Key Points
Question
What is the prevalence of noise-induced hearing loss among children aged 9 to 11 years in the Netherlands?
Findings
In this cross-sectional, population-based study among 3316 children with normal middle-ear function, audiometry data showed the prevalence of audiometric notches and high-frequency hearing loss was 14.2%. Portable music players, used by 40.0% of the cohort, were associated with high-frequency hearing loss.
Meaning
Signs of noise-induced hearing loss may already be present in children aged 9 to 11 years old and may be associated with portable music player use prior to exposure to known noise hazards, such as club and concert attendance.
Abstract
Importance
Portable music player use may have harmful effects on hearing. The magnitude and effect of frequent music exposure, especially at younger ages, on hearing are unclear.
Objectives
To examine the prevalence of noise-induced hearing loss in a 9- to 11-year-old population and associations with portable music player use and sociodemographic factors.
Design, Setting, and Participants
A cross-sectional study within an ongoing, prospective, birth cohort study within Rotterdam, the Netherlands was conducted. Between ages 9 and 11 years, 5355 children underwent their first audiometric evaluation. Children were excluded if they had missing or failed tympanometry results. The study was conducted from April 16, 2012, to October 25, 2015.
Exposures
Portable music player (PMP) use and sociodemographic factors assessed via parental questionnaires.
Main Outcomes and Measures
Hearing acuity measured by pure-tone audiometry at 0.5 to 8 kHz. Possible noise-induced hearing loss was contingent on a high-frequency notch and/or high-frequency hearing loss in the audiogram, or reported hearing-related symptoms.
Results
The final sample included 3116 participants who were a mean (interquartile range) age of 9.7 (9.6-9.9) years and equally distributed between boys (1550 [49.7%]) and girls (1566 [50.3%]). Of these, 1244 (39.9%) reported no PMP use, 577 (18.5%) reported use 1 or 2 days per week, 254 (8.2%) reported use 3 or more days per week, and for 1041 (33.4%), PMP use was not reported. Audiometric notches and high-frequency hearing loss were present in 443 (14.2%) of all children; 140 (4.5%) fulfilled the criteria of a notch, 238 (7.6%) of high-frequency hearing loss, and 65 (2.1%) of both. Of the cohort, 52 (1.7%) showed bilateral impairment. Hearing-related symptoms were reported for 232 (11.3%) of the respondents, and 831 (40.0%) of the respondents used portable music players. Portable music player use was associated with high-frequency hearing loss (odds ratio [OR], 2.88; 95% CI, 1.36-6.980 for 1 or 2 days per week and OR, 2.74; 95% CI, 1.22-6.96 for ≥3 days per week), but listening time and duration were not. There was no association of music exposure with high-frequency notches.
Conclusions and Relevance
In this study, 14.2% of school-aged children showed audiometric notches or high-frequency hearing loss. This hearing impairment is already present prior to exposure to known noise hazards, such as club and concert attendance, and may have lifelong consequences. Repeated measurements are needed to confirm the association of portable music player use with hearing impairment in children.
This population-based study examines the presence of early hearing loss in school-aged children in the Netherlands and its association with use of portable music players.
Introduction
Hearing loss is a major public health problem.1,2,3,4 Cumulative exposure to music or noise damages cochlear hair cells and synapses, which results in irreversible hearing loss and therefore a lifetime disability.5,6 Early exposure might lead to an increase of clinically relevant noise-induced hearing loss (NIHL) at younger ages and to more severe hearing loss in later life.7 Noise-induced hearing loss is considered to be a cumulative process and is often presented as a temporary or permanent notch around 3, 4, or 6 kHz in the audiogram, but higher frequencies have been shown to be affected as well.8,9 In addition, hearing-related symptoms, such as tinnitus or increased sensitivity for certain sounds, are often reported.10,11 Previous studies reported a prevalence of 0.9% to 16.8% of NIHL9,12 and up to 69% of noise-induced hearing-related symptoms9 in children, adolescents, and young adults. This prevalence suggests that harmful effects of frequent exposure to loud sounds through headphones might be present in children already.9
Portable music players (PMPs), including mobile phones and tablets, in combination with headphones are embedded in daily life and serve educational purposes in schools. Approximately 93.3% of children and adolescents between ages 12 and 19 years are reported to use PMPs on a daily basis.11 Moreover, up to 58.2% of mostly young adult PMP users exceed the recommended maximum noise dose.13 Attention for NIHL has risen and prevention programs have been launched. Evidence of the presence of NIHL among younger children is scarce.9,14,15 The previously published data on NIHL prevalence needs confirmation, and large-scale data on the European population are lacking.16 The Scientific Committee on Emerging and Newly Identified Health Risks emphasized the importance of more data on current PMP use and its association with hearing impairment (HI), as well as identifying potential subgroups more at risk.
