Key Points
Question
What were the demographic characteristics and trends of pediatric ocular injuries presenting to emergency departments in the United States from 2006 to 2014, based on data from the Nationwide Emergency Department Sample?
Findings
In this cohort study, 340 218 children from birth to age 17 years presented to Nationwide Emergency Department Sample emergency departments for care of acute ocular injuries, corresponding to 1 533 034 cases nationwide from 2006 to 2014. During the study period, there was a 26.1% decline in ocular injuries observed across all demographic characteristics, mechanisms of injury, and injury patterns.
Meaning
Between 2006 and 2014, pediatric ocular injuries declined in the United States, which may have resulted from prevention efforts.
Abstract
Importance
There is a lack of literature describing the incidence of pediatric acute ocular injury and associated likelihood of vision loss in the United States. Understanding national pediatric eye injury trends may inform future efforts to prevent ocular trauma.
Objective
To characterize pediatric acute ocular injury in the United States using data from a stratified, national sample of emergency department (ED) visits.
Design, Setting, and Participants
A retrospective cohort study was conducted. Study participants received care at EDs included in the 2006 to 2014 Nationwide Emergency Department Sample, comprising 376 040 children aged 0 to 17 years with acute traumatic ocular injuries. Data were analyzed from June 2016 to March 2018.
Exposures
International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes and external-cause-of-injury codes identified children with acute ocular injuries.
Main Outcomes and Measures
Demographic and clinical characteristics of children with acute traumatic ocular injuries were collected and temporal trends in the incidence of ocular injuries by age, risk of vision loss, and mechanism of injury were explored.
Results
In 2014, there were an estimated 163 431 (95% CI, 151 235-175 627) ED visits for pediatric acute ocular injury. Injured children were more often male (63.0%; 95% CI, 62.5-63.5) and in the youngest age category (birth to 4 years, 35.3%; 95% CI, 34.4-36.2; vs 10-14 years, 20.6%; 95% CI, 20.1-21.1). Injuries commonly resulted from a strike to the eye (22.5%; 95% CI, 21.3-23.8) and affected the adnexa (43.7%; 95% CI, 42.7-44.8). Most injuries had a low risk for vision loss (84.2%; 95% CI, 83.5-85.0), with only 1.3% (95% CI, 1.1-1.5) of injuries being high risk. Between 2006 and 2014, pediatric acute ocular injuries decreased by 26.1% (95% CI, −27.0 to −25.0). This decline existed across all patient demographic characteristics, injury patterns, and vision loss categories and for most mechanisms of injury. There were increases during the study in injuries related to sports (12.8%; 95% CI, 5.4-20.2) and household/domestic activities (20.7%; 95% CI, 16.2-25.2). The greatest decrease in high-risk injuries occurred with motor vehicle crashes (−79.8%; 95% CI, −85.8 to −74.9) and guns (−68.5%; 95% CI, −73.5 to −63.6).
Conclusions and Relevance
This study demonstrated a decline in pediatric acute ocular injuries in the United States between 2006 and 2014. However, pediatric acute ocular injuries continue to be prevalent, and understanding these trends can help establish future prevention strategies.
This study characterizes pediatric acute ocular injury in the United States using data from a stratified, national sample of emergency department visits.
Introduction
Approximately 387 000 patients per year present to US emergency departments (EDs) with eye injuries, and children represent up to one-third of those injured.1,2 Ocular injuries are among the leading causes of deprivation amblyopia, bilateral low vision, noncongenital monocular blindness, and long-term acquired visual disability.3,4 Children’s visual systems are not fully developed, rendering them particularly vulnerable to adverse effects from injury.5,6 Moreover, premature disability and its accompanying fiscal and psychological consequences disproportionately affect the lives of children.3,4,7
Designing prevention efforts requires a detailed understanding of the characteristics of children experiencing ocular injury. While prior studies report general demographic characteristics, settings, and mechanisms of ocular injury, the literature frequently lacks description of visual outcomes and demographic or mechanistic profiles of children at greatest risk for traumatic blindness.8 As an example, it has been reported that anywhere from 1% to 56% of patients with ocular trauma experience moderate to severe vision loss, while 1% to 59.3% experience subsequent blindness or enucleation.9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26 These estimates are highly variable, were generated from small study samples, and are difficult to compare owing to the dissimilar medical and economic infrastructures in each participating region of the world.
The US Centers for Disease Control and Prevention and the Agency for Healthcare Research and Quality have reported that ED visits for ocular injuries are decreasing; however, they do not identify specific patient or injury characteristics associated with this decline.1,2,4,5 Our study aimed to explore the national prevalence of pediatric acute ocular trauma in the United States and to explore trends during a 9-year span, with a focus on mechanisms of injury and their association with population demographic characteristics and risk of vision loss.
Methods
Data Source
The Nationwide Emergency Department Sample (NEDS) collects information on patients in a cross-section of US hospitals. Participating institutions are stratified according to geographic region defined by the US Census Bureau, urban or rural location, teaching or nonteaching status, ownership status, and trauma-level designation, thereby providing a representative sample of ED encounters nationwide.1 The NEDS is part of the Agency for Healthcare Research and Quality Healthcare Cost Utilization Project and is the largest all-payer ED database in the United States. To date, 947 hospitals in 30 states contribute to NEDS, representing approximately 20% of annual ED visits, which can be weighted for national estimates.1 The Healthcare Utilization Project databases conform to the definition of a limited data set. Institutional review board approval is not required for use of limited data sets, and patient consent was not needed. Users of the datasets must complete data use training and sign agreements, which address protection of patient and hospital confidentiality. From June 2016 to March 2018, we analyzed the NEDS records of children from birth to 17 years presenting to a participating ED between January 1, 2006, and December 31, 2014.
Identification of ED Visits Relating to Acute Ocular Trauma
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify ED visits for patients with acute ocular injury (eTable 1 in the Supplement). Previous studies exploring acute ocular injuries in the United States limited focus to ICD-9-CM codes for ocular injury within the injury and poisoning range, an approach that neglects diagnoses that reflect an injury when paired with an ICD-9-CM external-cause-of-injury code (E-code).27,28,29,30,31,32,33,34 These studies also included superficial eye injury codes (eg, insect on the eye), which do not represent ocular trauma unless accompanied by an E-code.27,28,29,30,31,32,33,34 To mitigate this, eye-related ICD-9-CM codes were reviewed and classified into 4 categories: ocular trauma by definition alone (eTable 1 in the Supplement); ocular trauma when occurring simultaneously with an appropriate E-code (eTable 2 in the Supplement); chronic complications of eye trauma; and injuries resulting from a nontraumatic mechanism.
We first queried NEDS records for any diagnosis in the acute or acute when paired with E-code categories. We excluded children whose ED disposition indicated transfer to another acute care facility to avoid double counting. Children who had concurrent diagnosis codes or E-codes indicative of chronic or nontraumatic eye injuries were excluded from the cohort to avoid double counting an injury event and to identify truly acute events. Children who had only ambiguous visual disturbances or injury to the optic pathway posterior to the optic chiasm were removed to exclude visual disturbances that were the result of nonocular neurologic etiologies. Data on all NEDS variables were collected for the final cohort, including information on patient demographic characteristics, mechanism of injury, treating ED characteristics, and ED disposition.
