Key Points
Question
Is higher cardiorespiratory fitness in midlife associated with a lower risk of cardiovascular mortality after incident depression past 65 years of age?
Findings
In this cohort study of Medicare-eligible patients, higher levels of fitness in midlife were associated with a 16% lower risk of depression. In addition, after a diagnosis of depression, higher levels of fitness were associated with a 56% lower risk of cardiovascular mortality.
Meaning
Men and women who are more physically fit at midlife have a lower risk of depression and cardiovascular mortality after a diagnosis of depression in later life, suggesting that fitness is an important part of a primary preventive strategy for cardiovascular disease and depression across the lifespan.
Abstract
Importance
Cardiorespiratory fitness (hereinafter referred to as fitness) as estimated by exercise testing is a modifiable risk factor independently associated with chronic diseases, cardiovascular disease (CVD) events, and mortality, but the association of fitness at midlife with incidence of later-life depression and the risk of CVD mortality after a depression diagnosis is unknown.
Objective
To determine whether fitness measured in midlife would be inversely associated with later-life CVD mortality with antecedent depression.
Design, Setting, and Participants
This retrospective cohort study at a single-center, community-based preventive medicine clinic was performed as part of the Cooper Center Longitudinal Study. Data were collected from January 13, 1971, through December 31, 2009, and analyzed from October 6, 2015, through August 14, 2017. Participants included generally healthy men and women who presented for preventive medicine examinations at midlife and who were eligible for Medicare from 1999 to 2010. Those with a self-reported history of depression, myocardial infarction, or stroke at examination were excluded.
Exposures
Objective midlife fitness estimated from results of treadmill exercise testing.
Main Outcomes and Measures
Depression diagnosis from Medicare claims files using established algorithms and CVD mortality from National Death Index records.
Results
A total of 17 989 participants (80.2% men) with a mean (SD) age of 50.0 (8.7) years were included. After 117 218 person-years of Medicare follow-up, 2701 depression diagnoses, 610 deaths due to CVD without prior depression, and 231 deaths due to CVD after depression were observed. A high level of fitness in midlife was associated with a 16% lower risk of depression (hazard ratio [HR], 0.84; 95% CI, 0.74-0.95) compared with a low level of fitness. A high fitness level was also associated with a 61% lower risk of death due to CVD without depression (HR, 0.39; 95% CI, 0.31-0.48) compared with a low level of fitness. After a diagnosis of depression, a high fitness level was associated with a 56% lower risk of death due to CVD (HR, 0.44; 95% CI, 0.31-0.64) compared with a low fitness level.
Conclusions and Relevance
Midlife fitness is associated with a lower risk of later-life depression, CVD mortality, and CVD mortality after incident later-life depression. These findings suggest the importance of midlife fitness in primary prevention of depression and subsequent CVD mortality in older age and should encourage physicians to consider fitness and physical activity in promoting healthy aging.
This cohort study assesses whether fitness measured in midlife is associated with later life depression and death due to cardiovascular disease in a population of Medicare recipients.
Introduction
Depression and depressive disorders are common conditions affecting older individuals and are associated with cardiovascular disease (CVD). In the presence of CVD events, the prevalence of depression is high, with as many as 1 in 5 patients with CVD having depression, especially after stroke.1 Conversely, depression is linked with CVD mortality.2,3,4 In fact, a 2014 American Heart Association Scientific Statement evaluated 53 studies and concluded that depression should be elevated as a risk factor for adverse outcomes in patients with acute coronary syndrome.5
Given that CVD remains a leading cause of death in the United States, primary prevention of CVD has been advocated through assessment of multiple risk factors and practice guidelines with ongoing updates.6 The American Psychological Association has also encouraged engagement by psychologists in primary prevention for behavioral and mental disorders.7 Considering the large health burden of depressive disorders, interventional approaches alone may be inadequate and lack cost-effectiveness, further supporting incorporation of a preventive approach.8,9 Because many of the risk factors for depression, such as life events or adverse socioeconomic factors, are not easily modifiable, the specific approach to prevention may not be clear, and research specifically addressing long-term risk reduction in this area has been advocated.10
A modifiable risk factor for depressive and CVD conditions is cardiorespiratory fitness (hereinafter referred to as fitness).11,12,13,14,15,16 Fitness is inversely associated with all-cause and CVD mortality11,13,17 and a lower incidence of depression and physician visits concerning depression.18,19,20,21
Considering the link of depression to CVD, a modifiable risk factor such as fitness with the potential to lower the risk of depression and CVD sequelae in aging adults would be useful. However, the association between midlife fitness and later-life depression with subsequent CVD mortality has not been evaluated. We hypothesized that a higher level of fitness in middle age would be associated with a lower risk of depression in older age and a lower risk of CVD mortality after incident depression. By linking the Cooper Center Longitudinal Study (CCLS) with claims data from the Centers for Medicare & Medicaid Services, we studied the association of fitness in midlife with the subsequent risk of depression diagnosis and CVD mortality.
