Key Points
Question
What is the incidence of myopia and high myopia among school-aged students in China?
Findings
In this cohort study of 4741 Chinese children, the incidence of myopia was 20% to 30% each year from grade 1 to grade 6 and from grade 7 to grade 9 based on refraction without cycloplegia.
Meanings
The incidence of myopia among Chinese students determined by refraction without cycloplegia is among the highest of any cultural or ethnic group; if confirmed with cycloplegic refraction, the findings might support earlier interventions in this population.
This cohort study assesses the incidence of myopia and high myopia in Chinese children in primary and junior high schools, based on refraction without cycloplegia.
Abstract
Importance
Myopia has reached epidemic levels among children in regions of East and Southeast Asia. High myopia is associated with myopic macular degeneration, glaucoma, and retinal detachment.
Objective
To determine the incidence of myopia and high myopia based on refraction without cycloplegia among children in primary and junior high schools in China.
Design, Setting, and Participants
This observational cohort study was completed in Guangzhou, China. It consisted of a cohort from 19 primary schools, who were followed up from 2010 to 2015, and a cohort from 22 junior high schools, who were followed up from 2010 to 2012. All schools were randomly chosen at rates proportional to the number of schools in each of the city’s 11 districts. Students with or without myopia in grade 1 (primary school) or grade 7 (junior high school) were eligible for inclusion. Data analysis occurred from February 2017 to October 2017.
Main Outcomes and Measures
Myopia was defined as a spherical equivalent refraction (SER) of −0.50 diopters (D) or less, as measured by subjective refraction without cycloplegia; high myopia was defined as a SER of −6.0 D or less. Annual incidences were defined as the proportion of participants each year found to have myopia or high myopia who did not previously have the condition. Height, weight, axial length (AL), corneal radius of curvature (CRC), and AL/CRC ratio were examined to assess if these measures were associated with future myopia or high myopia.
Results
A total of 4741 students with or without myopia in either grade 1 for the primary school cohort (mean [SD] age 7.2 [0.4] years; 932 of 1975 [47.2%] female) or grade 7 for the junior high school cohort (mean [SD] age 13.2 [0.5] years; 1254 of 2670 [47.0%] female) were included. Baseline mean (SD) SER was 0.31 (0.86) D among 1975 students in grade 1 vs −1.60 (2.00) D among 2670 students in grade 7. Baseline prevalence of myopia was 12.0% in grade 1 students (n = 237 of 1969) and 67.4% in grade 7 students (n = 1795 of 2663). The incidence of myopia was 20% to 30% each year throughout both cohorts. The incidence of high myopia was initially less than 1% in the primary school cohort (grade 1: n = 2 of 1825; 0.1% [95% CI, 0.0%-0.3%]), but incidence exceeded 2% in the junior high school cohort (in grade 9: n = 48 of 2044; 2.3% [95% CI, 1.0%-3.7%]).
Conclusions and Relevance
The incidence of myopia among Chinese students based on refraction without cycloplegia is among the highest of any cultural or ethnic group. If confirmed with cycloplegic refraction, interventions to prevent myopia onset in Chinese populations should be initiated in primary schools.
Introduction
Myopia is a leading cause of visual impairment worldwide and has reached epidemic levels in parts of East and Southeast Asia.1 Uncorrected refractive error, largely caused by myopia, affects more than 100 million people globally.2 Even when corrected, the consequences of myopia extend beyond the cost and inconvenience of spectacles and contact lenses. High myopia (≤−6.0 diopters [D]) is associated with complications that include myopic maculopathy, glaucoma, and retinal detachment, all of which lead to visual impairment.3 Additionally, socioeconomic effects of myopia on young children cannot be overstated, because the condition most commonly develops during childhood and can worsen educational outcomes.4 It is no surprise that especially in regions of high prevalence, myopia represents a growing public health concern.
While there are currently no definitive treatments for myopia, several potential interventions have exhibited promise. Randomized clinical trials using low-dose atropine eyedrops showed efficacy in slowing myopic progression over short intervals,5,6 and 2 small trials using orthokeratology lenses demonstrated modest reduction of axial elongation.7 There is also evidence that increasing time spent outdoors can be protective against myopia.8
With methods to slow myopic progression on the horizon, 2 important steps toward alleviating the global burden of myopia will be determining in which individuals to intervene and deciding the timing of intervention. Myopia can appear as early as primary school,9 and because myopia with younger onset is more likely to progress to high myopia,10 it would be valuable to prospectively identify those children most susceptible to developing either condition. Currently, assessing the likelihood of myopia and high myopia even several years into the future is still difficult, in part because of the relatively paucity of multiyear longitudinal data collected from large-scale population cohorts during childhood.11,12,13 In China, numerous studies have assessed the prevalence of myopia among schoolchildren.9,14,15,16 However, it is still unclear in this age group when exactly the transition from emmetropia or hyperopia to myopia most often occurs. Such information would be helpful to define the appropriate timing of treatments for myopia in the future.
