Key Points
Question
What are the causes and risks of mortality in the 12 months after nonfatal opioid overdose?
Findings
In this US national longitudinal study, during the first 12 months after opioid overdose, common causes of death included substance use–associated diseases, circulatory diseases, and cancer. Compared with the demographically matched general population, standardized mortality rate ratios were 24.2 for all-cause mortality, 132.1 for drug use–associated diseases, 45.9 for HIV, 41.1 for chronic respiratory diseases, 30.9 for viral hepatitis, and 25.9 for suicide.
Meaning
The high and broadly distributed mortality risks after nonfatal opioid overdose underscore the importance of coordinating medical, substance use, and mental health management after opioid overdose.
This national longitudinal cohort study of US adults who had experienced a nonfatal opioid overdose determines rates of all-cause and cause-specific mortality and standardized mortality rate ratios in the first year after the overdose.
Abstract
Importance
A recent increase in patients presenting with nonfatal opioid overdoses has focused clinical attention on characterizing their risks of premature mortality.
Objective
To describe all-cause mortality rates, selected cause-specific mortality rates, and standardized mortality rate ratios (SMRs) of adults during their first year after nonfatal opioid overdose.
Design, Setting, and Participants
This US national longitudinal study assesses a cohort of patients aged 18 to 64 years who were Medicaid beneficiaries and experienced nonfatal opioid overdoses. The Medicaid data set included the years 2001 through 2007. Death record information was obtained from the National Death Index. Data analysis occurred from October 2017 to January 2018.
Main Outcomes and Measures
Crude mortality rates per 100 000 person-years were determined in the first year after nonfatal opioid overdose. Standardized mortality rate ratios (SMR) were estimated for all-cause and selected cause-specific mortality standardized to the general population with respect to age, sex, and race/ethnicity.
Results
The primary cohort included 76 325 adults and 66 736 person-years of follow-up. During the first year after nonfatal opioid overdose, there were 5194 deaths, the crude death rate was 778.3 per 10 000 person-years, and the all-cause SMR was 24.2 (95% CI, 23.6-24.9). The most common immediate causes of death were substance use–associated diseases (26.2%), diseases of the circulatory system (13.2%), and cancer (10.3%). For every cause examined, SMRs were significantly elevated, especially with respect to drug use–associated diseases (SMR, 132.1; 95% CI, 125.6-140.0), HIV (SMR, 45.9; 95% CI, 39.5-53.0), chronic respiratory diseases (SMR, 41.1; 95% CI, 36.0-46.8), viral hepatitis (SMR, 30.6; 95% CI, 22.9-40.2), and suicide (SMR, 25.9; 95% CI, 22.6-29.6), particularly including suicide among females (SMR, 47.9; 95% CI, 39.8-52.3).
Conclusions and Relevance
In a US national cohort of adults who had experienced a nonfatal opioid overdose, a marked excess of deaths was attributable to a wide range of substance use–associated, mental health, and medical conditions, underscoring the importance of closely coordinating the substance use, mental health, and medical care of this patient population.
Introduction
There has been a recent substantial national increase in opioid-associated emergency department visits and hospital admissions. Between 2005 and 2014, opioid-associated emergency department visits in the United States approximately doubled on a per capita basis, while opioid-associated inpatient stays increased by nearly two-thirds.1 A portion of these episodes of health care utilization are associated with nonfatal overdoses. As the number of patients with nonfatal opioid overdoses has increased, there is heightened clinical interest in characterizing their subsequent risk of death, not only resulting from overdoses but also from other causes. An increased understanding of these risks could inform efforts to provide preventive and potentially lifesaving medical care after nonfatal opioid overdose and to better integrate general medical care with the treatment of opioid use disorders.
Dependent use of opioids is associated with an elevated risk of premature mortality.2 According to a meta-analysis, the annual risk of death is nearly 15 times higher among regular and dependent opioid users in treatment than among their demographically matched peers.3 Overdose is the most common cause of death among nonelderly adult opioid users.2,3,4,5 Some other causes of excess mortality in this population include suicide,6 unintentional injuries,4 liver diseases,4,7,8 AIDS-related illnesses,3,7 and cancer.4,9 The relative magnitude of these risks varies by study design and patient population.
In contrast with the fairly extensive literature on mortality risks among outpatients under care for dependent opioid use, much less is known about risks of dying after nonfatal opioid overdose. Among a cohort of opioid-using patients in Austria who experienced a total of 2108 nonfatal opioid overdoses while receiving maintenance treatment, the all-cause mortality rate was 52.6 per 1000 person-years during a mean of 0.8 years of follow-up time. In that study,10 nearly all of these deaths (61 of 69; 88.4%) involved intoxication with illicit substances or alcohol. In a second cohort of 4884 nonfatal heroin overdoses in Melbourne, Australia, the subsequent rate of drug overdose death was 12.0 per 1000 person-years during a mean follow-up time of 2.2 years.11 Beyond high rates of overall mortality and high rates of fatal drug overdose, however, the magnitude and sources of excess mortality after nonfatal opioid overdose is unknown.
To help fill this gap in our understanding of the opioid overdose problem in the United States, we examined causes of death in a large cohort of nonelderly adults who were enrolled in the Medicaid program during their first year after nonfatal opioid overdose. Mortality rates and mortality ratios standardized to the general population by sex, age, and race/ethnicity were used to describe excess mortality from several common causes of death. By characterizing sources of excess death, we sought to identify potentially avoidable causes and opportunities for prevention through integration of general medical, mental health, and addiction services. We anticipated that in addition to an excess of drug use–associated deaths, there would also be an excess of suicide6 and homicide12 consistent with findings in general patient populations with dependent opioid users. For similar reasons, we further anticipated that risks of death from HIV, liver disease, and cancer would be increased among patients after nonfatal opioid overdose.
