Key Points
Question
Is hospital participation in Medicare’s Bundled Payments for Care Improvement (BPCI) program for lower extremity joint replacement (LEJR) associated with changes in overall procedural volume, case mix, or both?
Findings
In this observational study involving 1 717 243 Medicare beneficiaries who underwent LEJR, hospital participation in the BPCI initiative was not associated with changes in overall market-level LEJR volume (adjusted difference-in-differences estimate, 0.32%) and largely was not associated with changes in hospital case mix, with only 1 of 20 case-mix characteristics associated with a lower likelihood of undergoing LEJR at a BPCI-participating hospital.
Meaning
The lack of associations between Bundled Payments for Care Improvement program participation and changes in volume or the majority of patient case-mix factors may provide reassurance about 2 potential unintended effects of voluntary bundled payments for lower extremity joint replacement.
Abstract
Importance
Medicare’s Bundled Payments for Care Improvement (BPCI) initiative for lower extremity joint replacement (LEJR) surgery has been associated with a reduction in episode spending and stable-to-improved quality. However, BPCI may create unintended effects by prompting participating hospitals to increase the overall volume of episodes paid for by Medicare, which could potentially eliminate program-related savings or prompt them to shift case mix to lower-risk patients.
Objective
To evaluate whether hospital BPCI participation for LEJR was associated with changes in overall volume and case mix.
Design, Setting, and Participants
Observational study using Medicare claims data and a difference-in-differences method to compare 131 markets (hospital referral regions) with at least 1 BPCI participant hospital (n = 322) and 175 markets with no participating hospitals (n = 1340), accounting for 580 043 Medicare beneficiaries treated before (January 2011-September 2013) and 462 161 after (October 2013-December 2015) establishing the BPCI initiative. Hospital-level case-mix changes were assessed by comparing 265 participating hospitals with a 1:1 propensity-matched set of nonparticipating hospitals from non-BPCI markets.
Exposures
Hospital BPCI participation.
Main Outcomes and Measures
Changes in market-level LEJR volume in the before vs after BPCI periods and changes in hospital-level case mix based on demographic, socioeconomic, clinical, and utilization factors.
Results
Among the 1 717 243 Medicare beneficiaries who underwent LEJR (mean age, 75 years; 64% women; and 95% nonblack race/ethnicity), BPCI participation was not significantly associated with a change in overall market-level volume. The mean quarterly market volume in non-BPCI markets increased 3.8% from 3.8 episodes per 1000 beneficiaries before BPCI to 3.9 episodes per 1000 beneficiaries after BPCI was launched. For BPCI markets, the mean quarterly market volume increased 4.4% from 3.6 episodes per 1000 beneficiaries before BPCI to 3.8 episodes per 1000 beneficiaries after BPCI was launched. The adjusted difference-in-differences estimate between the market types was 0.32% (95% CI, −0.06% to 0.69%; P = .10). Among 20 demographic, socioeconomic, clinical, and utilization factors, BPCI participation was associated with differential changes in hospital-level case mix for only 1 factor, prior skilled nursing facility use (adjusted difference-in-differences estimate, −0.53%; 95% CI, −0.96% to −0.10%; P = .01) in BPCI vs non-BPCI markets.
Conclusions and Relevance
In this observational study of Medicare beneficiaries who underwent LEJR, hospital participation in Bundled Payments for Care Improvement was not associated with changes in market-level lower extremity joint replacement volume and largely was not associated with changes in hospital case mix. These findings may provide reassurance regarding 2 potential unintended effects associated with bundled payments for LEJR.
This before-after study uses Centers for Medicare and Medicaid Services’ (CMS’s) claims data to compare changes in lower extremity joint replacement surgery volume and case mix associated with participation vs nonparticipation in CMS' Bundled Payments for Care Improvement program.
Introduction
In 2013, the Centers for Medicare & Medicaid Services (CMS) initiated the Bundled Payments for Care Improvement (BPCI) voluntary program.1 Overall, 322 hospitals have participated in the program for lower extremity joint replacement (LEJR) surgery, which represents 36% of all episode volume across BPCI’s 48 clinical episodes.2 The predominant model in BPCI is Model 2, which bundles payment for acute hospitalization and up to 90 days of postacute care.
Model 2 LEJR evaluations by CMS demonstrated a 3.8% greater decrease in mean episode spending and a stable to improved quality relative to comparison hospitals.3,4 Other studies have shown that Model 2 hospitals have reduced expenditures by as much as 20% in supply costs, care standardization, and postacute care use.4,5,6 However, existing evaluations have not examined changes in overall episode volume and have included limited analysis of changes in case mix. Consequently, 2 major policy concerns remain: Are bundled payments associated with increases in the overall volume of episodes paid for by Medicare, and are they associated with changes in case mix?
Experts have expressed concern that Medicare savings could decrease or be eliminated if bundled payments prompt hospitals to perform more LEJR episodes than they otherwise would under fee-for-service payment plans.7,8 Critics have also noted that voluntary bundled payments may prompt hospitals to cherry pick lower-risk patients based on socioeconomic, racial, or clinical factors to improve quality and cost performance.9,10,11
Empirical evidence for both would be highly relevant as policy makers continue promoting voluntary bundled payments via the forthcoming BPCI Advanced program,12 which extends major elements of the BPCI Model 2 and includes LEJR. Therefore, this study analyzed Medicare data using a difference-in-differences approach to evaluate whether participation in Model 2 for LEJR was associated with changes in procedural volume or case mix.
Methods
This study was approved by the University of Pennsylvania Institutional Review Board with a waiver of informed consent because contacting study participants was not feasible.
Data and Study Period
We used 100% Medicare provider analysis and review files from 2011 and 2015, which contain encounter-level information about inpatient hospitalizations, and the BPCI analytic file to identify hospitals participating in BPCI Model 2.1 All hospitalizations were examined to identify procedures as complicated, defined as procedures designated under Medicare severity–diagnosis related group (MS-DRG) 469 as having major complications or comorbidities or as uncomplicated, procedures designated under MS-DRG 470 and without major complications or comorbidities.
Data from the American Hospital Association (AHA), Hospital Compare, and Medicare’s provider of service, beneficiary summary, and accountable care organization (ACO) provider-level research-identifiable files were used to obtain market and hospital characteristics.13,14,15,16 Hospital safety net status was determined by the amount of the disproportionate share hospital payments recorded in the CMS Impact file. Two study periods were defined: the pre-BPCI period, which spanned the first quarter of 2011 through the third quarter of 2013 (January 2011-September 2013) and the BPCI period, which spanned the fourth quarter of 2013 through the fourth quarter of 2015 (October 2013-December 2015).
Unit of Analysis
Analysis of hospital LEJR volume could have been confounded had clinicians and hospitals directed patients to bundled-payment hospitals and away from nonbundled-payment hospitals, driving market share changes rather than changes in the overall number of episodes paid for by Medicare.11 Therefore, the primary analysis evaluated quarterly LEJR volume at the level of health care markets, defined by hospital referral regions.7 Hospital-level sensitivity analyses were conducted to corroborate findings from earlier work.17 Conversely, the association between BPCI participation and case mix was analyzed at the hospital rather than market level because lower-risk patients may be preferentially directed to BPCI-participant hospitals.
