Key Points
Question
Does an educational intervention designed to inform primiparous mothers about responsive parenting behaviors affect weight outcomes of children at age 3 years?
Findings
In this randomized clinical trial that included 279 mother-child dyads, a responsive parenting intervention significantly reduced body mass index z scores compared with controls (−0.13 vs 0.15, respectively) at age 3 years.
Meaning
Among primiparous mother-child dyads, an educational intervention that provided instruction about responsive parenting behaviors improved body mass index z score at age 3 years compared with a control intervention.
Abstract
Importance
Rapid growth and elevated weight status in early childhood increase risk for later obesity, but interventions that improve growth trajectories are lacking.
Objective
To examine effects of a responsive parenting intervention designed to promote developmentally appropriate, prompt, and contingent responses to a child’s needs on weight outcomes at 3 years.
Design, Setting, and Participants
A single-center randomized clinical trial comparing a responsive parenting intervention designed to prevent childhood obesity vs a home safety intervention (control) among 279 primiparous mother-child dyads (responsive parenting group, 140; control group, 139) who enrolled and completed the first home visit from January 2012 through March 2014 with follow-up to age 3 years (completed by April 2017).
Interventions
Research nurses conducted 4 home visits during infancy and annual research center visits. The responsive parenting curriculum focused on feeding, sleep, interactive play, and emotion regulation. The control curriculum focused on safety.
Main Outcomes and Measures
The primary outcome was body mass index (BMI) z score at 3 years (z score of 0 represents the population mean; 1 and −1 represent 1 SD above and below the mean, respectively). BMI percentile at 3 years was designated previously as the primary outcome. Secondary outcomes included the prevalence of overweight (BMI ≥85th percentile and <95th percentile) and obesity (BMI ≥95th percentile) at 3 years.
Results
Among 291 mother-child dyads randomized, 279 received the first home visit and were included in the primary analysis. 232 mother-child dyads (83.2%) completed the 3-year trial. Mean age of the mothers was 28.7 years; 86% were white and 86% were privately insured. At age 3 years, children in the responsive parenting group had a lower mean BMI z score (−0.13 in the responsive parenting group vs 0.15 in the control group; absolute difference, −0.28 [95% CI, −0.53 to −0.01]; P = .04). Mean BMI percentiles did not differ significantly (47th in the responsive parenting group vs 54th in the control group; reduction in mean BMI percentiles of 6.9 percentile points [95% CI, −14.5 to 0.6]; P = .07). Of 116 children in the responsive parenting group, 13 (11.2%) were overweight vs 23 (19.8%) of 116 children in the control group (absolute difference, −8.6% [95% CI, −17.9% to 0.0%]; odds ratio [OR], 0.51 [95% CI, 0.25 to 1.06]; P = .07); 3 children (2.6%) in the responsive parenting group were obese vs 9 children (7.8%) in the control group (absolute difference, −5.2% [95% CI, −10.8% to 0.0%]; OR, 0.32 [95% CI, 0.08 to 1.20]; P = .09).
Conclusions and Relevance
Among primiparous mother-child dyads, a responsive parenting intervention initiated in early infancy compared with a control intervention resulted in a modest reduction in BMI z scores at age 3 years, but no significant difference in BMI percentile. Further research is needed to determine the long-term effect of the intervention and assess its efficacy in other settings.
Trial Registration
ClinicalTrials.gov Identifier: NCT01167270
This randomized clinical trial compares the effects of a responsive parenting intervention designed to promote developmentally appropriate, prompt, and contingent responses to an infant’s needs vs a home safety intervention on child weight outcomes at 3 years.
Introduction
Infancy is a critical period of developmental plasticity with long-lasting metabolic and behavioral consequences.1 Data demonstrating associations between overweight and rapid weight gain during infancy with increased risk for obesity2,3 and comorbidities3,4 later in the lifecourse support this concept. These findings and US data from 2011 to 2016 indicating that 23% of children aged 2 to 5 years are overweight5 and 9% to 14% are obese6,7 underscore the need for research on preventing obesity beginning in infancy. To date, research efforts to prevent rapid infant weight gain and early life overweight have had limited success,8 but educational strategies using a responsive parenting framework have shown promise at improving infant behaviors that contribute to later obesity.9 Responsive parenting is defined as developmentally appropriate, prompt, and contingent parenting responses to a child’s needs,10 and it promotes a range of positive adaptive outcomes in children.11
The Intervention Nurses Start Infants Growing on Health Trajectories (INSIGHT) study was a randomized clinical trial focused on reducing rapid weight gain in infancy and establishing healthy growth trajectories during early life by providing first-time mothers with caregiving guidance within a responsive parenting framework.12 Previous reports from the study have demonstrated that the responsive parenting intervention compared with a home safety intervention (control) reduced rapid infant weight gain, reduced prevalence of overweight at age 1 year,13 improved infant sleep and sleep-related behaviors,14 and improved adherence to current dietary guidance.15 This report focuses on the primary outcome of the trial: weight status at age 3 years.
