This cross-sectional study examines the annual burden of total out-of-pocket health expenses among low-income US families that included a member with atherosclerotic cardiovascular disease (ASCVD).
Key Points
Question
What are the financial implications of out-of-pocket health care expenses for low-income families with members with atherosclerotic cardiovascular disease?
Findings
In this cross-sectional study of a nationally representative sample of US families, 1 in 4 low-income families with a member with atherosclerotic cardiovascular disease had a high financial burden, and 1 in 10 experienced a catastrophic financial burden owing to cumulative out-of-pocket health care expenses, representing nearly 2 million low-income US families each year. Even among those with health insurance in the contemporary era, low-income families have 3-fold higher odds of high financial burden and 9-fold higher odds of catastrophic financial burden compared with mid/high–income families.
Meaning
To alleviate economic disparities, policy interventions must extend focus to improving not only access, but also quality of the coverage, particularly for low-income families that include members with chronic diseases.
Abstract
Importance
Health insurance is effective in preventing financial hardship from unexpected major health care events. However, it is also essential to assess whether vulnerable patients, particularly those from low-income families, are adequately protected from longitudinal health care costs for common chronic conditions such as atherosclerotic cardiovascular disease (ASCVD).
Objective
To examine the annual burden of total out-of-pocket health expenses among low-income families that included a member with ASCVD.
Design, Setting, and Participants
In this cross-sectional study of the Medical Expenditure Panel Survey from January 2006 through December 2015, all families with 1 or more members with ASCVD were identified. Families were classified as low income if they had an income under 200% of the federal poverty limit. Analyses began December 2017.
Main Outcomes and Measures
Total annual inflation-adjusted out-of-pocket expenses, inclusive of insurance premiums, for all patients with ASCVD. We compared these expenses against annual family incomes. Out-of-pocket expenses of more than 20% and more than 40% of family income defined high and catastrophic financial burden, respectively.
Results
We identified 22 521 adults with ASCVD, represented in 20 600 families in the Medical Expenditure Panel Survey. They correspond to an annual estimated 23 million or 9.9% of US adults with a mean (SE) age of 65 (0.2) years and included 10.9 million women (47.1%). They were represented in 21 million or 15% of US families. Of these, 8.2 million families (39%) were low income. The mean annual family income was $57 143 (95% CI, $55 377-$58 909), and the mean out-of-pocket expense was $4415 (95% CI, $3735-$3976). While financial burden from health expenses decreased throughout the study, even in 2014 and 2015, low-income families had 3-fold higher odds than mid/high–income families of high financial burden (21.4% vs 7.6%; OR, 3.31; 95% CI, 2.55-4.31) and 9-fold higher odds of catastrophic financial burden (9.8% vs 1.2%; OR, 9.35; 95% CI, 5.39-16.20), representing nearly 2 million low-income families nationally. Further, even among the insured, 1.6 million low-income families (21.8%) experienced high financial burden and 721 000 low-income families (9.8%) experienced catastrophic out-of-pocket health care expenses in 2014 and 2015.
Conclusions and Relevance
One in 4 low-income families with a member with ASCVD, including those with insurance coverage, experience a high financial burden, and 1 in 10 experience a catastrophic financial burden due to cumulative out-of-pocket health care expenses. To alleviate economic disparities, policy interventions must extend focus to improving not only access, but also quality of coverage, particularly for low-income families.
Introduction
The financial impact of acute cardiovascular events, including acute myocardial infarction and stroke, have received attention, especially among those without insurance.1 However, patients with chronic cardiovascular diseases have longitudinal care needs that are not limited to acute hospitalization events, and the impact of these expenses on patients and their families is not well studied.
Approximately 10% of the US adult population has atherosclerotic cardiovascular disease (ASCVD)2 and requires continued medical care, including outpatient care visits, prescription medications, and often diagnostic and therapeutic procedures and repeated hospitalizations.3 The expansion of insurance coverage in recent years, particularly under the Affordable Care Act, has facilitated increased access to health insurance for more US residents.4 However, there have been concerns that the expanded coverage may not adequately protect individuals from financial adversity, especially due to high health insurance premiums and out-of-pocket expenses.5,6,7,8 Moreover, while contemporary insurance reforms introduced upper limits on out-of-pocket health care expenses,9 these limits have not been scaled to income.9 In addition, upcoming insurance policy changes may further limit the coverage of important services by insurance programs.10 As a result, even if access improves, people may be underinsured. Out-of-pocket health care expenditures for essential health care needs of those with chronic diseases, such as ASCVD, may impose a substantial burden on patients and their families. An appreciation of the financial burden of cumulative health care costs among those with and without health insurance may further stimulate efforts to mitigate the impact of ASCVD among vulnerable, low-income individuals and their families.
To address these gaps in knowledge, we used a nationally representative data set to identify US families with 1 or more members affected by ASCVD and examined their total out-of-pocket health care expenditures relative to their income. We examined how the burden of out-of-pocket health care expenses for such families has evolved throughout a 10-year period spanning the implementation of recent health care reforms.
Methods
Data Source
We used the Medical Expenditure Panel Survey (MEPS) of the Agency of Healthcare Research and Quality for a 10-year period (2006-2015).11,12 We used data collected in the “Household Component” of MEPS, which is a nationally representative serial cross-sectional study of US families that undergo detailed serial interviews on the health status of its members, their demographic and financial characteristics, health care access, and the financial support for their health care needs.11 Each year, nearly 14 000 families with 35 000 members are included as a part of a complex survey sampling strategy, and the characteristics of included individuals and their families are weighted in proportion of their representativeness to the US adult population.11 To obtain more precise estimates, we pooled together data in 2-year cycles and created combined 2-year weights, using an approach suggested by the Agency of Healthcare Research and Quality.13 This study was exempt from the purview of institutional review board and did not require patient consent as it uses publicly available deidentified survey data.
