Key Points
Question
Do electronic health record–delivered medication management tools with or without nurse-led medication education improve self-management and lower blood pressure at community health centers?
Findings
In this cluster randomized clinical trial of 794 patients with hypertension, electronic health record tools designed to support medication self-management improved medication reconciliation but may have worsened blood pressure. Electronic health record tools combined with nurse-led medication education were associated with lower blood pressure compared with electronic health record tools alone but had no effect on medication adherence or drug indication knowledge.
Meaning
This study highlights the importance of testing system-level changes for unintended effects and suggests that improving some aspects of medication self-management alone is not sufficient to improve hypertension control.
Abstract
Importance
Complex medication regimens pose self-management challenges, particularly among populations with low levels of health literacy.
Objective
To test medication management tools delivered through a commercial electronic health record (EHR) with and without a nurse-led education intervention.
Design, Setting, and Participants
This 3-group cluster randomized clinical trial was performed in community health centers in Chicago, Illinois. Participants included 794 patients with hypertension who self-reported using 3 or more medications concurrently (for any purpose). Data were collected from April 30, 2012, through February 29, 2016, and analyzed by intention to treat.
Interventions
Clinics were randomly assigned to to groups: electronic health record–based medication management tools (medication review sheets at visit check-in, lay medication information sheets printed after visits; EHR-alone group), EHR-based tools plus nurse-led medication management support (EHR plus education group), or usual care.
Main Outcomes and Measures
Outcomes at 12 months included systolic blood pressure (primary outcome), medication reconciliation, knowledge of drug indications, understanding of medication instructions and dosing, and self-reported medication adherence. Medication outcomes were assessed for all hypertension prescriptions, all prescriptions to treat chronic disease, and all medications.
Results
Among the 794 participants (68.6% women; mean [SD] age, 52.7 [9.6] years), systolic blood pressure at 12 months was greater in the EHR-alone group compared with the usual care group by 3.6 mm Hg (95% CI, 0.3 to 6.9 mm Hg). Systolic blood pressure in the EHR plus education group was not significantly lower compared with the usual care group (difference, −2.0 mm Hg; 95% CI, −5.2 to 1.3 mm Hg) but was lower compared with the EHR-alone group (−5.6 mm Hg; 95% CI, −8.8 to −2.4 mm Hg). At 12 months, hypertension medication reconciliation was improved in the EHR-alone group (adjusted odds ratio [OR], 1.8; 95% CI, 1.1 to 2.9) and the EHR plus education group (adjusted odds ratio [OR], 2.0; 95% CI, 1.3 to 3.3) compared with usual care. Understanding of medication instructions and dosing was greater in the EHR plus education group than the usual care group for hypertension medications (OR, 2.3; 95% CI, 1.1 to 4.8) and all medications combined (OR, 1.7; 95% CI, 1.0 to 2.8). Compared with usual care, the EHR tools alone and EHR plus education interventions did not improve hypertension medication adherence (OR, 0.9; 95% CI, 0.6-1.4 for both) or knowledge of chronic drug indications (OR for EHR tools alone, 1.0 [95% CI, 0.6 to 1.5] and OR for EHR plus education, 1.1 [95% CI, 0.7-1.7]).
Conclusions and Relevance
The study found that EHR tools in isolation improved medication reconciliation but worsened blood pressure. Combining these tools with nurse-led support suggested improved understanding of medication instructions and dosing but did not lower blood pressure compared with usual care.
Trial Registration
ClinicalTrials.gov identifier: NCT01578577
This cluster randomized clinical trial assesses medication management tools delivered through a commercial electronic health record (EHR) with and without a nurse-led education intervention vs usual care among patients with hypertension and complex drug regimens.
Introduction
Chronic health conditions often require complex medication regimens. However, many patients do not adhere to medication regimens, and nonpersistence is common. Some racial and ethnic minorities may be at increased risk for suboptimal behavior in terms of medication, including inadequate adherence and unintentional misuse.1,2 Complex regimens raise the risk of medication errors.3 Furthermore, patients and clinicians may not share a common understanding of which medications to use. Patients may inadvertently be out of agreement with their clinicians’ intended plan or may choose to discontinue taking medication without informing their clinicians, or the health care team may have made errors.4,5 These discrepancies are prevalent, particularly among individuals with low levels of health literacy.6,7
Medication therapy management support from nurses or pharmacists can improve self-management of multiple-drug regimens in some circumstances.8 However, the implementation of medication therapy management services using clinical staff is challenging to practices, whereas pharmacy-based services are often underused, and reimbursement is low. Less costly than individualized attention from clinicians would be use of electronic health records (EHRs) to deliver tools supporting self-management. We used a cluster randomized clinical trial to test medication management tools delivered through an EHR with and without a nurse-led educational intervention among patients with hypertension and complex medication regimens receiving care within a network of federally qualified health centers (FQHCs). We hypothesized that compared with usual care, either EHR-supported approach would improve systolic blood pressure and medication reconciliation, understanding, and adherence.
Methods
Study Design
The design of the Northwestern and Access Community Health Network Medication Education Study (NAMES) was previously reported.4 The approaches tested sought to overcome challenges in the execution of medical care plans, promote information exchange between clinicians and patients, and give patients knowledge and skills to successfully execute medication plans.4 The study protocol is found in Supplement 1. The institutional review board of Northwestern University, Chicago, Illinois, approved the study, and all participants provided written informed consent.