BPCI Participation as Exposure Measure
A dichotomous measure of whether each market had any BPCI-participant hospitals at any point was used for descriptive purposes. All other analyses used a lagged continuous quarterly measure of LEJR market share for BPCI-participant hospitals. To construct this measure, the first step included measuring LEJR market shares at each hospital before the BPCI program launched, to avoid circularity that would result from using LEJR market–quarter volume as both a dependent variable and as a component of the exposure variable. Second, in each quarter in the BPCI period, the pre-BPCI LEJR market shares for participant hospitals were summed in that market quarter, and this market-level value for BPCI participation was assigned as the quarterly exposure in BPCI markets (Figure 1; and eFigure 1 in Supplement 1). This market-quarter value was set to 0 in the pre-BPCI period and updated in each quarter in the BPCI period so that it increased as more hospitals joined BPCI within a market. All hospital-level analyses used a dichotomous time-varying indicator of BPCI participation by quarter.
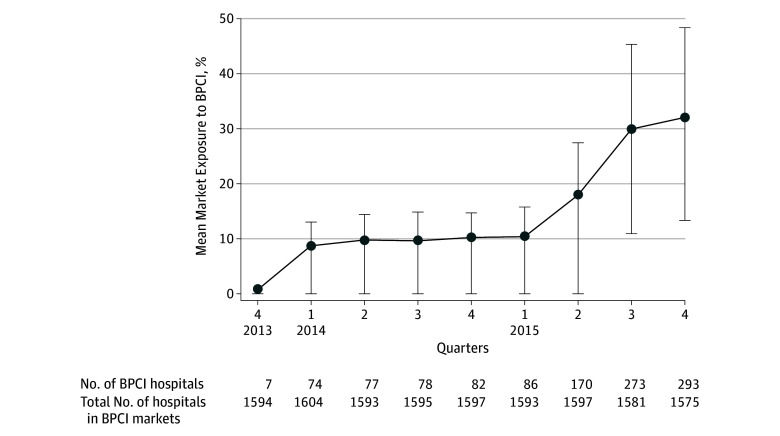
Figure 1. Mean Share of Lower Extremity Joint Replacement Surgery Episodes in Bundled Payments for Care Improvement Markets Performed by Participating Hospitals.
Abbreviations: BPCI, Bundled Payments for Care Improvement program by Medicare. This graph plots the mean share of 964 939 total beneficiaries who underwent LEJR episodes performed by 322 hospitals participating in BPCI in 131 BPCI markets. The numerator represents the number of LEJR episodes performed by hospitals participating in BPCI in a quarter and the denominator is the total number of LEJR episodes performed in the quarter. The error bars indicate the 25% and 75% percentiles rather than standard deviation due to skewness, and the mean share rather than median is shown because less than half of markets have a nonzero share for many quarters. Prior to 2013 quarter 4 there was no BPCI participation.
Outcome Measures
Market Volume was defined as the number of LEJR hospitalizations within each market per quarter, stratified by uncomplicated or complicated LEJR. Changes in case mix were evaluated through a series of hospital-level measures based on patient characteristics. Beneficiary-level case-mix outcomes were categorized by demographics, indicators of socioeconomic status, clinical indicators, and health care facility use in the prior 12 months. Demographic variables included advanced age (≥85 years), dichotomous indicators for black race (designated using Medicare claims data definitions, with an indicator for black race vs other races because of existing disparities in access to LEJR among patients with black race specifically), and sex. Indicators of socioeconomic status included dichotomous variables for dual eligibility for Medicare and Medicaid, and low education and income levels in area of residence (bottom quartile of zip codes nationally). Clinical indicators included dichotomous clinical variables representing presence of high complexity (top 20% of mean Elixhauser comorbidity index,18 calculated using conditions present in the year preceding LEJR hospitalization), obesity, diabetes, diabetes with complications, coronary heart disease, congestive heart failure, alcohol use, depression, psychoses, frailty,19,20 and 2 or more Elixhauser comorbidities. Health care facility use in the prior 12 months before LEJR hospitalization included acute care hospital, skilled nursing facility, or inpatient rehabilitation facility.
Covariates
Market- and hospital-level analyses incorporated covariates that reflected market-level characteristics of patients (age, sex, race), hospitals (number of beds), and market structure (hospital and skilled nursing facility concentration, ACO penetration, Medicare Advantage penetration, and presence of physician group practice). Hospital and skilled nursing facility market concentration was determined via the Herfindahl-Hirschman index (HHI).
Statistical Analysis
We described characteristics for BPCI and non-BPCI markets and hospitals, as well as quarterly trends in BPCI enrollment, number of markets with BPCI-participant hospitals, and market level BPCI participation.
To evaluate the association between BPCI participation and changes in LEJR volume, a difference-in-differences method21 was used to estimate differential changes in mean market volume, as well as mean market volume per 1000 beneficiaries to adjust for differences in market size, for BPCI and non-BPCI markets in both periods. In adjusted analysis with the covariates above, unconditional negative binomial models adjusted for market size (using the number of beneficiaries per market per quarter) were used for market volume (to avoid bias from large numbers of fixed effects in nonlinear regression). Within-market changes for BPCI markets before and after BPCI participation to changes in non-BPCI markets were compared using market and quarter fixed effects. Changes in market volume were plotted using predicted quarterly values for non-BPCI markets, BPCI markets, and the counterfactual of BPCI markets without any volume changes due to participation (eMethods 1 in Supplement 1).
In sensitivity analyses, negative binominal models containing hospital and quarter fixed effects along with the covariates in market-level analyses were used to evaluate the association of hospital BPCI participation with hospital-level LEJR volume and market share. We compared participant hospitals (1) with all nonparticipant hospitals in non-BPCI markets and (2) with a propensity-matched set of nonparticipant hospitals in non-BPCI markets to replicate methods in formal CMS evaluations (eMethods 2 in Supplement 1).2,3,17
The robustness of these results was evaluated in several ways. The assumption of parallel trends under our difference-in-differences method was tested using a generalized linear regression of volume on a BPCI market indicator, time variable, and the interaction, using a Wald test that did not indicate divergent secular trends during the pre-BPCI period (P = .92) (eTable 1 in the Supplement). To evaluate whether volume changes might arise from “pent-up demand” (ie, hospitals delaying procedures until they participated in BPCI), an analogous regression and Wald test was used to conduct a falsification test of whether market volume changed in the year before BPCI. We also examined whether an influx or outflow of volume from beneficiaries crossing over hospital referral regions, or high penetration (top quartile) of ACOs in markets, could explain any volume changes. In addition, volume changes for carotid endarterectomy (not covered under BPCI) and nonelective hip fracture surgery, procedures for which BPCI participation should not be associated with volume changes, were evaluated.