Methods
Study Population
The CCLS is an updated continuation of the Aerobics Center Longitudinal Study, an ongoing, prospective study at The Cooper Institute in Dallas, Texas, that began in 1970.11,13,22 Patients evaluated at the Cooper Clinic and included as participants in the CCLS are generally well-educated, non-Hispanic white patients with access to health care. Patients receive a preventive medical examination that includes self-reported medical and lifestyle history, physician-administered physical examination, anthropometric measurements, fasting laboratory studies, and a maximal treadmill fitness assessment. Data were collected from January 13, 1971, through December 31, 2009. Participants provide written informed consent for inclusion in the research database, and the study is reviewed and approved annually by the institutional review board of The Cooper Institute.
A total of 19 241 patients enrolled in the CCLS who had complete information to determine their midlife health status and were enrolled in fee-for-service Medicare coverage from January 1, 1999, through December 31, 2009, were considered for inclusion in the study. After excluding 901 individuals with a history of depression and 351 individuals with a history of CVD, including myocardial infarction and stroke, at the time of the midlife examination, a final sample size of 17 989 was included in this analysis. Participants were followed up from the date of initiating Medicare coverage until death or the end of follow-up on December 31, 2009.
The measurements of baseline variables in the CCLS have been well described and were obtained in accordance with standard protocols.11,13 Body mass index was calculated as measured weight in kilograms divided by measured height in meters squared. Seated resting blood pressure was obtained with a mercury sphygmomanometer. Fasting venous blood samples were assayed for serum cholesterol and glucose levels using standardized, automated techniques. The measurement of cardiorespiratory fitness was obtained from time to maximum effort using the modified Balke protocol.23 The test time using this protocol is highly correlated with directly measured maximum oxygen uptake (r = 0.92).24,25 Each participant’s treadmill time was categorized into age- and sex-specific quintiles derived from the CCLS as a whole, in accordance with a standard approach, using previously published definitions of fitness categories.11,26 Quintile 1 represented low fitness; quintiles 2 and 3, moderate fitness; and quintiles 4 and 5, high fitness.
The outcome measure of depression was ascertained from Medicare administrative data obtained from the Centers for Medicare & Medicaid Services. The diagnosis was determined from the Chronic Condition Warehouse included in the Beneficiary Annual Summary File using established algorithms for research purposes.27,28 Depression was defined using International Classification of Diseases, Ninth Revision (ICD-9) codes 296.20 to 296.36, 296.50 to 296.56, 296.60 to 296.66, 296.89, 298.0, 300.4, 309.1, and 311.29 Mortality information was obtained from the National Death Index, and the underlying cause of death was defined by ICD-9 codes for deaths before 1999 and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes for deaths from 1999 through 2009. Death due to CVD was defined by ICD-9 codes 410.0 to 458.9 and equivalent ICD-10 codes.
Statistical Analyses
Data were analyzed from October 6, 2015, through August 14, 2017. Patient characteristics at midlife were summarized by fitness level, and incidence rates of depression and CVD death were compared across strata of fitness using an exponential survival model. A failure time model was used to investigate the multivariate outcomes of incident depression, CVD mortality without previous depression, and CVD mortality after the diagnosis of depression.30 The model fits marginal Cox proportional hazards regression models to each outcome and uses the robust sandwich estimate of the covariance matrix to account for dependence of multiple failure times.31 Models were fit to attained age and adjusted for midlife age, sex, year of examination, smoking, systolic blood pressure, cholesterol level, body mass index, and fasting glucose level. The proportional hazards assumption was tested using weighted Schoenfeld residuals, and terms for the covariate × attained age were entered to address residual nonproportional hazards. A 2-sided P value of less than .05 was considered statistically significant. All analyses were programmed in SAS/STAT, version 9.4 (SAS Institute Inc). Unless otherwise indicated, data are expressed as mean (SD).