Setting
The study was conducted at 12 FQHCs in the Access Community Health Network in the Chicago area using a common EHR (EpicCare; Epic Systems Corporation). Because materials were in English, centers with predominantly non–English speaking patient populations were excluded.
Randomization
Health center–level interventions necessitated that the center was the unit of randomization. Centers were randomized in groups of 3 to (1) usual care (control), (2) EHR-based medication management tools alone (EHR alone), or (3) EHR tools plus nurse-led medication management education and support (EHR plus education). An individual not associated with the study randomized the first 3 health centers by manually selecting numbers concealed from view. Allocation was concealed until randomization was completed. Subsequent randomization rounds used a weighted randomization scheme to increase the likelihood that group sizes remained similar.4
Participants
We recruited participants from randomized health centers. Eligibility criteria were (1) 18 years or older; (2) self-report of 3 or more medications prescribed (for any purpose); (3) systolic blood pressure at enrollment of at least 130 mm Hg or diastolic blood pressure of at least 80 mm Hg with diabetes or systolic blood pressure of at least 135 mm Hg or diastolic blood pressure of at least 85 mm Hg without diabetes (the criteria for participants without diabetes was lowered by 5 mm Hg during the study); (4) a Mini-Cog examination score of at least 3 (scores range from 0-5, with lower scores indicating a greater chance of dementia)9; (5) self-report that no one else was responsible for administering medication; (6) no intention to change the source of care during the next year; and (7) ability to communicate in English. We used 2 recruitment strategies. First, we directly contacted patients with hypertension identified from EHR data who used 3 or more medications (physicians could indicate who should not be contacted). Second, we recruited from health center waiting rooms.
Outcomes and Measures
Participants had assessments at baseline and approximately 3, 6, and 12 months of follow-up. Baseline questions assessed sociodemographic characteristics, health conditions, and participant-reported outcomes. We used the Newest Vital Sign to group health literacy into categories of likely limited, possibly limited, and likely adequate.10 Systolic blood pressure, the primary outcome, was measured using an automated device (HEM-907XL; Omron) while seated quietly with the feet and back supported for 5 minutes before measurement. The mean of the second and third readings indicated the systolic blood pressure.4 Diabetes subgroup measures are in eMethods 1 in Supplement 2.
Medication reconciliation was assessed by physicians (blinded to group) directly comparing self-reported medications with the EHR active medication list from the same date. We classified medication lists as reconciled vs not reconciled for (1) antihypertensives, (2) all not-as-needed long-term prescription medications (not including nonsystemic medications), and (3) all medications, including as-needed and over-the-counter medications. Knowledge of medication indication was assessed by blinded physicians.11 Understanding of medication instructions and dosing was assessed by comparing medication prescription instructions to participants’ mock demonstration of how they take each medication by dose and frequency. We used binary classifications (full understanding of all medications in that category vs not) with the above 3 medication groups. Medication adherence was measured by self-report for each prescription medication using a 4-day assessment of pills taken and pills prescribed and classified as full adherence vs not for each medication class.12,13 Pill count was performed but not reported owing to excessive missing data. Additional information about the medication measures is provided in eMethods 2 in Supplement 2.
Health-related quality of life was measured using a modified version of the physical and mental health scores from the 12-Item Short Form Health Survey.14 Self-management engagement was assessed using the Patient Activation Measure.15,16
Interventions
The intervention for each participant lasted 1 year. Participants at health centers randomized to usual care received only study assessments.
EHR Tools
We implemented previously piloted EHR tools17 by incorporating them into health center workflows. Tools included medication lists whereby at registration, the EHR was triggered to print patients’ current medication lists, accompanied by plain-language instructions to (1) review medicines, (2) strike out medicines not taken, (3) identify whether medications were taken as described, (4) identify concerns about medications, and (5) add medicines or supplements not included on the list. A sample list is included in eFigure 1 in Supplement 2. We also created single-page, plain-language medication information sheets with content appropriately sequenced from a patient’s perspective (drug name, purpose, and benefit; how to take the medication and for how long; when to stop taking the medication and call your physician; when to call; and other information) (eFigure 2 in Supplement 2). Sheets were printed at checkout with after-visit summaries when 125 different common medications for chronic disease were ordered or refilled. The original content was developed by 2 pharmacists.17 Patients, physicians, and health literacy experts reviewed and revised the material.
EHR Tools Plus Nurse-Led Medication Therapy Management
Health centers in the EHR plus education group received the EHR tools. In addition, participants received a medication therapy management intervention from a nurse educator. The nurse educators reviewed the EHR medication lists and physician notes to identify potential medication errors (eg, duplicates, internal discrepancies) and identify areas for monitoring and follow-up. They then arranged medication counseling sessions in person at a health center or by telephone. Initial sessions included assessment of medication comprehension, review of the pattern of medication use, reconciliation with the EHR, assistance with regimen dosing consolidation when feasible, and development of a medication table for complex regimens. Nurses assessed adherence, patterns of improper use, and reasons for nonadherence. Teach back, a method to check understanding by asking someone to state in their own words what has been explained to them, was used to confirm understanding. Nurses also assessed patients’ knowledge of their chronic conditions, addressed misconceptions, and reinforced the role medications play in disease control.