Methods
Participants
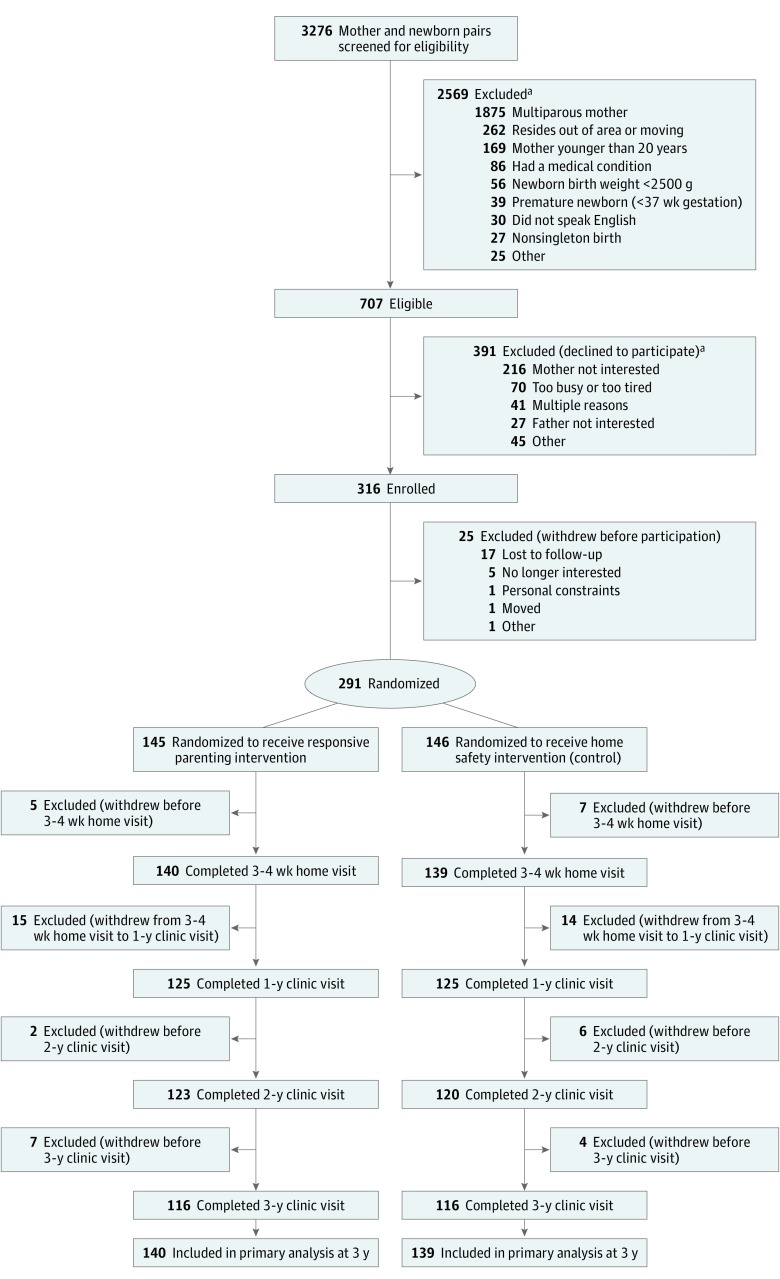
This study was approved by the Human Subjects Protection Office of the Penn State College of Medicine. All participating mothers provided written informed consent. Mothers and their newborns were recruited in-person by research staff shortly after delivery from 1 maternity ward (Penn State Milton S. Hershey Medical Center, Hershey, Pennsylvania) (Figure 1). The enrollment period spanned January 2012 to March 2014; the final participant’s 3-year study visit occurred in April 2017. Major eligibility criteria were full-term (≥37 weeks’ gestation), singleton newborns delivered to English-speaking, primiparous mothers 20 years and older. Infants born less than 2500 g were excluded. More details have been published elsewhere,12,13 and the study protocol is available in Supplement 1.
Figure 1. Flow of Primiparous Mother-Child Dyads Through the Study.
aPotential participants may have had multiple exclusions.
Interventions
Participants were randomized by research staff to the responsive parenting or home safety intervention (control) group using a secure Microsoft Excel application 10 to 14 days after delivery. The randomization scheme used permuted blocks of 6, and stratified on birth weight for gestational age16 (<50th percentile or ≥50th percentile) and intended feeding mode (breastfeeding or formula feeding).
