)15 only 16%-24% of children with CSI were classified by ED or EMS providers as under high suspicion category (>50% risk) for CSI based on symptomatology and initial presentation. In a retrospective review of 72 patients by Baker et al., all asymptomatic CSI patients had both high-risk mechanism and distracting mode of injuries.30 Hyperextension injuries can induce central cord syndrome, whose only presentation can be “burning hands.”35 In addition, tell-tale signs such as chin trauma, fractures of posterior teeth, and mandibular condyles are to be vigilantly picked up and given importance so that these kids are diagnosed and treated in timely manner.34
Physical examination
Examination of vitals, neck, and neurological examination are major components of physical examination. Collar may be removed for cervical spine examination; nevertheless, it should immediately be replaced if any evidence of CSI is identified.36 In situations of minor trauma, with normal neck examination (palpation for tenderness and active range of motion [ROM]) and neurological status, children can be clinically cleared.37 Positive neck examination (restricted ROM or tenderness) or evidence of neurological deficit necessitates reimmobilization and detailed imaging.29
Clinical Decision Rules
In 1987, a retrospective review involving 206 children (<16 years; 28% - 0–3 years, 42% - 4–12 years and 30% - 13–16 years) observed that the presence of one among eight variables (neck pain, neck tenderness, decreased ROM, history of neck trauma, abnormal reflexes, abnormal motor strength, sensory disturbances, or abnormal mentation) could identify 58 of 59 CSI patients, with 98% sensitivity and 54%, specificity.33
National Emergency X-Ray Utilization Study (NEXUS), United States, July 2000, and Canadian Cervical Spine Rule (CCR), Canada, October 2001 criteria were then developed to identify patients who require C-spine imaging among trauma victims. NEXUS criteria (sensitivity of 99% in ruling out CSI in adults) included midline cervical tenderness, focal neurological deficit, alertness, nonintoxicated state, and absence of clinically apparent, painful, distracting injuries.38 Low-risk CCR included simple, rear-end MVA, sitting in emergency department, ambulatory at any time, delayed onset of neck pain, and no midline tenderness.39 High-risk criteria included age more than 65 years, dangerous injury mechanism, and limb paresthesia.39 These criteria have been proven to decrease the need for imaging in adults, without risk of missing CSIs. In the original NEXUS trial, only 2.5% of studied patients and only 1.3% of patients with CSI were eight years or younger. All patients included in the CCR study were older than 16 years. Therefore, these studies could not give any conclusion on the usefulness of these criteria in children.38,39,40,41,42
Another large, multicentric, prospective trial evaluated NEXUS criteria in 3065 pediatric patients.40 All 30 children, who had CSI, had at least one-risk factor; while none without any risk factor had CSI. Of these children with CSI, none was <2 years, only four were eight years or younger and 26 belonged to the age group between 9 and 17 years. The two most common risk factors in children (both CSI and non-CSI groups) were cervical tenderness and distracting injuries. The mean numbers of positive findings in CSI and non-CSI pediatric patients were 1.8 and 1.4, respectively. Decision rule based on NEXUS criteria showed a sensitivity and negative predictive value of 100% in this pediatric population (predominantly involving 9–17 year olds). The authors “cautiously endorsed” the application of NEXUS criteria in children from 0 to 9 years of age.
In a retrospective, case-matched cohort study, Ehrlich et al. (2009)42 used both NEXUS and CCR in children younger than 10 years and observed that they had unacceptable sensitivities (43% for NEXUS and 86% for CCR) for diagnosing CSIs. Pediatric population has been classified broadly into three categories in most of these studies: 0–3 years (noncommunicative group), 3–8 years (immature spine), and 9–17 (older pediatric population).40 A multicenter study (2006)37 too concluded a simple algorithm including clinical examination and plain radiographs can reduce the need for neurosurgical consultation in clearing cervical spine by 60% in children >3 years of age. A multicenter retrospective study (2009)41 involving 12,537 children below 3 years, observed that one-third of their patients can be cleared of CSIs purely on the basis of clinical examination. All the 83 injuries identified on imaging could be suspected on initial evaluation itself. Four independent predictors (PEDSPINE rule) for CSIs were identified: Glasgow coma scale (GCS) <14, eye-opening score on GCS of 1, age between 24 and 36 months and motor vehicular accident. A score <2 demonstrated a negative predictive value of 99.93% in ruling out CSI, and no CSI was missed in this study.
A recent article by Rozzelle et al.43 recommended that clinical decision on clearing cervical spine (without additional imaging) can be made in children over than 3 years of age who have experienced trauma and are alert, have no neurological deficit, have no midline cervical tenderness, have no painful distracting injuries, do not have unexplained hypotension, and are not intoxicated. It was also recommended that cervical spine imaging is not required in children <3 years of age, who have experienced trauma and have a GCS more than 13, have no neurological deficit, have no midline cervical tenderness, have no painful distracting injuries, do not have unexplained hypotension, are not intoxicated, and do not have MVA, fall from a height of more than 10 feet or nonaccidental trauma as a possible mechanism of injury.
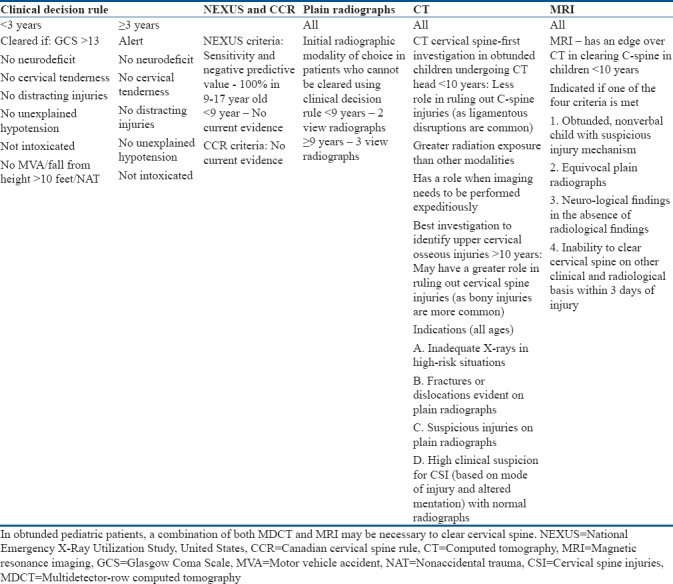
Radiological evaluation: How to rule out cervical spine injury?