Methods
Sources of Data
An opioid overdose cohort was extracted from national Medicaid Analytic Extract (MAX) data from the US Centers for Medicare and Medicaid Services. The data set included 45 states (excluding Arizona, Delaware, Nevada, Oregon, and Rhode Island) and covered the calendar years 2001 through 2007. MAX data provide information on enrollment as well as inpatient, emergency, and outpatient use of Medicaid beneficiaries. Dates and cause of death information were derived from linkage to the National Death Index, which provides a complete accounting of state-recorded deaths in the United States and is the most complete resource for tracing mortality in national samples.13 The US Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (WONDER) Underlying Cause of Death data set contains detailed annual mortality and population counts for all counties in the United States. WONDER data were used to generate age, sex, and race/ethnicity–matched mortality rates for each of the selected causes of death.14
This study was reviewed and approved by the Centers for Medicare and Medicaid Services and the Rutgers University institutional review board. Because the data were deidentified, informed consent was not required.
Assembly of Nonfatal Opioid Overdose Cohort
The cohort was restricted to adults aged 18 to 64 years who were eligible for Medicaid services during the 180 days preceding relevant opioid poisoning codes drawn from the International Statistical Classification of Diseases and Related Health Problems, Ninth Revision (ICD-9) (965.00-965.09, E850.0, E850.1, and E850.2),15 which include heroin and pharmaceutical overdoses. These codes capture opioid poisonings known to be unintentional and those without specified intent. The 180-day enrollment requirement provides a period in which to calculate the Elixhauser Comorbidity Index. The Elixhauser Comorbidity Index is a claims-based scale with good predictive validity of short-term mortality.16
When adults turn 65 years old, they become Medicare eligible, and their Medicaid claims records do not capture services that are entirely paid for by Medicare. For this reason, adults 65 years and older were not included in this analysis.
The first eligible nonfatal overdose was selected, and no patient contributed more than 1 observation to the cohort. First eligible overdoses that were fatal (n = 165) were excluded from the cohort. Fatal overdoses were defined as deaths resulting from opioid-associated causes (ICD-10 codes T40.0, T40.1, T40.2, T40.3, T40.4, or T40.6) on the date of opioid overdoses treated in outpatient settings or the discharge date of opioid overdoses treated in emergency department or inpatient settings. The cohort was followed up from their index date for 365 days, to the date of death from any cause, or to the end of 2007, whichever came first.
Causes of Mortality
In addition to all-cause mortality, the analysis focused on selected immediate causes of death that have been reported as elevated in analyses of adults with opioid use disorder.2 These included external causes (suicide, homicide, and unintentional injuries) excluding substance use–associated causes; causes associated with substance abuse (both drug use associated and alcohol use associated); infectious diseases overall as well as specific viral infections (hepatitis and HIV); diseases of the circulatory system; respiratory diseases overall, as well as influenza, pneumonia, and chronic respiratory diseases; digestive system diseases overall, as well as cirrhosis and alcohol liver disease; and cancers (eAppendix 1 in the Supplement).
Demographic and Clinical Characteristics
Based on Medicaid eligibility data, cohort members were classified by sex, age group (18-34, 35-44, or 45-64 years), and race/ethnicity (Hispanic; non-Hispanic white; non-Hispanic black; and non-Hispanic other, which included American Indian/Alaskan Native, Asian, Native Hawaiian/other Pacific Islander, and persons reporting more than 1 race). A separate variable counted the occurrence of 1 or more inpatient or outpatient diagnoses from the 31 conditions in the Elixhauser Comorbidity Index in the 180 days prior to the index nonfatal opioid overdose (eAppendix 2 in the Supplement).17
Analysis
From the nonfatal opioid overdose cohort, the number of observed deaths, person-years of follow-up, mortality rates per 10 000 person-years, expected deaths, and standardized mortality rate ratios were determined overall and stratified by demographic characteristics. For each selected cause, observed deaths, mortality rates, expected deaths, and SMRs were also calculated for the entire nonfatal opioid overdose cohort and stratified by sex. To help define the contribution of preexisting serious general medical illnesses to short-term mortality, separate analyses were performed with overdose patients with Elixhauser Comorbidity Index scores of either 0 (low) and 1 or higher (medium or high).
The SMRs were defined as the ratio of observed number of deaths in the nonfatal opioid overdose cohort to expected deaths. The number of expected deaths was calculated for a cohort of the size of the overdose cohort from the Centers for Disease Control and Prevention WONDER mortality data standardized by age, sex, and race/ethnicity. Kaplan-Meier curves of all-cause mortality were constructed by sex, and comparisons were assessed with the log-rank test. For the tabulated data, groups with nonoverlapping 95% CIs for SMRs were considered significantly different from each other. In this large exploratory study, no adjustments were made for the multiple comparisons. The significance of nonoverlapping CIs should therefore be interpreted with caution. All statistical analyses were performed with SAS version 9.4 (SAS Institute). Data analysis occurred from October 2017 to January 2018.
Results
All-Cause Mortality
The nonfatal opioid overdose cohort included 76 325 individuals, 66 736 person-years of follow-up, and 5194 deaths within 1 year (Table 1). The overall all-cause mortality rate for adults after opioid overdose was 778.3 per 10 000 person-years, which indicated a death rate more than 20 times higher than age, sex, and race/ethnicity–matched community controls (SMR, 24.2 [95% CI, 23.6-24.9]). The all-cause SMR was particularly elevated for young adults aged 18 to 34 years (SMR, 39.1 [95% CI, 36.3-42.1]). All-cause SMRs were significantly higher for women than men (women: SMR, 27.3 [95% CI, 26.3-28.3] vs men: SMR, 21.7 [95% CI, 20.9-22.6]) and were significantly higher for patients who were of white or Hispanic race/ethnicity than patients who were of black race/ethnicity (white: SMR, 28.6 [95% CI, 27.7-29.6] vs Hispanic: SMR, 24.9 [95% CI, 22.0-28.0] vs black: SMR, 13.1 [95% CI, 12.3-14.0]; Table 1).