Results
We included a total of 17 989 participants (3559 women [19.8%] and 14 430 men [80.2%]) with a mean (SD) age of 50.0 (8.7) years at the midlife examination. Baseline midlife characteristics of the study participants by fitness category are summarized in Table 1. Compared with participants in the low fitness category, those in the high fitness category had a lower mean body mass index (24.4 [2.9] vs 27.9 [4.7]), lower systolic blood pressure (120.8 [14.8] vs 123.6 [15.0] mm Hg), and more favorable mean levels of total cholesterol (208.8 [37.0] vs 219.7 [41.2] mg/dL [to convert to millimoles per liter, multiply by 0.0259]) and fasting glucose (98.5 [12.3] vs 103.3 [22.1] mg/dL [to convert to millimoles per liter, multiply by 0.0555]) (Table 1).
Table 1. Midlife Characteristics of CCLS Participants.
| Characteristic | Cardiorespiratory Fitness Categorya | ||
|---|---|---|---|
| Low (n = 2959) | Moderate (n = 7230) | High (n = 7800) | |
| Age at CCLS examination, mean (SD), yb | 46.9 (8.5) | 49.4 (8.7) | 51.6 (8.5) |
| Age at Medicare entry, mean (SD), y | 67.7 (4.7) | 67.8 (5.0) | 67.7 (4.9) |
| Medicare age, mean (SD), yc | 74.2 (6.3) | 74.5 (6.8) | 74.2 (6.9) |
| Women, No. (%) | 472 (16.0) | 1306 (18.1) | 1781 (22.8) |
| Smoking, No. (%)d | 899 (30.0) | 1332 (18.4) | 637 (8.2) |
| Treadmill time, mean (SD), min | 10.2 (2.9) | 14.2 (3.1) | 19.4 (4.3) |
| Fitness, mean (SD), MET | 8.1 (1.4) | 9.9 (1.4) | 12.3 (2.1) |
| BMI, mean (SD) | 27.9 (4.7) | 26.1 (3.5) | 24.4 (2.9) |
| Systolic blood pressure, mean (SD), mm Hg | 123.6 (15.0) | 121.3 (14.5) | 120.8 (14.8) |
| Total cholesterol level, mean (SD), mg/dL | 219.7 (41.2) | 215.0 (39.1) | 208.8 (37.0) |
| Fasting glucose level, mean (SD), mg/dL | 103.3 (22.1) | 100.6 (16.2) | 98.5 (12.3) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CCLS, Cooper Center Longitudinal Study; MET, metabolic equivalent.
SI conversion factors: To convert cholesterol to millimoles per liter, multiply by 0.0259; glucose to millimoles per liter, multiply by 0.0555.
Determined from age- and sex-adjusted CCLS quintiles as low fitness (quintile 1), moderate fitness (quintiles 2-3), and high fitness (quintiles 4-5).
Indicates age at the time of initial assessment.
Indicates mean of age attained during Medicare follow-up.
Owing to missing data, denominators may be less than the column headings.