The radiological examination usually includes 3-view cervical X-rays (anteroposterior, lateral, and open-mouth odontoid views).37 Additional radiological evaluations are computerized tomography (CT) and magnetic resonance imaging (MRI), need for which includes abnormal physical examination, abnormal X-rays, inability to obtain adequate X-rays, or to assess cord/soft tissue status.8
Plain radiographs
Anderson et al.44 in 2006 described a trauma evaluation algorithm involving radiological and clinical evaluation in children older than 3 years. This protocol recommended cervical spine X-rays as the initial line of investigation (even before clinical evaluation), in accordance with the guidelines outlined by the American College of Surgeons in patients with “significant trauma”. In children older than 5 years, he recommended three-view cervical X-rays (anteroposterior, lateral, and open-mouth odontoid views); while in children younger than 5 years, two-view (anteroposterior and lateral views) radiographs are advised. In children older than 3 years, with normal cervical spine X-rays and meets NEXUS clinical criteria, cervical spine can be cleared of any significant injury. In 2010,37 he recommended a similar protocol in children younger than 3 years of age. Anteroposterior and lateral radiographs are the initial line of management, while CT scans are advised if the radiographs indicate a suspicion of underlying cervical spine injury or are inadequate. In a child with normal radiographs, along with a history suggestive of high-energy trauma or abnormal neurological examination or intubated/abnormal mental status, MRI scan of cervical spine (short tau inversion recovery [STIR] or T2 suppression sequence) is recommended.45 In patients with equivocal findings on MRI scan, dynamic flexion/extension radiographs were recommended. Using this protocol, more than 80% of children (0–3 years of age) were cleared of CSI, and no C-spine injury was missed.45
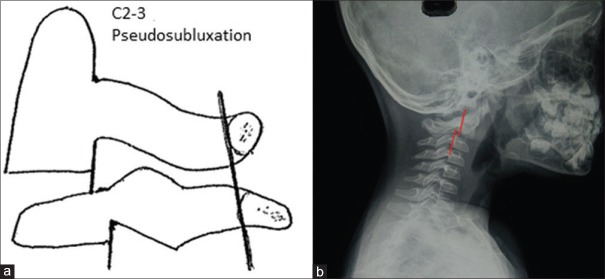
Obtaining an adequate radiograph (to include C7-T1 disc) is crucial and isolated lateral cervical X-ray can potentially diagnose 80% of CSIs.46,47 Interpretation of pediatric CSIs can still be difficult until 15 years of age. Normal anatomical variations in children [absent lordosis, nonossified posterior spinal elements, ligament laxity, and C2–C3 pseudo-subluxation [Figure 4] need to be differentiated from pathological findings.48,49 Disruption of any of the four curvilinear alignment lines [Figure 5] (anterior vertebral body line, posterior vertebral body line, spinolaminar line, and tips of spinous process) can be an indicator for possible CSI.50 In a retrospective study on atlantooccipital injury, interspinous ratio (C1–2:C2–C3) of more than 2.5 had a sensitivity of 87% and specificity of 100% for tectorial membrane disruption.51 Prevertebral (<1/3 AP diameter of vertebral body at C3/C4 level in comparison with 7 mm in adults) and predental spaces (<4–5 mm in children in comparison with 3 mm in adults) are other crucial radiological markers.52 Open-mouth odontoid view can be obtained in children older than 9 years of age; while in younger, uncooperative children, Water's view through the foramen can depict odontoid and upper cervical morphology.53 Flexion extension views do not offer additional information; with added disadvantage of precipitating spinal cord injury.54,55 If performed, only active flexion and extension within limits of pain tolerance should be obtained. The only situation where the dynamic stress views can offer additional information is in the setting of persistent neck pain with normal cervical radiographs and CT scan.56 In the subacute setting, after the muscle spasm subsides, these dynamic stress views can unmask underlying ligamentous disruptions.57 Oblique cervical radiographs are not recommended.57 The normal critical measurements [Figure 6] of upper cervical spine in plain radiographs include basion-dens interval <12 mm [Figure 6a], basion-axial interval of 12 mm anterior and 4 mm posterior, Power's ratio <1 [Figure 6b], condylar gap <5 mm, C1–C2 interspinous interval <12 mm [Figure 6d], and predental interval <5 mm in ≤8 years and <3 mm in >8 years old.58 Rozzelle et al.43 recommended two-view radiographs (antero-posterior and lateral) or high-resolution CT scan (HRCT) in children younger than 9 years of age, while three-view radiographs (anteroposterior, lateral, and open-mouth) or HRCT scan were advocated for the radiological assessment of cervical spine injury in children older than 9 years.
Figure 4.
(a) Diagrammatic representation of lateral cervical spine radiograph showing C2–C3 pseudosubluxation (normal relationship of the upper cervical spine determined using Swischuk's Line). (b) Lateral cervical spine radiograph showing C2–C3 pseudosubluxation
Figure 5.
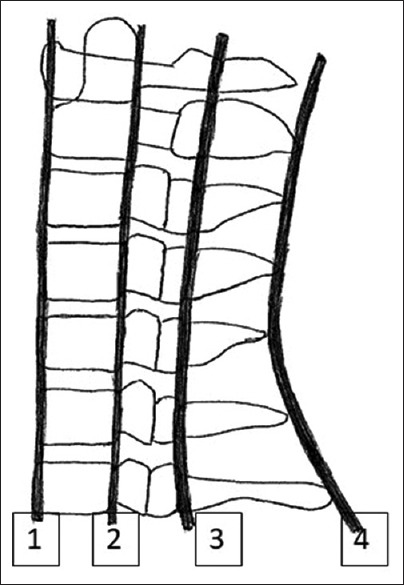
Diagrammatic representation of lateral cervical spine radiograph showing standard four curvilinear alignment lines: Anterior vertebral body line (1), posterior vertebral body line (2), spinolaminar line (3) and tips of spinous process (4). Any disruption of these lines should lead to suspicion of a possible fracture and need for further imaging
Figure 6.
