Key Points
Question
What are internal medicine residents’ professional development needs and perceptions of cardiology, and how are these associated with career choice?
Findings
Among internal medicine trainees, work-life balance is paramount, yet cardiology culture is perceived negatively in this regard. These factors were strongly associated with a decision to pursue or avoid a career in cardiology in both men and women.
Meaning
Efforts to increase the size and diversity of the cardiology workforce should address alignment of cardiology culture with trainees’ preferences and perceptions.
This study surveys internal medical residents physicians on the factors that encourage or dissuade them from pursuing careers in cardiology.
Abstract
Importance
Few data exist on internal medicine trainees’ selection of cardiology training, although this is important for meeting future cardiology workforce needs.
Objective
To discover trainees’ professional development preferences and perceptions of cardiology, and their relationship to trainees’ career choice.
Design, Setting, and Participants
We surveyed trainees to discover their professional development preferences and perceptions of cardiology and the influence of those perceptions and preferences on the trainees’ career choices. Participants rated 38 professional development needs and 19 perceptions of cardiology. Data collection took place from February 2009, through January 2010. Data analysis was conducted from May 2017 to December 2017.
Main Outcomes and Measures
Multivariable models were used to determine the association of demographics and survey responses with prospective career choice.
Results
A total of 4850 trainees were contacted, and 1123 trainees (of whom 625 [55.7%] were men) in 198 residency programs completed surveys (23.1% response; mean [SD] age, 29.4 [3.5] years). Principal component analysis of survey responses resulted in 8-factor and 6-factor models. Professional development preferences in descending order of significance were stable hours, family friendliness, female friendliness, the availability of positive role models, financial benefits, professional challenges, patient focus, and the opportunity to have a stimulating career. The top perceptions of cardiology in descending order of significance were adverse job conditions, interference with family life, and a lack of diversity. Women and future noncardiologists valued work-life balance more highly and had more negative perceptions of cardiology than men or future cardiologists, who emphasized the professional advantages available in cardiology. Professional development factors and cardiology perceptions were strongly associated with a decision to pursue or avoid a career in cardiology in both men and women.
Conclusions and Relevance
Alignment of cardiology culture with trainees’ preferences and perceptions may assist efforts to ensure the continued attractiveness of cardiology careers and increase the diversity of the cardiology workforce.
Introduction
Increasing cardiovascular disease prevalence, technological advances, and increasing patient diversity require continued successful recruitment of internal medicine (IM) resident physicians into cardiology fellowships to ensure an adequate future workforce.1 Although current cardiologists’ career satisfaction is high,2 little is known about what trainees (who represent the potential future cardiology workforce) value in their professional careers, how they perceive the field of cardiology, or what factors influence them to choose or avoid a career in cardiology. In particular, generational changes in career expectations and sex or racial/ethnic differences may influence specialty choice. The demographic question is especially important because diverse workforces produce better results and are needed to address stubbornly persistent health disparities,3 a particular need because cardiology currently lacks diversity.4,5
Most research on career choice in medicine explores the transition from medical school to primary residency. Many studies cite work-life balance, including lifestyle, flexibility, or hours and working conditions, as the most important factors in choosing or rejecting a specialty.6,7,8,9 Other important factors include a positive experience, exposure to role models or mentors in the chosen specialty, and interest in the subject matter or procedural focus. Learning whether these factors also drive career decisions by potential cardiology trainees is clearly germane to efforts to attract top talent into the profession. To address this data gap and to critically inform ongoing professional society efforts, including those associated with increasing the proportion of women entering cardiology, we surveyed IM resident physicians about their professional development preferences, how they perceive the field of cardiology, and how these combine to influence career choices.
Methods
A 61-item survey was emailed to 4850 trainees and 44 US program directors from February 10, 2009, through January 30, 2010. Questions regarding demographics and education/training, professional development needs, and perceptions of cardiology were answered using a 5-point Likert scale.
The survey was not sent to an institutional review board. The American College of Cardiology’s applicable policies requiring institutional review board review and exemption determination were not implemented at the time of this project; the organization retroactively determined that the study complied with the Declaration of Helsinki in April 2018.
At the time of survey completion, participants were informed that their responses would be anonymous and that survey results of the study would be analyzed in aggregate and published. A drawing for 10 iPod Touches was used to incentivize participation; names collected to facilitate the incentive award process were not used in data analysis and were made unavailable to all coauthors but 1 (A.K.R.).
Survey promotion occurred in multiple phases. In February 2008, the research team sent emails to 280 directors of cardiovascular programs asking for IM residency program director contact information at their institutions; 36 program directors responded. The physicians overseeing the survey also sent personal emails to the program directors they knew, asking them to consider participating in the survey. After this, the American College of Cardiology contacted IM program directors to secure survey participation; 44 programs agreed to circulate the survey. In February 2009, the survey was sent to the program directors to circulate to resident physicians. Finally, access to an email list of IM resident physicians was purchased from Medical Marketing Service with the 44 programs that were already participating removed. In October 2009, Medical Marketing Service sent the survey to 4850 IM resident physicians in the United States, followed by 1 reminder email.
Statistical Analyses
Principal component analysis with oblimin (oblique) rotation mapped the 38 professional development attributes into an 8-factor solution and the 19 cardiology perception attributes into a 6-factor solution. Mean values replaced missing values in factor models. To assess the weight of professional development preferences or cardiology perceptions, all of the attributes in each area were forced into a domain-specific 1-factor solution, and then a linear regression of the solution entered simultaneously on the 1 forced factor.