Table 1. All Causes of Death and Crude Mortality Rates for Adult Medicaid Patients During the First 12 Months After Nonfatal Opioid Overdose, Overall and Stratified by Demographic Characteristics.
| Demographic Groups | Total Opioid Overdoses (N = 76 325) | Deaths, No. | Person-Years of Follow-up | Crude Mortality Rate per 10 000 Person-Years | Expected Deaths, No.a | Standardized Mortality Rate Ratio (95% CI)a |
|---|---|---|---|---|---|---|
| Total sample | 76 325 | 5194 | 66 736 | 778.3 | 214.6 | 24.2 (23.6-24.9) |
| Age, y | ||||||
| 18-34 | 22 596 | 692 | 20 257 | 341.6 | 17.7 | 39.1 (36.3-42.1) |
| 35-44 | 21 620 | 1299 | 19 322 | 672.3 | 38.8 | 33.5 (31.7-35.3) |
| 45-64 | 32 109 | 3203 | 27 157 | 1179.5 | 154.5 | 20.7 (20.0-21.5) |
| Sex | ||||||
| Male | 31 232 | 2547 | 27 107 | 939.6 | 117.2 | 21.7 (20.9-22.6) |
| Female | 45 093 | 2647 | 39 629 | 667.9 | 97.0 | 27.3 (26.3-28.3) |
| Race/Ethnicity | ||||||
| Hispanic | 5859 | 266 | 5212 | 510.3 | 10.7 | 24.9 (22.0-28.0) |
| White, non-Hispanic | 52 962 | 3756 | 46 130 | 814.2 | 131.2 | 28.6 (27.7-29.6) |
| Black, non-Hispanic | 13 147 | 884 | 11 575 | 763.7 | 67.3 | 13.1 (12.3-14.0) |
| Other, non-Hispanicb | 2452 | 105 | 2189 | 479.7 | 5.8 | 18.0 (14.9-21.8) |
Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research data with age, sex, and race/ethnicity standardized to nonfatal opioid overdose cohort.
Includes American Indian/Alaskan Native, Asian, Native Hawaiian/Other Pacific Islander, and persons who reported more than 1 race.
Selected Causes of Mortality in Overall Cohort
In the overall cohort, substance use–associated diseases accounted for approximately one-quarter of deaths (n = 1363; 26.2%) and were followed numerically by diseases of the circulatory system (n = 689; 13.2%) and cancer (n = 536; 10.3%) (Table 2). For each cause of death examined, the SMR was significantly greater than the standardized reference population. As expected, the SMR for drug use–associated deaths (132.1 [95% CI, 125.6-140.0]) exceeded all other causes of death. Other causes of death with particularly elevated SMRs included HIV (45.9 [95% CI, 39.5-53.0]), chronic respiratory disease (41.1 [95% CI, 36.0-46.8]), viral hepatitis (30.6 [95% CI, 22.9-40.2]), and suicide (25.9 [95% CI, 22.6-29.6]).
Table 2. Selected Cause-Specific Crude Mortality Rates for Adult Medicaid Patients During the First Year After a Nonfatal Opioid Overdose.
| Cause of Death | Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Expected Deaths, No.a | Standardized Mortality Rate Ratio (95% CI)a |
|---|---|---|---|---|
| All causes | 5194 | 778.3 | 214.6 | 24.2 (23.6-24.9) |
| External causes | 348 (6.7) | 52.1 | 27.7 | 12.6 (11.3-13.9) |
| Suicide | 215 (4.2) | 32.2 | 8.3 | 25.9 (22.6-29.6) |
| Homicide | 24 (0.4) | 3.6 | 4.2 | 5.7 (3.7-8.4) |
| Unintentional injury | 109 (2.1) | 16.3 | 15.1 | 7.2 (6.0-8.7) |
| Substance use associated | 1363 (26.2) | 204.2 | 16.1 | 84.6 (80.2-89.2) |
| Drug use associated | 1300 (25.0) | 194.8 | 9.8 | 132.1 (125.6-140.0) |
| Alcohol use associated | 63 (1.2) | 9.4 | 6.3 | 10.0 (7.7-12.7) |
| Infectious | 314 (6.0) | 47.1 | 12.2 | 25.7 (23.0-28.7) |
| Viral hepatitis | 49 (0.9) | 7.3 | 1.6 | 30.6 (22.9-40.2) |
| HIV | 179 (3.4) | 26.8 | 3.9 | 45.9 (39.5-53.0) |
| Circulatory system | 689 (13.2) | 103.2 | 55.5 | 12.4 (11.5-13.4) |
| Respiratory system | 321 (6.2) | 48.1 | 10.2 | 31.5 (28.2-35.1) |
| Influenza and pneumonia | 53 (1.0) | 7.9 | 2.2 | 23.7 (18.2-31.3) |
| Chronic respiratory disease | 222 (4.3) | 33.3 | 5.4 | 41.1 (36.0-46.8) |
| Digestive system | 187 (3.6) | 28.0 | 11.9 | 15.7 (13.6-18.1) |
| Cirrhosis and alcoholic liver disease | 101 (1.9) | 15.1 | 6.5 | 15.5 (12.7-18.8) |
| Cancers | 536 (10.3) | 80.3 | 61.2 | 8.8 (8.0-9.5) |
Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research data with age, sex, and race/ethnicity standardized to nonfatal opioid overdose cohort (N = 76 325).