During the intervention year, nurses conducted medication education and review after office visits. When new medications for chronic disease were prescribed, the nurses attempted to reach participants within 4 to 7 days to determine whether the new prescription(s) had been obtained, assess use, and identify any problems. Nurses proactively telephoned participants who had not returned within 3 months if the patient had uncontrolled hypertension or diabetes or within 6 months if chronic conditions were controlled. The nurses communicated with treating clinicians using EHR-based email, telephone, or pager to clarify questions, documenting the results of reviews in the EHR. Other nurse-initiated actions included refilling prescriptions, directing patients who need renewal of state medical assistance to appropriate staff, and facilitating return visits or referrals. These nurses were employed by the Access Community Health Network and funded by the study.4
Implementation Assessments
The EHR tools were enabled for intervention health centers by the Access Community Health Network information technology group. Study staff met operational leaders and medical assistants to review work flows and observed health centers periodically during the intervention period to determine whether medication lists and information sheets were being provided and to reinforce these work flows. Nurses logged successful and attempted participant contacts, time spent, and the nature of the contact.
Sample Size
Sample size was based on the primary study outcome, systolic blood pressure at 12 months. With a sample of 1260 participants completing the 12-month study (approximately 105 participants per health center), the trial would be able to detect a 4–mm Hg difference for pairwise comparisons of intervention groups to usual care across a range of SDs for systolic blood pressure with 80% power, 5% type I error, and a residual health center correlation (after accounting for baseline value) of 0.001. Study recruitment was slower and more labor intensive than anticipated. Actual recruitment was lower than this number, and as conducted, in the primary analysis the study had 80% power to detect a 4.8–mm Hg difference between the usual care group and one of the intervention groups.
Statistical Analysis
Analysis was by intention to treat. We used generalized linear mixed models with baseline values and the 3 study groups as fixed effects and health center–level random intercept effects. Models were run for continuous blood pressure measurement (adjusted mean differences reported) or for the dichotomous outcomes (odds ratios [ORs] reported). Examination for potential confounders revealed differences between study groups in multiple participant characteristics (Table 1). Furthermore, collinearity occurred among these characteristics. Including additional nonredundant potentially confounding variables in the mixed models did not lead to meaningful changes in the results. Accordingly, we report all models with baseline outcome variables and study group as covariates and health center–level random effects. In addition to examining overall intervention effects, we examined the effects within health literacy subgroups and tested for interactions between health literacy and intervention effects (eMethods 3 in Supplement 2).
Table 1. Baseline Characteristics of Study Groups.
| Characteristic | Total (N = 794) | Study Group | ||
|---|---|---|---|---|
| Usual Care (n = 254) | EHR Tools Alone (n = 262) | EHR Tools Plus Education (n = 278) | ||
| Age, mean (SD) | 52.7 (9.6) | 53.0 (9.5) | 53.6 (9.7) | 51.6 (9.5) |
| Female sex | 545 (68.6) | 183 (72.0) | 175 (66.8) | 187 (67.3) |
| Race/ethnicity | ||||
| Black, non-Hispanic | 692 (87.2) | 234 (92.1) | 243 (92.7) | 215 (77.3) |
| White, non-Hispanic | 28 (3.5) | 3 (1.2) | 7 (2.7) | 18 (6.5) |
| Hispanic | 37 (4.7) | 10 (3.9) | 4 (1.5) | 23 (8.3) |
| Other or did not disclose | 37 (4.7) | 7 (2.8) | 8 (3.1) | 22 (7.9) |
| Education | ||||
| Less than grade 12 | 252 (31.7) | 102 (40.2) | 84 (32.1) | 66 (23.7) |
| High school graduate or equivalent | 278 (35.0) | 84 (33.1) | 92 (35.1) | 102 (36.7) |
| Some college | 218 (27.5) | 61 (24.0) | 72 (27.5) | 85 (30.6) |
| College graduate or greater | 45 (5.7) | 7 (2.8) | 14 (5.3) | 24 (8.6) |
| Refused to answer | 1 (0.1) | 0 | 0 | 1 (0.4) |
| Health insurance | ||||
| Medicaid | 406 (51.1) | 129 (50.8) | 111 (42.4) | 166 (59.7) |
| Medicare | 159 (20.0) | 54 (21.3) | 54 (20.6) | 51 (18.3) |
| Commercial insurance | 89 (11.2) | 35 (13.8) | 31 (11.8) | 23 (8.3) |
| Self-pay, other, or did not disclose | 142 (17.9) | 45 (17.7) | 70 (26.7) | 27 (9.7) |
| Diabetes | 348 (43.8) | 130 (51.2) | 111 (42.4) | 107 (38.5) |
| No. of total medications, median (IQR) | 5 (4-6) | 5 (4-7) | 5 (4-6) | 5 (4-6) |
| Blood pressure, mean (SD), mm Hg | ||||
| Systolic | 145.2 (17.2) | 141.5 (15.9) | 148.6 (17.5) | 145.5 (17.5) |
| Diastolic | 88.5 (12.2) | 86.9 (12.0) | 89.1 (12.4) | 89.5 (12.1) |
| Health literacy | ||||
| Likely limited | 375 (47.2) | 145 (57.1) | 126 (48.1) | 104 (37.4) |
| Possibly limited | 263 (33.1) | 75 (29.5) | 90 (34.4) | 98 (35.3) |
| Adequate | 156 (19.6) | 34 (13.4) | 46 (17.6) | 76 (27.3) |
| Medications reconcileda | ||||
| Hypertension | 348 (44.0) | 91 (36.1) | 116 (44.4) | 141 (50.7) |
| All chronic condition medications | 170 (21.5) | 27 (10.7) | 69 (26.4) | 74 (26.6) |
| All medications | 64 (8.1) | 4 (1.6) | 29 (11.1) | 31 (11.2) |
| Knowledge of medication indicationa | ||||
| Hypertension medications | 562 (80.1) | 178 (77.7) | 186 (78.2) | 198 (84.3) |
| All medications for chronic conditions | 539 (70.5) | 171 (69.2) | 166 (65.6) | 202 (76.2) |
| All medications | 382 (48.2) | 117 (46.1) | 126 (48.1) | 139 (50.2) |
| Understanding of medication instructions and dosinga | ||||
| Hypertension medications | 570 (82.0) | 183 (81.0) | 199 (84.7) | 188 (80.3) |
| All medications for chronic conditions | 553 (73.4) | 178 (73.0) | 188 (75.5) | 187 (71.9) |
| All medications | 513 (65.3) | 154 (61.1) | 181 (69.9) | 178 (64.7) |
| Medication adherence (4-d recall)a | ||||
| Hypertension medications | 434 (61.7) | 140 (61.1) | 160 (67.2) | 134 (56.8) |
| All medications for chronic conditions | 404 (53.0) | 132 (53.4) | 148 (58.7) | 124 (47.0) |
Abbreviations: EHR, electronic health record; IQR, interquartile range.