All quantitative variables in the instrument (excluding likelihood measures) were entered simultaneously into multivariable models that showed associations with cardiology career choice for all trainees, and women and men separately after controlling for sex, ethnicity, marital status, children, household support, salary, location, medical track, and level of training. The criterion for model entry was a P ≤ .05; the criterion for remaining in the model was a P ≤ .10. Analysis used SPSS version 24.0 (IBM) with the P values of t tests adjusted via the Bonferroni-Holmes method for multiple comparisons. Data analysis was conducted from May 2017 to December 2017.
Results
Description of Respondents
Of the 4850 individuals contacted, 1123 IM resident physicians from 198 programs completed the survey (23.2%); this group represented approximately 5% of all 2009-2010 IM trainees in the United States.10 Participants included 625 men (55.8% of the total); participants largely identified themselves as either white (n=629; 56.7%) or Asian (n=328; 29.6%) (Table 1).
Table 1. Characteristics of the Respondents Overall, by Sex, and by Career Choice.
| Characteristic | All Participants (N = 1123) | Sex, No. (%) | Cardiology Choice, No. (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men (n = 625) | Women (n = 494) | P Value | Current Cardiology (n = 267) | Considered Cardiology (n = 312) | Never Considered Cardiology (n = 542) | P Value (Current Cardiology vs Never Considered Cardiology) | P Value (Considered Cardiology vs Never Considered Cardiology) | Overall P Value | ||
| Age, mean (SD), y | 29.39 (3.47) | 29.37 (3.25) | 29.42 (3.74) | .82 | 29.01 (2.93) | 29.21 (3.69) | 29.68 (3.57) | .03 | .001 | .02 |
| Sex | ||||||||||
| Male | 625 (55.8) | 625 (100.0) | NA | NA | 210 (78.7)a | 184 (59.0) | 231 (42.6) | <.001 | <.001 | <.001 |
| Female | 494 (44.1) | NA | 494 (100.0) | NA | 57 (21.3)a | 128 (41.0) | 309 (57.0) | <.001 | <.001 | <.001 |
| Race/ethnicity | ||||||||||
| White | 629 (56.7) | 333 (53.7) | 296 (60.5) | .02 | 121 (45.7) | 167 (53.9) | 341 (63.9) | <.001 | .02 | <.001 |
| African American | 27 (2.4) | 11 (1.8) | 16 (3.3) | .27 | 9 (3.4) | 10 (3.2) | 8 (1.5) | .30 | .34 | .14 |
| Asian | 328 (29.6) | 196 (31.6) | 132 (27.0) | .16 | 92 (34.7) | 99 (31.9) | 137 (25.7) | .02 | .14 | .01 |
| Hispanic | 57 (5.1) | 30 (4.8) | 27 (5.5) | .84 | 13 (4.9) | 13 (4.2) | 31 (5.8) | >.99 | .96 | .60 |
| Native American | 3 (0.3) | 3 (0.5) | 0 | .30 | 1 (0.4) | 1 (0.3) | 1 (0.2) | >.99 | >.99 | .87 |
| Other | 96 (8.7) | 66 (10.6) | 30 (6.1) | .03 | 36 (13.6) | 31 (10.0) | 29 (5.4) | <.001 | .01 | <.001 |
| Current residency track | ||||||||||
| Categorical | 957 (85.4) | 546 (87.4) | 411 (83.2) | .13 | 259 (97.0)a | 270 (86.5) | 428 (79.0) | <.001 | .01 | <.001 |
| Preliminary | 37 (3.3) | 21 (3.4) | 16 (3.2) | .94 | 1 (0.4)a | 18 (5.8) | 18 (3.3) | .02 | .16 | .10 |
| Primary Care | 89 (7.9) | 39 (6.2) | 50 (10.1) | .02 | 4 (1.5) | 15 (4.8) | 70 (12.9) | <.001 | <.001 | <.001 |
| Medicine/ pediatrics | 26 (2.3) | 14 (2.2) | 12 (2.4) | .82 | 1 (0.4) | 5 (1.6) | 20 (3.7) | .01 | .15 | .01 |
| Medical school location | ||||||||||
| Outside US | 269 (24.0) | 183 (29.3) | 86 (17.4) | .07 | 80 (30.0) | 93 (29.8) | 96 (17.7) | .001 | <.001 | .18 |
| US | 714 (63.8) | 372 (59.5) | 342 (69.2) | .07 | 156 (58.4) | 185 (59.3) | 373 (68.8) | .01 | .02 | .18 |
| Year of medical school graduation | ||||||||||
