Abstract
Importance
Low-cost sequencing of multiple genes is increasingly available for cancer risk assessment. Little is known about uptake or outcomes of multiple-gene sequencing after breast cancer diagnosis in community practice.
Objective
To examine the effect of multiple-gene sequencing on the experience and treatment outcomes for patients with breast cancer.
Design, Setting, and Participants
For this population-based retrospective cohort study, patients with breast cancer diagnosed from January 2013 to December 2015 and accrued from SEER registries across Georgia and in Los Angeles, California, were surveyed (n = 5080, response rate = 70%). Responses were merged with SEER data and results of clinical genetic tests, either BRCA1 and BRCA2 (BRCA1/2) sequencing only or including additional other genes (multiple-gene sequencing), provided by 4 laboratories.
Main Outcomes and Measures
Type of testing (multiple-gene sequencing vs BRCA1/2-only sequencing), test results (negative, variant of unknown significance, or pathogenic variant), patient experiences with testing (timing of testing, who discussed results), and treatment (strength of patient consideration of, and surgeon recommendation for, prophylactic mastectomy), and prophylactic mastectomy receipt. We defined a patient subgroup with higher pretest risk of carrying a pathogenic variant according to practice guidelines.
Results
Among 5026 patients (mean [SD] age, 59.9 [10.7] years), 1316 (26.2%) were linked to genetic results from any laboratory. Multiple-gene sequencing increasingly replaced BRCA1/2-only testing over time: in 2013, the rate of multiple-gene sequencing was 25.6% and BRCA1/2-only testing, 74.4%; in 2015 the rate of multiple-gene sequencing was 66.5% and BRCA1/2-only testing, 33.5%. Multiple-gene sequencing was more often ordered by genetic counselors (multiple-gene sequencing, 25.5% and BRCA1/2-only testing, 15.3%) and delayed until after surgery (multiple-gene sequencing, 32.5% and BRCA1/2-only testing, 19.9%). Multiple-gene sequencing substantially increased rate of detection of any pathogenic variant (multiple-gene sequencing: higher-risk patients, 12%; average-risk patients, 4.2% and BRCA1/2-only testing: higher-risk patients, 7.8%; average-risk patients, 2.2%) and variants of uncertain significance, especially in minorities (multiple-gene sequencing: white patients, 23.7%; black patients, 44.5%; and Asian patients, 50.9% and BRCA1/2-only testing: white patients, 2.2%; black patients, 5.6%; and Asian patients, 0%). Multiple-gene sequencing was not associated with an increase in the rate of prophylactic mastectomy use, which was highest with pathogenic variants in BRCA1/2 (BRCA1/2, 79.0%; other pathogenic variant, 37.6%; variant of uncertain significance, 30.2%; negative, 35.3%).
Conclusions and Relevance
Multiple-gene sequencing rapidly replaced BRCA1/2-only testing for patients with breast cancer in the community and enabled 2-fold higher detection of clinically relevant pathogenic variants without an associated increase in prophylactic mastectomy. However, important targets for improvement in the clinical utility of multiple-gene sequencing include postsurgical delay and racial/ethnic disparity in variants of uncertain significance.
This population-based cohort study examines the effect of multiple-gene sequencing on the experiences and treatment outcomes of patients with breast cancer.
Key Points
Question
What are the results and outcomes of more comprehensive genetic sequencing after diagnosis of breast cancer?
Findings
In this population-based study, multiple-gene sequencing markedly replaced BRCA1- and BRCA2-only tests and enabled 2-fold higher detection of clinically relevant pathogenic variants without an associated increase in prophylactic mastectomy. Multiple-gene sequencing was more often delayed postsurgery and yielded much higher rates of variants of uncertain significance, particularly in racial/ethnic minorities.
Meaning
Multiple-gene sequencing rapidly replaced more limited testing and enabled 2-fold higher detection of clinically relevant findings, but important targets for improvement include postsurgical delay and racial/ethnic disparity in variants of uncertain significance.
Introduction
Germline genetic testing in patients newly diagnosed with cancer has the potential to reduce disease burden through secondary prevention and targeted therapies. Thus, there is enormous need to understand how genetic testing is being integrated into practice for patients newly diagnosed with cancer and the impact of results on treatment decisions.1 Additionally, testing relatives of patients with cancer who carry pathogenic variants is a potentially efficient strategy for population-wide cancer prevention.2 Recent advances in next-generation, massively parallel sequencing and regulatory changes have made low-cost, more comprehensive genetic testing increasingly accessible.3,4,5 After 2 decades when only 2 breast cancer–associated genes (BRCA1 and BRCA2 [BRCA1/2]) were routinely sequenced, panels of up to 90 cancer-associated genes are now widely available. As clinical whole-genome sequencing becomes increasingly feasible, it is crucial to understand the implications of expanded genetic testing on practice and patient experiences. Yet virtually nothing is known about the uptake, results, or consequences of multiple-gene sequencing in community practice.
