Key Points
Question
Does an initial strategy of a supraglottic airway device for advanced airway management during nontraumatic out-of-hospital cardiac arrest result in a better functional outcome compared with tracheal intubation?
Findings
In this cluster randomized clinical trial that included 1523 paramedics and 9296 patients with out-of-hospital cardiac arrest, favorable functional outcome (modified Rankin Scale score in 0-3 range) at hospital discharge or after 30 days (if still hospitalized) occurred in 6.4% of patients in the supraglottic airway group vs 6.8% of patients in the tracheal intubation group, a difference that was not statistically significant.
Meaning
In this study, a strategy of using a supraglottic airway device for advanced airway management did not provide a superior functional outcome.
Abstract
Importance
The optimal approach to airway management during out-of-hospital cardiac arrest is unknown.
Objective
To determine whether a supraglottic airway device (SGA) is superior to tracheal intubation (TI) as the initial advanced airway management strategy in adults with nontraumatic out-of-hospital cardiac arrest.
Design, Setting, and Participants
Multicenter, cluster randomized clinical trial of paramedics from 4 ambulance services in England responding to emergencies for approximately 21 million people. Patients aged 18 years or older who had a nontraumatic out-of-hospital cardiac arrest and were treated by a participating paramedic were enrolled automatically under a waiver of consent between June 2015 and August 2017; follow-up ended in February 2018.
Interventions
Paramedics were randomized 1:1 to use TI (764 paramedics) or SGA (759 paramedics) as their initial advanced airway management strategy.
Main Outcomes and Measures
The primary outcome was modified Rankin Scale score at hospital discharge or 30 days after out-of-hospital cardiac arrest, whichever occurred sooner. Modified Rankin Scale score was divided into 2 ranges: 0-3 (good outcome) or 4-6 (poor outcome; 6 = death). Secondary outcomes included ventilation success, regurgitation, and aspiration.
Results
A total of 9296 patients (4886 in the SGA group and 4410 in the TI group) were enrolled (median age, 73 years; 3373 were women [36.3%]), and the modified Rankin Scale score was known for 9289 patients. In the SGA group, 311 of 4882 patients (6.4%) had a good outcome (modified Rankin Scale score range, 0-3) vs 300 of 4407 patients (6.8%) in the TI group (adjusted risk difference [RD], −0.6% [95% CI, −1.6% to 0.4%]). Initial ventilation was successful in 4255 of 4868 patients (87.4%) in the SGA group compared with 3473 of 4397 patients (79.0%) in the TI group (adjusted RD, 8.3% [95% CI, 6.3% to 10.2%]). However, patients randomized to receive TI were less likely to receive advanced airway management (3419 of 4404 patients [77.6%] vs 4161 of 4883 patients [85.2%] in the SGA group). Two of the secondary outcomes (regurgitation and aspiration) were not significantly different between groups (regurgitation: 1268 of 4865 patients [26.1%] in the SGA group vs 1072 of 4372 patients [24.5%] in the TI group; adjusted RD, 1.4% [95% CI, −0.6% to 3.4%]; aspiration: 729 of 4824 patients [15.1%] vs 647 of 4337 patients [14.9%], respectively; adjusted RD, 0.1% [95% CI, −1.5% to 1.8%]).
Conclusions and Relevance
Among patients with out-of-hospital cardiac arrest, randomization to a strategy of advanced airway management with a supraglottic airway device compared with tracheal intubation did not result in a favorable functional outcome at 30 days.
Trial Registration
ISRCTN Identifier: 08256118
This cluster randomized clinical trial compares the effects on functional outcomes of paramedic use of a supraglottic airway device vs tracheal intubation as airway management for adults with nontraumatic out-of-hospital cardiac arrest.
Introduction
Out-of-hospital cardiac arrest is common, sudden, and often fatal. During 2014, emergency medical services (EMS) in England attempted resuscitation in almost 30 000 people; only 25% achieved a return of spontaneous circulation and 8% were discharged alive from the hospital.1
Few advanced life support therapies have been shown to improve outcome following out-of-hospital cardiac arrest.2 There is a lack of data from high-quality randomized clinical trials (RCTs), which are challenging to conduct in patients with out-of-hospital cardiac arrest. Consequently, many current clinical recommendations are based on observational studies and expert consensus.3
Optimal airway management during out-of-hospital cardiac arrest is a key area of uncertainty because there is very little high-quality research on which to base treatment recommendations.4 Options range from basic or minimal airway intervention to early advanced procedures that require training and expertise.
The advanced procedure of tracheal intubation has been considered a definitive airway management technique.5 However, large observational studies (including >100 000 patients) have consistently favored basic airway management (eg, bag-mask ventilation) over tracheal intubation.6,7 The introduction of a supraglottic airway device offers an alternative advanced airway management technique during out-of-hospital cardiac arrest.
Insertion of a supraglottic airway device is simpler and faster than tracheal intubation,8 and proficiency requires less training and ongoing practice.9 Observational evidence has suggested a possible survival advantage for tracheal intubation compared with a supraglottic airway device.10 However, a large-scale RCT is required to identify the optimal approach to advanced airway management during out-of-hospital cardiac arrest.
The objective of this trial was to estimate the between-group difference in modified Rankin Scale score at hospital discharge or 30 days after out-of-hospital cardiac arrest for patients treated by paramedics randomized to use either a supraglottic airway device or tracheal intubation as their initial advanced airway management strategy.
Methods
Study Design and Paramedic and Patient Populations
The trial protocol and statistical analysis plan for this multicenter, cluster RCT appear in Supplement 1; the trial protocol has been published.11 Paramedics were recruited from 4 large EMS provider organizations (ambulance services) in England, which respond to emergencies for approximately 21 million people (40% of England’s population). The trial population was adults who had a nontraumatic out-of-hospital cardiac arrest.
The patient inclusion criteria were (1) known or believed to be aged 18 years or older; (2) nontraumatic out-of-hospital cardiac arrest; (3) treated by a paramedic participating in the trial who was either the first or second paramedic to arrive at the patient’s side; and (4) resuscitation was commenced or continued by emergency medical services personnel.