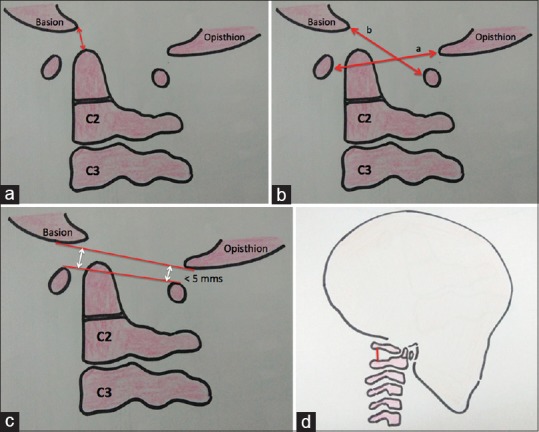
Diagrammatic representation of lateral cervical spine radiographs showing (a) Basion-dens interval. (b) Powers ratio: b/a. (c) Atlantooccipital joint not exceeding 5 mm. (d) C1–C2 interspinous distance
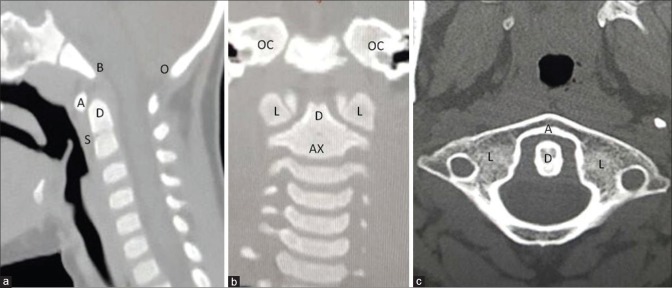
Computed tomography scan – cervical spine
CT scan should not be routinely performed for initial pediatric spine evaluation [Figure 7].59 In 2010, Silva et al.60 concluded that lateral radiographs alone had borderline sensitivity comparable to multidetector row CT (MDCT) in detecting pediatric CSI. Radiation exposure with CT is significantly greater than X-rays.61 Helical CT scan delivers 50% increased radiation dose in comparison with conventional radiographs.62,63 Jiminez et al.64 observed that radiation dose to thyroid from cervical spine CT was 90–200 fold greater than conventional X-rays and the mean risk for thyroid cancer was two times higher in children between 0 and 4 years of age. Estimated life time risk of malignancy in a 1-year old exposed to CT scan of cervical spine is 0.07–0.18.65
Figure 7.
Computerized tomography scan showing (a) mid-sagittal section, (b) coronal section (c) axial section. Showing specific points: A: Anterior arch of atlas, B: Basion, D: Dens, S: Synchondrosis, O: Opisthion, L: Lateral Mass of Atlas, AX: Vertebral body of atlas, OC: Occipital condyle
In pediatric population, where ligamentous injuries are more frequent, routine use of MDCT is not warranted.67,68 In the study by Anderson et al.,37 CT scan was necessary only in 14% of children to clear cervical spine. Schleehauf et al.69 (1989) concluded that CT alone should not be relied on to exclude ligamentous cervical injuries in pediatric patients. Hutchings et al.45 (2009) reviewed the role of CT in the evaluation of cervical spine in obtunded, major trauma pediatric patients. Although there is not strong evidence on this issue owing to small number of patients, it was recommended that the role of CT in clearing cervical spine may be less important in children <10 years, as a majority of lesions in this age group are ligamentous disruptions without fracture. MRI can play a greater role in excluding soft-tissue disruptions in these children. MDCT may be preferred over MRI in this age group when imaging needs to be performed expeditiously.4 In older children with a cervical spine injury, incidence of fracture is much higher than ligamentous injury (80% versus 20%), and CT scan has a greater role in ruling out C-spine injuries.
It can, however, be an adjunct to other modalities in certain special situations.70 CT cervical spine can be the first investigation in obtunded children, where it is performed along with CT head.67,68 Sun et al.71 recommended that the incorporation of CT cervical spine (till C3) in patients who underwent CT head, significantly reduced the overall radiation exposure by three-fold and potentially decreased the need for full CTs. Inadequate three-view X-rays in high-risk situations, fractures, or dislocations evident on plain radiographs, suspicious injuries on plain radiographs, and high clinical suspicion for CSI with normal radiographs are scenarios where CT can be valuable in evaluating the osseous integrity.72 Upper cervical spine fractures, which are typically noted in this age group, are best evaluated on MDCT. Rozzelle et al.43 recommended three-position CT with C1–C2 motion analysis to confirm the diagnosis of AA rotatory fixation in children. Garton et al.73 reported that in children younger than 8 years in whom higher cervical injuries were suspected, the combination of plain radiography and occiput-C3 CT showed a high sensitivity. In a study in pediatric patients with potential atlantooccipital dissociation, Pang et al.74 recommended that a specific protocol including sagittal and coronal reformatted CT images showed the highest diagnostic sensitivity and specificity among all radiographic methods. Normal critical measurements of upper cervical spine on MDCT include basion-dens interval <9.5 mm with ossification and <11.6 mm without ossification [Figure 6a], power's ratio <0.9 [Figure 6b], atlantodental interval <2.6 mm, atlantooccipital interval <2.5 mm, and AA interval <3.9 mm [Figure 6].75
Magnetic resonance imaging scan
MRI is the imaging of choice in patient with positive neurological signs and normal plain radiographs and/or CT scan [Figure 8].76 It is superior to CT scan in demonstrating morphology of spinal cord and soft tissue injuries.77 Imaging sequences of cervical spine must include a sagittal T1-weighted image, sagittal STIR, and axial T2-weighted gradient echo images. Axial T2-weighted image of C1–C2 level help in excluding injuries to transverse ligament and coronal STIR aid in evaluating capsular injuries and fluid accumulation within atlantooccipital and AA joints.4
Figure 8.