The purpose of this study was to determine rates of incidence and progression of myopia in 2 large cohorts of Chinese schoolchildren, based on refraction without cycloplegia during either primary (grades 1-6) or junior high school (grades 7-9). Using physical and ocular measures, such as axial length (AL), corneal radius of curvature (CRC), and spherical equivalent refraction (SER), we then performed Cox proportional hazard regression analysis to evaluate if these characteristics were associated with future myopia.
Methods
Study Design
This multicohort study was conducted over a 6-year period beginning in 2010 to determine the annual rate of progression of myopia among Chinese schoolchildren. Ethics approval was obtained from the human ethics committee of the Zhongshan Ophthalmic Center and Guangzhou Ministry of Education. The study was conducted in accordance with the Declaration of Helsinki. For all participants, parental written consent was obtained prior to baseline examination.
The study examined 2 closed cohorts of students in Guangzhou, China, beginning in 2010. A primary school cohort consisted of students in grade 1 in 2010 from 19 state-operated primary schools, while a junior high school cohort enrolled students in grade 7 from 22 junior high schools. These schools were classified as health-monitoring schools by the Guangzhou Ministry of Health in 2007-2008, and as a result, they undergo annual health monitoring. They were originally selected from 711 primary and 250 junior high schools in Guangzhou in random at rates proportional to the number of schools in each of the city’s 11 districts; thus, they are thought to compose a representative sample of the city’s primary and junior high school students. Data from each cohort were collected during annual health monitoring examinations until graduation at the completion of grade 6, which occurred in 2015 for the primary school cohort and grade 9 in 2012 for the junior high school cohort. (After this point, the students graduated and were distributed to various junior or senior high schools.)
Measurements and Outcomes
Age at each examination was defined as the year difference between the participant’s date of birth and the date of the examination. Biometric data were collected during annual examinations performed at schools by trained technicians. Height and body weight were collected annually starting in 2010, with the exception of 2015, for which these data were unavailable. Participants were measured once at each visit while standing without shoes on the TZG measuring device (Yilian Technology) for height to the nearest 0.1 cm and on the Seca 899 scale (Seca) for weight to the nearest 0.1 kg. After a general examination, axial length (AL) and corneal radius of curvature (CRC) for each eye were determined by an optometrist using the IOLMaster biometer (Carl Zeiss Meditec) as the average of 5 recordings. The coefficient of variation for all biometric measurements was less than 1%. Sphere and cylinder refractive errors were determined via noncycloplegic autorefraction using an autorefractor (Topcon 8800K), followed by subjective refraction measured monocularly at a principle of maximum plus followed by cross-cylinder to locate the axis within 5° and its power within 0.25 D. Clinical data collection was performed by the same optometrists (G.S. and G.Z.) using the same equipment and protocols throughout all follow-up visits. Both the autorefractor and biometer were calibrated at the beginning of each examination session.
Spherical equivalent refraction (SER) was calculated as the sum of sphere power and half of cylinder power. Myopia was defined as a SER of −0.50 D or less, based on the Refractive Error Study in Children.17 High myopia was defined as a SER of −6.0 D or less.
Students reported to be using orthokeratology lens correction or those whose autorefraction values were deemed unreliable by the optometry staff at any visit were removed from the analysis. Participants younger than 6 years or older than 16 years, ages atypical for the first year of primary or junior high school in China, were also excluded.
For all analyses, the right eye was arbitrarily chosen to represent the individual. The annual incidence of myopia was defined to be the proportion of participants with myopia who did not have myopia in the previous year or at any earlier date. Analogously, the annual incidence of high myopia was defined to be the proportion of participants with high myopia who did not have high myopia in the previous year or at any earlier date.
Statistical Analysis
Statistical analyses were performed using Excel 2016 (Microsoft) and Prism 5.0 (GraphPad). For comparisons, t tests, Pearson χ2 test, or Pearson correlation coefficient r was applied as appropriate. Two-tailed P values were used in all analyses. To examine factors associated with incident myopia, Cox proportional hazard regression analysis was conducted on all participants who did not have myopia at baseline, with adjustment for covariates. For comparing students by height, weight, AL, CRC, and AL/CRC ratio, the reference group was defined as participants in the bottom quartile (<the 25th percentile) of the entire cohort. Cox proportional hazard regression analysis was similarly performed to explore factors associated with incident high myopia on all participants without high myopia at baseline. Data analysis occurred from February 2017 to October 2017.
Results
The study enrolled a total of 4741 students in 2010. The students were attending 19 primary and 22 junior high schools in Guangzhou, China. Twenty participants were excluded from analyses because they used orthokeratology lenses, 63 for unreliable autorefraction values, and 13 for being younger than 6 years or older than 16 years at baseline. Of the remaining 4645 students, 1975 were in grade 1 (primary school cohort), and 2670 were in grade 7 (junior high school cohort).