The association of BPCI participation and case-mix changes was evaluated using a difference-in-differences method to test for differential changes in the likelihood that patients with certain characteristics would undergo LEJR at participant vs nonparticipant hospitals before and after BPCI was initiated. These analyses used linear regression adjusted for covariates and hospital and quarter fixed effects. As the primary approach, participant hospitals were compared with a 1:1 propensity-matched set of non-BPCI hospitals from non-BPCI markets (eMethods 2 in Supplement 1). In sensitivity analyses, participant hospitals were compared with nonpropensity matched nonparticipant hospitals from non-BPCI markets with and without risk-adjustment.
Hospitals with missing data were excluded from analysis. Statistical tests were 2-tailed and considered significant at α = .05. Robust standard errors were corrected for heteroscedasticity.22 Analyses were performed using SAS (version 9.4, SAS Institute Inc) and Stata (version 15.1, Stata Corp).
Results
The total number of beneficiaries who underwent LEJR from 2011 through 2015 was 1 717 243 at a BPCI hospital or at a comparison non-BPCI hospital located in a non-BPCI market (Table 1). In the pre-BPCI period, 175 non-BPCI markets represented approximately 13.6 million beneficiaries, 420 518 of whom underwent LEJR (mean LEJR procedures per quarter, 238.3) at 1558 non-BPCI hospitals in these markets (Table 1). During the same period, among approximately 18.0 million beneficiaries in 131 BPCI markets, 536 278 beneficiaries underwent a mean 406.7 LEJR procedures per quarter. Of these, 159 525 patients received LEJR at 322 hospitals that later became BPCI hospitals. The 1340 non-BPCI hospitals in non-BPCI markets that performed LEJR procedures and 322 eventual participant hospitals accounted for 580 043 Medicare beneficiaries undergoing LEJR before BPCI and 462 161 beneficiaries undergoing LEJR after BPCI. (Table 1; and eTable 2 in the Supplement).
Table 1. Patient Characteristics by BPCI Participation, 2011-2015a.
| Non-BPCI Markets | BPCI Markets | Difference-in-Differences Value | Difference-in-Differences P Value | |||||
|---|---|---|---|---|---|---|---|---|
| Before BPCI | BPCI | Difference Between Periods, % b | Before BPCI | BPCI | Difference Between Periods, %b | |||
| Market, No. | 175 | 175 | 131 | 131 | ||||
| Hospital, No.c | 1558 | 1520 | 1955 | 1928 | ||||
| Total No. of beneficiaries | 13 625 041 | 13 762 820 | 18 048 915 | 18 234 384 | ||||
| Underwent LEJR, No. | 420 518 | 331 786 | 536 278 | 428 661 | ||||
| Patient Characteristics | ||||||||
| Age, mean (SD), y | 75 (1) | 74 (1) | −1 | 75 (1) | 74 (1) | −1 | 0 | <.001 |
| ≥85, % (SD) | 11 (2) | 10 (2) | −1 | 11 (2) | 10 (2) | −1 | 0 | .47 |
| Race/ethnicity, % (SD)d | <.001 | |||||||
| Black | 4.5 (5.8) | 4.4 (5.5) | −0.1 | 4.5 (4.7) | 4.4 (4.4) | −0.2 | −0.1 | |
| Other | 95.5 (5.8) | 95.6 (5.5) | 0.1 | 95.5 (4.7) | 95.6 (4.4) | 0.2 | 0.1 | |
| Women, No. (%) | 64.4 (3.0) | 63.0 (2.8) | −1.4 | 65.1 (2.3) | 63.2 (2.3) | −2.0 | −0.6 | <.001 |
| Dual-eligible, No. (%)e | 8.4 (4.8) | 7.7 (4.1) | −0.7 | 9.1 (6.7) | 8.1 (5.7) | −1.0 | −0.3 | .24 |
| Zip code, % (SD)f | ||||||||
| Low income | 22.9 (18.2) | 22.2 (17.8) | −0.7 | 18.2 (16.5) | 17.3 (16.2) | −0.9 | −0.2 | <.001 |
| Low education | 14.7 (17.3) | 14.4 (17.1) | −0.4 | 13.4 (13.1) | 12.9 (12.7) | −0.6 | −0.2 | .002 |
| Elixhauser score, mean (SD)g | ||||||||
| Receiving LEJR | 2.0 (0.8) | 1.9 (0.8) | −0.1h | 1.9 (0.7) | 1.8 (0.6) | −0.1h | 0.2 | <.001 |
| Uncomplicated | 1.6 (0.7) | 1.4 (0.8) | −0.2h | 1.5 (0.6) | 1.4 (0.6) | −0.1h | 0.3 | <.001 |
| Complicated | 11.0 (2.1) | 11.2 (2.2) | 0.2h | 10.8 (1.7) | 11.3 (1.9) | 0.5h | 0.3 | <.001 |
| High complexity, %i | 20.4 (4.7) | 19.7 (4.5) | −0.7 | 19.8 (3.9) | 19.3 (3.5) | −0.5 | 0.2 | .002 |
| Comorbidities, % (SD) | ||||||||
| Obesity | 15.5 (5.4) | 18.3 (6.3) | 2.9 | 15.5 (4.5) | 18.2 (4.9) | 2.7 | −0.2 | <.001 |
| Diabetes | 23.2 (3.5) | 22.9 (3.7) | −0.2 | 22.1 (3.2) | 21.8 (3.2) | −0.3 | −0.1 | <.001 |
| Diabetes with complicationsj | 2.2 (0.7) | 2.8 (0.9) | 0.6 | 2.2 (0.7) | 2.7 (0.7) | 0.5 | −0.1 | .03 |
| Coronary artery disease | 20.0 (4.7) | 17.5 (4.0) | −2.5 | 18.9 (3.7) | 16.7 (3.5) | −2.2 | 0.3 | <.001 |
| Congestive heart failure | 6.2 (1.8) | 6.1 (1.9) | −0.1 | 5.7 (1.4) | 5.7 (1.5) | 0 | 0.1 | <.001 |
| Drug abuse | 0.1 (0.1) | 0.2 (0.2) | 0.1 | 0.1 (0.1) | 0.2 (0.2) | 0.1 | 0 | .40 |
| Alcohol use | 0.4 (0.3) | 0.6 (0.4) | 0.2 | 0.5 (0.2) | 0.6 (0.3) | 0.2 | 0 | <.001 |
| Depression | 13.2 (3.0) | 14.2 (3.1) | 1.1 | 12.7 (3.1) | 13.8 (3.2) | 1.0 | −0.1 | .002 |
| Psychoses | 2.3 (0.8) | 2.4 (0.9) | 0 | 2.2 (0.8) | 2.3 (0.8) | 0.1 | 0.1 | <.001 |
| Frailtyk | 2.4 (1.1) | 2.9 (1.2) | 0.5 | 3.0 (1.3) | 3.4 (1.4) | 0.4 | −0.1 | <.001 |
| ≥2 Comorbidities | 67.5 (6.8) | 67.2 (6.8) | −0.3 | 66.6 (6.1) | 66.1 (6.4) | −0.5 | −0.2 | .25 |
| Any Utilization in 12 mo Prior to Index Hospitalization, % (SD) | ||||||||
| Acute care hospital | 21.2 (2.2) | 20.1 (2.5) | −1.2 | 21.4 (1.8) | 19.9 (2.0) | −1.5 | −0.3 | <.001 |
| Inpatient rehabilitation facility | 1.8 (1.5) | 1.6 (1.4) | −0.2 | 2.0 (1.6) | 1.7 (1.4) | −0.3 | −0.1 | <.001 |
| Skilled nursing facility | 5.7 (2.0) | 5.3 (1.9) | −0.4 | 6.3 (1.9) | 5.6 (1.8) | −0.7 | −0.3 | <.001 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; LEJR, lower extremity joint replacement.