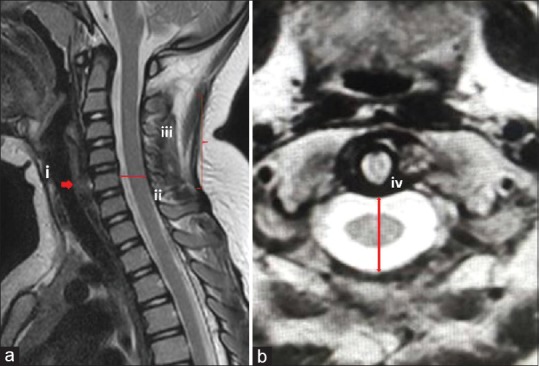
Magnetic resonance imaging showing (a) mid-sagittal T2W image (b) axial section. i: Prevertebral soft tissue, ii: Retro vertebral soft tissue, iii: Spinal cord morphology, iv: Space available for cord
Spinal cord injury without radiographic abnormality (SCIWORA) has been defined by Pang and Wilberger55 in 1982, as posttraumatic condition in children where neurological deficit is evident in the absence of obvious abnormality on plain radiographs, dynamic stress X-rays, and cervical CT scan.79 In 2004, Pang and Wilberger observed a mean incidence of SCIWORA of around 34.8%.55 Two specific categories were described in this study: delayed and recurrent types. The delayed presentation typically involved initial transient neurological symptoms, followed by delayed onset of symptoms (possibly from spinal cord ischemia).55,78,80 The other type is the recurrent SCIWORA, which is reported with an incidence of 17%. Since the inception of MRI scan, demonstrable injuries to spinal cord or other ligaments can be identified in SCIWORA.77 MRI has paved way for a better direct visualization of supporting soft tissue and ligamentous structures, cervical cord (including hemorrhage within cord), facetal capsular injuries, epidural hemorrhages, discal ruptures, occipital cervical ligamentous ruptures (as evidenced by hemorrhage along clivus), minor bony injuries (as evidenced by marrow edema), and injuries to synchondrosis.4 Nevertheless, the significance of certain soft-tissue injuries on MRI is not clear: contusions or edema in inter-spinous structures with intact anterior and middle spinal columns, or isolated disruption of nuchal ligaments.4 It has been demonstrated that there is little direct correlation between specific MRI abnormalities and intraoperative findings.81
According to Booth et al.,4 in children <5 years, MRI rather than MDCT should be considered, if advanced modalities are required. This was recommended because, in this younger population, dose of radiation exposure is a major concern. The higher incidence of ligamentous injury too, further raises the importance of MRI as a diagnostic modality. Flynn et al.77 described the need for obtaining MRI scan if one of the four criteria were met: (1) Obtunded, nonverbal child with suspicious injury mechanism (2) equivocal plain radiographs (3) neurological findings in the absence of radiological findings, and (4) inability to clear cervical spine on other clinical and radiological basis within 3 days of injury. Using these criteria, MRI altered diagnosis in 34% of patients.
Atlantoaxial rotatory subluxation
Fielding and Hawkins classified traumatic AARS into four types: type 1 – pure AA rotation with normal atlantodens interval (ADI); type 2 – AA rotation with ADI of 3–5 mm; type 3 – AA rotation with ADI more than 5 mm, indicating complete transverse ligament disruption; and type 4 – AA rotation with associated posterior atlantal dislocation.24,82 Axial and three-dimensional CT scans allow clear visualization of C1–C2 rotation, loss of congruence of facet joints and increased ADI, and therefore, can play a major role in the diagnosis of AARS.24 Such traumatic AARS needs to be differentiated from other nontraumatic causes for AARS. Nontraumatic AARS was initially described by Charles Bell in 1830 in a patient with syphilis; while Grisel described this syndrome in 1951 in a patient with pharyngitis.83,84 Parke et al. purported that hematogenous transport of septic exudates from pharynx to cervical spine through venous plexuses, leading to AA inflammatory reactions, transverse and alar ligament laxity; and facet capsule edema.85
C2–C3 pseudosubluxation
Scischuk observed C2/C3 pseudosubluxation as a normal common variant and defined the posterior cervical line as a reference to differentiate it from hangman's fracture.86,87 In another series involving 160 non-traumatic children, 9% presented with severe pseudosubluxation and 15% with moderate pseudosubluxation.50,88 Harrison et al.89 observed this phenomenon even in patients aged between 14 and 18 years. In a series involving pediatric patients presenting with polytrauma, 21.7% of kids presented with pseudo-subluxation. In such scenarios, it may be difficult to differentiate between true subluxation and pseudosubluxation. In physiological displacement, Swischuk line passes through or lie up to 1 mm anterior to the cortex of C2 posterior arch. If the cortex is within 1.5 mm posterior to Swischuk line, there is a suspicion for true injury, while a displacement of 2 mm or more indicates a true dislocation.50,90
Emergency department treatment options
Whenever a child with a suspected cervical spine injury is encountered, immediate immobilization in neutral position needs to be performed, until the injury is ruled out. Prompt consultation with a neurosurgeon also is necessary in situations of high suspicion for CSI.78 The scientific evidence behind spinal immobilization practice is still weak. A Cochrane collaboration systematic review in 2009 observed no association between the occurrence of neurological-deficit, death, or spinal instability and the application of immobilization devices.80,91 It is well-acknowledged that spinal immobilization is not entirely a benign practice.28 Immobilization has been associated with increased pain and decreased forced vital capacity.28 This is also compounded by the anatomical problem of a relatively large-sized head in young children, which according to Curran et al.91 up to 20% of children placed on spinal board had a cervical flexion of >10° [Figure 3].61 Herzenberg et al.92 recommended occipital recess or thoracic elevation to eliminate this iatrogenic flexion. Nypayer and Treloar93 determined that a thoracic elevation of 2.5 cm was necessary to maintain the neutral neck [position by having special pediatric spine board with recessed region to let head (occiput) lie posterior in anatomical position or rolled towel under neck]. Therefore, putting together, the limited evidence in favor of spinal immobilization and reported risks involved, need for immobilization must be evaluated at the earliest possible instance and discontinued as early as clinically permissible.92 In addition to the traditional rigid cervical collars, rigid collars with supplemental devices which partly enclose head (e.g., Kendrick Extrication Devices) and tape can be employed.93 In the presence of occipitoatlantal dissociation, sandbag, and tapes can provide better immobilization.86,87,94
Conclusions
Pediatric CSI are rare and therefore, management principles of this injury are still largely controversial. The current consensus on the diagnostic principles in pediatric CSI, on the basis of existing literature, has been tabulated in Table 2.
Table 2.