Study Population and Variables
Within MEPS, we used Clinical Classification Software codes to identify all individuals 18 years or older who have ASCVD, representing a health care event or a current limitation from coronary (Clinical Classification Software codes 100 and 101), cerebrovascular (Clinical Classification Software codes 109-113), and peripheral vascular (Clinical Classification Software code 114) disease or a reported history of coronary heart disease, angina, myocardial infarction, or stroke. This approach has been used in prior studies.12 Since the financial effects of health care are shared by members of a family,14,15 we defined families as the unit of assessing financial burden of health care expenses. Family units were defined based on the Current Population Survey of the US Census Bureau,16 representing groups of people related by birth, marriage, or adoption and residing together.16 In our study, for each year of the 10-year period, we identified all families that included 1 or more members with ASCVD.
Families were classified based on their income: low-income if their annual income was under 200% of the federal poverty limit and mid/high–income if it exceeded 200% of the federal poverty limit, as suggested in prior studies.17,18 All individuals were classified into broad groups based on private or public insurance coverage. Owing to substantially different financial implications of obtaining private insurance as part of a group (eg, from employment) compared with self-purchased insurance,19,20 individuals covered with private insurance were further classified into group vs nongroup private insurance. Public insurance includes those covered with Medicare, Medicaid, Tricare, and other state-funded public insurance programs. Those covered with private and public sources during a given year were classified in the respective groups based on the insurance group that covered the individual for the longest duration in that year.19,21 Finally, those without insurance coverage for all 12 months in a calendar year were classified as being uninsured.21
Study Outcomes
Annual cumulative out-of-pocket health costs were compiled based on expenses for inpatient care, outpatient (or ambulatory) care, emergency medical care, prescription medications, as well as other health care services (home health care and medical equipment) for each year. Further, annual out-of-pocket expenses on insurance premiums were obtained on a family level, as recommended by the Agency of Healthcare Research and Quality.6,19 The total out-of-pocket health expenses represent the sum of insurance premiums and costs of all health care services.
Family income was assessed after accounting for food-related expenses (ie, postsubsistence income).1 Mean food expenses by income level were derived from nomograms available from the Bureau of Labor Statistics.22 All cost and income estimates were inflation-adjusted to represent 2015 US dollars.23
Annual out-of-pocket health care expenses in excess of 20% of the annual postsubsistence income were defined as high financial burden. Expenses that exceeded 40% of the annual postsubsistence income were defined as catastrophic financial burden, consistent with its definition endorsed by the World Health Organization.1,24,25,26,27 These 2 outcomes were chosen to identify instances when insurance coverage was inadequate to prevent major out-of-pocket spending in health care.
Statistical Analysis
We used survey-specific methods that accounted for the complex sampling design of the MEPS28,29 and used patient-level and family-level discharge weights to obtain national estimates. First, we calculated out-of-pocket health care expenses for all patients with ASCVD over the 10-year period, both overall and among subgroups of age, sex, race/ethnicity, income, and insurance groups. Next, we compared the health care expenses for the family against their income after accounting for subsistence (or food-related) expenses22 and calculated rates of high and catastrophic financial burden, with expenses representing 20% and 40% of the postsubsistence income, respectively. To report the most conservative estimates for high and catastrophic financial burden, families with expected food-related expenses that exceeded their annual income for a given year were excluded, particularly because any health care costs would qualify as catastrophic among these individuals. We performed sensitivity analyses after including these families. We used survey-specific linear regression of log-transformed costs and incomes to assess for changes over time. For categorical outcomes of high and catastrophic financial burden, we used the Cochran-Armitage trend test and the Rao-Scott χ2 test for between-group comparisons.
Further, using characteristics (age, sex, race/ethnicity, Charlson comorbidity index, history of smoking, hypertension, diabetes, dyslipidemia, liver disease, chronic kidney disease, and cancer, as defined previously12) of the index patient with ASCVD in the family (or the oldest patient in families with >1 member with ASCVD), and the size of the family, number of members with ASCVD, and the US census region of their residence in a survey-specific logistic regression, we calculated risk-adjusted rates of high and catastrophic financial burden during the study. In sensitivity analyses, we additionally accounted for characteristics of members without ASCVD and their contribution to their family’s health care expenses.
Finally, we assessed for differences in trends between subgroups based on age and insurance group (private insurance, group and nongroup; public insurance; no insurance) among low-income families by assessing for the statistical interaction between insurance groups and calendar-years. Analyses were performed using SAS, version 9.4 (SAS Institute, Inc). All statistical tests were 2-sided and the level of significance was set at .05.
Results
Characteristics of Individuals With ASCVD
There were 22 521 adults with ASCVD, represented in 20 600 families sampled in MEPS over the 10-year study period. They corresponded to an annual estimated 23 million US adults (9.9%) and 21 million US families (15%). The mean (SE) age of individuals with ASCVD was 65.8 (0.2) years, 10.9 million (47.1%) were women, 19.7 million (85%) were white, and 2.7 million (11.5%) were black. An estimated 6.5 million (28.2%) were part of a single-person family, 11.1 million (47.9%) were part of 2-member families, and 5.5 million (23.9%) were part of families with 3 or more members. An estimated 8.9 million individuals (38.8%) were part of low-income families. Finally, a similar proportion of individuals were covered with private (10.8 million [46.8%]) and public (11 million [47.4%]) insurance, and 1.4 million US adults (5.9%) with ASCVD were uninsured for an average year during the 10-year period (Table 1).