| 2005 Or earlier | 214 (19.5) | 141 (22.9) | 73 (15.1) | .01 | 56 (21.8) | 65 (21.2) | 93 (17.4) | .58 | .57 | .28 |
| 2006 | 122 (11.1) | 63 (10.2) | 59 (12.2) | .32 | 25 (9.7) | 31 (10.1) | 66 (12.4) | .68 | .94 | .40 |
| 2007 | 294 (26.8) | 161 (26.2) | 133 (27.5) | .66 | 80 (31.1) | 70 (22.8) | 144 (27.0) | .91 | .56 | .12 |
| 2008 | 221 (20.1) | 110 (17.9) | 111 (23.0) | .42 | 48 (18.7) | 54 (17.6) | 119 (22.3) | .54 | .30 | .19 |
| 2009 Or later | 247 (22.5) | 140 (22.8) | 107 (22.2) | .77 | 49 (18.7)b | 86 (28.3) | 112 (21.0) | >.99 | .03 | .01 |
| Marital status | ||||||||||
| Single | 347 (30.9) | 180 (28.8) | 166 (33.6) | .19 | 92 (34.5) | 91 (29.2) | 164 (30.3) | .68 | >.99 | .35 |
| Partnered | 231 (20.6) | 125 (20.0) | 106 (21.5) | .65 | 40 (18.4) | 78 (25.0) | 104 (19.2) | >.99 | .13 | .08 |
| Married | 523 (46.6) | 312 (49.9) | 210 (42.5) | .05 | 122 (45.7) | 140 (44.9) | 261 (48.2) | >.99 | >.99 | .61 |
| Divorced or separated | 12 (1.1) | 5 (0.8) | 7 (1.4) | .60 | 4 (1.5) | 2 (0.6) | 6 (1.1) | >.99 | >.99 | .60 |
| Other | 8 (0.7) | 3 (0.5) | 5 (1.0) | .57 | 0 | 1 (0.3) | 7 (1.3) | .12 | .31 | .08 |
| Spouse or partner works outside the home | ||||||||||
| Yes | 640 (84.3) | 339 (77.4) | 301 (94.1) | <.001 | 133 (76.4) | 186 (85.3) | 321 (87.5) | .01 | >.99 | .01 |
| No | 118 (15.5) | 99 (22.6) | 18 (5.6) | <.001 | 40 (23.0) | 32 (14.7) | 46 (12.5) | .01 | >.99 | .01 |
| Have children | ||||||||||
| Yes | 199 (17.8) | 133 (21.3) | 66 (13.4) | .01 | 48 (18.0) | 52 (16.7) | 99 (18.3) | >.99 | >.99 | .84 |
| No | 922 (82.2) | 492 (78.7) | 428 (86.6) | .01 | 219 (82.0) | 260 (83.3) | 443 (81.7) | >.99 | >.99 | .84 |
| Planning to have more children in the future | ||||||||||
| Yes | 128 (62.9) | 93 (68.9) | 35 (52.2) | .03 | 32 (66.7) | 33 (63.5) | 63 (61.8) | >.99 | >.99 | .91 |
| No | 37 (18.0) | 20 (14.8) | 17 (25.4) | .07 | 4 (8.3) | 9 (17.3) | 24 (23.5) | .07 | .94 | .07 |
| Not sure | 35 (17.1) | 22 (16.3) | 13 (19.4) | .58 | 12 (25.0) | 10 (19.2) | 13 (12.7) | .22 | >.99 | .20 |
| Current cardiology | 267 (23.9) | 210 (33.6) | 57 (11.5) | <.001 | 267 (100.0) | 0 | 0 | NA | NA | NA |
| Considered cardiology | 312 (27.9) | 184 (29.4) | 128 (25.9) | .29 | 0 | 312 (100.0) | 0 | NA | NA | NA |
| Never considered cardiology | 542 (48.3) | 231 (37.0) | 309 (62.6) | <.001 | 0 | 0 | 542 (100.0) | NA | NA | NA |
Abbreviation: NA, not applicable.
Significant at .001 level between the subgroups current cardiology and considered cardiology.
Significant at .02 level between the subgroups current cardiology and considered cardiology.
The survey participant pool varied demographically from all 2009-2010 IM trainees,10 with more white individuals (56.7% in the survey participants vs 40% of all 2009-2010 IM trainees) and fewer Asian individuals (29.6% vs 39%), African American individuals (2.4% vs 6%), and Hispanic individuals (5.1% vs 9%). Of the 1123 survey participants, 267 (23.9%) had selected cardiology, intervention, or electrophysiology fellowships; an additional 312 (27.9%) had considered cardiology. Those choosing cardiology included a higher proportion of Asian individuals (92 of 328; 28.0%) and fewer white individuals (121 of 629; 19.2%), while more women than men said they never considered cardiology (women: 309 of 494; 62.6% vs men: 231 of 625; 37.0%) (Table 1). Careers selected by those not choosing cardiology are shown in eTable 1 in the Supplement.