The primary and junior high school cohorts were followed up for 5 years (until 2015) and 2 years (until 2012), respectively, at which time graduation of the cohorts occurred. Of the 1975 primary school students included for analysis at baseline, 1835 (92.9%) were reexamined after 1 year, 1812 (91.7%) after 2 years, 1781 (90.2%) after 3 years, 1742 (88.2%) after 4 years, and 1715 (86.8%) after 5 years at the completion of primary school. Of the 2670 junior high school students included at baseline, 2349 (88.0%) were reexamined after 1 year and 2167 (81.2%) after 2 years, at the completion of junior high school.
Characteristics for each cohort at baseline and at graduation are displayed in Table 1. From 2010 to 2015, highly significant increases were observed among primary school students for height (2010: mean [SD], 123.8 [5.4] cm; 2015: 146.8 [7.3] cm; P < .001), weight (2010: mean [SD], 23.5 [4.5] kg; 2015: 38.9 (9.3) kg; P < .001), AL (2010: mean [SD]: 22.78 [0.72] mm; 2015: 24.23 [1.0] mm; P < 01), and AL/CRC ratio (2010: mean [SD], 2.93 [0.07]; 2015: 3.11 [0.13]; P < .001), as well as more negative SER value (2010: mean [SD], 0.3 [0.9] D; 2015: −1.7 [1.9] D; P < .001). Junior high school students experienced similar changes from 2010 to 2012, but these were of lesser magnitude for all the same measures (height: 2010: mean [SD], 157.6 (7.4) cm; vs 2012: 164.2 [7.9] cm; weight: 2010: mean [SD], 46.7 [10.5] kg; 2012: 53.6 (11.0) kg; AL: 2010: mean [SD], 24.16 (1.08) mm; 2012: 24.51 (1.18); AL/CRC: 2010: mean [SD], 3.10 (0.13) D; 2012: 3.14 (0.14) D; P < .001 for all). Based on noncycloplegic refraction, the prevalence increased in both cohorts of myopia and high myopia, with 69.9% of primary school students having myopia at end of grade 6 (2010: 237 of 1969 [12.0%]; 2015: 1166 of 1669 [69.9%]; P < .001) and 79.4% of junior high school students having myopia at end of grade 9 (2010: 1795 of 2663 [67.4%]; 2012: 1721 of 2167 [79.4%]; P < .001). By the completion of junior high school, 7.0% of the junior high school cohort had high myopia (2010: 84 of 2663 [3.2%]; 2012: 151 of 2167 [7.0%]; P < .001).
Table 1. Characteristics of Primary and Junior High School Cohort Participants at Baseline and on Graduation.
| Characteristic | Primary School Cohort | Junior High School Cohort | ||||
|---|---|---|---|---|---|---|
| Baseline (2010) | Graduation (2015) | P Valuea | Baseline (2010) | Graduation (2012) | P Valuea | |
| No. | 1975 | 1715 | NA | 2670 | 2167 | NA |
| Female | 932 (47.2) | 793 (46.2) | .99 | 1254 (47.0) | 1033 (47.7) | .99 |
| Age, mean (SD), y | 7.2 (0.4) | 12.2 (0.4) | <.001 | 13.2 (0.5) | 15.2 (0.5) | <.001 |
| Height, mean (SD), cm | 123.8 (5.4) | 146.8 (7.3)b | <.001 | 157.6 (7.4) | 164.2 (7.9) | <.001 |
| Weight, mean (SD), kg | 23.5 (4.5) | 38.9 (9.3)b | <.001 | 46.7 (10.5) | 53.64 (11.0) | <.001 |
| AL, mean (SD), mm | 22.78 (0.72) | 24.23 (1.04) | <.001 | 24.16 (1.08) | 24.51 (1.18) | <.001 |
| CRC, mean (SD), mm | 7.78 (0.25) | 7.80 (0.25) | .04 | 7.79 (0.25) | 7.80 (0.25) | .23 |
| AL/CRC ratio (SD) | 2.93 (0.07) | 3.11 (0.13) | 3.10 (0.13) | 3.14 (0.14) | <.001 | |
| SER, mean (SD), Dc | 0.3 (0.9) | −1.7 (1.9) | <.001 | −1.6 (2.0) | −2.4(2.3) | <.001 |
| Prevalence of myopia, No./total No. (%) [95% CI]d | 237/1969 (12.0) [10.6 to 13.5] | 1166/1669 (69.9) [67.7 to 72.1] | <.001 | 1795/2663 (67.4) [65.6 to 69.2] | 1721/2167 (79.4) [77.7 to 81.1]) | <.001 |
| Prevalence of high myopia, No./total No. (%) [95% CI]d | 4/1969 (0.2) [0.0 to 0.4] | 51/1669 (3.1) [2.2 to 3.9] | <.001 | 84/2663 (3.2) [2.5 to 3.8] | 151/2167 (7.0) [5.9 to 8.0] | <.001 |
Abbreviations: AL, axial length; CRC, corneal radius of curvature; D, diopters; NA, not applicable; SER, spherical equivalent refraction.
Determined using t test or Pearson χ2 test.
Based on measurements from 2014.
Calculated as sum of sphere power and half of cylinder power.