See the Methods section for the definition of BPCI periods.
Except when otherwise indicated.
Includes hospitals with zero volume for all LEJR.
Black race was deliniated because of access to LEJR disparities. Other includes white, Asian, Hispanic, North American Native, and other.
Eligibile for both Medicare and Medicaid.
Resides in a zip code area with a median income in the bottom quartile of the national median zip code areas or in a zip code area in which residents with less than a high school education is in the top quartile nationally.
The score ranges from −20 to 90 with increasing scores highly correlated with increased probability of in-hospital death.
These values represent the differences in Elixhauser score between the periods.
Comorbidity score in the top 20% of all patients in the sample.
Evidence of chronic complications.
Before the BPCI initiative launched, the mean age of beneficiaries undergoing LEJR was 75 years; between 64% and 65% were women; and 5% were black. The mean Elixhauser comorbidity index for uncomplicated LEJR was 2 and for complicated, 11.
Market Characteristics
The number of markets with at least 1 BPCI-participant hospital increased to 122, with the mean market share of LEJR procedure paid for through BPCI program increasing to 32% (Figure 1; eFigure 1, and eFigure 2A in Supplement 1). Medicare Advantage penetration (23% vs 26%, respectively, P = .93), hospital concentration (HHI of 3856 vs 2629, respectively, P = .98), and skilled nursing facility concentration (HHI of 1860 vs 1168, respectively, P = .13) did not vary across non-BPCI and BPCI markets, whereas ACO penetration was higher in BPCI markets (4% vs 5%, P = .009) (Table 1 and Table 2).
Table 2. Market Characteristics by BPCI Participation, 2011-2015a.
| Non-BPCI Markets | BPCI Markets | Difference-in-Differences Value | Difference-in-Differences P Value | |||||
|---|---|---|---|---|---|---|---|---|
| Before BPCI | BPCI | Difference Between Periods, % b | Before BPCI | BPCI | Difference Between Periods, %b | |||
| Market Structure Characteristics c | ||||||||
| Market, No. | 175 | 175 | 131 | 131 | ||||
| Medicare Advantage penetration, % (SD)d | 23 (14) | 27 (14) | 4 | 26 (13) | 30 (13) | 4 | 0 | .93 |
| ACO penetration, % (SD)e | 4 (6) | 14 (13) | 10 | 5 (7) | 20 (15) | 15 | 5 | <.001 |
| Hospital concentration, HHI (SD)f | 3856 (2219) | 3890 (2218) | 1 | 2629 (1794) | 2670 (1795) | 2 | 1 | .98 |
| Skilled nursing facility concentration, HHI (SD)f | 1860 (1322) | 1708 (1202) | −8 | 1168 (860) | 1105 (809) | −5 | 3 | .12 |
| Markets with physician group practice, %g | 0 | 41 | 41 | 0 | 51 | 51 | 10.0 | NA |
Abbreviations: ACO, accountable care organization; BPCI, Bundled Payments for Care Improvement; HHI, Herfindahl-Hirschman index; NA, not applicable.
See the Methods section for the definition of BPCI periods.
Except when otherwise indicated.
Calculated based on total procedural (episode) volume.
Determined by the Medicare Beneficiary Summary File and computing at a market–quarter level the proportion of Medicare beneficiaries in Medicare Advantage any time during that quarter.
Determined from a random 20% sample of fee-for-service beneficiaries and the Centers for Medicare & Medicaid ACO Provider-level Research Identifiable File following methods for assignment based on the plurality of primary care spending.23
Determined using the HHI.24
Markets with a physician group practice participating in BPCI for the LEJR condition.
Hospital Characteristics
There were 7 BPCI-participant hospitals at the beginning of the BPCI period (eFigure 2B in Supplement 1)25 and a total of 1340 non-BPCI hospitals in non-BPCI markets. The number of BPCI-participant hospitals increased after the program began to a maximum number of 322, although only 293 hospitals participated in late 2015 due to drop out.25 Seven hundred twenty-nine non-BPCI hospitals and 21 BPCI-participant hospitals had at least one quarter without data on LEJR episodes and were thus considered to have zero volume for those quarters.
The BPCI participant and nonparticipant hospitals in non-BPCI markets varied with respect to a number of characteristics (Table 3). Compared with non-BPCI hospitals in non-BPCI markets, BPCI-participant hospitals were larger (mean number of beds, 324 vs 213; P < .001) and more likely to be urban (95% vs 72%), not-for-profit (76% vs 65%), and teaching (75% vs 48%) hospitals (P < .001 for all). The BPCI-participant hospitals had more total (12 939 vs 6796) and Medicare (5912 vs 3209) admissions (P < .001 for both). At baseline, BPCI-participant hospitals were more likely than non-BPCI hospitals to have joint replacement complication (5% vs 2%) and readmission (18% vs 8%) rates higher than national means (P < .001 for both).
Table 3. Hospital Characteristics by BPCI Participation, 2011-2015.
| Non-BPCI Hospitals With Nonzero Volume in Non-BPCI markets (n = 1340) |
BPCI Participating Hospitals (n = 322) |
P Value | |
|---|---|---|---|
| Beneficiaries receiving LEJR, No. | 753 304 | 289 900 | |
| Quarterly LEJR procedural volume per hospital, median (IQR) | 20 (7-44) | 35 (17-69) | <.001 |
| Annual admissions, median (IQR)a | |||
| Medicare | 3209 (1444-6235) | 5912 (3806-9513) | <.001 |
| Total | 6796 (2909-13 283) | 12 939 (7864-20 845) | <.001 |
| Hospital size, No. of beds, median (IQR)a | 158 (80-278) | 267 (160-401) | <.001 |
| Ownership status, No. (%)a | |||
| For-profit | 278 (21) | 67 (21) | <.001 |
| Not-for-profit | 876 (65) | 244 (76) | |
| Government | 186 (14) | 11 (4) | |
| Teaching status, No. (%)a,b | |||
| Major | 85 (6) | 46 (14) | <.001 |
| Minor | 561 (42) | 196 (61) | |
| None | 694 (53) | 80 (25) | |
| Urban status, No. (%)a | 964 (72) | 306 (95) | <.001 |
| Hospital margin %, median (IQR)a,c | 6 (1-12) | 7 (2-11) | .95 |
| Joint Commission accreditation, No. (%)a | 1072 (80) | 279 (87) | .01 |
| Safety net hospitals, No. (%)a,d | 330 (25) | 303 (23) | .48 |
| Net patient revenue paid on a shared risk basis, % (SD)a | 1.3 (7.2) | 2.5 (9.6) | .06 |
| Complication rate from Hospital Compare, No. (%)a,e | |||
| <National rate | 32 (2) | 12 (4) | <.001 |
| No different than the national rate | 1286 (96) | 296 (92) | |
| >National rate | 22 (2) | 14 (5) | |
| Readmission rate from Hospital Compare, No. (%)a,e | |||
| <National rate | 98 (7) | 26 (8) | <.001 |
| No different than the national rate | 1142 (85) | 239 (74) | |
| >National rate | 100 (8) | 57 (18) |
Abbreviations: BPCI, Bundled Payments for Care Improvement; IQR, interquartile range; LEJR, lower extremity joint replacement; MS-DRG, Medicare Severity-Diagnosis Related Group.