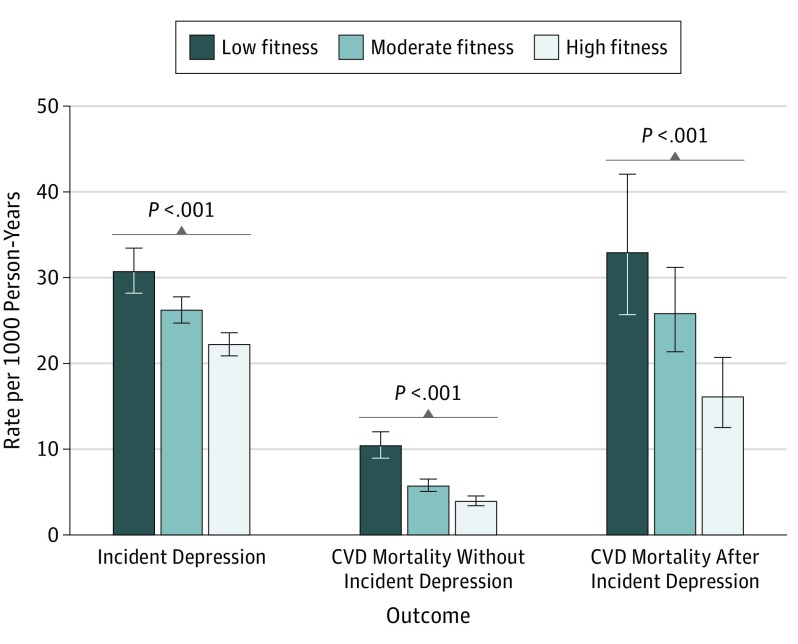
After 117 218 person-years of follow up, we observed 2701 diagnoses of depression and 841 deaths due to CVD. Two hundred thirty-one deaths were due to CVD after incident depression and 610 without incident depression. Incidence rates of depression and CVD mortality are summarized in the Figure. The rates of depression diagnosis in later life as well as CVD mortality after depression and CVD mortality without incident depression showed significant declines from low to moderate to high fitness categories assessed in midlife. Compared with the low fitness category, the rate of depression in the high fitness category was 22.2 per 1000 person-years (1041 diagnoses) and 26.2 in the moderate fitness category (1136 diagnoses) vs 30.7 in the low fitness category (524 diagnoses). For CVD mortality without incident depression, the rate in the high fitness category was 3.9 deaths per 1000 person-years (184 deaths) vs 5.7 in the moderate fitness category (249 deaths) and 10.4 in the low fitness category (177 deaths); for CVD mortality after depression, the rate in the high fitness category was 16.1 deaths per 1000 person-years (61 deaths) vs 25.8 in the moderate fitness category (107 deaths) and 32.9 in the low fitness category (63 deaths) (Figure).
Figure. Incidence Rates of Depression, CVD Mortality Without Incident Depression, and CVD Mortality After Incident Depression by Fitness Category.
Fitness categories are determined from age- and sex-adjusted Cooper Center Longitudinal Study quintiles as low (quintile 1), moderate (quintiles 2-3), and high (quintiles 4-5). P value indicates significant difference for trend across fitness categories. Error bars represent 95% CI for rates. CVD indicates cardiovascular disease.
Multivariate analyses revealed a consistent association with higher midlife fitness and a lower risk of incident depression, CVD mortality, and CVD mortality after a diagnosis of depression (Table 2 and Table 3). In analyses stratified by midlife fitness categories and adjusted for traditional risk factors, the high fitness category was associated with a 16% lower risk of depression (hazard ratio [HR], 0.84; 95% CI, 0.74-0.95) and a 61% lower risk of CVD mortality (HR, 0.39; 95% CI, 0.31-0.48) compared with low fitness. In those with incident depression, high fitness was associated with a 56% lower risk of CVD death (HR, 0.44; 95% CI, 0.31-0.64) (Table 2). Similarly, in analyses with fitness entered as a continuous variable expressed in units of metabolic equivalent, higher fitness was associated with a lower risk of depression per metabolic equivalent (HR, 0.95; 95% CI, 0.93-0.97), lower risk of CVD mortality without incident depression (HR, 0.84; 95% CI, 0.80-0.88), and lower risk of CVD mortality after depression (HR, 0.87; 95% CI, 0.81-0.93) (Table 3).
Table 2. Hazards for Incident Events by Fitness Categoriesa.
| Incident Event by Fitness Category | HR (95% CI) | |
|---|---|---|
| Model 1b | Model 2c | |
| Depression | ||
| High | 0.72 (0.64-0.80) | 0.84 (0.74-0.95) |
| Moderate | 0.84 (0.76-0.93) | 0.92 (0.83-1.03) |
| Low | 1 [Reference] | 1 [Reference] |
| CVD mortality without incident depression | ||
| High | 0.33 (0.27-0.41) | 0.39 (0.31-0.48) |
| Moderate | 0.48 (0.39-0.58) | 0.52 (0.43-0.64) |
| Low | 1 [Reference] | 1 [Reference] |
| CVD mortality after incident depression | ||
| High | 0.39 (0.27-0.56) | 0.44 (0.31-0.64) |
| Moderate | 0.69 (0.50-0.95) | 0.74 (0.54-1.02) |
| Low | 1 [Reference] | 1 [Reference] |
Abbreviations: CCLS, Cooper Center Logitudinal Study; CVD, cardiovascular disease; HR, hazard ratio.