Classification of Ocular Injury
Mechanism of Injury
We grouped E-codes into 30 categories based on US Centers for Disease Control and Prevention guidelines as well as the biomechanical forces and potential risk surrounding the activity (eTable 3 in the Supplement). Children who had more than 1 E-code were classified according to the mechanism that had the most descriptive quality and greatest potential to inform prevention efforts. For example, a patient with motor vehicle collision (MVC) and strike to the eye codes was included only in the MVC category. Codes for discrete causes of injury, such as MVCs, powder/nonpowder guns, and sports, were given higher priority compared with nonspecific mechanisms, such as falls, cutting/piercing, or strikes, because the latter are vague and not easily addressed through intervention.
Risk of Vision Loss
We consulted 6 clinical ophthalmologists to design a hierarchical model for classifying and ranking diagnosis codes based on risk of vision loss (eTable 4 in the Supplement). Diagnoses were assigned to 1 of 3 categories: high risk, considered pathognomonic for vision loss; variable risk, indicating a need for injury monitoring; and low risk, anticipated as vision sparing. Injuries were assigned to these classifications based on the location of the injury with the clinical premise that superficial and anterior injuries are less severe than those affecting the posterior pole. This classification scheme was generated using a modified Delphi approach, during which clinicians were cognitively debriefed on their reasoning for assigning diagnoses to various risk categories.
Statistical Analysis
Statistical analyses were conducted with SAS Enterprise Guide, version 7.11 HF3 (SAS Institute Inc). The NEDS database supplied weights and other sampling information, which allowed for the calculation of national estimates and 95% confidence intervals.1 Linear regression was used to calculate the percentage change in the annual point estimates during the study period. Because some E-codes for the definition of sports-related and household activity–related ocular injuries did not exist or were not used by all EDs before 2010, the percentage of change in these mechanism categories are estimated from 2010 to 2014. Prevalence rates were generated using population estimates for the corresponding age, sex, and region groups when appropriate; otherwise, the prevalence denominator was children from birth to age 17 years for each year.35,36 To identify associations between patient demographic characteristics, mechanisms of injury, and increased risk of vision loss, we fit 2 separate logistic regression models that compared the high-risk and variable-risk groups with the low-risk group. To protect patient confidentiality, HCUP data users agree not to show cells with sample sizes of 10 or less; thus, only confidence intervals are presented for national estimates with small sample sizes. We generated 95% confidence intervals for the percentage change over time and for the adjusted odds ratios. We set statistical significance at a 2-sided P value less than .05; for percentage change, this represents 95% confidence intervals that do not contain 0 and for odds ratios, 95% confidence intervals that do not contain 1.
Results
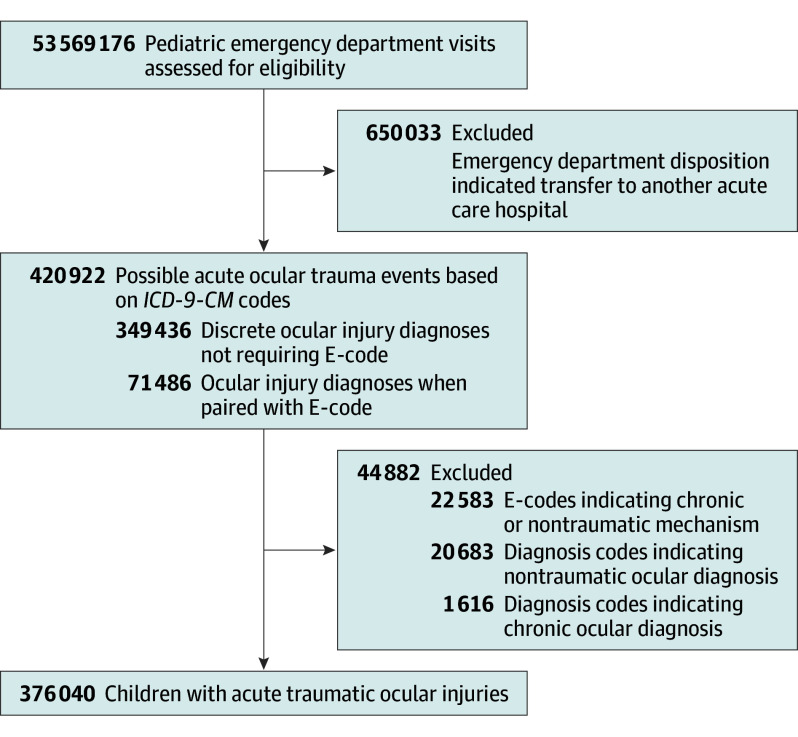
In total, NEDS data from 2006 to 2014 included 53 569 176 pediatric patient records. Following application of our inclusion and exclusion criteria, 376 040 discrete cases of pediatric acute ocular injury remained, which, when weighted, represents 1 713 710 ED visits for pediatric acute ocular injury nationally during the study period (Figure).
Figure. Study Cohort.
Flow diagram illustrating the inclusion and exclusion criteria used to identify a cohort of children with acute ocular injury–related emergency department visits between 2006 and 2014 using the National Emergency Department Sample. E-code indicates external-cause-of-injury code; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification.
Characteristics of Children Presenting to the ED With Acute Ocular Injury in 2014
The overall 2014 population prevalence rate for pediatric acute ocular injury ED visits was 2221 injuries per million children (95% CI, 2055-2387) (Table 1). Population prevalence rates were highest among boys (2740 injuries per million children; 95% CI, 2537-2943) and in children from birth to age 4 years (2903 per million children; 95% CI, 2632-3173).
Table 1. Demographic Characteristics for Pediatric Ocular Injury–Related ED Visits, NEDS 2006-2014.