To address this gap, we examined uptake and outcomes of multiple-gene sequencing in a large, population-based, contemporary cohort of patients recently diagnosed with breast cancer. The iCanCare study began accrual 1 month after a US Supreme Court decision led to markedly lower costs of multiple-gene sequencing for breast cancer risk.4 We linked information on genetic test use and results directly from 4 genetic laboratories that perform most germline testing for patients with breast cancer in the study regions. We integrated this information with patient survey and Surveillance, Epidemiology and End Results (SEER) registry clinical data to examine trends, results, and consequences of multiple-gene vs BRCA1/2-only sequencing.
Methods
Study Sample and Data Collection
As previously reported,6,7,8,9,10,11,12 the iCanCare study identified women aged 20 to 79 years, diagnosed with stages 0 to II breast cancer, and reported to the Georgia or Los Angeles County SEER registries. Exclusion criteria of the iCanCare study included: prior breast cancer, tumors larger than 5 cm or with more than 3 involved lymph nodes. Patients were mailed survey materials and a $20 cash gift between July 2013 and August 2015. We used a modified Dillman method13 to encourage response (median [SD] time from diagnosis to survey completion: 6.0 [2.8] months). We sent surveys to 7810 patients: 507 were ineligible owing to exclusions noted above or were deceased, institutionalized, too ill, or unable to complete a survey in Spanish or English, leaving 7303 patients. The survey was completed by 5080 eligible patients (response rate = 70%) and was published previously.11
Survey responses were merged with SEER clinical data and genetic testing information obtained from 4 laboratories (Ambry Genetics, Aliso Viejo, CA; GeneDx, Gaithersburg, MD; Invitae, San Francisco, CA; Myriad Genetics, Salt Lake City, UT) that tested patients in the study regions. Test type and results were merged to 5026 patients with complete information on all variables for SEER-genetic testing linkage using a probabilistic matching strategy performed by Information Management Services, Inc (IMS). The Safe Harbor method was used to deidentify the data set before transfer to the University of Michigan for analysis.14 Questions about germline testing experiences were added for the latter half of study participants.
The collaboration was covered under data use agreements between the University of Michigan, genetic laboratories, and IMS. The research was approved by institutional review boards of the University of Michigan, Emory University, the University of Southern California, the Georgia Department of Public Health, the California State Committee for the Protection of Human Subjects, and California Cancer Registry. Signed consent was waived for the survey. Waivers of informed consent and authorization were approved given the use of a third-party honest broker to conduct the linkage and create a deidentified data set for analyses.
Testing Measures From Laboratories
All participating laboratories were Clinical Laboratory Improvement Amendments (CLIA)-certified and conformed to variant interpretation standards of the American College of Medical Genetics.15,16 Genetic laboratories provided sequencing results at the level of the gene tested (eg, BRCA1) and the clinical interpretation sent to the ordering clinician (consisting of pathogenic, likely pathogenic, uncertain significance, likely benign, or benign). We grouped interpretations of pathogenic and likely pathogenic together as pathogenic, and grouped likely benign and benign together as benign. A test that assessed only BRCA1/2 was categorized as a BRCA1/2-only test; a test including any additional gene (eg, ATM, CHEK2) was categorized as multiple-gene sequencing. If patients received both on separate occasions (eg, a BRCA1/2-only test and later multiple-gene sequencing), they were coded as having received multiple-gene sequencing. We created mutually exclusive results categories as follows: (1) negative for a pathogenic variant or variant of uncertain significance (VUS) in any gene; (2) 1 or more VUS but no pathogenic variant in any gene; (3) positive for a pathogenic variant in BRCA1/2 (patients in this category could have VUS but no pathogenic variant in another gene); or (4) positive for a pathogenic variant in another gene (patients could have VUS in any gene).
Testing Experience Measures From Surveys
Test experience measures included timing (before cancer diagnosis, after diagnosis but before surgery, after surgery) along with who ordered the test and discussed results with the patient (surgeon, medical oncologist, genetic counselor, or multiple health professionals [both surgeon and medical oncologist]). Treatment experiences from patient report included how strongly the patient considered contralateral prophylactic mastectomy (5-point Likert scale from “not at all” to “very strongly,” collapsed to binary categories of “strongly” vs “less strongly”); how strongly their surgeon recommended prophylactic mastectomy (also collapsed to “strongly” vs “less strongly”); and whether they received prophylactic mastectomy.