Determined from age- and sex-adjusted CCLS quintiles as low fitness (quintile 1), moderate fitness (quintiles 2-3), and high fitness (quintiles 4-5). Low fitness is the referent category for HRs.
Adjusted for sex, age, examination year, and sex × stratum interaction.
Adjusted for sex, age, examination year, systolic blood pressure, total cholesterol level, body mass index, smoking status, and sex × stratum interaction.
Table 3. Hazards of Incident Events by Continuous Fitness.
| Incident Event | HR (95% CI) per MET Fitness | |||
|---|---|---|---|---|
| Model 1a | P Value | Model 2b | P Value | |
| Depression | 0.93 (0.91-0.95) | <.001 | 0.95 (0.93-0.97) | <.001 |
| CVD mortality | ||||
| Without incident depression | 0.82 (0.77-0.86) | <.001 | 0.84 (0.80-0.88) | <.001 |
| After incident depression | 0.84 (0.79-0.91) | 0.87 (0.81-0.93) | ||
Abbreviations: CVD, cardiovascular disease; HR, hazard ratio; MET, metabolic equivalent.
Adjusted for sex, age, examination year, and sex × stratum interaction.
Adjusted for sex, age, examination year, systolic blood pressure, total cholesterol level, body mass index, smoking status, and sex × stratum interaction.
Discussion
In the present study, we observed 2 important findings. First, in a large, generally healthy cohort of men and women, higher midlife fitness was associated with lower risk of a depression diagnosis after 65 years of age. Second, not only was higher midlife fitness associated with a lower risk of CVD mortality, but importantly, it was also associated with a lower risk of CVD mortality when CVD death was preceded by depression. This association was notable in later life years after the fitness assessment.
Depression and CVD are the most common causes of disability in the developed nations of the world, a connection between depression and CVD has been recognized for a number of years,32 and a higher prevalence of depression has been found in patients with myocardial infarction, stroke, and heart failure.33,34,35 Reviews of published studies of depression as a risk factor for mortality in CVD and coronary heart disease3 have shown considerable variation in methods, measurements, and cohorts and, in fact, some reluctance to assign depression as a risk factor for coronary heart disease because of the uncertainty as to the direction of causality. However, the preponderance of evidence supports classifying depression as a risk factor for adverse outcomes in CVD and coronary heart disease.2,5 Several physiologic mechanisms that may be common to depression and CVD have been suggested to explain the observed associations. These mechanisms include inflammatory changes, platelet aggregation, hypothalamic-pituitary-adrenal axis dysregulation, and autonomic dysfunction leading to an increase in arrhythmia and myocardial ischemia.36,37,38 Cardiorespiratory fitness has been shown to be favorably associated with risk of these proposed intermediaries, although the directionality of these associations is unclear.39,40,41
Higher fitness has been associated with a lower risk for all-cause and CVD mortality,11,13,42 and improvement in fitness level has also been shown to be associated with lower mortality risk.26 A number of studies have shown that higher fitness is associated with a lower risk of nonfatal outcomes, including myocardial infarction and heart failure, as well as depression.14,18,43,44
In an effort to intervene in CVD-associated depression from a psychological perspective, there has also been interest in depression screening among patients with CVD in different stages of disease and phases of treatment; however, screening methods and interventions are diverse, and the overall value of these efforts is inconsistent.45,46,47 Furthermore, arguments have been presented for and against screening, referral, and treatment of depression in patients with CVD based on current evidence and cost-effectiveness.5,45,46
Intervention studies have shown that exercise, which is known to increase fitness in individuals with depression,48 has an evident antidepressant effect when used in individuals with mild to moderate depression in the short term.20 A recent large cohort study of 33 908 healthy adults followed up for 11 years also showed that regular leisure time exercise of any intensity provided protection against future depression.9 Prior work14,16 has shown the association of higher levels of midlife fitness with a lower risk of CVD conditions in later life, such as stroke, that are associated with depression. In addition, fitness in the years before diagnosis of cancer can play a role in influencing the health outcomes after such a condition develops.49