In a population-based, prospective cohort study in Rotterdam, the Netherlands, our overall aim was to examine the prevalence and development of NIHL among children over time. As a first step, the present cross-sectional study assessed audiometric features possibly fitting NIHL among school-aged children. Subsequently, we intended to study the associations between PMP use and sociodemographic factors with possible signs of NIHL at this early age.
Methods
Study Design and Study Sample
This study was nested in the Generation R Study, a population-based, prospective cohort study in Rotterdam, the Netherlands, that commenced in 2002 and monitors its participants from early fetal life at least until young adulthood.17 Physical assessment at age 9 to 11 years was the first evaluation to include audiometry, among many other measurements.18,19 Although most participants completed all of these measurements during the extensive examination, some were incomplete because of, for example, lack of time, technical issues, or personal circumstances. All children who completed pure-tone audiometry at all frequencies were eligible for inclusion in the present study. In addition, participants were excluded on the basis of missing tympanometry data or in case of failed tympanometry testing in either ear, as discussed below. Oral and written informed consent of the parents was collected for all measurements. There was no financial compensation. The study has been approved by the Medical Ethics Committee of the Erasmus Medical Center, Rotterdam, the Netherlands.
Audiologic Measures and Definitions
Hearing acuity was assessed at age 9 to 11 years. Data were collected between April 16, 2012, and October 25, 2015. The participants underwent air-conduction pure-tone audiometry (at 0.5, 1, 2, 3, 4, 6, and 8 kHz) and tympanometry in an audio booth meeting the maximum permissible ambient sound pressure levels of International Organization for Standardization 8253-1. Testing was conducted by research assistants, trained by a member of the Speech and Hearing Center, using the shortened ascending method as described in more detail by le Clercq et al.19 Tympanometry was used to assess middle ear function. An ear canal volume of 0.3 mL or lower, compliance of 0.2 mL or lower, or middle ear pressure below −150 da Pascal was considered as a failed tympanogram consistent with the study of Henderson et al12 on NIHL. Failed tympanometry could represent external or middle ear pathology, such as potential ear canal collapse, impacted cerumen, or conductive hearing loss. Such abnormalities could be associated with the results owing to an overestimation of hearing impairment.20 Therefore, participants who had missing or failed tympanometry in either ear were excluded from the analyses.
Audiometric signs that possibly fit NIHL were defined as the presence of a notched audiogram or high-frequency hearing loss (HFHL) in either ear (eFigure in the Supplement). A high-frequency notch was defined from the criteria described by Niskar et al,21 which include (1) thresholds at 0.5 and 1 kHz of 15 dB or less HL; (2) the poorest threshold at 3, 4, or 6 kHz must be 15 dB or more higher (poorer) than the poorest threshold for 0.5 and 1 kHz; and (3) the threshold at 8 kHz must be 10 dB or more lower (better) than the poorest threshold for 3, 4, or 6 kHz. Participants were studied for the presence of no, unilateral, or bilateral notch. When these characteristics were present, but there was insufficient recovery of the hearing threshold at 8 kHz, the audiogram often fulfilled the criteria of HFHL. We defined HFHL as a hearing threshold 15 dB or less HL at 0.5 and 1 kHz and an average threshold of 3, 4, 6, and 8 kHz greater than 15 dB HL. Both notches and HFHL were categorized in degree of HI that is a notch with on average normal hearing (≤15 dB HL), slight notch or HFHL (16 to 25 dB HL), mild notch or HFHL (26 to 40 dB HL), and moderate to profound notch or HFHL (≥41 dB HL).
The presence of hearing-related symptoms was assessed using a cross-sectional parent questionnaire, namely, whether the child ever reported temporary hearing problems, such as ringing, decreased hearing, sensitivity to loud noises, or sound distortion. The presence of these hearing-related symptoms was additionally explored as a possible sign of early NIHL.
Music Exposure and PMP Use
Parent questionnaires when children were aged 9 to 11 years included questions on PMP use by the participants. Parents were asked about the average frequency per week that their children listened to music with headphones, the listening time on an average day, and the usual volume level of the PMP.
Sociodemographic Characteristics
Sociodemographic characteristics were included based on a previous study19 and included factors potentially associated with NIHL and listening behavior.12 Demographic information of the participants (sex, age, ethnicity) and information on maternal educational level and household income were collected via questionnaires at different time points.18 Ethnicity was grouped as Western and non-Western. Maternal education and household income were used as markers of socioeconomic status. Maternal education was grouped as no or primary education finished, secondary education finished, higher vocational education finished, or university education finished. Household income was grouped as low, middle, or high based on study sample tertiles. Because of the previously found association between a history of recurrent otitis media and HI within this cohort,19 the analyses were adjusted for having no, a history of (but not recurrent), or a recurrent history of otitis media.