Right eye data only. Myopia defined as spherical equivalent refraction of −0.50 D or fewer. High myopia defined as spherical equivalent refraction of −6.0 D or fewer.
None of the characteristics in either cohort at baseline differed significantly between participants enrolled for the entire duration of the study vs those who were lost to follow-up. Baseline SER values in the primary school cohort were 0.32 D (95% CI, 0.28 to 0.36 D) in those who completed follow-up examinations vs 0.25 D (95% CI, 0.14 to 0.36 D; P = .20) in those who were lost to follow-up, and values in the junior high school cohort were −1.61 D (95% CI, −1.70 to −1.53 D) vs −1.57 D [95% CI, −1.73 to −1.40 D; P = .66), respectively, for the same groups.
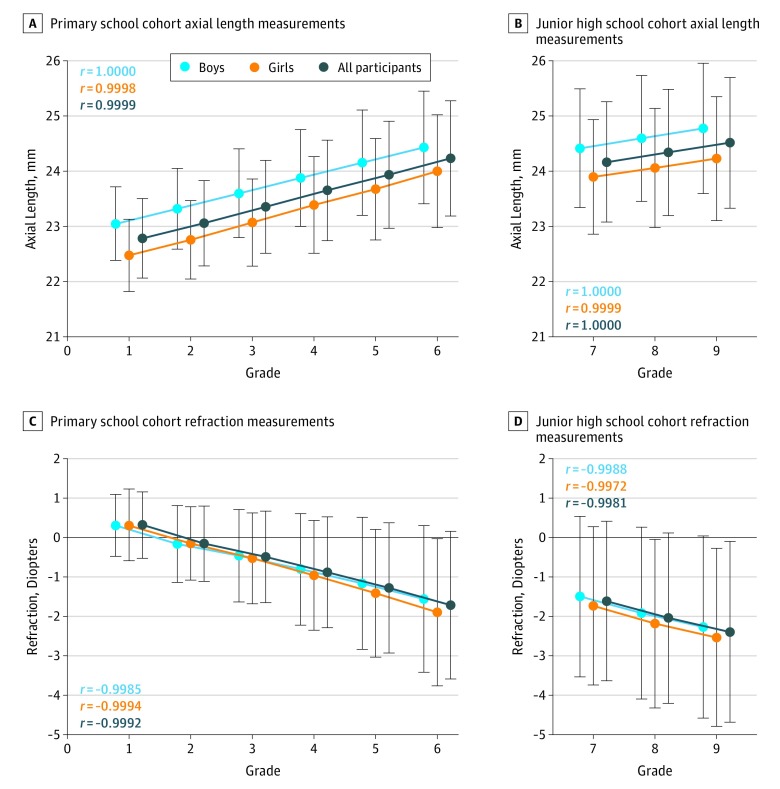
Yearly trends for AL and SER are shown in the Figure; trends for height, weight, CRC, and the AL/CRC ratio can be found in eFigure 1 and eFigure 2 in the Supplement. In both cohorts, grade showed strong showed strong positive associations with height (primary school cohort: r = 1.000; junior high school cohort: r = 1.000), weight (primary school cohort: r = 0.995; junior high school cohort: r = 0.997), AL (primary school cohort: r = 1.000; junior high school cohort: r = 1.0000), CRC (primary school cohort: r = 0.954; junior high school cohort: r = 0.947), and the AL/CRC ratio (primary school cohort: r = 1.000; junior high school cohort: r = 0.999), while SER demonstrated a strong negative association (r<−0.99 in both cohorts). Associations were statistically significant for all variables in the primary school cohort and for weight, AL, the AL/CRC ratio, and SER in the junior high school cohort.
Figure. Mean Axial Length and Refraction by School Grade.
Mean annual measures of axial length in the primary (grade 1-6) cohort (A) and junior high school (grade 7-9) cohort (B), with subanalyses by sex; mean annual measures of refraction in the primary cohort (C) and junior high school cohort (D). Error bars show SDs.
Trends were overall similar for both boys and girls. At all points, girls were found to have shorter axial length compared with boys of the same grade (grade 1: girls: mean [SD] AL, 22.48 [0.65] cm; boys: 23.05 [0.67] cm; P < .001; grade 7: girls: mean [SD] AL, 23.90 [1.04] vs boys: 24.42 [1.08]; P < .001). This was also true for CRC (grade 1: girls: mean [SD] CRD, 7.70 [0.23] vs boys: 7.85 [0.25]; P < .001; grade 1: girls: mean [SD] CRD, 7.71 [0.24] vs boys: 7.86 [0.24]; P < .001). Girls were also more likely to have worse SER than boys starting from grade 4 onward (in grade 4, girls: mean [SD] SER, −0.959 [1.391] D vs boys: −0.806 [1.417] D; P < .02).