Risk Measures From Surveys and SEER
We created a measure of higher pretest risk for pathogenic variant carriage using SEER-reported tumor characteristics and self-reported family cancer history, consistent with the National Comprehensive Cancer Network (NCCN) guidelines and used in our prior work.11,12,17 Patients were considered at higher pretest risk if they had any of the following: 45 years or younger at breast cancer diagnosis, triple-negative breast cancer diagnosed at younger than 60 years; any relative with ovarian cancer, sarcoma, or male breast cancer; 2 or more first-degree relatives with breast cancer (for patients diagnosed at 50 years or younger, 1 or more first-degree relative with breast cancer); Ashkenazi Jewish ancestry; or family history of a pathogenic variant conferring high risk (eg, BRCA1/2). Other covariates included age (<50 years vs ≥50 years), race/ethnicity (white non-Hispanic, black, Hispanic, or Asian), tumor laterality (unilateral, bilateral), partner status, income level, insurance status, and geographic site.
Statistical Methods
We examined testing use by test type and pretest risk among all patients. We used a generalized logit model without adjustment for covariates to estimate trends in test type among testers over time. Among tested patients, we evaluated the association of multiple-gene sequencing vs BRCA1/2-only testing with clinical and sociodemographic covariates using logistic regression that also controlled for time. We examined results by clinical and sociodemographic subgroups and treatment experiences by test results. We described patient testing experiences by test type in the subgroup that was asked these questions. We used survey design and nonresponse weights to compensate for the differential probability of patient selection and survey nonresponse among subgroups with various characteristics.12
Results
Patient Characteristics
Among 5026 respondents with complete data (eFigure 1 in the Supplement), 1316 (26.2%) had any genetic test results (588 multiple-gene sequencing and 728 BRCA1/2-only testing). The total sample was racially diverse, with 2508 non-Hispanic white patients (51.3%), 908 black patients (18.1%), 950 Hispanic patients (18.9%), 461 Asian patients (9.2%), and 127 patients (2.5%) of other, unknown, or missing race/ethnicity. Patients who received BRCA1/2-only were generally similar to those who received multiple-gene sequencing (eTable 1 in the Supplement).
Genetic Test Uptake Over Time
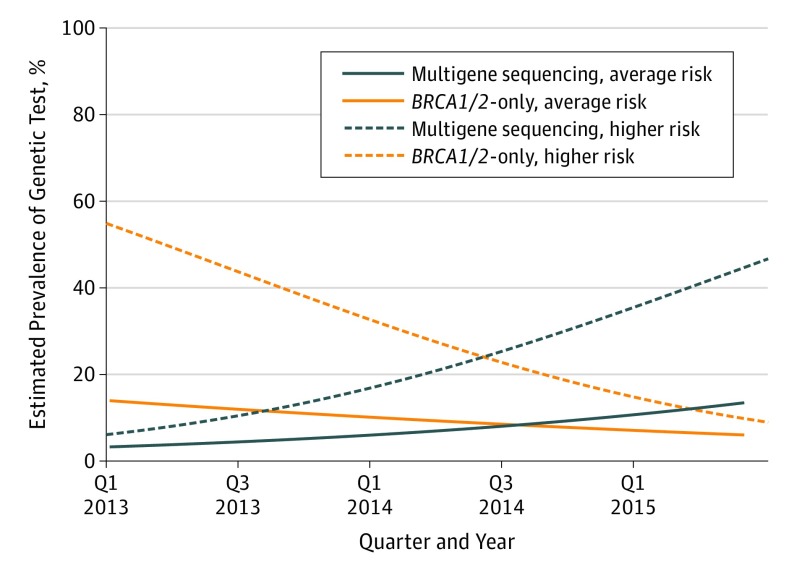
There was no change over time in the proportion of patients receiving any genetic test (approximately one-quarter). However, there was substantial change in test type over time, with multiple-gene sequencing increasingly replacing BRCA1/2-only testing for patients at both higher and average pretest risk (Figure). From the first half of 2013 to the first half of 2015, the rate of multiple-gene sequencing increased from 4.8% to 19.6% while the rate of BRCA1/2-only testing decreased from 22.6% to 10.0%. Thus, among tested patients, multiple-gene sequencing increasingly replaced BRCA1/2-only testing over time (2013: multiple-gene sequencing, 25.6%; BRCA1/2-only testing, 74.4% vs 2015: multiple-gene sequencing, 66.5%; BRCA1/2-only testing, 33.5%).
Figure. Trends in Genetic Test Type.
BRCA1 and BRCA2 (BRCA1/2)-only vs multiple-gene sequencing for 5026 patients with complete information on all variables. Blue lines represent multiple-gene sequencing, and orange lines represent BRCA1/2-only sequencing; solid lines represent patients at higher pretest risk of pathogenic mutation carriage, and dashed lines represent patients at average risk.