Patient Sex and Risks of Death
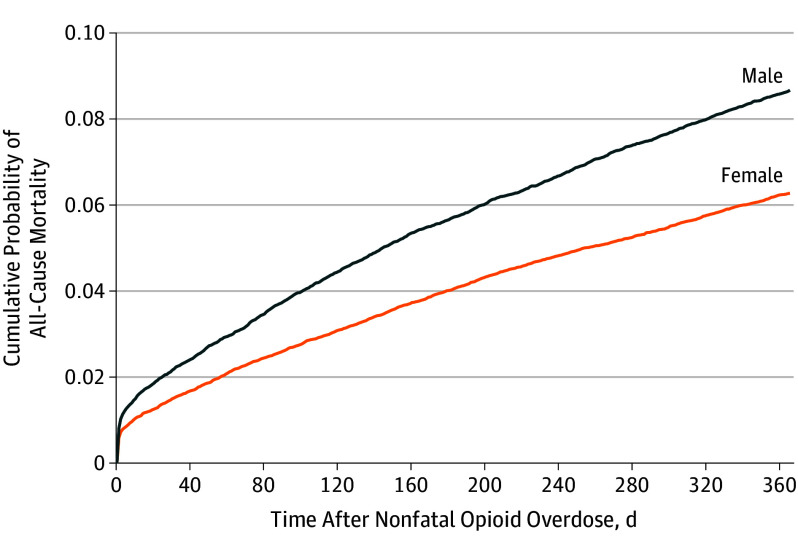
Despite all-cause SMR being higher for women than men, the cumulative risk of all-cause mortality was significantly higher for men than women (χ21 = 150.65; P < .001; Figure). This was because of the overall higher death rate in men in the general population. Among men and women, substance use–associated diseases were the most common cause of death, followed by diseases of the circulatory system (Table 3). The SMRs were significantly higher for women than men for several causes of death, including drug use–associated diseases (women: SMR, 153.4 [95% CI, 141.8-165.7] vs men: SMR, 115.7 [95% CI, 107.1-124.7]), suicide (women: SMR, 47.9 [95% CI, 39.8-52.3] vs men: SMR, 16.8 [95% CI, 13.7-20.3]), viral hepatitis (women: SMR, 49.8 [95% CI, 32.9-72.4] vs men: SMR, 21.4 [95% CI, 14.0-31.4]), HIV (women: SMR, 64.2 [95% CI, 50.4-80.6] vs men: SMR, 38.2 [95% CI, 31.6-46.0]), circulatory diseases (women: SMR, 17.7 [95% CI, 16.0-19.6] vs men: SMR, 9.1 [95% CI, 8.2-10.2]), and chronic respiratory diseases (women: SMR, 48.5 [95% CI, 41.1-56.9] vs men: SMR, 31.7 [95% CI, 25.2-39.4]).
Figure. Cumulative Probability of All-Cause Mortality During the 365 Days After a Nonfatal Opioid Overdose, Stratified by Sex.
Log-rank test, χ2 = 150.65; P < .001.
Table 3. All Causes and Selected Causes of Crude Mortality Rate Ratios and Standardized Mortality Ratios for Adult Medicaid Patients During the First Year After a Nonfatal Opioid Overdose, Stratified by Sex.
| Cause of Death | Men | Women | ||||
|---|---|---|---|---|---|---|
| Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Standardized Mortality Rate Ratio (95% CI)a | Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Standardized Mortality Rate Ratio (95% CI)a | |
| All causes | 2547 (100) | 939.6 | 21.7 (20.9-22.6) | 2647 (100) | 667.9 | 27.3 (26.3-28.3) |
| External causes | 180 (7.1) | 66.4 | 9.6 (8.2-11.0) | 168 (6.3) | 42.4 | 18.7 (16.0-21.6) |
| Suicide | 99 (3.9) | 36.5 | 16.8 (13.7-20.3) | 116 (4.3) | 29.3 | 47.9 (39.8-52.3) |
| Homicide | 19 (0.7) | 7.0 | 6.3 (3.9-9.7) | 5 (0.2) | 1.3 | 4.0 (1.5-8.9) |
| Unintentional injury | 62 (2.5) | 22.9 | 6.3 (4.9-8.1) | 47 (1.8) | 11.9 | 8.8 (6.5-11.6) |
| Substance use associated | 714 (28.0) | 263.4 | 70.7 (65.6-76.0) | 649 (24.5) | 163.8 | 106.9 (98.9-115.4) |
| Drug use associated | 665 (26.1) | 245.3 | 115.7 (107.1-124.7) | 635 (24.0) | 160.2 | 153.4 (141.8-165.7) |
| Alcohol use associated | 49 (1.9) | 18.1 | 11.1 (8.3-14.6) | 14 (0.5) | 3.5 | 7.2 (4.1-11.8) |
| Infectious | 170 (6.7) | 62.7 | 22.4 (19.2-25.9) | 144 (5.4) | 36.3 | 31.0 (26.2-36.4) |
| Viral hepatitis | 24 (0.9) | 8.9 | 21.4 (14.0-31.4) | 25 (0.9) | 6.3 | 49.8 (32.9-72.4) |
| HIV | 109 (4.3) | 40.2 | 38.2 (31.6-46.0) | 70 (2.6) | 17.7 | 64.2 (50.4-80.6) |
| Circulatory system | 318 (12.9) | 117.3 | 9.1 (8.2-10.2) | 371 (14.0) | 93.6 | 17.7 (16.0-19.6) |
| Respiratory system | 128 (5.0) | 47.2 | 26.1 (21.9-31.0) | 193 (7.3) | 48.7 | 36.0 (31.2-41.4) |
| Influenza and pneumonia | 29 (1.1) | 10.7 | 23.0 (15.7-32.6) | 24 (0.9) | 6.1 | 24.4 (16.0-35.7) |
| Chronic respiratory disease | 77 (3.0) | 28.4 | 31.7 (25.2-39.4) | 145 (5.5) | 36.6 | 48.5 (41.1-56.9) |
| Digestive system | 102 (4.0) | 37.6 | 14.1 (11.6-17.0) | 85 (3.6) | 21.4 | 17.8 (14.3-21.9) |
| Cirrhosis and alcoholic liver disease | 62 (2.4) | 22.9 | 14.6 (11.3-18.6) | 39 (1.5) | 9.8 | 17.0 (12.3-23.0) |
| Cancers | 255 (10.0) | 94.1 | 8.9 (7.9-10.0) | 281 (10.6) | 70.9 | 8.5 (7.5-9.5) |
Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research data with age, sex, and race/ethnicity standardized to nonfatal opioid overdose cohort.