Table 1. Out-of-Pocket Health Care Costs of Care for Individuals With Atherosclerotic Cardiovascular Disease in the United States.
| Characteristica | No. in National Population, × 1000 Persons | Total Out-of-Pocket Expenditures, $ | Insurance Premium, $b | Out-of-Pocket Health Care Costs, $ | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Inpatient | Outpatient | Medications | Emergency | Other | ||||
| Overall | 23 144 (459) | 2227 (37) | 722 (16) | 1505 (33) | 110 (10) | 278 (9) | 680 (13) | 30 (2) | 407 (23) |
| Age, y | |||||||||
| 18-44 | 1870 (844) | 1353 (82) | 521 (39) | 831 (69) | 84 (20) | 214 (23) | 329 (31) | 56 (12) | 149 (31) |
| 45-64 | 8016 (202) | 2277 (54) | 847 (27) | 1429 (43) | 153 (23) | 324 (17) | 663 (22) | 45 (5) | 244 (15) |
| ≥65 | 13 258 (352) | 2321 (51) | 675 (21) | 1646 (45) | 88 (10) | 259 (10) | 740 (16) | 18 (3) | 542 (38) |
| Sex | |||||||||
| Male | 12 243 (285) | 2218 (43) | 781 (20) | 1437 (35) | 120 (13) | 282 (13) | 639 (15) | 33 (4) | 363 (20) |
| Female | 10 901 (238) | 2238 (54) | 656 (20) | 1582 (49) | 100 (16) | 273 (10) | 726 (20) | 28 (3) | 456 (39) |
| Race | |||||||||
| White | 19 679 (435) | 2355 (42) | 762 (19) | 1593 (37) | 108 (11) | 298 (10) | 714 (15) | 30 (2) | 444 (26) |
| Black | 2670 (152) | 1450 (50) | 469 (22) | 982 (45) | 141 (27) | 151 (10) | 482 (20) | 39 (9) | 169 (23) |
| Income, % of federal poverty limit | |||||||||
| <100 | 3525 (108) | 1224 (63) | 256 (25) | 969 (49) | 87 (17) | 142 (9) | 485 (24) | 33 (6) | 222 (35) |
| 100-125 | 1573 (62) | 1481 (69) | 335 (31) | 1146 (62) | 78 (19) | 145 (11) | 569 (32) | 20 (3) | 334 (51) |
| 125-200 | 3950 (113) | 1901 (75) | 505 (29) | 1397 (64) | 108 (27) | 201 (11) | 676 (27) | 38 (9) | 373 (48) |
| 200-400 | 6674 (181) | 2385 (64) | 765 (22) | 1621 (61) | 131 (24) | 297 (20) | 735 (25) | 26 (2) | 432 (46) |
| >400 | 7421 (224) | 2894 (55) | 1104 (33) | 1790 (47) | 111 (15) | 393 (15) | 748 (21) | 31 (4) | 506 (26) |
| Marital status | |||||||||
| Married | 12 443 (315) | 2460 (45) | 885 (24) | 1575 (35) | 121 (13) | 331 (14) | 734 (20) | 30 (3) | 360 (18) |
| Previously married | 8700 (239) | 2020 (66) | 525 (19) | 1495 (61) | 108 (19) | 215 (9) | 649 (18) | 26 (3) | 497 (53) |
| Never married | 2001 (75) | 1679 (107) | 566 (52) | 1113 (85) | 53 (12) | 216 (18) | 481 (44) | 53 (17) | 309 (53) |
| Family size, No. of persons | |||||||||
| 1 | 6531 (192) | 2249 (78) | 635 (27) | 1615 (74) | 100 (23) | 244 (11) | 671 (23) | 31 (5) | 569 (66) |
| 2 | 11 087 (287) | 2474 (46) | 844 (25) | 1630 (37) | 109 (12) | 323 (15) | 751 (21) | 31 (4) | 415 (21) |
| ≥3 | 5525 (156) | 1707 (48) | 582 (23) | 1125 (42) | 124 (21) | 225 (13) | 548 (22) | 29 (3) | 199 (15) |
| Insurance type | |||||||||
| Private, group | 8690 (235) | 2907 (58) | 1217 (29) | 1690 (49) | 133 (22) | 370 (17) | 722 (20) | 26 (3) | 438 (30) |
| Private, nongroup | 2131 (114) | 3634 (114) | 1748 (68) | 1886 (91) | 88 (18) | 320 (26) | 873 (44) | 41 (9) | 564 (62) |
| Public | 10 962 (274) | 1507 (45) | 200 (11)b | 1307 (44) | 92 (11) | 198 (9) | 612 (16) | 19 (2) | 386 (35) |
| Uninsured | 1361 (61) | 1490 (92) | 165 (19)c | 1324 (92) | 147 (35) | 266 (29) | 652 (62) | 126 (28) | 134 (18) |
Unless otherwise specified, numbers represent mean costs in US dollars, and those in parentheses represent standard errors for national estimates.
Premium for either period with private insurance and/or for patient’s share of coverage by family.
Patient’s share of premium expenditures for other members of the family.
Individual-Level Health Care Expenses
During the study, the mean individual-level annual out-of-pocket health expenditures among those with ASCVD were $2227, including $722 for insurance premiums and $1505 on other health expenditures, with medication costs representing nearly half (45%) of the direct spending (Table 1). While there were differences in spending across subgroups of individuals, they had a similar relative distribution of categories of spending (Table 1).
Family-Level Health Care Expenses
During the study, there were 8.2 million low-income US families annually with a member with ASCVD, representing 17.5% of all low-income families and 39.4% of families with a member with ASCVD. Further, there were 12.6 million such US families in the mid/high–income group, representing 14.3% of all mid/high–income US families (eFigure 1 in the Supplement). The mean family income was $57 143 (95% CI, $55 377-$58 909) and was 5-fold higher in the mid/high–income group than the low-income group across study years ($83 034 [95% CI, 81 014-85 055] vs $17 286 [95% CI, 16 922-17 651]; P < .001) (Table 2 and eFigure 2 in the Supplement). Notably, the mean billed health care expenditures were similar between both income groups ($20 776 in the mid/high–income group vs $19 071 in the low-income group), but low-income families had substantially lower out-of-pocket expenses ($4895 in the mid/high–income group vs $2254 in the low-income group; P < .001), with both lower insurance premiums and lower out-of-pocket expenses (Table 2). The 95% range (2.5th and 97.5th centile) for out-of-pocket spending was $58 to $15 476 in the overall population, $110 to $17 127 for mid/high–income families, and $0 to $11 084 for low-income families. This represents a mean expense-to-income ratio of 15.7% (95% range, 0.1%-62.8%) overall, 8.3% (95% range, 0.2%-32.2%) for mid/high–income families, and 28.4% (95% range, 0%-111.2%) for low-income families.