Recommendations regarding cervical spine injury diagnosis in pediatric patients
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN, et al. Spinal injuries in children. J Pediatr Surg. 2004;39:607–12. doi: 10.1016/j.jpedsurg.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 2.McGrory BJ, Klassen RA, Chao EY, Staeheli JW, Weaver AL. Acute fractures and dislocations of the cervical spine in children and adolescents. J Bone Joint Surg Am. 1993;75:988–95. doi: 10.2106/00004623-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Mathur N, Jain S, Kumar N, Srivastava A, Purohit N, Patni A, et al. Spinal cord injury: Scenario in an Indian state. Spinal Cord. 2015;53:349–52. doi: 10.1038/sc.2014.153. [DOI] [PubMed] [Google Scholar]
- 4.Booth TN. Cervical spine evaluation in pediatric trauma. AJR Am J Roentgenol. 2012;198:W417–25. doi: 10.2214/AJR.11.8150. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton MG, Myles ST. Pediatric spinal injury: Review of 61 deaths. J Neurosurg. 1992;77:705–8. doi: 10.3171/jns.1992.77.5.0705. [DOI] [PubMed] [Google Scholar]
- 6.Hale AT, Alvarado A, Bey AK, Pruthi S, Mencio GA, Bonfield CM, et al. X-ray vs. CT in identifying significant C-spine injuries in the pediatric population. Childs Nerv Syst. 2017;33:1977–83. doi: 10.1007/s00381-017-3448-4. DOI 10.1007/s00381-017-3448-4. [DOI] [PubMed] [Google Scholar]
- 7.Anissipour AK, Agel J, Bellabarba C, Bransford RJ. Cervical facet dislocations in the adolescent population: a report of 21 cases at a Level 1 trauma center from 2004 to 2014. Eur Spine J. 2017;26:1266–71. doi: 10.1007/s00586-017-5003-0. DOI 10.1007/s00586-017-5003-0. [DOI] [PubMed] [Google Scholar]
- 8.Henry MK, Zonfrillo MR, French B, Song L, Feudtner C, Wood JN. Hospital Variation in Cervical Spine Imaging of Young Children with Traumatic Brain Injury. Acad Pediatr. 2016;16(7):684–91. doi: 10.1016/j.acap.2016.01.017. doi: 10.1016/j.acap.2016.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell EC, Leonard JR, Olsen CS, Jaffe DM, Anders J, Leonard JC. Atlantoaxial Rotatory Subluxation in Children? Pediatr Emerg Care. 2017;33(2):86–91. doi: 10.1097/PEC.0000000000001023. doi: 10.1097/PEC.0000000000001023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang YH, Shao J, Chou D, Wu JF, Song J, Zhang J. C1-C2 Pedicle Screw Fixation for Atlantoaxial Dislocation in Pediatric Patients Younger than 5 Years: A Case Series of 15 Patients. [Epub 2017 Sep 18];World Neurosurg. 2017 108:498–505. doi: 10.1016/j.wneu.2017.09.050. Available from: https://doi.org/10.1016/j.wneu.2017.09.050 . [DOI] [PubMed] [Google Scholar]
- 11.Knox J. Epidemiology of spinal cord injury without radiographic abnormality in children: a nationwide perspective. J Child Orthop. 2016;10:255–60. doi: 10.1007/s11832-016-0740-x. DOI 10.1007/s11832-016-0740-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC, Pediatric Emergency Care Applied Research Network (PECARN) Cervical Spine Study Group et al. Cervical spine injury patterns in children. Pediatrics. 2014;133:1179–88. doi: 10.1542/peds.2013-3505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitale MG, Vitale MA, Lehmann CL, Hyman JE, Roye DP, Jr, Skaggs DL, et al. Towards a national pediatric musculoskeletal trauma outcomes registry: The pediatric orthopaedic trauma outcomes research group (POTORG) experience. J Pediatr Orthop. 2006;26:151–6. doi: 10.1097/01.bpo.0000218520.98244.37. [DOI] [PubMed] [Google Scholar]
- 14.Kim C, Vassilyadi M, Forbes JK, Moroz NW, Camacho A, Moroz PJ, et al. Traumatic spinal injuries in children at a single level 1 pediatric trauma centre: Report of a 23-year experience. Can J Surg. 2016;59:205–12. doi: 10.1503/cjs.014515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Browne LR, Schwartz DH, Ahmad FA, Wallendorf M, Kuppermann N, Lerner EB, et al. Interobserver Agreement In Pediatric CSI Assessment. Academic Emergency Medicine. 2017;24(12):1501–10. doi: 10.1111/acem.13312. [DOI] [PubMed] [Google Scholar]
- 16.Rehan VK, Seshia MM. Spinal cord birth injury – Diagnostic difficulties. Arch Dis Child. 1993;69:92–4. doi: 10.1136/adc.69.1_spec_no.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abroms IF, Bresnan MJ, Zuckerman JE, Fischer EG, Strand R. Cervical cord injuries secondary to hyperextension of the head in breech presentations. Obstet Gynecol. 1973;41:369–78. [PubMed] [Google Scholar]
- 18.Cantu RC, Li YM, Abdulhamid M, Chin LS. Return to play after cervical spine injury in sports. Curr Sports Med Rep. 2013;12:14–7. doi: 10.1249/JSR.0b013e31827dc1fb. [DOI] [PubMed] [Google Scholar]
- 19.Moore JM, Hall J, Ditchfield M, Xenos C, Danks A. Utility of plain radiographs and MRI in cervical spine clearance in symptomatic non-obtunded pediatric patients without high-impact trauma. Childs Nerv Syst. 2017;33:249–58. doi: 10.1007/s00381-016-3273-1. DOI: 10.1007/s00381-016-3273-1. [DOI] [PubMed] [Google Scholar]
- 20.Hutton MJ, McGuire RA, Dunn R, Williams R, Robertson P, Twaddle B, et al. Catastrophic Cervical Spine Injuries in Contact Sports. Global Spine Journal. 2016;6(7):721–34. doi: 10.1055/s-0036-1586744. Available from: http://dx.doi.org/10.1055/s-0036-1586744.ISSN 2192-5682 . Epub 2016 Sep 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oh A, Sawvel M, Heaner D, Bhatia A, Reisner A, Tubbs RS, et al. Changes in use of cervical spine magnetic resonance imaging for pediatric patients with nonaccidental trauma. J Neurosurg Pediatr. 2017;20:271–7. doi: 10.3171/2017.2.PEDS16644. [DOI] [PubMed] [Google Scholar]