The responsive parenting intervention guidance advised parents on how to respond to their child’s needs across 4 behavioral states: drowsy, sleeping, fussy, and alert (ie, interactive play and feeding).12 Following randomization, mothers in the responsive parenting group were mailed initial intervention content to be reviewed and practiced prior to the first study visit. These materials included a DVD demonstrating infant soothing techniques,17 a CD with white noise tracks, and handouts on infant stomach size, feeding guidance, lactation support, and postpartum depression. At study visits, age-appropriate sleep instructions promoted longer sleep duration, including putting infants to bed drowsy but awake, avoiding feeding infants to sleep, and anticipating and responding to night awakening. The emotion regulation component encouraged parents to use alternatives to feeding to calm fussy but not hungry infants. Parents were later instructed on establishing routines and expectations, and setting limits, rules, and consequences. The feeding component taught parents to recognize hunger and satiety cues, provide age appropriate portion sizes, and to feed in response to hunger only and not as a reward, punishment, or soothing strategy for a distressed but not hungry child. The responsive parenting guidance emphasized feeding a child exhibiting signs of hunger and to use infant fullness signals to determine when to stop feeding. Guidance during the introduction of solid foods included use of repeated exposure to promote acceptance of healthy foods, the importance of modeling healthy eating behaviors, and the concept of shared feeding responsibility, which recognizes the parent’s role is to provide healthy choices while the child’s role is to determine how much and whether to eat. The interactive play component focused on developmentally appropriate physical activities beginning with daily prone position playtime and later with outdoor play. Limit-setting specific to screen time was discussed. Growth chart education instructed parents on typical patterns of child growth and weight gain using color-coded growth charts, providing feedback based on the individual child’s anthropometrics.
The control group received a home safety intervention that was dose-matched to ensure equivalent time and intensity.12 For example, early visits included developmentally relevant information on prevention of sudden infant death syndrome for sleep, breast milk storage and formula preparation for feeding, and safe bathing of infants as part of the drowsy time guidance, among others.
To maintain the integrity of these behavioral interventions, scripted manuals were used for training, and fidelity was monitored.13 Measurement of fidelity and maternal acceptance of the intervention are described in the eMethods in Supplement 2.
Research nurses were trained in both responsive parenting and safety interventions, and generally an individual nurse completed all study visits for each family. The intervention was delivered via mailed instructions at 2 weeks, at home visits at child age 3 to 4, 16, 28, and 40 weeks, research center visits at 1 and 2 years, and through telephone contacts at 18 and 30 months. The final study visit at age 3 years did not include any intervention.
Measures
Background Characteristics
Family demographic information was collected at enrollment. Self-identified race/ethnicity was collected using fixed categories consistent with National Institutes of Health enrollment tables as required by the funding agency. Maternal age, prepregnancy weight, and infant gestational age were extracted from medical records.
Anthropometrics
Trained research staff obtained all study measurements except birth weight and length, which were obtained from medical records. At the 1-, 2-, and 3-year visits measurements were performed by staff blinded to study group. At all study time points, weight was measured in duplicate to the nearest 0.1 kg using an electronic scale (Seca 354 or Seca 874; Seca). Lengths and heights were measured to the nearest 0.1 cm. Additional measurements were taken until 2 measurements differed by no more than 0.1 kg or 1 cm, and means of the measurements were used for analysis.
At visits before age 2 years, length was measured using a recumbent length board (Shorr Productions). At 2 and 3 years, standing heights for children were measured with a stadiometer (Seca 216; Seca). Child body mass index (BMI; calculated as weight in kilograms divided by height in meters squared)-for-age was converted to percentiles and z scores using the 2000 Centers for Disease Control and Prevention growth reference for children 2 years and older.18 At 2 and 3 years, BMI at or above the 85th percentile but below the 95th percentile was defined as overweight, and BMI at or above the 95th percentile was defined as obese.19
Maternal height was measured (n = 256) using a stadiometer (Seca 240; Seca) or obtained from medical records (n = 23). Maternal prepregnancy BMI was calculated as prepregnancy weight (kg) divided by height (m2).
Growth-Related Adverse Events
A data and safety monitoring plan was developed to monitor for insufficient growth using 2 definitions: (1) weight-for-age <5th percentile and (2) downward crossing of 2 major growth chart percentile lines between study visits.
Outcomes
This trial was designed in 2010; the primary outcome listed in the protocol and trial registration in 2010 was BMI percentile at age 3 years, although it was powered on BMI z score. The primary outcome was not changed in the protocol or trial registration, but in 2012 the study team recognized the use of imprecise terminology for the primary outcome. Therefore, the published methods article in 2014 clarified the primary outcome to be BMI z score at age 3 years12 prior to any analysis of data. This decision reflected the fact that percentiles are not normally distributed, and they should be converted to z scores, which are normally distributed, before using parametric analyses such as analysis of variance (ANOVA) that assume normal distribution.20 Both BMI z scores and percentiles are reported at age 3 years. A BMI z score of 0 represents the population mean, whereas a BMI z score of 1 and −1 represent 1 SD above and below the mean, respectively. Secondary outcomes include the proportion overweight or obese at 3 years; BMI z scores, BMI percentiles, proportion overweight and obese at 2 years; and the proportion with accelerated weight gain (0.67 difference in BMI z score) between numerous study intervals (eg, birth to 4 months, birth to 1 year). The a priori analysis plan included a repeated measures analysis of the treatment effect from birth to 1 year; analysis to age 3 is included as a post hoc analysis. We have previously reported the secondary outcomes of conditional weight gain during the first 6 months and weight-for-length percentile at 1 year.13 Post hoc analyses of conditional weight gain and weight outcomes at 3 years are reported. Additional study outcomes related to infant sleep, feeding, diet, temperament, and parent feeding style are not reported here.