Throughout primary and junior high school, the annual incidence of myopia based on refraction without cycloplegia was approximately 20% to 30% (Table 2). While progression of myopia was observed as early as between grades 1 and 2 (during which 307 of 1607 nonmyopic students [19.1%] developed myopia), the highest incidence rate was seen between grades 5 and 6, during which 30.2% of nonmyopic students developed myopia (140 of 463 [30.2%; 95% CI, 26.0%-34.4%]). Yearly incidence rates for high myopia were initially less than 1% for the primary school cohort (grade 1-2: 2 of 1825 students [0.1%; 95% CI, 0.0%-0.3%]) but consistently grew each year and exceeded 2% in the junior high school cohort (grade 8-9: 48 of 2044 students [2.3%; 95% CI, 1.0%-3.7%]).
Table 2. Annual Incidence of Myopia and High Myopia in Primary and Junior High School Cohorts Based on Refraction Without Cycloplegia.
| Perioda | No./Total No. (%) [95% CI] | |
|---|---|---|
| Myopiab | High Myopiab | |
| Primary school | ||
| 1-2 | 307/1607 (19.1) [17.2-21.0] | 2/1825 (0.1) [0.0-0.3] |
| 2-3 | 305/1288 (23.7) [21.4-26.0] | 4/1799 (0.2) [0.0-0.5] |
| 3-4 | 226/879 (25.7) [22.8-28.6] | 8/1770 (0.5) [0.0-0.9] |
| 4-5 | 194/674 (28.8) [25.4-32.2] | 16/1712 (0.9) [0.2-1.7] |
| 5-6 | 140/463 (30.2) [26.0-34.4] | 26/1620 (1.6) [0.5-2.7] |
| Junior high school | ||
| 7-8 | 221/759 (29.1) [25.9-32.3] | 43/2265 (1.9) [0.9-2.9] |
| 8-9 | 123/495 (24.8) [21.0-28.7] | 48/2044 (2.3) [1.0-3.7] |
Each row is the period during which the incidence of new myopia is calculated; fields display the number of students who converted from nonmyopic to myopic between the first stated grade and the second stated grade.
Myopia defined as spherical equivalent refraction of −0.50 diopters or less. High myopia defined as spherical equivalent refraction of −6.0 diopters or less.
Results from Cox proportional hazard regression analysis for incident myopia in the primary and junior high school cohorts are shown in Tables 3 and 4. After adjustment, factors that were statistically significantly associated with incident myopia among primary school students included female sex (hazard ratio [HR], 1.39 [95% CI, 1.22 to 1.58] compared with males), higher baseline AL/CRC ratio (HR, 2.13 [95% CI, 1.71 to 2.66] for the top quartile compared with the bottom quartile), and a more negative baseline SER (HR, 4.69 [95% CI, 3.46 to 6.35] for SER values between 0.5 and 0 D compared with SER values >1.0 D). For junior high school students, factors associated with incident myopia included female sex (HR, 1.33 [95% CI, 1.04 to 1.69], compared with males), higher baseline AL/CRC ratio (HR, 18.03 [95% CI, 2.16 to 150.70] for the top quartile compared with the bottom quartile), and more negative baseline SER (HR, 10.16 [95% CI, 4.97 to 20.77] for those with SER values between −0.5 and 0 D compared with those with SER values more than 0.5 D), as well as higher baseline AL (HR, 2.13 [95% CI, 1.10 to 5.06] for the top quartile compared with the bottom quartile). In both cohorts, baseline height, weight, and CRC were not found to be associated with incident myopia. Cox proportional hazard regression analysis was also attempted to evaluate factors associated with incident high myopia; however, no significant factors were identified.
Table 3. Factors Associated With Incident Myopia in Primary School Cohort by Cox Proportional Hazard Regression Analysis.
| Baseline Characteristica | No. | Adjusted Hazard Ratio (95% CI)b | P Value |
|---|---|---|---|
| Sex | |||
| Male | 908 | 1 [Reference] | |
| Female | 824 | 1.39 (1.22 to 1.58) | <.001 |
| Height, cm | |||
| <120.0 (25th Percentile) | 411 | 1 [Reference] | |
| 120.0-127.5 | 936 | 1.03 (0.87 to 1.22) | .73 |
| >127.5 (75th Percentile) | 384 | 1.02 (0.81 to 1.29) | .85 |
| Weight, kg | |||
| <20.5 (25th Percentile) | 442 | 1 [Reference] | |
| 20.5-25.3 | 871 | 1.06 (0.89 to 1.25) | .52 |
| >25.3 (75th Percentile) | 418 | 1.03 (0.83 to 1.28) | .81 |
| AL, mm | |||
| <22.31 (25th Percentile) | 457 | 1 [Reference] | |
| 22.31-23.24 | 903 | 1.11 (0.91 to 1.34) | .31 |
| >23.24 (75th Percentile) | 365 | 1.10 (0.82 to 1.48) | .51 |
| CRC, mm | |||
| <7.61 (25th Percentile) | 427 | 1 [Reference] | |
| 7.61-7.95 | 894 | 1.09 (0.90 to 1.32) | .38 |
| >7.95 (75th Percentile) | 407 | 1.13 (0.84 to 1.53) | .41 |
| AL/CRC ratio | |||
| <2.89 (25th Percentile) | 485 | 1 [Reference] | |
| 2.89-2.97 | 876 | 1.48 (1.25 to 1.74) | <.001 |
| >2.97 (75th Percentile) | 364 | 2.13 (1.71 to 2.66) | <.001 |
| SER, D | |||
| >1.0 | 169 | 1 [Reference] | |
| 0.5 to 1.0 | 580 | 1.71 (1.28 to 2.28) | <.001 |
| 0 to 0.5 | 692 | 2.66 (2.00 to 3.54) | <.001 |
| −0.5 to 0 | 291 | 4.69 (3.46 to 6.35) | <.001 |
Abbreviations: AL, axial length; CRC, corneal radius of curvature; D, diopters; SER, spherical equivalent refraction.