| Characteristic | 2014 National Estimates | Change From 2006, % (95% CI) | 2014 Prevalence per Million Children, No. (95% CI)a | |
|---|---|---|---|---|
| No. (95% CI) | % (95% CI) | |||
| Total | 163 431 (151 235 to 175 627) | 100 | −26.1 (−27.0 to −25.0) | 2221 (2055 to 2387) |
| Sex | ||||
| Male | 102 975 (95 342 to 110 609) | 63.0 (62.5 to 63.5) | −27.5 (−28.7 to −26.4) | 2740 (2537 to 2943) |
| Female | 60 445 (55 753 to 65 137) | 37.0 (36.5 to 37.5) | −23.4 (−24.9 to −21.9) | 1679 (1549 to 1809) |
| Age, y | ||||
| 0-4 | 57 697 (52 326 to 63 068) | 35.3 (34.4 to 36.2) | −22.0 (−23.2 to −20.7) | 2903 (2632 to 3173) |
| 5-9 | 44 441 (40 893 to 47 990) | 27.2 (26.7 to 27.7) | −15.3 (−17.0 to −13.6) | 2166 (1993 to 2339) |
| 10-14 | 33 642 (31 262 to 36 022) | 20.6 (20.1 to 21.1) | −30.4 (−31.9 to −29.0) | 1627 (1512 to 1743) |
| 15-17 | 27 651 (26 125 to 29 177) | 16.9 (16.2 to 17.6) | −41.0 (−42.2 to −39.8) | 2209 (2087 to 2331) |
| Urban-rural designation for patient’s county of residence | ||||
| Large metropolitan areas (>1 million population) | 81 942 (71 443 to 92 440) | 50.3 (46.8 to 53.8) | −22.1 (−24.0 to −20.2) | NA |
| Medium metropolitan areas (250 000-999 999 population) | 39 767 (34 394 to 45 141) | 24.4 (21.3 to 27.6) | −23.2 (−25.8 to −20.6) | NA |
| Small metropolitan areas (50 000-249 999 population) | 14 882 (12 034 to 17 730) | 9.1 (7.3 to 11.0) | −31.0 (−33.0 to −29.1) | NA |
| Micropolitan/noncore areas (<50 000 population) | 26 230 (24 480 to 27 980) | 16.1 (14.7 to 17.5) | −35.9 (−36.9 to −34.9) | NA |
| Median household income quartiles for patient’s zip code, % | ||||
| 0-25 | 48 112 (42 703 to 53 521) | 29.9 (27.6 to 32.2) | −17.6 (−19.2 to −16.0) | NA |
| 25-50 | 44 909 (40 931 to 48 887) | 27.9 (26.1 to 29.7) | −23.9 (−25.2 to −22.7) | NA |
| 50-75 | 34 969 (31 535 to 38 402) | 21.7 (20.3 to 23.2) | −29.3 (−31.4 to −27.2) | NA |
| 75-100 | 33 045 (28 330 to 37 760) | 20.5 (18.1 to 22.9) | −33.3 (−35.9 to −30.7) | NA |
| Expected primary payer | ||||
| Public | 92 393 (84 924 to 99 863) | 56.6 (54.9 to 58.4) | 15.9 (13.5 to 18.3) | NA |
| Private | 60 820 (55 375 to 66 265) | 37.3 (35.5 to 39.1) | −49.3 (−50.1 to −48.5) | NA |
| Other | 9909 (8891 to 10 926) | 6.1 (5.6 to 6.5) | −53.9 (−56.9 to −50.9) | NA |
| Region of hospital | ||||
| Northeast | 36 807 (31 200 to 42 415) | 22.5 (19.5 to 25.6) | −26.2 (−27.8 to −24.6) | 3075 (2607 to 3544) |
| Midwest | 34 575 (30 368 to 38 782) | 21.2 (18.6 to 23.7) | −36.6 (−38.6 to −34.7) | 2202 (1934 to 2470) |
| South | 57 548 (49 956 to 65 139) | 35.2 (31.6 to 38.9) | −22.1 (−23.9 to −20.3) | 2050 (1780 to 2320) |
| West | 34 501 (28 022 to 40 980) | 21.1 (17.7 to 24.5) | −18.1 (−20.1 to −16.0) | 1934 (1571 to 2297) |
| Trauma center level | ||||
| Nontrauma or trauma level III | 104 268 (97 165 to 11 1371) | 63.8 (59.6 to 68.0) | −33.2 (−34.5 to −31.9) | NA |
| Trauma level I or II | 59 163 (49 248 to 69 077) | 36.2 (32.0 to 40.4) | 18.7 (13.2 to 24.3) | NA |
| Teaching status of hospital | ||||
| Metropolitan nonteaching | 44 282 (40 370 to 48 194) | 27.1 (24.5 to 29.7) | −41.8 (−43.5 to −40.0) | NA |
| Metropolitan teaching | 94 917 (83 487 to 106 347) | 58.1 (54.8 to 61.4) | −4.5 (−7.9 to −1.1) | NA |
| Nonmetropolitan | 24 232 (22 557 to 25 906) | 14.8 (13.4 to 16.2) | −37.8 (−38.9 to −36.6) | NA |
| Children’s hospital | ||||
| No | 151 148 (141 639 to 160 658) | 92.5 (86.8 to 98.1) | −25.0 (−25.9 to −24.2) | NA |
| Yes | 12 283 (2486 to 22 079) | 7.5 (1.9 to 13.2) | −37.8 (−48.1 to −27.6) | NA |
| ED disposition | ||||
| Discharged | 159 265 (147 508 to 171 022) | 97.5 (97.1 to 97.8) | −22.6 (−23.6 to −21.5) | NA |
| Admitted | 3993 (3274 to 4711) | 2.4 (2.1 to 2.8) | −40.4 (−42.2 to −38.5) | NA |
| Deceased, 95% CIb | 0 to 22 | NA | −33.6 (−48.0 to −19.2) | NA |
| Unknown | 164 (0 to 330) | 0.1 (0.0 to 0.2) | −131.5 (−147.9 to −115.1) | NA |
Abbreviations: ED, emergency department; NA, not applicable; NEDS, Nationwide Emergency Department Sample.
Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin.
Cells with sample sizes of 10 or less are reported as 95% CIs only to protect patient confidentiality.
The highest proportion of affected children lived in the South (35.2%; 95% CI, 31.6-38.9). However, prevalence rates were highest for children residing in the Northeast (3075 per million children; 95% CI, 2607-3544). Most injured children resided in large metropolitan regions (50.3%; 95% CI, 46.8-53.8) with populations greater than 1 000 000. The largest proportion of children resided in zip codes where the median household income was in the lowest quartile (29.9%; 95% CI, 27.6-32.2), and most injured children were covered by public insurance (56.6%; 95% CI,54.9-58.4).
Strikes (22.5%; 95% CI, 21.3-23.8), falls (10.5%; 95% CI, 9.8-11.3), and foreign bodies (8.5%; 95% CI, 7.9-9.0) were common reported mechanisms of acute ocular injury (Table 2). Sports injuries were also prevalent (14.2%; 95% CI, 12.2-16.1), with the specific subcategories of ball sports, ball sports with stick/racquet, and road sports being more common causes of acute ocular injury than winter sports, water sports, sports from a height, and dance sports/sports from moderate height.
Table 2. Mechanisms of Pediatric Acute Ocular Injury, NEDS 2006-2014.