The patient exclusion criteria were (1) detained by Her Majesty’s Prison Service; (2) previously recruited to the trial (determined retrospectively); (3) resuscitation deemed inappropriate (using guidelines from the Joint Royal Colleges Ambulance Liaison Committee12); (4) advanced airway already in place (inserted by another paramedic, physician, or nurse) when a paramedic participating in the trial arrived at the patient’s side; (5) known to be enrolled in another prehospital RCT; and (6) the patient’s mouth opened less than 2 cm.
Paramedics could not be blinded to their allocation and mechanisms were required to avoid the risk of differential recruitment by paramedics based on the patient’s perceived likely outcome. Therefore, every eligible patient treated by a participating paramedic was automatically enrolled in the study under a waiver of consent provided by the confidentiality advisory group (reference No. 14/CAG/1030).
Ethics review and approval was provided by the South Central–Oxford C research ethics committee (reference No. 14/SC/1219), which included a process of written informed consent for participating paramedics. A disadvantage of automatic enrollment was that enrolled patients might not be treated according to the study protocol if the enrolling paramedic could not recall the protocol details (an out-of-hospital cardiac arrest is a relatively rare event) or if the paramedic mistakenly deemed the patient to be ineligible.
Randomization
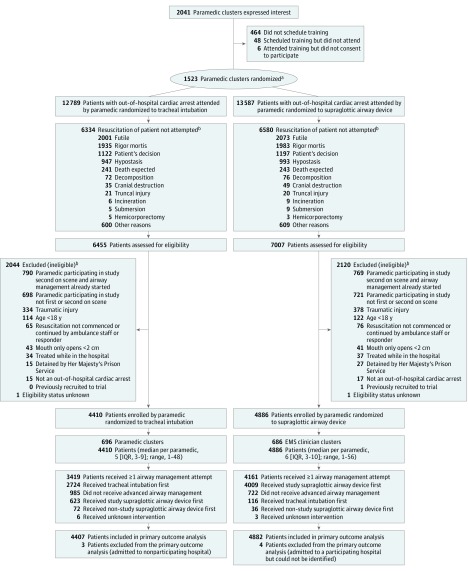
Because out-of-hospital cardiac arrest requires immediate treatment, randomizing patients at the point of out-of-hospital cardiac arrest was considered impractical. Therefore, paramedics were randomized to use 1 of the 2 advanced airway management strategies for the eligible patients that they treated (Figure 1). This design created many clusters with a small average number of patients per paramedic that minimized the effect of intracluster correlation and lowered the risk of chance imbalances between groups.
Figure 1. Flow of Study Paramedics and Patients.
Grouped according to the randomization assignment of the first paramedic on the scene who was participating in the study.
aThere were 113 paramedics who withdrew after randomization (58 randomized to tracheal intubation [TI] and 55 randomized to the supraglottic airway device [SGA]). The median number of patients with out-of-hospital cardiac arrest treated by a paramedic who later withdrew is 7 for TI (interquartile range [IQR], 3-12; range, 1-54) and 6 for SGA (IQR, 4-11; range, 1-31). The median number of trial patients treated by a paramedic who later withdrew is 3 for TI (IQR, 1.0-5.5; range, 1-10) and 2 for SGA (IQR, 1-4; range, 1-12). These trial patients were retained and included in the analysis.
bPatients can have more than 1 reason.
Paramedics were randomized in a 1:1 ratio using a purpose-designed secure internet-based system. The computer-generated random sequence was done in advance using varying block sizes (range, 4-8) and stratified by EMS provider organization (4 levels), paramedic experience (2 levels), and distance from the paramedic’s base ambulance station to the usual destination hospital (2 levels).
Intervention
The intervention was the insertion of a second-generation supraglottic airway device with a soft noninflatable cuff (i-gel; Intersurgical). Because of its speed and ease of insertion, this device has become the most commonly used supraglottic airway device during out-of-hospital cardiac arrest in England.13,14 The current standard of care is tracheal intubation using direct laryngoscopy; video laryngoscopy is not used by paramedics in England.
A standard approach to airway management (from basic to advanced techniques) was agreed on by the participating ambulance services. This included the use of bag-mask ventilation and simple airway adjuncts prior to advanced airway management. Apart from the initial advanced airway management, care proceeded as usual for patients with out-of-hospital cardiac arrest enrolled in the trial. All other care was delivered according to standard international resuscitation guidelines.3
Paramedics received additional training in their allocated advanced airway management intervention immediately after randomization. Training comprised theoretical and simulation-based practice over 1 hour with a brief assessment to confirm competence. For tracheal intubation, a 2-person technique using an intubating bougie was recommended. End-tidal carbon dioxide monitoring was used to confirm correct device placement in all patients.
Protocol deviations could arise because paramedics have both strategies available to them. Usual practice follows a step-wise approach from simple to more advanced techniques, but paramedics have the clinical freedom to adapt airway management during out-of-hospital cardiac arrest to the patient’s anatomy, position, and perceived needs. The trial protocol specified 2 attempts using the allocated strategy before proceeding to the alternative; however, paramedics had discretion to deviate from the trial protocol on clinical grounds.
Allowing discretion was necessary to avoid a paramedic feeling obliged to undertake an intervention that he or she believed to be contrary to the patient’s best interests. This also was necessary to secure approval from the research ethics committee and professional support.
Outcomes
The primary outcome was modified Rankin Scale score at hospital discharge or at 30 days if the patient remained in the hospital. Patients were transported to and followed up at each hospital by assessors blinded to treatment group who collected the modified Rankin Scale score. The modified Rankin Scale score is used widely in out-of-hospital cardiac arrest research,15,16 and is usually divided into 2 ranges: 0 to 3 (good outcome) or 4 to 6 (poor outcome to death).
The following secondary outcomes were collected for all eligible patients and all but the last 2 were reported by the paramedics: (1) initial ventilation success, which was defined as visible chest rise and was classified as “yes” when advanced airway management was not used; (2) regurgitation (stomach contents visible in the mouth or nose) or aspiration (stomach contents visible below the vocal cords or inside a correctly placed tracheal tube or airway channel of a supraglottic airway device) and each was classified as “no” when advanced airway management was not used; (3) any unintended loss of a previously established airway (patients with advanced airway management only); (4) sequence of airway interventions delivered (patients with advanced airway management only); (5) return of spontaneous circulation (patients with advanced airway management only; patients who died at the scene classified as “no” for return of spontaneous circulation at hospital admission); (6) airway management in place when return of spontaneous circulation was achieved or resuscitation was discontinued (patients with advanced airway management only); (7) chest compression fraction (in a subset of patients in 2 EMS provider organizations); and (8) time to death.