Sample Size and Power Calculation
The study was powered to detect a 0.67 difference in BMI z score (the difference between growth chart major percentile lines)18 at 3 years at 90% power, 5% type I error rate, with an anticipated attrition rate of 30%. This difference has often been used in epidemiologic studies of early growth.2 However, a 2017 statement from the US Preventive Services Task Force indicated that a BMI z score reduction in the range of 0.20 to 0.25 is a suitable threshold for clinically important change.21 Given the attrition rate that occurred prior to the first visit in our pilot trial, the 3- to 4-week time point was chosen to establish the study cohort as opposed to at enrollment or randomization.22 Two hundred seventy-six participants were required to complete the first study home visit at age 3 to 4 weeks. The final cohort size of 279 resulted from participants in the “run-in” phase of the trial when the sample size goal was met.
Statistical Analysis
As determined prior to study onset, all analyses followed modified intention-to-treat principles, including randomized participants who received the first study home visit. For cross-sectional analyses of weight outcomes at ages 2 years and 3 years, ANOVAs estimated the effects of intervention group on BMI z score. Logistic regression was used to compare intervention effects on the dichotomous outcomes of overweight and obesity. To evaluate the treatment effect across 7 postrandomization visits, we fit a mixed-model repeated measures ANOVA, with visit and treatment group as within and between factors. Two-factor ANOVA was used for post hoc analyses of intervention effect moderation by child sex and by intended feeding mode. To address missing data for those who did not complete the trial, an iterative Markov chain Monte Carlo imputation analysis of BMI z score was performed as described in the eMethods in Supplement 2. Conditional weight gain from birth to 28 weeks was calculated and the association with weight outcomes at 3 years examined as described in the eMethods in Supplement 2.13 Statistical significance was defined as a P value less than .05, and all tests of the intervention were 2-sided. The analysis plan did not adjust for multiple comparisons, so secondary outcomes should be viewed as exploratory. Data were analyzed using SAS (SAS Institute), version 9.4.
Results
Of 316 consenting mother-child dyads, 291 were randomized; 279 dyads completed the first home visit at 3 to 4 weeks after birth and were considered the study cohort for outcomes per the study protocol (Figure 1). Among those who received the first home visit, study groups were similar on demographic and baseline variables including birth weight, length, and BMI (Table). Mothers were predominantly white (86%), non-Hispanic (93%), married (75%), working full-time (72%) at enrollment, college educated (62%), and privately insured (86%). Breastfeeding rates were similar at randomization and subsequent assessment points (eTable 1 in Supplement 2). Forty-seven dyads completed the first home visit but withdrew from the trial by age 3 years; attrition did not vary by study group (P = .98), but was significantly more likely to occur for dyads with mothers who were Hispanic, unmarried, younger, and had a high school education or less (eTable 2 in Supplement 2).
Table. Mother and Child Characteristics Among Those Completing the First Nurse Home Visit (N = 279)a.
| No. (%) | ||
|---|---|---|
| Responsive Parenting Group (n = 140) | Control Group (n = 139) | |
| Neonates and Infants | ||
| Boys | 75 (54) | 69 (50) |
| Gestational age, mean (SD), wk | 39.6 (1.2) | 39.5 (1.1) |
| Birth weight, mean (SD), kg | 3.40 (0.43) | 3.46 (0.43) |
| Birth length, mean (SD), cm | 50.9 (2.4) | 51.0 (2.1) |
| Birth BMI, mean (SD) | 13.1 (1.2) | 13.3 (1.3) |
| Mothers | ||
| Age, mean (SD), y | 28.7 (4.6) | 28.7 (4.9) |
| Prepregnancy BMI, mean (SD) | 25.5 (5.0) | 25.3 (5.6) |
| Gestational weight gain, mean (SD), kg | 15.6 (6.4) | 15.0 (6.0) |
| Diabetes during pregnancy | 6 (4.3) | 13 (9.4) |
| Smoked during pregnancy | 12 (8.6) | 9 (6.5) |
| Hispanic ethnicity | 10 (7.1) | 9 (6.5) |
| Race | ||
| White | 122 (87.1) | 127 (91.4) |
| Black | 10 (7.1) | 7 (5.0) |
| Asian | 5 (3.6) | 4 (2.9) |
| Native Hawaiian or Pacific Islander | 1 (0.7) | 0 |
| Other | 2 (1.4) | 1 (0.7) |
| Marital status | ||
| Married | 102 (72.9) | 108 (77.7) |
| Not married, living with partner | 25 (17.9) | 19 (13.7) |
| Single | 12 (8.6) | 12 (8.6) |
| Divorced or separated | 1 (0.7) | 0 |
| Education | ||
| ≤High school graduate | 16 (11.4) | 16 (11.5) |
| Some college | 37 (26.4) | 36 (25.9) |
| College graduate | 48 (34.3) | 52 (37.4) |
| ≥Graduate degree | 39 (27.9) | 35 (25.2) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
First nurse home visit occurred at child age 3 to 4 weeks.