Correlates Among Testers of Test Type
On multivariable analysis of receiving multiple-gene sequencing vs BRCA1/2-only testing, there was no association with pretest risk of pathogenic variant carriage (eFigure 2 in the Supplement). Educational attainment was also not associated with test type. Somewhat greater use of multiple-gene sequencing was observed in older patients, Asian patients, and Georgia residents.
Patient Experiences of Genetic Test Ordering, Discussion, and Timing
Among the second half of the study cohort that was asked questions about testing experiences (n = 2443), 639 patients linked to genetic test results from any laboratory, of whom 547 recalled testing (Table 1). Although surgeons most frequently ordered both types of genetic testing, genetic counselors were more often the ordering clinician for multiple-gene sequencing vs BRCA1/2-only testing (25.5% vs 15.3%; P < .001). Testing results were most commonly discussed by a genetic counselor, particularly for patients who received multiple-gene sequencing vs BRCA1/2-only testing (69.8% vs 42.0%; P < .001). Although most tests were performed before surgery, multiple-gene sequencing recipients were more likely to report delay in testing until after surgery (32.5% vs 19.9% for BRCA1/2-only testing; P < .001).
Table 1. Patient Experiences with Genetic Testinga by Genetic Test Type.
| Test Characteristic | Multiple-Gene Sequencingb (n = 341) | BRCA1/2 Onlyb (n = 298) |
|---|---|---|
| Clinician ordering test results (n = 504) | ||
| Surgeon | 47.3 | 50.2 |
| Medical oncologist | 27.2 | 34.5 |
| Genetic counselor | 25.5 | 15.3 |
| Clinician(s) who discussed test results (n = 500) | ||
| Surgeon only | 14.6 | 25.8 |
| Medical oncologist only | 11.4 | 24.4 |
| Genetic counselor | 69.8 | 42.0 |
| Multiple health professionalsc | 4.2 | 7.8 |
| Timing of test (n = 541) | ||
| Before diagnosis | 3.9 | 3.0 |
| After diagnosis but before surgery | 63.6 | 77.1 |
| After surgery | 32.5 | 19.9 |
Abbreviation: BRCA1/2, BRCA1 and BRCA2.
In the second half of the survey (n = 2443), 639 patients linked to genetic testing of whom 547 recalled that they received testing. Differing numbers in the Table rows reflect small numbers of missing responses to the items. Analyses are weighted to compensate for the differential probability of patient selection and survey nonresponse among subgroups with various characteristics.
Weighted percentages are shown. All comparisons are statistically significant (P < .001).
Surgeons and medical oncologists.
Genetic Test Results Among Testers by Pretest Risk
The 51 genes for which test results were provided by laboratories are in eTable 2 in the Supplement. In both patients deemed higher risk and average pretest risk, pathogenic variants were detected 2 times as often with multiple-gene sequencing (in any gene: higher pretest risk, 12.5%; average risk, 4.2%) (Table 2) as BRCA1/2-only testing (in BRCA1/2: higher risk, 7.8%; average risk, 2.2%). The other genes in which patients had pathogenic variants were: APC (n = 2), ATM (n = 3), BARD1 (n = 1), BRIP1 (n = 2), CHEK2 (n = 4), MLH1 (n = 1), MSH6 (n = 1), NBN (n = 1), NF1 (n = 1), PALB2 (n = 3), PMS2 (n = 2), RAD50 (n = 1), RAD51C (n = 2), and RAD51D (n = 1). No patient had pathogenic variants in BRCA1/2 and another gene. Variants of uncertain significance were 10-fold more frequent with multiple-gene sequencing (higher risk, 27.1%; average risk, 32.9%) than BRCA1/2-only testing (higher risk, 3.6%; average risk, 1.8%). There were substantial racial/ethnic differences in VUS prevalence. These differences were much larger in magnitude with multiple-gene sequencing (white patients, 23.7%; black patients, 44.5%; Asian patients, 50.9%) than with BRCA1/2-only testing (white patients, 2.2%; black patients, 5.6%; Asian patients, 0% (Table 2).
Table 2. Genetic Test Results by Test Type, Pretest Risk, and Racial/Ethnic Groupsa.
| Characteristic | Multiple-Gene Sequencing (n = 588) |
BRCA1/2 Only (n = 728) |
||||
|---|---|---|---|---|---|---|
| Pathogenic Variantb | VUS | Negative | Pathogenic Variantb | VUS | Negative | |
| Patient Pretest Risk Levelc | ||||||
| Average risk | 4.2 | 32.9 | 63.0 | 2.2 | 1.8 | 96.0 |
| Higher risk | 12.5 | 27.1 | 60.5 | 7.8 | 3.6 | 88.6 |
| Race | ||||||
| White, non-Hispanic | 9.3 | 23.7 | 67.0 | 5.3 | 2.2 | 92.5 |
| Black | 7.1 | 44.5 | 48.4 | 6.9 | 5.6 | 87.5 |
| Hispanic | 13.9 | 23.8 | 62.3 | 5.2 | 3.7 | 91.0 |
| Asian | 1.6 | 50.9 | 47.5 | 1.7 | 0.0 | 98.3 |
Abbreviations: BRCA1/2, BRCA1 and BRCA2; VUS, variant of unknown significance.