Percentiles correspond to baseline examination values for all primary school participants.
Hazard ratios for each group were adjusted for all other covariates.
Table 4. Factors Associated With Incident Myopia in Junior High School Cohort by Cox Proportional Hazard Regression Analysis.
| Baseline Characteristica | No. | Adjusted Hazard Ratio (95% CI)b | P Value |
|---|---|---|---|
| Sex | |||
| Male | 500 | 1 [Reference] | |
| Female | 367 | 1.33 (1.04 to 1.69) | .02 |
| Height, cm | |||
| <152.5 (25th Percentile) | 215 | 1 [Reference] | |
| 152.5-162.5 | 408 | 0.93 (0.70 to 1.25) | .64 |
| >162.5 (75th Percentile) | 195 | 0.79 (0.54 to 1.16) | .24 |
| Weight, kg | |||
| <39.9 (25th Percentile) | 215 | 1 [Reference] | |
| 39.9-51.4 | 428 | 1.14 (0.84 to 1.54) | .40 |
| >51.4 (75th Percentile) | 224 | 0.89 (0.61 to 1.31) | .56 |
| AL, mm | |||
| <23.41 (25th Percentile) | 418 | 1 [Reference] | |
| 23.41-24.87 | 407 | 1.48 (1.10 to 1.99) | .01 |
| >24.87 (75th Percentile) | 21 | 2.36 (1.10 to 5.06) | .03 |
| CRC, mm | |||
| <7.62 (25th Percentile) | 162 | 1 [Reference] | |
| 7.62-7.95 | 431 | 1.03 (0.74 to 1.45) | .85 |
| >7.95 (75th Percentile) | 244 | 0.78 (0.48 to 1.27) | .32 |
| AL/CRC ratio | |||
| <3.00 (25th Percentile) | 448 | 1 [Reference] | |
| 3.00-3.19 | 383 | 1.24 (0.95 to 1.63) | .12 |
| >3.19 (75th Percentile) | 2 | 18.03 (2.16 to 150.70) | <.01 |
| SER, D | |||
| >0.5 | 113 | 1 [Reference] | |
| 0 to 0.5 | 350 | 4.27 (2.07 to 8.80) | <.001 |
| −0.5 to 0 | 384 | 10.16 (4.97 to 20.77) | <.001 |
Abbreviations: AL, axial length; CRC, corneal radius of curvature; D, diopters; SER, spherical equivalent refraction.
Percentiles correspond to baseline examination values for all junior high school participants.
Hazard ratios for each group were adjusted for all other covariates.
eFigure 3 in the Supplement shows survival curves for incident myopia in the 2 cohorts among participants without myopia at baseline. For primary school students who were nonmyopic in grade 1, the probability of remaining nonmyopic throughout primary school was 28.9%, with a median onset of myopia after 3 years. For junior high school students who were nonmyopic in grade 7, the probability of remaining nonmyopic until grade 9 was 54.0%.