Table 2. Out-of-Pocket Health Care Costs of Care for Families With 1 or More Members With ASCVD in the United States.
| Variablea | 2006-2007 | 2008-2009 | 2010-2011 | 2012-2013 | 2014-2015 | P Value for Trendb |
|---|---|---|---|---|---|---|
| Overall | ||||||
| National population, 1000 families | 42 138 (1000) | 44 934 (1094) | 47 914 (1274) | 49 565 (1225) | 48 254 (1355) | NA |
| Family income | 59 523 (1443) | 56 777 (1473) | 56 676 (1585) | 56 287 (1581) | 57 047 (1536) | .24 |
| Total medical costs | 20 497 (662) | 19 106 (556) | 20 034 (625) | 19 137 (718) | 21 763 (642) | <.001 |
| Total out-of-pocket expenses | 4415 (130) | 4008 (109) | 3628 (103) | 3704 (144) | 3670 (107) | <.001c |
| Insurance premiums | 1686 (75) | 1521 (59) | 1480 (67) | 1549 (62) | 1670 (71) | .57 |
| Out-of-pocket health service expenses | 2729 (93) | 2487 (87) | 2148 (68) | 2156 (121) | 2000 (69) | <.001c |
| Out-of-pocket expenses for member(s) with ASCVD | 1926 (62) | 1792 (74) | 1514 (51) | 1483 (94) | 1434 (58) | <.001c |
| Mid/high–income families | ||||||
| National population, 1000 families | 36 099 (940) | 36 502 (927) | 39 458 (1109) | 40 567 (1056) | 39 413 (1239) | NA |
| Family income | 84 627 (1736) | 81 975 (1889) | 82 601 (1812) | 83 705 (2015) | 82 651 (1830) | .65 |
| Total medical costs | 21 120 (967) | 19 424 (749) | 20 627 (807) | 20 386 (1083) | 22 296 (844) | .002 |
| Total out-of-pocket expenses | 5292 (171) | 5039 (134) | 4567 (126) | 4869 (188) | 4801 (143) | <.001b |
| Insurance premiums | 2213 (101) | 2069 (85) | 2013 (89) | 2196 (87) | 2319 (99) | .71 |
| Out-of-pocket health service expenses | 3078 (125) | 2970 (106) | 2554 (84) | 2672 (169) | 2482 (95) | <.001c |
| Out-of-pocket expenses for member(s) with ASCVD | 2063 (76) | 2029 (92) | 1735 (66) | 1762 (134) | 1713 (82) | <.001c |
| Low-income families | ||||||
| National population, in 1000 families | 6039 (224) | 8432 (359) | 8456 (359) | 8999 (329) | 8841 (340) | NA |
| Family income | 17 215 (345) | 17 759 (367) | 16 991 (357) | 17 507 (376) | 16 941 (336) | .21 |
| Total medical costs | 19 446 (744) | 18 615 (697) | 19 127 (1027) | 17 371 (689) | 20 927 (969) | .004 |
| Total out-of-pocket expenses | 2937 (132) | 2412 (129) | 2192 (107) | 2057 (135) | 1899 (107) | <.001c |
| Insurance premiums | 798 (75) | 672 (46) | 664 (58) | 632 (51) | 653 (68) | .76 |
| Out-of-pocket health service expenses | 2139 (98) | 1740 (112) | 1528 (93) | 1425 (115) | 1246 (82) | <.001c |
| Out-of-pocket expenses for member(s) with ASCVD | 1697 (84) | 1424 (98) | 1177 (87) | 1089 (98) | 996 (73) | <.001c |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; NA, not applicable.
Unless otherwise specified, numbers represent mean costs in US dollars, and those in parentheses represent standard errors for national estimates.
P value for trend for log of corresponding income or expense.
P value for negative trend.
Mean out-of-pocket spending decreased in both income groups, with a larger relative decrease among low-income families vs mid/high–income families (35.3% relative decrease vs 9.3% relative decrease; P for interaction <.001 [year × income group]) (Table 2). Further, health care spending on family members with ASCVD represented a mean of 70% of the overall family out-of-health spending and 82% for low-income families (Table 2 and eTable 1 in the Supplement). Insurance premiums and prescription medications were the largest categories of spending for families, representing 44% and 22% of spending on health care of mid/high–income families, respectively, and 30% and 34% of health care expenses for low-income families, respectively (eTable 1 and eFigure 3 in the Supplement).
High and Catastrophic Financial Burden
A mean of 13.7% (or 2.7 million) of families that had a member with ASCVD experienced high financial burden (ie, expenses exceeding 20% of postsubsistence income) each year from 2006 to 2015 and 4.9% (or 1 million families) experienced catastrophic financial burden (ie, expenses exceeding 40% of postsubsistence income) owing to out-of-pocket health expenses. Compared with mid/high–income families, low-income families had nearly 4-fold higher odds of high financial burden (7.0% vs 25.0%; OR, 4.42; 95% CI, 3.91-4.99). Further, low-income families had nearly 10-fold higher odds of experiencing catastrophic financial burden from out-of-pocket heath costs (1.1% vs 11.1%; OR, 10.78; 95% CI, 8.72-13.33). This represents a mean of 1.8 million low-income and 878 000 mid/high–income families with high financial burden, and 825 000 low-income and 144 000 mid/high–income families with catastrophic financial burden, respectively, each year. After accounting for differences in patient and family characteristics, low-income families had 8-fold higher odds for high financial burden (risk-adjusted OR, 8.32; 95% CI, 7.20-9.60) and 16-fold higher odds of catastrophic burden from health expenses (risk-adjusted OR, 16.84; 95% CI, 13.08-20.69).
