Key Points
Question
What are the differences in clinical presentation between elderly (age ≥65 years) and younger patients with multifocal fibromuscular dysplasia?
Findings
In this multicenter registry study, elderly patients with multifocal fibromuscular dysplasia were more likely to be asymptomatic and less likely to have had a major vascular event or revascularization procedure.
Meaning
Elderly patients with fibromuscular dysplasia may represent a more benign clinical phenotype.
Abstract
Importance
Fibromuscular dysplasia (FMD) is a nonatherosclerotic arterial disease that predominately affects women and is most commonly diagnosed in middle age. The natural history of FMD among patients diagnosed at an older age is not well understood.
Objective
To examine the differences in clinical presentation, arterial bed involvement, vascular events, and need for vascular procedures between younger and older patients with FMD.
Design, Setting, and Participants
Analysis of baseline data for patients enrolled in the US Registry for FMD as of December 15, 2016, at referral centers participating in the US Registry for FMD. Patients 18 years and older at the time of enrollment and those with only confirmed multifocal (string of beads type) FMD were included. Patients were categorized according to age at the time of diagnosis (≥65 years vs <65 years).
Main Outcomes and Measures
Prevalence of specific symptoms, vascular events, and prior vascular procedures at the time of enrollment in the registry.
Results
A total of 1016 patients were included in the analysis, of whom, 170 (16.7%) were 65 years or older at the time of diagnosis. Older patients with FMD were more likely to be asymptomatic at the time of diagnosis (4.2% vs 1.4%; P = .02). Headache and pulsatile tinnitus, both common manifestations of FMD, were less common in older patients (40.5% vs 69.1%; P < .001 and 30% vs 44.6%; P < .001, respectively). Extracranial carotid arteries were more commonly involved in patients 65 years or older at time of diagnosis (87% vs 79.4%; P = .03). There was no difference in prevalence of renal artery involvement, number of arterial beds involved, or diagnosis of any aneurysm. Patients 65 years or older were less likely to have had a major vascular event (37.1% vs 46.1%; P = .03) and fewer had undergone a therapeutic vascular procedure (18.5% vs 33.1%; P < .001).
Conclusions and Relevance
In the US Registry for FMD, patients 65 years or older at the time of diagnosis of multifocal FMD were more likely to be asymptomatic, had lower prevalence of major vascular events, and had undergone fewer therapeutic vascular procedures than younger patients. Patients with multifocal FMD diagnosed at an older age may have a more benign phenotype and fewer symptoms.
This study examines the differences in clinical presentation, arterial bed involvement, vascular events, and need for vascular procedures between younger and older patients with fibromuscular dysplasia.
Introduction
Fibromuscular dysplasia (FMD) is nonatherosclerotic arterial disease that predominately affects women. Fibromuscular dysplasia has historically been considered a disease of young women, but data have shown that it can affect all age groups and is most commonly diagnosed in middle age.1,2 The prevalence of FMD in the general population is unknown.3 Some reports suggest it may be as high as 4%, but this is based on data derived from potential living kidney donors, which is subject to selection bias.3 Clinical manifestations of FMD are determined by location and severity of arterial lesions. Clinical presentation is variable and may be limited to symptoms affecting quality of life, such as headaches and pulsatile tinnitus, or may result in more serious sequelae including arterial dissections and/or aneurysms.4 Fibromuscular dysplasia has been reported in nearly every arterial bed, although the renal and carotid/vertebral arteries are most commonly involved.1 In this report, we present baseline data from the US Registry for FMD regarding presenting manifestations, vascular events, and procedures among elderly and younger patients.
Methods
The design of the US Registry for FMD has been previously published; enrollment began in January 2009.1 Each participating center obtained approval from its respective institutional board review. Written informed consent was obtained from all patients enrolled at 11 clinical centers. One clinical center had a waiver of informed consent from its institutional review board. Baseline data for patients enrolled in the US Registry for FMD as of December 15, 2016, who were 18 years or older at the time of enrollment and with confirmed multifocal (string of beads type) FMD were included in this analysis.5 Patients were categorized as 65 years and older or younger than 65 years at the time of diagnosis of FMD based on Medicare definition. A history of a major vascular event was defined as 1 or more of the following occurring up to the date of enrollment: arterial dissection, transient ischemic attack, stroke, subarachnoid hemorrhage, mesenteric ischemia, renal infarction, myocardial infarction (MI, including spontaneous coronary artery dissection), and coronary revascularization. t Tests, Wilcoxon rank sum tests, χ2, and Fisher exact tests were used to evaluate the differences between the 2 age groups. All P values reported were 2-sided, with a significance level of .05 throughout. This report presents data collected from the baseline data forms for patients enrolled in the registry.