Weighted row percentages within test type. Rates may not sum to 100% due to rounding. Test result differences between test types were compared using Rao Scott χ2 tests and were significant (P < .001) for every risk and race group category.
In total, 64 pathogenic variants were in BRCA1/2, and 24 were in other genes. The other genes in which patients had pathogenic variants were: APC (2), ATM (3), BARD1 (1), BRIP1 (2), CHEK2 (4), MLH1 (1), MSH6 (1), NBN (1), NF1 (1), PALB2 (3), PMS2 (2), RAD50 (1), RAD51C (2), and RAD51D (1). The total number of pathogenic variants is 25 because 1 patient had 2 pathogenic variants.
Patients were considered at higher pretest risk if they had any of the following: 45 years or younger at breast cancer diagnosis, triple-negative breast cancer diagnosed at age younger than 60 years; any relative with ovarian cancer, sarcoma, or male breast cancer; 2 or more first-degree relatives with breast cancer (for patients diagnosed at 50 years or younger, 1 or more first-degree relative with breast cancer); Ashkenazi Jewish ancestry; or family history of a pathogenic variant conferring high risk (eg, BRCA1/2), consistent with criteria for genetic testing according to guidelines of the National Comprehensive Cancer Network.
Impact of Genetic Results on Prophylactic Mastectomy Outcomes
Pathogenic BRCA1/2 variants were more strongly associated than any other test result with all prophylactic mastectomy-related outcomes (Table 3). This included patients who strongly considered prophylactic mastectomy (BRCA1/2 pathogenic variant, 80.3%; other pathogenic variant, 39.8%; P < .001), patients’ report of surgeons’ strong recommendation for prophylactic mastectomy (BRCA1/2-positive disease, 51.4%; other pathogenic variant, 10.3%; P < .001) and prophylactic mastectomy receipt (BRCA1/2 pathogenic variant, 79.0%; other pathogenic variant, 37.6%; VUS, 30.2%; no pathogenic variants or VUS, 35.3%; P < .001).
Table 3. Impact of Test Results on Prophylactic Mastectomy Outcomes.
| Genetic Test Result | Patient Strongly Considered Prophylactic Mastectomya | Surgeon Recommended Prophylactic Mastectomya | Patient Received Prophylactic Mastectomya |
|---|---|---|---|
| BRCA1/2 pathogenic variant (n = 64) | 80.3 | 51.4 | 79.0 |
| Other pathogenic variantb (n = 24) | 39.8 | 10.3 | 37.6 |
| VUS only (n = 198) | 38.8 | 14.4 | 30.2 |
| Negative (n = 1030) | 43.7 | 14.1 | 35.3 |
Abbreviation: VUS, variant of unknown significance.
Weighted percent consideration, recommendation, and receipt of prophylactic mastectomy: all P < .001.
The other genes in which patients had pathogenic variants were APC (2), ATM (3), BARD1 (1), BRIP1 (2), CHEK2 (4), MLH1 (1), MSH6 (1), NBN (1), NF1 (1), PALB2 (3), PMS2 (2), RAD50 (1), RAD51C (2), and RAD51D (1). The total number of pathogenic variants is 25 because 1 patient had 2 pathogenic variants.
Discussion
We report the first population-based study of germline multiple-gene sequencing in community practice, with results supplied directly from testing laboratories and linked to SEER data. One-quarter of patients with newly diagnosed breast cancer had a linked genetic test result, and multiple-gene sequencing largely replaced BRCA1/2-only tests over a 2-year period. Similar to other reports in noncommunity based samples,18,19,20,21,22,23,24,25 we found that multiple-gene sequencing was 2 times more likely to detect a pathogenic variant for which guidelines advise a change in care.17,26 The greater yield of clinically relevant information with multiple-gene sequencing offers a major potential advantage over more limited BRCA1/2-only tests. Yet we identified 2 important limitations in the clinical utility of multiple-gene sequencing that must be addressed.