Statistical Analysis
First, prevalence estimates with 95% CIs were calculated for the presence of unilateral or bilateral notches and HFHL, hearing-related symptoms, and the included covariates. Summary statistical analyses and comparisons were performed using Fisher exact tests. The main evaluation comprised multivariable logistic regression analyses to study the association between music exposure and possible signs of NIHL (ie, notches, HFHL, and hearing-related symptoms), while adjusting for potential confounders (ie, age, sex, race/ethnicity, maternal educational level, household income, and a history of otitis media). Sensitivity analyses assessed whether the main analyses differed when specific audiometric characteristics were studied. The reason for this further testing was the concern of including unilateral HI instead of solely bilateral HI in the defined phenotype, as well as the high proportion of false-positive results in literature.20,22 Additional evaluation, using multivariable logistic regression analyses, assessed the association between the previously described sociodemographic characteristics and signs of NIHL, adjusted for PMP use and a history of otitis media. Missing data on covariates were imputed using multiple imputation. Hypothesis testing was 2-sided with a significance level set at P < .05. SPSS Statistics, version 21.0 for Windows (IBM Corp) and R Statistics, version 3.3.2 (R Foundation) with the imputation package MICE were used for data management and analyses.
Results
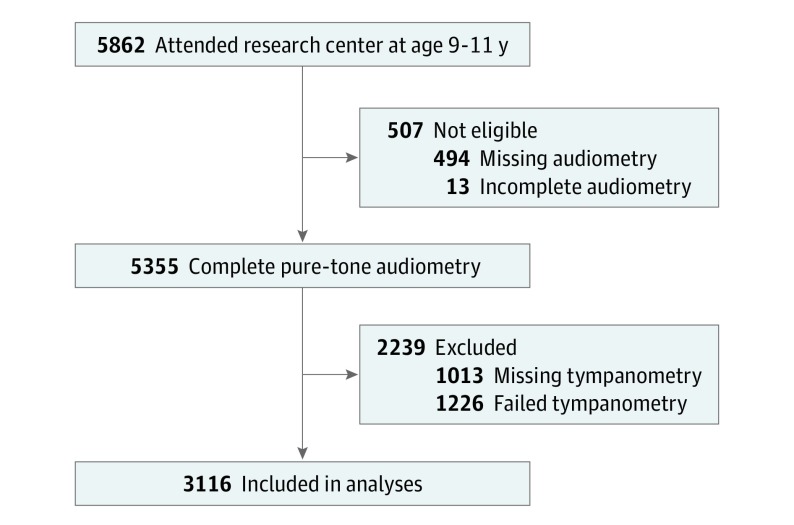
At the age of 9 to 11 years, 5862 children visited the research center for an extensive physical examination. Of these children, 5355 completed pure-tone audiometry at all frequencies and were eligible for inclusion (Figure). Based on the tympanometry criteria, 2239 participants were excluded from the analyses because of missing or failed tympanometry. The final analytical sample therefore included 3116 participants aged 9 to 11 years with complete and adequate audiometry data (Figure). The characteristics of these participants are presented in Table 1.
Figure. Selection of the Included Study Sample.
Complete and adequate audiometry data were available in 3116 children.
Table 1. Characteristics of the Study Sample .
| Characteristic | No. (%)a | ||
|---|---|---|---|
| Total Study Population | Notch | HFHL | |
| No. (%) | 3116 | 205 (6.6) | 303 (9.7) |
| Age, median (IQR) | 9.7 (9.6-9.9) | 9.8 (9.7-9.9) | 9.8 (9.6-9.9) |
| Sex | |||
| Male | 1550 (49.7) | 112 (54.6) | 154 (50.8) |
| Female | 1566 (50.3) | 93 (45.4) | 149 (49.2) |
| Ethnicity | |||
| Western | 2121 (68.1) | 133 (64.9) | 215 (71.0) |
| Non-Western | 917 (29.4) | 65 (31.7) | 83 (27.4) |
| Unknown | 78 (2.5) | 7 (3.4) | 5 (1.7) |
| Maternal educational level | |||
| No or primary | 78 (2.5) | 6 (2.9) | 6 (2.0) |
| Secondary | 1011 (32.4) | 73 (35.6) | 107 (35.3) |
| Higher vocational | 775 (24.9) | 49 (23.9) | 55 (18.2) |
| University | 799 (25.6) | 46 (22.4) | 92 (30.4) |
| Unknown | 453 (14.5) | 31 (15.1) | 43 (14.2) |
| Household income | |||
| Low | 681 (21.9) | 39 (19.0) | 61 (20.1) |
| Middle | 968 (31.1) | 67 (32.7) | 82 (27.1) |
| High | 879 (28.2) | 54 (26.3) | 103 (34.0) |
| Unknown | 588 (18.9) | 45 (22.0) | 57 (18.8) |
| History of AOM | |||
| No history | 1279 (41.0) | 94 (45.9) | 105 (34.7) |
| AOM | 1337 (42.9) | 80 (39.0) | 131 (43.2) |
| rAOM | 313 (10.0) | 20 (9.8) | 49 (16.2) |
| Unknown | 187 (6.0) | 11 (5.4) | 18 (5.9) |
| PMP use | |||