High-quality, continuous cardiopulmonary resuscitation (CPR) is associated with increased survival and improved function following out-of-hospital cardiac arrest; the concept of compression fraction has been developed to standardize its measurement.17 Therefore, compression fraction was measured and compared in a subset of patients treated by 2 ambulance services using the “CPR Card” (Laerdal), which is a small disposable device placed in the center of the patient’s chest during CPR. The device gives no feedback to the paramedic but records data that can be retrieved later.
Data on resource use to support a cost-effectiveness analysis and longer-term function also were collected. These data are not reported herein.
Sample Size
In a previous feasibility study, 9% of patients survived to hospital discharge.18 No data were available for the modified Rankin Scale score. However, death and poor functional outcome after out-of-hospital cardiac arrest are closely related because death is the most common outcome.16
An improvement of 2% in the proportion of patients achieving a good outcome (modified Rankin Scale score range, 0-3) was judged to be clinically important and consistent with the 2.4% difference observed in retrospective data19 between tracheal intubation and a supraglottic airway device for survival to hospital discharge. This meant that 9070 patients in total were needed to detect a difference of 8% vs 10% at the significance level of 5% with 90% power after allowing for clustering.11
Statistical Analysis
Analysis of the primary outcome and exploratory analyses of secondary outcomes were performed according to a prespecified statistical analysis plan, which was finalized before data lock and any comparative analysis, but after the end of recruitment due to staff changes within the statistical team. Some typographical errors were corrected in version 2 and some points were clarified, but no substantive changes were made. No comparative post hoc analyses were performed.
The primary analyses included all eligible patients with outcome data available except for the following secondary outcomes that only applied to those who received advanced airway management: (1) any unintended loss of a previously established airway; (2) return of spontaneous circulation during airway management; and (3) airway management in place when return of spontaneous circulation was achieved or resuscitation was discontinued. Chest compression fraction was only measured in a small subset of patients. Patients were grouped by the allocation of the first participating paramedic on the scene (main analyses). The analyses were adjusted for stratification factors as fixed effects.
For binary outcomes, mixed-effects logistic regression was used to estimate the odds ratios (ORs) for the primary analysis and paramedic was fitted as a random effect. Risk differences and risk ratios also were estimated using generalized linear regression and standard errors were calculated using a sandwich estimator to allow for clustering. The risk ratios are reported in Supplement 2.
For time-to-event outcomes, Cox proportional hazards regression was used. The proportionality assumption, which was checked using Schoenfeld residuals, was met.
Multiple imputation was not done because the level of missing data was only 7 patients (0.08%) for the primary outcome and less than 1.5% for all but 1 of the secondary outcomes, which had missing data for 6.4% of patients.
Two prespecified exploratory subgroup analyses were performed for the primary outcome: (1) out-of-hospital cardiac arrest with a likely cardiac cause that is witnessed and has an initial rhythm amenable to defibrillation (Utstein comparator group)20 vs a noncomparator group and (2) out-of-hospital cardiac arrest witnessed by a paramedic vs not witnessed by a paramedic. The treatment effect in the subgroups was compared by testing for a paramedic randomization × subgroup variable interaction.
Three prespecified exploratory sensitivity analyses were performed for the primary outcome. The first extended the population to include patients treated by a participating paramedic but who were not resuscitated (ie, trial patients plus nonresuscitated patients). This was prompted by feedback from the data and safety monitoring committee on a preplanned closed interim analysis of half the sample.
The second and third sensitivity analyses were planned from the outset and were restricted to the cohort of patients who received advanced airway management. Comparisons were made as allocated and by the treatment received.
A 2-sided significance level of 5% was used. The 2 groups were compared using Wald tests. No adjustment was made for multiple testing; therefore, the secondary outcomes should be considered exploratory.21 All analyses were performed using Stata version 15.1 (StataCorp).
Results
There were 1523 paramedics who were recruited and randomized. Of the 13 462 potentially eligible patients treated by the participating paramedics between June 2015 and August 2017, 4166 (31%) were excluded and 9296 (69%) were enrolled (median age, 73 years; 3373 were women [36.3%]; Figure 1 and Table 1).
Table 1. Patient Demographics and Cardiac Arrest Details.
| No. of Patients/Total No. (%)a | ||
|---|---|---|
| Tracheal Intubation (n = 4410) |
Supraglottic Airway Device (n = 4886) |
|
| Patient Demographics | ||
| Sex, No. (%) | ||
| Men | 2791 (63.3) | 3132 (64.1) |
| Women | 1619 (36.7) | 1754 (35.9) |
| Age, median (IQR), y | 74 (62-83) | 73 (61-82) |
| Cardiac Arrest Details | ||
| Time, median (IQR), min | ||
| From emergency call to first paramedic arrival | 8 (5-11) | 7 (5-11) |
| From first paramedic arrival to trial paramedic arrivalb | 0 (0-4) | 1 (0-4) |
| Presenting rhythm | ||
| Asystole | 2356/4316 (54.6) | 2597/4791 (54.2) |
| Ventricular fibrillation | 979/4316 (22.7) | 1094/4791 (22.8) |
| Pulseless ventricular tachycardia | 44/4316 (1.0) | 39/4791 (0.8) |
| Pulseless electrical activity | 937/4316 (21.7) | 1061/4791 (22.1) |
| Witnessed cardiac arrest | 2788/4407 (63.3) | 3101/4883 (63.5) |
| Witnessed by a bystander | 2231/2788 (80.0) | 2493/3100 (80.4) |
| Witnessed by a paramedic | 557/2788 (20.0) | 607/3100 (19.6) |
| Type of bystander or responder action | ||
| CPR before paramedic arrival | 2774/4406 (63.0) | 3149/4883 (64.5) |
| Defibrillation before paramedic arrivalc | 146/4390 (3.3) | 176/4863 (3.6) |
| Return of spontaneous circulation achieved | 20/146 (13.7) | 27/176 (15.3) |
| At Arrival of Study Paramedic | ||
| Airway management in progress | 1384/4389 (31.5) | 1463/4863 (30.1) |
| Type of airway management | ||
| Bag-mask ventilation only | 273/1383 (19.7) | 307/1463 (21.0) |
| Oropharyngeal airway and bag-mask ventilation | 766/1383 (55.4) | 875/1463 (59.8) |
| Nasopharyngeal airway and bag-mask ventilation | 11/1383 (0.8) | 11/1463 (0.8) |
| Trial supraglottic airway device | 262/1383 (18.9) | 190/1463 (13.0) |
| Intubation | 3/1383 (0.2) | 3/1463 (0.2) |
| Other supraglottic airway device | 44/1383 (3.2) | 57/1463 (3.9) |
| Mouth-to-mouth resuscitation | 8/1383 (0.6) | 10/1463 (0.7) |
| Face shield or pocket mask | 5/1383 (0.4) | 4/1463 (0.3) |
| Suction | 3/1383 (0.2) | 2/1463 (0.1) |
| Other | 8/1383 (0.6) | 4/1463 (0.3) |
| Ongoing successful ventilation | 1110/1372 (80.9) | 1154/1455 (79.3) |
| Return of spontaneous circulation | 300/4393 (6.8) | 328/4862 (6.8) |
Abbreviations: CPR, cardiopulmonary resuscitation; IQR, interquartile range.