Discussion
Many studies have examined the prevalence of myopia in an racially/ethnically diverse range of populations; however, only a handful have addressed questions of myopia incidence. In the current study monitoring 2 cohorts of Chinese schoolchildren, we found that from grade 1 onward, approximately 20% to 30% of nonmyopic students newly develop myopia each year. This incidence, based on refraction without cycloplegia, is among the highest of any cultural or ethnic group and is similar to the first year of data reported by Tsai et al18 in 2016. Tsai et al18 found the annual incidence of myopia (defined as a SER value of −0.50 D or less) with cycloplegic refraction among 7-year-old to 8-year-old schoolchildren in Taipei City to be 31.7%. In contrast, this figure is much higher than what has been reported among white and multiethnic populations11,19,20 and nearly double what was previously observed in other regions of China and East Asia.21,22 Examining 7-year-old, 8-year-old, and 9-year-old children in Hong Kong, Fan et al21 in 2004 reported a 13% to 15% incidence of new myopia (defined as a SER value of −0.50 D or less) in 1 year. Likewise, in a 2002 study of 5-year-old to 12-year-old children based in Shunyi, China, a semirural area, the incidence of myopia (SER≤−0.50 D) in a period of 28 months was 14.1%.22 While variations in myopia incidence could arise from differences in geography or methodology, it should be noted that both the results in Hong Kong21 and Shunyi22 represent data collected a decade earlier than either Tsai et al18 or the present study. The higher annual incidence rates of myopia seen in our cohorts may therefore reflect recent upward trends in myopia coinciding with global urbanization.23,24
Within our cohorts, both the prevalence and severity of myopia rose throughout primary school and junior high school, with 79.4% and 7.0% of students by the end of grade 9 affected by myopia and high myopia, respectively. For high myopia, the incidence also grew with each successive grade, suggesting that many of the children who develop high myopia may do so after grade 9 or approximately age 15 years. Preventing high myopia and its associated visual pathologies remains a key challenge, and the ability to prospectively identify those individuals at greatest risk could help to determine in whom to intervene. We found that among primary school students, a SER value between 0 and −0.5 D and an AL/CRC ratio higher than the 75th percentile at baseline were the independent factors associated most strongly with incident myopia in the next 5 years. Determining factors associated with incident myopia from baseline characteristics in the junior high school cohort demonstrated analogous findings, with the greatest adjusted hazard ratios again observed for more negative baseline SER and AL/CRC ratio higher than the 75th percentile. These findings were overall consistent with prior cohort studies in the United States and Taiwan, which reported more negative baseline refractive status to be the factor associated most strongly with developing myopia,11,18 as well as cross-sectional data from the Baoshan Eye Study in Shanghai, which found measures of an AL/CRC ratio to be the more effective than AL or uncorrected visual acuity in detecting childhood myopia.25 On the other hand, despite examining large cohorts, we were unable to identify any significant factors associated at baseline with incident high myopia, in part because of the condition’s relatively low prevalence.
Limitations
Limitations of the present study should be acknowledged. Notably, refractive error was determined by noncycloplegic autorefraction followed by subjective refraction. Obtaining refractive error in the absence of cycloplegia may overestimate myopic power.26 There may also be measurement error in subjective refraction, given the nature of the method. For these 2 reasons, some participants in the study may have been erroneously classified as myopic. In addition, important factors associated with myopia including outdoor activity, near work, and parental myopia were not accounted for in this study. Without these data, the incidence of and factors associated with myopia and high myopia may have been incorrectly estimated.
As with most cohort studies, our investigation experienced loss to follow-up from the initiation of data collection in 2010 to completion in 2015. Comparing participants lost to follow-up with those who remained for all visits, baseline values for all physical and ocular characteristics were similar, including baseline refractive error; therefore, bias because of loss of follow-up should be minimal.
Considering our geographic setting in one of China’s largest cities, another possible limitation is generalizability of the study outside of urban Chinese populations, a demographic known to have one of the highest rates of myopia in the world.8,9,23 It is still unclear whether the near universality of myopia among Chinese people is primarily because of a genetic predisposition for myopia or a cultural lifestyle more associated with the condition. In a Singaporean cohort study, Saw et al27 found that new cases of myopia were twice as frequent among Chinese students compared with non-Chinese students, despite adjusting for the hereditary factor of parental myopia and the largest suspected behavioral factor of reading. Further research is needed to clarify the incidence of myopia in other regions of the world and confirm if our results are more broadly generalizable.
Conclusions
In conclusion, the data presented here update our perspective on the rapid escalation of myopia in China with implications for eye care professionals and health administrators. We found the annual incidence of myopia in a population of urban Chinese schoolchildren based on refraction without cycloplegia to range from 20% to 30% throughout primary and junior high school. While baseline measures of refractive error and AL/CRC ratio taken during grade 1 or grade 7 could help infer the onset of myopia later on, the association of these values with future high myopia was limited. Future studies using cycloplegic refraction are needed to verify the high incidence and prevalence of myopia we observed as early as grade 1. If confirmed, then interventions intent on preventing the development of myopia in Chinese children might aim to take place by the start of primary school.
eFigure 1. Mean height and weight by grade.
eFigure 2. Mean corneal radius of curvature and AL/CRC ratio by grade.
eFigure 3. Survival analysis for incident myopia by grade.