Numbers do not always equal total number of participants in each arm in cases where no Access Community Health Network record was available (medication reconciliation), no patient-reported medications could be identified in the category, dosing instructions were not available, or owing to nonresponse.
Participants with complete baseline and 12-month data were included in the primary analysis. We used multiple imputation for missing 3- and 6-month blood pressure data.18 Exploratory post hoc analyses are described in eMethods 4 in Supplement 2. P < .05 indicated significance using the Wald χ2 test.
Results
Overview and Participant Characteristics
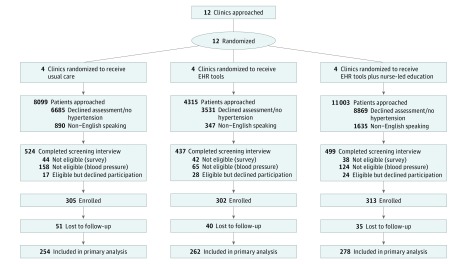
Participant recruitment and participation in the intervention occurred from April 30, 2012, through February 29, 2016. The trial was stopped as scheduled. Twelve health centers were randomized in 4 batches of 3 each, with 920 participants enrolled. Seven hundred ninety-four participants (86.3%) completed the 12-month follow-up visit and were included in the analysis (545 women [68.6%] and 249 men [31.4%]; mean [SD] age, 52.7 [9.6] years) (Figure 1). Most participants were black (692 [87.2%]) and had Medicaid insurance (406 [51.1%]). The median number of self-reported medications at baseline was 5 (interquartile range, 4-6), and 375 participants (47.2%) likely had limited health literacy (Table 1).
Figure 1. CONSORT Flow Diagram of the Northwestern and Access Community Health Network Medication Education Study.
EHR indicates electronic health record.
Blood Pressure Outcomes
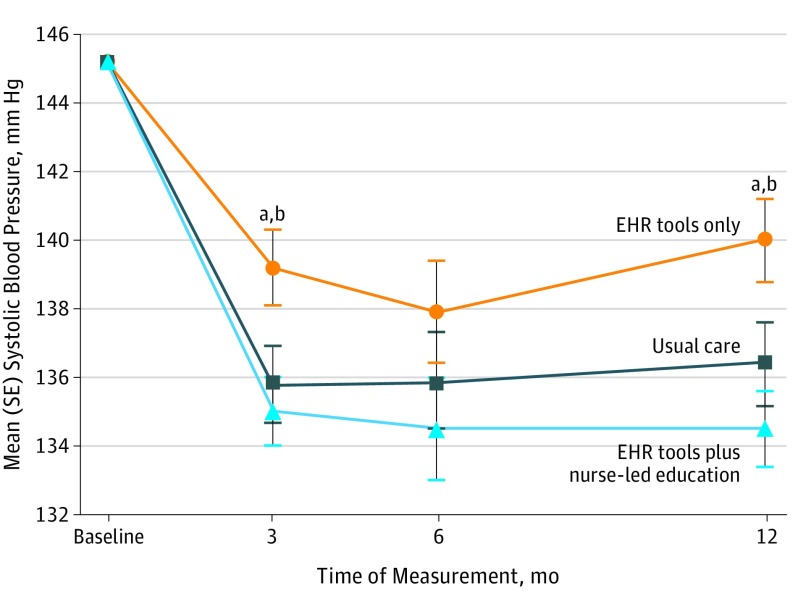
Systolic blood pressure at 12 months was greater in the EHR-alone group compared with usual care (adjusted mean difference, 3.6 mm Hg; 95% CI, 0.3 to 6.9 mm Hg; P = .03). Systolic blood pressure in the EHR plus education group was not significantly lower compared with usual care at 12 months (adjusted mean difference, −2.0 mm Hg; 95% CI, −5.2 to 1.3 mm Hg), but was significantly lower compared with the EHR-alone group (adjusted mean difference, −5.6 mm Hg; 95% CI, −8.8 to −2.4 mm Hg; P < .001). Additional blood pressure outcomes are given in Table 2 and Figure 2.