Unless otherwise indicated. Patients are grouped by the randomization assignment of the first study paramedic on the scene.
There were missing data for 3 patients randomized to tracheal intubation and 1 patient randomized to the study supraglottic airway device.
This was achieved using an automated external defibrillator available at the scene.
Enrolled patients were transported to 95 hospitals and followed up to hospital discharge. Follow-up ended in February 2018. The randomization of paramedics was well balanced (759 to the supraglottic airway device group and 764 to the tracheal intubation group). There were 113 paramedics who withdrew after randomization (58 randomized to tracheal intubation and 55 randomized to the supraglottic airway device; additional information appears in the eText in Supplement 2).
There were more patients in the supraglottic airway device group (n = 4886) than in the tracheal intubation group (n = 4410). The proportion of patients with out-of-hospital cardiac arrest was similar in the 2 groups for attempted resuscitation (7007 of 13 587 patients [51.6%] in the supraglottic airway device group vs 6455 of 12 789 patients [50.5%] in the tracheal intubation group) and eligibility (4886 of 7006 patients [69.7%] in the supraglottic airway device group vs 4410 of 6454 [68.3%] in the tracheal intubation group).
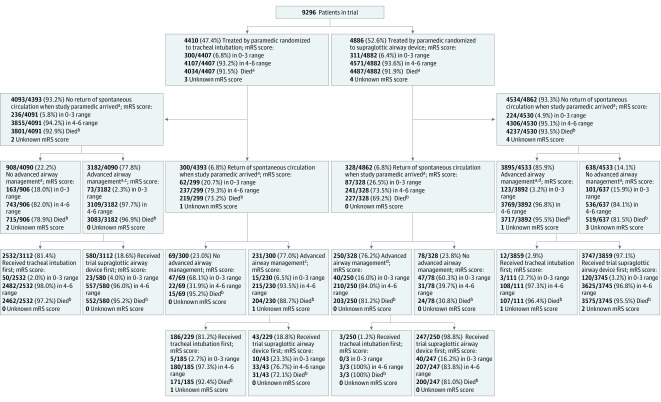
The patient characteristics and cardiac arrest details were balanced between the groups (Table 1; eTables 1 and 2 in Supplement 2). Patients randomized to tracheal intubation were more likely to crossover to the supraglottic airway device as a result of a clinical decision made by the paramedic on scene (Figure 2; eTable 3 and eFigure 1 [contains further information regarding return of spontaneous circulation during or after advanced airway management] in Supplement 2).
Figure 2. Patient Interventions and Outcomes by Trial Randomization Assignment of Study Paramedics.
aThere were missing data (see eText in Supplement 2).
bHad modified Rankin Scale (mRS) score of 6.
cThere were 72 patients (2.1%) in tracheal intubation group treated only with a nontrial supraglottic airway device (SGA; all had mRS score in 4-6 range; 2 had return of spontaneous circulation at paramedic arrival; 71 deaths).
dThere were 36 patients (0.9%) in SGA group treated only with a nontrial SGA (all had mRS score in 4-6 range; 35 deaths).
Primary Outcome
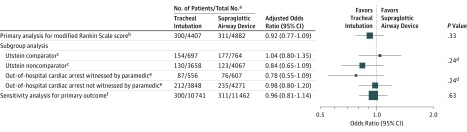
The primary outcome was available for 9289 of 9296 patients (99.9%; Table 2). In the supraglottic airway device group, 311 of 4882 patients (6.4%) had a good outcome (modified Rankin Scale score range, 0-3) vs 300 of 4407 patients (6.8%) in the tracheal intubation group (adjusted OR, 0.92 [95% CI, 0.77 to 1.09]; adjusted risk difference [supraglottic airway device minus tracheal intubation], −0.6% [95% CI, −1.6% to 0.4%]; Figure 3 and eFigure 2 in Supplement 2).