First, for many patients, multiple-gene sequencing was performed too late to influence treatment decision making. Patients more often had it postsurgery (32.5% vs 19.9% of patients with BRCA1/2-only testing), limiting use of results in decisions about surgical prevention of second cancers. This delay was not owing to patient characteristics, as we found no meaningful differences according to test type; nor was it likely owing to test characteristics, as turnaround time does not generally vary by gene number. The postsurgical delay associated with multiple-gene sequencing may reflect clinicians’ recognition of its greater complexity and need for genetics expertise, as we found that multiple-gene sequencing was significantly more likely to be ordered and discussed by a genetic counselor than was BRCA1/2-only testing. However, clinicians may not consult experts early enough and rapid access to genetic counseling is not universally available, which may explain the delay associated with testing more genes.11,12,27 Since results often come too late to guide surgical choices, the full benefits of multiple-gene sequencing are not achieved.
A second limitation with multiple-gene sequencing was a substantial racial disparity in the clinical validity of results. There was a marked difference in VUS rates on multiple-gene sequencing by race/ethnicity, from 23.7% in non-Hispanic white patients to 50.9% among Asian patients. The cause of this racial VUS gap is more social than biological: most genes were first sequenced in white patients, such that understanding of the normal spectrum of variation in other racial groups is limited (and perpetuated by testing access disparities).28 Prior studies reported a racial/ethnic VUS disparity on BRCA1/2-only testing29; we previously found that the racial VUS gap widens as more genes are sequenced.30 With broader testing of a gene within a population, most VUS are reclassified to benign variants that are normal for that group.28 Extensive VUS reclassification occurred over the last 2 decades of clinical BRCA1/2 testing. Importantly, our results are the first to demonstrate its success in a population-based setting. While there is still some racial/ethnic disparity in VUS rates with BRCA1/2-only testing (non-Hispanic white patients, 2.2%; non-Hispanic black patients, 5.6%; Hispanic patients, 3.7%; Asian patients, 0%), the absolute magnitude of this disparity is much smaller than it used to be.29 Our findings with BRCA1/2-only testing offer strong, population-based evidence that the racial/ethnic VUS gap can be bridged. It is a crucial priority to resolve persistent racial/ethnic disparities in genetic information, particularly as increasingly comprehensive sequencing tests enter clinical practice.
Outcomes including prophylactic surgery have been studied after BRCA1/2 testing,31,32,33 but little is known about outcomes after sequencing other cancer-associated genes. We assessed patients’ consideration, reports of their surgeons’ recommendation, and use of prophylactic mastectomy. These were no higher among patients with other pathogenic variants than among patients testing negative. This finding makes clinical sense because for most cancer-associated genes other than BRCA1/2, breast cancer risks are lower or nonexistent, and the evidence base is insufficient to support guideline recommendations for prophylactic mastectomy.17,26 Another concern is the high VUS rate with multiple-gene sequencing, as we and others have found that clinicians may misinterpret VUS as an indication for prophylactic mastectomy.12,34 Thus, our observation that the rate of prophylactic mastectomy was no higher for those with VUS vs negative results is reassuring. We note that the baseline rate of prophylactic mastectomy was high (35% among patients who tested negative), likely reflecting pretest preferences for this approach among patients who sought genetic testing. An important caveat is the more frequent postsurgical delay of multiple-gene sequencing, which may mean that our findings underestimate the results of multiple-gene sequencing on surgical decision making. Longer-term follow-up will be essential to understand the impact of multiple-gene sequencing results on patients’ decisions about breast cancer treatment and secondary cancer prevention.
Strengths and Limitations
This study has strengths and limitations. Its strengths include a diverse, population-based contemporary sample accrued from SEER registries and enriched by genetic results provided directly by testing laboratories; detailed clinical data; and a high response rate. Limitations include uncertainty about the completeness of testing ascertainment. Some tests may have been missed if performed outside of collaborating laboratories. However, surveyed clinicians reported sending nearly all germline genetic tests to these 4 laboratories, and the linkage rate of 26% closely approximates patient report of testing in our prior work.11,12 Given the small number of pathogenic variants in genes other than BRCA1/2, we could not analyze outcomes such as prophylactic mastectomy by specific gene affected. We did not collect data on other outcomes such as prophylactic salpingo-oophorectomy, secondary cancer screening, or genetic testing of family members. The iCanCare study oversampled patients with hormone-receptor positive disease and thus underrepresents patients with triple-negative cancers who may have higher mutation prevalence.25,35 Patients were accrued from 2 large, diverse regions, and results may not generalize to all patients in the United States with breast cancer. Genetic testing has evolved rapidly: ongoing follow-up will be needed to capture the latest uptake trends. Despite limitations, this study demonstrates the power of genetic data linkage to enhance clinical relevance of information from population-based cancer registries.