Professional Development Importance
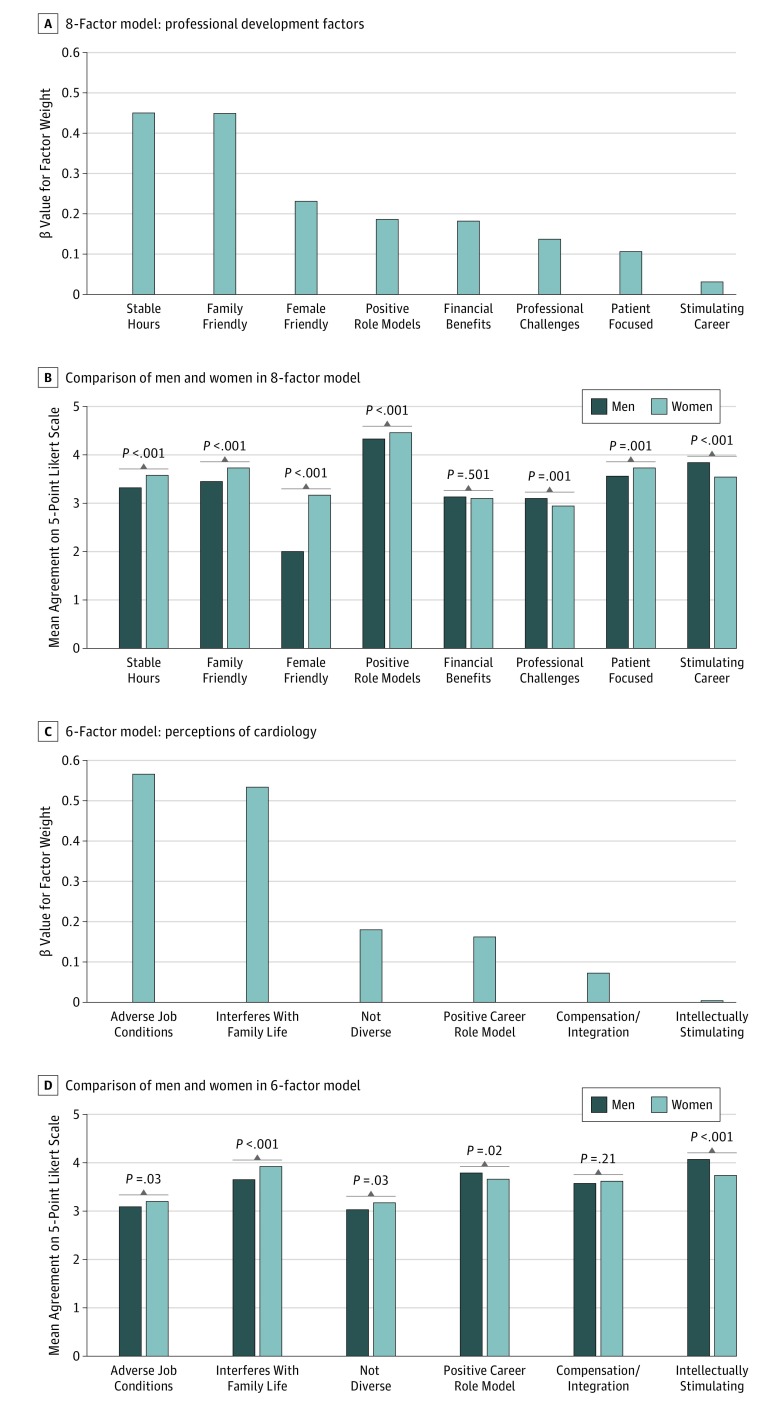
The perceived importance of the 38 professional development factors was highest for subject matter in my field of choice, followed by supportive role model and positive encouragement (eTable 2 in the Supplement). Principal component analysis revealed 8 major factors explaining 59% of the variance (in decreasing order of influence): stable hours, family friendliness, female friendliness, positive role model, financial benefits, professional challenges, patient focus, and stimulating career (eTable 2 in the Supplement; Figure 1A and 1B).
Figure 1. Importance of Professional Development Considerations and Agreement With Survey Statements on Perceptions of Cardiology.
A, Professional development factors for all respondents by β value for the factor weight; this model explains 59% of variance. B, Professional development factors by sex by β value. C, Agreement with perceptions of cardiology for all respondents by β value for the factor weight; this model explains 62% of variance. D, Perceptions of cardiology by sex by β value.
Survey participants scored all survey items on a Likert scale of 1 (agreement) to 5 (disagreement). Compared with men, women more highly valued stable hours (men: mean score, 3.32; women: 3.58; P < .001), family friendliness (men: 3.45; women: 3.73; P < .001) and female friendliness (men: 1.98; women: 3.17; P < 001), patient focus (men: 3.56; women: 3.73; P = .001), and positive role models (men: 4.33; women: 4.46; P < .001), although most differences were small, while men more highly valued professional challenges (men: 3.10; women: 2.94; P = .001) and a stimulating career (men: 3.84; women: 3.54; P < .001). Future cardiologists valued professional challenges (current cardiologists: 3.32; those who considered cardiology: 3.20; those who never considered cardiology: 2.79; P < .001) and a stimulating career more highly (current cardiologists: 4.16; those who considered cardiology: 3.73; those who never considered cardiology: 3.47; P < .001), while noncardiologists emphasized stable hours (current cardiologists: 3.11; those who considered cardiology: 3.54; those who never considered cardiology: 3.53; P < .001), family friendliness (current cardiologists: 3.38; those who considered cardiology: 3.64; those who never considered cardiology: 3.63; P < .001), and female friendliness (current cardiologists: 2.26; those who considered cardiology: 2.65; those who never considered cardiology: 2.57; P < .001) (eTable 2 in the Supplement).
Cardiology Perceptions
Agreement with the 19 perceptions of cardiology was highest with the item having met positive role models in the field of cardiology (a mean score of 4.11 on a scale of 5 across all participants), followed by intellectual attractiveness of cardiac pathophysiology (a mean score of 3.92), salaries of cardiologists in private practice are reasonable (a mean score of 3.89), and statements regarding the field’s interference with family life (a mean score of 3.77) (eTable 3 in the Supplement). Principal component analysis explained 62% of variance and revealed 6 major factors (in decreasing order of influence): adverse job conditions (β = 0.566; mean score 3.14), family life and having children (β = 0.534; mean score of 3.77), diversity of the field (β = 0.180; mean score of 3.09), positive role models (β = 0.162; mean score of 3.74), compensation and work-life integration (β = 0.072; mean score of 3.60), and intellectual stimulation (β = 0.004; mean score of 3.92) (eTable 3 in the Supplement; Figure 1C and 1D). Compared with men, women were more likely to associate cardiology with adverse job conditions (men: mean score, 3.09; women: 3.20; P = .03), interference with family life (men: mean score, 3.65; women: 3.92; P < .001), and a lack of diversity (men: mean score, 3.03; women: 3.17; P = .03), while men found cardiology more intellectually stimulating (men: mean score, 4.07; women: 3.74; P < .001) and perceived it to be a field with positive role models (men: mean score, 3.79; women: 3.66; P = .02) (eTable 3 in the Supplement).