Table 2. Primary Outcome, Survival Status, and Main Secondary Outcomes.
| No. of Patients/Total No. (%)a | Adjusted Estimate (95% CI)b |
P Valuec | ICC | Adjusted Risk Difference Estimate (95% CI), %b |
P Valuec | ||
|---|---|---|---|---|---|---|---|
| Tracheal Intubation (n = 4410) |
Supraglottic Airway Device (n = 4886) |
||||||
| Primary Outcome: Modified Rankin Scale Score at Hospital Discharge or 30 d | |||||||
| 0-3 range (good outcome) | 300/4407 (6.8) | 311/4882 (6.4) | OR, 0.92 (0.77 to 1.09) | .33 | 0.05 | −0.6 (−1.6 to 0.4) | .24 |
| 0 (no symptoms) | 124/4407 (2.8) | 117/4882 (2.4) | |||||
| 1 | 48/4407 (1.1) | 41/4882 (0.8) | |||||
| 2 | 50/4407 (1.1) | 58/4882 (1.2) | |||||
| 3 | 78/4407 (1.8) | 95/4882 (1.9) | |||||
| 4-6 range (poor outcome to death) | 4107/4407 (93.2) | 4571/4882 (93.6) | |||||
| 4 | 46/4407 (1.0) | 45/4882 (0.9) | |||||
| 5 | 27/4407 (0.6) | 39/4882 (0.8) | |||||
| 6 (died) | 4034/4407 (91.5) | 4487/4882 (91.9) | |||||
| Secondary Outcomes | |||||||
| Survival status | |||||||
| Died at scene | 2488/4407 (56.5) | 2623/4882 (53.7) | |||||
| Died prior to ICU admission | 1058/4407 (24.0) | 1226/4882 (25.1) | |||||
| Died prior to ICU discharge | 369/4407 (8.4) | 503/4882 (10.3) | |||||
| Died prior to hospital discharge | 120/4407 (2.7) | 138/4882 (2.8) | |||||
| Survived to 30 d or hospital discharge | 372/4407 (8.4) | 392/4882 (8.0) | |||||
| Time to death | |||||||
| No. of patientsd | 4400 | 4871 | |||||
| Median (IQR), min | 63 (41 to 216) | 67 (41 to 267) | HR, 0.97 (0.93 to 1.02) | .22 | |||
| Time to death was 0-72 h | |||||||
| No. of patientsd | 4400 | 4871 | |||||
| Median (IQR), min | 63 (41 to 205) | 67 (41 to 246) | HR, 0.96 (0.92 to 1.00) | .07 | |||
| 72-h Survival | 575/4395 (13.1) | 664/4872 (13.6) | OR, 1.04 (0.92 to 1.18) | .54 | 0.02 | 0.4 (−1.0 to 1.9) | .54 |
| Initial ventilation success (≤2 attempts at advanced airway management) | 3473/4397 (79.0) | 4255/4868 (87.4) | OR, 1.92 (1.66 to 2.22) | <.001 | 0.12 | 8.3 (6.3 to 10.2) | <.001 |
| Tracheal intubation | 1891/2723 (69.4) | 92/116 (79.3) | |||||
| Trial supraglottic airway device | 542/617 (87.8) | 3412/3994 (85.4) | |||||
| Other supraglottic airway device | 55/72 (76.4) | 29/36 (80.6) | |||||
| Any unintended loss of a previously established airwaye | 153/3081 (5.0) | 412/3900 (10.6) | OR, 2.29 (1.86 to 2.82) | <.001 | 0.07 | 5.9 (4.6 to 7.2) | <.001 |
| Tracheal intubation | 70/2149 (3.3) | 33/570 (5.8) | |||||
| Trial supraglottic airway device | 84/981 (8.6) | 389/3455 (11.3) | |||||
| Other supraglottic airway device | 5/171 (2.9) | 3/33 (9.1) | |||||
| Regurgitation at any time | 1072/4372 (24.5) | 1268/4865 (26.1) | OR, 1.08 (0.96 to 1.20) | .21 | 0.06 | 1.4 (−0.6 to 3.4) | .17 |
| Aspiration at any time | 647/4337 (14.9) | 729/4824 (15.1) | OR, 1.01 (0.88 to 1.16) | .84 | 0.08 | 0.1 (−1.5 to 1.8) | .86 |
| Initial attempt with supraglottic airway device or tracheal intubation | |||||||
| Regurgitation before | 923/4379 (21.1) | 846/4869 (17.4) | |||||
| Aspiration before | 589/4355 (13.5) | 532/4840 (11.0) | |||||
| Regurgitation during or after | 543/4361 (12.5) | 875/4857 (18.0) | |||||
| Aspiration during or after | 304/4344 (7.0) | 473/4829 (9.8) | |||||
| Admitted to ED or hospital | 1922/4410 (43.6) | 2263/4886 (46.3) | |||||
| Return of spontaneous circulation at arrival to ED or hospital | 1249/4404 (28.4) | 1495/4880 (30.6) | OR, 1.12 (1.02 to 1.23) | .02 | 0.01 | 2.2 (0.3 to 4.2) | .03 |
| Survived to ED discharge | 861/1919 (44.9) | 1033/2259 (45.7) | |||||
Abbreviations: ED, emergency department; HR, hazard ratio; ICC, intracluster correlation coefficient; ICU, intensive care unit; IQR, interquartile range; OR, odds ratio.
Unless otherwise indicated. Patients are grouped by the randomization assignment of the first study paramedic on the scene.
The ORs and risk differences were adjusted for stratification factors fitted as fixed effects. The ORs were obtained from a mixed-effects logistic regression model with study paramedic fitted as a random effect. Risk differences were obtained by fitting a generalized linear model (binomial family and identity link) and standard errors adjusted for clustering. The HRs were adjusted for paramedic experience and distance from usual hospital and stratified by emergency medical services provider organization and standard errors adjusted for clustering.
The Wald test was used to make comparisons.
Patients who survived to ICU discharge but did not consent to active or passive follow-up were censored at ICU discharge because research approvals did not permit analysis of subsequent data apart from the modified Rankin Scale score.
Had at least 1 advanced airway management attempt.
Figure 3. Forest Plot of Primary and Subgroup Analyses.
The area of the squares is proportional to the number of patients included. The odds ratios were estimated from a mixed-effects logistic regression model with stratification factors fitted as fixed effects and study paramedic as a random effect. The Wald test was used for the P value comparisons. Patients are grouped by the randomization assignment of the first study paramedic on the scene. A breakdown of the modified Rankin Scale scores in the form of horizontally stacked bar charts appears in eFigure 2 in Supplement 2.
aNo. of patients with a modified Rankin Scale score in the range of 0 to 3 (good outcome).
bThere were missing data for 7 patients (3 in the tracheal intubation group and 4 in the supraglottic airway device group).
cThe Utstein comparator includes patients with an out-of-hospital cardiac arrest with a likely cardiac cause that is witnessed and has an initial rhythm amenable to defibrillation. For the Utstein comparator and noncomparator analyses, there were missing data for 103 patients (52 in the tracheal intubation group and 51 in the supraglottic airway device group).
dIndicates a P value for interaction.
eThe not witnessed group includes all arrests not witnessed by a study paramedic. For the witnessed and not witnessed analyses, there were missing data for 7 patients (3 in the tracheal intubation group and 4 in the supraglottic airway device group).
fIncludes patients treated by a study paramedic who were not resuscitated. There were missing data for 4 patients (1 in the tracheal intubation group and 3 in the supraglottic airway device group).