Because effective, acute management of depression alone is not likely to relieve more than a portion of the overall burden of depressive disorders, early prevention of depression and CVD would be valuable if the primary risk modification was effective and enduring across the lifespan.6,7,8,9 A new and interesting finding in this study is that higher fitness assessed in middle age is associated with a lower risk of CVD mortality even in the presence of incident depression, with the fitness effect extending many years into older age. Health care costs and use of services are greatly increased in the setting of heart disease combined with the comorbid condition of depression, and these findings suggest that lowering risk through early prevention efforts may have economic as well as health benefits.50,51
We were not able to gauge how changes in fitness would affect risk in the later years of the cohort; however, fitness50,51 can be improved in most individuals by aerobic training, which need not be complicated or expensive.52,53 Despite this finding, surveys indicate that only about 50% of adults meet aerobic exercise guidelines and far fewer meet muscle-strengthening and aerobic guidelines.54,55
Strengths and Limitations
This study has several important strengths, including a large, homogeneous population and long follow-up. Although the primary racial/ethnic composition of non-Hispanic white patients and generally higher socioeconomic class may decrease generalizability, the healthy nature of this population with access to preventive health care allows evaluation of the association of fitness on a primordial basis and avoids the effect of unmeasured confounders. The association of risk factors and lifetime risk of CVD have been shown to be similar to that of the general population.42 The fitness measurement is objective and hence provides a more accurate picture of midlife physical activity level than self-report would because fitness correlates well with activity level. In addition, the outcomes are based on administrative claims data provided by the health care professional and are likely more accurate than self-report, especially in older patients.56
Limitations include that diagnoses determined from Medicare claims data are not clinically adjudicated. We were not able to detect outcomes or physician visits occurring between the midlife examination and Medicare eligibility, nor were we able to determine severity of the depression. However, Medicare data has been used by other researchers with a similar approach to provide informative findings regarding the association of traditional risk factors with Medicare outcomes.57,58,59 Of importance, information about the use of medication that could influence the presence or the absence of depression diagnosis is not available for this cohort. Finally, we cannot eliminate the possibility of depression and CVD leading to lower fitness levels. However, the relatively long mean period from fitness measure to Medicare observation makes such reverse causation less likely.
Conclusions
This study shows that being fit at midlife is associated with a lower risk of later-life depression and subsequent CVD mortality, even in the presence of depression. These findings suggest the importance of fitness in primary prevention of heart disease and associated CVD mortality in older aging adults. This study further supports the critical need for health care professionals to consider fitness and physical activity as part of overall preventive care to promote healthy aging.
References
- 1.Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28(11):1295-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813. [DOI] [PubMed] [Google Scholar]
- 3.Frasure-Smith N, Lespérance F. Depression and cardiac risk: present status and future directions. Heart. 2010;96(3):173-176. [DOI] [PubMed] [Google Scholar]
- 4.Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33(3):203-216. [DOI] [PubMed] [Google Scholar]