Results
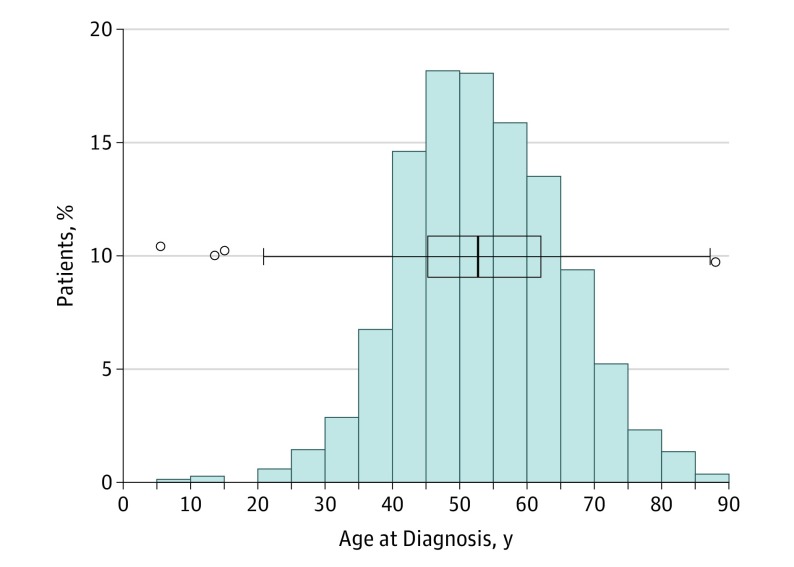
One thousand sixteen patients were included in the analysis. Age distribution is shown in the Figure; 170 patients (16.7%) were 65 years or older at the time of diagnosis of FMD. Mean (SD) age at diagnosis among older patients was 71.4 (5.1) years. Mean (SD) age at diagnosis among younger patients was 49.9 (9.2) years. There was no significant difference in percentage of patients 65 years or older at the time of diagnosis enrolled in the registry from 2009 to 2016 (2009, n = 14 of 88 [15.9%]; 2016, n = 25 of 143 [ 17.5%]; test for trend, P = .46). Most patients enrolled in the registry were women (94.9%), and there was no significant difference in sex distribution among older or younger patients (93.5% female [n = 159 of 170] among those 65 years and older vs 95.2% [n = 805 of 846] among those younger than 65 years; P = .38). Most patients in the registry were white (n = 913 of 997 [91.6%]): 88.0% among older patients (n = 147 of 167) and 92.3% among younger patients (n = 766 of 830) (P = .07). Presenting manifestations by age at diagnosis are shown in Table 1. Older patients with FMD were more likely to be asymptomatic (4.2% [n = 7 of 167] vs 1.4% [n = 12 of 840]; P = .02). Time lapse between onset of symptoms and diagnosis of FMD was longer in patients 65 years and older (7.2 years vs 3.5 years; P < .001). Headache and pulsatile tinnitus, both common manifestations of FMD, were less common in older patients. In contrast, older patients were more likely to have hypertension as a presenting manifestation of FMD. Older patients were taking more antihypertensive medications at the time of enrollment (median, 2; interquartile range, 1-2 vs median, 1; interquartile range, 0-2; P < .001). Older patients were more likely to have a carotid bruit at the baseline physical examination, but there was no significant difference in presence of bruits at other locations (epigastric, flank, and femoral; data not shown). Patients 65 years or older were less likely to have had a major vascular event (37.1% vs 46.1%; P = .03) at the baseline assessment. There was no significant difference in history of stroke, renal infarction, or subarachnoid hemorrhage between the 2 age groups. Distribution of arterial bed involvement, aneurysms, and vascular procedures is shown in Table 2. The extracranial carotid arteries were more commonly involved among older patients. There were no differences in renal, vertebral, mesenteric, or intracranial involvement between the 2 groups. There was no difference in the mean number of arterial beds involved, percentage of patients with more than 1 arterial bed (multivessel) involved, or diagnosis of aneurysm between the 2 age groups. Fewer patients 65 years or older had undergone a therapeutic vascular procedure at baseline assessment.