2015 data.
From the American Hospital Association Annual Survey, major teaching hospitals are members of the Council of Teaching Hospitals (COTH), minor teaching hospitals are non-COTH members that had a medical school affiliation reported to the American Medical Association, and nonteaching hospitals are all other institutions.
Hospital margin is a percentage calculated as the difference between total net revenue and total expenses divided by total net revenue.
Safety net hospitals were in the top quartile of disproportionate share payment percentage, using the fiscal year 2017 Centers for Medicare & Medicaid IMPACT file.
The 30-day joint replacement complication and readmissions rate designations as lower than, no different from, or higher than the national rate were drawn for each hospital directly from the Centers for Medicare & Medicaid Hospital Compare website.15 The method adjusts for patient factors but does not adjust for hospital characteristics.26
Market Volume
There were similar increases in the number of beneficiaries between the before and after periods in both the non-BPCI markets (increase from ≈13.6 to ≈13.8 million beneficiaries) and BPCI markets (increase from ≈18.0 to ≈18.2 million beneficiaries; Table 1).
In non-BPCI markets, quarterly mean market volume was 238 for all LEJR episodes in the pre-BPCI period and 252 for episodes in the BPCI period, corresponding to 3.8 and 3.9 episodes per 1000 beneficiaries, respectively (P < .001) (Table 4; and eTable 3 in Supplement 1). Quarterly mean volume for uncomplicated LEJR increased from 229 to 243 episodes, corresponding to 3.6 to 3.8 episodes per 1000 beneficiaries (P < .001), but did not change significantly for complicated LEJR (10 episodes or 0.16 episodes per 1000 beneficiaries in both periods, P = .87). Similarly, in BPCI markets, quarterly mean market volume increased for all LEJR procedures (407 episodes or 3.6 episodes per 1000 beneficiaries in the pre-BPCI period and 436 episodes or 3.8 episodes per 1000 beneficiaries in the BPCI period, P < .001) and for uncomplicated LEJR (390 episodes or 3.5 episodes per 1000 beneficiaries to 419 episodes or 3.7 episodes per 1000 beneficiaries, respectively, P < .001), but not for complicated LEJR (17 episodes or 0.15 episodes per 1000 beneficiaries in both periods, P = .05).
Table 4. Changes in Market Volume of LEJR Surgery Associated With BPCI Participation, 2011-2015a.
| Unadjusted Analysisb | Adjusted Analysisc | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-BPCI Markets | BPCI Markets | Differential Change in Markets, No. per 1000 beneficiaries (%) | P Value | Adjusted Differential Change in Markets, % (95% CI) | P Value | |||||||
| Mean (SD) per 1000 Beneficiaries | Difference (% Over Baseline Rate) | P Value | Mean (SD) per 1000 Beneficiaries | Difference (% Over Baseline Rate) | P Value | |||||||
| Before BPCI | BPCI | Before BPCI | BPCI | |||||||||
| Market Volume per Quarter per 1000 Beneficiaries | ||||||||||||
| All LEJR | 3.8 (1.1) | 3.9 (1.2) | 0.1 (3.8) | <.001 | 3.6 (0.9) | 3.8 (1.0) | 0.2 (4.4) | <.001 | 0.01 (0.6) | .54 | 0.32 (−0.06 to 0.69) |
.10 |
| Uncomplicatedd | 3.6 (1.1) | 3.8 (1.1) | 0.2 (4.0) | <.001 | 3.5 (0.9) | 3.7 (1.0) | 0.2 (4.8) | <.001 | 0.0 (0.8) | .45 | 0.39 (.01to 0.77) |
.04 |
| Complicatedd | 0.16 (0.09) | 0.16 (0.09) | 0 | .87 | 0.15 (0.07) | 0.15 (0.06) | 0.0 (−3.7) | .05 | 0.0 (−3.7) | .42 | −1.1 (−2.38 to 0.20) |
.10 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; LEJR, lower extremity joint replacement.
See the Methods section for the definition of BPCI periods. The nonparticipating category included 175 markets, 1340 hospitals, and 27 387 861 beneficiaries. The participating category included 131 markets, 1955 hospitals, and 36 283 299 beneficiaries.
Unadjusted analysis does not control for time-varying participation or dose of exposure to BPCI at the market level in BPCI markets.
Adjusted analysis models have market fixed effects; quarter fixed effects to adjust for the secular trend, additional time-varying market-level covariates including beneficiary characteristics such as distributions of age, sex, race, and market structure controls including market size (number of beneficiaries); hospital capacity and concentration; postacute care capacity and concentration; Medicare Advantage penetration; ACO penetration; and BPCI physician group practice participation. Mean BPCI exposure for BPCI markets in the BPCI period was 14%. Positive values were interpreted as differential increases in volume in BPCI markets compared with non-BPCI markets. Negative values were interpreted as differential decreases in volume in BPCI markets as compared with non-BPCI markets.
See the Methods section for a definition of complicated and uncomplicated.