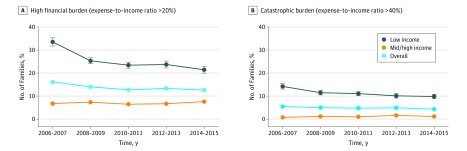
Between 2006/2007 and 2014/2015, rates of high financial burden decreased from 16.2% (95% CI, 14.6%-17.7%) to 12.7% (95% CI, 11.1%-14.3%), and catastrophic burden decreased from 5.5% (95% CI, 4.6%-6.3%) to 4.3% (95% CI, 3.5%-5.2%) (P for trend <.001 for both). There was a 30% reduction in high financial burden in low-income families (33.5% [95% CI, 30%-37%] to 21.4% [95% CI, 18.6%-24.2%]), while the rates in mid/high–income families increased by a relative 12% (6.8% [95% CI, 5.4%-8.1%] to 7.6% [95% CI, 6.0%-9.2%]; P for trend <.001 for both, P for interaction <.001 [year × income group]) (Figure 1). In 2014 and 2015, low-income families still had 3-fold higher odds of high financial burden relative to mid/high–income families (OR, 3.31; 95% CI, 2.55-4.31). Similarly, catastrophic burden decreased only in low-income families (14.2% [95% CI, 11.9%-16.5%] to 9.8% [95% CI, 7.8%-11.8%]), and their rates were still 9-fold higher than high-income families in 2014 and 2015 (OR for low- vs mid/high–income, 9.35; 95% CI, 5.39-16.20; P for interaction<.001 [year × income group]) (Figure 1).
Figure 1. Trends in Rates of High and Catastrophic Financial Burden From Out-of-Pocket Health Expenditures by Income Group.
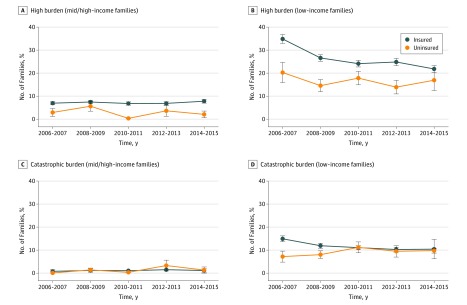
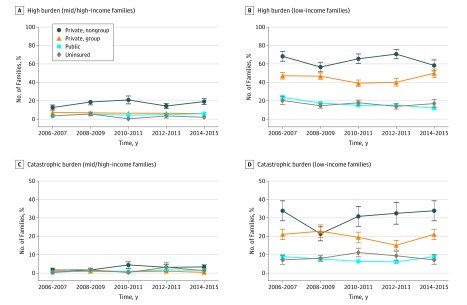
Among low-income families that incurred a catastrophic financial burden from health care costs, most of their health care expenses were spent on members with ASCVD (eFigure 4 in the Supplement). Further, families with either catastrophic or high burden from health care expenses, insurance premiums, prescription medications, and ancillary care services, including home health care, represented the major categories of spending (eFigure 5 in the Supplement). Moreover, rates of high financial burden were higher in those with health insurance (Figure 2) but varied substantially by insurance type (eFigure 6 in the Supplement). Despite improvements during the study, in 2014 and 2015, 1.6 million low-income families (21.8%) with insurance experienced high financial burden, and 721 000 (9.8%) experienced catastrophic burden. This risk was highest in those insured by nongroup private insurance (high burden, 58.4% and catastrophic burden, 26.3%, representing an estimated 442 000 and 199 000 of 758 000 families, respectively, with nongroup private insurance), compared with either group-based private insurance (high burden, 49.8% and catastrophic burden, 23.5%, representing an estimated 491 000 and 232 000 of 986 000 families, respectively, with group-based private insurance) or public insurance (high burden, 12.0% and catastrophic burden, 5.2%, representing 675 000 and 290 000 of 5.6 million families with public insurance, respectively) (Rao-Scott χ2 = 155.5 for high burden; Rao-Scott χ2 = 59.5 for catastrophic burden; P < .001 for all) (Figure 3). The association between insurance groups and financial outcomes was consistent in risk-adjusted analyses, with the highest odds of catastrophic expenses among those covered with nongroup private insurance (eFigure 7 in the Supplement). The association between income as well as insurance groups and catastrophic expenses was consistent in sensitivity analyses that additionally accounted for characteristics and health expenses of family members without ASCVD (eFigure 8 and eTable 2 in the Supplement).
Figure 2. Trends in Rates of High and Catastrophic Financial Burden From Out-of-Pocket Health Expenditures by Access to Insurance.
Figure 3. Trends in Rates of High and Catastrophic Financial Burden From Out-of-Pocket Health Expenditures by Insurance Group.
In additional sensitivity analyses that included families with very low incomes who would have substantial financial burden from any health care expenses, there was an even higher burden of financial burden from health care expenses (eResults and eFigures 9 to 12 in the Supplement).
Discussion
One in 4 low-income families that included a member with ASCVD experienced a high financial burden, and 1 in 10 experienced a catastrophic financial burden owing to cumulative out-of-pocket health care expenses, representing nearly 2 million low-income US families each year. Although financial hardship from out-of-pocket health care expenses decreased for low-income families over the last decade, even in the contemporary era, low-income families remain at 3-fold higher odds of high financial burden and 9-fold higher odds of catastrophic financial burden than mid/high–income families. Moreover, even low-income families with health insurance are not sufficiently protected, as in recent years, a third of low-income families with either self-purchased or employment-based private insurance coverage still faced a catastrophic expense from out-of-pocket longitudinal health care costs.