| Mechanism of Injury | 2014 National Estimates | Change From 2006, % (95% CI) | 2014 Prevalence per Million Children, No. (95% CI)a | |
|---|---|---|---|---|
| No. (95% CI) | % (95% CI) | |||
| Sports | 23 134 (19 377 to 26 891) | 14.2 (12.2 to 16.1) | 12.8 (5.4 to 20.2) | 314 (263 to 365) |
| Road sports | 2235 (1835 to 2635) | 1.4 (1.2 to 1.6) | 40.3 (31.9 to 48.7) | 30 (25 to 36) |
| Winter sports | 247 (167 to 328) | 0.2 (0.1 to 0.2) | 4.5 (−9.9 to 18.9) | 3 (2 to 4) |
| Water sports | 307 (225 to 389) | 0.2 (0.1 to 0.2) | 8.0 (−8.7 to 24.6) | 4 (3 to 5) |
| Sports from height | 114 (64 to 164) | 0.1 (0.0 to 0.1) | −16.7 (−35.2 to 1.9) | 2 (1 to 2) |
| Ball sports | 3823 (3299 to 4348) | 2.3 (2.1 to 2.6) | 49.8 (40.9 to 58.7) | 52 (45 to 59) |
| Ball sports with stick/racquet | 2384 (2003 to 2766) | 1.5 (1.3 to 1.7) | 31.1 (23.3 to 38.9) | 32 (27 to 38) |
| Dance sports/sports from moderate height | 342 (257 to 427) | 0.2 (0.2 to 0.3) | 43.5 (35.3 to 51.7) | 5 (3 to 6) |
| Strike due to sports | 4692 (4071 to 5314) | 2.9 (2.5 to 3.2) | −22.5 (−31.7 to −13.3) | 64 (55 to 72) |
| Other sport/physical activity | 8989 (5876 to 12 102) | 5.5 (3.7 to 7.3) | 21.6 (11.2 to 32.0) | 122 (80 to 164) |
| Household/domestic activity | 2935 (2626 to 3244) | 1.8 (1.6 to 2.0) | 20.7 (16.2 to 25.2) | 40 (36 to 44) |
| Animal care | 2039 (1797 to 2281) | 1.2 (1.1 to 1.4) | 16.9 (10.2 to 23.6) | 28 (24 to 31) |
| Home activities | 896 (735 to 1058) | 0.5 (0.5 to 0.6) | 29.6 (25.3 to 33.9) | 12 (10 to 14) |
| Vehicle | 5687 (5061 to 6314) | 3.5 (3.1 to 3.8) | −59.8 (−62.3 to −57.3) | 77 (69 to 86) |
| Motor vehicle crash (automobile occupant) | 3738 (3292 to 4184) | 2.3 (2.0 to 2.5) | −58.2 (−60.7 to −55.7) | 51 (45 to 57) |
| Hit by motor vehicle (includes cyclists hit) | 719 (569 to 870) | 0.4 (0.4 to 0.5) | −57.9 (−62.2 to −53.5) | 10 (8 to 12) |
| Nonmotorized vehicle crash | 796 (656 to 935) | 0.5 (0.4 to 0.6) | −65.2 (−68.7 to −61.8) | 11 (9 to 13) |
| Other motorized vehicle crash | 434 (342 to 527) | 0.3 (0.2 to 0.3) | −63.4 (−67.6 to −59.3) | 6 (5 to 7) |
| Fall | 17 229 (15 292 to 19 166) | 10.5 (9.8 to 11.3) | −40.7 (−42.8 to −38.5) | 234 (208 to 260) |
| Fall from ground-level height | 7684 (6773 to 8595) | 4.7 (4.3 to 5.1) | −41.7 (−44.2 to −39.2) | 104 (92 to 117) |
| Fall from moderate/great height | 538 (428 to 648) | 0.3 (0.3 to 0.4) | −48.5 (−53.0 to −44.0) | 7 (6 to 9) |
| Other fall | 9007 (7919 to 10 095) | 5.5 (5.1 to 6.0) | −39.3 (−41.4 to −37.3) | 122 (108 to 137) |
| Miscellaneous | 65 970 (60 353 to 71 586) | 40.4 (38.5 to 42.3) | −48.4 (−50.4 to −46.5) | 897 (820 to 973) |
| Strike to eye | 36 836 (33 317 to 40 354) | 22.5 (21.3 to 23.8) | −41.9 (−43.9 to −40.0) | 501 (453 to 548) |
| Foreign body in eye | 13 816 (12 686 to 14 947) | 8.5 (7.9 to 9.0) | −57.0 (−59.4 to −54.5) | 188 (172 to 203) |
| Cutting/piercing instrument | 3024 (2645 to 3403) | 1.9 (1.7 to 2.0) | −53.1 (−54.9 to −51.3) | 41 (36 to 46) |
| Chemical or thermal injury to eye | 3784 (3363 to 4204) | 2.3 (2.1 to 2.5) | −62.3 (−65.3 to −59.3) | 51 (46 to 57) |
| Bite | 3185 (2765 to 3604) | 1.9 (1.8 to 2.1) | −28.7 (−32.0 to −25.3) | 43 (38 to 49) |
| Violence | 4176 (3593 to 4758) | 2.6 (2.3 to 2.8) | −55.4 (−57.2 to −53.7) | 57 (49 to 65) |
| Gun (powder and nonpowder) | 1150 (969 to 1332) | 0.7 (0.6 to 0.8) | −60.9 (−63.8 to −57.9) | 16 (13 to 18) |
| Other | 35 583 (31 411 to 39 755) | 21.8 (19.7 to 23.9) | 73.9 (64.2 to 83.6) | 484 (427 to 540) |
| Unknown | 12 892 (9459 to 16 325) | 7.9 (5.9 to 9.9) | −50.5 (−54.1 to −46.9) | 175 (129 to 222) |
Abbreviation: NEDS, Nationwide Emergency Department Sample.
Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged race, and Hispanic origin.
Most pediatric acute ocular injuries occurred in the adnexa (43.7%; 95% CI, 42.7-44.8) and cornea (27.2%; 95% CI, 26.1-28.2) (Table 3). Accordingly, injuries at low risk for vision loss (84.2%; 95% CI, 83.5-85.0) were more prevalent than high-risk (1.3%; 95% CI, 1.1-1.5) and variable-risk (14.5%; 95% CI, 13.8-15.1) injuries. Most children were cared for at nontrauma or trauma level III centers (63.8%; 95% CI, 59.6-68.0) compared with trauma level I or II hospitals (Table 1). Nationally, 7.5% (95% CI, 1.9-13.2) were treated at a children’s hospital, and 2.4% (95% CI, 2.1-2.8) were admitted for inpatient care (estimates exclude patients transferred to another hospital).
Table 3. Location in Eye of Injury and Risk of Vision Loss, NEDS 2006-2014.
| Category | 2014 National Estimates | Change From 2006, % (95% CI) | 2014 Prevalence per Million Children, No. (95% CI)a | |
|---|---|---|---|---|
| No. (95% CI) | % (95% CI) | |||
| Location in the eye | ||||
| Adnexa | 71 474 (65 590 to 77 357) | 43.7 (42.7 to 44.8) | −33.6 (−34.4 to −32.7) | 971 (891 to 1051) |
| Choroid and/or retina | 497 (346 to 648) | 0.3 (0.2 to 0.4) | −28.0 (−33.3 to −22.6) | 7 (5 to 9) |
| Conjunctiva | 11 768 (10 671 to 12 865) | 7.2 (6.8 to 7.6) | −14.9 (−16.4 to −13.5) | 160 (145 to 175) |
| Cornea | 44 387 (41 033 to 47 742) | 27.2 (26.1 to 28.2) | −28.5 (−30.4 to −26.6) | 603 (558 to 649) |
| Globe | 35 148 (31 830 to 38 465) | 21.5 (20.3 to 22.7) | −3.8 (−5.5 to −2.2) | 478 (433 to 523) |
| Iris, 95% CIb | (3 to 54) | NA | −49.2 (−63.7 to −34.7) | (0 to 1) |
| Lens, 95% CIb | (4 to 45) | NA | −75.6 (−83.6 to −67.6) | (0 to 1) |
| Nerve | 104 (59 to 149) | 0.1 (0.0 to 0.1) | −15.0 (−21.3 to −8.8) | 1 (1 to 2) |
| Risk of vision loss | ||||
| High risk | 2104 (1759 to 2448) | 1.3 (1.1 to 1.5) | −42.3 (−45.0 to −39.7) | 29 (24 to 33) |
| Variable risk | 23 650 (21 461 to 25 840) | 14.5 (13.8 to 15.1) | −24.3 (−26.0 to −22.6) | 321 (292 to 351) |
| Low risk | 137 677 (127 514 to 147 839) | 84.2 (83.5 to 85.0) | −26.0 (−27.3 to −24.8) | 1871 (1733 to 2009) |
Abbreviations: NA, not applicable; NEDS, Nationwide Emergency Department Sample.
Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin.
Cells with sample sizes of 10 or less are reported as 95% CIs only to protect patient confidentiality.
Trends in Pediatric Acute Ocular Injuries
Pediatric ocular injury–related ED visits decreased overall by −26.1% (95% CI, −27.0 to −25.0) from 2006 to 2014 (Table 1). Decreases were greatest for children aged 15 to 17 years (−41.0%; 95% CI, −42.2 to −39.8), those living in rural communities (−35.9%; 95% CI, −36.9 to −34.9), and those with median incomes in the highest quartile (−33.3%; 95% CI, −35.9 to −30.7).
When stratified by risk for vision loss, decreases were greatest in the high-risk subcategory (−42.3%; 95% CI, −45.0 to − 39.7) compared with variable risk (−24.3%; 95% CI, −26.0 to −22.6) and low risk (−26.0%; 95% CI, −27.3 to −24.8) (Table 3). Accordingly, the most substantial decreases were observed for injuries to the lens (−75.6%; 95% CI, −83.6 to −67.6) and iris (−49.2%; 95% CI, −63.7 to −34.7).
Table 2 reports percentage changes from 2006 to 2014 in ED visits for pediatric acute ocular injury according to mechanism. The greatest decreases were observed for mechanisms involving chemical or thermal burns (−62.3%; 95% CI, −65.3 to −59.3), guns (−60.9%; 95% CI, −63.8 to −57.8), and vehicles (−59.8%; 95% CI, −62.3 to −57.3). The greatest decrease in high-risk injuries occurred with MVCs (−79.8%; 95% CI, −84.8 to −74.9) and guns (−68.5%; 95% CI, −73.5 to −63.6) (eTable 5 in the Supplement). Increases during the study occurred in several mechanism categories, notably sports (ball sports, 49.8%; 95% CI, 40.9-58.7; dance sports/sports from moderate height, 43.5%; 95% CI, 35.3-51.7; road sports, 40.3%; 95% CI, 31.9-48.7; and ball sports with stick/racquet, 31.1%; 95% CI, 23.3-38.9) (Table 2). Injuries from household/domestic activities also increased over time (animal care, 16.9%; 95% CI, 10.2-23.6; other home activities, 29.6%; 95% CI, 25.3-33.9) (Table 2). These overarching trends were observed across all vision loss risk categories and age groups (eTables 5 and 6 in the Supplement).
Independent Risk Factors for Sustaining Acute Ocular Injuries at High and Variable Risk for Vision Loss
Compared with children with low-risk injuries, young age (birth to 4 years) and sex were associated with high-risk injuries, while being older than 4 years and living in a household with a median income in the lowest quartile were associated with variable risk injuries (Table 4). Specific mechanism categories were associated with high-risk injuries when using ground-level falls for comparison, including other sports activities, animal care, being hit by a motor vehicle, cutting/piercing instruments, chemical/thermal burns, violence, and guns. Specific mechanism categories associated with variable-risk injuries included road sports, winter sports, water sports, ball sports, ball sports with stick/racquet, dance sports/sports from moderate height, strikes owing to sports, other sports/physical activities, other home activities except animal care, strikes to the eye, chemical/thermal burns, violence, and guns.
Table 4. Logistic Regression Models Comparing Children With Injuries at Low Risk for Vision Loss With Those With High-Risk and Variable-Risk Injuries, NEDS 2006-2014.
| Independent Variable | OR (95% CI) | |
|---|---|---|
| Model 1: High Risk vs Low Risk | Model 2: Variable Risk vs Low Risk | |
| Sex | ||
| Male | 1 [Reference] | 1 [Reference] |
| Female | 0.85 (0.79-0.90) | 0.98 (0.96-1.00) |
| Age, y | ||
| 0-4 | 1 [Reference] | 1 [Reference] |
| 5-9 | 0.67 (0.60-0.73) | 1.34 (1.30-1.38) |
| 10-14 | 0.62 (0.53-0.74) | 1.73 (1.67-1.79) |
| 15-17 | 0.46 (0.36-0.58) | 1.55 (1.49-1.62) |
| Region of hospital | ||
| Northeast | 1 [Reference] | 1 [Reference] |
| Midwest | 0.91 (0.63-1.32) | 0.95 (0.87-1.04) |
| South | 1.08 (0.76-1.52) | 1.06 (0.98-1.14) |
| West | 1.22 (0.86-1.74) | 1.09 (1.01-1.18) |
| Urban-rural designation for patient’s county of residence | ||
| Large metropolitan areas (>1 million population) | 1 [Reference] | 1 [Reference] |
| Medium metropolitan areas (250 000-999 999 population) | 0.94 (0.81-1.09) | 0.96 (0.90-1.02) |
| Small metropolitan areas (50 000-249 999 population) | 0.91 (0.76-1.09) | 0.96 (0.90-1.03) |
| Micropolitan/noncore areas (<50 000 population) | 0.94 (0.80-1.10) | 1.00 (0.94-1.06) |
| Median household income quartiles for patient’s zip code, % | ||
| 0-25 | 1 [Reference] | 1 [Reference] |
| 25-50 | 1.05 (0.96-1.14) | 0.94 (0.90-0.98) |
| 50-75 | 1.03 (0.93-1.14) | 0.91 (0.88-0.95) |
| 75-100 | 0.97 (0.81-1.15) | 0.86 (0.82-0.91) |
| Mechanism of injury | ||
| Fall from ground-level height | 1 [Reference] | 1 [Reference] |
| Fall from moderate/great height | 0.88 (0.54-1.45) | 0.89 (0.72-1.10) |
| Other fall | 0.64 (0.51-0.80) | 0.82 (0.76-0.88) |
| Road sports | 0.74 (0.45-1.24) | 1.32 (1.11-1.57) |
| Winter sports | 0.68 (0.16-2.81) | 1.65 (1.16-2.34) |
| Water sports | 0.64 (0.15-2.66) | 1.68 (1.21-2.33) |
| Sports from height | 0.46 (0.06-3.37) | 0.96 (0.57-1.61) |
| Ball sports | 0.92 (0.59-1.44) | 1.84 (1.64-2.06) |
| Ball sports with stick/racquet | 0.66 (0.36-1.21) | 2.30 (2.02-2.61) |
| Dance sports/sports from moderate height | <0.001 | 1.82 (1.36-2.43) |
| Strike due to sports | 0.79 (0.59-1.05) | 1.97 (1.83-2.13) |
| Other sport/physical activity | 1.65 (1.22-2.21) | 1.75 (1.58-1.94) |
| Animal care | 2.00 (1.50-2.67) | 0.65 (0.56-0.76) |
| Home activities | 1.55 (0.90-2.67) | 1.50 (1.21-1.87) |
| Motor vehicle crash (automobile occupant) | 1.14 (0.86-1.52) | 1.02 (0.92-1.12) |
| Hit by motor vehicle (includes cyclists hit) | 2.19 (1.45-3.31) | 1.03 (0.85-1.25) |
| Nonmotorized vehicle crash | 1.02 (0.66-1.58) | 0.92 (0.79-1.07) |
| Other motorized vehicle crash | 1.07 (0.58-1.99) | 0.67 (0.52-0.86) |
| Strike to eye | 1.08 (0.88-1.31) | 1.75 (1.64-1.87) |
| Cutting/piercing instrument | 5.31 (4.32-6.52) | 0.83 (0.75-0.93) |
| Chemical or thermal injury to eye | 4.34 (3.44-5.46) | 6.51 (5.99-7.07) |
| Bite | 0.72 (0.52-0.99) | 0.24 (0.20-0.29) |
| Violence | 6.77 (4.93-9.31) | 1.73 (1.58-1.89) |
| Gun (powder and nonpowder) | 11.20 (8.78-14.29) | 5.75 (5.22-6.33) |
| Other | 0.93 (0.76-1.13) | 1.60 (1.48-1.74) |
| Unknown | 2.27 (1.40-3.68) | 1.49 (1.31-1.70) |
Abbreviations: NEDS, Nationwide Emergency Department Sample; OR, odds ratio.