Primary Outcomes of BMI and Weight at Age 3 Years
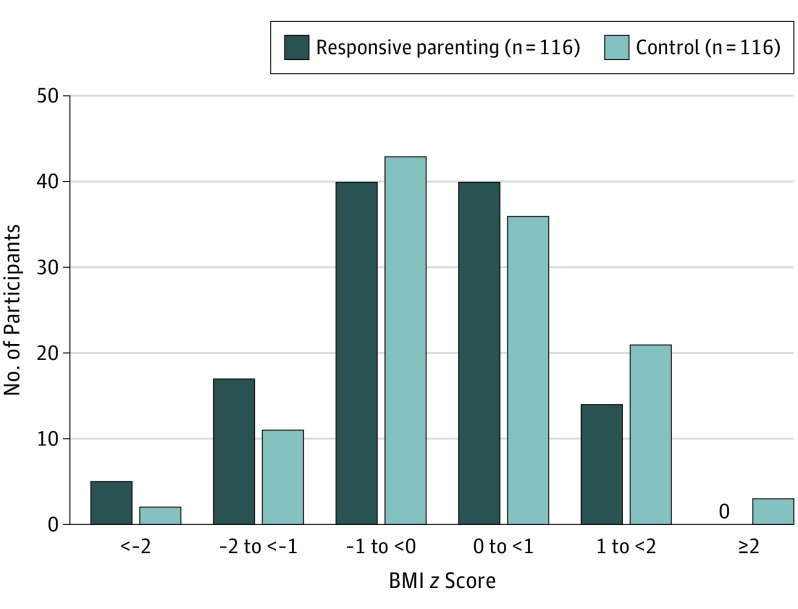
For the primary outcome at 3 years, the responsive parenting group had a lower mean BMI z score than controls (−0.13 in the responsive parenting group vs 0.15 in the control group; absolute difference, −0.28 [95% CI, −0.53 to −0.01]; P = .04) (Figure 2). Mean BMI percentiles did not differ significantly (47th in the responsive parenting group vs 54th in the control group; reduction in mean BMI percentiles of 6.9 percentile points [95% CI, −14.5 to 0.6]; P = .07).
Figure 2. Distribution of BMI z Score at Age 3 Years Among Children Receiving Responsive Parenting vs Home Safety (Control) Interventionsa.
BMI indicates body mass index (calculated as weight in kilograms divided by height in meters squared).
aMean BMI z scores: −0.13 for responsive parenting vs 0.15 for control; absolute difference, −0.28 (95% CI, −0.53 to −0.01); analysis of variance P = .04.
Secondary Outcomes
For secondary outcomes, among 116 children in the responsive parenting group, 13 (11.2%) were overweight at 3 years vs 23 children (19.8%) of 116 in the control group (absolute difference, −8.6% [95% CI, −17.9% to 0.0%]; P = .07); 3 children (2.6%) in the responsive parenting group were obese vs 9 children (7.8%) in the control group (absolute difference, −5.2% [95% CI, −10.8% to 0.0%]; P = .08). The odds ratios (ORs) that children in the responsive parenting group would be overweight or obese at age 3 years compared with controls were 0.51 (95% CI, 0.25 to 1.06; P = .07) and 0.32 (95% CI, 0.08 to 1.20; P = .09).
At age 2 years, the mean BMI z score was −0.09 for the responsive parenting group compared with 0.11 for the control group (absolute difference, −0.21 [95% CI, −0.65 to 0.06]; P = .10). Mean BMI percentiles did not differ significantly (48th in the responsive parenting group vs 52nd in the control group; reduction in mean BMI percentiles of 4.2 percentile points [95% CI, −11.7 to 3.2]; P = .26). Among 123 children in the responsive parenting group, 14 (11.4%) were overweight at age 2 years vs 25 children (20.8%) of 120 in the control group (absolute difference, −9.4% [95% CI, −18.6% to −0.03%]; P = .04); 1 child (0.8%) in the responsive parenting group was obese compared with 10 children (8.3%) in the control group (absolute difference, −7.5% [95% CI, −12.7% to −2.3%; P = .005). The ORs that children in the responsive parenting group would be overweight or obese at age 2 years compared with controls were 0.49 (95% CI, 0.24 to 0.99; P = .048) and 0.09 (95% CI, 0.01 to 0.72; P = .02).