Figure. Age at Diagnosis of Patients Enrolled in the US Registry for Fibromuscular Dysplasia.
Table 1. Presenting Symptoms, Prior Vascular Events, and Age at Menopause of Patients With FMDa.
| Presenting Signs and Symptoms | No./Total No. (%) | P Value | ||
|---|---|---|---|---|
| Total (n = 1016) | Patients <65 y at the Time of Diagnosis (n = 846) | Patients ≥65 y at the Time of Diagnosis (n = 170) | ||
| Asymptomatic | 19/1007 (1.9) | 12/840 (1.4) | 7/167 (4.2) | .02 |
| Headache | 626/974 (64.3) | 560/811 (69.1) | 66/163 (40.5) | <.001 |
| Pulsatile tinnitus | 392/932 (42.1) | 344/772 (44.6) | 48/160 (30.0) | <.001 |
| Hypertension | 558/983 (56.8) | 442/819 (54.0) | 116/164 (70.7) | <.001 |
| Chest pain/dyspnea | 197/927 (21.3) | 170/768 (22.1) | 27/159 (17) | .15 |
| Carotid bruit | 352/950 (37.1) | 277/790 (35.1) | 75/160 (46.9) | .005 |
| Renal insufficiency | 18/475 (3.8) | 13/398 (3.3) | 5/77 (6.5) | .19 |
| Prior vascular events | ||||
| Any major vascular events | 453/1016 (44.6) | 390/846 (46.1) | 63/170 (37.1) | .03 |
| Arterial dissection | 298/1006 (29.6) | 271/837 (32.4) | 27/169 (16) | <.001 |
| Stroke | 115/998 (11.5) | 101/830 (12.2) | 14/168 (8.3) | .16 |
| Hemispheric TIA | 132/984 (13.4) | 104/817 (12.7) | 28/167 (16.8) | .16 |
| Subarachnoid hemorrhage | 24/977 (2.5) | 19/809 (2.3) | 5/168 (3) | .59 |
| Horner syndrome | 70/953 (7.3) | 67/789 (8.5) | 3/164 (1.8) | .002 |
| Renal infarction | 24/847 (2.8) | 22/701 (3.1) | 2/146 (1.4) | .41 |
| Mesenteric ischemia | 11/969 (1.1) | 9/802 (1.1) | 2/167 (1.2) | >.99 |
| CV event | 73/988 (7.4) | 69/820 (8.4) | 4/168 (2.4) | .005 |
| MI | 65/987 (6.6) | 62/819 (7.6) | 3/168 (1.8) | .003 |
| Coronary revascularization | 39/988 (3.9) | 35/820 (4.3) | 4/168 (2.4) | .38 |
| Age at menopause, mean (SD), yb | 47.8 (6.4) | 47.5 (6.5) | 48.9 (6.1) | .13 |
Abbreviations: CV, cardiovascular; FMD, fibromuscular dysplasia; MI, myocardial infarction; TIA, transient ischemic attack.
Denominator represents patients from whom data field was available.
Female patients only.
Table 2. Arterial Bed Involvement and Therapeutic Procedures of Patients With FMDa.