| Never | 1244 (39.9) | 83 (40.5) | 110 (36.3) |
| 1 or 2 d/wk | 577 (18.5) | 35 (17.1) | 65 (21.5) |
| ≥3 d/wk | 254 (8.2) | 11 (5.4) | 31 (10.2) |
| Unknown | 1041 (33.4) | 76 (37.1) | 97 (32.0) |
| PMP listening time | |||
| No use | 1117 (35.8) | 69 (33.7) | 103 (34.0) |
| <1 h/d | 877 (28.1) | 58 (28.3) | 90 (29.7) |
| ≥1 h/d | 83 (2.7) | 2 (1.0) | 13 (4.3) |
| Unknown | 1039 (33.3) | 76 (37.1) | 97 (32.0) |
| PMP volume level | |||
| No use | 1172 (37.6) | 78 (38.0) | 108 (35.6) |
| Very soft to soft | 268 (8.6) | 15 (7.3) | 35 (11.6) |
| Normal, halfway | 533 (17.1) | 31 (15.1) | 51 (16.8) |
| Loud to loudest | 42 (1.3) | 2 (1.0) | 5 (1.7) |
| Unknown | 1101 (35.3) | 79 (38.5) | 104 (34.3) |
| Hearing-related symptoms | |||
| No | 1817 (58.3) | 116 (56.6) | 169 (55.8) |
| Almost never | 121 (3.9) | 5 (2.4) | 14 (4.6) |
| Sometimes | 95 (3.0) | 6 (2.9) | 18 (5.9) |
| Often to always | 16 (0.5) | 1 (0.5) | 2 (0.7) |
| Unknown | 1067 (34.2) | 77 (37.6) | 100 (33.0) |
Abbreviations: AOM, acute otitis media; HFHL, high-frequency hearing loss; IQR, interquartile range; PMP, portable music player; rAOM, recurrent AOM.
Data were missing in some categories, resulting in discrepancies between the numbers.
Age, sex, ethnicity, maternal education level, household income, and PMP use did not differ significantly between children who were included in the analyses and children who were not (eTable 1 in the Supplement).
Prevalence and Characteristics of High-Frequency Notches and HFHL
Of the 3116 children included in the analyses, 443 children (14.2%; 95% CI, 13.0%-15.5%) had audiometric notches or HFHL in 1 or both ears. The criteria of high-frequency notches were fulfilled by 140 children (4.5%; 95% CI, 3.7%-5.2%), 238 children fulfilled the criteria of HFHL (7.6%; 95% CI, 6.7%-8.6%), and 65 children met the criteria of both notches and HFHL (2.1%; 95% CI, 1.6%-2.6%) (Table 2). Table 1 reports the characteristics of the children with notches and HFHL, in addition to the characteristics of the total study sample. Hearing-related symptoms were reported for 232 children (11.3% of 2049 respondents), 16 of whom (0.8%) had frequent to permanent symptoms. Overall, PMP use was reported in 831 children (40.0% of 2075 respondents), and these children generally listened to less than 1 hour per day and on normal (halfway) volume. Parents reported for 101 children (4.9%) that their children used PMPs on a nearly daily basis.
Table 2. Distribution of Hearing Impairment Among the Study Sample.
| Notch | HFHL, No. (%) | |||
|---|---|---|---|---|
| None | Unilateral | Bilateral | ||
| Right Ear | Left Ear | |||
| No notch | 2673 (85.8) | 126 (4.0) | 83 (2.7) | 29 (0.9) |
| Unilateral notch right ear | 42 (1.3) | 15 (0.5) | 1 (0.0) | 4 (0.1) |
| Unilateral notch left ear | 91 (2.9) | 8 (0.3) | 25 (0.8) | 8 (0.3) |
| Bilateral notch | 7 (0.2) | 1 (0.0) | 0 (0.0) | 3 (0.0) |
Abbreviation: HFHL, high-frequency hearing loss.
Notches were most often unilateral in the left ear (64.4%) and less frequently unilateral in the right ear (30.2%); few children had bilateral notches (5.4%) (Table 2). The degree of the notches was 8.8% within the range of normal hearing; 57.1% were slight, 30.7% were mild, and 3.4% were moderate to profound (eTable 2 in the Supplement). The notches involved most often 6 kHz (eTable 3 in the Supplement) and a single frequency (95.6%). Two frequencies were involved in 2.9% of the children, and in 1.5% of the participants, all 3-, 4-, and 6-kHz frequencies were involved.