- 5.Lichtman JH, Froelicher ES, Blumenthal JA, et al. ; American Heart Association Statistics Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing . Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129(12):1350-1369. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin EJ, Blaha MJ, Chiuve SE, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics–2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Psychological Association Guidelines for prevention in psychology. Am Psychol. 2014;69(3):285-296. [DOI] [PubMed] [Google Scholar]
- 8.Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry. 2004;184:526-533. [DOI] [PubMed] [Google Scholar]
- 9.Harvey SB, Overland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: results of the HUNT Cohort Study. Am J Psychiatry. 2018;175(1):28-36. [DOI] [PubMed] [Google Scholar]
- 10.Cuijpers P. Prevention of depressive disorders: towards a further reduction of the disease burden of mental disorders. Early Interv Psychiatry. 2011;5(3):179-180. [DOI] [PubMed] [Google Scholar]
- 11.Blair SN, Kohl HW III, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262(17):2395-2401. [DOI] [PubMed] [Google Scholar]
- 12.DeFina LF, Barlow CE, Radford NB, Leonard D, Willis BL. The association between midlife cardiorespiratory fitness and later life chronic kidney disease: the Cooper Center Longitudinal Study. Prev Med. 2016;89:178-183. [DOI] [PubMed] [Google Scholar]
- 13.Blair SN, Kampert JB, Kohl HW III, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276(3):205-210. [PubMed] [Google Scholar]
- 14.Willis BL, Gao A, Leonard D, DeFina LF, Berry JD. Midlife fitness and the development of chronic conditions in later life. Arch Intern Med. 2012;172(17):1333-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeFina LF, Willis BL, Radford NB, et al. The association between midlife cardiorespiratory fitness levels and later-life dementia: a cohort study. Ann Intern Med. 2013;158(3):162-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pandey A, Patel MR, Willis B, et al. Association between midlife cardiorespiratory fitness and risk of stroke: the Cooper Center Longitudinal Study. Stroke. 2016;47(7):1720-1726. [DOI] [PubMed] [Google Scholar]
- 17.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024-2035. [DOI] [PubMed] [Google Scholar]
- 18.Dishman RK, Sui X, Church TS, Hand GA, Trivedi MH, Blair SN. Decline in cardiorespiratory fitness and odds of incident depression. Am J Prev Med. 2012;43(4):361-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Galper DI, Trivedi MH, Barlow CE, Dunn AL, Kampert JB. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006;38(1):173-178. [DOI] [PubMed] [Google Scholar]
- 20.Schuch FB, Vancampfort D, Sui X, et al. Are lower levels of cardiorespiratory fitness associated with incident depression? a systematic review of prospective cohort studies. Prev Med. 2016;93:159-165. [DOI] [PubMed] [Google Scholar]
- 21.Sui X, Laditka JN, Church TS, et al. Prospective study of cardiorespiratory fitness and depressive symptoms in women and men. J Psychiatr Res. 2009;43(5):546-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sui X, Laditka JN, Hardin JW, Blair SN. Estimated functional capacity predicts mortality in older adults. J Am Geriatr Soc. 2007;55(12):1940-1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willis BL, Morrow JR Jr, Jackson AW, DeFina LF, Cooper KH. Secular change in cardiorespiratory fitness of men: Cooper Center Longitudinal Study. Med Sci Sports Exerc. 2011;43(11):2134-2139. [DOI] [PubMed] [Google Scholar]
- 24.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92(1):39-46. [DOI] [PubMed] [Google Scholar]
- 25.Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A. Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J. 1982;103(3):363-373. [DOI] [PubMed] [Google Scholar]
- 26.Blair SN, Kohl HW III, Barlow CE, Paffenbarger RS Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093-1098. [PubMed] [Google Scholar]
- 27.Virnig BA, McBean M. Administrative data for public health surveillance and planning. Annu Rev Public Health. 2001;22:213-230. [DOI] [PubMed] [Google Scholar]
- 28.Gorina Y, Kramarow EA. Identifying chronic conditions in Medicare claims data: evaluating the Chronic Condition Data Warehouse algorithm. Health Serv Res. 2011;46(5):1610-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Medicare and Medicaid Services Chronic Condition Data Warehouse user guide. 2011:1-22. https://www.ccwdata.org/web/guest/condition-categories. Accessed August 29, 2017.