- 22.Baerg J, Thirumoorthi A, Hazboun R, Vannix R, Krafft P, Zouros A. Cervical spine injuries in young children: pattern and outcomes in accidental versus inflicted trauma. J Surg Res. 2017;219:366–73. doi: 10.1016/j.jss.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 23.Pang D, Thompson DN. Embryology and bony malformations of the craniovertebral junction. Childs Nerv Syst. 2011;27:523–64. doi: 10.1007/s00381-010-1358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basu S. Spinal injuries in children. Front Neurol. 2012;3:96. doi: 10.3389/fneur.2012.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reilly CW, Leung F. Synchondrosis fracture in a pediatric patient. Can J Surg. 2005;48:158–9. [PMC free article] [PubMed] [Google Scholar]
- 26.Roche C, Carty H. Spinal trauma in children. Pediatr Radiol. 2001;31:677–700. doi: 10.1007/s002470100532. [DOI] [PubMed] [Google Scholar]
- 27.Orenstein JB, Klein BL, Gotschall CS, Ochsenschlager DW, Klatzko MD, Eichelberger MR, et al. Age and outcome in pediatric cervical spine injury: 11-year experience. Pediatr Emerg Care. 1994;10:132–7. doi: 10.1097/00006565-199406000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Nitecki S, Moir CR. Predictive factors of the outcome of traumatic cervical spine fracture in children. J Pediatr Surg. 1994;29:1409–11. doi: 10.1016/0022-3468(94)90131-7. [DOI] [PubMed] [Google Scholar]
- 29.Dietrich AM, Ginn-Pease ME, Bartkowski HM, King DR. Pediatric cervical spine fractures: Predominantly subtle presentation. J Pediatr Surg. 1991;26:995–9. doi: 10.1016/0022-3468(91)90850-s. [DOI] [PubMed] [Google Scholar]
- 30.Baker C, Kadish H, Schunk JE. Evaluation of pediatric cervical spine injuries. Am J Emerg Med. 1999;17:230–4. doi: 10.1016/s0735-6757(99)90111-0. [DOI] [PubMed] [Google Scholar]
- 31.Parent S, Mac-Thiong JM, Roy-Beaudry M, Sosa JF, Labelle H. Spinal cord injury in the pediatric population: A systematic review of the literature. J Neurotrauma. 2011;28:1515–24. doi: 10.1089/neu.2009.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herman MJ, Pizzutillo PD. Cervical spine disorders in children. Orthop Clin North Am. 1999;30:457–66. doi: 10.1016/s0030-5898(05)70098-5. ix. [DOI] [PubMed] [Google Scholar]
- 33.Jaffe DM, Binns H, Radkowski MA, Barthel MJ, Engelhard HH., 3rd Developing a clinical algorithm for early management of cervical spine injury in child trauma victims. Ann Emerg Med. 1987;16:270–6. doi: 10.1016/s0196-0644(87)80171-3. [DOI] [PubMed] [Google Scholar]
- 34.Bertolami CN, Kaban LB. Chin trauma: A clue to associated mandibular and cervical spine injury. Oral Surg Oral Med Oral Pathol. 1982;53:122–6. doi: 10.1016/0030-4220(82)90274-2. [DOI] [PubMed] [Google Scholar]
- 35.Maroon JC. ‘Burning hands’ in football spinal cord injuries. JAMA. 1977;238:2049–51. [PubMed] [Google Scholar]
- 36.Finch GD, Barnes MJ. Major cervical spine injuries in children and adolescents. J Pediatr Orthop. 1998;18:811–4. [PubMed] [Google Scholar]
- 37.Anderson RC, Kan P, Vanaman M, Rubsam J, Hansen KW, Scaife ER, et al. Utility of a cervical spine clearance protocol after trauma in children between 0 and 3 years of age. J Neurosurg Pediatr. 2010;5:292–6. doi: 10.3171/2009.10.PEDS09159. [DOI] [PubMed] [Google Scholar]
- 38.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National emergency X-radiography utilization study group. N Engl J Med. 2000;343:94–9. doi: 10.1056/NEJM200007133430203. [DOI] [PubMed] [Google Scholar]
- 39.Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, et al. The canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286:1841–8. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 40.Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108:E20. doi: 10.1542/peds.108.2.e20. [DOI] [PubMed] [Google Scholar]
- 41.Pieretti-Vanmarcke R, Velmahos GC, Nance ML, Islam S, Falcone RA, Jr, Wales PW, et al. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: A multi-center study of the american association for the surgery of trauma. J Trauma. 2009;67:543–9. doi: 10.1097/TA.0b013e3181b57aa1. [DOI] [PubMed] [Google Scholar]
- 42.Ehrlich PF, Wee C, Drongowski R, Rana AR. Canadian C-spine rule and the national emergency X-radiography utilization low-risk criteria for C-spine radiography in young trauma patients. J Pediatr Surg. 2009;44:987–91. doi: 10.1016/j.jpedsurg.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 43.Rozzelle CJ, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Ryken TC, et al. Management of pediatric cervical spine and spinal cord injuries. Neurosurgery. 2013;72(Suppl 2):205–26. doi: 10.1227/NEU.0b013e318277096c. [DOI] [PubMed] [Google Scholar]
- 44.Anderson RC, Scaife ER, Fenton SJ, Kan P, Hansen KW, Brockmeyer DL, et al. Cervical spine clearance after trauma in children. J Neurosurg. 2006;105:361–4. doi: 10.3171/ped.2006.105.5.361. [DOI] [PubMed] [Google Scholar]
- 45.Hutchings L, Atijosan O, Burgess C, Willett K. Developing a spinal clearance protocol for unconscious pediatric trauma patients? J Trauma. 2009;67(4):681–6. doi: 10.1097/TA.0b013e3181a5f0ed. doi: 10.1097/TA.0b013e3181a5f0ed. [DOI] [PubMed] [Google Scholar]