Residents choosing cardiology emphasized positive aspects of cardiology. Those not choosing cardiology were more likely to agree with perceptions describing interference with family life (those who never considered cardiology: 3.84; those who considered cardiology: 3.86; current cardiologists: 3.53; P = .001), challenges of having children during cardiology fellowship (those who never considered cardiology: 3.95; those who considered cardiology: 3.96; current cardiologists: 3.56; P < .001), and excessive demands of a cardiology career (those who never considered cardiology: 3.27; those who considered cardiology: 3.35; current cardiologists: 2.99; P < .001).
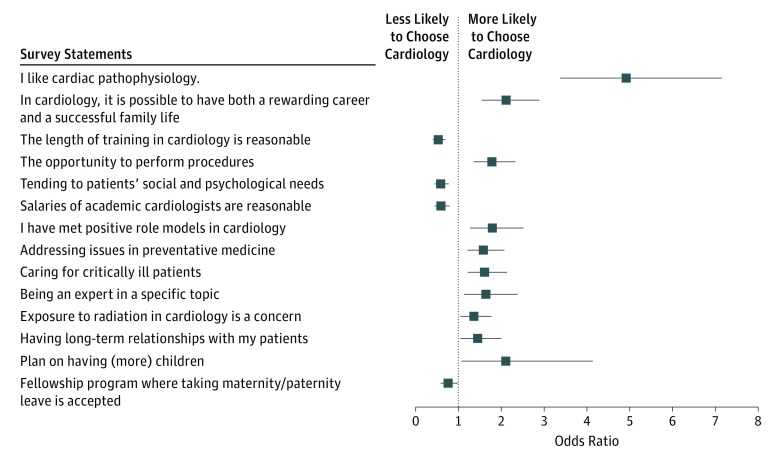
Factors Associated With Cardiology Career Choice
Multivariate analysis of demographics, professional development needs, and perceptions of cardiology yielded a model of 14 elements associated with choosing cardiology as a career with 89.4% accuracy, 75.3% sensitivity, and 93.8% specificity (Table 2 and Figure 2). The greatest driver of choosing cardiology was agreement with the statement “I like cardiac pathophysiology” (OR, 4.91 [95% CI, 3.37-7.14]). Other factors included agreement that cardiology offers the possibility of a rewarding career and family life (OR, 2.11 [95% CI, 1.54-2.88]) and the importance of the opportunity to perform procedures (OR, 1.78 [95% CI, 1.36-2.32]).
Table 2. Multivariate Factors Associated With Choosing or Not Choosing Cardiologya.
| Variable | Source of Variable | All Respondents (n = 1123) | Men (n = 625) | Women (n = 494) | ||||
|---|---|---|---|---|---|---|---|---|
| Factor Within Domain | Domain | Wald Statistic | Adjusted OR (95% CI) | Wald Statistic | Adjusted OR (95% CI) | Wald Statistic | Adjusted OR (95% CI) | |
| I like cardiac pathophysiology | Intellectually stimulating | PC | 68.88 | 4.91 (3.37-7.14) | 39.78 | 4.42 (2.79-7.02) | 12.25 | 190.96 (10.08-3616.92) |
| In cardiology, it is possible to have both a rewarding career /successful family life | Compensation and work integration | PC | 21.86 | 2.11 (1.54-2.88) | 12.70 | 2.06 (1.38-3.05) | NS | NS |
| The length of training in cardiology is reasonableb | Compensation and work integration | PC | 20.80 | 0.53 (0.4-0.69) | 10.61 | 0.57 (0.40-0.80) | 6.88 | 0.06 (0.01-0.50) |
| The opportunity to perform procedures | Professional challenges | PD | 17.60 | 1.78 (1.36-2.32) | 12.57 | 2.00 (1.37-2.94) | 6.86 | 7.53 (1.66-34.13) |
| Tending to patients’ social and psychological needsb | Patient focus | PD | 14.23 | 0.58 (0.44-0.78) | 10.41 | 0.53 (0.36-0.78) | NS | NS |
| Salaries of academic cardiologists are reasonableb | Compensation and work integration | PC | 12.20 | 0.59 (0.44-0.79) | 10.36 | 0.55 (0.38-0.79) | 10.45 | 0.03 (0.00-0.27) |
| I have met positive role models in cardiology | Cardiovascular role model | PC | 11.07 | 1.79 (1.27-2.51) | 7.65 | 1.97 (1.22-3.18) | NS | NS |
| Addressing issues in preventative medicine | Patient focus | PD | 11.02 | 1.58 (1.21-2.07) | 7.21 | 1.63 (1.14-2.33) | NS | NS |
| Caring for critically ill patients | Stimulating career | PD | 10.86 | 1.61 (1.21-2.13) | 9.01 | 1.74 (1.21-2.50) | NS | NS |
| Being an expert in a specific topic | Stimulating Career | PD | 6.72 | 1.64 (1.13-2.38) | 3.91 | 1.67 (1.00-2.76) | NS | NS |
| Exposure to radiation in cardiology is a concern | Adverse job conditions | PC | 5.09 | 1.36 (1.04-1.77) | 5.53 | 1.55 (1.08-2.24) | NS | NS |
| Having long-term relationships with my patients | Patient focus | PD | 5.05 | 1.45 (1.05-2.0) | 4.31 | 1.53 (1.02-2.27) | NS | NS |
| Plan on having (more) children | Demographic | D | 4.62 | 2.10 (1.07-4.13) | NS | NS | 6.16 | 128.08 (2.78-5909.54) |
| Fellowship program where taking maternity/paternity leave is acceptedb | Family-friendly | PD | 4.34 | 0.76 (0.58-0.98) | NS | NS | NS | NS |
| The ability to hire a nanny or pay for private daycare/schoolb | Financial benefits | PD | NS | NS | 7.28 | 0.66 (0.48-0.89) | NS | NS |
| Desire to pursue a challenge | Stimulating career | PD | NS | NS | 7.35 | 2.18 (1.24-3.83) | 5.46 | 0.07 (0.01-0.65) |
| The desire for a less competitive application processa | Professional challenges | PD | NS | NS | NS | NS | 8.02 | 0.15 (0.04-0.55) |
| Having a supportive role model or mentor in my field of choice | Positive role models | PD | NS | NS | NS | NS | 6.54 | 0.09 (0.02-0.57) |
| The ability to work part-timeb | Stable hours | PD | NS | NS | NS | NS | 5.70 | 0.21 (0.06-0.75) |
Abbreviations: D, demographic; NS, not significant; PC, perceptions of cardiology; PD, professional development.