- 30.Wei LJ, Lin DY, Weissfeld L. Regression analysis of multivariate incomplete failure time data by modeling marginal distribution. J Am Stat Assoc. 1989;84:1065-1073. [Google Scholar]
- 31.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc. 1989;84(408):1074-1078. [Google Scholar]
- 32.Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365-1372. [DOI] [PubMed] [Google Scholar]
- 33.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330-1340. [DOI] [PubMed] [Google Scholar]
- 34.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol. 2002;7(pt 1):11-21. [DOI] [PubMed] [Google Scholar]
- 35.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527-1537. [DOI] [PubMed] [Google Scholar]
- 36.de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med. 2007;69(8):735-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parissis JT, Fountoulaki K, Filippatos G, Adamopoulos S, Paraskevaidis I, Kremastinos D. Depression in coronary artery disease: novel pathophysiologic mechanisms and therapeutic implications. Int J Cardiol. 2007;116(2):153-160. [DOI] [PubMed] [Google Scholar]
- 38.Ziegelstein RC, Parakh K, Sakhuja A, Bhat U. Depression and coronary artery disease: is there a platelet link? Mayo Clin Proc. 2007;82(11):1366-1368. [DOI] [PubMed] [Google Scholar]
- 39.Heber S, Volf I. Effects of physical (in)activity on platelet function. BioMed Res Int. 2015;2015:165078. doi: 10.1155/2015/165078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lucertini F, Ponzio E, Di Palma M, et al. High cardiorespiratory fitness is negatively associated with daily cortisol output in healthy aging men. PLoS One. 2015;10(11):e0141970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Silverman MN, Deuster PA. Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus. 2014;4(5):20140040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berry JD, Willis B, Gupta S, et al. Lifetime risks for cardiovascular disease mortality by cardiorespiratory fitness levels measured at ages 45, 55, and 65 years in men: the Cooper Center Longitudinal Study. J Am Coll Cardiol. 2011;57(15):1604-1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berry JD, Pandey A, Gao A, et al. Physical fitness and risk for heart failure and coronary artery disease. Circ Heart Fail. 2013;6(4):627-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1-8. [DOI] [PubMed] [Google Scholar]
- 45.Davidson KW, Korin MR. Depression and cardiovascular disease: selected findings, controversies, and clinical implications from 2009. Cleve Clin J Med. 2010;77(suppl 3):S20-S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elderon L, Smolderen KG, Na B, Whooley MA. Accuracy and prognostic value of American Heart Association: recommended depression screening in patients with coronary heart disease: data from the Heart and Soul Study. Circ Cardiovasc Qual Outcomes. 2011;4(5):533-540. [DOI] [PubMed] [Google Scholar]
- 47.Thombs BD, Ziegelstein RC, Stewart DE, Abbey SE, Parakh K, Grace SL. Usefulness of persistent symptoms of depression to predict physical health status 12 months after an acute coronary syndrome. Am J Cardiol. 2008;101(1):15-19. [DOI] [PubMed] [Google Scholar]
- 48.Stubbs B, Rosenbaum S, Vancampfort D, Ward PB, Schuch FB. Exercise improves cardiorespiratory fitness in people with depression: a meta-analysis of randomized control trials. J Affect Disord. 2016;190:249-253. [DOI] [PubMed] [Google Scholar]
- 49.Lakoski SG, Willis BL, Barlow CE, et al. Midlife cardiorespiratory fitness, incident cancer, and survival after cancer in men: the Cooper Center Longitudinal Study. JAMA Oncol. 2015;1(2):231-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Frasure-Smith N, Lespérance F, Gravel G, et al. Depression and health-care costs during the first year following myocardial infarction. J Psychosom Res. 2000;48(4-5):471-478. [DOI] [PubMed] [Google Scholar]
- 51.Rutledge T, Vaccarino V, Johnson BD, et al. Depression and cardiovascular health care costs among women with suspected myocardial ischemia: prospective results from the WISE (Women’s Ischemia Syndrome Evaluation) Study. J Am Coll Cardiol. 2009;53(2):176-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11(3):216-222. [DOI] [PubMed] [Google Scholar]
- 53.Warburton DE, Nicol CW, Bredin SS. Prescribing exercise as preventive therapy. CMAJ. 2006;174(7):961-974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Centers for Disease Control and Prevention (CDC) Adult participation in aerobic and muscle-strengthening physical activities—United States, 2011. MMWR Morb Mortal Wkly Rep. 2013;62(17):326-330. [PMC free article] [PubMed] [Google Scholar]
- 55.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: US Dept of Health & Human Services; 2008. [Google Scholar]
- 56.Jiang L, Zhang B, Smith ML, et al. Concordance between self-reports and Medicare claims among participants in a national study of chronic disease self-management program. Front Public Health. 2015;3:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Daviglus ML, Liu K, Greenland P, et al. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339(16):1122-1129. [DOI] [PubMed] [Google Scholar]
- 58.Daviglus ML, Liu K, Pirzada A, et al. Cardiovascular risk profile earlier in life and Medicare costs in the last year of life. Arch Intern Med. 2005;165(9):1028-1034. [DOI] [PubMed] [Google Scholar]
- 59.Daviglus ML, Liu K, Yan LL, et al. Relation of body mass index in young adulthood and middle age to Medicare expenditures in older age. JAMA. 2004;292(22):2743-2749. [DOI] [PubMed] [Google Scholar]