Exploratory Sensitivity and Subgroup Analyses for the Primary Outcome
Including patients treated by a participating paramedic who were not resuscitated did not change the conclusion for the primary outcome (311 of 11 462 patients [2.7%] in the supraglottic airway device vs 300 of 10 741 patients [2.8%] in the tracheal intubation group had a good outcome; adjusted OR, 0.96 [95% CI, 0.81 to 1.14]; risk difference, −0.2% [95% CI, −0.6% to 0.3%]; Figure 3 and eTable 4 in Supplement 2).
However, of the 7576 (81%) patients who received advanced airway management, more patients in the supraglottic airway device group had a good outcome (163 of 4158 patients [3.9%] vs 88 of 3418 patients [2.6%] in the tracheal intubation group; adjusted OR, 1.57 [95% CI, 1.18 to 2.07]; risk difference, 1.4% [95% CI, 0.5% to 2.2%]).
This effect also was observed in the analysis of patients grouped according to the first type of advanced airway management intervention received (193 of 4630 patients [4.2%] in the supraglottic airway device group vs 58 of 2838 patients [2.0%] in the tracheal intubation group; adjusted OR, 2.06 [95% CI, 1.51 to 2.81]; risk difference, 2.1% [95% CI, 1.2% to 2.9%]).
There was no interaction between randomization group and either subgroup (Figure 3; Utstein comparator group vs Utstein noncomparator group, P = .24; out-of-hospital cardiac arrest witnessed by a paramedic vs not witnessed by a paramedic, P = .24).
Secondary Outcomes
The secondary outcomes appear in Table 2 and in eTable 5 in Supplement 2. The supraglottic airway device treatment strategy was significantly more successful in achieving ventilation after up to 2 attempts (4255 of 4868 patients [87.4%] vs 3473 of 4397 patients [79.0%] with tracheal intubation; adjusted OR, 1.92 [95% CI, 1.66 to 2.22]; risk difference, 2.1% [95% CI, 1.2% to 2.9%]).
Two of the secondary outcomes (regurgitation and aspiration) were not significantly different between groups when all instances occurring before, during, or after advanced airway management were combined. Regurgitation occurred among 1268 of 4865 patients (26.1%) in the supraglottic airway device group compared with 1072 of 4372 patients (24.5%) in the tracheal intubation group (adjusted OR, 1.08 [95% CI, 0.96 to 1.20]; adjusted risk difference, 1.4% [95% CI, −0.6% to 3.4%]). Aspiration occurred among 729 of 4824 patients (15.1%) in the supraglottic airway device group compared with 647 of 4337 patients (14.9%) in the tracheal intubation group (adjusted OR, 1.01 [95% CI, 0.88 to 1.16]; adjusted risk difference, 0.1% [95% CI, −1.5% to 1.8%]).
The median time to death was not significantly different between the groups (67 minutes for the supraglottic airway device in 4871 patients vs 63 minutes for tracheal intubation in 4400 patients), and neither was the compression fraction in a very small sample of 66 patients (median of 86% [interquartile range, 81%-91%] in 34 patients for the supraglottic airway device vs median of 83% [interquartile range, 74%-89%] in 32 patients for tracheal intubation (P = .14; eTable 6 in Supplement 2).
Discussion
In this pragmatic, multicenter, cluster RCT, no significant difference was found between tracheal intubation and the supraglottic airway device for the primary outcome of modified Rankin Scale score (range, 0-3; good outcome) at hospital discharge or 30 days after an out-of-hospital cardiac arrest for all trial patients.
Patients with a short duration of cardiac arrest and who receive bystander resuscitation, defibrillation, or both, are considerably more likely to survive and are also less likely to require advanced airway management.22 This problem of confounding by indication is an important limitation of many large observational studies that show an association between advanced airway management and poor outcome in out-of-hospital cardiac arrest.23 This study found that 21.1% (360/1704) of patients who did not receive advanced airway management achieved a good outcome compared with 3.3% (251/7576) of patients who received advanced airway management.
Paramedics randomized to use tracheal intubation were less likely to use advanced airway management than paramedics randomized to use the supraglottic airway device. Tracheal intubation is a more complex skill than supraglottic airway device insertion and requires 2 practitioners, additional equipment, and good access to the patient’s airway24; however, out-of-hospital cardiac arrest often occurs in locations where patient access is challenging.
Tracheal intubation has been associated with potential harms including unrecognized esophageal intubation, lengthy pauses in chest compressions, and overventilation.25,26 No evidence of a difference in compression fraction was found in a small subsample of the enrolled patients, but the potential for harm associated with tracheal intubation persists.
At the outset, it was expected that most patients with a favorable outcome would not receive advanced airway management, and that some crossover would occur. For these reasons, 2 exploratory sensitivity analyses were prespecified only in patients who received advanced airway management, even though these analyses are susceptible to bias.27
Patients who received advanced airway management were similar in the 2 groups (eTable 1 and eTable 2 in Supplement 2), and a strategy of using a supraglottic airway device first was associated with better outcomes whenever advanced airway management was undertaken by a trial paramedic (eTable 4); however, the between-group difference was less than the prespecified clinically important difference and less than the minimally important difference of approximately 3% reported by others.28
The strategy of using a supraglottic airway device first also achieved initial ventilation success more often. Although regurgitation and aspiration occurred with similar frequency overall, regurgitation and aspiration during or after advanced airway management were significantly more common in the supraglottic airway device group. Conversely, patients in the tracheal intubation group were significantly more likely to regurgitate and aspirate before advanced airway management, possibly due to less frequent use of advanced techniques to secure the airway in this group and the increased time required for tracheal intubation compared with insertion of a supraglottic airway device.