Multivariate analysis to determine factors associated with choosing cardiology compared with not choosing cardiology (including those who considered or never considered cardiology). A mark of nonsignificant (NS) indicates that this variable was not independently associated with career choice in a given group and was therefore not part of the model for that group.
Variables decreasing the likelihood of choosing cardiology.
Figure 2. Odds Ratios for Choosing Cardiology.
Items are ranked by order of importance to overall choice. Overall accuracy is 89.4% (sensitivity, 75,3% and specificity, 93.8%); for men, accuracy is 89.1% (sensitivity, 82.9%; specificity, 92.3%); for women, accuracy is 96.8% (sensitivity, 84.2%; specificity, 98.4%).
Although models for both men and women were highly accurate (with overall accuracy of 89.1%, sensitivity of 82.9%, and specificity of 92.3% for men, and overall accuracy of 96.8%, sensitivity of 84.2%, and specificity of 98.4% for women), fewer elements achieved significance in the women-only model (9 vs 14), with only 1 factor reaching significance in opposite directions (the desire to pursue a challenge). For women, only 3 of 9 elements were associated with a higher likelihood of choosing cardiology, with the remainder associated with another choice, vs 10 of 14 elements associated with men choosing cardiology.
Discussion
Little is known about factors influencing the selection of cardiology as a career. Our survey data suggest that IM trainees’ most valued aspects of professional development related to work-life balance and mentorship, while their strongest perceptions of cardiology were of a negative culture and job description at odds with their perceived needs. Both areas were strongly associated with career choice. Understanding and addressing those factors found in our survey to influence trainees’ career choice may help in ensuring the continued attractiveness of the field as well as achieving cardiology’s goal of ensuring a robust and diverse future workforce.
Among professional development needs, stable hours, family friendliness, and having a role model were more highly rated than career-specific factors such as professional challenges, patient focus, and a stimulating career. Although this may seem counter to older generations’ career expectations and perhaps even pride in long hours, physicians from Generation X (who were born from 1964 to 1980) and members of the millennial generation (who were born from 1980 to 1999), the groups that make up the survey participant group, value work-life balance, are comfortable with change and career change or mobility, and are team-oriented rather than hierarchical or workaholics, which are characteristics more common among baby boomers (those born from 1945 to 1964).11 Adoption of the “cardiology team” may stabilize work hours and improve the family friendliness of cardiology, making it a more attractive field for those who value combined agentic and communal leadership traits often seen in members of the millennial generation.12
In the most recent American College of Cardiology Professional Life Survey (2015), 88% of female cardiologists and 90% of male cardiologists reported high satisfaction with their choice of a career and would recommend cardiology to others.2 However, female cardiologists also reported greater professional constraints from family concerns, a reality that is reflected in our findings by the greater importance that women placed on stable hours and family friendliness compared with men. Gender differences in social roles may contribute to differences in career choice as well as career trajectories, including in matters of hiring13 and income.14
In contrast with the factors rated most important for professional development, trainees’ strongest perceptions of cardiology were of a negative culture and job description. While no hard data are available to substantiate or refute trainees’ perceptions, our models note that these are barriers to choosing cardiology, indicating their importance to the future workforce. Indeed, it is worth noting that negative culture, clinician burnout, and fatigue can adversely affect the quality of medical care and patient health. These issues are being increasingly addressed in medicine by diverse organizations, such as the Institute for Healthcare Improvement, which has added a fourth aim of “improving the work life of health care clinicians and staff”15(p573) to its triple aim of health care, making it a quadruple aim, and the American College of Surgeons, which has adopted a series of policy papers on issues such as parental leave,16 fatigue,17 and salary equity.18 Other professional societies have instituted broad communications campaigns to influence the pervasive culture to become more inclusive.19
There were differences in almost every perception of cardiology between trainees who chose cardiology for their fellowship and those who did not. Cardiology trainees reported more positive feelings and were less likely to report having been discouraged from considering cardiology as a career, or to consider cardiology male dominated or lacking in racial/ethnic diversity. Although it is impossible to determine whether these differences resulted from or drove trainees’ choices, it is likely that such stereotypes can and do shape decisions regarding cardiology culture and fit, even without conscious awareness.