Among the children with HFHL (n = 303), HFHL was unilateral in 85.5% and bilateral in 14.5% (Table 2). The severity was most often of a slight degree (94.1%); 5.0% was of a mild degree, and 1.0% was of a moderate to profound degree.
Sociodemographic Characteristics and Possible Signs of NIHL
Age and sex were not associated with notches, HFHL, or hearing-related symptoms (Table 3). A secondary educational level of the mother was borderline associated with the presence of notched audiograms, compared with university education (OR, 1.54; 95% CI, 1.02-2.36). Maternal educational level as a continuum was also associated with the presence of notches, with increasing odds of notches for a lower educational level (OR, 1.26; 95% CI, 1.04-1.53 as a continuum). Having a low or medium household income was associated with decreased odds of HFHL (OR, 0.61; 95% CI, 0.42-0.89, and OR, 0.72; 95% CI, 0.53-0.98, respectively) (Table 3).
Table 3. Associations of Sociodemographic Characteristics With High-Frequency Notches, High-Frequency Hearing Loss, and Hearing-Related Symptoms.
| Variable | OR (95% CI) | ||
|---|---|---|---|
| Notcha | HFHLb | Symptomsc | |
| Aged | 1.25 (0.80-1.88) | 1.10 (0.75-1.58) | 1.09 (0.66-1.73) |
| Sex | |||
| Male | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Female | 0.83 (0.62-1.10) | 0.96 (0.75-1.22) | 0.78 (0.56-1.07) |
| Ethnicity | |||
| Western | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Non-Western | 1.11 (0.79-1.54) | 0.93 (0.69-1.23) | 0.90 (0.62-1.31) |
| Maternal education | |||
| No or primary education | 2.37 (0.99-5.22) | 1.39 (0.62-2.86) | 1.98 (0.83-4.42) |
| Secondary education | 1.54 (1.02-2.36) | 1.19 (0.85-1.66) | 1.11 (0.70-1.78) |
| Higher vocational education | 1.31 (0.88-1.98) | 0.77 (0.55-1.08) | 0.89 (0.56-1.43) |
| University | 1 [Reference]e | 1 [Reference] | 1 [Reference] |
| Household income | |||
| Low | 0.64 (0.41-1.01) | 0.61 (0.42-0.89) | 1.58 (0.95-2.61) |
| Medium | 0.93 (0.65-1.34) | 0.72 (0.53-0.98) | 1.36 (0.88-2.12) |
| High | 1 [Reference] | 1 [Reference]f | 1 [Reference] |
Abbreviations: HFHL, high-frequency hearing loss; OR, odds ratio.
Baseline proportion of notches when all reference categories 5.1%.
Baseline proportion of HFHL when all reference categories 8.8%.
Baseline proportion of hearing-related symptoms when all reference categories 2.0%.
Reference value for age, 8.5 years.
Significant association for trend: OR, 1.3 (95% CI, 1.0-1.5).
Significant association for trend: OR, 0.8 (95% CI, 0.7-0.9).
Music Exposure and Possible Signs of NIHL
We did not find associations of music exposure, namely frequency, duration, and volume level of PMP use, with notches or hearing-related symptoms (Table 4). Use of PMPs was also not associated with bilateral notches and separating the high-frequency notches by degree of notch depth or affected frequency, revealed no associations (eTables 2 and 3 in the Supplement).
Table 4. Associations of Music Exposure With High-Frequency Notches, High-Frequency Hearing Loss, and Hearing-Related Symptoms.
| Variable | OR (95% CI) | ||
|---|---|---|---|
| Notcha | HFHLb | Symptomsc | |
| PMP use | |||
| Never | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1 or 2 d/wk per week | 0.77 (0.39-1.67) | 2.88 (1.36-6.98) | 0.86 (0.40-2.09) |
| ≥3 d/wk | 1.09 (0.51-2.51) | 2.74 (1.22-6.96) | 1.00 (0.42-2.58) |
| PMP listening time | |||
| No use | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| <1 h/d | 1.55 (0.79-2.84) | 0.82 (0.39-1.60) | 1.12 (0.48-2.36) |
| ≥1 h/d | 0.61 (0.16-1.90) | 1.14 (0.44-2.75) | 1.50 (0.47-4.31) |
| PMP volume level | |||
| No use | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Very soft to soft | 0.81 (0.32-1.92) | 0.72 (0.26-1.84) | 0.62 (0.20-1.78) |
| Normal, halfway | 0.74 (0.30-1.73) | 0.49 (0.17-1.24) | 1.02 (0.36-2.74) |
| Loud to loudest | 0.61 (0.14-2.07) | 0.48 (0.14-1.53) | 1.25 (0.32-4.41) |
Abbreviations: HFHL, high-frequency hearing loss; OR, odds ratio; PMP, portable music player.