Table 2. Blood Pressure Outcomes by Study Group.
| Time of SBP Measurement | Usual Care (n = 254) | EHR Tools Alone (n = 262) | EHR Tools Alone vs Usual Care (n = 278) |
EHR Tools Plus Education | EHR Tools Plus Education vs Usual Care | EHR Tools Plus Education vs EHR Tools Alone | |||
|---|---|---|---|---|---|---|---|---|---|
| Adjusted Model Outcome (95% CI)a | P Value | Adjusted Model Outcome (95% CI)a | P Value | Adjusted Model Outcome (95% CI)a | P Value | ||||
| Mean (SD), mm Hg | |||||||||
| Baseline | 141.5 (15.9) | 148.6 (17.5) | NA | NA | 145.5 (17.5) | NA | NA | NA | NA |
| 3 mob | 133.5 (20.3) | 141.2 (20.5) | 3.3 (0.3 to 6.3) | .03 | 135.2 (19.9) | −0.9 (−3.8 to 2.1) | .57 | −4.2 (−7.1 to −1.2) | .005 |
| 6 moc | 134.2 (20.6) | 139.9 (21.1) | 2.1 (−2.0 to 6.2) | .31 | 134.8 (20.5) | −1.3 (−5.4 to 2.8) | .53 | −3.4 (−7.5 to 0.6) | .10 |
| 12 mod | 134.5 (20.4) | 141.7 (22.1) | 3.6 (0.3 to 6.9) | .03 | 134.6 (19.9) | −2.0 (−5.2 to 1.3) | .23 | −5.6 (−8.8 to −2.4) | <.001 |
| <140/90 mm Hg, % | |||||||||
| Baseline | 37.4 | 32.1 | NA | NA | 30.9 | NA | NA | NA | NA |
| 3 mob | 57.5 | 47.0 | 0.7 (0.5 to 0.97) | .04 | 58.3 | 1.1 (0.8 to 1.6) | .50 | 1.7 (1.2 to 2.4) | .005 |
| 6 moc | 56.7 | 52.3 | 0.9 (0.6 to 1.3) | .47 | 57.9 | 1.1 (0.8 to 1.6) | .50 | 1.3 (0.9 to 1.8) | .16 |
| 12 mo | 60.2 | 45.4 | 0.6 (0.4 to 0.8) | .002 | 61.2 | 1.1 (0.8 to 1.6) | .59 | 2.0 (1.4 to 2.8) | <.001 |
Abbreviations: EHR, electronic health record; NA, not applicable; SBP, systolic blood pressure.
Model for continuous SBP measurement is given as adjusted mean difference; for percentage of participants with SBP of less than 140/90 mm Hg, as adjusted odds ratio. All models contain baseline values for the outcome, study group, and health center–level random effects.
Includes 8.1% imputed values.
Includes 6.2% imputed values.
Indicates primary study outcome.
Figure 2. Model-Estimated Mean Systolic Blood Pressure by Study Group Over Time.
The model used included individuals’ baseline systolic blood pressure and health center–level random effects. As a result, baseline systolic blood pressure for comparison appears as the overall mean for all groups.
aP < .05 between groups receiving electronic health record (EHR) tools alone and usual care.
bP < .05 between groups receiving EHR tools alone and EHR tools plus nurse-led education.
Medication Management and Other Outcomes
At 12 months, both EHR intervention groups had greater medication reconciliation compared with the usual care group for hypertension medications (EHR-alone OR, 1.8 [95% CI, 1.1-2.9; P = .01]; EHR plus education OR, 2.0 [95% CI, 1.3-3.3; P = .003]) and all long-term medications (OR for both comparisons, 2.5; 95% CI, 1.2-5.2; P = .02). Reconciliation of all medications was greater in the EHR plus education group compared with the usual care group (OR, 6.0; 95% CI, 1.1-32.2; P = .04) (Table 3). Understanding of medication instructions and dosing was significantly greater in the EHR plus education group than in the usual care group for hypertension medications (OR, 2.3; 95% CI, 1.1-4.8; P = .03) and all medications combined (OR, 1.7; 95% CI, 1.0-2.9; P = .047). Knowledge of medication indication and medication adherence did not differ between groups. Comparisons for the 3- and 6-month points are in eTable 1 in Supplement 2; additional study outcomes, Patient Activation Measure, and health-related quality of life are in eTable 2 in Supplement 2. Among participants with diabetes (eTable 3 in Supplement 2), outcomes were better in the EHR plus education group compared with the EHR-alone group for hemoglobin A1c levels of 9% or less at 6 (OR, 2.0; 95% CI, 1.0-4.0; P = .03) and 12 months (OR, 2.3; 95% CI, 1.1-4.8; P = .02) and levels of less than 8% at 6 (OR, 2.1; 95% CI, 1.1-4.2; P = .03) and 12 months (OR, 2.4; 95% CI, 1.1-5.3; P = .03) (eTable 4 in Supplement 2). Reconciliation of diabetes medications was greater in the EHR plus education group compared with the usual care group at 12 months (OR, 2.6; 95% CI, 1.4-4.8; P = .002).