Patient Age and Risks of Death
Substance use–associated diseases, nearly all of which were drug use–associated (rather than associated with alcohol use), were the leading causes of death in all 3 age groups (Table 4). The percentage of deaths because of substance use–associated diseases declined with age from the youngest age group (n = 290 of 692; 41.9%) to the middle age group (n = 461 of 1299; 35.5%) and oldest age group (n = 612 of 3203; 19.1%), although even in the youngest group most deaths were not because of substance use–associated diseases.
Table 4. All Causes and Selected Causes of Crude Mortality Rate Ratios and Standardized Mortality Ratios for Adult Medicaid Patients During the First Year After a Nonfatal Opioid Overdose, Stratified by Age Group.
| Cause of Death | Patients Aged 18-34 y | Patients Aged 35-44 y | Patients Aged 45-64 y | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Standardized Mortality Ratio (95% CI)a | Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Standardized Mortality Ratio (95% CI)a | Observed Deaths, No. (%) | Crude Mortality Rate per 10 000 Person-Years | Standardized Mortality Ratio (95% CI)a | |
| All causes | 692 (100) | 341.6 | 39.1 (36.3-42.1) |
1299 (100) | 672.3 | 33.5 (31.7-35.3) |
3203 (100) | 1179.5 | 20.7 (20.0-21.5) |
| External causes | 82 (11.8) | 40.5 | 10.1 (9.1-12.5) |
101 (7.8) | 52.3 | 12.3 (10.1-14.9) |
165 (5.2) | 60.8 | 14.3 (12.2-16.6) |
| Suicide | 40 (5.8) | 19.7 | 22.0 (15.9-26.3) |
75 (5.8) | 38.8 | 27.6 (21.8-34.4) |
100 (3.1) | 36.8 | 26.3 (21.5-31.9) |
| Homicide | 10 (1.4) | 4.9 | 6.0 (3.0-10.7) |
3 (0.2) | 1.6 | 2.3 (0.6-6.3) |
11 (0.3) | 4.1 | 8.2 (4.3-14.3) |
| Unintentional injury | 32 (4.6) | 15.8 | 6.9 (4.8-9.6) |
23 (1.8) | 11.9 | 5.4 (3.5-8.0) |
54 (1.7) | 19.9 | 8.4 (6.4-10.9) |
| Substance use associated | 290 (41.9) | 143.2 | 137.8 (122.6-154.4) |
461 (35.5) | 238.6 | 92.2 (84.1-100.9) |
612 (19.1) | 225.4 | 68.1 (62.8-73.6) |
| Drug use associated | 289 (41.8) | 142.7 | 148.1 (131.8-165.9) |
444 (34.2) | 229.8 | 124.0 (112.9-136.0) |
567 (17.7) | 208.8 | 130.2 (119.8-141.3) |
| Alcohol use associated | 1 (0.1) | 0.5 | 6.5 (0.3-32.1) |
17 (1.3) | 8.8 | 12.0 (7.2-18.8) |
45 (1.4) | 16.6 | 9.7 (7.2-12.9) |
| Infectious | 23 (3.3) | 11.4 | 31.0 (20.1-45.8) |
107 (8.2) | 55.4 | 34.0 (28.0-40.9) |
184 (5.7) | 67.8 | 22.5 (19.4-25.9) |
| Viral hepatitis | 2 (0.3) | 1.0 | NA | 9 (0.7) | 4.7 | 40.3 (19.7-74.0) |
38 (1.2) | 14.0 | 27.8 (20.0-37.8) |
| HIV | 15 (2.2) | 7.4 | 67.7 (39.3-109.1) |
79 (6.1) | 40.9 | 54.3 (43.3-67.3) |
85 (2.7) | 31.3 | 37.9 (30.5-46.6) |
| Circulatory system | 39 (5.6) | 19.3 | 29.2 (21.0-39.5) |
139 (10.7) | 71.9 | 18.4 (15.5-21.7) |
511 (16.0) | 188.2 | 11.2 (10.3-12.2) |
| Respiratory system | 16 (2.3) | 7.9 | 47.4 (28.0-75.3) |
45 (3.5) | 23.3 | 38.3 (28.3-50.8) |
260 (8.1) | 95.7 | 30.5 (27.0-34.4) |
| Influenza and pneumonia | 6 (1.1) | 3.0 | 62.8 (25.4-130.6) |
11 (0.8) | 5.7 | 27.6 (14.5-48.0) |
36 (1.6) | 13.3 | 21.0 (14.9-28.8) |
| Chronic respiratory disease | 5 (0.7) | 2.5 | 61.7 (22.6-136.8) |
24 (1.8) | 12.4 | 56.8 (36.1-85.4) |
193 (6.0) | 71.1 | 40.3 (34.9-46.3) |
| Digestive system | 4 (0.6) | 2.0 | 13.8 (4.4-33.3) |
30 (2.3) | 15.5 | 13.9 (9.6-19.6) |
153 (4.8) | 56.3 | 16.4 (14.0-19.2) |
| Cirrhosis and alcoholic liver disease | 1 (0.1) | 0.5 | 16.6 (0.8-81.9) |
17 (1.3) | 8.8 | 14.0 (8.4-22.0) |
83 (2.6) | 30.6 | 16.1 (12.9-19.9) |
| Cancers | 20 (2.9) | 9.9 | 12.6 (7.9-19.1) |
71 (5.5) | 36.7 | 9.9 (7.8-12.4) |
445 (13.9) | 163.9 | 8.7 (7.9-9.5) |
Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research data with age, sex, and race/ethnicity standardized to nonfatal opioid overdose cohort.