Baseline proportion of notches when all reference categories 5.5%.
Baseline proportion of HFHL when all reference categories 7.7%.
Baseline proportion of hearing-related symptoms when all reference categories 1.9%.
The use of PMPs was significantly associated with HFHL (OR, 2.88; 95% CI, 1.36-6.98, and OR, 2.74; 95% CI, 1.22-6.96, for 1 or 2 days and for more than 3 days per week, respectively) (Table 4), independent of time and volume level of use. This association seemed based on slight rather than worse HFHL (eTable 2 in the Supplement). Focusing on solely bilateral HFHL, a loud to loudest volume level was associated with bilateral HFHL compared with no use (eTable 2 in the Supplement). This association was irrespective of frequency and duration of PMP use.
Discussion
The present study showed that 14.2% of children aged 9 to 11 years had audiometric high-frequency notches and/or HFHL. These findings suggest that 1 of 7 children this young already exhibits HI possibly correlated with NIHL. Use of PMPs and markers of socioeconomic background seemed associated with HFHL and notched audiograms, respectively.
We defined signs of possible NIHL as the presence of high-frequency notches and/or HFHL in the audiogram or reported hearing-related symptoms, such as tinnitus. The prevalence of notches in the present study is lower than that reported for US children aged 6 to 11 years in 1988-1994 (8.5%)21 and among US children aged 12 to 15 years in 2005-2006 (16.0%).12 In our study, notches occurred most often at 6 kHz and included that single frequency, analogous to reports of Niskar et al21 in children aged 6 to 19 years. In total, 9.7% of the children met the criteria of HFHL, again slightly lower than the prevalence rates of 12.9% to 19.2% for comparable age groups in the literature.12,23 The slightly younger age with concomitant likely less exposure to risk factors might contribute to the lower prevalence rates in our study, rather than true international epidemiologic differences. Nearly all notches and HFHL were of a slight or mild degree. Although these findings might seem encouraging in terms of severity within this young population, one can assume that both the prevalence as well as the severity of HI will increase with increasing age and cumulative exposure.24 Hearing-related symptoms were reported for 11.3% of the participants. Both higher and lower proportions have been reported in the literature among children of similar ages.10,25 The main difference here is that our questionnaire did not differentiate tinnitus from other hearing-related symptoms. Frequent to permanent symptoms were reported for 0.8% of the children, which is comparable with other studies.9,10
Lower educational level of the mother was associated with higher odds of notched audiograms. In contrast, lower household income was associated with lower odds for HFHL. Adverse associations of socioeconomic status with signs of NIHL were previously described.21 One possibility is that, within this young age group, the different results represent different sources. Owing to reasons of power and the lack of information on other factors, this possibility was not explored any further and the reason for these contrasting results remains unclear.
The proportion of children in our Dutch cohort who reported PMP use was 40.0%, and in children with HFHL this rate was 46.6%. The rate of PMP use was slightly lower among Australian children aged 7 to 11 years in 2010 (20%-36%)26 and higher among Swedish children aged 9 years in 2016 (52.5%).25 The time of data collection probably was associated with these differences, with PMPs recently changing from separate devices to a standard feature of widely used smartphones. Notable are the few children who use their PMP on a regular basis (4.9%), in contrast to the study of Båsjö et al,25 where 27.8% of the similar-aged children used PMPs regularly. This variance could be a true difference, but another explanation is the use of child vs parent questionnaires to collect the data. In our study, the use of PMPs was positively associated with HFHL, irrespective of the time and volume of use. This finding is similar to that reported by Berg and Serpanos23 among adolescent girls. However, to our knowledge, ours is the first large-scale study that investigated and reported an association between HFHL and PMP use at this young age. The association was probably driven by HFHL of a slight degree rather than worse HFHL. The association of frequency of PMP use was not present when focusing on solely bilateral cases. In this analysis, using PMPs on loud to loudest volume level showed an association with bilateral HFHL. Because the proportion of bilateral HFHL was low, the absence of associations could be because of insufficient power. We found no significant association between PMP use and high-frequency notches, in line with studies among adolescents.12,27 There were no significant differences in the analyses for the total study sample or when stratifying on degree, bilaterality, or affected frequency. The estimates associating PMP use with HFHL seemed stronger in bilateral or more severe notches, but analyses failed to reach significance. Again, insufficient power is likely to play a role among the few cases in these analyses.
Whereas HFHL with normal middle ear function is likely permanent, noise-induced notches are known to occur temporarily as well.9 The different findings among children with notches and children with HFHL suggest a different cause and possibly different subgroups at risk. Still, because noise exposure is expected to affect high-frequency hearing thresholds, it is unclear why different results were obtained.