| FMD Arterial Bed Involvement | No./Total No. (%) | P Value | ||
|---|---|---|---|---|
| Total (n = 1016) | Patients <65 y at the Time of Diagnosis (n = 846) | Patients ≥65 y at the Time of Diagnosis (n = 170) | ||
| EC and/or vertebral | 777/946 (82.1) | 642/791 (81.2) | 135/155 (87.1) | .08 |
| EC | 757/939 (80.6) | 623/785 (79.4) | 134/154 (87.0) | .03 |
| Vertebral | 300/766 (39.2) | 255/646 (39.5) | 45/120 (37.5) | .68 |
| Intracranial | 122/712 (17.1) | 101/599 (16.9) | 21/113 (18.6) | .66 |
| Renal | 559/888 (63) | 473/747 (63.3) | 86/141 (61) | .60 |
| Mesenteric | 105/657 (16) | 87/561 (15.5) | 18/96 (18.8) | .42 |
| No. of arterial beds, mean (SD); median | 2.0 (1.1); 2 | 2.0 (1.1); 2 | 2.0 (1.0); 2 | .54 |
| Patients with multivessel involvement | 610/1016 (60) | 510/846 (60.3) | 100/170 (58.8) | .72 |
| Arterial aneurysm | 233/1000 (23.3) | 191/832 (23) | 42/168 (25) | .57 |
| Therapeutic procedures | ||||
| Any therapeutic vascular procedures at time of enrollment | 309/1007 (30.7) | 278/839 (33.1) | 31/168 (18.5) | <.001 |
Abbreviations: EC, extracranial carotid; FMD, Fibromuscular dysplasia.
Denominator represents patients from whom data field was available or who underwent imaging assessment of a listed arterial bed.
Discussion
To our knowledge, this study is the first to describe the presentation and clinical features of FMD among patients 65 years or older at time of FMD diagnosis. Patients 65 years and older at the time of diagnosis of FMD had lower frequency of major vascular events and had undergone fewer vascular procedures, although the frequency of multivessel involvement and aneurysms was not significantly different between the groups. These findings suggest the possibility of a milder clinical phenotype of FMD when diagnosed in elderly patients.
Patients 65 years or older at time of diagnosis constituted 16.7% of the study population, which confirms previous data that FMD is a vascular disease of all age groups.1,2 Savard et al2 reported that focal and multifocal FMD were associated with different clinical phenotypes and patients with focal FMD were significantly younger than patients with multifocal FMD. As a result, patients with focal FMD were excluded from this analysis. It has been suggested that focal FMD may represent an entirely distinct disease entity than multifocal disease.6
Headache and pulsatile tinnitus were the most common presenting symptoms of FMD in the US registry.5 Older patients were less likely to experience these symptoms compared with younger patients, which could potentially contribute to the later age at diagnosis. Furthermore, although few patients were asymptomatic in both age groups, older patients were more likely to be asymptomatic at time of diagnosis and perhaps diagnosed incidentally during imaging studies performed for non–FMD-related reasons.
Arterial dissections, including spontaneous coronary artery dissection, have been associated with FMD4,7,8 and are a common mechanism of ischemic events, including MI and stroke, in this patient population. In this cohort, older patients had fewer major vascular events including arterial dissection and MI. Subarachnoid hemorrhage was rare in both age groups. Hypertension was more common in the older patients. While FMD is a known etiology for renovascular hypertension,9,10 essential hypertension and uncontrolled hypertension are independently associated with age.11
Multifocal FMD usually involves more than 1 arterial bed,12,13 and the percentage of patients with multivessel involvement was similar in both age groups (approximately 60%). Aneurysm is common among patients with FMD and was previously reported in 21.7% of patients in the US registry.4 Women with FMD have higher prevalence of intracranial aneurysm compared with the general population.14 In this analysis, aneurysm prevalence was not significantly different in the age groups. While the extracranial carotid arteries were more commonly involved in older patients, involvement of other arterial beds was similar. Given the lower frequency of vascular events, headache, and pulsatile tinnitus among older patients, it is possible that fewer imaging studies were obtained, contributing to a delay in diagnosis of FMD until imaging is performed for another indication.
It is not clear how hormonal factors and menopause play a role in FMD.3 While most patients enrolled in the US Registry for FMD were women, we found no difference in mean age at diagnosis or percentage of patients diagnosed at 65 years or older between female and male patients. Among female patients, there was no difference in age at onset of menopause between those diagnosed at an older or younger age.
Limitations
The study sample is derived from patients enrolled in the US registry for FMD. The registry is subject to referral bias because academic referral centers represent most sites. The elderly population may be underrepresented in the registry because FMD is not usually considered in older patients. Health care clinicians may attribute nonspecific symptoms to the aging process, and elderly patients may not be referred as often for vascular imaging. In contrast, younger patients may be overrepresented because they may be more likely to seek online health information regarding rare diseases and self-refer to a specialty center. Additionally, not all patients underwent assessment of all arterial beds with imaging studies. The mechanism of hypertension (ie, renovascular or essential) and that of vascular events (eg, whether a stroke or MI was owing to dissection or atherosclerotic disease) is not captured in the US registry nor is there centralized imaging or angiogram review. Despite these limitations, we believe that the finding of fewer vascular events in older patients with FMD is important.