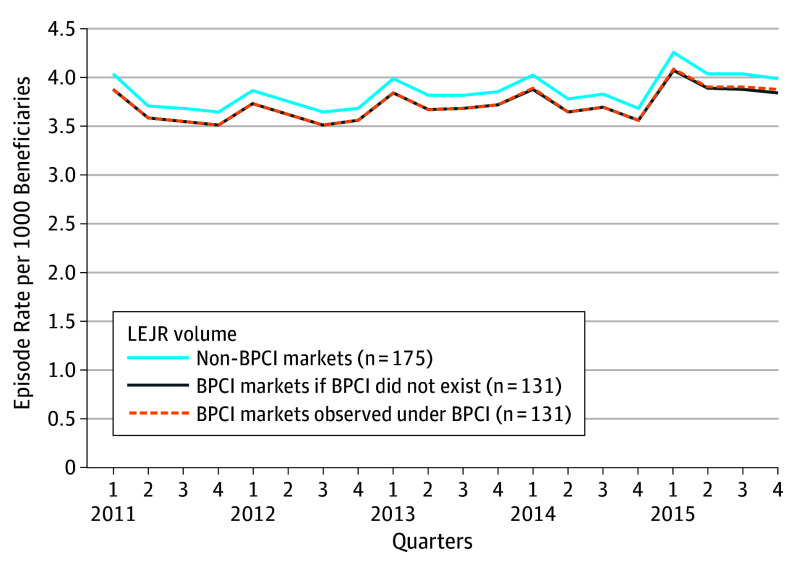
In unadjusted analysis, the differential change in market volume in BPCI vs non-BPCI markets was 0.01 episodes per 1000 beneficiaries (0.6%, P = .54) for all LEJR episodes, 0.0 episodes per 1000 beneficiaries (0.8%, P = .45) for uncomplicated LEJR, and 0.0 episodes per 1000 beneficiaries (−3.3%, P = .42) for complicated LEJR. In adjusted analysis, BPCI participation was not significantly associated with an increase in market-level LEJR volume (adjusted difference-in-differences estimate, 0.32% increase in LEJR market volume from before BPCI to the BPCI period for BPCI vs non-BPCI markets, 95% CI, −0.06% to 0.69%, P = .10; Table 4 and Figure 2). Participation was associated with a statistically significant 0.39% differential increase for uncomplicated LEJR (95% CI , 0.01% to 0.77%, P = .04), but not for complicated LEJR (−1.1%; 95% CI, −2.38% to 0.20%, P = .10; eFigure 3 in Supplement 1).
Figure 2. Changes in Lower Extremity Joint Replacement Surgery Market Volume per 1000 Beneficiaries From Bundled Payments for Care Improvement (BPCI) Participation in BPCI Markets vs Non-BPCI Markets, 2011-2015.
The total number of beneficiaries in the sample who underwent lower extremity joint replacement (LEJR) from 2011-2015 was 1 717 243 across the 175 non-BPCI markets comprising 1558 non-BPCI hospitals and 131 BPCI markets comprising 1955 hospitals (of which 322 participated in BPCI for LEJR). The LEJR corresponds to Medicare severity-–diagnosis related group 469 and 470, major joint replacement or reattachment of lower extremity with and without major complications or comorbidities. We plotted estimated (1) LEJR volume per 1000 beneficiaries in non-BPCI markets; (2) LEJR volume per 1000 beneficiaries in BPCI markets if BPCI did not exist, which reflects secular trends in volume plus the influence of BPCI on episode spending but without any potential changes on overall LEJR volume; and (3) LEJR volume per 1000 beneficiaries in BPCI markets observed under BPCI, which reflects observed LEJR volume in BPCI that is composed of secular trends in volume plus the influence of BPCI on procedural volume (eMethods 1 in Supplement 1). The lack of difference in LEJR volume between LEJR volume in BPCI markets if BPCI did not exist and LEJR volume in BPCI markets observed under BPCI scenarios is illustrated (estimate of 0.3%, P = .10).
Case mix
Of 322 BPCI hospitals, 265 were propensity matched with 265 non-BPCI hospitals in non-BPCI markets with balanced hospital characteristics across matched hospitals (eTable 4 in Supplement 1). In adjusted analysis, hospital participation was associated with case-mix changes for prior skilled nursing facility use, with these patients less likely to undergo LEJR at participant hospitals vs nonparticipant hospitals (difference-in-difference estimate −0.53%, 95% CI −0.96% to −0.10%, P = .01) (Figure 3). There were no significant associations of BPCI participation with 19 other demographic, socioeconomic, clinical, and prior utilization factors.
Figure 3. Changes in Case Mix at BPCI-Participant Hospitals vs Matched Non-BPCI Hospitals Before and After BPCI .
There were 212 922 beneficiaries who underwent lower extremity joint replacement (LEJR) surgery at the 265 matched Bundled Payments for Care Improvement (BPCI) hospitals and 212 951 beneficiaries at the 265 matched non-BPCI hospitals. The association between BPCI participation and the change in probability of a beneficiary with each characteristic receiving LEJR surgery between hospital types and between periods is estimated with a separate difference-in-differences linear probability regression model (ordinary least squares). The estimate for each patient characteristic indicates the difference in the probability comparing the before and after changes at BPCI vs non-BPCI hospitals. The propensity matching model is described in detail in eMethods 2 in the Supplement.
aRace was broken out as black vs others because of existing disparities in access to LEJR among black patients specifically. Other race/ethnicity includes white, Asian, Hispanic, North American Native, and other as defined by Medicare.
bDual eligible indicates eligibility for both the Medicare and Medicaid programs as an indicator of low socioeconomic status.
cThe variables low-median income level zip code and low-education level zip code are binary variables indicating that a beneficiary resides in a zip code with a median income in the bottom quartile of median zip code income nationally or with a proportion of residents with less than a high school education that is in the top quartile among zip codes nationally, respectively.
dSee the Methods section for definition of complexity.
eEvidence of chronic complications.
Sensitivity Analysis
Results from analyzing LEJR volume and market share at the hospital level were qualitatively similar to market-level results (eTable 5 in Supplement 1). Trends in case-mix changes were generally similar between primary and sensitivity analyses (eFigures 4 and 5 in Supplement 1).
Additional Analyses
Differential changes in uncomplicated LEJR volume were not associated with shifting procedures from the year immediately before to the year after BPCI participation was initiated and were consistent with the primary analysis when analyzing markets based on patient residence rather than hospital location (eTable 6 in Supplement 1). Participation was not associated with volume increases for nonelective hip fracture surgery or carotid endarterectomy or when stratifying analyses by ACO penetration (eTables 6 and 7 in Supplement 1).
Discussion
In this study, BPCI participation was not significantly associated with a change in overall volume of LEJR episodes, estimated as a nonsignificant differential increase in episodes of 0.32% (95% CI, −0.06% to 0.69%, P = .10). Participation was not associated with changes in most case-mix factors but was associated with a small, statistically significant reduction of 0.53% in the likelihood of undergoing LEJR among beneficiaries with prior skilled nursing facility use (95% CI, −0.96% to −0.10%, P = .01). These findings have 2 important policy implications in light of the forthcoming BPCI-Advanced program.
First, to our knowledge, this study provides the first empirical evidence that there were no significant changes in overall LEJR volume under the BPCI initiative. Supported by analyses adjusted for a range of patient, hospital, and market factors, this result is important for mitigating concerns that hospital participation in voluntary bundles may increase the overall number of LEJR procedures paid for by Medicare and decrease or altogether eliminate the program’s savings.7,8
In particular, this finding suggests that the 3.8% savings per episode observed in prior BPCI evaluations17 is not reduced through an increase in procedural volume. Furthermore, hospital-level analyses demonstrate that if BPCI-participant hospitals experienced any volume changes relative to non-BPCI hospitals, they would have more likely reflected shifts between hospitals within markets (ie, an increase in market share for BPCI-participant hospitals) rather than increases in overall market volume.