Conclusions
Much is at stake with efforts to integrate multiple-gene sequencing into cancer care. Guidelines for managing pathogenic variants in various cancer susceptibility genes are evolving rapidly, as is genetically targeted treatment with the success of poly (adenosine diphosphate-ribose) polymerase inhibitors.17,36 Furthermore, a strategy of widespread and more comprehensive testing in patients with cancer may be the most cost-effective approach to identifying genetic predisposition in families.2,37
Breast cancer is an important early exemplar of the experiences and consequences of more expansive genetic testing in practice. Our findings demonstrate that sequencing more genes offers the potential advantage of more clinically valuable information and also pinpoints gaps that must be bridged to realize that potential. First, testing needs to be optimally targeted to patients deemed higher risk and accompanied by appropriate counseling. Second, testing must be more timely for patients with newly diagnosed cancer. Solving this problem will require more attention by surgeons and availability of efficient patient triage to genetic expertise, enabling faster test selection, results communication and follow-up. New care delivery models, encompassing more and better-integrated genetic counselors along with supportive technology, such as clinical decision tools, will be crucial to the success of precision oncology. Third, VUS reclassification efforts are essential to resolve the racial/ethnic disparity in the clinical utility of sequencing more and less familiar genes. Finally, although outcomes suggest clinically appropriate response to test results (pathogenic variants in BRCA1/2 were strongly associated with prophylactic mastectomy; other pathogenic variants, VUS and negative results were less so), more research is needed about the long-term consequences of multiple-gene sequencing in cancer patients and their relatives.
eFigure 1. Patient flow diagram
eTable 1. Demographic and clinical characteristics of patients by genetic test type
eFigure 2. Multivariable analysis among tested patients of the correlates of receiving multiple-gene sequencing versus a BRCA1/2-only test
eTable 2. Tested genes and pathogenic variants
References
- 1.Katz SJ, Kurian AW, Morrow M. Treatment decision making and genetic testing for breast cancer: mainstreaming mutations. JAMA. 2015;314(10):997-998. [DOI] [PubMed] [Google Scholar]
- 2.Samimi G, Bernardini MQ, Brody LC, et al. Traceback: a proposed framework to increase identification and genetic counseling of brca1 and brca2 mutation carriers through family-based outreach. J Clin Oncol. 2017;35(20):2329-2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Domchek SM, Bradbury A, Garber JE, Offit K, Robson ME. Multiplex genetic testing for cancer susceptibility: out on the high wire without a net? J Clin Oncol. 2013;31(10):1267-1270. [DOI] [PubMed] [Google Scholar]
- 4.Offit K, Bradbury A, Storm C, Merz JF, Noonan KE, Spence R. Gene patents and personalized cancer care: impact of the Myriad case on clinical oncology. J Clin Oncol. 2013;31(21):2743-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurian AW, Ford JM. Multigene panel testing in oncology practice: how should we respond? JAMA Oncol. 2015;1(3):277-278. [DOI] [PubMed] [Google Scholar]
- 6.Hawley ST, Janz NK, Griffith KA, et al. Recurrence risk perception and quality of life following treatment of breast cancer. Breast Cancer Res Treat. 2017;161(3):557-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jagsi R, Abrahamse PH, Lee KL, et al. Treatment decisions and employment of breast cancer patients: Results of a population-based survey. Cancer. 2017;123(24):4791-4799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jagsi R, Hawley ST, Griffith KA, et al. Contralateral prophylactic mastectomy decisions in a population-based sample of patients with early-stage breast cancer. JAMA Surg. 2017;152(3):274-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurian AW, Bondarenko I, Jagsi R, et al. Recent trends in chemotherapy use and oncologists' treatment recommendations for early-stage breast cancer [published online December 11, 2017]. J Natl Cancer Inst. doi: 10.1093/jnci/djx239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurian AW, Friese CR, Bondarenko I, et al. Second opinions from medical oncologists for early-stage breast cancer: prevalence, correlates, and consequences. JAMA Oncol. 2017;3(3):391-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurian AW, Griffith KA, Hamilton AS, et al. Genetic testing and counseling among patients with newly diagnosed breast cancer. JAMA. 2017;317(5):531-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurian AW, Li Y, Hamilton AS, et al. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dillman DA, Smythe J, Christian LM. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. 3rd ed Hoboken, New Jersey: John Wiley & Sons; 2009. [Google Scholar]
- 14.United States Department of Health and Human Services Guidance Regarding Methods for De-identification of Protected Health Information in Accordance with the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. https://www.hhs.gov/hipaa/for-professionals/privacy/special-topics/de-identification/index.html#safeharborguidance. Accessed January 4, 2018.