Table 3. Medication Management Outcomes at 12 Months by Study Groupa.
| Outcome | No. With Finding/Total No. (%) | EHR Tools Alone vs Usual Care | EHR Tools Plus Education Group, No. With Finding/Total No. (%) | EHR Tools Plus Education vs Usual Care | EHR Tools Plus Education vs EHR Tools Alone | ||||
|---|---|---|---|---|---|---|---|---|---|
| Usual Care Group | EHR Tools Alone Group | Adjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | ||
| Medications Reconciled | |||||||||
| Hypertension medications | |||||||||
| Baseline | 91/252 (36.1) | 116/261 (44.4) | NA | NA | 141/278 (50.7) | NA | NA | NA | NA |
| 12 mo | 91/252 (36.1) | 133/261 (51.0) | 1.8 (1.1-2.9) | .01 | 154/278 (55.4) | 2.0 (1.3-3.3) | .003 | 1.1 (0.7-1.8) | .62 |
| All mediations for chronic conditions | |||||||||
| Baseline | 27/252 (10.7) | 69/261 (26.4) | NA | NA | 74/278 (26.6) | NA | NA | NA | NA |
| 12 mo | 30/252 (11.9) | 72/261 (27.6) | 2.5 (1.2-5.2) | .02 | 71/278 (25.5) | 2.5 (1.2-5.2) | .02 | 1.0 (0.5-2.0) | .98 |
| All medications | |||||||||
| Baseline | 4/252 (1.6) | 29/261 (11.1) | NA | NA | 31/278 (11.2) | NA | NA | NA | NA |
| 12 mo | 4/252 (1.6) | 18/261 (6.9) | 4.0 (0.7-22.2) | .11 | 21/278 (7.6) | 6.0 (1.1-32.3) | .04 | 1.5 (0.4-6.1) | .58 |
| Knowledge of Medication Indication | |||||||||
| Hypertension medications | |||||||||
| Baseline | 178/229 (77.7) | 186/238 (78.2) | NA | NA | 198/235 (84.3) | NA | NA | NA | NA |
| 12 mo | 194/240 (80.8) | 212/255 (83.1) | 1.3 (0.8-2.4) | .32 | 233/267 (87.3) | 1.4 (0.8-2.5) | .30 | 1.0 (0.6-1.9) | .95 |
| All medications for chronic conditions | |||||||||
| Baseline | 171/247 (69.2) | 166/253 (65.6) | NA | NA | 202/265 (76.2) | NA | NA | NA | NA |
| 12 mo | 177/250 (70.8) | 175/259 (67.6) | 1.0 (0.6-1.5) | .82 | 209/277 (75.5) | 1.1 (0.7-1.7) | .69 | 1.2 (0.7-1.8) | .53 |
| All medications | |||||||||
| Baseline | 117/254 (46.1) | 126/262 (48.1) | NA | NA | 139/277 (50.2) | NA | NA | NA | NA |
| 12 mo | 137/253 (54.2) | 149/261 (57.1) | 1.1 (0.6-2.0) | .71 | 176/277 (63.5) | 1.3 (0.7-2.4) | .34 | 1.2 (0.6-2.2) | .57 |
| Understanding of Medication Instructions and Dosing | |||||||||
| All medications for hypertension | |||||||||
| Baseline | 183/226 (81.0) | 199/235 (84.7) | NA | NA | 188/234 (80.3) | NA | NA | NA | NA |
| 12 mo | 177/238 (74.4) | 200/255 (78.4) | 1.3 (0.6-2.5) | .53 | 225/264 (85.2) | 2.3 (1.1-4.8) | .03 | 1.8 (0.9-3.9) | .11 |
| All medications for chronic conditions | |||||||||
| Baseline | 178/244 (73.0) | 188/249 (75.5) | NA | NA | 187/260 (71.9) | NA | NA | NA | NA |
| 12 mo | 158/248 (63.7) | 180/261 (69.0) | 1.2 (0.7-2.0) | .47 | 201/275 (73.1) | 1.7 (1.0-2.8) | .05 | 1.4 (0.8-2.3) | .22 |
| All medications | |||||||||
| Baseline | 154/252 (61.1) | 181/259 (69.9) | NA | NA | 178/275 (64.7) | NA | NA | NA | NA |
| 12 mo | 143/253 (56.5) | 164/261 (62.8) | 1.2 (0.7-2.0) | .54 | 186/276 (67.4) | 1.7 (1.0-2.9) | .047 | 1.5 (0.9-2.5) | .17 |
| Medication Adherence, 4-d Recall | |||||||||
| Hypertension medications | |||||||||
| Baseline | 140/229 (61.1) | 160/238 (67.2) | NA | NA | 134/236 (56.8) | NA | NA | NA | NA |
| 12 mo | 178/239 (74.5) | 189/256 (73.8) | 0.9 (0.6-1.4) | .64 | 191/267 (71.5) | 0.9 (0.6-1.4) | .59 | 1.0 (0.6-1.5) | .94 |
| All medications for chronic conditions | |||||||||
| Baseline | 132/247 (53.4) | 148/252 (58.7) | NA | NA | 124/264 (47.0) | NA | NA | NA | NA |
| 12 mo | 159/249 (63.9) | 160/261 (61.3) | 0.8 (0.6-1.2) | .34 | 164/277 (59.2) | 0.8 (0.6-1.2) | .33 | 1.0 (0.7-1.4) | .99 |
Abbreviations: EHR, electronic health record; NA, not applicable; OR, odds ratio.
Numbers do not always equal total number of participants in each arm in cases where no Access Community Health Network record was available (medication reconciliation), no patient-reported medications could be identified in the category, dosing instructions were not available, or owing to nonresponse. All models contain baseline values for the outcome, study group, and health center–level random effects.