Second, the lack of changes in likelihood of undergoing LEJR at BPCI hospitals along most demographic, socioeconomic, and clinical patient characteristics is reassuring, particularly in light of preexisting disparities in access to and outcomes for LEJR and concerns that hospitals accountable for cost and quality may try to avoid patients with unfavorable risk profiles.27,28,29,30 However, though small, the observed change for patients with prior use of skilled nursing facilities is notable because many hospitals achieved savings by decreasing discharges to institutional postacute care facilities.5,17 This finding does raise the possibility that hospitals avoided these patients based on high perceived risk of poor clinical and financial outcomes. Such patient selection may represent a negative unintended consequence of bundled payments and occurs at a relatively notable rate for some patients. For example, the 0.53% (95% CI, −0.96% to −0.10%) reduction in patients with prior skilled nursing facility use undergoing LEJR at BPCI-participant hospitals corresponds to a relative reduction of 8.4%.
Conversely, it is not clear that reductions in LEJR for beneficiaries with prior skilled nursing facility use definitively reflects a decrease in patient welfare. For these patients, a lower likelihood of undergoing LEJR under BPCI might reflect clinically appropriate discretion in assessing surgical candidacy (ie, reductions among those for whom LEJR may be inappropriate due to high operative or complication risk). Although this study is unable to distinguish between appropriate and inappropriate patient selection and therefore whether changes were detrimental or beneficial for patients more generally, it is reassuring that patient selection was not observed.31,32
Nevertheless, these findings reinforce the need to monitor trends in access and outcomes for vulnerable beneficiaries who may be candidates for LEJR under bundled payments, particularly because of well-known disparities under fee-for-service reimbursement.28,30 Given that bundled payments have been associated with improvements in quality and lower cost of LEJR, further research is needed to evaluate whether vulnerable beneficiaries and their communities can access and experience such benefits.
Limitations
This study has several limitations. First, results were limited by the inability to examine long-term effects as well as potential confounding from omitted variables with coincident trends, and downward bias from low market-level BPCI participation that may have led to inadequate power to detect a statistically significant difference between the 3.8% and 4.4% changes in volume in non-BPCI and BPCI markets, respectively. However, the chance of spurious findings was mitigated by consistency of results across robustness checks (eg, falsification tests, tests of alternate explanations, and hospital-level analyses). Second, strong secular trends could have been driven by the profitability of LEJR, dampening the ability to observe volume increases under BPCI. However, the effect of BPCI policy would have been analogously dampened, and methods that account for secular trends were used. Third, analyses may not generalize to other episodes, particularly for medical conditions. Fourth, while this study focuses on BPCI Model 2, it is the largest model by enrollment and is the basis for BPCI-Advanced. Fifth, because this study evaluated BPCI-participant hospitals, findings may not generalize to episodes initiated by physician groups. Sixth, results were based on voluntary participation, and results may not apply to mandatory bundled payment programs such as Medicare’s Comprehensive Care for Joint Replacement.33 Seventh, while the analyses used a range of measures to evaluate case mix, some changes may have been unobservable in claims data.
Conclusions
In this observational study of Medicare beneficiaries who underwent lower extremity joint replacement, hospital participation in Bundled Payments for Care Improvement was not associated with changes in market-level lower extremity joint replacement volume and largely was not associated with changes in hospital case mix. These findings may provide reassurance regarding 2 potential unintended effects associated with bundled payments for lower extremity joint replacement.
eFigure 1. Comparison of Mean share of LEJR episodes in BPCI markets performed by BPCI participant hospitals with summed pre-BPCI share (exposure variable) in the BPCI period (2013 Quarter 4 to 2015 Quarter 4)
eMethods 1. Evaluating estimated changes in Market Volume
eMethods 2. Propensity score matching of BPCI hospitals to non-BPCI hospitals in non-BPCI markets
eTable 1. Tests of Parallel Trends between BPCI and Non-BPCI Markets for All and Uncomplicated LEJR Market Volume
eTable 2. Patient and Market Characteristics by BPCI participation, 2011-2015
eFigure 2a. Number of markets with a hospital participating in BPCI for LEJR by quarter, 2011-2015
eFigure 2b. Number of hospitals enrolled in BPCI for LEJR by quarter, 2011-2015
eTable 3. Changes in Lower Extremity Joint Replacement (LEJR) Market Volume Associated with BPCI Participation, 2011-2015
eFigure 3. Estimated Changes in Uncomplicated LEJR Market Volume per 1,000 Beneficiaries from BPCI participation in BPCI Markets compared to Non-BPCI Markets, 2011-2015
eTable 4. Comparison of characteristics of BPCI hospitals and non-BPCI hospitals before and after propensity matching
eTable 5. Changes in Lower Extremity Joint Replacement (LEJR) Volume at BPCI participant hospitals compared to Non-BPCI hospitals, 2011-2015
eFigure 4. Changes in case mix at BPCI participant hospitals compared to all Non-BPCI hospitals in Non-BPCI markets from the pre-BPCI to BPCI period
eFigure 5. Risk-Adjusted Changes in case mix at BPCI participant hospitals compared to all Non-BPCI hospitals in Non-BPCI markets from the pre-BPCI to BPCI period
eTable 6. Additional Analyses and Falsification Tests Examining the Association between BPCI Participation and Changes in Market Volume for Uncomplicated LEJR (MS-DRG 470), 2011-2015
eTable 7. The Association between BPCI Participation and Changes in Market Volume for All LEJR, stratified by ACO penetration
Data Sharing Statement.
References
- 1.CMS.gov . Bundled Payments for Care Improvement (BPCI) initiative: general information. https://innovation.cms.gov/initiatives/bundled-payments/. 2017. Accessed June 23, 2018.
- 2.The Lewin Group . CMS Bundled Payments for Care Improvement initiative: models 2-4: year 3 evaluation and monitoring annual report. https://downloads.cms.gov/files/cmmi/bpci-models2-4yr3evalrpt.pdf. 2017. Accessed June 22, 2018.
- 3.The Lewin Group . CMS Bundled Payments for Care Improvement initiative models 2-4: year 2 evaluation and monitoring annual report. https://innovation.cms.gov/Files/reports/bpci-models2-4-yr2evalrpt.pdf. 2016. Accessed June 21, 2018.
- 4.Liao JM, Holdofski A, Whittington GL, et al. Baptist Health System: succeeding in bundled payments through behavioral principles. Healthc (Amst). 2017;5(3):136-140. doi: 10.1016/j.hjdsi.2016.04.008 [DOI] [PubMed] [Google Scholar]
- 5.Navathe AS, Troxel AB, Liao JM, et al. Cost of joint replacement using bundled payment models. JAMA Intern Med. 2017;177(2):214-222. doi: 10.1001/jamainternmed.2016.8263 [DOI] [PubMed] [Google Scholar]
- 6.Ryan AM, Krinsky S, Adler-Milstein J, Damberg CL, Maurer KA, Hollingsworth JM. Association between hospitals’ engagement in value-based reforms and readmission reduction in the hospital readmission reduction program. JAMA Intern Med. 2017;177(6):862-868. doi: 10.1001/jamainternmed.2017.0518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher ES. Medicare’s bundled payment program for joint replacement: promise and peril? JAMA. 2016;316(12):1262-1264. doi: 10.1001/jama.2016.12525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berenson RA, Delbanco SF, Guterman S, et al. ACA implementation—monitoring and tracking. https://www.urban.org/research/publication/refining-framework-payment-reform. Published September 18, 2016. Accessed August 10, 2018.