All-cause SMRs significantly declined with increasing group age (age 18-34 years: SMR, 39.1 [95% CI, 36.3-42.1] vs age 35-44 years: SMR, 33.5 [95% CI, 31.7-35.3] vs age 45-64 years: SMR, 20.7 [95% CI, 20.0-21.5]). A similar pattern occurred for SMRs resulting from substance use–associated diseases (age 18-34 years: SMR, 137.8 [95% CI, 122.6-154.4] vs age 35-44 years: SMR, 92.2 [95% CI, 84.1-100.9] vs age 45-64 years: SMR, 68.1 [95% CI, 62.8-73.6]) and circulatory diseases (age 18-34 years: SMR, 29.2 [95% CI, 21.0-39.5] vs age 35-44 years: SMR, 18.4 [95% CI, 15.5-21.7] vs age 45-64 years: SMR, 11.2 [95% CI, 10.3-12.2]). The SMR for infectious disease was significantly higher for adults aged 35 to 44 years (SMR, 34.0 [95% CI, 28.0-40.9]) than for those aged 45 to 64 years (SMR, 22.5 [95% CI, 19.4-25.9]). For most other causes of death, however, the SMRs did not significantly differ across the 3 adult age groups.
Major Medical Comorbidities and Risks of Death
Most of the patients in the cohort (n = 61 030; 80.0%) were diagnosed with 1 or more medical conditions in the Elixhauser Comorbidity Index in the 180 days prior to their initial opioid overdose. The rate of all-cause mortality during the first year after overdose for those with these comorbidities was 871.2 per 10 000 person-years, more than twice as high as for patients with none of these medical diagnoses (416.8 per 10 000 person-years) (eTable in the Supplement). Although substance use–associated deaths accounted for nearly twice the percentage of deaths among patients with an Elixhauser Comorbidity Index score of 0 (n = 254 of 569; 44.6%) than with an index of at least 1 (n = 1109 of 4625; 24.0%; P < .001), substance use–associated SMRs for the 2 patient groups were similar (comorbidity of 0: SMR, 94.4 [95% CI, 83.3-106.5] vs comorbidity ≥1: SMR, 84.6 [95% CI, 79.7-89.7]). For several causes of death, including cancer, digestive, respiratory, circulatory, and infectious diseases, the crude rates and SMRs were significantly higher for patients with Elixhauser Comorbidity Index score of at least 1 than those with a score of 0 (eTable in the Supplement). The suicide SMR after nonfatal opioid overdose was particularly elevated among adults with Elixhauser Comorbidity Index score of 1 or more (SMR, 119.2 [95% CI, 102.8-137.6]) compared with adults with a score of 0 (SMR, 21.6 [95% CI, 15.2-29.8]).
Discussion
In the year after nonfatal opioid overdose, patients died at approximately 24 times the rate of the general population. Although drug use–associated deaths accounted for a substantial share of these deaths, overdoses did not account for most of the deaths. Diseases of the circulatory system, cancer, respiratory system, and suicide also made important contributions to the excess deaths. The magnitude and pattern of the premature mortality, which varied by patient sex, background level of diagnosed medical conditions, and age group, have implications for the medical and behavioral health management of adults after nonfatal opioid overdose.
The overall increase in all-cause mortality during the first year after nonfatal overdose exceeded most prior estimates of mortality in cohorts of opioid-using or dependent adults. In a review3 of 27 opioid-dependent samples, the pooled all-cause SMR (14.7) was significantly less than the present all-cause SMR estimate (24.2). A high rate of mortality after nonfatal overdose is consistent with the view that underlying pulmonary, hepatic, cardiac, and other diseases can increase the risk of overdose in patients who use opioids.18
Patients with nonfatal opioid overdoses had a high subsequent risk of drug use–associated death. In the following year, their rate of drug use–associated death was more than 132 times greater than the corresponding rate in the standardized reference population. High rates of drug use–associated death were observed in men and women, in all 3 age groups, and in patients with and without recent major clinical medical diagnoses. Yet, in practice, after nonfatal opioid overdose, a substantial proportion of patients fill prescriptions for opioids15,19 and only a minority initiate medication-assisted treatment19 or engage in other substance use treatment.20 Beyond stabilizing patients after nonfatal opioid overdoses, clinicians in acute care settings have opportunities to initiate medication-assisted treatment and engage patients in ongoing medication-assisted treatment in primary care21 or through specialty addiction services.
In the year after opioid overdose, some of the subsequent mortality likely reflects known common health risk factors among patients with opioid use disorders. A high prevalence of cigarette smoking among people with substance use problems22 likely contributes to their high standardized mortality risks for respiratory diseases, circulatory diseases, and cancer. In addition, HIV risk behaviors, such as needle sharing and unsafe sexual behaviors, are also common among adults with substance use disorders,23 and the prevalence of HIV is elevated among adults with injection drug use.24 Hepatitis C virus is also highly prevalent among heroin and prescription-opioid users,25,26 and these patients frequently have problems adhering to hepatitis C medication regimens.27 In 1 study, 80% of patients in treatment for opioid dependence were positive for the hepatitis C antigen.26
The high medical disease burden of patients with overdoses underscores the importance of connecting these patients to continuing medical care after overdose. Yet challenges engaging patients with substance use disorders in primary care and a high prevalence of nonadherence with medical treatment frequently complicate delivery of primary care.28 In one study, more than one-third of all patients entering addiction treatment did not have a primary care physician.29 In another study, most patients received no primary care during the 2 years after inpatient detoxification.30 Such gaps may contribute to risk of mortality after a medically treated overdose occurs. Although it is unknown to what extent improved engagement in general medical care could reduce this toll, this is clearly a patient population with a high need for ongoing primary care as well as substance use treatment.