- 46.Hernandez JA, Chupik C, Swischuk LE. Cervical spine trauma in children under 5 years: Productivity of CT. Emerg Radiol. 2004;10:176–8. doi: 10.1007/s10140-003-0320-5. [DOI] [PubMed] [Google Scholar]
- 47.Apple JS, Kirks DR, Merten DF, Martinez S. Cervical spine fractures and dislocations in children. Pediatr Radiol. 1987;17:45–9. doi: 10.1007/BF02386594. [DOI] [PubMed] [Google Scholar]
- 48.Ehara S, el-Khoury GY, Sato Y. Cervical spine injury in children: Radiologic manifestations. AJR Am J Roentgenol. 1988;151:1175–8. doi: 10.2214/ajr.151.6.1175. [DOI] [PubMed] [Google Scholar]
- 49.Sanchez JI, Paidas CN. Childhood trauma. Now and in the new millennium. Surg Clin North Am. 1999;79:1503–35. doi: 10.1016/s0039-6109(05)70090-6. [DOI] [PubMed] [Google Scholar]
- 50.Swischuk LE. Anterior displacement of C2 in children: Physiologic or pathologic. Radiology. 1977;122:759–63. doi: 10.1148/122.3.759. [DOI] [PubMed] [Google Scholar]
- 51.Harris MB, Duval MJ, Davis JA, Jr, Bernini PM. Anatomical and roentgenographic features of atlantooccipital instability. J Spinal Disord. 1993;6:5–10. [PubMed] [Google Scholar]
- 52.Bonadio WA. Cervical spine trauma in children: Part I. General concepts, normal anatomy, radiographic evaluation. Am J Emerg Med. 1993;11:158–65. doi: 10.1016/0735-6757(93)90112-o. [DOI] [PubMed] [Google Scholar]
- 53.Buhs C, Cullen M, Klein M, Farmer D. The pediatric trauma C-spine: Is the ‘odontoid’ view necessary? J Pediatr Surg. 2000;35:994–7. doi: 10.1053/jpsu.2000.6951. [DOI] [PubMed] [Google Scholar]
- 54.Pollack IF, Pang D, Sclabassi R. Recurrent spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1988;69:177–82. doi: 10.3171/jns.1988.69.2.0177. [DOI] [PubMed] [Google Scholar]
- 55.Pang D, Wilberger JE., Jr Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57:114–29. doi: 10.3171/jns.1982.57.1.0114. [DOI] [PubMed] [Google Scholar]
- 56.Frohna WJ. Emergency department evaluation and treatment of the neck and cervical spine injuries. Emerg Med Clin North Am. 1999;17:739–91. doi: 10.1016/s0733-8627(05)70097-3. v. [DOI] [PubMed] [Google Scholar]
- 57.Freemyer B, Knopp R, Piche J, Wales L, Williams J. Comparison of five-view and three-view cervical spine series in the evaluation of patients with cervical trauma. Ann Emerg Med. 1989;18:818–21. doi: 10.1016/s0196-0644(89)80203-3. [DOI] [PubMed] [Google Scholar]
- 58.Egloff AM, Kadom N, Vezina G, Bulas D. Pediatric cervical spine trauma imaging: A practical approach. Pediatr Radiol. 2009;39:447–56. doi: 10.1007/s00247-008-1043-2. [DOI] [PubMed] [Google Scholar]
- 59.Djang WT. Radiology of acute spinal trauma. Crit Care Clin. 1987;3:495–518. [PubMed] [Google Scholar]
- 60.Silva CT, Doria AS, Traubici J, Moineddin R, Davila J, Shroff M, et al. Do additional views improve the diagnostic performance of cervical spine radiography in pediatric trauma? AJR Am J Roentgenol. 2010;194:500–8. doi: 10.2214/AJR.09.2837. [DOI] [PubMed] [Google Scholar]
- 61.Rybicki F, Nawfel RD, Judy PF, Ledbetter S, Dyson RL, Halt PS, et al. Skin and thyroid dosimetry in cervical spine screening: Two methods for evaluation and a comparison between a helical CT and radiographic trauma series. AJR Am J Roentgenol. 2002;179:933–7. doi: 10.2214/ajr.179.4.1790933. [DOI] [PubMed] [Google Scholar]
- 62.Adelgais KM, Grossman DC, Langer SG, Mann FA. Use of helical computed tomography for imaging the pediatric cervical spine. Acad Emerg Med. 2004;11:228–36. doi: 10.1111/j.1553-2712.2004.tb02202.x. [DOI] [PubMed] [Google Scholar]
- 63.Adelgais KM, Browne L, Holsti M, Metzger RR, Murphy SC, Dudley N, et al. Cervical spine computed tomography utilization in pediatric trauma patients. J Pediatr Surg. 2014;49:333–7. doi: 10.1016/j.jpedsurg.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 64.Jimenez RR, Deguzman MA, Shiran S, Karrellas A, Lorenzo RL. CT versus plain radiographs for evaluation of c-spine injury in young children: Do benefits outweigh risks? Pediatr Radiol. 2008;38:635–44. doi: 10.1007/s00247-007-0728-2. [DOI] [PubMed] [Google Scholar]
- 65.Frush DP, Donnelly LF, Rosen NS. Computed tomography and radiation risks: What pediatric health care providers should know. Pediatrics. 2003;112:951–7. doi: 10.1542/peds.112.4.951. [DOI] [PubMed] [Google Scholar]
- 66.Crim JR, Moore K, Brodke D. Clearance of the cervical spine in multitrauma patients: The role of advanced imaging. Semin Ultrasound CT MR. 2001;22:283–305. doi: 10.1016/s0887-2171(01)90023-x. [DOI] [PubMed] [Google Scholar]
- 67.Keenan HT, Hollingshead MC, Chung CJ, Ziglar MK. Using CT of the cervical spine for early evaluation of pediatric patients with head trauma. AJR Am J Roentgenol. 2001;177:1405–9. doi: 10.2214/ajr.177.6.1771405. [DOI] [PubMed] [Google Scholar]
- 68.Chung S, Mikrogianakis A, Wales PW, Dirks P, Shroff M, Singhal A, et al. Trauma association of canada pediatric subcommittee national pediatric cervical spine evaluation pathway: Consensus guidelines. J Trauma. 2011;70:873–84. doi: 10.1097/TA.0b013e3182108823. [DOI] [PubMed] [Google Scholar]
- 69.Schleehauf K, Ross SE, Civil ID, Schwab CW. Computed tomography in the initial evaluation of the cervical spine. Ann Emerg Med. 1989;18(8):815–7. doi: 10.1016/s0196-0644(89)80202-1. [DOI] [PubMed] [Google Scholar]