Our study contributes to the national debate on health care coverage in several ways. While health care expenses are the leading cause of bankruptcy in the United States,30 health policy interventions have thus far mainly focused on expanding access to health insurance.4 Our study suggests that even among those with insurance coverage, there is a substantial financial impact of out-of-pocket health expenses for families with members needing chronic cardiovascular care, indicating underinsurance. A similar high burden of out-of-pocket health expenses has previously been suggested for those seeking care for cancer19,31 and for patients with diabetes and hypertension.22,23 The adverse financial and health implications of inadequate protection from health care costs among those with insurance has also been shown.32,33 However, these studies predated the implementation of the Affordable Care Act, were limited to specific populations, and/or did not specifically assess individuals with ASCVD. Our nationally representative study throughout a 10-year period spanning major health care reform suggests that while the financial burden among low-income patients with ASCVD has improved throughout the last decade, such individuals and their families remain at a much higher risk for financial hardship from out-of-pocket health care expenses. Further, our study specifically found that expenses frequently exceed thresholds that portend a risk for bankruptcy and financial ruin for families.24,27
The study also offers insights into specific expenses that impose the highest burden for low-income families. The 2 largest categories of spending are insurance premiums and medications, consistent with studies for other conditions.6,19,22 These expenses are particularly high among those covered with self-purchased private insurance. Under these insurance programs, patients are more likely to bear out-of-pocket costs for services that are usually subsidized by employers and manifest as high insurance premiums, as well as high deductible expenses and coinsurance payments for most health care services.19,20,34
Our findings have certain potential implications. Although provisions in recent health care reforms that set upper limits on out-of-pocket payments have been associated with improvements in total spending,6 these limits do not reflect the financial capacity of low-income families facing costs of care for chronic disease.35 Our findings highlight that high insurance premiums and out-of-pocket spending on prescription medications represent potential targets for health policy interventions with the goal of reducing financial hardship from health care costs. Until high health care expenses are addressed, use of health care services will likely impede the financial stability and upward mobility of low-income families.33,36,37 Moreover, patients and their families will continue to be at risk for negative health consequences from major financial hardship.32,38,39,40,41 Therefore, a better understanding of the financial burden of health care costs in low-income families with chronic health care needs, a financially vulnerable population, is critical before implementing any insurance reform.
A seemingly counterintuitive observation is that low-income families with insurance coverage had high rates of adverse financial outcomes that exceeded those without insurance. These differences persisted despite accounting for differences in patient and family characteristics, which suggests that the lower rates of financial hardship in uninsured low-income individuals might represent deferred health care, similar to observations in prior studies.32,42 Alternatively, uninsured patients with major health care needs may purchase insurance in anticipation of major expenses.43 By extension, those without insurance may overly represent those without active care needs. Finally, it remains unclear whether in the group with insurance coverage, access to insurance is associated with overuse of health care services. Therefore, an understanding of how access to and lack of health insurance in low-income individuals with ASCVD affects their care-seeking behavior merits dedicated investigation.
Limitations
The study should be interpreted in light of the following limitations. First, the diagnosis of ASCVD was not independently verified with medical records. However, MEPS uses a network of trained interviewers who encourage participants to share objective information11 such as medical records, if possible. Similarly, cost information is frequently compiled by MEPS interviewers with information from bills for various health care services availed by participants. Moreover, both our study population with ASCVD and our exposure of cost and family income are based on the approach used by several prior studies.6,12,19,22 Second, while MEPS includes income from diverse sources, including pension funds and retirement accounts,44 we do not specifically address access to financial savings or other assets that may help avert the financial consequences of high out-of-pocket health care costs. Third, differences in out-of-pocket expenses across groups may not represent differences in insurance coverage alone and may also be affected by the care they sought. We cannot account for differences in care-seeking behaviors between different patient groups that may underlie some of the observed differences. Further, while we assessed for confounding by disease severity using a combination of comorbidities, given the lack of detailed clinical information, there is likely to be residual confounding in the assessment of risk-adjusted differences between groups. However, our assessment of the overall financial impact of ASCVD on families does not rely on this information.
Fourth, we used an approach in which health care expenses were compared against income after accounting for subsistence expenses, which would reflect as financial adversity for a larger number of families, compared with using an approach that compares expenses and income directly. However, our approach is more consistent with the assessment of health care–related financial burden endorsed by the World Health Organization,24,27 as it specifically accounts for financial priorities in low-income families. Further, while such high health care expenses may portend financial ruin, it is unclear what proportion actually experience major adverse financial outcomes from longitudinal health care costs. This is germane because even single hospitalization events are associated with a modest increase in rates of bankruptcy.45 Whether bankruptcy provisions in the United States help avert major health care costs, as has been suggested previously,46 merits additional investigation. Finally, the current study focuses on annual health care expenses. Owing to the lack of longitudinal family follow-up, we are unable to evaluate if these costs represent excessive spending in a particular year or represent chronic financial hardship. Given the chronicity of ASCVD and the observation that high spending is driven by costs of insurance premiums and prescription medications, as opposed to hospitalization events, it is likely that health care costs would pose a cumulative burden over the lifetime of a patient.
Conclusions
Despite decreasing out-of-pocket expenses over the last decade, nearly 2 million low-income US families that have a member with ASCVD, including those with insurance, have annual out-of-pocket health care costs that far exceed their means and put them at risk for financial catastrophe each year. Alleviating economic disparities resulting from health care costs requires that policy interventions extend their focus to improving the quality and extent of coverage for low-income families.