Strengths and Limitations
We cannot exclude other causes factoring into the obtained results. By requiring normal hearing at low frequencies and limiting the study sample to children who pass tympanometry testing in both ears, we attempted to target NIHL as much as possible. We considered this to be the best available alternative in the absence of bone-conduction thresholds to exclude irreversible and not noise-exposure–related middle ear abnormalities associated with hearing thresholds, but the phenotype remains inconclusive.19 In return, these strict criteria may have caused an underestimation of the prevalence of presumed NIHL, reducing the power of the analyses and influencing the obtained results.
No inferences can be made on the cause of increased hearing thresholds in this cross-sectional audiologic assessment. Besides other causes, it is unknown whether temporary thresholds shifts instead of permanent HI were present. Another concern is the presence of false-positive results, especially for high-frequency notches. These are most often seen at 6 kHz and are of slight degree.22 Sensitivity analyses showed no significant differences when stratifying on these characteristics. Whether false-positive results were a problem in our study is unclear and might become clear after repeated measurements.
Strengths of the present study are its large sample size and protocolled formal audiometry conducted by specific personnel. An important limitation of the study was the assessment of music exposure via parental questionnaires. As with all questionnaire data, recall bias cannot be excluded and the parent proxy to measure exposure could be unreliable. In addition, our data on PMP use was not appropriate to determine an exposure index and reliably examine a dose effect. No information was available on other (environmental) noise sources or otologic or family history. These possible confounders are missing and limit the consideration of the observed HI as NIHL. It is possible that other causes of HI have contributed to the presented prevalence numbers, because we did not correct for congenital hearing loss or other causes of acquired hearing loss. However, by using the strict criteria regarding normal hearing at low frequencies, we targeted as much as possible audiograms fitting possible NIHL.
Conclusions
Our findings suggest that 1 in 7 children aged 9 to 11 years showed high-frequency notches and/or HFHL. Of the cohort, 52 (1.7%) had bilateral impairment. This HI is already present prior to exposure to known noise hazards, such as club and concert attendance, and may have lifelong consequences. Although not conclusive, our findings suggest a possible association of PMP use with high-frequency HI. To our knowledge, this is the first time this association has been reported in such a young age group, suggesting a need for early education on the risks of PMP use in children and young adolescents. Future repeated assessments are essential to provide clarity on this association and whether the obtained results truly represent NIHL at young age.
eFigure. Examples of Audiograms With Signs of Noise-Induced Hearing Loss, Including the Possible Range of Hearing Thresholds to Fulfill the Criteria
eTable 1. Characteristics and Comparison of Included and Excluded Participants
eTable 2. Associations of Music Exposure With Bilateral High-Frequency Notches and High-Frequency Hearing Loss, Stratified by Degree
eTable 3. Associations of Music Exposure With High-Frequency Notches, Stratified by the Frequency at Which the Notch Occurred
References
- 1.Arlinger S. Negative consequences of uncorrected hearing loss–a review. Int J Audiol. 2003;42(suppl 2)(suppl 2):S17-S20, S20. [PubMed] [Google Scholar]
- 2.Bess FH, Dodd-Murphy J, Parker RA. Children with minimal sensorineural hearing loss: prevalence, educational performance, and functional status. Ear Hear. 1998;19(5):339-354. [DOI] [PubMed] [Google Scholar]
- 3.Lieu JE. Speech-language and educational consequences of unilateral hearing loss in children. Arch Otolaryngol Head Neck Surg. 2004;130(5):524-530. [DOI] [PubMed] [Google Scholar]
- 4.Mathers C, Smith A, Concha M Global Burden of Hearing Loss in the Year 2000. 2003:1-30. http://www.who.int/healthinfo/statistics/bod_hearingloss.pdf. Accessed October 19, 2017.