- 70.McCulloch PT, France J, Jones DL, Krantz W, Nguyen TP, Chambers C, et al. Helical computed tomography alone compared with plain radiographs with adjunct computed tomography to evaluate the cervical spine after high-energy trauma. J Bone Joint Surg Am. 2005;87:2388–94. doi: 10.2106/JBJS.E.00208. [DOI] [PubMed] [Google Scholar]
- 71.Sun R, Skeete D, Wetjen K, Lilienthal M, Liao J, Madsen M, et al. A pediatric cervical spine clearance protocol to reduce radiation exposure in children. J Surg Res. 2013;183:341–6. doi: 10.1016/j.jss.2012.12.048. [DOI] [PubMed] [Google Scholar]
- 72.Borock EC, Gabram SG, Jacobs LM, Murphy MA. A prospective analysis of a two-year experience using computed tomography as an adjunct for cervical spine clearance. J Trauma. 1991;31:1001–5. doi: 10.1097/00005373-199107000-00021. [DOI] [PubMed] [Google Scholar]
- 73.Garton HJ, Hammer MR. Detection of pediatric cervical spine injury. Neurosurgery. 2008;62:700–8. doi: 10.1227/01.NEU.0000311348.43207.B7. [DOI] [PubMed] [Google Scholar]
- 74.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: Part 1 – Normal occipital condyle-C1 interval in 89 children. Neurosurgery. 2007;61:514–21. doi: 10.1227/01.NEU.0000290897.77448.1F. [DOI] [PubMed] [Google Scholar]
- 75.Bertozzi JC, Rojas CA, Martinez CR. Evaluation of the pediatric craniocervical junction on MDCT. AJR Am J Roentgenol. 2009;192:26–31. doi: 10.2214/ajr.08.1058. [DOI] [PubMed] [Google Scholar]
- 76.Levitt MA, Flanders AE. Diagnostic capabilities of magnetic resonance imaging and computed tomography in acute cervical spinal column injury. Am J Emerg Med. 1991;9:131–5. doi: 10.1016/0735-6757(91)90173-h. [DOI] [PubMed] [Google Scholar]
- 77.Flynn JM, Closkey RF, Mahboubi S, Dormans JP. Role of magnetic resonance imaging in the assessment of pediatric cervical spine injuries. J Pediatr Orthop. 2002;22:573–7. [PubMed] [Google Scholar]
- 78.Pang D. Spinal cord injury without radiographic abnormality in children, 2 decades later. Neurosurgery. 2004;55:1325–42. doi: 10.1227/01.neu.0000143030.85589.e6. [DOI] [PubMed] [Google Scholar]
- 79.Selden NR, Quint DJ, Patel N, d’Arcy HS, Papadopoulos SM. Emergency magnetic resonance imaging of cervical spinal cord injuries: Clinical correlation and prognosis. Neurosurgery. 1999;44:785–92. doi: 10.1097/00006123-199904000-00057. [DOI] [PubMed] [Google Scholar]
- 80.Dickman CA, Zabramski JM, Rekate HL, Sonntag VK. Spinal cord injuries in children without radiographic abnormalities. West J Med. 1993;158:67–8. [PMC free article] [PubMed] [Google Scholar]
- 81.Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC, et al. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol. 2007;28:209–15. [PMC free article] [PubMed] [Google Scholar]
- 82.Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation.(Fixed rotatory subluxation of the atlanto-axial joint) J Bone Joint Surg Am. 1977;59:37–44. [PubMed] [Google Scholar]
- 83.Barcelos AC, Patriota GC, Netto AU. Nontraumatic atlantoaxial rotatory subluxation: Grisel syndrome. Case report and literature review. Global Spine J. 2014;4:179–86. doi: 10.1055/s-0033-1363936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Grisel P. Enucleation de l’atlas et torticollis nasopharyngien. Presse Med. 1951;59:1647–8. [Google Scholar]
- 85.Parke WW, Rothman RH, Brown MD. The pharyngovertebral veins: an anatomical rationale for Grisel's syndrome. Journal of Bone and Joint Surgery. 1984;66A:568–74. [PubMed] [Google Scholar]
- 86.Huerta C, Griffith R, Joyce SM. Cervical spine stabilization in pediatric patients: Evaluation of current techniques. Ann Emerg Med. 1987;16:1121–6. doi: 10.1016/s0196-0644(87)80468-7. [DOI] [PubMed] [Google Scholar]
- 87.Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: Classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38:44–50. doi: 10.1097/00006123-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 88.Cattell HS, Filtzer DL. Pseudosubluxation and other normal variations in the cervical spine in children. A study of one hundred and sixty children. J Bone Joint Surg Am. 1965;47:1295–309. [PubMed] [Google Scholar]
- 89.Harrison RB, Keats TE, Winn HR, Riddervold HO, Pope TL., Jr Pseudosubluxation of the axis in young adults. J Can Assoc Radiol. 1980;31:176–7. [PubMed] [Google Scholar]
- 90.Shaw M, Burnett H, Wilson A, Chan O. Pseudosubluxation of C2 on C3 in polytraumatized children – prevalence and significance. Clin Radiol. 1999;54:377–80. doi: 10.1053/crad.1999.0192. [DOI] [PubMed] [Google Scholar]
- 91.Curran C, Dietrich AM, Bowman MJ, Ginn-Pease ME, King DR, Kosnik E, et al. Pediatric cervical-spine immobilization: Achieving neutral position? J Trauma. 1995;39:729–32. doi: 10.1097/00005373-199510000-00022. [DOI] [PubMed] [Google Scholar]
- 92.Herzenberg JE, Hensinger RN, Dedrick DK, Phillips WA. Emergency transport and positioning of young children who have an injury of the cervical spine. The standard backboard may be hazardous. J Bone Joint Surg Am. 1989;71:15–22. [PubMed] [Google Scholar]
- 93.Nypaver M, Treloar D. Neutral cervical spine positioning in children. Ann Emerg Med. 1994;23:208–11. doi: 10.1016/s0196-0644(94)70032-x. [DOI] [PubMed] [Google Scholar]
- 94.Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;2:CD002803. doi: 10.1002/14651858.CD002803. [DOI] [PMC free article] [PubMed] [Google Scholar]