eResults. Sensitivity analyses
eFigure 1. Proportion of low-income and mid/high-income families with a member with atherosclerotic cardiovascular disease
eFigure 2. Median family income by calendar-year in the mid/high-income and low-income families
eFigure 3. Mean out-of-pocket expenses across categories of healthcare, by family income group
eFigure 4. Mean healthcare expenses in low-income families incurring a catastrophic financial burden from out-of-pocket health costs (A), and relative spending on member with ASCVD among these families (B)
eFigure 5. Mean healthcare expenses across categories in low-income families
eFigure 6. Trends in overall rates of high and catastrophic financial burden from out-of-pocket health expenditures, by insurance group
eFigure 7. Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families
eFigure 8. Sensitivity analysis: Risk-adjusted odds ratio for high and catastrophic financial burden from out-of-pocket health expenses in low vs mid/high income families after adjusting for characteristics of members without atherosclerotic cardiovascular disease
eFigure 9. Sensitivity analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by income group
eFigure 10. Sensitivity Analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by access to insurance
eFigure 11. Sensitivity Analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by insurance group
eFigure 12. Sensitivity Analysis: Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families
eTable 1. Proportional out-of-pocket spending on different categories of healthcare services, by income group
eTable 2. Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families
References
- 1.Khera R, Hong JC, Saxena A, et al. . Burden of catastrophic health expenditures for acute myocardial infarction and stroke among uninsured in the United States. Circulation. 2018;137(4):408-410. doi: 10.1161/CIRCULATIONAHA.117.030128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Blaha MJ, Chiuve SE, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith SC Jr, Benjamin EJ, Bonow RO, et al. ; World Heart Federation and the Preventive Cardiovascular Nurses Association . AHA/ACCF Secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458-2473. doi: 10.1161/CIR.0b013e318235eb4d [DOI] [PubMed] [Google Scholar]
- 4.Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316(5):525-532. doi: 10.1001/jama.2016.9797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manchikanti L, Helm Ii S, Benyamin RM, Hirsch JA. A critical analysis of Obamacare: affordable care or insurance for many and coverage for few? Pain Physician. 2017;20(3):111-138. [PubMed] [Google Scholar]
- 6.Goldman AL, Woolhandler S, Himmelstein DU, Bor DH, McCormick D. Out-of-pocket spending and premium contributions after implementation of the Affordable Care Act. JAMA Intern Med. 2018;178(3):347-355. doi: 10.1001/jamainternmed.2017.8060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Claxton G, Rae M, Long M, Damico A, Whitmore H, Foster G. Health benefits in 2016: family premiums rose modestly, and offer rates remained stable. Health Aff (Millwood). 2016;35(10):1908-1917. doi: 10.1377/hlthaff.2016.0951 [DOI] [PubMed] [Google Scholar]
- 8.Collins SR, Rasmussen PW, Beutel S, Doty MM. The problem of underinsurance and how rising deductibles will make it worse: findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014. Issue Brief (Commonw Fund). 2015;13:1-20. [PubMed] [Google Scholar]
- 9.HealthCare.gov Out-of-pocket maximum/limit. https://www.healthcare.gov/glossary/out-of-pocket-maximum-limit. Accessed February 14, 2018.
- 10.Centers for Medicare and Medicaid Services Fact Sheet: Short-Term, Limited-Duration Insurance Proposed Rule. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2018-Fact-sheets-items/2018-02-20.html. Accessed February 20, 2018.
- 11.Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7)(suppl 1):S44-S50. doi: 10.1097/MLR.0b013e3181a23e3a [DOI] [PubMed] [Google Scholar]
- 12.Salami JA, Valero-Elizondo J, Ogunmoroti O, et al. . Association between modifiable risk factors and pharmaceutical expenditures among adults with atherosclerotic cardiovascular disease in the United States: 2012-2013 Medical Expenditures Panel Survey. J Am Heart Assoc. 2017;6(6):e004996. doi: 10.1161/JAHA.116.004996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grotto I, Grossman E, Huerta M, Sharabi Y. Prevalence of prehypertension and associated cardiovascular risk profiles among young Israeli adults. Hypertension. 2006;48(2):254-259. doi: 10.1161/01.HYP.0000227507.69230.fc [DOI] [PubMed] [Google Scholar]
- 14.Auter Z. Healthcare Costs Top US Families' Financial Concerns. http://news.gallup.com/poll/191126/healthcare-costs-top-families-financial-concerns.aspx. Published April 27, 2016. Accessed February 12, 2018.
- 15.Emanuel EJ, Glickman A, Johnson D. Measuring the burden of health care costs on US families: the affordability index. JAMA. 2017;318(19):1863-1864. doi: 10.1001/jama.2017.15686 [DOI] [PubMed] [Google Scholar]
- 16.United States Census Bureau Current Population Survey (CPS) - Subject Definitions. https://www.census.gov/programs-surveys/cps/technical-documentation/subject-definitions.html#family. Accessed February 10, 2018.
- 17.Roberts B, Povich D, Mather M. Low-Income Working Families: The Growing Economic Gap. The Working Poor Families Project; 2013. [Google Scholar]
- 18.Dubay L, Kenney GM. Health care access and use among low-income children: who fares best? Health Aff (Millwood). 2001;20(1):112-121. doi: 10.1377/hlthaff.20.1.112 [DOI] [PubMed] [Google Scholar]
- 19.Bernard DS, Farr SL, Fang Z. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol. 2011;29(20):2821-2826. doi: 10.1200/JCO.2010.33.0522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Banthin JS, Cunningham P, Bernard DM. Financial burden of health care, 2001-2004. Health Aff (Millwood). 2008;27(1):188-195. doi: 10.1377/hlthaff.27.1.188 [DOI] [PubMed] [Google Scholar]
- 21.Agency for Healthcare Research and Quality Medical Expenditure Panel Survey (MEPS): MEPS HC-181: 2015 Full Year Consolidated Data File. https://meps.ahrq.gov/data_stats/download_data/pufs/h181/h181doc.shtml. Accessed May 1, 2018.