- 15.Richards S, Aziz N, Bale S, et al. ; ACMG Laboratory Quality Assurance Committee . Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richards CS, Bale S, Bellissimo DB, et al. ; Molecular Subcommittee of the ACMG Laboratory Quality Assurance Committee . ACMG recommendations for standards for interpretation and reporting of sequence variations: revisions 2007. Genet Med. 2008;10(4):294-300. [DOI] [PubMed] [Google Scholar]
- 17.Daly MB, Pilarski R, Berry M, et al. NCCN guidelines insights: genetic/familial high-risk assessment: breast and ovarian, version 2.2017. J Natl Compr Canc Netw. 2017;15(1):9-20. [DOI] [PubMed] [Google Scholar]
- 18.Kurian AW, Hare EE, Mills MA, et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32(19):2001-2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tung N, Battelli C, Allen B, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25-33. [DOI] [PubMed] [Google Scholar]
- 20.LaDuca H, Stuenkel AJ, Dolinsky JS, et al. Utilization of multigene panels in hereditary cancer predisposition testing: analysis of more than 2,000 patients. Genet Med. 2014;16(11):830-837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desmond A, Kurian AW, Gabree M, et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 2015;1(7):943-951. [DOI] [PubMed] [Google Scholar]
- 22.Maxwell KN, Wubbenhorst B, D’Andrea K, et al. Prevalence of mutations in a panel of breast cancer susceptibility genes in BRCA1/2-negative patients with early-onset breast cancer. Genet Med. 2015;17(8):630-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thompson ER, Rowley SM, Li N, et al. Panel testing for familial breast cancer: calibrating the tension between research and clinical care. J Clin Oncol. 2016;34(13):1455-1459. [DOI] [PubMed] [Google Scholar]
- 24.Selkirk CG, Vogel KJ, Newlin AC, et al. Cancer genetic testing panels for inherited cancer susceptibility: the clinical experience of a large adult genetics practice. Fam Cancer. 2014;13(4):527-536. [DOI] [PubMed] [Google Scholar]
- 25.Couch FJ, Hart SN, Sharma P, et al. Inherited mutations in 17 breast cancer susceptibility genes among a large triple-negative breast cancer cohort unselected for family history of breast cancer. J Clin Oncol. 2015;33(4):304-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tung N, Domchek SM, Stadler Z, et al. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol. 2016;13(9):581-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delikurt T, Williamson GR, Anastasiadou V, Skirton H. A systematic review of factors that act as barriers to patient referral to genetic services. Eur J Hum Genet. 2015;23(6):739-745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manrai AK, Funke BH, Rehm HL, et al. Genetic misdiagnoses and the potential for health disparities. N Engl J Med. 2016;375(7):655-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall MJ, Reid JE, Burbidge LA, et al. BRCA1 and BRCA2 mutations in women of different ethnicities undergoing testing for hereditary breast-ovarian cancer. Cancer. 2009;115(10):2222-2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caswell-Jin JL, Gupta T, Hall E, et al. Racial/ethnic differences in multiple-gene sequencing results for hereditary cancer risk. Genet Med. 2018;20(2):234-239. doi: 10.1038/gim.2017.96 [DOI] [PubMed] [Google Scholar]
- 31.Metcalfe KA, Birenbaum-Carmeli D, Lubinski J, et al. ; Hereditary Breast Cancer Clinical Study Group . International variation in rates of uptake of preventive options in BRCA1 and BRCA2 mutation carriers. Int J Cancer. 2008;122(9):2017-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wainberg S, Husted J. Utilization of screening and preventive surgery among unaffected carriers of a BRCA1 or BRCA2 gene mutation. Cancer Epidemiol Biomarkers Prev. 2004;13(12):1989-1995. [PubMed] [Google Scholar]
- 33.Weitzel JN, McCaffrey SM, Nedelcu R, MacDonald DJ, Blazer KR, Cullinane CA. Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Arch Surg. 2003;138(12):1323-1328. [DOI] [PubMed] [Google Scholar]
- 34.Pal T, Cragun D, Lewis C, et al. A statewide survey of practitioners to assess knowledge and clinical practices regarding hereditary breast and ovarian cancer. Genet Test Mol Biomarkers. 2013;17(5):367-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Atchley DP, Albarracin CT, Lopez A, et al. Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008;26(26):4282-4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377(6):523-533. [DOI] [PubMed] [Google Scholar]
- 37.Ladabaum U, Wang G, Terdiman J, et al. Strategies to identify the Lynch syndrome among patients with colorectal cancer: a cost-effectiveness analysis. Ann Intern Med. 2011;155(2):69-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Patient flow diagram
eTable 1. Demographic and clinical characteristics of patients by genetic test type
eFigure 2. Multivariable analysis among tested patients of the correlates of receiving multiple-gene sequencing versus a BRCA1/2-only test
eTable 2. Tested genes and pathogenic variants