Discussion
During the study, ED visits for pediatric acute ocular injury decreased by 26.1%, with a 42.3% decrease in injuries at high risk for vision loss. Despite this decline, a child visited the ED for acute ocular injury every 3 minutes in 2014, and 1 of 100 of these visits were for vision-compromising injuries. Sports and household/domestic activities were causes of acute ocular injury that increased and were associated with variable or high risk for vision loss. Notable declines occurred in injuries related to motor vehicles, chemical or thermal burns, and guns.
Consistent with other studies, we observed that most acute ocular injuries in children had a low risk of vision loss.28,37 However, there were particular demographic characteristics and mechanisms that were prevalent and associated with high or variable risk for vision loss that can serve to guide public health efforts. Children from birth to age 4 years had the highest probability of experiencing ocular trauma and were more likely to sustain a high risk of vision loss injury compared with other age groups. This is perhaps explained by parent or caregiver inattention combined with domestic hazards, such as exposure to household cleaners or pets.9,10,27,38,39,40,41 Household cleaners, children’s toys incorporating projectiles, and sharp-edged domestic items are leading causes of vision-threatening burns or penetration of the globe, particularly in young children.38 Laws requiring manufacturers to inform consumers of potential dangers and minimize the inherent risks associated with particular products by including child-resistant packaging, printed warnings, and age recommendations are successful prevention approaches.42 However, manufacturer standards are often reactionary, and there is an opportunity for better premarket safety testing guidelines. Colorful or otherwise appealing packaging poses an ongoing hazard to young children, as do incomplete instructions for parents regarding storage or disposal of potentially dangerous household items.43 Primary care clinicians can play a role in prevention by educating caregivers regarding items that can threaten their child’s vision if mishandled and making recommendations for keeping chemical products out of reach in locked cupboards and for eye protection and supervision when children are playing with toys that have sharp edges or kinetic properties.
Ocular injuries related to animal care increased during our study and were associated with injuries at high risk of vision loss. It is estimated that more than one-third of US households own at least 1 dog and that most dog bites occur in the home and involve the face and head.41,44,45,46 Young children in these studies were much more likely to be bit and to have more severe bites.41,44,45 Young children do not have the cognitive capacity to appropriately interact with dogs without supervision. Targeted education of pet owners regarding the risk of dog bites to young children can be provided by veterinarians and physicians or through public service media campaigns in partnership with the pet industry.
Across all age groups, sports were a prevalent cause of injury that increased during the study period and were associated with variable risk injuries. More than 70% of US children participate in sports, and accordingly, there are efforts to reduce sports-related ocular trauma.47 Standards for sport-specific protective eyewear include recommendations for polycarbonate versions of baseball faceguards, football helmet shields, hockey masks, and lenses or goggles for other ball and water sports.48 There are also regulations regarding manufacturing specifications and use of eye protectors for children playing baseball, basketball, lacrosse, soccer, hockey, skiing, and paintball.49 However, protective eyewear use in sports is not compulsory in schools or youth sports leagues.50 In studies where mandatory protective eyewear rules were enforced, high school field hockey and lacrosse players experienced up to 80% fewer eye/orbital injuries.51,52
No singular demographic characteristic or mechanism accounts for the observed decrease in ocular injury–related ED visits during the study period. This trend may reflect a shift in children’s use of free time away from unstructured, active play toward sedentary, indoor activities, such as watching television or playing video games.53 Children now engage in less kinetic play and thus have fewer opportunities for accidental eye injury.53 Notably, we did find proportionately greater decreases in high-risk eye injuries related to MVCs and guns (powder and nonpowder) over the study period. We hypothesize that these robust decreases were likely the result of cumulative prevention efforts.
Within the automotive industry, standards required that a 1993 through 2003 upgrade in cars incorporate head protection and airbags, followed by a 2003 phase-in reducing the speed and force at which airbags are deployed in cars.37 From 2007 to 2014, legislation was passed in 17 states mandating an appropriate form of child restraint for children younger than 8 years.54 These measures, which are intended to stabilize passengers, cushion impact, prevent head injury, and restrict unopposed momentum during crashes, may secondarily decrease the potential for eye injuries. As older cars without these improvements are phased out of circulation, we anticipate continued decreases in eye injuries via this mechanism.
The substantial decrease in firearm-related eye injuries observed over the study period is also notable because numerous publications have detailed the role of powder and nonpowder guns in severe, vision-threatening injuries, such as enucleation, traumatic cataracts, retinal detachment, sympathetic ophthalmitis, hyphema, and intraorbital pellets.55 The observed decline may be attributable in part to the 2005 Protection of Lawful Commerce in Arms Act, which prohibits manufacturers from selling handguns without a safety device.56 Additionally, beginning in 1997, children’s access to firearms has declined because of increased state-level legislation that restricts access, promotes safe storage, and requires the sale of locking devices for firearms when they are not in use.57
Limitations
This study has limitations. The NEDS data are gathered from ED billing data, which may not accurately capture diagnosis codes. Certain sport and home activity E-codes were not introduced until 2009; thus, information for these mechanisms is unavailable for 2006 to 2008. Investigators using the National Electronic Injury Surveillance System demonstrated slight decreases in sports and recreational ocular injuries during a similar study period.58 Sports-related and household injuries in this study increased, and estimates of change over time may be biased by missing data in earlier years; however, we adjusted for this by using regression analysis to calculate percentage change with confidence intervals over the study period. This study was designed to examine acute ocular trauma, and it is important to acknowledge that not all acute injuries have immediate effects or are evaluated in the ED.4
Conclusions
Our study demonstrates that pediatric acute ocular injuries decreased between 2006 and 2014 but remain a significant source of preventable monocular blindness. There are likely multiple initiatives that have reduced high-risk ocular injuries. There is a need to explore which prevention efforts have contributed to the observed nationwide decrease in pediatric ocular injuries overall and to identify further interventions to reduce ocular injury for mechanisms that are prevalent, on the rise, and place children at greatest risk for vision loss.