A recent RCT of French and Belgian patients with out-of-hospital cardiac arrest that compared bag-mask ventilation with tracheal intubation delivered by physicians as part of an EMS team proved inconclusive.29 To our knowledge, no RCT has compared bag-mask ventilation with a supraglottic airway device in patients with out-of-hospital cardiac arrest.
Reported rates of ventilation and tracheal intubation success have been higher in previous studies29,30,31; however, these rates were based on selected populations and practitioners with greater training and experience, including physicians. The current study reflects both the reality of current paramedic practice in England, and the challenges of airway management in a patient group for which regurgitation and poor airway access are common.
Any unintended loss of a previously established airway occurred twice as frequently in the supraglottic airway device group than in the tracheal intubation group. There are some patients with cardiac arrest for whom effective ventilation cannot be achieved with basic airway management techniques or with a supraglottic airway device, and for whom tracheal intubation may be the only way of achieving effective ventilation. The exact role of different advanced airway management techniques in adults with out-of-hospital cardiac arrest, and the associated implications for skill acquisition and maintenance, remain to be determined.
Limitations
This study has several limitations. First, the trial population included patients who did and did not receive advanced airway management, and the use of advanced airway management was greater among paramedics in the supraglottic airway device group compared with those in the tracheal intubation group, which could result in confounding by indication.32
Second, there was an imbalance in the number of patients in the 2 groups, probably due to unequal distribution of a small number of paramedics who recruited considerably more patients than the average; however, it was not possible to stratify for this because these individuals could not be identified in advance.
Third, there was crossover between groups, which was inevitable on practical and ethical grounds.
Fourth, although other elements of care (eg, initial basic airway management and subsequent on-scene and in-hospital care, such as targeted temperature management and access to angiography) followed established guidelines, between-group differences in these factors could have influenced the findings.
Fifth, the participating paramedics were volunteers, and their airway skills may not be representative of those who chose not to participate in the study.
Sixth, the findings are applicable to use of the particular supraglottic airway device in countries with similar EMS provision to England where paramedics treat most patients with out-of-hospital cardiac arrest. The findings may not be applicable in countries with physician-led EMS provision or to another supraglottic airway device that may have different characteristics. However, the principles underpinning the insertion and function of all supraglottic airway devices are similar.
Conclusions
Among patients with out-of-hospital cardiac arrest, randomization to a strategy of advanced airway management with a supraglottic airway device compared with tracheal intubation did not result in a favorable functional outcome at 30 days.
Trial protocol and statistical analysis plan
eText. Further information relating to Figure 1 and Figure 2
eTable 1. Patient demography and cardiac arrest details of trial patients, by allocated intervention and use of airway management
eTable 2. Patient demography and cardiac arrest details of trial patients who received at least one advanced airway management attempt, by first intervention received
eTable 3. Protocol deviations
eTable 4. Sensitivity analyses for primary outcome (modified Rankin Scale (mRS) score at discharge or 30 days)
eTable 5. Additional secondary outcomes
eTable 6. Compression fraction (used in two ambulance trusts for a subset of patients)
eTable 7. Risk ratios for the primary and secondary outcomes and the sensitivity analyses
eFigure 1. Interventions received and patient outcome by study allocation extended
eFigure 2. Breakdown of mRS scores for the main and sensitivity analyses
References
- 1.Hawkes C, Booth S, Ji C, et al. ; OHCAO Collaborators . Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017;110:133-140. doi: 10.1016/j.resuscitation.2016.10.030 [DOI] [PubMed] [Google Scholar]
- 2.Jentzer JC, Clements CM, Wright RS, White RD, Jaffe AS. Improving survival from cardiac arrest: a review of contemporary practice and challenges. Ann Emerg Med. 2016;68(6):678-689. doi: 10.1016/j.annemergmed.2016.05.022 [DOI] [PubMed] [Google Scholar]
- 3.Monsieurs KG, Nolan JP, Bossaert LL, et al. ; ERC Guidelines 2015 Writing Group . European Resuscitation Council guidelines for resuscitation 2015: section 1: executive summary. Resuscitation. 2015;95:1-80. doi: 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 4.Gwinnutt CL. Should we intubate patients during cardiopulmonary resuscitation? BMJ. 2017;357:j1772. doi: 10.1136/bmj.j1772 [DOI] [PubMed] [Google Scholar]
- 5.Soar J, Nolan JP. Airway management in cardiopulmonary resuscitation. Curr Opin Crit Care. 2013;19(3):181-187. doi: 10.1097/MCC.0b013e328360ac5e [DOI] [PubMed] [Google Scholar]
- 6.Hasegawa K, Hiraide A, Chang Y, Brown DFM. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309(3):257-266. doi: 10.1001/jama.2012.187612 [DOI] [PubMed] [Google Scholar]
- 7.Fouche PF, Simpson PM, Bendall J, Thomas RE, Cone DC, Doi SA. Airways in out-of-hospital cardiac arrest: systematic review and meta-analysis. Prehosp Emerg Care. 2014;18(2):244-256. doi: 10.3109/10903127.2013.831509 [DOI] [PubMed] [Google Scholar]
- 8.Kurola J, Harve H, Kettunen T, et al. Airway management in cardiac arrest—comparison of the laryngeal tube, tracheal intubation and bag-valve mask ventilation in emergency medical training. Resuscitation. 2004;61(2):149-153. doi: 10.1016/j.resuscitation.2004.01.014 [DOI] [PubMed] [Google Scholar]
- 9.Cook T, Howes B. Supraglottic airway devices: recent advances. Contin Educ Anaesth Crit Care Pain. 2011;11(2):56-61. doi: 10.1093/bjaceaccp/mkq058 [DOI] [Google Scholar]