- 9.Mechanic RE. Mandatory Medicare Bundled Payment—is it ready for prime time? N Engl J Med. 2015;373(14):1291-1293. doi: 10.1056/NEJMp1509155 [DOI] [PubMed] [Google Scholar]
- 10.Mechanic RE. Opportunities and challenges for episode-based payment. N Engl J Med. 2011;365(9):777-779. doi: 10.1056/NEJMp1105963 [DOI] [PubMed] [Google Scholar]
- 11.Alexander D. How do doctors respond to incentives? unintended consequences of paying doctors to reduce costs. http://scholar.princeton.edu/sites/default/files/dalexand/files/alexander_jmp.pdf. Accessed June 22, 2018.
- 12.Centers for Medicare & Medicaid Services . BPCI advanced. 2018; https://innovation.cms.gov/initiatives/bpci-advanced. Accessed January 9, 2018.
- 13.American Hospital Association annual survey database. http://www.ahadata.com/aha-annual-survey-database-asdb. Accessed August 17, 2018.
- 14.Centers for Medicare & Medicaid Services . Provider of services current files, 2011-2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/index.html. Accessed June 22, 2018.
- 15.Centers for Medicare & Medicaid Services . Hospital Compare. web page. https://www.medicare.gov/hospitalcompare/search.html? Accessed June 22, 2018.
- 16.Centers for Medicare & Medicaid Services . Shared savings program accountable care organizations (ACO) PUF. 2017; https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/SSPACO/index.html. Accessed June 22, 2018.
- 17.Dummit LA, Kahvecioglu D, Marrufo G, et al. Association between hospital participation in a Medicare Bundled Payment Initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016;316(12):1267-1278. doi: 10.1001/jama.2016.12717 [DOI] [PubMed] [Google Scholar]
- 18.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. doi: 10.1097/MLR.0b013e31819432e5 [DOI] [PubMed] [Google Scholar]
- 19.Kim DH, Schneeweiss S. Measuring frailty using claims data for pharmacoepidemiologic studies of mortality in older adults: evidence and recommendations. Pharmacoepidemiol Drug Saf. 2014;23(9):891-901. doi: 10.1002/pds.3674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joynt KE, Figueroa JF, Beaulieu N, Wild RC, Orav EJ, Jha AK. Segmenting high-cost Medicare patients into potentially actionable cohorts. Healthc (Amst). 2017;5(1-2):62-67. doi: 10.1016/j.hjdsi.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 21.Meyer BD. Natural and quasi-experiments in economics. J Bus Econ Stat. 1995;13(2):151-161. [Google Scholar]
- 22.MacKinnon JG, White H. Some heteroskedasticity-consistent covariance matrix estimators with improved finite sample properties. J Econom. 1985;29(3):305-325. doi: 10.1016/0304-4076(85)90158-7 [DOI] [Google Scholar]
- 23.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early performance of accountable care organizations in Medicare. N Engl J Med. 2016;374(24):2357-2366. doi: 10.1056/NEJMsa1600142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhoades SA. The herfindahl-hirschman index. Fed Reserve Bull. 1993;79:188. [Google Scholar]
- 25.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Participation and Dropout in the Bundled Payments for Care Improvement Initiative. JAMA. 2018;319(2):191-193. doi: 10.1001/jama.2017.14771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Measure methodology. Centers for Medicare & Medicaid web page. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Updated June 27, 2018. Accessed August 18, 2018.
- 27.Escalante A, Espinosa-Morales R, del Rincón I, Arroyo RA, Older SA. Recipients of hip replacement for arthritis are less likely to be Hispanic, independent of access to health care and socioeconomic status. Arthritis Rheum. 2000;43(2):390-399. doi: [DOI] [PubMed] [Google Scholar]
- 28.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73(12):2107-2115. doi: 10.1136/annrheumdis-2013-203494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barrack RL, Ruh EL, Chen J, et al. Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin Orthop Relat Res. 2014;472(1):86-97. doi: 10.1007/s11999-013-3002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ibrahim SA, Kim H, McConnell KJ. The CMS Comprehensive Care Model and racial disparity in joint replacement. JAMA. 2016;316(12):1258-1259. doi: 10.1001/jama.2016.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liao JM, Navathe AS, Chu D. Reframing the value proposition of coronary artery bypass graft bundles. JAMA Surg. 2018;153(3):199-200. doi: 10.1001/jamasurg.2017.4903 [DOI] [PubMed] [Google Scholar]
- 32.Navathe AS, Liao JM, Emanuel EJ. Volume increases and shared decision-making in joint replacement bundles. Ann Surg. 2018;267(1):35-36. doi: 10.1097/SLA.0000000000002283 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Medicare & Medicaid Services . Comprehensive care for joint replacement model. 2017; https://innovation.cms.gov/initiatives/cjr. Accessed June 22, 2018. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Comparison of Mean share of LEJR episodes in BPCI markets performed by BPCI participant hospitals with summed pre-BPCI share (exposure variable) in the BPCI period (2013 Quarter 4 to 2015 Quarter 4)
eMethods 1. Evaluating estimated changes in Market Volume
eMethods 2. Propensity score matching of BPCI hospitals to non-BPCI hospitals in non-BPCI markets
eTable 1. Tests of Parallel Trends between BPCI and Non-BPCI Markets for All and Uncomplicated LEJR Market Volume
eTable 2. Patient and Market Characteristics by BPCI participation, 2011-2015
eFigure 2a. Number of markets with a hospital participating in BPCI for LEJR by quarter, 2011-2015
eFigure 2b. Number of hospitals enrolled in BPCI for LEJR by quarter, 2011-2015
eTable 3. Changes in Lower Extremity Joint Replacement (LEJR) Market Volume Associated with BPCI Participation, 2011-2015
eFigure 3. Estimated Changes in Uncomplicated LEJR Market Volume per 1,000 Beneficiaries from BPCI participation in BPCI Markets compared to Non-BPCI Markets, 2011-2015
eTable 4. Comparison of characteristics of BPCI hospitals and non-BPCI hospitals before and after propensity matching
eTable 5. Changes in Lower Extremity Joint Replacement (LEJR) Volume at BPCI participant hospitals compared to Non-BPCI hospitals, 2011-2015
eFigure 4. Changes in case mix at BPCI participant hospitals compared to all Non-BPCI hospitals in Non-BPCI markets from the pre-BPCI to BPCI period
eFigure 5. Risk-Adjusted Changes in case mix at BPCI participant hospitals compared to all Non-BPCI hospitals in Non-BPCI markets from the pre-BPCI to BPCI period
eTable 6. Additional Analyses and Falsification Tests Examining the Association between BPCI Participation and Changes in Market Volume for Uncomplicated LEJR (MS-DRG 470), 2011-2015
eTable 7. The Association between BPCI Participation and Changes in Market Volume for All LEJR, stratified by ACO penetration
Data Sharing Statement.