None of the prespecified secondary outcomes of accelerated weight gain at various intervals using the definition of 0.67 z score change were statistically significant (eResults in Supplement 2).
Post Hoc Outcomes and Sensitivity Analyses
Results using multiple imputation for the primary outcome, BMI z score at 3 years, were similar to the main analysis (eTables 3 and 4 in Supplement 2).
A post hoc analysis with sex as a moderator of the treatment effect on BMI z score at 3 years indicated a significant interaction (F1,228 = 4.2; P = .04) with a larger effect for girls. The estimated mean responsive parenting group treatment effect on BMI z score for girls was −0.55 (95% CI, −0.91 to −0.19) and for boys was −0.01 (95% CI, −0.37 to 0.35). A post hoc analysis with intended feeding mode (breastfeeding or formula feeding) as a moderator of the treatment effect on BMI z score indicated no significant interaction (F1,228 = 0.7; P = .42).
The post hoc analysis with sex as a moderator on the treatment effect on BMI z score at 2 years indicated no significant interaction (F1,239 = 2.5; P = .14). The estimated mean treatment effect on BMI z score for girls was −0.41 (95% CI, −0.77 to −0.05) and for boys was −0.03 (95% CI, −0.39 to 0.33).
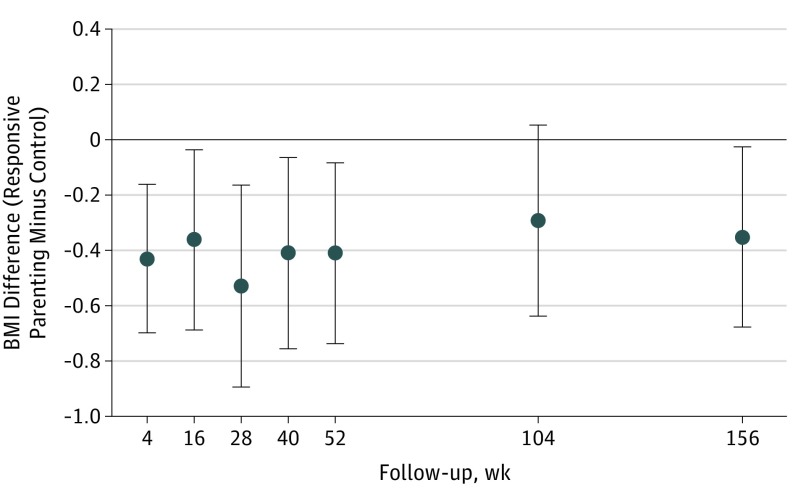
The effect of the responsive parenting intervention on BMI over the entire intervention period was statistically significant (F1,277 = 12.44; P < .001). The main effect across the 7 measurement time points in the trial (Figure 3) demonstrated lower values for the responsive parenting group with a mean BMI difference of −0.43 (95% CI, −0.67 to −0.19). Conditional weight gain between birth and 28 weeks was positively related to BMI z score, overweight, and obesity at 3 years (eResults in Supplement 2).
Figure 3. Mean Difference in BMI Between Children Receiving Responsive Parenting vs Home Safety (Control) Interventions at Each Study Assessment Pointa.
BMI indicates body mass index (calculated as weight in kilograms divided by height in meters squared). Error bars indicate 95% CIs. Data are presented as BMI units.
aResponsive parenting intervention began following randomization at 10 to 14 days.
Fidelity and maternal acceptance of the intervention were high (eResults in Supplement 2).
Growth-Related Adverse Events
Twenty-five growth-related adverse events were detected during the study period with no significant differences by study group. Seventeen growth-related adverse events were for weight-for-age below the 5th percentile (11 children in the responsive parenting group vs 6 children in the control group) and 8 were for downward crossing of 2 major percentile lines (3 children in the responsive parenting group vs 5 children in the control group).
Discussion
A responsive parenting educational intervention designed for the primary prevention of obesity beginning shortly after birth resulted in a reduction in BMI z scores at age 3 years. Differences between study groups were modest, not all study outcomes achieved statistical significance (such as BMI percentiles and proportion overweight and obese at 3 years), and the pattern of significant results from age 2 to 3 years varied. However, the direction of the differences consistently favored the responsive parenting intervention group.