Health Literacy Subgroups
The effects of the 2 different interventions on systolic blood pressure were most pronounced in the subgroup with likely limited health literacy (eTable 5 in Supplement 2). For this subgroup, EHR tools plus education resulted in significantly lower systolic blood pressure compared with EHR tools alone at 3 (adjusted mean difference, −5.2 mm Hg; 95% CI, −9.8 to −0.7 mm Hg; P = .02), 6 (adjusted mean difference, −5.0 mm Hg; 95% CI, −10.0 to −0.1 mm Hg; P = .047), and 12 months (adjusted mean difference, −7.6 mm Hg; 95% CI, −13.2 to −2.1 mm Hg; P = .006). Formal testing revealed no significant interactions between health literacy and intervention effects for 12-month outcomes for systolic blood pressure, medication reconciliation, understanding of instructions and dosing, or other outcomes.
Implementation
We conducted 52 in-person process evaluations at sites using EHR tools. Printing medication review sheets at check-in was observed for 286 of 298 patient visits (96.0%) and 46 of 50 evaluations (92.0%). We observed sheets handed out at 235 of 292 patient visits (80.5%) and at 44 of 50 evaluations (88.0%). We observed medication information sheets printed for 212 of 214 patient visits (99.1%) and at 46 of 47 evaluations (97.9%) and handed out at 196 of 200 patient visits (98.0%) and 45 of 47 evaluations (95.7%).
Among participants receiving EHR tools plus education, a nurse was unable to conduct one-on-one education for 37 (13.3%). Eighty-six participants (30.9%) completed 1 educational session; 58 (20.9%), 2; 51 (18.3%), 3; 19 (6.8%), 4; and 27 (9.7%), 5 or more. Delivery of the nurse education intervention cost approximately $55 per patient in 2015 US dollars.
Exploratory Analysis
Post hoc analyses examining changes in number of hypertension medications did not show differences by group. The median change was zero in each group (eTable 6 in Supplement 2). Changes in the number of antihypertension medications did not attenuate the associations between systolic blood pressure at 12 months and study group (eTable 7 in Supplement 2).
Discussion
In this 3-group cluster randomized clinical trial, we evaluated the effectiveness of EHR tools with and without nurse-led medication self-management education among patients with hypertension and complex drug regimens at FQHCs. At 12 months, the EHR-alone group had the highest systolic blood pressure, and the EHR plus education group had the lowest. Both interventions improved medication reconciliation compared with usual care. Participants who received the EHR tools plus nurse-led education demonstrated more frequent correct understanding of medication instructions and dosing for several measures compared with usual care. These interventions had no meaningful effect on knowledge of medication indications or self-reported adherence.
Several explanations for these findings may apply. First, the interventions tested may have been too low intensity to lower blood pressure. Modest improvement in medication reconciliation does not mean that patients received more intensive treatment. Other interventions to improve medication reconciliation commonly detected medication discrepancies while yielding limited evidence of improved clinical outcomes.19 The nurse intervention we tested along with EHR tools appeared to improve understanding of proper medication self-administration as well as medication reconciliation, but medication adherence was unchanged and blood pressure was not lowered compared with usual care. Prior interventions using nonphysician clinicians to address hypertension have generally been most effective when these clinicians were empowered to intensify treatment if blood pressure was uncontrolled.20,21,22 The nurse educators in our study focused on reducing medication errors and improving self-management and were not tasked with intensification of therapy. Empowering nurses to adjust medication based on home blood pressure measurements may yield stronger effects on blood pressure.
The finding of higher blood pressure among the group that received EHR tools alone was unexpected. We speculate that medication information sheets (which contain some information on adverse drug effects) may have led some patients to stop or reduce antihypertensive therapy. Medication review may have uncovered some cases where individuals were using duplicate medications. We did not observe significant differences in medication adherence or the number of hypertension medications used that directly support this speculation, but the measures may not have been precise enough to detect all changes, and some medications that patients could not identify at baseline may have been among hypertensive treatments discontinued but not accounted for.
Strengths and Limitations
Study strengths include the use of pragmatic interventions conducted in FQHCs and the testing of medication support interventions in a population where low levels of health literacy were prevalent. Several limitations that demonstrate the real-world challenges of delivering interventions in these settings should also be noted. First, the effects on medication self-management may have been small because nurse educators were not always able to engage participants as frequently as intended. A total of 30.9% participants had only 1 medication educational session with a nurse educator, and 13.3% had none. Other investigators23 have observed challenges with adherence to practice-based interventions in settings such as ours. Second, office visits were required for exposure to the EHR tools. Participants who rarely had health center visits had little opportunity for the tools to influence care. Third, study recruitment was smaller than originally intended, which decreased our ability to detect differences between groups. Fourth, to account for differences in participant characteristics at the different sites, we included site-level random effects and individuals’ baseline values for the outcome of interest in our models. Although we examined measured covariates for potential confounding, we cannot exclude the possibility of residual confounding owing to unmeasured factors. Fifth, the medication measures we used may be imprecise, and the self-reported measure may have overestimated medication adherence. Finally, conducting the study within 1 network of FQHCs and limiting the population to English speakers prevents us from knowing whether these findings are generalizable to other locations or to non-English speakers.
Conclusions
Implementing EHR tools to support medication self-management—printed medication lists at each visit and lay language information sheets—improved medication reconciliation but may have worsened blood pressure when used in isolation. This unexpected finding highlights the importance of testing system-level changes and checking for unintended effects. Combining EHR tools with nurse-led self-management education lowered blood pressure more than EHR tools alone and improved some measures of demonstrated understanding of medication instructions and dosing. Even with the combined intervention, self-administration errors, medication discrepancies, and incomplete adherence were common, leaving much room for improvement.