Women had more negative perceptions about the field associated with family and work-life balance than men did; it is not surprising that female trainees might be more sensitive to such issues, because women physicians spend a far larger percentage of their time on home and family matters than do their male spouses with medical careers.20 Men were more likely to emphasize the intellectually stimulating aspects of cardiology as a career than women were; perhaps men felt less constrained by the negative perceptions of the field and could thus focus more on this positive aspect. With regard to perceptions surrounding compensation, women were more likely than men to agree that compensation for academic cardiologists is reasonable, perhaps because men earn higher salaries and achieve faster promotions, and women consequently may have lower compensation goals in academic medicine.21,22,23 Women were also more likely to negatively perceive the lack of diversity and suitable role models in cardiology. Given the slight majority of female medical-school matriculants and IM resident physicians, identifying and addressing cultural and societal barriers in women’s perceptions of cardiology is crucial for the field to access the full range of talent in IM.
We performed multivariate analyses to determine which factors were associated with trainees’ selecting a cardiology fellowship, including demographics, professional development needs, and perceptions of cardiology. The resulting model was highly accurate (89%) and specific (94%) overall, indicating that the survey questions captured most if not all assessable career decision factors, and that the prospective cardiology specialty choice is readily assessed. Future cardiologists are both attracted to the field (liking cardiac pathophysiology, caring for critically ill patients, and doing procedures) and not deterred as noncardiologists are by work-life imbalance, long training periods, or inflexible schedules. While some of the barriers perceived by trainees may appropriately filter candidates, others may discourage outstanding candidates from choosing cardiology, thus hampering recruitment. These findings can inform efforts to diversify the cardiology workforce, with the robustness of the data strongly supporting an actionable strategy of emphasizing positive elements and addressing the negative ones. For example, energy and passion in teaching cardiovascular physiology and pathology to medical students and residents and the availability of positive role models, coupled with flexible scheduling and parental leave policies, are likely to increase the attractiveness of the field.
Our findings also provide important guidance to such efforts to increase the proportion of women in the cardiology workforce, because the career choice models, while equally accurate, were strikingly different between men and women. In general, the model for women was a negative one, incorporating elements causing them to avoid the specialty, while the model for men emphasized positive drivers. As with all resident physicians, attracting women requires emphasizing the positive elements while mitigating the negative. However, for women, addressing the deterrents is especially important and likely to be most influential. Given the striking paucity of women considering cardiology compared with men, it appears that formal efforts may be required to achieve sex parity.
Implications
Our findings regarding IM trainees’ professional development preferences and perceptions of cardiology represent the first exploration of how such issues influence the future cardiology workforce. Because the composition, capacity, and diversity of the workforce is associated with the quality of patient care and reducing health care disparities,3 our data are crucial.
Despite high satisfaction among cardiologists,2 trainees’ negative perceptions are not wholly unfounded, indicating that targeted efforts to address work-life balance and enhance mentorship are important to influencing career choice as well as improving career satisfaction. Along with other organizations, the American College of Cardiology is currently increasing its emphasis on the importance of clinician well-being, recognizing its importance to optimizing patient care.15,25 The adoption of the quadruple aim by the Institute for Healthcare Improvement acknowledges that the responsibility for meaningful change lies with professional organizations and health care systems and not solely with the individual practitioner. While further research is needed to determine which efforts are most effective, visible, and helpful for trainees, initiatives to increase the capacity and diversity of the future cardiology workforce should address the apparent misalignment of cardiology culture with trainees’ professional needs.
Limitations
Broader deployment of this survey was limited by logistic factors, but it was still representative10 and congruent with demographics of the class of 2015-2016, the most recent group for which data have been published. Indeed, our results are well aligned with the literature in terms of what influences career choice among physicians,6,7,8,9 and there is little reason to expect substantial deviation over the last 5 to 10 years. In addition, the validity and importance of our findings is supported by the lack of meaningful increase in the proportion of female trainees in cardiology since 2010.24 While comparison of men and women choosing cardiology is interesting, this was precluded by the small number of women choosing cardiology (n = 57; 5.1% of the overall sample); similarly, small sample sizes meant that we could not analyze choices by race/ethnicity. An additional possible consideration is potential bias with a higher proportion of those interested in cardiology as a career more likely to respond to a survey on cardiology career choice.
Conclusions
In this first-ever survey of IM trainees, we found that work-life balance is seen as paramount for professional development, yet cardiology culture is perceived negatively in this area. This is especially true for women and future noncardiologists and is associated with choosing careers other than cardiology. Among those choosing cardiology fellowships, these negative factors are offset by an attraction to the cardiology discipline. Efforts to increase the capacity and diversity of the future cardiology workforce should address the apparent misalignment of cardiology culture with trainees’ professional needs.