- 5.Lu X, Shu Y, Tang M, Li H. Mammalian cochlear hair cell regeneration and ribbon synapse reformation. Neural Plast. 2016;2016:2523458. doi: 10.1155/2016/2523458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pourbakht A, Yamasoba T. Cochlear damage caused by continuous and intermittent noise exposure. Hear Res. 2003;178(1-2):70-78. [DOI] [PubMed] [Google Scholar]
- 7.Hong O, Kerr MJ, Poling GL, Dhar S. Understanding and preventing noise-induced hearing loss. Dis Mon. 2013;59(4):110-118. [DOI] [PubMed] [Google Scholar]
- 8.Rösler G. Progression of hearing loss caused by occupational noise. Scand Audiol. 1994;23(1):13-37. [DOI] [PubMed] [Google Scholar]
- 9.le Clercq CMP, van Ingen G, Ruytjens L, van der Schroeff MP. Music-induced hearing loss in children, adolescents, and young adults: a systematic review and meta-analysis. Otol Neurotol. 2016;37(9):1208-1216. [DOI] [PubMed] [Google Scholar]
- 10.Piotrowska A, Raj-Koziak D, Lorens A, Skarżyński H. Tinnitus reported by children aged 7 and 12 years. Int J Pediatr Otorhinolaryngol. 2015;79(8):1346-1350. [DOI] [PubMed] [Google Scholar]
- 11.Vogel I, Verschuure H, van der Ploeg CP, Brug J, Raat H. Estimating adolescent risk for hearing loss based on data from a large school-based survey. Am J Public Health. 2010;100(6):1095-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henderson E, Testa MA, Hartnick C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics. 2011;127(1):e39-e46. [DOI] [PubMed] [Google Scholar]
- 13.Jiang W, Zhao F, Guderley N, Manchaiah V. Daily music exposure dose and hearing problems using personal listening devices in adolescents and young adults: A systematic review. Int J Audiol. 2016;55(4):197-205. [DOI] [PubMed] [Google Scholar]
- 14.Carter L, Williams W, Black D, Bundy A. The leisure-noise dilemma: hearing loss or hearsay? What does the literature tell us? Ear Hear. 2014;35(5):491-505. [DOI] [PubMed] [Google Scholar]
- 15.Portnuff CD. Reducing the risk of music-induced hearing loss from overuse of portable listening devices: understanding the problems and establishing strategies for improving awareness in adolescents. Adolesc Health Med Ther. 2016;7:27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scientific Committee on Emerging and Newly Identified Health Risks Potential Health Risks of Exposure to Noise From Personal Music Players and Mobile Phones Including a Music Playing Function: Preliminary Report. Brussels, Begium: European Commission; 2008.
- 17.Hofman A, Jaddoe VWV, Mackenbach JP, et al. . Growth, development and health from early fetal life until young adulthood: the Generation R Study. Paediatr Perinat Epidemiol. 2004;18(1):61-72. [DOI] [PubMed] [Google Scholar]
- 18.Kooijman MN, Kruithof CJ, van Duijn CM, et al. . The Generation R Study: design and cohort update 2017. Eur J Epidemiol. 2016;31(12):1243-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.le Clercq CMP, van Ingen G, Ruytjens L, et al. . Prevalence of hearing loss among children 9 to 11 years old: the Generation R Study. JAMA Otolaryngol Head Neck Surg. 2017;143(9):928-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schlauch RS, Carney E. The challenge of detecting minimal hearing loss in audiometric surveys. Am J Audiol. 2012;21(1):106-119. [DOI] [PubMed] [Google Scholar]
- 21.Niskar AS, Kieszak SM, Holmes AE, Esteban E, Rubin C, Brody DJ. Estimated prevalence of noise-induced hearing threshold shifts among children 6 to 19 years of age: the Third National Health and Nutrition Examination Survey, 1988-1994, United States. Pediatrics. 2001;108(1):40-43. [DOI] [PubMed] [Google Scholar]
- 22.Bhatt IS, Guthrie O. Analysis of audiometric notch as a noise-induced hearing loss phenotype in US youth: data from the National Health and Nutrition Examination Survey, 2005-2010. Int J Audiol. 2017;56(6):392-399. [DOI] [PubMed] [Google Scholar]
- 23.Berg AL, Serpanos YC. High frequency hearing sensitivity in adolescent females of a lower socioeconomic status over a period of 24 years (1985-2008). J Adolesc Health. 2011;48(2):203-208. [DOI] [PubMed] [Google Scholar]
- 24.Katz J. Handbook of Clinical Audiology. Baltimore, MD: Williams & Wilkins; 1994:20-21, 283-291, 534-551, 627. [Google Scholar]
- 25.Båsjö S, Möller C, Widén S, Jutengren G, Kähäri K. Hearing thresholds, tinnitus, and headphone listening habits in nine-year-old children. Int J Audiol. 2016;55(10):587-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cone BK, Wake M, Tobin S, Poulakis Z, Rickards FW. Slight-mild sensorineural hearing loss in children: audiometric, clinical, and risk factor profiles. Ear Hear. 2010;31(2):202-212. [DOI] [PubMed] [Google Scholar]
- 27.Dehnert K, Raab U, Perez-Alvarez C, et al. . Total leisure noise exposure and its association with hearing loss among adolescents. Int J Audiol. 2015;54(10):665-673. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Examples of Audiograms With Signs of Noise-Induced Hearing Loss, Including the Possible Range of Hearing Thresholds to Fulfill the Criteria
eTable 1. Characteristics and Comparison of Included and Excluded Participants
eTable 2. Associations of Music Exposure With Bilateral High-Frequency Notches and High-Frequency Hearing Loss, Stratified by Degree
eTable 3. Associations of Music Exposure With High-Frequency Notches, Stratified by the Frequency at Which the Notch Occurred