The absolute z score difference of 0.28 that occurred between groups in this trial is less than the prespecified clinically important difference of 0.67 commonly used in evaluating associations with later morbidity in epidemiologic studies.2 The corresponding mean BMI percentile difference (47th in the responsive parenting group vs 54th in the control group) is relatively small and could call into question the clinical significance of the effect of the responsive parenting intervention. However, the 0.28 difference in BMI z score is greater than the 0.20 to 0.25 difference suggested by the US Preventive Services Task Force as a threshold for a clinically important difference.21 Furthermore, when reviewed against population-level changes over the past 3 decades,6 such a difference, if applied broadly, would be meaningful particularly given that weight status at 3 years has been established as a predictor of later obesity and its comorbidities.23,24 Additionally, there were no significant group differences in adverse events in this trial, which is important because early intervention trials for obesity prevention must balance the aim of promoting healthy growth while simultaneously not increasing rates of failure to thrive.
Three other obesity prevention trials beginning during infancy have shown initial success through age 1 to 2 years,22,25,26 but primary outcome findings of this trial reveal the most sustained effects on BMI associated with an early parenting educational intervention. The protective effect of the responsive parenting intervention on rapid infant weight gain was previously reported,13 and the intervention was associated with a significantly reduced BMI at 6 of 7 study assessment points including the primary end point at 3 years. This suggests that it may be possible for early effects to be maintained longitudinally.
The responsive parenting framework used for the intervention was expected to affect multiple domains of child behavior including feeding, sleep, and activity12 while promoting the development of children’s self-regulation.27,28,29,30 Positive parenting during infancy has been associated with greater regulation of negative emotions during the toddler years, which has been shown to predict lower BMI at age 3 years.31 The UK Millennium Cohort Study extended these associations by demonstrating that emotional self-regulation at age 3 is an independent predictor of obesity at age 11 years.32
The post hoc analysis that revealed sex as a moderator of the treatment effect at age 3 years is hypothesis generating. It is possible that parenting in response to the intervention differed by child sex, and this question will be investigated with data from the present study. Additionally, future studies should prospectively explore whether potential differences in effects of responsive parenting intervention components exist based on sex and other factors known to be associated with childhood obesity such as maternal prepregnancy BMI, gestational weight gain, and infant temperament.
Limitations
This study has several limitations. First, the sample was relatively homogeneous, recruited from a single center with mostly white, middle-income, predominantly well-educated, and English-speaking first-time mothers, and attrition was more likely to occur among higher risk participants. Second, the sample included only first-time mothers because it is typically easier to establish new behaviors than to change existing ones. Third, although it appears that intervening early was important, the 2-group randomized design precludes definitively determining which intervention components or combination of components were responsible for the positive effects. Fourth, the use of BMI for assessment of early life adiposity is debatable,33 though it remains a widely used and generally accepted outcome measure.
Conclusions
Among primiparous mother-child dyads, a responsive parenting intervention initiated in early infancy compared with a control intervention resulted in a modest reduction in BMI z scores at age 3 years, but no significant difference in BMI percentile. Further research is needed to determine the long-term effect of the intervention and assess its efficacy in other settings.
Trial Protocol and Statistical Analysis Plan
eMethods.
eResults.
eTable 1. Breastfeeding Rates at Study Assessment Points
eTable 2. Study Attrition Through 3 Years By Demographic Group
eTable 3. Summary Statistics for BMI z Scores at 3 Years for the Complete Data Set (A) and the Imputed Data Sets (B)
eTable 4. Linear Model Estimates for Responsive Parenting Group vs Control From Both Completer and Imputed 3 Year BMI z Scores Data Sets
References
- 1.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359(1):61-73. doi: 10.1056/NEJMra0708473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ. 2000;320(7240):967-971. doi: 10.1136/bmj.320.7240.967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA. 2009;301(21):2234-2242. doi: 10.1001/jama.2009.761 [DOI] [PubMed] [Google Scholar]
- 4.Singhal A, Cole TJ, Fewtrell M, Deanfield J, Lucas A. Is slower early growth beneficial for long-term cardiovascular health? Circulation. 2004;109(9):1108-1113. doi: 10.1161/01.CIR.0000118500.23649.DF [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814. doi: 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292-2299. doi: 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723-1725. doi: 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for childhood obesity in the first 1000 days a systematic review. Am J Prev Med. 2016;50(6):780-789. doi: 10.1016/j.amepre.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Healthy Eating Research Feeding guidelines for infants and young toddlers: a responsive parenting approach. 2017. http://healthyeatingresearch.org/research/feeding-guidelines-for-infants-and-young-toddlers-a-responsive-parenting-approach/. Accessed July 3, 2018.