Trial Protocol.
eMethods 1. Diabetes Subgroup Analysis
eMethods 2. Additional Details Regarding Medication Measures
eMethods 3. Health Literacy Analyses
eMethods 4. Exploratory Analysis
eTable 1. Medication Management Outcomes at 3, 6, and 12 Months by Study Group
eTable 2. Additional Outcomes at 12 Months by Study Group
eTable 3. Baseline Characteristics Diabetes Subgroup
eTable 4. Laboratory and Medication Outcomes in the Diabetes Subgroup at 3, 6, and 12 Months by Study Group
eTable 5. Systolic Blood Pressure Differences by Study Group Stratified by Health Literacy
eTable 6. Exploratory Analysis Examining Changes in the Number of Hypertension Medications by Study Group
eTable 7. Model Adjusted Mean Difference in Systolic Blood Pressure at 12 Months by Study Group in Models With and Without Changes between Baseline and 12 Months in the Number of Antihypertensive Medications Used
eFigure 1. Sample Medication List Review Sheet
eFigure 2. Sample Medication Information Sheet
References
- 1.Adams AS, Uratsu C, Dyer W, et al. Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA Intern Med. 2013;173(1):54-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hargrove JL, Pate V, Casteel CH, et al. Antihypertensive adherence trajectories among older adults in the first year after initiation of therapy. Am J Hypertens. 2017;30(10):1015-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis TC, Wolf MS, Bass PF III, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145(12):887-894. [DOI] [PubMed] [Google Scholar]
- 4.Persell SD, Eder M, Friesema E, et al. EHR-based medication support and nurse-led medication therapy management: rationale and design for a three-arm clinic randomized trial. J Am Heart Assoc. 2013;2(5):e000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nassaralla CL, Naessens JM, Chaudhry R, Hansen MA, Scheitel SM. Implementation of a medication reconciliation process in an ambulatory internal medicine clinic. Qual Saf Health Care. 2007;16(2):90-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Persell SD, Osborn CY, Richard R, Skripkauskas S, Wolf MS. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22(11):1523-1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mackey LM, Doody C, Werner EL, Fullen B. Self-management skills in chronic disease management: what role does health literacy have? Med Decis Making. 2016;36(6):741-759. [DOI] [PubMed] [Google Scholar]
- 8.Viswanathan M, Kahwati LC, Golin CE, et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med. 2015;175(1):76-87. [DOI] [PubMed] [Google Scholar]
- 9.Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The Mini-Cog: a cognitive “vital signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021-1027. [DOI] [PubMed] [Google Scholar]
- 10.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Persell SD, Heiman HL, Weingart SN, et al. Understanding of drug indications by ambulatory care patients. Am J Health Syst Pharm. 2004;61(23):2523-2527. [DOI] [PubMed] [Google Scholar]
- 12.DeMasi RA, Graham NM, Tolson JM, et al. Correlation between self-reported adherence to highly active antiretroviral therapy (HAART) and virologic outcome. Adv Ther. 2001;18(4):163-173. [DOI] [PubMed] [Google Scholar]
- 13.Waite KR, Paasche-Orlow M, Rintamaki LS, Davis TC, Wolf MS. Literacy, social stigma, and HIV medication adherence. J Gen Intern Med. 2008;23(9):1367-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ware J, Kosinski M, Turner-Bowker DM, Gandek B. User’s Manual for the SF-12v2 Health Survey. Lincoln, RI: QualityMetric; 2007. [Google Scholar]
- 15.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4, pt 1):1005-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greene J, Hibbard JH. Why does patient activation matter? an examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Webb JR, Feinglass J, Makoul G, et al. Can electronic health records help improve patients’ understanding of medications? Am J Manag Care. 2010;16(12):919-922. [PMC free article] [PubMed] [Google Scholar]
- 18.Schafer JL. Analysis of Incomplete Multivariate Data. Boca Raton, FL: Chapman & Hall/CRC; 1997. [Google Scholar]
- 19.Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48(10):1298-1312. [DOI] [PubMed] [Google Scholar]
- 20.Proia KK, Thota AB, Njie GJ, et al. ; Community Preventive Services Task Force . Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014;47(1):86-99.24933494 [Google Scholar]
- 21.Tucker KL, Sheppard JP, Stevens R, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med. 2018;168(2):110-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129(20):2044-2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.
eMethods 1. Diabetes Subgroup Analysis
eMethods 2. Additional Details Regarding Medication Measures
eMethods 3. Health Literacy Analyses
eMethods 4. Exploratory Analysis
eTable 1. Medication Management Outcomes at 3, 6, and 12 Months by Study Group
eTable 2. Additional Outcomes at 12 Months by Study Group
eTable 3. Baseline Characteristics Diabetes Subgroup
eTable 4. Laboratory and Medication Outcomes in the Diabetes Subgroup at 3, 6, and 12 Months by Study Group
eTable 5. Systolic Blood Pressure Differences by Study Group Stratified by Health Literacy
eTable 6. Exploratory Analysis Examining Changes in the Number of Hypertension Medications by Study Group
eTable 7. Model Adjusted Mean Difference in Systolic Blood Pressure at 12 Months by Study Group in Models With and Without Changes between Baseline and 12 Months in the Number of Antihypertensive Medications Used
eFigure 1. Sample Medication List Review Sheet
eFigure 2. Sample Medication Information Sheet