- 10.Wang HE, Szydlo D, Stouffer JA, et al. ; ROC Investigators . Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation. 2012;83(9):1061-1066. doi: 10.1016/j.resuscitation.2012.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor J, Black S, J Brett S, et al. Design and implementation of the AIRWAYS-2 trial: a multi-centre cluster randomised controlled trial of the clinical and cost effectiveness of the i-gel supraglottic airway device versus tracheal intubation in the initial airway management of out of hospital cardiac arrest. Resuscitation. 2016;109:25-32. doi: 10.1016/j.resuscitation.2016.09.016 [DOI] [PubMed] [Google Scholar]
- 12.Joint Royal Colleges Ambulance Liaison Committee Clinical Practice Guidelines: 2016. London, England: Class Publishing; 2016. [Google Scholar]
- 13.Duckett J, Fell P, Han K, Kimber C, Taylor C. Introduction of the I-gel supraglottic airway device for prehospital airway management in a UK ambulance service. Emerg Med J. 2014;31(6):505-507. doi: 10.1136/emermed-2012-202126 [DOI] [PubMed] [Google Scholar]
- 14.Häske D, Schempf B, Gaier G, Niederberger C. Performance of the i-gel™ during pre-hospital cardiopulmonary resuscitation. Resuscitation. 2013;84(9):1229-1232. doi: 10.1016/j.resuscitation.2013.04.025 [DOI] [PubMed] [Google Scholar]
- 15.Whitehead L, Perkins GD, Clarey A, Haywood KL. A systematic review of the outcomes reported in cardiac arrest clinical trials: the need for a core outcome set. Resuscitation. 2015;88:150-157. doi: 10.1016/j.resuscitation.2014.11.013 [DOI] [PubMed] [Google Scholar]
- 16.Rittenberger JC, Raina K, Holm MB, Kim YJ, Callaway CW. Association between cerebral performance category, modified Rankin Scale, and discharge disposition after cardiac arrest. Resuscitation. 2011;82(8):1036-1040. doi: 10.1016/j.resuscitation.2011.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christenson J, Andrusiek D, Everson-Stewart S, et al. ; Resuscitation Outcomes Consortium Investigators . Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241-1247. doi: 10.1161/CIRCULATIONAHA.109.852202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benger J, Coates D, Davies S, et al. Randomised comparison of the effectiveness of the laryngeal mask airway supreme, i-gel and current practice in the initial airway management of out of hospital cardiac arrest: a feasibility study. Br J Anaesth. 2016;116(2):262-268. [DOI] [PubMed] [Google Scholar]
- 19.Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83(3):313-319. doi: 10.1016/j.resuscitation.2011.10.028 [DOI] [PubMed] [Google Scholar]
- 20.Perkins GD, Jacobs IG, Nadkarni VM, et al. ; Utstein Collaborators . Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for out-of-hospital cardiac arrest. Resuscitation. 2015;96:328-340. doi: 10.1016/j.resuscitation.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 21.Schulz KF, Grimes DA. Multiplicity in randomised trials I: endpoints and treatments. Lancet. 2005;365(9470):1591-1595. doi: 10.1016/S0140-6736(05)66461-6 [DOI] [PubMed] [Google Scholar]
- 22.Andersen LW, Grossestreuer AV, Donnino MW. Resuscitation time bias—a unique challenge for observational cardiac arrest research. Resuscitation. 2018;125:79-82. doi: 10.1016/j.resuscitation.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carlson JN, Reynolds JC. Does advanced airway management improve outcomes in adult out-of-hospital cardiac arrest? Ann Emerg Med. 2014;64(2):163-164. doi: 10.1016/j.annemergmed.2013.12.003 [DOI] [PubMed] [Google Scholar]
- 24.Higgs A, McGrath BA, Goddard C, et al. ; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists . Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323-352. doi: 10.1016/j.bja.2017.10.021 [DOI] [PubMed] [Google Scholar]
- 25.Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med. 2009;54(5):645-652.e1. doi: 10.1016/j.annemergmed.2009.05.024 [DOI] [PubMed] [Google Scholar]
- 26.Kramer-Johansen J, Wik L, Steen PA. Advanced cardiac life support before and after tracheal intubation—direct measurements of quality. Resuscitation. 2006;68(1):61-69. doi: 10.1016/j.resuscitation.2005.05.020 [DOI] [PubMed] [Google Scholar]
- 27.Swanson SA, Robins JM, Miller M, Hernán MA. Selecting on treatment: a pervasive form of bias in instrumental variable analyses. Am J Epidemiol. 2015;181(3):191-197. doi: 10.1093/aje/kwu284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nichol G, Brown SP, Perkins GD, et al. What change in outcomes after cardiac arrest is necessary to change practice? results of an international survey. Resuscitation. 2016;107:115-120. doi: 10.1016/j.resuscitation.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 29.Jabre P, Penaloza A, Pinero D, et al. Effect of bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after out-of-hospital cardiorespiratory arrest: a randomized clinical trial. JAMA. 2018;319(8):779-787. doi: 10.1001/jama.2018.0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hubble MW, Brown L, Wilfong DA, Hertelendy A, Benner RW, Richards ME. A meta-analysis of prehospital airway control techniques part I: orotracheal and nasotracheal intubation success rates. Prehosp Emerg Care. 2010;14(3):377-401. doi: 10.3109/10903121003790173 [DOI] [PubMed] [Google Scholar]
- 31.Dyson K, Bray JE, Smith K, et al. Paramedic intubation experience is associated with successful tube placement but not cardiac arrest survival. Ann Emerg Med. 2017;70(3):382-390.e1. doi: 10.1016/j.annemergmed.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 32.Kyriacou DN, Lewis RJ. Confounding by indication in clinical research. JAMA. 2016;316(17):1818-1819. doi: 10.1001/jama.2016.16435 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial protocol and statistical analysis plan
eText. Further information relating to Figure 1 and Figure 2
eTable 1. Patient demography and cardiac arrest details of trial patients, by allocated intervention and use of airway management
eTable 2. Patient demography and cardiac arrest details of trial patients who received at least one advanced airway management attempt, by first intervention received
eTable 3. Protocol deviations
eTable 4. Sensitivity analyses for primary outcome (modified Rankin Scale (mRS) score at discharge or 30 days)
eTable 5. Additional secondary outcomes
eTable 6. Compression fraction (used in two ambulance trusts for a subset of patients)
eTable 7. Risk ratios for the primary and secondary outcomes and the sensitivity analyses
eFigure 1. Interventions received and patient outcome by study allocation extended
eFigure 2. Breakdown of mRS scores for the main and sensitivity analyses