eTable 1. International Classification of Diseases, Ninth Revision, Clinical Modification Diagnosis Codes Used to Identify Acute Ocular Injury
eTable 2. International Classification of Diseases, Ninth Revision, Clinical Modification External-Cause-of-Injury Codes Used to Classify Mechanism of Injury
eTable 3. Mechanism of Injury Categories and Hierarchy
eTable 4. Stratification of Acute Ocular Injury International Classification of Diseases, Ninth Revision, Clinical Modification Diagnosis Codes by Risk of Vision Loss
eTable 5. Mechanisms of Pediatric Acute Ocular Injuries by Risk of Vision Loss, National Estimates, NEDS 2006-2014
eTable 6. Mechanisms of Pediatric Acute Ocular Injuries by Age Group, National Estimates, NEDS 2006-2014
References
- 1.Owens PL, Mutter R. Emergency department visits related to eye injuries, 2008: statistical brief #112. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb112.pdf. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Accessed November 3, 2017.
- 2.Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2014 emergency department summary tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2014_ed_web_tables.pdf. Accessed May 1, 2018.
- 3.Li X, Zarbin MA, Bhagat N. Pediatric open globe injury: a review of the literature. J Emerg Trauma Shock. 2015;8(4):216-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Negral AD. Magnitude of eye injuries worldwide. Comm Eye Health. 1997;10(24):49-53. [Google Scholar]
- 5.Acuna OM, Yen KG. Outcome and prognosis of pediatric patients with delayed diagnosis of open-globe injuries. J Pediatr Ophthalmol Strabismus. 2009;46(4):202-207. [DOI] [PubMed] [Google Scholar]
- 6.Bai H, Meng X, Wang D, Han J. Treatment for amblyopia after surgery for cataract and vitreoretina in pediatric ocular trauma. Eye Sci. 2013;28(2):68-72. [PubMed] [Google Scholar]
- 7.Polinder S, Haagsma JA, Toet H, Brugmans MJ, van Beeck EF; EUROCOST and APOLLO reference groups . Burden of injury in childhood and adolescence in 8 European countries. BMC Public Health. 2010;10:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan T, O’Keefe M, Bowell R, Lanigan B. Childhood penetrating eye injuries. Ir Med J. 1995;88(5):168-170. [PubMed] [Google Scholar]
- 9.Lee CH, Su WY, Lee L, Yang ML. Pediatric ocular trauma in Taiwan. Chang Gung Med J. 2008;31(1):59-65. [PubMed] [Google Scholar]
- 10.MacEwen CJ, Baines PS, Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999;83(8):933-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Bdour MD, Azab MA. Childhood eye injuries in North Jordan. Int Ophthalmol. 1998;22(5):269-273. [DOI] [PubMed] [Google Scholar]
- 12.Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs. 2011;19(4):186-191. [DOI] [PubMed] [Google Scholar]
- 13.El-Sebaity DM, Soliman W, Soliman AM, Fathalla AM. Pediatric eye injuries in upper Egypt. Clin Ophthalmol. 2011;5:1417-1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rapoport I, Romem M, Kinek M, et al. Eye injuries in children in Israel: a nationwide collaborative study. Arch Ophthalmol. 1990;108(3):376-379. [DOI] [PubMed] [Google Scholar]
- 15.Beby F, Roche O, Kodjikian L, et al. Penetrating ocular injuries in children: visual outcome and prognostic factors. Acta Ophthalmol Scand. 2006;84(2):266-267. [DOI] [PubMed] [Google Scholar]
- 16.Mela EK, Georgakopoulos CD, Georgalis A, Koliopoulos JX, Gartaganis SP. Severe ocular injuries in Greek children. Ophthalmic Epidemiol. 2003;10(1):23-29. [DOI] [PubMed] [Google Scholar]
- 17.Takvam JA, Midelfart A. Survey of eye injuries in Norwegian children. Acta Ophthalmol (Copenh). 1993;71(4):500-505. [DOI] [PubMed] [Google Scholar]
- 18.Cascairo MA, Mazow ML, Prager TC. Pediatric ocular trauma: a retrospective survey. J Pediatr Ophthalmol Strabismus. 1994;31(5):312-317. [DOI] [PubMed] [Google Scholar]
- 19.Moreira CA Jr, Debert-Ribeiro M, Belfort R Jr. Epidemiological study of eye injuries in Brazilian children. Arch Ophthalmol. 1988;106(6):781-784. [DOI] [PubMed] [Google Scholar]
- 20.Serrano JC, Chalela P, Arias JD. Epidemiology of childhood ocular trauma in a northeastern Colombian region. Arch Ophthalmol. 2003;121(10):1439-1445. [DOI] [PubMed] [Google Scholar]
- 21.Cao H, Li L, Zhang M, Li H. Epidemiology of pediatric ocular trauma in the Chaoshan Region, China, 2001-2010. PLoS One. 2013;8(4):e60844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu ML, Chang YS, Tseng SH, et al. Major pediatric ocular trauma in Taiwan. J Pediatr Ophthalmol Strabismus. 2010;47(2):88-95. [DOI] [PubMed] [Google Scholar]
- 23.Poon AS, Ng JS, Lam DS, Fan DS, Leung AT. Epidemiology of severe childhood eye injuries that required hospitalisation. Hong Kong Med J. 1998;4(4):371-374. [PubMed] [Google Scholar]
- 24.Saxena R, Sinha R, Purohit A, Dada T, Vajpayee RB, Azad RV. Pattern of pediatric ocular trauma in India. Indian J Pediatr. 2002;69(10):863-867. [DOI] [PubMed] [Google Scholar]
- 25.Kadappu S, Silveira S, Martin F. Aetiology and outcome of open and closed globe eye injuries in children. Clin Exp Ophthalmol. 2013;41(5):427-434. [DOI] [PubMed] [Google Scholar]
- 26.LaRoche GR, McIntyre L, Schertzer RM. Epidemiology of severe eye injuries in childhood. Ophthalmology. 1988;95(12):1603-1607. [DOI] [PubMed] [Google Scholar]
- 27.Nash EA, Margo CE. Patterns of emergency department visits for disorders of the eye and ocular adnexa. Arch Ophthalmol. 1998;116(9):1222-1226. [DOI] [PubMed] [Google Scholar]
- 28.Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006;117(6):e1263-e1271. [DOI] [PubMed] [Google Scholar]
- 29.Haring RS, Canner JK, Haider AH, Schneider EB. Ocular injury in the United States: emergency department visits from 2006-2011. Injury. 2016;47(1):104-108. [DOI] [PubMed] [Google Scholar]
- 30.McGwin G Jr, Hall TA, Xie A, Owsley C. Trends in eye injury in the United States, 1992-2001. Invest Ophthalmol Vis Sci. 2006;47(2):521-527. [DOI] [PubMed] [Google Scholar]
- 31.Smith D, Wrenn K, Stack LB. The epidemiology and diagnosis of penetrating eye injuries. Acad Emerg Med. 2002;9(3):209-213. [DOI] [PubMed] [Google Scholar]
- 32.Garcia TA, McGetrick BA, Janik JS. Ocular injuries in children after major trauma. J Pediatr Ophthalmol Strabismus. 2005;42(6):349-354. [DOI] [PubMed] [Google Scholar]
- 33.Garcia TA, McGetrick BA, Janik JS. Spectrum of ocular injuries in children with major trauma. J Trauma. 2005;59(1):169-174. [DOI] [PubMed] [Google Scholar]
- 34.Scruggs D, Scruggs R, Stukenborg G, Netland PA, Calland JF. Ocular injuries in trauma patients: an analysis of 28,340 trauma admissions in the 2003-2007 National Trauma Data Bank National Sample Program. J Trauma Acute Care Surg. 2012;73(5):1308-1312. [DOI] [PubMed] [Google Scholar]
- 35.US Centers for Disease Control and Prevention. Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin. https://wonder.cdc.gov/bridged-race-v2014.html. Accessed March 9, 2018.