- 10.Eshel N, Daelmans B, de Mello MC, Martines J. Responsive parenting: interventions and outcomes. Bull World Health Organ. 2006;84(12):991-998. doi: 10.2471/BLT.06.030163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guttentag CL, Landry SH, Williams JM, et al. “My Baby & Me”: effects of an early, comprehensive parenting intervention on at-risk mothers and their children. Dev Psychol. 2014;50(5):1482-1496. doi: 10.1037/a0035682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul IM, Williams JS, Anzman-Frasca S, et al. The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study. BMC Pediatr. 2014;14:184. doi: 10.1186/1471-2431-14-184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savage JS, Birch LL, Marini M, Anzman-Frasca S, Paul IM. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: a randomized clinical trial. JAMA Pediatr. 2016;170(8):742-749. doi: 10.1001/jamapediatrics.2016.0445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Mindell JA, Birch LL. INSIGHT responsive parenting intervention and infant sleep. Pediatrics. 2016;138(1):138. doi: 10.1542/peds.2016-0762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hohman EE, Paul IM, Birch LL, Savage JS. INSIGHT responsive parenting intervention is associated with healthier patterns of dietary exposures in infants. Obesity (Silver Spring). 2017;25(1):185-191. doi: 10.1002/oby.21705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karp H, Montee N. The Happiest Baby on the Block: The New Way to Calm Crying and Help Your Baby Sleep Longer [DVD]. New York, NY: Bantam Books; 2006. [Google Scholar]
- 18.US Centers for Disease Control and Prevention National Center for Health Statistics. https://www.cdc.gov/growthcharts/. Accessed July 3, 2018.
- 19.Krebs NF, Jacobson MS; American Academy of Pediatrics Committee on Nutrition . Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424-430. doi: 10.1542/peds.112.2.424 [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Chen H. Use of Percentiles and z Scores in Anthropometry In: Preedy VR, ed. Handbook of Anthropometry: Physical Measures. New York, NY: Springer; 2012:29-48. doi: 10.1007/978-1-4419-1788-1_2 [DOI] [Google Scholar]
- 21.Grossman DC, Bibbins-Domingo K, Curry SJ, et al. ; US Preventive Services Task Force . Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2017;317(23):2417-2426. doi: 10.1001/jama.2017.6803 [DOI] [PubMed] [Google Scholar]
- 22.Paul IM, Savage JS, Anzman SL, et al. Preventing obesity during infancy: a pilot study. Obesity (Silver Spring). 2011;19(2):353-361. doi: 10.1038/oby.2010.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76(3):653-658. doi: 10.1093/ajcn/76.3.653 [DOI] [PubMed] [Google Scholar]
- 24.Nader PR, O’Brien M, Houts R, et al. ; National Institute of Child Health and Human Development Early Child Care Research Network . Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594-e601. doi: 10.1542/peds.2005-2801 [DOI] [PubMed] [Google Scholar]
- 25.Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. BMJ. 2012;344:e3732. doi: 10.1136/bmj.e3732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Daniels LA, Mallan KM, Battistutta D, Nicholson JM, Perry R, Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of 2 intervention modules. Int J Obes (Lond). 2012;36(10):1292-1298. doi: 10.1038/ijo.2012.96 [DOI] [PubMed] [Google Scholar]
- 27.Sulik MJ, Blair C, Mills-Koonce R, Berry D, Greenberg M; Family Life Project Investigators . Early parenting and the development of externalizing behavior problems: longitudinal mediation through children’s executive function. Child Dev. 2015;86(5):1588-1603. doi: 10.1111/cdev.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anzman-Frasca S, Stifter CA, Paul IM, Birch LL. Infant temperament and maternal parenting self-efficacy predict child weight outcomes. Infant Behav Dev. 2013;36(4):494-497. doi: 10.1016/j.infbeh.2013.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Connell LE, Francis LA. Positive parenting mitigates the effects of poor self-regulation on body mass index trajectories from ages 4-15 years. Health Psychol. 2014;33(8):757-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med. 2009;163(4):297-302. doi: 10.1001/archpediatrics.2008.579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braungart-Rieker JM, Lefever JB, Planalp EM, Moore ES. Body mass index at 3 years of age: cascading effects of prenatal maternal depression and mother-infant dynamics. J Pediatr. 2016;177:128-132.e1. doi: 10.1016/j.jpeds.2016.06.023 [DOI] [PubMed] [Google Scholar]
- 32.Anderson SE, Sacker A, Whitaker RC, Kelly Y. Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. Int J Obes (Lond). 2017;41(10):1459-1466. doi: 10.1038/ijo.2017.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child. 2006;91(7):612-617. doi: 10.1136/adc.2005.085522 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol and Statistical Analysis Plan
eMethods.
eResults.
eTable 1. Breastfeeding Rates at Study Assessment Points
eTable 2. Study Attrition Through 3 Years By Demographic Group
eTable 3. Summary Statistics for BMI z Scores at 3 Years for the Complete Data Set (A) and the Imputed Data Sets (B)
eTable 4. Linear Model Estimates for Responsive Parenting Group vs Control From Both Completer and Imputed 3 Year BMI z Scores Data Sets