High risk of death from circulatory, respiratory, infectious, and other diseases after a nonfatal opioid overdose calls attention to the need to develop effective models of organizing and coordinating their primary care and substance use treatment. Research on the screening, brief intervention, referral, and treatment approach has generally yielded disappointing results31 as have efforts to enhance primary care with brief integrated drug use counseling services.32,33 More recently, several promising models have been developed for integrating medication-assisted treatment within primary care.34 Within Medicaid systems, 8 states are developing certified community behavioral health centers that aim to integrate mental health and substance use treatment.
After nonfatal overdose, men and especially women were also at exceptionally high risk of suicide. In a recent study of veterans, the association between opioid use disorder and suicide was also significantly stronger for women than men.6 In the present study, the rate of suicide during the first year after overdose for women (29.3 per 10 000 person-years) resembled the rate of suicide for women during the first year after deliberate self-harm (30.9 per 10 000 person-years).35 Although deliberate self harm and nonfatal overdose are distinct behaviors with different correlates and separate approaches to prevention, they can co-occur within an individual and careful clinical assessment may be necessary to distinguish them.36 A high risk of suicide after nonfatal opioid overdose underscores the importance of careful mental health assessment with appropriate follow-up for selected patients.37
Limitations
This study has several potential limitations. First, our study is based on data from 2001 through 2007. Since then opioid use, naloxone reversal, medication-assisted treatment, and other drug use patterns including risks associated with fentanyl-contaminated heroin38 have changed the composition of patients with opioid overdoses and may have changed their subsequent risks of death. Second, there is a potential for misclassification of causes of death that may vary by age. In older adults, for example, more frequent medical comorbidities and competing mortality risks may complicate detection of substance use–associated deaths39 and contribute to undercounting substance use–associated deaths in this age group. Third, many patients who overdose do not present for medical care.40 Fourth, different results might have been obtained if privately insured and uninsured patients with opioid overdoses were included in the analysis or if the follow-up period was extended for more than 1 year. Finally, the underlying risk of mortality among Medicaid enrollees likely differs from the standardized reference population. The reported standardized mortality rate ratios would likely be attenuated by adjustment for poverty associated with Medicaid eligibility; moreover, the level of attenuation might differ by sex and race/ethnicity because of disparities in poverty and disability.
Conclusions
In light of the recent increase in opioid-related inpatient admissions and emergency department visits in the United States,1 there is increased clinical and public health urgency to understanding and addressing the medical and behavioral health care needs of these patients. Adults who survive an opioid overdose are at high risk of dying in the year after the incident, not only from drug use–associated causes but also from suicide and a wide range of general medical diseases. The magnitude of this loss of life and variety of medical diseases that contribute to these excess deaths underscores the medical frailty of these patients and emphasizes the importance of coordinating addiction treatment, general medical services, and mental health care after opioid overdose.
eAppendix 1. ICD-10 Codes – Selected Causes of Death Groups.
eAppendix 2. Diseases and ICD-9-CM Codes included in Elixhauser Comorbidity Index.
eTable. All causes and selected causes of crude mortality rates and standardized mortality ratios for adult Medicaid patients during the first year following a nonfatal opioid overdose by low or moderate to high Elixhauser comorbidity score.
References
- 1.Weiss AJ, Elixhauser A, Barret ML, Steiner CA, Bailer MK, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009-2014; Statistical Brief 219. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.jsp. Published December 2016. Accessed May 11, 2018.
- 2.Pierce M, Bird SM, Hickman M, Millar T. National record linkage study of mortality for a large cohort of opioid users ascertained by drug treatment or criminal justice sources in England, 2005-2009. Drug Alcohol Depend. 2015;146:17-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106(1):32-51. [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, Larney S, Randall D, Burns L, Hall W. Causes of death in a cohort treated for opioid dependence between 1985 and 2005. Addiction. 2014;109(1):90-99. [DOI] [PubMed] [Google Scholar]
- 5.Bargagli AM, Hickman M, Davoli M, et al. ; COSMO European Group . Drug-related mortality and its impact on adult mortality in eight European countries. Eur J Public Health. 2006;16(2):198-202. [DOI] [PubMed] [Google Scholar]
- 6.Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112(7):1193-1201. [DOI] [PubMed] [Google Scholar]
- 7.Larney S, Randall D, Gibson A, Degenhardt L. The contributions of viral hepatitis and alcohol to liver-related deaths in opioid-dependent people. Drug Alcohol Depend. 2013;131(3):252-257. [DOI] [PubMed] [Google Scholar]
- 8.Gibson A, Randall D, Degenhardt L. The increasing mortality burden of liver disease among opioid-dependent people: cohort study. Addiction. 2011;106(12):2186-2192. [DOI] [PubMed] [Google Scholar]
- 9.Randall D, Degenhardt L, Vajdic CM, et al. Increasing cancer mortality among opioid-dependent persons in Australia: a new public health challenge for a disadvantaged population. Aust N Z J Public Health. 2011;35(3):220-225. [DOI] [PubMed] [Google Scholar]
- 10.Risser D, Hönigschnabl S, Stichenwirth M, et al. Mortality of opiate users in Vienna, Austria. Drug Alcohol Depend. 2001;64(3):251-256. [DOI] [PubMed] [Google Scholar]
- 11.Stoové MA, Dietze PM, Jolley D. Overdose deaths following previous non-fatal heroin overdose: record linkage of ambulance attendance and death registry data. Drug Alcohol Rev. 2009;28(4):347-352. [DOI] [PubMed] [Google Scholar]
- 12.Chermack ST, Bohnert ASB, Price AM, Austin K, Ilgen MA. Substance use disorders and homicide death in veterans. J Stud Alcohol Drugs. 2012;73(1):10-14. [DOI] [PubMed] [Google Scholar]
- 13.Wojcik NC, Huebner WW, Jorgensen G. Strategies for using the National Death Index and the Social Security Administration for death ascertainment in large occupational cohort mortality studies. Am J Epidemiol. 2010;172(4):469-477. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention . About underlying cause of death, 1999-2016. https://wonder.cdc.gov/ucd-icd10.html. Published December 20, 2017. Accessed May 11, 2018.