- 36.United States Census Bureau . United States population growth by region 2016. https://www.census.gov/popclock/data_tables.php?component=growth. Accessed March 9, 2018.
- 37.Owens PL, Mutter R. Emergency department visits related to eye injuries, 2008: statistical brief #112. In: Healthcare Cost and Utilization Project Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 38.Niiranen M, Raivio I. Eye injuries in children. Br J Ophthalmol. 1981;65(6):436-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parver LM, Dannenberg AL, Blacklow B, Fowler CJ, Brechner RJ, Tielsch JM. Characteristics and causes of penetrating eye injuries reported to the National Eye Trauma System Registry, 1985-91. Public Health Rep. 1993;108(5):625-632. [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson CG, Kumar N, Billson FA, Martin F. The aetiology of perforating ocular injuries in children. Br J Ophthalmol. 2002;86(8):920-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fein J, Bogumil D, Upperman JS, Burke RV. Pediatric dog bites: a population-based profile. Inj Prev. 2018;injuryprev-2017-042621. [DOI] [PubMed] [Google Scholar]
- 42.Peden M, Oyegbite K, Ozanne-Smith J, et al. , eds. World Report on Child Injury Prevention. Geneva, Switzerland: World Health Organization Press; http://apps.who.int/iris/bitstream/handle/10665/43851/9789241563574_eng.pdf;jsessionid=16A95598705BDCF7DD451E9ECE9BA284?sequence=1. Accessed May 1, 2018. [PubMed] [Google Scholar]
- 43.Schwebel DC, Evans WD, Hoeffler SE, et al. Unintentional child poisoning risk: a review of causal factors and prevention studies. Child Health Care. 2017;46(2):109-130. doi: 10.1080/02739615.2015.1124775 [DOI] [Google Scholar]
- 44.Bykowski MR, Shakir S, Naran S, et al. Pediatric dog bite prevention: are we barking up the wrong tree or just not barking loud enough? [published online April 11, 2017]. Pediatr Emerg Care. [DOI] [PubMed] [Google Scholar]
- 45.Shuler CM, DeBess EE, Lapidus JA, Hedberg K. Canine and human factors related to dog bite injuries. J Am Vet Med Assoc. 2008;232(4):542-546. [DOI] [PubMed] [Google Scholar]
- 46.The Humane Society of the United States . Pets by the numbers. https://www.animalsheltering.org/page/pets-by-the-numbers. Accessed March 29, 2018.
- 47.National Council of Youth Sports . Report on trends and participation in organized youth sports. http://www.ncys.org/pdfs/2008/2008-ncys-market-research-report.pdf. Accessed March 26, 2018.
- 48.Prevent Blindness . Recommended sports eye protectors. https://www.preventblindness.org/recommended-sports-eye-protectors. Accessed March 21, 2018.
- 49.Hoskin AK, Philip SS, Yardley AM, Mackey DA. Eye injury prevention for the pediatric population. Asia Pac J Ophthalmol (Phila). 2016;5(3):202-211. [DOI] [PubMed] [Google Scholar]
- 50.Harrison A, Telander DG. Eye injuries in the young athlete: a case-based approach. Pediatr Ann. 2002;31(1):33-40. [DOI] [PubMed] [Google Scholar]
- 51.Kriz PK, Comstock RD, Zurakowski D, Almquist JL, Collins CL, d’Hemecourt PA. Effectiveness of protective eyewear in reducing eye injuries among high school field hockey players. Pediatrics. 2012;130(6):1069-1075. [DOI] [PubMed] [Google Scholar]
- 52.Lincoln AE, Caswell SV, Almquist JL, et al. Effectiveness of the women’s lacrosse protective eyewear mandate in the reduction of eye injuries. Am J Sports Med. 2012;40(3):611-614. [DOI] [PubMed] [Google Scholar]
- 53.National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention . Trends in the prevalence of physical activity and sedentary behaviors national YRBS: 1991-2015. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2015_us_physical_trend_yrbs.pdf. Accessed March 29, 2018.
- 54.The Policy Surveillance Program. Child car seat safety laws. http://lawatlas.org/datasets/child-restraint. Accessed March 20, 2018.
- 55.Christoffel T, Christoffel K. Nonpowder firearm injuries: whose job is it to protect children? Am J Public Health. 1987;77(6):735-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Giffords Law Center to Prevent Gun Violence . Regulating guns in America: a comprehensive analysis of gun law nationwide. http://lawcenter.giffords.org/wp-content/uploads/2014/10/RGIA-For-Web.pdf. Accessed March 20, 2018.
- 57.Simonetti JA, Rowhani-Rahbar A, Mills B, Young B, Rivara FP. State firearm legislation and nonfatal firearm injuries. Am J Public Health. 2015;105(8):1703-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Miller KN, Collins CL, Chounthirath T, Smith GA. Pediatric sports- and recreation-related eye injuries treated in US emergency departments. Pediatrics. 2018;141(2):e20173083. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. International Classification of Diseases, Ninth Revision, Clinical Modification Diagnosis Codes Used to Identify Acute Ocular Injury
eTable 2. International Classification of Diseases, Ninth Revision, Clinical Modification External-Cause-of-Injury Codes Used to Classify Mechanism of Injury
eTable 3. Mechanism of Injury Categories and Hierarchy
eTable 4. Stratification of Acute Ocular Injury International Classification of Diseases, Ninth Revision, Clinical Modification Diagnosis Codes by Risk of Vision Loss
eTable 5. Mechanisms of Pediatric Acute Ocular Injuries by Risk of Vision Loss, National Estimates, NEDS 2006-2014
eTable 6. Mechanisms of Pediatric Acute Ocular Injuries by Age Group, National Estimates, NEDS 2006-2014