eTable 1. Career Choices of Those Not Selecting Cardiology
eTable 2. Importance of Factors in Professional Development
eTable 3. Agreement with Perceptions of the Cardiology Field
eAppendix. Internal Medicine Residents Survey – 2009-2010
References
- 1.Rodgers GP, Conti JB, Feinstein JA, et al. ACC 2009 survey results and recommendations: addressing the cardiology workforce crisis; a report of the ACC board of trustees workforce task force. J Am Coll Cardiol. 2009;54(13):1195-1208. doi: 10.1016/j.jacc.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 2.Lewis SJ, Mehta LS, Douglas PS, et al. ; American College of Cardiology Women in Cardiology Leadership Council . Changes in the professional lives of cardiologists over 2 decades. J Am Coll Cardiol. 2017;69(4):452-462. doi: 10.1016/j.jacc.2016.11.027 [DOI] [PubMed] [Google Scholar]
- 3.Xierali IM, Castillo-Page L, Zhang K, Gampfer KR, Nivet MA. AM last page: the urgency of physician workforce diversity. Acad Med. 2014;89(8):1192. doi: 10.1097/ACM.0000000000000375 [DOI] [PubMed] [Google Scholar]
- 4.Douglas PS, Williams KA Sr, Walsh MN. Diversity matters. J Am Coll Cardiol. 2017;70(12):1525-1529. doi: 10.1016/j.jacc.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 5.Page KR, Castillo-Page L, Poll-Hunter N, Garrison G, Wright SM. Assessing the evolving definition of underrepresented minority and its application in academic medicine. Acad Med. 2013;88(1):67-72. doi: 10.1097/ACM.0b013e318276466c [DOI] [PubMed] [Google Scholar]
- 6.Reed CE, Vaporciyan AA, Erikson C, et al. Factors dominating choice of surgical specialty. J Am Coll Surg. 2010;210(3):319-324. doi: 10.1016/j.jamcollsurg.2009.11.016 [DOI] [PubMed] [Google Scholar]
- 7.Goldacre MJ, Goldacre R, Lambert TW. Doctors who considered but did not pursue specific clinical specialties as careers: questionnaire surveys. J R Soc Med. 2012;105(4):166-176. doi: 10.1258/jrsm.2012.110173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grigg M, Arora M, Diwan AD. Australian medical students and their choice of surgery as a career: a review. ANZ J Surg. 2014;84(9):653-655. doi: 10.1111/ans.12389 [DOI] [PubMed] [Google Scholar]
- 9.Smith F, Lambert TW, Pitcher A, Goldacre MJ. Career choices for cardiology: cohort studies of UK medical graduates. BMC Med Ed. 2013;13:10. doi: 10.1186/1472-6920-13-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brotherton SE, Etzel SI. Graduate medical education, 2009-2010. JAMA. 2010;304(11):1255-1270. doi: 10.1001/jama.2010.1273 [DOI] [PubMed] [Google Scholar]
- 11.Mohr NM, Moreno-Walton L, Mills AM, Brunett PH, Promes SB; Society for Academic Emergency Medicine Aging and Generational Issues in Academic Emergency Medicine Task Force . Generational influences in academic emergency medicine: teaching and learning, mentoring, and technology (part I). Acad Emerg Med. 2011;18(2):190-199. doi: 10.1111/j.1553-2712.2010.00985.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bass BM. Two decades of research and development in transformational leadership. Eur J Work Organ Psychol. 1999;8(1):9-32. doi: 10.1080/135943299398410 [DOI] [Google Scholar]
- 13.Isaac C, Lee B, Carnes M. Interventions that affect gender bias in hiring: a systematic review. Acad Med. 2009;84(10):1440-1446. doi: 10.1097/ACM.0b013e3181b6ba00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jagsi R, Biga C, Poppas A, et al. Work activities and compensation of male and female cardiologists. J Am Coll Cardiol. 2016;67(5):529-541. doi: 10.1016/j.jacc.2015.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi: 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Surgeons Statement on the importance of parental leave. https://www.facs.org/about-acs/statements/84-parental-leave. Published February 24, 2016. Accessed April 20, 2018. [PubMed]
- 17.American College of Surgeons Statement on peak performance and management of fatigue. https://www.facs.org/about-acs/statements/70-peak-performance. Published August 1, 2014. Accessed April 20, 2018. [PubMed]
- 18.American College of Surgeons Statement on gender salary equity. https://www.facs.org/about-acs/statements/101-gender-salary-equity. Published August 2, 2017. Accessed April 20, 2018.
- 19.Royal Australasian College of Surgeons Diversity & inclusion plan. https://www.surgeons.org/media/24924140/2016_12_20_diversity_and_inclusion_plan.pdf. Published November 2016. Accessed January 9, 2018.
- 20.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344-353. doi: 10.7326/M13-0974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holliday EB, Jagsi R, Wilson LD, Choi M, Thomas CR Jr, Fuller CD. Gender differences in publication productivity, academic position, career duration, and funding among U.S. academic radiation oncology faculty. Acad Med. 2014;89(5):767-773. doi: 10.1097/ACM.0000000000000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. JAMA. 2012;307(22):2410-2417. doi: 10.1001/jama.2012.6183 [DOI] [PubMed] [Google Scholar]
- 23.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in salary in a recent cohort of early-career physician-researchers. Acad Med. 2013;88(11):1689-1699. doi: 10.1097/ACM.0b013e3182a71519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Association of American Medical Colleges Active physicians by sex and specialty. https://www.aamc.org/data/workforce/reports/458712/1-3-chart.html. Published 2015. Accessed January 9, 2018.
- 25.American College of Cardiology ACC sets new vision for the future. http://www.acc.org/latest-in-cardiology/articles/2017/09/20/09/28/acc-sets-new-vision-for-the-future. Published September 20, 2017. Accessed January 9, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Career Choices of Those Not Selecting Cardiology
eTable 2. Importance of Factors in Professional Development
eTable 3. Agreement with Perceptions of the Cardiology Field
eAppendix. Internal Medicine Residents Survey – 2009-2010