- 22.Li R, Barker LE, Shrestha S, et al. . Changes over time in high out-of-pocket health care burden in U.S. adults with diabetes, 2001-2011. Diabetes Care. 2014;37(6):1629-1635. doi: 10.2337/dc13-1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fang J, Zhao G, Wang G, Ayala C, Loustalot F. Insurance status among adults with hypertension-the impact of underinsurance. J Am Heart Assoc. 2016;5(12):e004313. doi: 10.1161/JAHA.116.004313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111-117. doi: 10.1016/S0140-6736(03)13861-5 [DOI] [PubMed] [Google Scholar]
- 25.Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014;11(9):e1001701. doi: 10.1371/journal.pmed.1001701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shrime MG, Dare A, Alkire BC, Meara JG. A global country-level comparison of the financial burden of surgery. Br J Surg. 2016;103(11):1453-1461. doi: 10.1002/bjs.10249 [DOI] [PubMed] [Google Scholar]
- 27.Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(suppl 2):S38-S44. doi: 10.1016/S2214-109X(15)70085-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khera R, Angraal S, Couch T, et al. . Adherence to methodological standards in research using the national inpatient sample. JAMA. 2017;318(20):2011-2018. doi: 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khera R, Krumholz HM. With great power comes great responsibility: big data research from the national inpatient sample. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003846. doi: 10.1161/CIRCOUTCOMES.117.003846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741-746. doi: 10.1016/j.amjmed.2009.04.012 [DOI] [PubMed] [Google Scholar]
- 31.Chino F, Peppercorn JM, Rushing C, et al. . Out-of-pocket costs, financial distress, and underinsurance in cancer care. JAMA Oncol. 2017;3(11):1582-1584. doi: 10.1001/jamaoncol.2017.2148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297(10):1063-1072. doi: 10.1001/jama.297.10.1063 [DOI] [PubMed] [Google Scholar]
- 33.Dumont D, Cooper T, Jiang Y. Uninsurance is only half the problem: underinsurance and healthcare-related financial burden in RI. R I Med J (2013). 2014;98(4):46-49. [PubMed] [Google Scholar]
- 34.Magge H, Cabral HJ, Kazis LE, Sommers BD. Prevalence and predictors of underinsurance among low-income adults. J Gen Intern Med. 2013;28(9):1136-1142. doi: 10.1007/s11606-013-2354-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riggs KR, Buttorff C, Alexander GC. Impact of out-of-pocket spending caps on financial burden of those with group health insurance. J Gen Intern Med. 2015;30(5):683-688. doi: 10.1007/s11606-014-3127-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lenzer J. Underinsurance threatens physical and financial wellbeing of US families. BMJ. 2008;336(7658):1399. doi: 10.1136/bmj.a419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woolhandler S, Himmelstein DU. Life or debt: underinsurance in America. J Gen Intern Med. 2013;28(9):1122-1124. doi: 10.1007/s11606-013-2460-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kalousova L, Burgard SA. Unemployment, measured and perceived decline of economic resources: contrasting three measures of recessionary hardships and their implications for adopting negative health behaviors. Soc Sci Med. 2014;106:28-34. doi: 10.1016/j.socscimed.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 39.Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a negative wealth shock with all-cause mortality in middle-aged and older adults in the United States. JAMA. 2018;319(13):1341-1350. doi: 10.1001/jama.2018.2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boen C, Yang YC. The physiological impacts of wealth shocks in late life: evidence from the Great Recession. Soc Sci Med. 2016;150:221-230. doi: 10.1016/j.socscimed.2015.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pool LR, Needham BL, Burgard SA, Elliott MR, de Leon CFM. Negative wealth shock and short-term changes in depressive symptoms and medication adherence among late middle-aged adults. J Epidemiol Community Health. 2017;71(8):758-763. doi: 10.1136/jech-2016-208347 [DOI] [PubMed] [Google Scholar]
- 42.Mallow JA, Theeke LA, Barnes ER, Whetsel T, Mallow BK. Free care is not enough: barriers to attending free clinic visits in a sample of uninsured individuals with diabetes. Open J Nurs. 2014;4(13):912-919. doi: 10.4236/ojn.2014.413097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diamond R, Dickstein MJ, McQuade T, Persson P Take-up, drop-out, and spending in ACA marketplaces. Proceedings of the 7th Conference of the American Society of Health Economics. https://ashecon.confex.com/ashecon/2018/webprogram/Paper5529.html. Accessed May 23, 2018.
- 44.Banthin JS, Selden TM Income Measurement in the Medical Expenditure Panel Survey. https://meps.ahrq.gov/data_files/publications/workingpapers/wp_06005.pdf. Accessed May 1, 2018.
- 45.Dobkin C, Finkelstein A, Kluender R, Notowidigdo MJ. Myth and measurement: the case of medical bankruptcies. N Engl J Med. 2018;378(12):1076-1078. doi: 10.1056/NEJMp1716604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mahoney N. Bankruptcy as implicit health insurance. Am Econ Rev. 2015;105(2):710-746. doi: 10.1257/aer.20131408 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eResults. Sensitivity analyses
eFigure 1. Proportion of low-income and mid/high-income families with a member with atherosclerotic cardiovascular disease
eFigure 2. Median family income by calendar-year in the mid/high-income and low-income families
eFigure 3. Mean out-of-pocket expenses across categories of healthcare, by family income group
eFigure 4. Mean healthcare expenses in low-income families incurring a catastrophic financial burden from out-of-pocket health costs (A), and relative spending on member with ASCVD among these families (B)
eFigure 5. Mean healthcare expenses across categories in low-income families
eFigure 6. Trends in overall rates of high and catastrophic financial burden from out-of-pocket health expenditures, by insurance group
eFigure 7. Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families
eFigure 8. Sensitivity analysis: Risk-adjusted odds ratio for high and catastrophic financial burden from out-of-pocket health expenses in low vs mid/high income families after adjusting for characteristics of members without atherosclerotic cardiovascular disease
eFigure 9. Sensitivity analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by income group
eFigure 10. Sensitivity Analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by access to insurance
eFigure 11. Sensitivity Analysis: Trends in rates of high and catastrophic financial burden from out-of-pocket health expenditures, by insurance group
eFigure 12. Sensitivity Analysis: Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families
eTable 1. Proportional out-of-pocket spending on different categories of healthcare services, by income group
eTable 2. Predictors for catastrophic financial burden from out-of-pocket health expenditures in low-income families