Conclusions
In the US Registry for FMD, patients 65 years or older at the time of diagnosis of multifocal FMD were more likely to be asymptomatic, had lower prevalence of major vascular events, and were less likely to have undergone therapeutic vascular procedures at enrollment compared with younger patients. Patients diagnosed as having FMD at an older age may have a more benign disease process and less severe symptoms.
References
- 1.Olin JW, Froehlich J, Gu X, et al. The United States Registry for Fibromuscular Dysplasia: results in the first 447 patients. Circulation. 2012;125(25):3182-3190. [DOI] [PubMed] [Google Scholar]
- 2.Savard S, Steichen O, Azarine A, Azizi M, Jeunemaitre X, Plouin PF. Association between 2 angiographic subtypes of renal artery fibromuscular dysplasia and clinical characteristics. Circulation. 2012;126(25):3062-3069. [DOI] [PubMed] [Google Scholar]
- 3.Shivapour DM, Erwin P, Kim ESh. Epidemiology of fibromuscular dysplasia: a review of the literature. Vasc Med. 2016;21(4):376-381. [DOI] [PubMed] [Google Scholar]
- 4.Kadian-Dodov D, Gornik HL, Gu X, et al. Dissection and aneurysm in patients with fibromuscular dysplasia: findings from the US Registry for FMD. J Am Coll Cardiol. 2016;68(2):176-185. [DOI] [PubMed] [Google Scholar]
- 5.Olin JW, Gornik HL, Bacharach JM, et al. ; American Heart Association Council on Peripheral Vascular Disease; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Functional Genomics and Translational Biology; American Heart Association Council for High Blood Pressure Research; American Heart Association Council on the Kidney in Cardiovascular Disease; American Heart Association Stroke Council . Fibromuscular dysplasia: state of the science and critical unanswered questions: a scientific statement from the American Heart Association. Circulation. 2014;129(9):1048-1078. [DOI] [PubMed] [Google Scholar]
- 6.Olin JW. Is fibromuscular dysplasia a single disease? Circulation. 2012;126(25):2925-2927. [DOI] [PubMed] [Google Scholar]
- 7.Prasad M, Tweet MS, Hayes SN, et al. Prevalence of extracoronary vascular abnormalities and fibromuscular dysplasia in patients with spontaneous coronary artery dissection. Am J Cardiol. 2015;115(12):1672-1677. [DOI] [PubMed] [Google Scholar]
- 8.Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7(5):645-655. [DOI] [PubMed] [Google Scholar]
- 9.Stanley JC, Fry WJ. Renovascular hypertension secondary to arterial fibrodysplasia in adults: criteria for operation and results of surgical therapy. Arch Surg. 1975;110(8):922-928. [DOI] [PubMed] [Google Scholar]
- 10.Harrison EG Jr, Hunt JC, Bernatz PE. Morphology of fibromuscular dysplasia of the renal artery in renovascular hypertension. Am J Med. 1967;43(1):97-112. [DOI] [PubMed] [Google Scholar]
- 11.Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation. 2005;112(11):1651-1662. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor SC, Gornik HL. Recent developments in the understanding and management of fibromuscular dysplasia. J Am Heart Assoc. 2014;3(6):e001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plouin PF, Baguet JP, Thony F, et al. ; ARCADIA Investigators . High prevalence of multiple arterial bed lesions in patients with fibromuscular dysplasia: the ARCADIA Registry (Assessment of Renal and Cervical Artery Dysplasia). Hypertension. 2017;70(3):652-658. [DOI] [PubMed] [Google Scholar]
- 14.Lather HD, Gornik HL, Olin JW, et al. Prevalence of intracranial aneurysm in women with fibromuscular dysplasia: a report from the US Registry for Fibromuscular Dysplasia. JAMA Neurol. 2017;74(9):1081-1087. [DOI] [PMC free article] [PubMed] [Google Scholar]