- 15.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1-9. [DOI] [PubMed] [Google Scholar]
- 16.Chu YT, Ng YY, Wu SC. Comparison of different comorbidity measures for use with administrative data in predicting short- and long-term mortality. BMC Health Serv Res. 2010;10:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. [DOI] [PubMed] [Google Scholar]
- 18.Zedler BK, Waunderes WB, Joyce AR, Vick CC, Murrelle EL. Validation of a screening risk index for serious prescription opioid-induced respiratory depression or overdose in a US commercial health plan claims database. Pain Med. 2018;19(1):68-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frazier W, Cochran G, Lo-Ciganic WH, et al. Medication-assisted treatment and opioid use before and after overdose in Pennsylvania Medicaid. JAMA. 2017;318(8):750-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naeger S, Mutter R, Ali MM, Mark T, Hughey L. Post-discharge treatment engagement among patients with an opioid-use disorder. J Subst Abuse Treat. 2016;69:64-71. [DOI] [PubMed] [Google Scholar]
- 21.D’Onofrio G, Chawarski MC, O’Connor PG, et al. Emergency department–initiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660-666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stanton CA, Keith DR, Gaalema DE, et al. Trends in tobacco use among US adults with chronic health conditions: National Survey on Drug Use and Health 2005-2013. Prev Med. 2016;92:160-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelley JL, Petry NM. HIV risk behaviors in male substance abusers with and without antisocial personality disorder. J Subst Abuse Treat. 2000;19(1):59-66. [DOI] [PubMed] [Google Scholar]
- 24.Murrill CS, Weeks H, Castrucci BC, et al. Age-specific seroprevalence of HIV, hepatitis B virus, and hepatitis C virus infection among injection drug users admitted to drug treatment in 6 US cities. Am J Public Health. 2002;92(3):385-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy E, Arruda N, Bourgois P. The growing popularity of prescription opioid injection in downtown Montréal: new challenges for harm reduction. Subst Use Misuse. 2011;46(9):1142-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gombas W, Fischer G, Jagsch R, et al. Prevalence and distribution of hepatitis C subtypes in patients with opioid dependence. Eur Addict Res. 2000;6(4):198-204. [DOI] [PubMed] [Google Scholar]
- 27.Belfiori B, Chiodera A, Ciliegi P, et al. Treatment for hepatitis C virus in injection drug users on opioid replacement therapy: a prospective multicentre study. Eur J Gastroenterol Hepatol. 2007;19(8):731-732. [DOI] [PubMed] [Google Scholar]
- 28.Rogal SS, McCarthy R, Reid A, et al. Primary care and hepatology provider–perceived barriers to and facilitators of hepatitis C treatment candidacy and adherence. Dig Dis Sci. 2017;62(8):1933-1943. [DOI] [PubMed] [Google Scholar]
- 29.Saitz R, Mulvey KP, Samet JH. The substance-abusing patient and primary care: linkage via the addiction treatment system? Subst Abus. 1997;18:187-195. [Google Scholar]
- 30.Saitz R, Larson MJ, Horton NJ, Winter M, Samet JH. Linkage with primary medical care in a prospective cohort of adults with addictions in inpatient detoxification: room for improvement. Health Serv Res. 2004;39(3):587-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glass JE, Hamilton AM, Powell BJ, Perron BE, Brown RT, Ilgen MA. Specialty substance use disorder services following brief alcohol intervention: a meta-analysis of randomized controlled trials. Addiction. 2015;110(9):1404-1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312(5):492-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saitz R, Palfai TPA, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;412(5):502-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Korthuis PT, McCarty D, Weimer M, et al. Primary care-based models for the treatment of opioid use disorder: a scoping review. Ann Intern Med. 2017;166(4):268-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174(8):765-774. [DOI] [PubMed] [Google Scholar]
- 36.Maloney E, Degenhardt L, Darke S, Nelson EC. Are non-fatal opioid overdoses misclassified suicide attempts? Comparing the associated correlates. Addict Behav. 2009;34(9):723-729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oqueno M. Opioid use disorders and suicide: a hidden tragedy. National Institute on Drug Abuse Blog. https://www.drugabuse.gov/about-nida/noras-blog/2017/04/opioid-use-disorders-suicide-hidden-tragedy-guest-blog. Published April 20, 2017. Accessed May 11, 2018.
- 38.Peterson AB, Gladden RM, Delcher C, et al. Increases in fentanyl-related overdose deaths - Florida and Ohio, 2013-2015. MMWR Morb Mortal Wkly Rep. 2016;65(33):844-849. [DOI] [PubMed] [Google Scholar]
- 39.Ødegård E, Amundsen EJ, Kielland KB. Fatal overdoses and deaths by other causes in a cohort of Norwegian drug abusers–a competing risk approach. Drug Alcohol Depend. 2007;89(2-3):176-182. [DOI] [PubMed] [Google Scholar]
- 40.Merchant RC, Schwartzapfel BL, Wolf FA, Li W, Carlson L, Rich JD. Demographic, geographic, and temporal patterns of ambulance runs for suspected opiate overdose in Rhode Island, 1997-20021. Subst Use Misuse. 2006;41(9):1209-1226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. ICD-10 Codes – Selected Causes of Death Groups.
eAppendix 2. Diseases and ICD-9-CM Codes included in Elixhauser Comorbidity Index.
eTable. All causes and selected causes of crude mortality rates and standardized mortality ratios for adult Medicaid patients during the first year following a nonfatal opioid overdose by low or moderate to high Elixhauser comorbidity score.