References
- 1.Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. Lancet. 2012;379(9827):1739-1748. doi: 10.1016/S0140-6736(12)60272-4 [DOI] [PubMed] [Google Scholar]
- 2.Bourne RRA, Stevens GA, White RA, et al. ; Vision Loss Expert Group . Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339-e349. doi: 10.1016/S2214-109X(13)70113-X [DOI] [PubMed] [Google Scholar]
- 3.Verhoeven VJM, Wong KT, Buitendijk GHS, Hofman A, Vingerling JR, Klaver CCW. Visual consequences of refractive errors in the general population. Ophthalmology. 2015;122(1):101-109. doi: 10.1016/j.ophtha.2014.07.030 [DOI] [PubMed] [Google Scholar]
- 4.Ma X, Zhou Z, Yi H, et al. Effect of providing free glasses on children’s educational outcomes in China: cluster randomized controlled trial. BMJ. 2014;349:g5740. doi: 10.1136/bmj.g5740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chia A, Chua W-H, Cheung Y-B, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-354. doi: 10.1016/j.ophtha.2011.07.031 [DOI] [PubMed] [Google Scholar]
- 6.Tong L, Huang XL, Koh ALT, Zhang X, Tan DTH, Chua W-H. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine. Ophthalmology. 2009;116(3):572-579. doi: 10.1016/j.ophtha.2008.10.020 [DOI] [PubMed] [Google Scholar]
- 7.Cho P, Cheung S-W. Protective role of orthokeratology in reducing risk of rapid axial elongation: a reanalysis of data from the ROMIO and TO-SEE studies. Invest Ophthalmol Vis Sci. 2017;58(3):1411-1416. doi: 10.1167/iovs.16-20594 [DOI] [PubMed] [Google Scholar]
- 8.He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142-1148. doi: 10.1001/jama.2015.10803 [DOI] [PubMed] [Google Scholar]
- 9.Guo L, Yang J, Mai J, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye (Lond). 2015;2016(30):796-804. doi: 10.1038/eye.2016.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gwiazda J, Hyman L, Dong LM, et al. ; Comet Group . Factors associated with high myopia after 7 years of follow-up in the Correction of Myopia Evaluation Trial (COMET) cohort. Ophthalmic Epidemiol. 2007;14(4):230-237. doi: 10.1080/01658100701486459 [DOI] [PubMed] [Google Scholar]
- 11.Zadnik K, Sinnott LT, Cotter SA, et al. ; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group . Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015;133(6):683-689. doi: 10.1001/jamaophthalmol.2015.0471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chua SYL, Sabanayagam C, Cheung Y-B, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-394. doi: 10.1111/opo.12305 [DOI] [PubMed] [Google Scholar]
- 13.Jones-Jordan LA, Sinnott LT, Manny RE, et al. ; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group . Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci. 2010;51(1):115-121. doi: 10.1167/iovs.08-3210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma Y, Qu X, Zhu X, et al. Age-specific prevalence of visual impairment and refractive error in children aged 3-10 years in Shanghai, China. Invest Ophthalmol Vis Sci. 2016;57(14):6188-6196. doi: 10.1167/iovs.16-20243 [DOI] [PubMed] [Google Scholar]
- 15.He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114(2):374-382. doi: 10.1016/j.ophtha.2006.08.020 [DOI] [PubMed] [Google Scholar]
- 16.Guo K, Yang DY, Wang Y, et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert Children Eye Study. Invest Ophthalmol Vis Sci. 2015;56(3):1769-1774. doi: 10.1167/iovs.14-15737 [DOI] [PubMed] [Google Scholar]
- 17.Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive Error Study in Children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129(4):421-426. doi: 10.1016/S0002-9394(99)00455-9 [DOI] [PubMed] [Google Scholar]
- 18.Tsai D-C, Fang S-Y, Huang N, et al. Myopia development among young schoolchildren: the myopia investigation study in Taipei. Invest Ophthalmol Vis Sci. 2016;57(15):6852-6860. doi: 10.1167/iovs.16-20288 [DOI] [PubMed] [Google Scholar]
- 19.French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120(7):1482-1491. doi: 10.1016/j.ophtha.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 20.McCullough SJ, O’Donoghue L, Saunders KJ. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PLoS One. 2016;11(1):e0146332. doi: 10.1371/journal.pone.0146332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fan DSP, Lam DSC, Lam RF, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45(4):1071-1075. doi: 10.1167/iovs.03-1151 [DOI] [PubMed] [Google Scholar]
- 22.Zhao J, Mao J, Luo R, Li F, Munoz SR, Ellwein LB. The progression of refractive error in school-age children: Shunyi district, China. Am J Ophthalmol. 2002;134(5):735-743. doi: 10.1016/S0002-9394(02)01689-6 [DOI] [PubMed] [Google Scholar]
- 23.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042. doi: 10.1016/j.ophtha.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 24.Ip JM, Rose KA, Morgan IG, Burlutsky G, Mitchell P. Myopia and the urban environment: findings in a sample of 12-year-old Australian school children. Invest Ophthalmol Vis Sci. 2008;49(9):3858-3863. doi: 10.1167/iovs.07-1451 [DOI] [PubMed] [Google Scholar]
- 25.He X, Zou H, Lu L, et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS One. 2015;10(2):e0111766. doi: 10.1371/journal.pone.0111766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hashemi H, Khabazkhoob M, Asharlous A, et al. Cycloplegic autorefraction versus subjective refraction: the Tehran Eye Study. Br J Ophthalmol. 2016;100(8):1122-1127. doi: 10.1136/bjophthalmol-2015-307871 [DOI] [PubMed] [Google Scholar]
- 27.Saw S-M, Tong L, Chua W-H, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005;46(1):51-57. doi: 10.1167/iovs.04-0565 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Mean height and weight by grade.
eFigure 2. Mean corneal radius of curvature and AL/CRC ratio by grade.
eFigure 3. Survival analysis for incident myopia by grade.